Abstract
Background
In China, both percutaneous microwave/radiofrequency ablation liver partition plus portal vein embolization (PALPP) and transarterial chemoembolization (TACE) plus portal vein embolization (PVE) have been utilized in planned hepatectomy. However, there is a lack of comparative studies on the effectiveness of these two techniques for cases with insufficient future liver remnant (FLR).
Methods
Patients were categorized into either the PALPP group or the TACE + PVE group. Clinical data, including FLR growth rate, complications, secondary resection rate, and overall survival rate, were compared and analyzed for both groups retrospectively.
Results
Between December 2014 and October 2021, a total of 29 patients underwent TACE + PVE (n = 12) and PALPP (n = 17). In the TACE + PVE group, 7 patients successfully underwent two-stage hepatectomy, while in the PALPP group, 13 patients underwent the procedure (two-stage resection rate: 58.3% vs. 76.5%, P = 0.42). There were no significant differences in postoperative complications of one-stage procedures (11.8% vs. 8.3%, P > 0.05) and second-stage resection complication (0% vs. 46.2%, P = 0.05) between the TACE + PVE and PALPP groups. However, the PALPP group demonstrated a shorter time to FLR volume growth for second-stage resection (18.5 days vs. 66 days, P = 0.001) and KGR (58.5 ml/week vs. 7.7 ml/week, P = 0.001).
Conclusions
Compared with TACE + PVE, PALPP results in a more significant increase in FLR volume and a higher rate of two-stage resection without increasing postoperative complications.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12885-024-12666-z.
Keywords: Microwave/radiofrequency ablation, Liver partition, Planned hepatectomy, Transarterial chemoembolization, Portal vein mbolization, Future liver remnant
Introduction
Surgery remains the mainstay of curative treatment for liver-related malignant tumors, particularly primary hepatocarcinoma. Unfortunately, only a small percentage, ranging from 5–10%, of new cases of primary liver cancer annually are eligible for surgical resection [1]. Among those unable to undergo surgical resection, approximately 30% face inoperability due to insufficient future liver remnant (FLR), a condition predominantly contributing to postoperative liver failure [2, 3].
In addressing this challenge, Makuuchi et al. introduced portal vein embolization (PVE) in 1990. Subsequently, in 2012, Schnitzbauer et al. proposed the Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) method to achieve compensatory liver enlargement and mitigate the risk of postoperative liver failure [2].
However, it is now understood that PVE typically takes 4–6 weeks to stimulate FLR growth, accompanied by an increased risk of tumor progression due to compensatory hepatic arterial blood flow. To address this, Gruttadauria et al. in 2006 proposed combining PVE with transcatheter arterial chemoembolization (TACE), aiming to enhance FLR volume to surgical standards within a shorter 4-week period [4]. While ALPPS significantly increases FLR volume, some studies have reported a rapid induction of liver hypertrophy within one week, reaching up to 93%. Nevertheless, its serious complications and high mortality compromise its clinical efficacy [5]. In 2015, Professor Gall TM and Cillo U introduced percutaneous radiofrequency ablation (PRA) and microwave ablation (PMA) to separate liver parenchyma. Hong et al. later refined this method, replacing portal vein ligation with the PVE method, resulting in percutaneous microwave ablation liver partition and portal vein embolization for planned hepatectomy (PALPP) [6–8], which achieves the surgical FLR requirement in about one week.
Despite the substantial enhancements in FLR growth efficiency and safety observed with these modified procedures, clinical selection remains contentious. Therefore, this study sought to compare FLR volume growth, safety, two-stage resection rates, and prognosis between the two surgical methods to inform future clinical practice.
Materials and Methods
Selection of patients
A retrospective study was conducted, including a total of 45 patients who underwent PVE at Zhejiang Provincial People's Hospital between December 2014 and October 2021. All interventional and surgical procedures were conducted at the same hospital.
Inclusion criteria: (I) age ≥ 18 years old; (II) Liver resection planned with insufficient FLR for primary surgical resection (FLR ≥ 25–30% is recommended for patients with a normal healthy liver and > 40% for those with severe cirrhosis or portal hypertension) [9–11]. (III) Liver function categorized as Child–Pugh class A, B, or per WHO criteria with performance status (PS) of 0, 1, or 2. (IV) No preoperative adjuvant therapy received.(V) All liver malignancies.
Exclusion criteria: (I) Non-malignant intrahepatic lesions. (II) PVE alone.
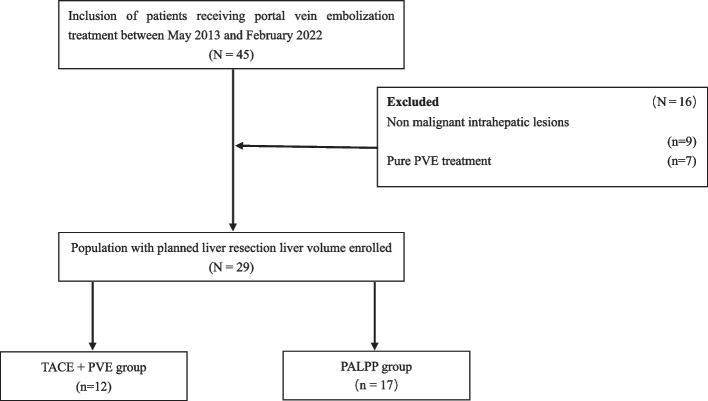
A total of 29 patients were enrolled in this study, including 12 patients treated with TACE + PVE. 17 patients were treated with PALPP(Fig. 1).
Fig. 1.
Flow chart of enrolled patients. TACE + PVE, transarterial chemoembolization plus portal vein embolization; PALPP, percutaneous microwave/radiofrequency ablation liver partition and portal vein embolization
Procedure of operation
PVE: After administering general anesthesia, ultrasound-guided percutaneous portal vein puncture was performed. The hemihepatic portal vein, along with its branches in the segment where the lesion was located, were embolized with coils under transcatheter portal vein angiography by digital subtraction angiography (DSA) navigation. Following this procedure, appropriate embolization was carried out using a mixture of isobutyl cyanoacrylate (NBCA) and lipiodol in a 1:1 ratio until angiography demonstrated complete occlusion of the target vessels [12].
TACE: The main artery and its branches of the hepatic lesion were superselectively accessed through percutaneous femoral artery puncture under DSA navigation. Tumor vessels were embolized with ultra-liquefied lipiodol combined with epirubicin/cisplatin + famacin or drug-loaded microspheres and gelatin sponge particles [13].
Percutaneous microwave coagulation therapy (PMCT)/Percutaneous radiofrequency ablation (PRFA): (I) PMCT: Ultrasound-guided PMCT was performed using a microcomputer cold circulation microwave therapeutic apparatus with a frequency of 2450 MHz and a maximum power of 100W (Fuzhong Medical High-tech Co., LTD., Jiangsu, China). A demarcation line in the hepatic parenchyma was delineated 2 cm from the primary hepatic vein, and this demarcation was conserved using real-time ultrasound guidance. The ablation line was ensured to be more than 1 cm away from the tumor boundary. Subsequently, the ablation needle was placed on the pre-tangent line during percutaneous puncture under ultrasound guidance, and the multi-point and multi-axis sector ablation method was used to separate the liver parenchyma. The ablation time was 2–3 min per point, the power was 50-60W, the temperature was around 90 °C, and the end of the needle track was coagulated to prevent bleeding.
As for the TACE + PVE cohort, PVE was performed 2 to 4 weeks after TACE in patients who underwent sequential therapy. Otherwise, PVE was performed immediately after successful TACE treatment, and then the second-stage resection was performed after about 4 weeks until the FLR reached the standard. For patients who underwent PALPP, a two-stage hepatectomy was performed as long as up to FLR requirement. All procedures were performed by the same team.
The liver volume measurement standard of the two groups was based on the liver-enhanced CT three-dimensional reconstruction before each intervention or operation. FLR was evaluated using three-dimensional visualization technology. The standard liver volume (SLV) was calculated according to the formula proposed by Urata and Bruix et al. (SLV (mL) = 706.2 × BSA (m2) + 2.4). The kinetic growth rate (KGR) was calculated as the ratio of the degree of liver volume increase (%) to the time from baseline to the liver volume before the second stage hepatectomy (weeks) [14–16]. Due to the slow growth effect observed in the TACE + PVE group, tumor progression occurred during the waiting period, which was addressed by TACE treatment. After the first stage of surgery, the FLR was reviewed weekly, and if the FLR met the prespecified criteria, patients in the two groups underwent the second stage of surgery.
Treatment failure was considered if (I) tumor progression occurred while waiting, (II) complications caused the failure of the two-stage hepatectomy, or (III) treatment was abandoned by the patient after one-stage treatment. Patients who failed treatment received palliative care (chemotherapy, targeted therapy, intervention, etc.).
Outcomes and Follow-up
The primary outcomes were the rate of two-stage resection. Secondary outcomes included: (I) the growth rate of FLR, (II) postoperative complications, and mortality (complications were classified according to Clavien-Dindo) [17].
The surgical margin was defined as the shortest distance from the tumor edge to the resection plane, with R0 resection defined as a negative microscopic margin and R1 resection defined as a positive microscopic margin. Patients were followed up one month after surgical resection, and then serum AFP, enhanced CT, or enhanced MRI scans and liver function were reviewed every 3 months. Patients with recurrence or metastasis were treated with further therapy.
Data analysis
Continuous variables with a normal distribution were expressed as mean ± standard deviation (SD), and those with a skewed distribution were expressed as median and interquartile range (IQR). The Mann–Whitney U test was used for comparison. Categorical variables were expressed as frequencies and percentages and compared using Pearson's chi-square test or Fisher's exact test. Finally, multivariate COX regression analysis was included to determine the significant factors affecting the volume growth rate of FLR. All calculations were analyzed using standard software (SPSS Statistics 25.0). A two-tailed P-value < 0.05 was statistically significant.
Research methods and ethics
This study is a retrospective study on patients with liver malignancies who received TACE + PVE or PALPP treatment due to insufficient FLR. Our research was conducted in accordance with the principles outlined in the Helsinki Declaration, and all procedures involving human participants strictly adhere to the ethical standards of the Zhejiang Provincial People's Hospital Ethics Review Committee. Given the retrospective nature of this study, which involved the use and analysis of unverified data, the Ethics Review Committee of Zhejiang Provincial People's Hospital waived the requirement for written informed consent.
Result
A total of 45 patients who underwent PVE from December 2014 to October 2021 were included in this study. Nine patients with non-neoplastic lesions receiving PVE were excluded, along with 7 patients who underwent PVE alone. Finally, 29 patients were included in the study (Fig. 1).
Comparison of baseline data between the two groups
There were no significant differences between the two groups at baseline (Table 1).
Table 1.
Baseline characteristics between TACE + PVE and PALPP groups
| Characteristic | Level | TACE + PVE group (n = 12) |
PALPP group(N = 17) PMA(n = 8) PRA(n = 9) |
P |
|---|---|---|---|---|
| Age (year) (median [IQR]) | 50.5 (43.8, 57.0) | 49.0 (46.0, 59.0) | 0.76 | |
| Sex (%) | Male | 10 (83.3) | 14 (82.4) | 1.00 |
| Female | 2 (16.7) | 3 (17.7) | ||
| BMI (kg/m2) (median [IQR]) | 23.0 (21.1, 23.6) | 22.2 (20.5, 23.4) | 0.35 | |
| ASA (%) | I | 4 (33.3) | 1 (5.9) | 0.16 |
| II | 7 (58.3) | 14 (82.4) | ||
| III | 1 (8.3) | 2 (11.8) | ||
| PS (%) | 0 | 9 (75.0) | 15 (88.2) | 0.43 |
| 1 | 2 (16.7) | 2 (11.8) | ||
| 2 | 1 (8.3) | 0 (0.0) | ||
| Tumor type (%) | HCC | 11 (91.7) | 13 (76.5) | 0.65 |
| ICC | 1 (8.3) | 2 (11.8) | ||
| Other tumors | 0 (0.0) | 2 (11.8) | ||
| Number of tumors (%) | Single tumor | 8 (66.7) | 7 (41.8) | 0.26 |
| Multiple tumors | 4 (33.3) | 10 (58.8) | ||
| Maximum tumor diameter (mm) | 96.0 (47.5, 118.0) | 80.0 (44.5, 112.5) | 0.57 | |
| Macrovascular invasion (%) | No | 6 (50.0) | 8 (47.1) | 1.00 |
| Yes | 6 (50.0) | 9 (52.9) | ||
| TB (μmol/L) (median [IQR]) | 13.1 (11.3, 20.9) | 20.1 (14.6, 25.7) | 0.03 | |
| ALT (U/L) (median [IQR]) | 31.5 (24.5, 47.0) | 42.0 (17.5, 72.5) | 0.83 | |
| AST (U/L) (median [IQR]) | 47.0 (32.8, 72.5) | 55.0 (34.5, 83.5) | 0.72 | |
| AFP (%) | < 20 μg/L | 2 (16.7) | 6 (35.3) | 0.41 |
| > 20 μg/L | 10 (83.3) | 11 (64.7) | ||
| Cirrhosis (%) | No | 1 (8.3) | 4 (23.5) | 0.37 |
| Yes | 11 (91.7) | 13 (76.5) | ||
| HBV (%) | No | 0 (0.0) | 4 (23.5) | 0.21 |
| Yes | 12 (100.0) | 13 (76.5) | ||
| Protal hypertension (%) | No | 7 (58.3) | 7 (41.2) | |
| Yes | 5 (41.7) | 10 (58.8) | 0.59 | |
| Child–Pugh grade | 1 | 12 (100.0) | 14 (82.4) | 0.36 |
| 2 | 0 (0.0) | 3 (17.7) |
BMI body mass index, ASA American Society of Anesthesiologists, PS performance status, HCC hepatocellular carcinoma, ICC intrahepatic cholangiocarcinoma, PLT platelet, TB total bilirubin, ALT alanine aminotransferase, AST aspartate aminotransferase, AFP alpha-fetoprotein, HBV hepatitis B virus
Comparison of treatment outcomes and intraoperative variables between the PALPP group and TACE + PVE group
In the TACE + PVE group, 58.3% of patients (n = 7) underwent two-stage hepatectomy, while in the PALPP group, the proportion was higher at 76.5% (n = 13). The reasons for the failure to undergo a two-stage hepatectomy are detailed in Table 2. Importantly, there was no significant difference in the rate of two-stage hepatectomy completion between the two groups (P = 0.42). Within the PALPP group, all patients experienced sufficient FLR volume growth, and among those who did not undergo two-stage surgery, two patients underwent TACE due to tumor progression. Conversely, in the TACE + PVE group, two patients experienced insufficient FLR volume growth. One patient underwent TACE + PVE treatment again, but the growth effect was limited, leading the family to discontinue treatment. The other patient declined the second treatment and opted for conservative management. Among the two patients with tumor progression in this group, one chose to discontinue treatment, while the other received sorafenib. The choice of hepatectomy types varied between the groups, with right trisegmentectomy being the predominant approach in the PALPP group (69.2% vs. 14.3%, P = 0.06) and right hemihepatectomy being more common in the TACE + PVE group (57.1% vs. 15.1%). Although intraoperative blood loss was lower in the TACE + PVE group, and the operative duration was shorter in the PALPP group, there were no significant differences between the two groups (P = 0.6, P = 0.38).
Table 2.
Intraoperative and postoperative data of TACE + PVE and PALPP groups were compared
| Index | TACE + PVE group | PALPP group | P |
|---|---|---|---|
| Data of first step | (n = 12) | (n = 17) | |
| Preoperative variables | |||
| AST (U/L) (median [IQR]) | 47.0 (32.8, 72.5) | 55.0 (34.5, 83.5) | 0.72 |
| ALT (U/L) (median [IQR]) | 31.5 (24.5, 47.0) | 42.0 (17.5, 72.5) | 0.83 |
| AFP (> 20 μg/L) (%) | 10 (83.3) | 11 (64.7) | 0.41 |
| TB (μmol/L) (median [IQR]) | 13.1 (11.3, 20.9) | 20.1 (14.6, 25.7) | 0.03 |
| Postoperative complications (Clavien Dindo) (%) | |||
| > Grade II | 1 (8.3) | 2 (11.8) | 1.00 |
| Details | Liver failure ( n = 1, 8.3%) | Perioperative mortality (n = 1, 5.9%), pleural effusion (n = 1, 5.9%) | |
| Data of second step | (n = 7) | (n = 13) | |
| Second step | Second step (n = 7, 58.3%) | Second step (n = 13, 76.5%) | 0.42 |
| Reasons for not proceeding to second step hepatectomy | Total:n = 5 (41.7%), Tumor progression (n = 2, 11.8%), Liver failure (n = 1, 8.3%), insufficient hypertrophy of FLR (n = 2, 16.7%) | Total:n = 4 (23.5%), Tumor progression (n = 2, 11.8%), Liver failure (n = 1, 5.9%), loss to follow-up (n = 1, 5.9%) | |
| Second step variables | |||
| AST (U/L) (median [IQR]) | 30.0 (25.0, 37.0) | 49.0 (27.5, 87.5) | 0.19 |
| ALT (U/L) (median [IQR]) | 24.0 (18.0, 47.0) | 42.0 (23.0, 66.5) | 0.23 |
| AFP (> 20 μg/L) (%) | 5 (71.4) | 7 (53.8) | 0.64 |
| TB (μmol/L) (median [IQR]) | 16.6 (13.3, 18.5) | 18.9 (12.3, 31.3) | 0.38 |
| Second step variables | |||
| Operation time (min) (median [IQR]) | 300.0 (205.0, 350.0) | 285.0 (245.0, 295.0) | 0.38 |
| Pringle maneuver (min) (median [IQR]) | 0.0 (0.0, 45.0) | 12.0 (0.0, 29.0) | 0.54 |
| Blood transfusion (%) | 5 (71.4) | 10 (83.3) | 0.60 |
| Intraoperative blood loss (ml) (median [IQR]) | 700.0 (200.0, 1000.0) | 800.0 (450.0, 1100.0) | 0.84 |
| Type of hepatectomy (%) | NA | ||
| Right hepatectomy | 4 (57.1) | 2 (15.4) | |
| Right trisegmentectomy | 1 (14.3) | 9 (69.2) | |
| Palliative hepatectomy | 0 (0.0) | 2 (15.4) | |
| 2 segmental liver resection/tumor resection | 2 (28.6) | 0 (0.0) | |
| Sceond step complications (Clavien Dindo) (%) | |||
| > Grade II | 0 (0.0) | 6 (46.2) | 0.05 |
| Details | Abdominal bleedinga (n = 1, 7.7%), Liver failure (n = 1, 7.7%), Intestinal obstruction (n = 1, 7.7%), pneumothorax (n = 1, 7.7%), Thoracic effusion requires puncture and drainage (n = 3, 23.1%) | ||
| R0 (%) | 7 (100.0) | 11 (84.6) | 0.52 |
| Death 90 days after surgery (%) | 0 (0.0) | 2 (15.4) | |
| Cuase of death | Liver failure (n = 1, 7.7%), Tumor progression (n = 1, 7.7%) | ||
| Postoperative tumor recurrence (%) | 3 (42.9) | 11 (84.6) | 0.12 |
| Treatment after recurrence | (n = 3) | (n = 11) | |
| Rehepatectomy (%) | 0 (0.0) | 2 (18.2) | |
| Ablation (%) | 1 (33.3) | 1 (9.1) | |
| TACE (%) | 1 (33.3) | 2 (18.2) | |
| Radiotherapy (%) | 0 (0.0) | 1 (9.1) | |
| Chemotherapy (%) | 0 (0.0) | 1 (9.1)b | |
| Targeted therapy (%) | 0 (0.0) | 0 (0.0) | |
| Chemotherapy + Targeted therapy (%) | 1 (0.0)c | 0 (0.0) | |
| Supportive treatment (%) | 0 (0.0) | 4 (36.4) | |
aAbdominal bleeding requires secondary surgical hemostasis
bChemotherapy (tegafur)
cChemotherapy (FOLFOX) + Targeted therapy (sorafenib)
FLR volume growth and FLR changes after stage 1 surgery
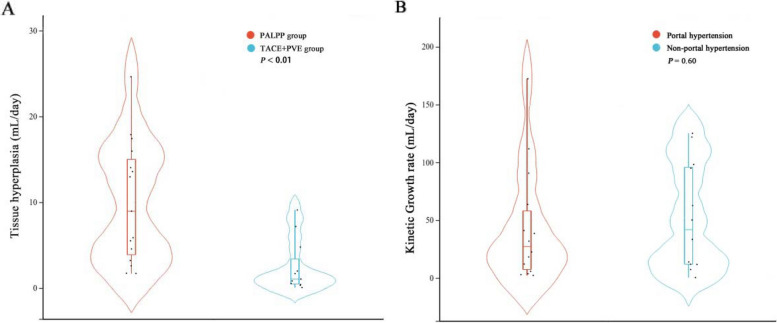
Two patients died after stage 1 surgery (one PALPP, one TACE + PVE) and were excluded from the analysis. The final FLR volume was comparable between groups (526.0 vs 502.2 mL, P = 0.657) (Table 3). However, the inter-stage interval was shorter for PALPP (18.5 vs 66 days, P = 0.001), with a faster FLR growth rate (43% vs 23%, P = 0.026) and higher weekly liver hypertrophy rate (58.5 vs 7.7 mL/week, P = 0.001). PALPP demonstrated superior FLR expansion over TACE + PVE (Fig. 2A), unaffected by portal hypertension (Fig. 2B). In addition, Table 4 shows the impact of different types of intrahepatic tumors on FLR proliferation.
Table 3.
Growth of FLR under two surgical methods
| Index | TACE + PVE group (n = 11) |
PALPP group (n = 16) |
P value |
|---|---|---|---|
| SLV (ml) (median [IQR]) | 1147.9 (1068.6, 1251.5) | 1192.8 (1133.4, 1241.7) | 0.278 |
| Liver volume growth time (day) (median [IQR]) | 66 (41.0, 118.0) | 18.5 (12.5, 37.0) | 0.001 |
| FLR1 (ml) (median [IQR]) | 383.3 (339.5, 447.0) | 368.1 (308.3, 400.8) | 0.43 |
| FLR2 (ml) (median [IQR]) | 502.2 (400.0, 586.8) | 526.0 (456.6, 569.6) | 0.657 |
| FLR3 (ml) (median [IQR]) | 83.1 (43.9, 182.8) | 158.4 (95.5, 206.4) | 0.043 |
| FLR † (%) (median [IQR]) | 23 (12.0,47.0) | 43 (29, 58.5) | 0.026 |
| KGR (ml/w) (median [IQR]) | 7.7 (3.2, 33.7) | 58.5 (25.2 108.6) | 0.001 |
SLV standard liver volume; Liver volume growth time, The waiting time between procedures or the time span from phase I surgery to treatment failure, FLR1 First pre-operative FLR, FLR2 FLR before second surgery or FLR at the time of treatment failure, FLR3 FLR3 = FLR2-FLR1; FLR †, The increase in FLR between the two procedures was divided by the FLR before the first procedure (FLR † = FLR3/ FLR1); KGR, Degree of liver volume increase (%)/time elapsed from baseline to final volume before stage II hepatectomy (weeks)
Fig. 2.
Subgroup analysis of future liver volume growth. A The difference in daily hypertrophy volume of liver tissue under different operating methods; B The effect of portal hypertension on the increase of FLR
Table 4.
Liver Volume Hyperplasia under Different Pathological Types
| TACE + PVE group (n = 11) |
PALPP group (n = 16) |
|||||
|---|---|---|---|---|---|---|
| HCC (n = 11) |
ICC (n = 0) |
MLC (n = 0) |
HCC (n = 12) |
ICCa (n = 2) |
MLCa (n = 2) |
|
| SLV (ml) (median [IQR]) | 1147.9 (1068.6, 1251.5) | NA | NA | 1178.9 (1128.4, 1241.7) | (1232.7, 1268.6) | (1139.2, 1170.3) |
| Liver volume growth time (day) (median [IQR]) | 66 (41.0, 118.0) | NA | NA | 19 (14.3, 40.8) | (11.0, 15.0) | (12.0, 15.0) |
| FLR1 (ml) (median [IQR]) | 383.3 (339.5, 447.0) | NA | NA | 257.2 (199.8, 365.1) | (353.7, 367.4) | (367.4, 372.7) |
| FLR2 (ml) (median [IQR]) | 502.2 (400.0, 586.8) | NA | NA | 523.4 (400.7, 576.7) | (508.5, 518.0) | (540.0, 558.5) |
| FLR3 (ml) (median [IQR]) | 83.1 (43.9, 182.8) | NA | NA | 157.1 (89.3, 212.6) | (146.4, 150.6) | (162.0, 185.8) |
| FLR † (%) (median [IQR]) | 23 (12.0,47.0) | NA | NA | 39.1(26.9, 78.7) | (38.4, 41.1) | (42.9, 49.9) |
| KGR (ml/w) (median [IQR]) | 7.7 (3.2, 33.7) | NA | NA | 40.1(19.6, 107.8) | (54.0, 76.2) | (20.7, 92.6) |
HCC hepatocellular carcinoma, ICC Cholangiocarcinoma, MLC Metastatic liver cancer, SLV standard liver volume; Liver volume growth time, The waiting time between procedures or the time span from phase I surgery to treatment failure, FLR1 First pre-operative FLR, FLR2 FLR before second surgery or FLR at the time of treatment failure, FLR3 FLR3 = FLR2-FLR1; FLR †, The increase in FLR between the two procedures was divided by the FLR before the first procedure (FLR † = FLR3/ FLR1); KGR, Degree of liver volume increase (%)/time elapsed from baseline to final volume before stage II hepatectomy (weeks)
aThe column representation method is (minimum, maximum)
Comparison of postoperative outcomes between the PALPP and TACE + PVE groups
Complications
All patients in both groups successfully completed the first stage operation, with only one case with complications above Grade II in the TACE + PVE group, specifically postoperative liver failure, which improved after comprehensive medical treatment. In contrast, the PALPP group encountered 2 cases of postoperative complications above Grade II: one patient succumbed during the perioperative period due to postoperative liver failure, and another developed postoperative pleural effusion, relieved after transthoracic puncture drainage. There was no significant difference in the incidence of complications exceeding Grade II after stage 1 surgery between the two groups (8.3% vs. 11.8%, P > 0.05) (Table 2). Among patients who underwent two-stage surgery (7 patients (58.3%) in the TACE + PVE group; 13 cases (76.5%) in the PALPP group), no complications exceeding Grade II were reported in the TACE + PVE group. In the PALPP group, however, 6 patients experienced complications higher than Grade II (P = 0.05). The complications of abdominal bleeding and intestinal obstruction in the PALPP group were addressed by a second operation to relieve intestinal obstruction. Pneumothorax and pleural effusion were treated with closed thoracic drainage and thoracentesis drainage. Unfortunately, the family members of patients with postoperative liver failure chose to discontinue treatment.
Survival analysis
We further compared the prognostic impact of different surgical methods and pathological types.When the pathology is HCC, the TACE + PVE group had a median follow up period of 14.5 months, with a recurrence rate of 63.6% and a mortality rate of 45.5%. During the median folllow up period of 17.5 mongths; the recurrence rate of the PALPP group was 83.3%,and the mortality rate was 58.3%.
Discussion
ALPPS, as a revolutionary breakthrough in hepatobiliary surgery, offers a radical approach for resecting mid to late-stage liver cancer with insufficient FLR. However, its clinical application has faced challenges due to high complication and mortality rates. Consequently, alternative technologies like TACE + PVE and PALPP have gained prominence in China, offering enhanced efficiency in promoting residual liver hyperplasia while maintaining minimally invasive and safe characteristics.
TACE + PVE serves as a safe strategy for increasing FLR volume, exhibiting a larger growth rate compared to PVE alone and mitigating the risk of tumor progression during the waiting period for liver volume growth [18]. However, the rate of secondary liver resection in patients with PVE + TACE has been reported at around 60% [19]. In contrast, PALPP is a novel strategy that has been associated with a remarkable 92% rate for increasing FLR volume after second-stage hepatectomy [20]. While both procedures demonstrate safety and clinical effectiveness, there remain controversies regarding their scope of use and clinical selection, and a direct comparison of their effects on insufficient FLR has not been reported.
The principle of TACE + PVE involves blocking blood flow to the tumor side of the liver, promoting regeneration of the residual liver tissue. Highly selective TACE is then employed to further block the tumor blood supply, inhibiting growth and reducing the time for recurrence and progression. PALPP, on the other hand, involves cutting off the tumor-side liver through PRA/PMA and combining it with PVE to block the blood flow further, promoting the proliferation of the residual liver volume and reducing the risk of complications like bile leakage and bleeding.
Modified TACE + PVE has been effective in reducing the growth time required for the remnant liver volume to reach a tolerable level for hepatectomy from the original 4–8 weeks to less than 4 weeks [4]. However, the median interval between the two operations at our center was 66 days, with a mean interval of 85.3 days, significantly longer than in previous studies. In response, we conducted an analysis to identify reasons for this prolonged interval in our study cases, which included severe postoperative complications, poor liver reserve function evaluation indicators and extended waiting intervals between surgeries due to patient-related reasons. In contrast, PALPP demonstrated superior results, achieving a median time of only 18.5 days and a mean time of 26.6 days (P = 0.001) to reach a resectable standard. Additionally, the surgical resection rate in the PALPP group was significantly higher than in the TACE + PVE group (76.5% vs. 58.3%, P = 0.42). In both groups, two patients each lost the opportunity for a second surgery due to tumor progression. In the TACE + PVE group, one case resulted in liver failure, while two cases developed dysplasia after the first step (Table 2). The liver growth rate per week was notably higher in the PALPP group (58.5 ml/w vs. 7.7 ml/w, P = 0.001). Similarly, when comparing the increase in liver volume between the two groups, the median increase in the TACE + PVE group was 23%, whereas, in the PALPP group, the median increase was 43% (P = 0.026) (Table 3), similar to the literature [21, 22].
The observed superior results of PALPP compared to TACE + PVE may be attributed to the similarity between PALPP and ALPPS in promoting residual liver hyperplasia. PALPP, like ALPPS, involves ablation and separation of liver parenchyma, replacing the disconnection of liver parenchyma. This process can effectively block the communicating branches of the portal veins on both sides of the preserved and resected liver, facilitating rapid growth of the FLR. The key distinction between PALPP and TACE + PVE lies in the absence of hepatic artery embolization chemotherapy in PALPP, minimizing the impact on the blood supply to the tumor-side liver. This avoids the potential complications associated with TACE + PVE, such as tumor-side liver ischemic necrosis, abscess formation, and even acute liver failure. Consequently, once the resectability criteria are met, PALPP allows timely liver resection.
To identify potential factors influencing growth, a stratified analysis was performed. The average growth of hepatocellular carcinoma, cholangiocarcinoma, and metastatic liver cancer using the PALPP method was 172.7 ml, 150.6 ml, and 185.8 ml, respectively. This variation may be associated with the absence of underlying liver diseases and better liver function reserves in patients with metastatic liver cancer compared to other types. Besides, portal hypertension was present in 41.7% and 58.8% of patients in the TACE + PVE group and PALPP group, respectively. In cases where both groups had portal hypertension, the median increase in liver volume in the TACE + PVE group was 14.7%, while in the PALPP group, it was 29.2% [23](Fig. 2). Factors influencing liver volume growth not only include portal hypertension but also encompass body reactions, inflammation levels, and liver hemodynamics. [24–26]
The incidence of complications and causes of death in both groups were reviewed (Table 2). After the initial surgery, the PALPP group experienced two cases of severe complications (> Grade II). One case involved pleural effusion, which improved after thoracic puncture drainage, while the other resulted in perioperative death due to postoperative liver failure leading to gastrointestinal bleeding. In the TACE + PVE group, there was one case of severe complication (> Grade II), specifically liver failure, which improved after conservative treatment. Considering the occurrence of postoperative liver failure and considering patient medical history, it was noted that two cases with liver failure had severe cirrhosis and liver dysfunction before the operation. Although their liver function was corrected before the operation, the surgical procedure acted as a trigger, leading to postoperative liver failure. The incidence of severe complications (above Grade II) after the first step in the TACE + PVE group and PALPP group was 8.3% and 11.8%, respectively. These rates were lower than the incidence of complications after the initial surgery in radiofrequency-assisted ALPPS, as reported by Wang Q et al. [21].
In terms of prognosis, the overall mortality rates in the TACE + PVE group and PALPP group were 66.7% and 76.5% (P = 0.85) over a median follow-up time of 14 months. For the population undergoing the two-stage surgery, the overall mortality rate was 42.9% and 76.9% (P = 0.32) in the TACE + PVE group and PALPP group, respectively, at a median follow-up time of 18.8 months. The impact of PALPP on the prognosis of patients was explored, revealing a positive correlation between postoperative complications and prognosis in the PALPP group, especially with the extent of surgical resection. Among the patients who underwent two-stage surgery (n = 13), extended hemihepatectomy was performed in 77% of cases, compared to 14.3% in the TACE + PVE group. Additionally, the occurrence of postoperative complications, such as abdominal infection and pleural effusion, was directly related to the operation time and prognosis [26, 27]. However, further studies are warranted to ascertain whether PALPP has a direct effect on prognosis. Overall, our findings suggest that PALPP can improve the resection rate of secondary surgery without increasing the incidence of complications.
Based on the experience of our center, PALPP is considered appropriate for the following categories of the population: (1) Patients with liver malignant tumors, especially secondary liver malignant tumors; (2) Presence of cirrhosis or portal hypertension; (3) Liver function classified as Child–Pugh B; (4) Major liver resection (> 4 segments). PALPP can be performed to increase the remnant liver volume in planned hepatectomy when the liver volume is insufficient, with priority given to PALPP selection in the specified cases, though further verification by multiple centers is required.
Certain considerations should be noted during PALPP: (1) FLR volume growth can be accelerated by embolization of peripheral vessels during PVE [28]. (2) When selecting PRA and PMA, a safety margin of at least 10 mm around the outer edge of the lesion is recommended when choosing PMA, especially when the liver partition surface is small. PRA is suitable for various scenarios and can achieve the purpose of one-stage radical surgery for sub-lesions on the side of the liver. After PRA and PMA, the ablation margin is defined to ensure a 1-cm thick tumor-free margin, consistent with the tumor-free principle [29]. Once the tumor-free boundary of the liver parenchyma is established, an additional 50 to 80% of the liver tissue, typically to a depth of 2 to 4 cm, is cut off to facilitate the growth of the residual liver volume. In the meta-analysis conducted by Fadi et al., there was no significant difference between partial partition and complete partition in terms of liver volume increase (P = 0.067) and FLR increase (P = 0.477) [30]. In addition, the partial disconnection method reduced the incidence of postoperative complications (P = 0.03) and mortality (P = 0.12) [31].
Although two patients in the PALPP group included in our study lost the opportunity for the two-stage hepatectomy, they still survived for a significant period through remedial treatment measures such as TACE. Given that the primary pathway of Hepatocellular Carcinoma (HCC) metastasis is intrahepatic portal vein metastasis, PALPP effectively hinders tumor progression by severing the liver parenchyma through radiofrequency or microwave ablation methods. Additionally, PALPP blocks the portal vein communicating branch through PVE. PALPP exhibits better safety, a lower complication rate, less impact on liver injury, increased opportunities for remedial treatment, controlled tumor progression, and prolonged survival [32].
This study is subject to several limitations that should be acknowledged. First, the sample size was relatively small, and the findings are specific to the experience of our institution. Besides, the utilization of chemotherapy following inadequate liver volume hyperplasia, as opposed to remedial measures, diminished the exposure to factors associated with inadequate liver volume hyperplasia. Moreover, the exclusion of patients with benign liver lesions undergoing surgical treatment might obscure the method's efficacy in benign lesions' proliferation. Consequently, additional prospective studies or randomized controlled trials are warranted to assess the clinical efficacy of PALPP.
Conclusions
Overall, this study indicates that compared to TACE + PVE, PALPP can effectively shorten the proliferation time of future liver residues and improve proliferation efficiency. These findings indicate that PALPP is also a feasible method for improving FLR.
Supplementary Information
Acknowledgements
All authors acknowledge the support of Zhejiang Provincial People's Hospital.
Abbreviations
- PALPP
Percutaneous microwave/radiofrequency ablation liver partition plus portal vein embolization
- TACE
Transarterial chemoembolization
- PVE
Portal vein mbolization
- FLR
Future liver remnant
- BMI
Body mass index
- ASA
American Society of Anesthesiologists
- PS
Performance status
- HCC
Hepatocellular carcinoma
- ICC
Intrahepatic cholangiocarcinoma
- MLC
Metastatic liver cancer
- PLT
Platelet
- TB
Total bilirubin
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- AFP
Alpha-fetoprotein
- HBV
Hepatitis B virus
- SLV
Standard liver volume
- KGR
Degree of liver volume increase (%)/time elapsed from baseline to final volume before stage II hepatectomy (weeks)
Authors’ contributions
T-W Y, T-W F, C-F D and R–C Y contributed equally to this work. Dr. J C and Dr.Z-Q X had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: T-W Y, Z-Q X and J C. Acquisition, analysis, or interpretation of data: T-W F, C-F D, Z-H Z, Q-T J, Q Z, C-W Z, J L, J-W L. Drafting of the manuscript: T-W Y and T-W F. Critical revision of the manuscript for important intellectual content: J C and Z-Q X. Statistical analysis: T-W Y and T-W F. Obtained funding: None. Administrative, technical, or material support: C-W Z, X-M F, D-F H, Z-Y L, J C and Z-Q X. Study supervision: J C and Z-Q X.
Funding
Basic Scientific Research Funds of Department of Education of Zhejiang Province(KYQN202118).
Availability of data and materials
Data is provided within the supplementary information files.
Declarations
Ethics approval and consent to participate
This retrospective study complies with the Declaration of Helsinki and was approved by the institutional ethical committee and the need for informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tai-Wei Ye, Tian-Wei Fu, Cheng-Fei Du and Ru-Chi Yue these authors contributed equally to this work.
Contributor Information
Jian Cheng, Email: chengj0523@163.com.
Zun-Qiang Xiao, Email: zqxiao@zcmu.edu.cn.
References
- 1.Ganesan P, Kulik LM. Hepatocellular Carcinoma: New Developments. Clin Liver Dis. 2023;27(1):85–102. 10.1016/j.cld.2022.08.004 [DOI] [PubMed] [Google Scholar]
- 2.Kishi Y, Abdalla EK, Chun YS, et al. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg. 2009;250(4):540–8. 10.1097/SLA.0b013e3181b674df [DOI] [PubMed] [Google Scholar]
- 3.Schnitzbauer AA, Lang SA, Goessmann H, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255(3):405–14. 10.1097/SLA.0b013e31824856f5 [DOI] [PubMed] [Google Scholar]
- 4.Gruttadauria S, Luca A, Mandala L, et al. Sequential preoperative ipsilateral portal and arterial embolization in patients with colorectal liver metastases. World J Surg. 2006;30(4):576–8. 10.1007/s00268-005-0423-0 [DOI] [PubMed] [Google Scholar]
- 5.Zhang GQ, Zhang ZW, Lau WY, et al. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): a new strategy to increase resectability in liver surgery. International journal of surgery (London, England). 2014;12(5):437–41. 10.1016/j.ijsu.2014.03.009 [DOI] [PubMed] [Google Scholar]
- 6.Gall TM, Sodergren MH, Frampton AE, et al. Radio-frequency-assisted liver partition with portal vein ligation (RALPP) for liver regeneration. Ann Surg. 2015;261(2):e45–6. 10.1097/SLA.0000000000000607 [DOI] [PubMed] [Google Scholar]
- 7.Cillo U, Gringeri E, Feltracco P, et al. Totally Laparoscopic Microwave Ablation and Portal Vein Ligation for Staged Hepatectomy : A New Minimally Invasive Two-Stage Hepatectomy. Ann Surg Oncol. 2015;22(8):2787–8. 10.1245/s10434-014-4353-7 [DOI] [PubMed] [Google Scholar]
- 8.Jiao LR. Percutaneous Microwave Ablation Liver Partition and Portal Vein Embolization for Rapid Liver Regeneration: A Minimally Invasive First Step of ALPPS for Hepatocellular Carcinoma. Ann Surg. 2016;264(1): e3. 10.1097/SLA.0000000000001718 [DOI] [PubMed] [Google Scholar]
- 9.van den Broek MA, Olde Damink SW, Dejong CH, et al. Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver international : official journal of the International Association for the Study of the Liver. 2008;28(6):767–80. 10.1111/j.1478-3231.2008.01777.x [DOI] [PubMed] [Google Scholar]
- 10.Imamura H, Seyama Y, Kokudo N, et al. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg 2003;138(11):1198-206; discussion 1206. 10.1001/archsurg.138.11.1198 [DOI] [PubMed] [Google Scholar]
- 11.Schindl MJ, Redhead DN, Fearon KC, et al. The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection. Gut. 2005;54(2):289–96. 10.1136/gut.2004.046524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu Q, Zeng Z, Zhang Y, et al. Study of ultrasound-guided percutaneous microwave ablation combined with portal vein embolization for rapid future liver remnant increase of planned hepatectomy. Front Oncol. 2022;12:926810. 10.3389/fonc.2022.926810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ikeda M, Arai Y, Inaba Y, et al. Conventional or drug-eluting beads? Randomized controlled study of chemoembolization for hepatocellular carcinoma: JIVROSG-1302. Liver cancer. 2022;11(5):440–50. 10.1159/000525500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bruix J, Reig M, Sherman M. Evidence-Based Diagnosis, Staging, and Treatment of Patients With Hepatocellular Carcinoma. Gastroenterology. 2016;150(4):835–53. 10.1053/j.gastro.2015.12.041 [DOI] [PubMed] [Google Scholar]
- 15.Urata K, Kawasaki S, Matsunami H, et al. Calculation of child and adult standard liver volume for liver transplantation. Hepatology (Baltimore, Md). 1995;21(5):1317–21. 10.1002/hep.1840210515 [DOI] [PubMed] [Google Scholar]
- 16.Shindoh J, Truty MJ, Aloia TA, et al. Kinetic growth rate after portal vein embolization predicts posthepatectomy outcomes: toward zero liver-related mortality in patients with colorectal liver metastases and small future liver remnant. J Am Coll Surg. 2013;216(2):201–9. 10.1016/j.jamcollsurg.2012.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. 10.1097/01.sla.0000133083.54934.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foucher J, Chanteloup E, Vergniol J, et al. Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Gut. 2006;55(3):403–8. 10.1136/gut.2005.069153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li PP, Huang G, Jia NY, et al. Associating liver partition and portal vein ligation for staged hepatectomy versus sequential transarterial chemoembolization and portal vein embolization in staged hepatectomy for HBV-related hepatocellular carcinoma: a randomized comparative study. Hepatobiliary surgery and nutrition. 2022;11(1):38–51. 10.21037/hbsn-20-264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jiao LR, Fajardo Puerta AB, Gall TMH, et al. Rapid Induction of Liver Regeneration for Major Hepatectomy (REBIRTH): A Randomized Controlled Trial of Portal Vein Embolisation versus ALPPS Assisted with Radiofrequency. Cancers 2019;11(3):302. 10.3390/cancers11030302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Q, Yan J, Feng X, et al. Safety and efficacy of radiofrequency-assisted ALPPS (RALPPS) in patients with cirrhosis-related hepatocellular carcinoma. International journal of hyperthermia : the official journal of European Society for Hyperthermic Oncology, North American Hyperthermia Group. 2017;33(7):846–52. [DOI] [PubMed] [Google Scholar]
- 22.Tustumi F, Ernani L, Coelho FF, et al. Preoperative strategies to improve resectability for hepatocellular carcinoma: a systematic review and meta-analysis. HPB (Oxford). 2018;20(12):1109–18. 10.1016/j.hpb.2018.06.1798 [DOI] [PubMed] [Google Scholar]
- 23.Schadde E, Ardiles V, Robles-Campos R, et al. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg 2014;260(5):829-36; discussion 836-8. 10.1097/SLA.0000000000000947 [DOI] [PubMed] [Google Scholar]
- 24.Edmondson MJ, Sodergren MH, Pucher PH, et al. Variations and adaptations of associated liver partition and portal vein ligation for staged hepatectomy (ALPPS): Many routes to the summit. Surgery. 2016;159(4):1058–72. 10.1016/j.surg.2015.11.013 [DOI] [PubMed] [Google Scholar]
- 25.Jackson T, Siegel KA, Siegel CT. Rescue ALPPS: intraoperative conversion to ALPPS during synchronous resection of rectal cancer and liver metastasis. Case Rep Surg. 2014;2014:487852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tomassini F, D’Asseler Y, Giglio MC, et al. Hemodynamic changes in ALPPS influence liver regeneration and function: results from a prospective study. HPB (Oxford). 2019;21(5):557–65. 10.1016/j.hpb.2018.09.005 [DOI] [PubMed] [Google Scholar]
- 27.Kang D, Schadde E. Hypertrophy and Liver Function in ALPPS: Correlation with Morbidity and Mortality. Visceral medicine. 2017;33(6):426–33. 10.1159/000479477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peng SY, Huang CY, Wang XA, et al. The clinical value of terminal branches portal vein embolization for hepatocellular carcinoma with insufficient future liver remnant. Zhonghua wai ke za zhi [Chinese journal of surgery]. 2021;59(10):829–35. [DOI] [PubMed] [Google Scholar]
- 29.Izzo F, Granata V, Grassi R, et al. Radiofrequency Ablation and Microwave Ablation in Liver Tumors: An Update. Oncologist. 2019;24(10):e990–1005. 10.1634/theoncologist.2018-0337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rassam F, Olthof PB, van Lienden KP, et al. Comparison of functional and volumetric increase of the future remnant liver and postoperative outcomes after portal vein embolization and complete or partial associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Annals of translational medicine. 2020;8(7):436. 10.21037/atm.2020.03.191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu X, Rao J, Zhou X, et al. Partial ALPPS versus complete ALPPS for staged hepatectomy. BMC Gastroenterol. 2019;19(1):170. 10.1186/s12876-019-1090-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheng J, Hong DF, Zhang CW, et al. Transcatheter arterial chemoembolization after percutaneous microwave ablation and portal vein embolization for advanced hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2023;22(2):213–6. 10.1016/j.hbpd.2022.06.013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is provided within the supplementary information files.