Abstract
Background
Early percutaneous coronary intervention (PCI) is recommended for ST-segment elevation myocardial infarction (STEMI) treatment. Delays in time-to-PCI, kept within guideline recommendations, have seldom been investigated.
Objectives
The purpose of this study was to investigate the consequences of delay, due to system factors or hospital distance, for the time between last patient distress call and PCI.
Methods
Registry-based cohort study including times of first call to medical services, admission and PCI for patients admitted with STEMI in Copenhagen, Denmark (2014-2018). The main combined outcome included death, recurrent myocardial infarction, or heart failure estimated at 30 days and 1 year from event. Outcomes according to time from call to PCI (system delay) and door-to-balloon time were standardized to the STEMI population using multivariate logistic regression.
Results
In total, 1,822 STEMI patients (73.5% male, median age 63.3 years [Q1-Q3: 54.6-72.9 years]) called the emergency services ≤72 hours before PCI (1,735, ≤12 hours). The combined endpoint of 1-year cumulative incidence was 13.9% (166/1,196) for patients treated within 120 minutes of the call and 21.2% (89/420) for patients treated later. Standardized 30-day outcomes were 7.33% (95% CI: 5.41%-9.63%) for patients treated <60 minutes, and 11.1% (95% CI: 8.39%-14.2%) for patients treated >120 minutes.
Conclusions
The risk of recurrent myocardial infarction, death, and heart failure following PCI treatment of STEMI increases rapidly when delay exceeds 1 hour. This indicates a particular advantage of minimizing time from first contact to PCI.
Key words: PCI, STEMI, system delay, time-to-treatment
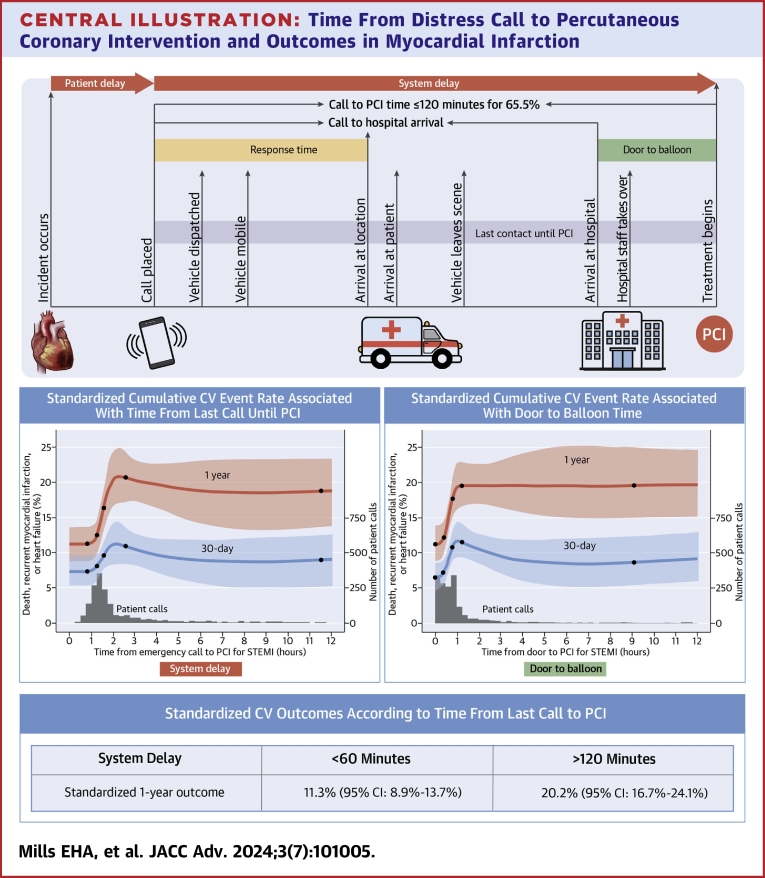
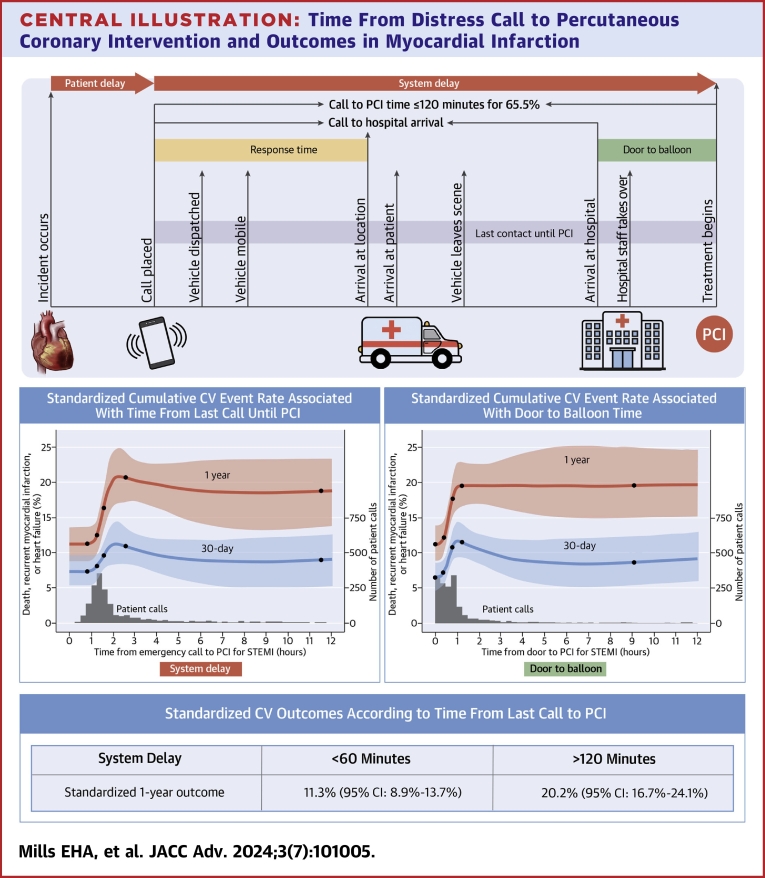
Central Illustration
The European Society of Cardiology’s treatment guidelines for ST-segment elevation myocardial infarction (STEMI) recommend that a primary percutaneous coronary intervention (PCI) be performed within 120 minutes of electrocardiographic diagnosis in the prehospital setting, within 60 minutes if diagnosed in hospital capable of primary PCI, or within 90 minutes if diagnosed in a hospital with no primary PCI. Primary PCI should be performed at least 12 hours after symptom onset.1 In a metanalysis of trials randomizing between PCI and fibrinolysis, the advantage of PCI was most marked when treatment was initiated within 60 minutes of hospital arrival.2 The problem of establishing a potential threshold from such an analysis is hampered by the many studies with varying definitions of and varying accuracy of establishing delay. For example, in a large study from Germany, mortality increased gradually with time from ambulance arrival until PCI.3 An advantage of keeping symptom to balloon time below 3 hours was demonstrated in a study from Japan.4 In addition, a study using gadolinium enhancement cardiac magnetic resonance imaging demonstrated increased necrosis when symptom to balloon time exceeded 120 minutes.5 Animal experiments indicate that necrosis occurs early following occlusion of a pericardial artery.6 These studies all indicate that time is an important factor in relation to minimizing adverse events, but studies have rarely examined times much shorter than guideline recommendations. It is therefore important to further examine the difference in clinical outcomes with increasing time delays, which can be accomplished in systems where times are recorded automatically and accurately.
The system in the Capital Region of Denmark has electronic recording of time of patient distress calls to health authorities, at the Copenhagen emergency medical services,7 providing a useful setting to examine in detail the consequences of delays. Furthermore, Copenhagen Emergency Medical Services records electrocardiograms in ambulances and helicopter services enabling telemedical diagnosis, triage, and direct transfer of STEMI patients to an invasive center, which shortens time until revascularization. The present study examines the consequences of delay, due to system factors or distance to hospital, for the time between last patient distress call and PCI.
Methods
Ethics
Registry-based studies do not require ethical approval or informed consent in Denmark.8 However, approval to use the data sources for research purposes was granted by the Capital Region of Denmark approval numbers P-2019-191 and 3-3013-2795/1.
Setting
The Capital Region of Denmark has approximately 1.8 million inhabitants. Most municipalities either have at least 1 city with more than 45,000 inhabitants or are within 30 minutes driving distance of a city of more than 45,000 inhabitants.9 In case of acute health conditions, patients may phone the Copenhagen emergency medical services, a prehospital emergency medical service that handles all emergency calls as well as out-of-hours telephone calls to health authorities within this region.7 The emergency medical service personnel also ensure that electrocardiograms are obtained in suspected cardiac cases and evaluated through telemedicine such that patients with signs of STEMI are taken directly to the Capital Region’s sole primary PCI center, where primary PCIs are intended to be performed. Excepting the island of Bornholm, the distance to the primary PCI center is mainly below 70 km. A study of out-of-hospital cardiac arrests found that the median distance to the invasive center for patients in the Capital Region of Denmark was 9 km.10
Population
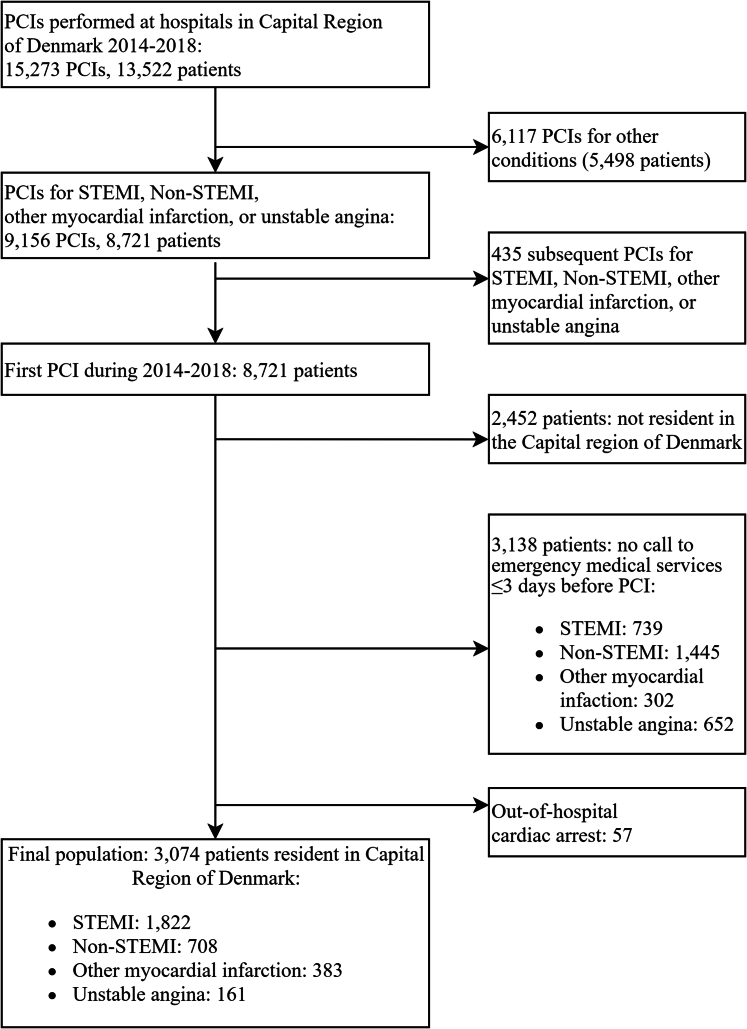
Patients were included in the study if they within the period of 2014 to 2018 had: 1) a PCI procedure performed (procedure code KFNG11); 2) a diagnosis of acute myocardial infarction (International Classification of Diseases-10th version code I21); 3) were resident in the Capital Region of Denmark; and 4) called Copenhagen emergency medical services for help by telephone up to 72 hours prior to the PCI. This study focused on STEMI patients only (I213, I210B, and I211B). Diagnosis codes are presented in Supplemental Table 1. Patients were only included once during the study period corresponding to the first PCI in the study period. Likewise, patients were excluded if registered in the Danish out-of-hospital cardiac arrest registry12 immediately prior to the PCI. Figure 1 shows the flowchart of patient inclusion, the final population included 1,822 patients.
Figure 1.
Flowchart of Patient Inclusion
Other myocardial infarction: International Classification of Diseases-10th version code I21 That is neither STEMI nor non-STEMI. PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction.
Data sources
In Denmark all residents are provided a civil person registration number which is used in all contacts with authorities and used in all Danish nationwide registers. This study used data from the prehospital emergency organization of Copenhagen. Date of birth and sex were obtained from the Danish Civil Registration System.13 International Classification of Diseases-10th version codes were obtained from the National Patient Registry.14 Redeemed prescriptions were obtained from the National prescription database.15 Data on PCI and the affected vessel from 2014 and 2015 were obtained from the East Danish Heart registry; additional years (2016-2018) were obtained from the National Patient Registry.14,16
Outcomes
The predefined primary outcome was the first occurrence of: 1) all-cause mortality; 2) rehospitalization with the main diagnosis of myocardial infarction; or 3) hospitalization with the primary diagnosis of heart failure. The primary outcome was evaluated both at 30 days and 1 year. Secondary outcomes were components of the primary outcome, that is: all-cause mortality, rehospitalization due to myocardial infarction or hospitalization due to heart failure at 30 days and 1 year. Date of death was obtained from the Danish registries of causes of death.17
Exposure and covariates
System delay was defined as the time from the start of the last electronically recorded telephone call within 72 hours to the prehospital emergency services and until the beginning of the PCI procedure. Guidelines accept different treatment delays of at most 2 (preferred for STEMI), 12 (maximum for STEMI), and 72 hours (non-STEMI). Based on the European Society of Cardiology’s clinical guidelines,1,18 boundaries of <120 minutes, 120 minutes to 6 hours, 6 to 12 hours, and 12 to 72 hours were used for grouped analyses. Door-to-balloon time was defined as the time from hospital arrival until the beginning of the PCI procedure. Ambulance response time was defined as the time from the patient’s call until the first medical contact1 with ambulance personnel.
Comorbidities included from the Danish National Patient register were prior PCI, ischemic heart disease, heart failure as primary or secondary diagnosis, kidney disease, chronic obstructive lung disease, hypertension, diabetes (glucose-lowering medication or diagnosis), peripheral vascular disease, cerebral transient ischemic attack, and stroke. Information on prior redemptions of antihypertensive medications and antidiabetic medication was obtained from the National Prescription database.15
Statistical analysis
Descriptive analysis was subdivided by groups of system delay. Summaries for continuous variables used the median, percentiles (25th, 75th), and the Kruskal-Wallis test, for categorical variables percentages, counts, and the chi-square test were used. Discretion rules from Statistic Denmark meant that cells with 3 or less individuals were shown as ≤3.19
The relation between time from symptoms to PCI and outcomes was examined by standardizing the outcomes to the covariate distribution for STEMI patients using multivariable logistic regression (G-formula).20 The covariates included in the model were age, sex, prior heart failure, prior myocardial infarction, diabetes, and chronic kidney disease. Time was included as a restricted cubic spline.21 The 95% CIs were estimated using 1,000 bootstraps. The covariates were prespecified prior to analysis. For the restricted cubic splines, the software selected default knots. The knots were used to select time points for which to display standardized outcome risks. Knots were placed using the rcspline.eval function in the R-package Hmisc, with 5 knots. The outer quantiles were placed at 0.05 and 0.95, with the remaining 3 knots equally spaced in between.22 The association between door-to-PCI time and outcomes was also explored for STEMI. As a sensitivity analysis, the same method as above was applied to non-STEMI, for the time interval of 0 to 72 hours to explore the association between time from call to PCI and outcomes, and to test the robustness of the model in relation to the result. Kaplan-Meier survival curves were also estimated. Data management and analysis was performed using R, version 4.0.3,23 in particular the Hmisc package, version 4.4-1 was used for splines.22
Results
This study included 1,822 patients with STEMI. Patient selection is shown in Figure 1 and demographic characteristics are presented in Table 1. The majority (73.5%) of STEMI patients were male, with a median age of 63.3 years (Q1-Q3: 54.6-72.9 years). The majority (99.3%) of PCIs were performed at Rigshospitalet (the main hospital and primary PCI center in the Capital Region of Denmark), the remaining PCIs were performed at hospitals in Herlev, Gentofte, or Hillerød. Most patients, 1,196 (65.6%) had a system delay of at most 120 minutes between call to health services and PCI. For the 1,735 patients treated within 12 hours, the median system delay was 92.7 minutes. Information concerning the affected vessel was available for 584 patients (2014-2015). Most (92.8%) had a culprit lesion in a single coronary artery; the remainder (7.2%) had 2 to 3 coronary arteries with culprit lesions. Affected arteries were left anterior descendant (43.2%), left main (1.5%), right (43.2%), and circumflex coronary artery (16.8%).
Table 1.
Characteristics for Patients With ST-Segment Elevation Myocardial Infarction and a Prior Call Within 72 Hours
| 0-120 min (n = 1,196) | 120 min to 6 h (n = 420) | 6-12 h (n = 119) | 12-72 h (n = 87) | Total (N = 1,822) | P Value | |
|---|---|---|---|---|---|---|
| Age (y) | 62.7 (54.1, 72.3) | 65.3 (55.6, 74.3) | 65.2 (53.5, 73.7) | 64.8 (56.6, 76.0) | 63.3 (54.6, 72.9) | 0.088 |
| Male | 899 (75.2) | 306 (72.9) | 80 (67.2) | 55 (63.2) | 1,340 (73.5) | 0.030 |
| PCI time of day | ||||||
| 8-16 | 558 (46.7) | 204 (48.6) | 84 (70.6) | 67 (77.0) | 913 (50.1) | |
| 16-24 | 421 (35.2) | 139 (33.1) | 23 (19.3) | 20 | NA | |
| 0-8 | 217 (18.1) | 77 (18.3) | 12 (10.1) | NA | <0.001 | |
| Year of PCI | ||||||
| 2014 | 205 (17.1) | 57 (13.6) | 10 (8.4) | 14 (16.1) | 286 (15.7) | |
| 2015 | 288 (24.1) | 88 (21.0) | 32 (26.9) | 22 (25.3) | 430 (23.6) | |
| 2016 | 245 (20.5) | 90 (21.4) | 52 (43.7) | 26 (29.9) | 413 (22.7) | |
| 2017 | 166 (13.9) | 117 (27.9) | 14 (11.8) | 11 (12.6) | 308 (16.9) | |
| 2018 | 292 (24.4) | 68 (16.2) | 11 (9.2) | 14 (16.1) | 385 (21.1) | <0.001 |
| EMS call type | ||||||
| 112 | 846 (70.7) | 242 (57.6) | 62 (52.1) | 39 (44.8) | 1,189 (65.3) | |
| 1,813 | 350 (29.3) | 178 (42.4) | 57 (47.9) | 48 (55.2) | 633 (34.7) | <0.001 |
| Response time (min) | 8.3 (6.4, 11.1) | 9.6 (7.0, 13.4) | 9.2 (7.3, 12.8) | 9.9 (7.5, 14.3) | 8.7 (6.6, 11.9) | <0.001 |
| Missing | 41 | 78 | 23 | 33 | 175 | |
| Call to hospital admission (min) | 42.9 (32.5, 57.3) | 68.6 (44.1, 111.3) | 55.5 (38.7, 145.5) | 129.6 (51.5, 271.9) | 48.2 (35.0, 68.2) | <0.001 |
| Missing | <4 | <4 | 0 | 0 | NA | |
| Door to PCI (min) | 33 (15, 49) | 97 (56.0, 152.8) | 412 (315.5, 505) | 1,183 (755.5, 1,907) | 47 (21, 82) | <0.001 |
| Missing | <4 | <4 | 0 | 0 | NA | |
| Prior heart failure | 52 (4.3) | 27 (6.4) | 4 (3.4) | 9 (10.3) | 92 (5.0) | 0.034 |
| Prior myocardial infarction | 131 (11.0) | 56 (13.3) | 8 (6.7) | 14 (16.1) | 209 (11.5) | 0.101 |
| Hypertension | 363 (30.4) | 146 (34.8) | 37 (31.1) | 38 (43.7) | 584 (32.1) | 0.037 |
| Peripheral vascular disease | 60 (5.0) | 22 (5.2) | 10 (8.4) | 6 (6.9) | 98 (5.4) | 0.414 |
| Cerebrovascular disease | 93 (7.8) | 49 (11.7) | 9 (7.6) | 9 (10.3) | 160 (8.8) | 0.095 |
| Diabetes | 141 (11.8) | 56 (13.3) | 17 (14.3) | 14 (16.1) | 228 (12.5) | 0.534 |
| Kidney disease | 32 (2.7) | 14 (3.3) | 0 (0.0) | <4 | NA | 0.246 |
| Liver disease | 22 (1.8) | 8 (1.9) | <4 | <4 | NA | 0.856 |
| Cancer | 122 (10.2) | 44 (10.5) | 13 (10.9) | 12 (13.8) | 191 (10.5) | 0.767 |
| Chronic pulmonary disease | 118 (9.9) | 42 (10.0) | 11 (9.2) | 18 (20.7) | 189 (10.4) | 0.015 |
| Peptic disease | 43 (3.6) | 24 (5.7) | 4 (3.4) | <4 | NA | 0.125 |
| Rheumatic disease | 36 (3.0) | 17 (4.0) | 8 (6.7) | 5 (5.7) | 66 (3.6) | 0.116 |
Values are median (1st, 3rd quartile), n (%), or n. Table data from Copenhagen in 2014 to 2018.
EMS = emergency medical services; NA = not available due to Statistics Denmark’s rule on avoiding the report of microdata from the research environment; PCI = percutaneous coronary intervention.
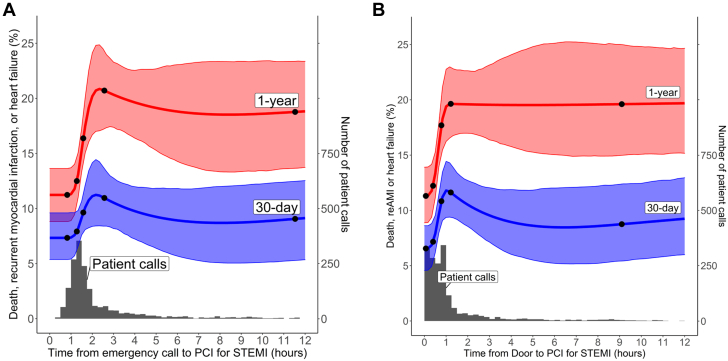
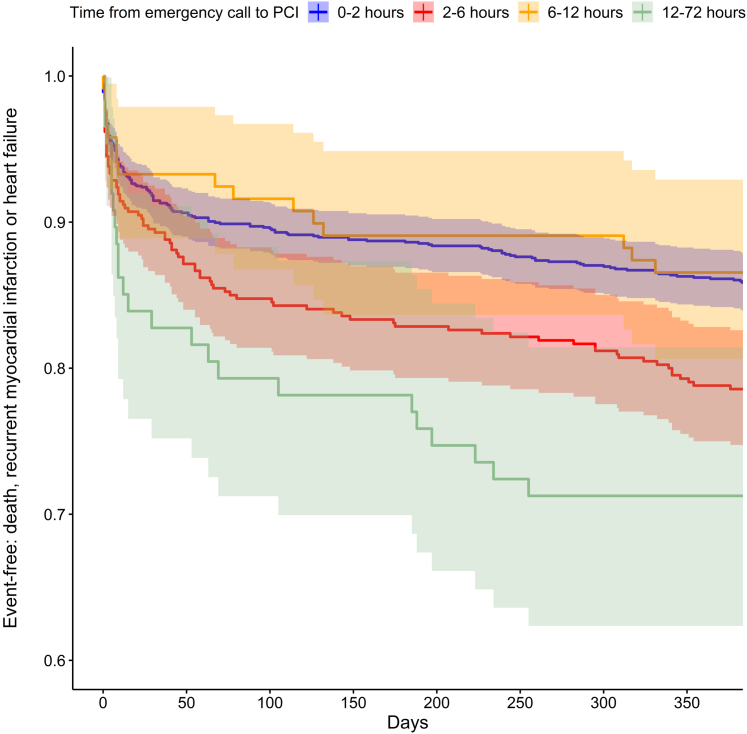
Overall, 9.3% of patients experienced a combined event (death, recurrent infarction, heart failure hospitalization) within 30 days, and 16.2% within 1 year (Table 2). Events within 1 year were 13.9% for the group with 0 to 120 minutes between call and PCI, 21.2% for 120 minutes to 6 hours system delay, 13.4% for 6 to 12 hours system delay, and 28.7% for 12 to 72 hours system delay. The most common component of the composite endpoint was heart failure admission within 1 year (7.8%). In the statistical analyses where risk of outcome was standardized to patients’ age, sex, and selected comorbidities, shorter times to treatment were associated with a lower risk of the composite outcome of death, recurrent infarction, and heart failure hospitalization both after 30 and 365 days (Figure 2A, Central Illustration, left). Risks of event rose sharply after 60 minutes. Standardized 1-year outcomes were 11.31% (95% CI: 8.9%-13.7%), 15.28% (95% CI: 13.33%-17.27%), 20.2% (95% CI: 16.7%-24.14%), 18.8% (95% CI: 14.28%-23.06%), and 18.83% (95% CI: 13.74%-23.36%) for 60, 90, and 120 minutes and 6, 12 hours system delay, respectively (Table 3). Similarly, for door-to-PCI times, event incidence rose sharply after 15 to 30 minutes (Figure 2B, Central Illustration, right). Kaplan-Meier survival estimates show similar results to Table 2 (Figure 3).
Table 2.
Patient Outcomes in ST-Segment Elevation Myocardial Infarction and a Prior Call Within 72 Hours
| System Delay Times (Call to PCI) |
|||||
|---|---|---|---|---|---|
| 0-120 min (n = 1,196) | 120 min to 6 h (n = 420) | 6-12 h (n = 119) | 12-72 h (n = 87) | Total (N = 1,822) | |
| Any event | |||||
| 30-d | 102 (8.5) | 44 (10.5) | 8 (6.7) | 15 (17.2) | 169 (9.3) |
| 1-y | 166 (13.9) | 89 (21.2) | 16 (13.4) | 25 (28.7) | 296 (16.2) |
| Recurrent infarction | |||||
| 30-d | 24 (2.0) | 7 (1.7) | <4 | 4 (4.6) | NA |
| 1-y | 49 (4.1) | 22 (5.2) | 5 (4.2) | 8 (9.2) | 84 (4.6) |
| Heart failure | |||||
| 30-d | 49 (4.1) | 22 (5.2) | 4 (3.4) | 5 (5.7) | 80 (4.4) |
| 1-y | 80 (6.7) | 46 (11.0) | 6 (5.0) | 11 (12.6) | 143 (7.8) |
| Mortality | |||||
| 30-d | 30 (2.5) | 19 (4.5) | <4 | 7 (8.0) | NA |
| 1-y | 50 (4.2) | 35 (8.3) | 7 (5.9) | 10 (11.5) | 102 (5.6) |
Figure 2.
System Delay, Door to Balloon Time and Standardized 30-Day and 1-Year Cumulative Event Rates
Standardized cumulative event rate and 95% confidence limits after 30 days and 1 year associated with (A) time from last contact and start of percutaneous coronary intervention (PCI), and (B) time of arrival at hospital door and start of PCI. Standardization was based on age, sex, prior diabetes/myocardial infarction/heart failure/chronic kidney disease, with the time from call to PCI time and time from door-to balloon changed for the entire population (N = 1,822). Also shown is the distribution of patients with time for (A) 1,735 patients with <12 hours between call and PCI, (B) 1,749 patients with <12 hours between hospital arrival and PCI. In both plots, the left y-axis is the cumulative event rate, and the right y-axis is the number of patients at each time point. The x-axis is the time for all curves and histograms. Black circles are knots for the restricted cubic splines. Knots in Figure 2A were at 49.3, 76.4, 94.6, 154, and 691.9 minutes. Knots in Figure 2B were at 4, 24, 47, 73, and 546 minutes.
Central Illustration.
Time From Distress Call to Percutaneous Coronary Intervention and Outcomes in Myocardial Infarction
Registry-based study with 1-year follow of 1,822 STEMI patients from the capital region of Denmark. System delay was measured from time of call until time of PCI. Outcomes were the risk of recurrent myocardial infarction, death and heart failure within 1 year. Outcomes were more frequent when system delay until PCI exceeds 1 hour. This indicates a particular advantage of minimizing time from first contact to PCI. Abbreviations as in Figure 1.
Table 3.
Absolute Risk (Percent) of Outcomes With System Delays of 60, 90, and 120 Minutes
| System Delay Times (Call to PCI) |
|||||
|---|---|---|---|---|---|
| 60 min | 90 min | 120 min | 6 h | 12 h | |
| Any event | |||||
| 30-d | 7.37 (5.43-9.62) | 9.17 (7.60-10.66) | 11.12 (8.39-14.17) | 8.93 (5.69-11.83) | 9.14 (5.35-12.54) |
| 1-y | 11.31 (8.90-13.7) | 15.28 (13.33-17.27) | 20.20 (16.70-24.14) | 18.81 (14.28-23.06) | 18.83 (13.74-23.36) |
| Recurrent infarction | |||||
| 30-d | 1.57 (0.73-2.65) | 2.09 (1.30-2.98) | 2.62 (1.29-4.52) | 1.34 (0.36-2.58) | 1.38 (0.24-2.99) |
| 1-y | 3.37 (2.13-4.69) | 4.40 (3.34-5.51) | 5.63 (3.92-8.00) | 4.72 (2.51-6.99) | 5.00 (2.28-7.90) |
| Heart failure | |||||
| 30-d | 3.80 (2.36-5.38) | 4.57 (3.44-5.75) | 5.28 (3.23-7.79) | 3.50 (1.61-5.64) | 3.53 (1.38-6.00) |
| 1-y | 5.49 (3.81-7.54) | 7.64 (6.16-9.16) | 10.33 (7.48-13.72) | 8.11 (5.16-11.13) | 7.98 (4.68-11.32) |
| Mortality | |||||
| 30-d | 1.99 (1.05-3.19) | 2.76 (1.94-3.68) | 3.87 (2.43-5.68) | 4.55 (2.55-6.83) | 4.51 (2.18-7.12) |
| 1-y | 3.21 (1.93-4.80) | 4.67 (3.55-5.90) | 6.82 (4.92-8.99) | 8.32 (5.45-11.57) | 7.93 (4.74-11.44) |
Values are estimate (95% CI).
Standardized outcome risks with covariates age, sex, prior heart failure, prior myocardial infarction, diabetes, and chronic kidney disease.
Abbreviations as in Table 1.
Figure 3.
Groups of System Delay and 1-Year Event-Free Survival
Kaplan-Meier curves for event-free survival up to 1 year subdivided by groups of system delay from emergency call to PCI. Abbreviation as in Figure 1.
As a sensitivity analysis comparison of 708 patients that received PCI for non-STEMI during the study period, 383 for unspecified myocardial infarction and 161 for unstable angina (Figure 1) was conducted. In these patients, events occurred within 30 days for 13.6% of unspecified myocardial infarctions, 7.3% of non-STEMIs, and 2.5% of unstable angina patients. Events within 1 year occurred for 19.1% of unspecified myocardial infarction patients, 16.5% of non-STEMI patients, and 7.5% of unstable angina patients. The analysis of non-STEMI did not indicate a clear association of outcome with time since last call to emergency medical services (Supplemental Figure 1).
Discussion
The main finding of this study was an increase in outcome beyond a threshold of 60 minutes system delay between the patient’s distress call and a PCI for STEMI. The risk of adverse events after 30 days and 1 year increased markedly after this delay and then leveled off. The times to PCI attained in the study were below maximal recommended guideline times of 120 minutes1 for 65.6% of individuals, a larger proportion compared to other studies.24
This study found that system delay below 60 minutes in STEMI was associated with improved outcome and showed how incremental increases above 60 minutes were associated with more adverse outcomes, even within guideline-recommended treatment times of 120 minutes of prehospital diagnosis. Previous studies comparing PCI with fibrinolysis found that if the door-to-needle time exceeded 60 to 120 minutes, PCI was no longer superior with regard to outcomes of death, recurrent infarction, or stroke.2,25,26 A systematic review of time to treatment in STEMI found that shorter symptom onset-to-balloon times were associated with improved outcomes.24 Compared to the present study, the studies included in the review had longer median times to treatment (minimum median of 113 minutes).24 A study of system delay for 6,209 patients undergoing primary PCI, with data from 2002 to 2008, found increases in mortality per whole hour, however the study had longer median system delay (97 minutes) than the present study (92.7 minutes), and field electrocardiograms were only fully implemented in the study period from 2006 onward.27 In a prospective study of in-hospital mortality, contact-to-treatment times below 90 minutes were associated with improved outcomes and in-hospital mortality was found to almost linearly increase from 60 to 180 minutes contact to PCI time.3 This finding was confirmed in the present study, with a clear threshold after 60 minutes system delay followed by a marked increase in adverse outcomes, both short-term and long-term, with longer call-to-PCI time. This is consistent with results of a study of long-term outcomes of stable patients with a persistent occlusion of a coronary artery treated with late PCI (3-28 days after MI) where no additional benefit was found for patients treated with PCI compared to those only treated medically.28
Many studies have focused on door-to-balloon times, where most of the studies found shorter times were associated with better outcomes. Door-to-balloon time does not account for the prehospital time for those transported with ambulance,29 and does not accurately reflect time since symptom onset. Park et al30 found door-to-balloon time to be important, with reductions of door-to-balloon time from 90 to 60 minutes associated with improved survival. However, Shiomi et al4 found that short door-to-balloon times in STEMI were only associated with improved survival if symptom onset-to-balloon time was likewise short, however symptom onset time was self-reported. A study by Roswell et al31 found that door-to-balloon times should be kept under 50 minutes to achieve first medical contact to device times below 90 minutes. Finally, De Luca et al32 found that time from symptom onset-to-balloon but not time from door-to-balloon was associated with mortality. The present study confirms these prior findings that symptom-to-balloon time is associated with improved outcomes but also gives an enhanced understanding of the importance of time to treatment, with an exposure time that better represents the heart’s biological ischemic time.
Including out-of-hospital time is important, as time from emergency call to balloon better represents the total myocardial ischemic time than door-to-balloon time. The difference between these time intervals may arise from considerable variations and delays in prehospital time due to differences in distance to nearest primary PCI hospital or time spent with resuscitation and stabilization after an out-of-hospital cardiac arrest or cardiogenic shock.3,33,34 Time to treatment may be divided into patient delay and system delay. Patient delay is time from symptoms until the patients choose to call for help. System delay being time from call to emergency medical services or other contact to the health care system until treatment. As patient delay is subjective and often difficult to change, system delay may more easily be influenced by changing the system.33,35 Patients with cardiac symptoms are less likely to delay seeking treatment than those without.36 For patients with no symptoms or atypical symptoms, time of symptom onset may be hard to determine and may be prone to recall bias.33
The results of the sensitivity analysis for non-STEMI were that longer system delay was not associated with worse outcomes, as has been shown in a meta-analysis of 8 randomized controlled trials that did not find benefits for shorter time to treatment for all non-STEMIs.37 Possibly, shorter system delay appears to have had more outcomes in the present study, which might be explained by treatment guidelines at the time indicating that unstable patients, or patients with a Global Registry of Acute Coronary Events score >140 (at risk of worse outcomes) should be treated within 24 hours using an early invasive strategy rather than be treated within 72 hours.18 Benefits of early invasive treatment have been found for patients with elevated biomarkers (troponin) and Global Registry of Acute Coronary Events scores above 140.37,38
A major strength of this study was the use of high-quality data from Danish registries, with more detailed information and no self-reported information. This minimizes loss to follow-up and selection bias which in turn increases generalizability to similar settings. The diagnosis of myocardial infarction has been validated in the Danish registries,39 enhancing the accuracy of the measurement. Another strength was that the exposure of time to PCI (system delay) incorporated prehospital time from when the patient called, which might be assumed to be shortly after time of symptom onset. Using an automatically collected time, recall bias with regard to time of symptom onset is avoided.
Study limitations
The study had some limitations. For instance, when individuals had longer time to PCI, for example, above 48 hours, using time of last call as proxy for symptom onset may be inaccurate as patients might have suffered from something else when they phoned, and only developed the myocardial infarction later, perhaps in-hospital. Additionally, the length of the patient delay was not available in the present study, which means the system delay in this study may underestimate the total symptom to balloon time. Furthermore, the study only includes patients treated with a PCI, that is, not considering angiographies leading directly to coronary artery bypass graft surgery, or STEMIs where PCI is not indicated. Clinical variables such as shock state were not available in the data. The patient also needs to have arrived at hospital to have PCI treatment, meaning immediate deaths after STEMI where resuscitation was unsuccessful or terminated are not included. The geography of the Capital Region of Denmark means the distance to PCI center is no longer than 70 km (excepting, eg, the island of Bornholm). This leads to shorter transport times and thus shorter system delay with improved outcomes accordingly. This could potentially influence the generalizability of the study. Finally, the observational nature of the study creates potential for unmeasured confounding.
Conclusions
The risk of recurrent myocardial infarction, death, and heart failure following PCI treatment of STEMI increased rapidly when system delay exceeds 1 hour. This indicates a particular advantage of minimizing time from first contact to PCI and aiming to keep it below 1 hour. Strategies to ensure rapid transport, diagnosis, and treatment are important for the outcome following STEMI. Investment in prehospital electrocardiograms and rapid transport directly to primary PCI centers is therefore important.
PERSPECTIVES.
COMPETENCY IN MEDICAL KNOWLEDGE: The risk of recurrent myocardial infarction, death, and heart failure following PCI treatment of STEMI increased rapidly when system delay exceeds 1 hour. This implication could further the discussion on clinical guidelines for time to treatment. Systems-Based Practice: Investment in prehospital electrocardiograms enabling prehospital diagnosis, enabling subsequent rapid transport directly to primary PCI centers is important.
TRANSLATIONAL OUTLOOK: The current findings were based on a Danish cohort, further research in an international setting is required to clarify the area. Challenges to such research include the implantation of similar electronic registries of both pre-hospital and in-hospital data as well as accurate collection of follow-up data.
Funding support and author disclosures
The work was supported by the Danish Heart Foundation. This organization had no influence on the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review, or approval of the manuscript. Dr Møller has received funding from Sygeforsikringen “danmark”. Dr Engstrøm received speaker’s fee from and is on advisory board of Abbott. Dr Folke has received NovoNordisk Research Grant NNF19OC0055142, Unrestricted Research Grant Laerdal Foundation; and teaches general practitioners resuscitation paid by AstraZeneca. Dr Køber has received speaker honorarium from AstraZeneca, Bayer, Boehringer, and Novartis. Dr Gnesin has a relationship with Danish Cardiovascular Academy-Novo Nordisk Foundation and Danish Heart Foundation. Dr Zylyftari has received funding from the European Union’s Horizon 2020 Research and Innovation Program European Sudden Cardiac Arrest Network Towards Prevention, Education, New Effective Treatment, the COST Action PARQ supported by European Cooperation in Science and Technology, and Helsefonden. Dr Kragholm has received grants from The Laerdal Foundation. Dr Lippert has received unrestricted research grants from the Danish TrygFoundation, Laerdal Foundation, and Novo Nordic Foundation. Dr Christensen has received funding from TrygFoundation, Laerdal, and Region Zealand Research fund. Dr Torp-Pedersen has received grants for randomized study and epidemiological study from Bayer and Novo Nordisk. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The authors would like to extend their gratitude toward Research Services at Statistics Denmark for their excellent help in relation to data accessibility.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a supplemental table and figure, please see the online version of this paper.
Supplementary data
References
- 1.Ibanez B., James S., Agewall S., et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society. Eur Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 2.Nallamothu B.K., Bates E.R. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol. 2003;92(7):824–826. doi: 10.1016/s0002-9149(03)00891-9. [DOI] [PubMed] [Google Scholar]
- 3.Scholz K.H., Maier S.K.G., Maier L.S., et al. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: results from the German prospective, multicentre FITT-STEMI trial. Eur Heart J. 2018;39(13):1065–1074. doi: 10.1093/eurheartj/ehy004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shiomi H., Nakagawa Y., Morimoto T., et al. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ. 2012;344 doi: 10.1136/bmj.e3257. [DOI] [PubMed] [Google Scholar]
- 5.Greulich S., Mayr A., Gloekler S., et al. Time-dependent myocardial necrosis in patients with ST-segment-elevation myocardial infarction without angiographic collateral flow visualized by cardiac magnetic resonance imaging: results from the multicenter STEMI-SCAR project. J Am Heart Assoc. 2019;8(12) doi: 10.1161/JAHA.119.012429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reimer K.A., Lowe J.E., Rasmussen M.M., Jennings R.B. The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs. Circulation. 1977;56(5):786–794. doi: 10.1161/01.cir.56.5.786. [DOI] [PubMed] [Google Scholar]
- 7.Zinger N.D., Blomberg S.N., Lippert F., Krafft T., Christensen H.C. Impact of integrating out-of-hours services into Emergency Medical Services Copenhagen: a descriptive study of transformational years. Int J Emerg Med. 2022;15(1):40. doi: 10.1186/s12245-022-00442-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andersen M.P., Valeri L., Starkopf L., et al. The mediating effect of pupils’ physical fitness on the relationship between family socioeconomic status and academic achievement in a Danish school cohort. Sports Med. 2019;49(8):1291–1301. doi: 10.1007/s40279-019-01117-6. [DOI] [PubMed] [Google Scholar]
- 9.Folketingstidende. Redegørelse om regional- og landdistriktspolitisk redegørelse 2023. https://www.folketingstidende.dk/samling/20231/redegoerelse/R2/20231_R2.pdf
- 10.Tranberg T., Lippert F.K., Christensen E.F., et al. Distance to Invasive Heart Centre, performance of acute coronary angiography, and angioplasty and associated outcome in out-of-hospital cardiac arrest: a nationwide study. Eur Heart J. 2017;38(21):1645–1652. doi: 10.1093/eurheartj/ehx104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dansk Hjerteregister; Årsberetning (Danish) https://www.sundhed.dk/content/cms/72/4672_dhr-aarsberetning-2019_censureret.pdf
- 12.Jensen T.W., Blomberg S.N., Folke F., et al. The National Danish Cardiac Arrest Registry for out-of-hospital cardiac arrest - a registry in transformation. Clin Epidemiol. 2022;14:949–957. doi: 10.2147/CLEP.S374788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmidt M., Pedersen L., Sørensen H.T. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi: 10.1007/s10654-014-9930-3. [DOI] [PubMed] [Google Scholar]
- 14.Lynge E., Sandegaard J.L., Rebolj M. The Danish national patient register. Scand J Public Health. 2011;39(7 Suppl):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 15.Kildemoes H.W., Sørensen H.T., Hallas J. The Danish national prescription registry. Scand J Public Health. 2011;39(7 Suppl):38–41. doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- 16.Özcan C., Juel K., Flensted Lassen J., von Kappelgaard L.M., Mortensen P.E., Gislason G. The Danish heart registry. Clin Epidemiol. 2016;8:503–508. doi: 10.2147/CLEP.S99475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Helweg-Larsen K. The Danish register of causes of death. Scand J Public Health. 2011;39(7 Suppl):26–29. doi: 10.1177/1403494811399958. [DOI] [PubMed] [Google Scholar]
- 18.Roffi M., Patrono C., Collet J.-P., et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of. Eur Heart J. 2016;37(3):267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 19.Danmarks Statistik Hjemsendelse af analyseresultater fra Danmarks Statistiks mikrodataordninger og sanktioner ved databrud. https://www.dst.dk/Site/Dst/SingleFiles/GetArchiveFile.aspx?fi=2486967504&fo=0&ext=forskning
- 20.Hernán M.A., Robins J.M. 2020. Causal Inference: What if. Boca Rat Chapman Hall/CRC.https://www.hsph.harvard.edu/miguel-hernan/causal-inference-book/ [Google Scholar]
- 21.Devlin T.F., Weeks B.J. Spline functions for logistic regression modelling. Proceedings of the 11th Annual SAS Users Group International Conference. https://support.sas.com/resources/papers/proceedings-archive/SUGI86/Sugi-11-119DevlinWeeks.pdf
- 22.Hmisc. https://cran.r-project.org/web/packages/Hmisc/index.html
- 23.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2012. R: A Language and Environment for Statistical Computing. [Google Scholar]
- 24.Fu X., Wilson P., Chung W.S.F. Time-to-reperfusion in patients with acute myocardial infarction and mortality in prehospital emergency care: meta-analysis. BMC Emerg Med. 2020;20(1):65. doi: 10.1186/s12873-020-00356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boersma E. Primary Coronary Angioplasty vs Thrombolysis Group. Does time matter? A pooled analysis of randomized clinical trials comparing primary percutaneous coronary intervention and in-hospital fibrinolysis in acute myocardial infarction patients. Eur Heart J. 2006;27(7):779–788. doi: 10.1093/eurheartj/ehi810. [DOI] [PubMed] [Google Scholar]
- 26.Betriu A., Masotti M. Comparison of mortality rates in acute myocardial infarction treated by percutaneous coronary intervention versus fibrinolysis. Am J Cardiol. 2005;95(1):100–101. doi: 10.1016/j.amjcard.2004.08.069. [DOI] [PubMed] [Google Scholar]
- 27.Terkelsen C.J., Sørensen J.T., Maeng M., et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304(7):763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 28.Hochman J.S., Reynolds H.R., Dzavík V., et al. Long-term effects of percutaneous coronary intervention of the totally occluded infarct-related artery in the subacute phase after myocardial infarction. Circulation. 2011;124(21):2320–2328. doi: 10.1161/CIRCULATIONAHA.111.041749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doll J.A., Roe M.T. Time to treatment as a quality metric for acute STEMI care. Lancet. 2015;385(9973):1056–1057. doi: 10.1016/S0140-6736(14)62051-1. [DOI] [PubMed] [Google Scholar]
- 30.Park J., Choi K.H., Lee J.M., et al. Prognostic implications of door-to-balloon time and onset-to-door time on mortality in patients with ST-segment-elevation myocardial infarction treated with primary percutaneous coronary intervention. J Am Heart Assoc. 2019;8(9) doi: 10.1161/JAHA.119.012188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roswell R.O., Greet B., Parikh P., et al. From door-to-balloon time to contact-to-device time: predictors of achieving target times in patients with ST-elevation myocardial infarction. Clin Cardiol. 2014;37(7):389–394. doi: 10.1002/clc.22278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De L.G., Suryapranata H., Zijlstra F., et al. Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2003;42(6):991–997. doi: 10.1016/S0735-1097(03)00919-7. [DOI] [PubMed] [Google Scholar]
- 33.Varcoe R.W., Clayton T.C., Gray H.H., et al. Impact of call-to-balloon time on 30-day mortality in contemporary practice. Heart. 2017;103(2):117–124. doi: 10.1136/heartjnl-2016-309658. [DOI] [PubMed] [Google Scholar]
- 34.Antman E.M. Time is muscle: translation into practice. J Am Coll Cardiol. 2008;52(15):1216–1221. doi: 10.1016/j.jacc.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 35.Bates E.R., Jacobs A.K. Time to treatment in patients with STEMI. N Engl J Med. 2013;369(10):889–892. doi: 10.1056/NEJMp1308772. [DOI] [PubMed] [Google Scholar]
- 36.Ottesen M.M., Dixen U., Torp-Pedersen C., Køber L. Prehospital delay in acute coronary syndrome--an analysis of the components of delay. Int J Cardiol. 2004;96(1):97–103. doi: 10.1016/j.ijcard.2003.04.059. [DOI] [PubMed] [Google Scholar]
- 37.Jobs A., Mehta S.R., Montalescot G., et al. Optimal timing of an invasive strategy in patients with non-ST-elevation acute coronary syndrome: a meta-analysis of randomised trials. Lancet. 2017;390(10096):737–746. doi: 10.1016/S0140-6736(17)31490-3. [DOI] [PubMed] [Google Scholar]
- 38.Kofoed K.F., Kelbæk H., Hansen P.R., et al. Early versus standard care invasive examination and treatment of patients with non-ST-segment elevation acute coronary syndrome. Circulation. 2018;138(24):2741–2750. doi: 10.1161/CIRCULATIONAHA.118.037152. [DOI] [PubMed] [Google Scholar]
- 39.Sundbøll J., Adelborg K., Munch T., et al. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ Open. 2016;6(11) doi: 10.1136/bmjopen-2016-012832. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.