Abstract
Objective
To investigate the relationship between uric acid to high-density lipoprotein cholesterol ratio (UHR) and circulating α-klotho levels in U.S. adults.
Methods
A cross-sectional study used data from the National Health and Nutrition Examination Survey (NHANES) from 2007 to 2016. Circulating α-klotho was defined as the dependent variable and UHR was defined as the independent variable. Multivariable linear regression was performed to assess the relationship between the independent and dependent variables. The nonlinear relationship and effect size between UHR and α-klotho were evaluated using smooth curve fitting and threshold effect analysis. Subgroup analysis and sensitivity analysis were conducted to determine the stability of the results. The diagnostic performance of UHR and α-klotho in common elderly diseases was compared using ROC (Receiver Operating Characteristic) analysis.
Results
Among 12,849 participants, there was a negative relationship between the UHR and circulating α-klotho. In the fully adjusted overall model, each unit increase in UHR was associated with a decrease of 4.1 pg/mL in α-klotho. The threshold effect analysis showed that before the inflection point of 8.2, each unit increase in UHR was associated with a decrease of 15.0 pg/mL in α-klotho; beyond the inflection point of 8.2, each unit increase in UHR was associated with a decrease of 2.8 pg/mL in α-klotho. Subgroup analyses and sensitivity analysis indicated that the relationship between UHR and α-klotho remained stable across most populations. The ROC diagnostic test indicated that the evaluative efficacy of UHR in diagnosing age-related diseases was comparable to that of α-klotho.
Conclusion
This study revealed that the UHR was associated with the circulating α-klotho concentration, with a negative association observed in most cases. This finding suggested that the UHR might be a promising indicator for evaluating circulating α-klotho levels.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12944-024-02234-6.
Keywords: α-klotho, HDL cholesterol, Uric acid, Cross-sectional study, UHR index, NHANES database
Introduction
Since Kuro-OM, Midentified aging phenotypes such as arteriosclerosis, osteoporosis, skin aging, and shortened lifespan in transgenic mice with disrupted klotho genes [1], extensive research has explored the relationship between α-klotho, the predominant klotho protein, and health [2]. Subsequent studies have determined that α-klotho, which is primarily expressed in the kidneys, choroid plexus, and parathyroid glands, manifests in two forms: membrane-bound and circulating [3]. The membrane-bound α-klotho is crucial for regulating the balance of calcium and phosphate within the body, whereas the circulating form, derived from the cleavage of its membrane-bound counterpart, functions hormonally throughout the body. This form exhibits anti-aging, anti-inflammatory, and anti-fibrotic properties; regulates the cell cycle; alleviates oxidative stress; and inhibits the progression of various diseases [4–7]. Recent studies consistently demonstrate that lower levels of circulating α-klotho are associated with an increased mortality risk, while higher levels correlate with extended survival times [8–10]. Therefore, identifying a convenient predictor of circulating α-klotho levels holds clinical significance for health monitoring and prognostic assessment.
Historically, research on α-klotho has focused on its impact on diseases and prognosis, often neglecting that its levels may be influenced by factors such as inflammation, metabolism, and hormones. The uric acid (UA) to high-density lipoprotein cholesterol (HDL) ratio (UHR) emerges as a promising marker, reflecting inflammation and metabolic status with superior evaluative capabilities in conditions such as type 2 diabetes, metabolic syndrome, coronary artery disease, and hypertension, compared to evaluating HDL and UA independently [11–14]. While the relationship between UHR and serum α-klotho is not fully established, indirect evidence hints at a potential connection. Uric acid is primarily excreted by the kidneys, which also predominantly secrete α-klotho [15]. In cases of renal dysfunction, serum uric acid levels rise as α-klotho secretion diminishes [16], suggesting a negative association between uric acid and α-klotho. Furthermore, ionic homeostasis may play a role in this interaction. Fluctuations in calcium and phosphate ion levels may prompt calciprotein particles (comprising calcium phosphate and serum protein fetuin-A) to mediate phosphate-induced secretion of Fibroblast Growth Factor 23 (FGF23) by osteocytes. This process facilitates renal phosphate excretion and calcium retention [17–19]. Concurrently, FGF23 reduces renal and serum α-klotho levels [20]. Elevated FGF23 levels often coincide with increased uric acid, potentially due to FGF23’s role in inhibiting active vitamin D production [21], promoting parathyroid hormone (PTH) secretion, and downregulating uric acid transporters, leading to uric acid accumulation [22]. Although this relationship has not been conclusively validated, it is commonly observed in clinical settings [23, 24]. We propose that a reverse relationship consistently exists between uric acid and α-klotho. Additionally, there may be a link between HDL and α-klotho. Patients with metabolic syndrome and diabetes typically experience chronic inflammation [25, 26], where inflammatory factors suppress HDL secretion by the liver [27, 28] and enhance FGF23 levels, thereby reducing circulating α-klotho [29]. Another clinical study suggests that different klotho genotypes correlate with HDL levels, deepening the intrinsic connection between circulating α-klotho and HDL [30]. Therefore, although reductions in HDL commonly coincide with decreases in α-klotho, their relationship might be more intricate. In summary, uric acid and α-klotho often display a reverse trend, while HDL and α-klotho generally show a synchronous trend. Thus, we hypothesize that the UHR index, derived from these factors, could serve as an indicator of circulating α-klotho levels.
To validate the relationship between UHR and serum α-klotho and to identify a simple and convenient health assessment indicator, we utilized data from the National Health and Nutrition Examination Survey (NHANES) to provide evidence for the clinical application of this index.
Materials and methods
The study utilized data from the NHANES conducted by the National Center for Health Statistics (NCHS). NHANES is a comprehensive survey designed to collect representative information on the health and nutrition of the civilian population in the United States, including demographics, socio-economic status, dietary habits, and health-related issues. To ensure the diversity of the sample, NHANES employs a stratified, multistage probability sampling method to select participants from across the country. The study protocol was approved by the Research Ethics Review Board of the NCHS at the Centers for Disease Control and Prevention (CDC), and all participants provided written informed consent. Detailed information can be found on the NHANES website.
Data and sample sources
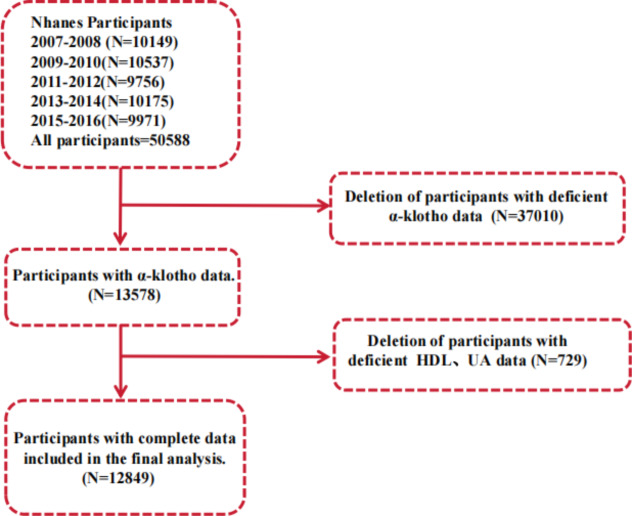
In this study, we primarily focused on adults from the NHANES 2007–2016 study cycle. The initial sample included 50,588 participants. We first excluded participants with missing serum α-klotho data (n = 37,010). Next, we excluded those with HDL and UA data missing(n = 729). Ultimately, 12,849 participants were included as the primary study subjects. Details are shown in Fig. 1.
Fig. 1.
Flow chart of the participants selection process
Assessment of UHR and circulation α-klotho level
HDL and uric acid were measured from blood samples drawn from participants in a fasting state in the morning. The steps for HDL measurement were as follows: A magnesium sulfate/dextran solution was added to the sample, forming water-soluble complexes with non-HDL cholesterol, which did not react with the measurement reagents in subsequent steps. Then, by adding polyethylene glycol esterase, HDL cholesterol esters were converted to HDL cholesterol. The hydrogen peroxide generated in this reaction reacted with 4-aminoantipyrine and HSDA to form a purple or blue dye. Finally, laboratory researchers determined HDL levels by photometric measurement at 600 nm. The steps for UA measurement were as follows: Serum uric acid concentration was measured using the timed endpoint method with a DxC800 automated chemical analyzer. Uric acid was oxidized by uricase to produce allantoin and hydrogen peroxide. Hydrogen peroxide reacted with 4-aminoantipyrine (4-AAP) and 3,5-dichloro-2-hydroxybenzenesulfonate (DCHBS) in a peroxidase-catalyzed reaction to produce a colored product, which was then measured photometrically at 520 nm to determine uric acid levels. Then, UHR (%) was then calculated by dividing UA (mg/dL) by HDL (mg/dL) and multiplying by 100 [31, 32].
Serum Klotho levels was determined by the IBL ELISA method. Blood samples were also drawn from participants in a fasting state in the morning. Until the formal operation, samples received on dry ice were stored at -80 °C. The researchers analyzed the samples in duplicate, and the average of the two measurements was used to calculate the final serum free α-klotho value [33].
Covariables
This study considered multiple variables that could influence the association between UHR and circulation α-klotho. These variables encompassed a range of demographic characteristics of the study population, including age, race, marital status, education level, and income-to-poverty ratio. Additionally, lifestyle factors such as smoking and drinking habits, BMI, and metabolic diseases were included. Smoking history was determined by whether the participant had ever smoked more than 100 cigarettes. Drinking history was assessed based on whether the participant had consumed 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of liquor within the past year. In addition, the study considered common causes and diseases that may affect metabolic levels and α-klotho, such as eGFR, serum vitamin D (VD), hypertension (HTN), coronary vascular disease (CVD), diabetes (DM), stroke, chronic kidney disease (CKD) and Cancer. These conditions were identified through questionnaires and laboratory indicators. Specific questionnaire content can be found on the NHANES website.
Statistical analyses
According to NCHS recommendations, appropriate weights were applied to each analysis conducted in this study. For normally distributed data, t-tests were used to compare groups, while non-normally distributed data were compared using the Mann-Whitney U test or Kruskal-Wallis rank sum test. For comparisons between categorical variables, the chi-square test or Fisher’s exact test was employed. Participants were stratified into three groups based on UHR tertiles, specifically tertile 1 (CMIQ1 ≤ 33rd percentile), tertile 2 (CMIQ2 > 33rd percentile to ≤ 66th percentile), and tertile 3 (CMIQ3 > 66th percentile).
In assessing association between independent and dependent variables, multivariable linear regression models were utilized. Smooth curve fitting was employed to illustrate the non-linear association between UHR and circulation α-klotho levels. In case of non-linear association, a recursive algorithm was applied to determine the threshold effects of non-linear models and identify meaningful inflection points. Notably, this study employed three different models for multivariable linear regression analysis to ascertain the association between UHR and circulation α-klotho levels. In Model 1, adjustments were not made for any covariables. In Model 2, adjustments were made for age, sex, and race. In Model 3, adjustments were made for age, sex, marital status, race, income-to-poverty ratio, education level, smoking and drinking habits, BMI, eGFR, serum vitamin D levels, HTN, CVD, DM, Stroke, Cancer, and CKD. Additionally, subgroup analyses were conducted on several covariables of interest to assess the stability and reliability of the study. Furthermore, to demonstrate the stability of UHR and serum α-klotho levels across different populations, drug-naive participants were selected, and their association would be validated through multivariable linear regression analysis. Lastly, ROC analysis was performed to compare the diagnostic performance of UHR and serum α-klotho levels for several common diseases. All analyses were performed using R (version 4.2.1) and Empower Stats (version 4.1).
Results
Characteristics of participants
We analyzed data from 12,849 participants collected by NHANES from 2007 to 2016 to investigate the relationship between UHR and serum α-klotho. Since both UHR and α-klotho are continuous variables, we grouped the participants according to tertiles of UHR. Significant differences (P < 0.05) were observed in the distribution of age, sex, lipid levels, blood glucose, α-klotho, eGFR, serum vitamin D, BMI, income-to-poverty ratio, marital status, smoking, drinking, HTN, blood lipids, DM, stroke, CVD and CKD across the three tertiles. Participants in the T3 group exhibited higher disease risk, poorer lifestyle habits, and higher UHR levels compared to the other groups, as detailed in Table 1.
Table 1.
Characteristics of participants
| T1 | T2 | T3 | P | |
|---|---|---|---|---|
| N | 4277 | 4224 | 4348 | - |
| Age(years) | 56.1 ± 10.5 | 56.5 ± 10.2 | 56.0 ± 10.5 | 0.0358 |
| BMI | 26.7 ± 5.7 | 30.0 ± 6.4 | 32.1 ± 6.5 | < 0.0001 |
| GLU(mg/dL) | 103.0 ± 27.7 | 112.7 ± 37.9 | 117.6 ± 37.6 | < 0.0001 |
| HDL(mg/dL) | 70.2 ± 17.1 | 51.7 ± 9.1 | 39.7 ± 7.6 | < 0.0001 |
| TC(mg/dL) | 206.7 ± 39.1 | 199.7 ± 40.8 | 195.3 ± 45.6 | < 0.0001 |
| TG(mg/dL) | 93.4 ± 95.6 | 129.3 ± 76.0 | 183.0 ± 130.8 | < 0.0001 |
| LDL(mg/dL) | 117.6 ± 34.8 | 120.6 ± 35.0 | 117.4 ± 37.8 | 0.0071 |
| eGFR(mL/min/1.73 m²) | 97.84 ± 32.57 | 108.40 ± 37.22 | 114.64 ± 40.13 | < 0.0001 |
| Uric acid(mg/dL) | 4.36 ± 0.96 | 5.49 ± 0.97 | 6.68 ± 1.24 | < 0.0001 |
| α-klotho(pg/mL) | 881.3 ± 311.3 | 839.4 ± 289.8 | 810.8 ± 266.9 | < 0.0001 |
| VD(nmol/L) | 80.0 ± 32.5 | 71.8 ± 27.2 | 67.6 ± 24.5 | < 0.0001 |
| Income-poverty ratio (%) | 3.4 ± 1.6 | 3.2 ± 1.6 | 3.1 ± 1.6 | < 0.0001 |
| Male(%) | 19.4 | 51.2 | 75.2 | < 0.0001 |
| Ethnic(%) | 0.058 | |||
| Non-Hispanic White | 74.1 | 71.4 | 73.3 | |
| Non-Hispanic Black | 9.4 | 9.1 | 8.8 | |
| Other Race | 16.6 | 19.5 | 17.9 | |
| Married(%) | 64.1 | 66 | 67.9 | < 0.0001 |
| College and above(%) | 67.3 | 60 | 57.3 | < 0.0001 |
| Drinking(%) | 76.7 | 76.4 | 80.1 | < 0.0001 |
| Smoking(%) | 43.3 | 46.5 | 54.5 | < 0.0001 |
| CVD(%) | 2.1 | 4.3 | 6.5 | < 0.0001 |
| DM(%) | 7.2 | 13.8 | 20 | < 0.0001 |
| HTN(%) | 31.5 | 42.5 | 51.6 | < 0.0001 |
| CKD(%) | 8.39 | 5.69 | 6.26 | < 0.0001 |
| Cancer(%) | 13.1 | 13.9 | 13.5 | 0.5701 |
| Stroke(%) | 2.5 | 2.9 | 4.5 | < 0.0001 |
Note T: Tertile, TC: Total Cholesterol, TG: Triglycerides, LDL: Low-Density Lipoprotein Cholesterol, HDL: High-Density Lipoprotein Cholesterol, GLU: Glucose, eGFR: Estimated Glomerular Filtration Rate, VD: serum vitamin D, CVD: Cardiovascular Disease, DM: Diabetes Mellitus, HTN: Hypertension, CKD: Chronic Kidney Disease
Association between UHR and a-klotho
After conducting multivariable logistic regression analysis across three models, we observed a negative association between UHR and serum α-klotho levels. In fully adjusted Model 3, the independent effect of UHR on serum α-klotho levels was (β=-4.1, 95% CI: -5.4, -2.7), indicating that with each unit increase in UHR, serum α-klotho decreases by 4.1 pg/mL (see Table 2). This negative association persisted across UHR tertile groups (P for Trend < 0.001), with the most pronounced decline in α-klotho observed in the T3 group (β=-37.5, 95% CI: -54.3, -20.7) (see Table 3).
Table 2.
Multivariable regression analysis of the relationship between UHR and its components with circulating α-klotho
| Exposure | Model1 | Model2 | Model3 | |||
|---|---|---|---|---|---|---|
| β(95% CI) | P | β(95% CI) | P | β(95% CI) | P | |
| UHR | -6.6 (-7.6, -5.5) | < 0.001 | -6.2 (-7.2, -5.2) | < 0.001 | -4.1 (-5.4, -2.7) | < 0.001 |
| UA | -33.3(-36.9, -29.6) | < 0.001 | -30.7 (-34.7, -26.8) | < 0.001 | -25.7 (-30.5, -21.0) | < 0.001 |
| HDL | 0.5 (0.2, 0.8) | < 0.001 | 0.1 (-0.2, 0.4) | 0.507 | -0.0 (-0.4, 0.4) | 0.93 |
Note Model 1:unadjusted; Model 2: adjust for gender, age, race; Model 3: adjust for gender, age, race, marital status, Income-poverty ratio, BMI, education, smoking, drinking, eGFR, VD, CVD, DM, HTN, Cancer, CKD, Stroke
Table 3.
Multivariable regression analysis of the relationship between UHR groups and its components groups with circulating α-klotho
| Exposure | Tertile group | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|
| β(95% CI) | P | β(95% CI) | P | β(95% CI) | P | ||
| UHR | 0.68–8.73 | Ref | - | Ref | - | Ref | - |
| 8.73–12.85 | -46.4 (-59.4, -33.4) | < 0.001 | -44.1 (-57.1, -31.2) | < 0.001 | -35.1 (-49.4, -20.8) | < 0.001 | |
| 12.93–39.62 | -72.6 (-85.5, -59.7) | < 0.001 | -54.7 (-68.8, -40.6) | < 0.001 | -37.5 (-54.3, -20.7) | < 0.001 | |
| groups trend | -7.5 (-8.9, -6.2) | < 0.001 | -5.6 (-7.1, -4.1) | < 0.001 | -3.8 (-5.5, -2.0) | < 0.001 | |
| UA | 0.40–4.70 | Ref | Ref | Ref | - | ||
| 4.80–5.90 | -46.7 (-59.8, -33.6) | < 0.001 | -38.3 (-51.7, -24.9) | < 0.001 | -32.8 (-47.6, -17.9) | < 0.001 | |
| 6.10–13.00 | -98.9 (-111.8, -86.0) | < 0.001 | -86.5 (-100.5, -72.5) | < 0.001 | -68.7 (-85.0, -52.4) | < 0.001 | |
| groups trend | -36.7 (-41.4, -31.9) | < 0.001 | -32.1 (-37.3, -27.0) | < 0.001 | -25.5 (-31.5, -19.4) | < 0.001 | |
| HDL | 10.82–42.92 | Ref | Ref | Ref | - | ||
| 44.08–56.84 | 10.5 (-2.5, 23.6) | 0.113 | 0.8 (-12.3, 13.9) | 0.905 | 0.2 (-14.2, 14.6) | 0.98 | |
| 58.00-225.83 | 25.7 (12.4, 39.0) | < 0.001 | 7.4 (-6.5, 21.3) | 0.296 | 2.5 (-13.6, 18.6) | 0.759 | |
| groups trend | 0.8 (0.4, 1.3) | < 0.001 | 0.3 (-0.2, 0.7) | 0.265 | 0.1 (-0.4, 0.6) | 0.742 | |
Note Model 1:unadjusted; Model 2: adjust for gender, age, race; Model 3: adjust for gender, age, race, marital status, Income-poverty ratio, BMI, education, smoking, drinking, eGFR, VD, CVD, DM, HTN, Cancer, CKD, Stroke
Simultaneously, we found that the association between HDL and α-klotho was not significant. Although there was a significant association between UA and α-klotho, the multivariable regression analysis by tertiles showed that the 95% CI for UA’s T3 group [-68.7 (-85.0, -52.4)] was wider than that for UHR’s T3 group [-37.5 (-54.3, -20.7)], indicating that the stability of the association between UA and α-klotho is weaker compared to that of UHR and α-klotho.
Non-linear relationship between UHR and α-klotho
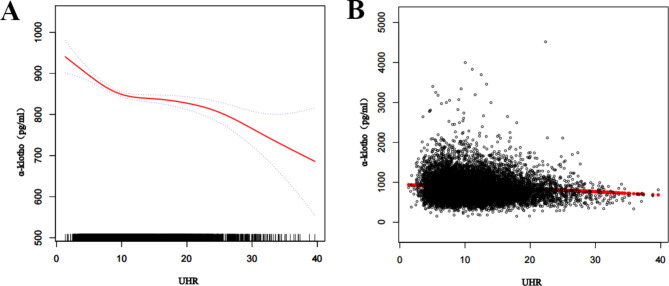
We performed smooth curve fitting and threshold effect analysis to investigate the relationship between UHR levels and serum α-klotho. The results indicated a negative, nonlinear relationship, as shown in Fig. 2. The threshold effect analysis revealed a significant difference in the effect of UHR on α-klotho before and after the inflection point at UHR 8.2. Specifically, at the UHR inflection point of 8.2, the serum α-klotho level was 862 pg/mL. Before the inflection point of 8.2, each 1% increase in UHR was associated with a 15.0 pg/mL decrease in α-klotho levels. After the inflection point, each 1% increase in UHR was associated with a 2.8 pg/mL decrease in α-klotho levels (see Table 4).
Fig. 2.
The association between UHR and α-klotho level. (A) The red line represents the curve fitting between the independent variable and the dependent variable. The blue line indicates the 95% confidence interval for the fit. (B) Each black dot represents a sample from a participant
Table 4.
Threshold effect analysis of the relationship between UHR and circulating α-klotho
| Results of threshold effect analysis | Outcome | P-value |
|---|---|---|
| Model 1 | - | - |
| one-line effect | -4.1 (-5.4, -2.7) | <0.001 |
| Model 2 | - | - |
| Break point (K) | 8.2 | - |
| < K | -15.0 (-20.9, -9.0) | <0.001 |
| > K | -2.8 (-4.3, -1.3) | <0.001 |
| Difference in effect before and after the breakpoint | 12.2 (5.7, 18.7) | <0.001 |
| α-klotho content at the folding point | 862.0 (852.6, 871.4) | - |
| Logarithmic likelihood ratio test P-value | - | < 0.001 |
Results of subgroup analyses
To determine the stability of the association between UHR and serum α-klotho levels, we conducted subgroup analyses. The results indicated that the negative association between UHR and serum α-klotho levels remained stable across most subgroups, supporting the reliability of the study. Additionally, the subgroup analyses revealed that gender and BMI might influence the association between UHR and serum α-klotho levels, as detailed in Table 5.
Table 5.
Subgroup analyses of the association between UHR and serum α-klotho
| Subgroup | β(95% CI) | P for interaction |
|---|---|---|
| Male | -2.8 (-4.4, -1.1) | 0.0058 |
| Female | -6.3 (-8.4, -4.2) | |
| Age < 60 | -4.5 (-6.3, -2.8) | 0.3878 |
| Age > 60 | -3.6 (-5.4, -1.8) | |
| Drinking | -4.2 (-5.7, -2.7) | 0.7155 |
| No Drinking | -3.7 (-6.1, -1.4) | |
| Smoking | -3.7 (-5.4, -2.1) | 0.4771 |
| No Smoking | -4.5 (-6.4, -2.7) | |
| BMI < 25 | -8.0 (-11.3, -4.7) | 0.0010 |
| BMI:25–30 | -3.5 (-5.8, -1.2) | |
| BMI > 30 | -2.3 (-4.0, -0.5) | |
| CVD | -6.6 (-10.8, -2.3) | 0.2230 |
| No CVD | -3.9 (-5.3, -2.4) | |
| DM | -4.7 (-7.3, -2.1) | 0.5408 |
| No DM | -3.8 (-5.3, -2.3) | |
| Cancer | -2.1 (-5.6, 1.4) | 0.2236 |
| No Cancer | -4.4 (-5.8, -3.0) | |
| HTN | -4.0 (-5.7, -2.4) | 0.9115 |
| No HTN | -4.2 (-6.0, -2.3) | |
| Stroke | -3.0 (-8.2, 2.3) | 0.6781 |
| No Stroke | -4.1 (-5.5, -2.7) | |
| CKD | -3.8 (-7.4, -0.2) | 0.8855 |
| No CKD | -4.1 (-5.5, -2.6) |
Note BMI: Body Mass Index, CVD: Cardiovascular Disease, DM: Diabetes Mellitus, HTN: Hypertension, CKD: Chronic Kidney Disease
Sensitivity analyses
Considering the impact of medications on serum α-klotho, uric acid, and lipid profiles, this section focuses on the association between UHR and α-klotho in a population not taking medications. We excluded individuals taking RAAS inhibitors (Including angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, and aldosterone receptor antagonists.), statins, allopurinol, and febuxostat, as well as other medications. ultimately including 7442 participants for the study. Similar to the main study, we analyzed the association between UHR and α-klotho using three multivariable regression models. The results confirmed that the association between UHR and α-klotho persisted, indicating the stability of the association between UHR and circulating α-klotho. Details can be found in Table 6.
Table 6.
Multivariable regression analysis of UHR and circulating α-klotho in unmedicated population
| Exposure | Model1 | Model2 | Model3 | |||
|---|---|---|---|---|---|---|
| β(95% CI) | P | β(95% CI) | P | β(95% CI) | P | |
| UHR | -6.1 (-7.5, -4.6) | < 0.001 | -4.2 (-5.8, -2.6) | < 0.001 | -4.2 (-6.2, -2.3) | < 0.001 |
| UHR T1: 1.35–8.12 | ref | ref | ref | |||
| UHR T2: 8.12–12.26 | -42.8 (-60.0, -25.7) | < 0.001 | -32.8 (-50.4, -15.3) | < 0.001 | -33.3 (-53.1, -13.4) | < 0.001 |
| UHR T3: 12.26–37.05 | -65.2 (-82.3, -48.0) | < 0.001 | -41.3 (-60.3, -22.2) | < 0.001 | -40.9 (-63.7, -18.1) | < 0.001 |
| UHR groups trend | -6.9 (-8.8, -5.1) | < 0.001 | -4.3 (-6.3, -2.2) | < 0.001 | -4.1 (-6.6, -1.6) | < 0.001 |
Note Model 1:unadjusted; Model 2: adjust for gender, age, race; Model 3: adjust for gender, age, race, marital status, Income-poverty ratio, BMI, education, smoking, drinking, eGFR, VD, CVD, DM, HTN, Cancer, CKD, Stroke
ROC curves of UHR and α-klotho in Age-related diseases
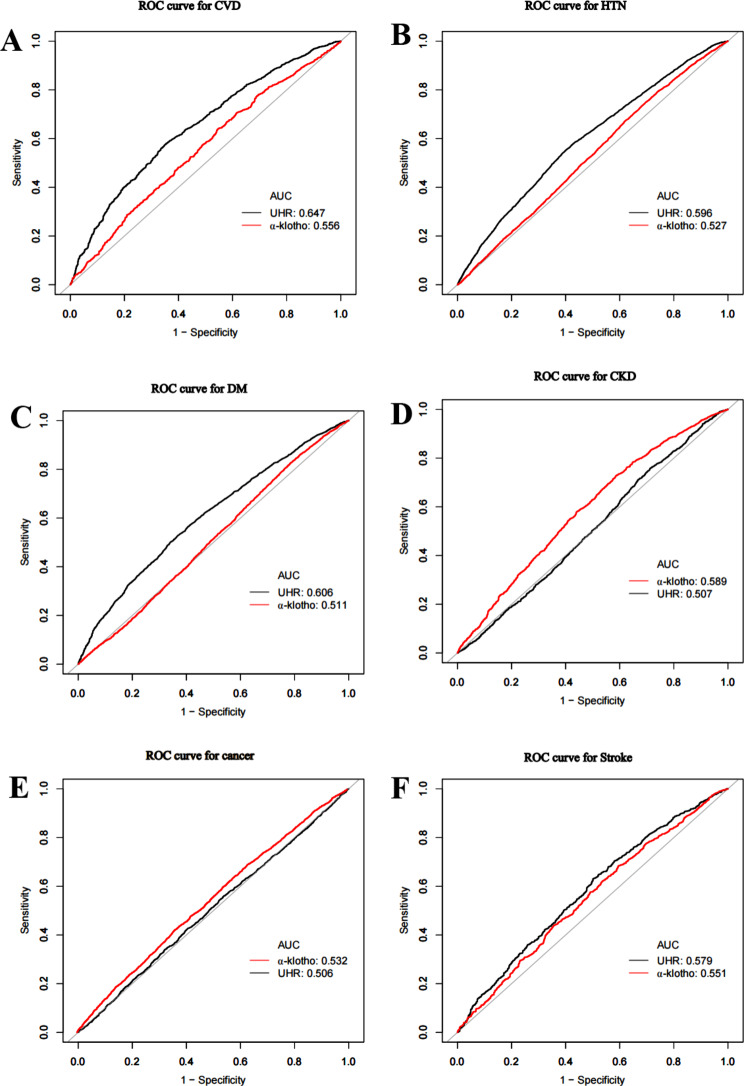
To better evaluate the diagnostic efficacy of UHR and α-klotho in age-related diseases, we conducted diagnostic tests on four common diseases. The results showed that UHR has slightly lower evaluative value compared to α-klotho in diagnosing CKD. For diagnosing DM, HTN, stroke, and CVD, UHR exhibits evaluative efficacy that is no less than that of circulating α-klotho. However, both of them are less effective in diagnosing cancer, as detailed in Fig. 3 and Table S1.
Fig. 3.
ROC curves of UHR and α-klotho in Age-related diseases: (A) ROC curves of UHR and α-klotho in CVD (B) ROC curves of UHR and α-klotho in HTN (C) ROC curves of UHR and α-klotho in DM (D) ROC curves of UHR and α-klotho in CKD (E) ROC curves of UHR and α-klotho in Cancer (F) ROC curves of UHR and α-klotho in Stroke
Discussion
This cross-sectional study encompassed a total of 12,849 participants. Among these, those with poor lifestyle habits and metabolic diseases exhibited higher UHR levels and lower serum α-klotho levels. Additionally, after adjusting for other covariables, multivariable regression analysis across three models consistently indicated a negative association between UHR and serum α-klotho. Subsequent smooth curve fitting analysis reinforced the negative nonlinear relationship between UHR and serum α-klotho, while threshold effect analysis confirmed varying impacts of UHR values before and after the inflection point. Consequently, the results suggest that the UHR index is negatively related to α-klotho, supporting its potential as a novel biomarker for assessing circulating α-klotho levels.
Currently, research on the relationship between UHR and circulating α-klotho is sparse, with no direct evidence to corroborate this link. However, indirect evidence points to a connection. The two major components of UHR, UA and HDL, may be implicated in the pathophysiological mechanisms related to α-klotho. Lee HJ proposed that UA might associated with α-klotho via FGF23 as an intermediary [34]. When FGF23 and α-klotho interact with FGFR in the parathyroid gland, they can diminish PTH [35, 36], enhancing the excretion of uric acid in renal tubules [37]. Conversely, impaired FGF23/α-klotho signaling elevates PTH, diminishes UA excretion, and increases serum UA levels [38]. This mechanism links α-klotho and uric acid to some extent. Additionally, hyperuricemia often corresponds with reduced circulating α-klotho levels. Various studies indicate that elevated uric acid levels are frequently observed in patients with renal insufficiency [39–43], and interventions targeting uric acid may alleviate kidney damage [44, 45]. Given that the kidneys are the primary production site for α-klotho, a decline in renal function would reduce α-klotho levels while uric acid accumulates, leading to simultaneous increases in uric acid and decreases in α-klotho. Similarly, HDL and α-klotho levels often decline concurrently. Chronic inflammation can affect liver ApoA-I synthesis, thus reducing HDL production [46]. Inflammatory factors may also elevate FGF23 through inflammatory pathways, reducing circulating α-klotho levels [47]. Interestingly, treatments like statins, niacin, and fibrates are known to increase HDL levels and simultaneously elevate α-klotho content [48, 49]. Moreover, while our study did not find statistical significance between HDL and α-klotho, they exhibited a similar trend in the baseline characteristics of the population. Though the underlying mechanism remains unclear, HDL, and α-klotho consistently fluctuate showed a similar trend in fluctuating in the same direction. In summary, this study’s conclusion that UHR is negatively association with α-klotho is align with clinical and physiological evidence, affirming UHR’s potentialaligns with clinical and physiological insights. Therefore, UHR indeed shows promise as an indicator for assessing α-klotho levels in the body.
Moreover, subgroup analyses indicated that gender and BMI might influence the association between UHR and serum α-klotho levels. The negative relationship of UHR and α-klotho was significantly observed in female participants compared to males, possibly due to differences in how estrogen and androgen affect UA, HDL, and α-klotho. Influenced by estrogen, UA and HDL levels are generally lower in females [50]. However, once females reach menopause, the rapid decline in estrogen accelerates aging and exacerbates metabolic diseases. This could explain the more pronounced negative impact of UHR on α-klotho among 40-79-year-old female participants in this study [51, 52]. Additionally, patients with lower BMI showed a more significant negative association between UHR and α-klotho, possibly due to higher HDL and lower UA levels, resulting in reduced UHR values. This is consistent with the threshold analysis, which indicated more significant fluctuations in α-klotho before a UHR value of 8.2. This may be because individuals with lower BMI have fewer pro-inflammatory factors in their blood; conversely, increased BMI sharply elevates pro-inflammatory factors released by adipocytes, leading to abnormal lipid profiles and the rapid development of adverse conditions, causing a sudden drop in α-klotho levels [53, 54]. Furthermore, many studies have observed that lighter-weight patients have higher circulating α-klotho levels, which might explain the greater fluctuations in serum α-klotho among lower BMI patients [55]. Meanwhile, Considering the impact of urate-lowering drugs, RAAS inhibitors, statins, and other medications on UHR and α-klotho, we conducted a sensitivity analysis. The results confirmed that the association between UHR and α-klotho remained robust, even after excluding individuals taking these medications. Despite the known effects of kidney disease, metabolic disorders, diabetes, age, and medications on HDL, UA, and α-klotho [56–58], our study determined that these factors did not influence the association between UHR and α-klotho. To verify that the UHR metric can assess α-klotho levels while maintaining diagnostic efficacy for age-related diseases akin to that of α-klotho, we conducted ROC diagnostic tests. The results indicated that UHR, though less effective than α-klotho in diagnosing CKD, performed slightly better than α-klotho in diagnosing other common age-related diseases such as CVD, DM, stroke, and HTN. However, both metrics were less effective in diagnosing cancer. These findings suggest that UHR can effectively assess α-klotho levels in most cases and has the potential to be an indicator for evaluating age-related diseases and α-klotho levels in the body.
In conclusion, our study has several strengths. To our knowledge, this is the first study to explore and establish the relationship between UHR and α-klotho, demonstrating its novelty. Secondly, we observed that the measurement cost of α-klotho is higher than that of HDL and UA, and current α-klotho testing kits on the market vary in quality, with inconsistent measurement standards. Therefore, our study recommends using the simple and portable UHR index to estimate α-klotho fluctuations and levels, significantly reducing the cost and variability of assessing α-klotho [59]. However, there are some limitations to our study. Firstly, many potential factors influence UHR and α-klotho, and the physiological role of α-klotho is highly complex and not fully understood. Although this study included covariables such as CKD, HTN, and DM, we cannot exclude all potential confounding variables affecting the results. Therefore, the conclusions of this study should be validated by subsequent research. Secondly, although cross-sectional studies are useful for preliminary exploratory research and hypothesis generation, they cannot provide causal evidence. Although we found a negative association between the UHR index and blood α-klotho, we could not explain the intrinsic mechanisms underlying their association. Future research should consider longitudinal designs or experimental methods to deepen the understanding of this issue. Thirdly, the range for determining low circulating α-klotho levels is not yet established, limiting our ability to compare the sensitivity and accuracy of UHR and other evaluative indicators in assessing low α-klotho levels. Although the ROC curve indicates that UHR has slightly strength diagnostic efficacy for age-related diseases than α-klotho, its effectiveness is modest. Therefore, further research is necessary to identify more effective indicators. Finally, significant differences in genetic background, lifestyle, medical standards, and socioeconomic conditions exist across different countries and regions. Our findings may not be entirely applicable to other countries, so caution is needed when applying these results globally, taking into account local environmental and population characteristics. Future research should expand the sample size to include more countries and cultures, enhancing the generalizability and applicability of the findings.
Conclusion
This study confirmed a negative association between UHR and circulating α-klotho, with different evaluative effects of α-klotho values before and after the inflection point. Additionally, the study found that the negative association between UHR and α-klotho applies to most situations, indicating that this index has a certain stability in assessing circulating α-klotho levels.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge NHANES databases for providing their platforms and contributing meaningful datasets.
Abbreviations
- NCHS
National Center for Health Statistics
- BMI
Body Mass Index
- NHANES
National Health and Nutrition Examination Survey
- PTH
Parathyroid Hormone
- TG
Triglyceride
- HDL
High-Density Lipoprotein
- LDL
Low-density lipoprotein cholesterol
- UA
Uric Acid
- UHR
Uric acid to High-density lipoprotein cholesterol ratio
- FGF23
Fibroblast Growth Factor 23
- VD
Serum vitamin D
- CVD
Cardiovascular Disease
- DM
Diabetes Mellitus
- HTN
Hypertension
- CKD
Chronic Kidney Disease
Author contributions
Writing the first draft of the manuscript, statistical analyses, data organization, writing review, and editing : XC Huang and LS Hu.Research, statistical analyses, and editing : SY Tao, TT Xue, CZ Hou. Design research, supervision, editing, review, revision of the manuscript, and funding: J Li.All authors approved the final version of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81973836), National Key Research and Development Program of China (No. 2022YFC3500102), Scientifc and technological innovation project of China Academy of Chinese Medical Sciences (CI2021A00902), and High Level Chinese Medical Hospital Promotion Project (No. HLCMHPP2023065). The funders had no role in study design, data collection and analyses, decision to publish, or preparation of the manuscript.
Data availability
The data supporting the results of this study are available in NHANES database.Our analyses was conducted on the basis of publicly available data, and previous subjects signed an informed consent form. Thus, our research does not require renewed informed consent from participants or ethical approval from the NCHS Research Ethics Review Board. More detailed information can be obtained from the official NHANES website. (https://www.cdc.gov/nchs/nhanes/irba98.htm).
Declarations
Ethics approval and consent to participate
Our analyses were performed on the basis of publicly available data, with previous subjects signing an informed consent form.Therefore, this study has no ethical implications. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xuanchun Huang and Lanshuo Hu contributed equally to this work and share first authorship.
Contributor Information
Chengzhi Hou, Email: houchengzhijack@163.com.
Jun Li, Email: gamyylj@163.com.
References
- 1.Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;3906655:45–51. 10.1038/36285 [DOI] [PubMed] [Google Scholar]
- 2.Kuro- OM. The Klotho proteins in health and disease. Nat Rev Nephrol. 2019;15(1):27–44. 10.1038/s41581-018-0078-3 [DOI] [PubMed] [Google Scholar]
- 3.Lindberg K, Amin R, Moe OW, Hu MC, Erben RG, Östman Wernerson A, et al. The kidney is the principal organ mediating klotho effects. J Am Soc Nephrol. 2014;25(10):2169–75. 10.1681/ASN.2013111209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Sun Z. Current understanding of klotho. Ageing Res Rev. 2009;8(1):43–51. 10.1016/j.arr.2008.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu M, Liu T, Shang P, Zhang Y, Liu L, Liu T, et al. Acetyl-11-keto-β-boswellic acid ameliorates renal interstitial fibrosis via Klotho/TGF-β/Smad signalling pathway. J Cell Mol Med. 2018;2210:4997–5007. 10.1111/jcmm.13766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Oliveira RM. Klotho RNAi induces premature senescence of human cells via a p53/p21 dependent pathway. FEBS Lett. 2006;58024:5753–8. 10.1016/j.febslet.2006.09.036 [DOI] [PubMed] [Google Scholar]
- 7.Wang Y, Kuro-o M, Sun Z. Klotho gene delivery suppresses Nox2 expression and attenuates oxidative stress in rat aortic smooth muscle cells via the cAMP-PKA pathway. Aging Cell. 2012;11(3):410–7. 10.1111/j.1474-9726.2012.00796.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chuang MH, Wang HW, Huang YT, Jiang MY. Association between soluble α-klotho and mortality risk in middle-aged and older adults. Front Endocrinol (Lausanne). 2023(14)1246590. [DOI] [PMC free article] [PubMed]
- 9.Kresovich JK, Bulka CM. Low serum Klotho Associated with all-cause Mortality among a nationally Representative Sample of American adults. J Gerontol Biol Sci Med Sci. 2022;77(3):452–6. 10.1093/gerona/glab308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Semba RD, Cappola AR, Sun K, Bandinelli S, Dalal M, Crasto C. Plasma klotho and mortality risk in older community-dwelling adults. J Gerontol Biol Sci Med Sci. 2011;667:794–800. 10.1093/gerona/glr058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu J, Du X, Zhang S, Zang X, Xiao Z, Su R, et al. Diagnostic value of uric acid to high-density lipoprotein cholesterol ratio in abdominal aortic aneurysms. Ann Med. 2024;56:12357224. 10.1080/07853890.2024.2357224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deng F, Jia F, Sun Y, Zhang L, Han J, Li D, et al. Predictive value of the serum uric acid to high-density lipoprotein cholesterol ratio for culprit plaques in patients with acute coronary syndrome. BMC Cardiovasc Disord. 2024;24(1):155. 10.1186/s12872-024-03824-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou X, Xu J. Association between serum uric acid-to-high-density lipoprotein cholesterol ratio and insulin resistance in patients with type 2 diabetes mellitus. J Diabetes Investig. 2024;15(1):113–20. 10.1111/jdi.14086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang Y, Zhang J, Jia L, Su J, Ma M, Lin X. Uric acid to high-density lipoprotein cholesterol ratio predicts adverse cardiovascular events in patients with coronary chronic total occlusion. Nutr Metab Cardiovasc Dis. 2023;33(12):2471–8. 10.1016/j.numecd.2023.07.037 [DOI] [PubMed] [Google Scholar]
- 15.Adomako EA, Moe OW. Uric acid transport, transporters, and their pharmacological targeting. Acta Physiol (Oxf). 2023(238)2e13980. [DOI] [PubMed]
- 16.Martín-Vírgala J, Martín-Carro B, Fernández-Villabrille S, Ruiz-Torres MP, Gómez-Alonso C, Rodríguez-García M, et al. Soluble Klotho, a potential biomarker of chronic kidney Disease-Mineral Bone disorders involved in healthy ageing: lights and shadows. Int J Mol Sci. 2024;25(3):1843. [DOI] [PMC free article] [PubMed]
- 17.Quinn SJ, Thomsen AR, Pang JL, Kantham L, Bräuner-Osborne H, Pollak M, et al. Interactions between calcium and phosphorus in the regulation of the production of fibroblast growth factor 23 in vivo. Am J Physiol Endocrinol Metab. 2013;3043:E310–20. 10.1152/ajpendo.00460.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takashi Y, Fukumoto S. FGF23 beyond Phosphotropic Hormone. Trends Endocrinol Metab. 2018;2911:755–67. 10.1016/j.tem.2018.08.006 [DOI] [PubMed] [Google Scholar]
- 19.Akiyama KI, Miura Y, Hayashi H, Sakata A, Matsumura Y, Kojima M et al. Calciprotein particles regulate fibroblast growth factor-23 expression in osteoblasts. Kidney Int. 2020(97)4:702–12. [DOI] [PubMed]
- 20.Marsell R, Krajisnik T, Göransson H, Ohlsson C, Ljunggren O, Larsson TE et al. Gene expression analysis of kidneys from transgenic mice expressing fibroblast growth factor-23. Nephrol Dial Transpl. 2008(23)3827–33. [DOI] [PubMed]
- 21.Quarles LD. Skeletal secretion of FGF-23 regulates phosphate and vitamin D metabolism. Nat Rev Endocrinol. 2012;8(5):276–86. [DOI] [PMC free article] [PubMed]
- 22.Sugimoto R, Watanabe H, Ikegami K, Enoki Y, Imafuku T, Sakaguchi Y, et al. Down-regulation of ABCG2, a urate exporter, by parathyroid hormone enhances urate accumulation in secondary hyperparathyroidism. Kidney Int. 2017;913:658–70. 10.1016/j.kint.2016.09.041 [DOI] [PubMed] [Google Scholar]
- 23.Sakoh T, Nakayama M, Tsuchihashi T, Yoshitomi R, Tanaka S, Katafuchi E, et al. Associations of fibroblast growth factor 23 with urate metabolism in patients with chronic kidney disease. Metabolism. 2016;65(10):1498–507. 10.1016/j.metabol.2016.07.005 [DOI] [PubMed] [Google Scholar]
- 24.Bacchetta J, Cochat P, Salusky IB, Wesseling-Perry K. Uric acid and IGF1 as possible determinants of FGF23 metabolism in children with normal renal function. Pediatr Nephrol. 2012(27)7:1131–8. [DOI] [PMC free article] [PubMed]
- 25.Catrysse L, van Loo G. Inflammation and the metabolic syndrome: the tissue-specific functions of NF-κB. Trends Cell Biol. 2017;27(6):417–29. 10.1016/j.tcb.2017.01.006 [DOI] [PubMed] [Google Scholar]
- 26.Rohm TV, Meier DT, Olefsky JM, Donath MY. Inflammation in obesity, diabetes, and related disorders. Immunity. 2022;55(1):31–55. 10.1016/j.immuni.2021.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zuliani G, Volpato S, Blè A, Bandinelli S, Corsi AM, Lauretani F, et al. High interleukin-6 plasma levels are associated with low HDL-C levels in community-dwelling older adults: the InChianti study. Atherosclerosis. 2007;192:2384–90. 10.1016/j.atherosclerosis.2006.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nazir S, Jankowski V, Bender G, Zewinger S, Rye KA, van der Vorst EPC. Interaction between high-density lipoproteins and inflammation: function matters more than concentration! Adv Drug Deliv Rev. 2020;159:94–119. [DOI] [PubMed]
- 29.Czaya B, Faul C. FGF23 and inflammation-a vicious coalition in CKD. Kidney Int. 2019;964:813–5. 10.1016/j.kint.2019.05.018 [DOI] [PubMed] [Google Scholar]
- 30.Arking DE, Atzmon G, Arking A, Barzilai N, Dietz HC. Association between a functional variant of the KLOTHO gene and high-density lipoprotein cholesterol, blood pressure, stroke, and longevity. Circ Res. 2005(96)4:412–8. [DOI] [PubMed]
- 31.Zhou X, Xu J. Association between serum uric acid-to-high-density lipoprotein cholesterol ratio and insulin resistance in an American population: a population-based analysis. J Diabetes Investig. 2024;156:762–71. 10.1111/jdi.14170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bazmandegan G, Dehghani MH, Karimifard M, Kahnooji M, Balaee P, Zakeri MA, et al. Uric acid to HDL ratio: a marker for predicting incidence of metabolic syndrome in patients with type II diabetes. Nutr Metab Cardiovasc Dis. 2024;344:1014–20. 10.1016/j.numecd.2023.12.022 [DOI] [PubMed] [Google Scholar]
- 33.Yamazaki Y, Imura A, Urakawa I, Shimada T, Murakami J, Aono Y, et al. Establishment of sandwich ELISA for soluble alpha-klotho measurement: age-dependent change of soluble alpha-klotho levels in healthy subjects. Biochem Biophys Res Commun. 2010;398(3):513–8. 10.1016/j.bbrc.2010.06.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee HJ, Choi JY, Lee J, Kim D, Min JY, Min KB. Association between serum uric acid and α-klotho protein levels in the middle-aged population. Aging. 2022;6(14):2537–47. 10.18632/aging.203987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Silver J, Naveh-Many T. FGF23 and the parathyroid glands. Pediatr Nephrol. 2010;2511:2241–5. 10.1007/s00467-010-1565-3 [DOI] [PubMed] [Google Scholar]
- 36.Martin A, David V, Quarles LD. Regulation and function of the FGF23/klotho endocrine pathways. Physiol Rev. 2012;92(1):131–55. 10.1152/physrev.00002.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu L, Shi Y, Zhuang S, Liu N. Recent advances on uric acid transporters. Oncotarget. 2017;8(59):100852–62. 10.18632/oncotarget.20135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hu MC, Shiizaki K, Kuro-o M, Moe OW. Fibroblast growth factor 23 and Klotho: physiology and pathophysiology of an endocrine network of mineral metabolism. Annu Rev Physiol. 2013(75):503–33. [DOI] [PMC free article] [PubMed]
- 39.Li X, Sun J, Bu Q, Zhou B, Li L, Man X, et al. Association between serum uric acid levels and clinical outcomes in patients with acute kidney injury. Ren Fail. 2023;45(1):2169617. 10.1080/0886022X.2023.2169617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lapsia V, Johnson RJ, Dass B, Shimada M, Kambhampati G, Ejaz NI, et al. Elevated uric acid increases the risk for acute kidney injury. Am J Med. 2012;125(3):e3029–17. 10.1016/j.amjmed.2011.06.021 [DOI] [PubMed] [Google Scholar]
- 41.Mok Y, Lee SJ, Kim MS, Cui W, Moon YM, Jee SH. Serum uric acid and chronic kidney disease: the severance cohort study. Nephrol Dial Transpl. 2012;27(5):1831–5. 10.1093/ndt/gfr530 [DOI] [PubMed] [Google Scholar]
- 42.Chonchol M, Shlipak MG, Katz R, Sarnak MJ, Newman AB, Siscovick DS, et al. Relationship of uric acid with progression of kidney disease. Am J Kidney Dis. 2007;50(2):239–47. 10.1053/j.ajkd.2007.05.013 [DOI] [PubMed] [Google Scholar]
- 43.Ma Z, Wang X, Zhang J, Yang C, Du H, Dou F et al. The bidirectional relationship between chronic kidney Disease and Hyperuricemia: evidence from a Population-based prospective cohort study. Int J Environ Res Public Health. 2023(20)3:1728. [DOI] [PMC free article] [PubMed]
- 44.Peng YL, Tain YL, Lee CT, Yang YH, Huang YB, Wen YH et al. Comparison of uric acid reduction and renal outcomes of febuxostat vs allopurinol in patients with chronic kidney disease. Sci Rep. 2020(10)1:10734. [DOI] [PMC free article] [PubMed]
- 45.Chou HW, Chiu HT, Tsai CW, Ting IW, Yeh HC, Huang HC, et al. Comparative effectiveness of allopurinol, febuxostat and benzbromarone on renal function in chronic kidney disease patients with hyperuricemia: a 13-year inception cohort study. Nephrol Dial Transpl. 2018;9(33):1620–7. [DOI] [PubMed] [Google Scholar]
- 46.Grao-Cruces E, Lopez-Enriquez S, Martin ME, Montserrat-de la Paz S. High-density lipoproteins and immune response: a review. Int J Biol Macromol. 2022 (195):117–23. [DOI] [PubMed]
- 47.Rodríguez-Ortiz ME, Díaz-Tocados JM, Muñoz-Castañeda JR, Herencia C, Pineda C, Martínez-Moreno JM et al. Inflammation both increases and causes resistance to FGF23 in normal and uremic rats. Clin Sci (Lond). 2020(134)1:15–32. [DOI] [PubMed]
- 48.Janić M, Lunder M, Novaković S, Škerl P, Šabovič M. Expression of longevity genes Induced by a low-dose fluvastatin and Valsartan Combination with the potential to Prevent/Treat aging-related disorders. Int J Mol Sci. 2019;20(8):1844. 10.3390/ijms20081844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ostojic SM, Hillesund ER, Øverby NC, Vik FN, Medin AC. Individual nutrients and serum klotho levels in adults aged 40–79 years. Food Sci Nutr. 2023;116:3279–86. 10.1002/fsn3.3310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Palmisano P BT, Zhu L, Eckel RH, Stafford JM. Sex differences in lipid and lipoprotein metabolism. Mol Metab. 2018;15:45–55. [DOI] [PMC free article] [PubMed]
- 51.El Khoudary SR. Gaps, limitations and new insights on endogenous estrogen and follicle stimulating hormone as related to risk of cardiovascular disease in women traversing the menopause: a narrative review. Maturitas. 2017;104:44–53. [DOI] [PubMed]
- 52.El Khoudary SR, Thurston RC. Cardiovascular implications of the menopause transition: endogenous sex hormones and vasomotor symptoms. Obstet Gynecol Clin North Am. 2018;45(4):641–61. 10.1016/j.ogc.2018.07.006 [DOI] [PubMed] [Google Scholar]
- 53.Cui J, Yang Z, Wang J, Yin S, Xiao Y, Bai Y et al. A cross-sectional analysis of association between visceral adiposity index and serum anti-aging protein Klotho in adults. Front Endocrinol (Lausanne). 2023(14):1082504. [DOI] [PMC free article] [PubMed]
- 54.Poursistany H, Azar ST, Azar MT, Raeisi S. The current and emerging klotho-enhancement strategies. Biochem Biophys Res Commun. 2024(693):149357. [DOI] [PubMed]
- 55.Orces CH. The Association of Obesity and the Antiaging Humoral Factor Klotho in Middle-Aged and Older Adults. ScientificWorldJournal. 2022(2022):7274858. [DOI] [PMC free article] [PubMed]
- 56.Mao S, Wang X, Wu L, Zang D, Shi W. Association between klotho expression and malignancies risk and progression: a meta-analysis. Clin Chim Acta. 2018;484:14–20. 10.1016/j.cca.2018.05.033 [DOI] [PubMed] [Google Scholar]
- 57.Tang A, Zhang Y, Wu L, Lin Y, Lv L, Zhao L et al. Klotho’s impact on diabetic nephropathy and its emerging connection to diabetic retinopathy. Front Endocrinol (Lausanne). 2023(14):1180169. [DOI] [PMC free article] [PubMed]
- 58.Ihira H, Nakano S, Yamaji T, Katagiri R, Sawada N, Inoue M, et al. Plasma albumin, Bilirubin, and uric acid and the subsequent risk of Cancer: a case-cohort study in the Japan Public Health Center-based prospective study. Am J Epidemiol. 2024;29:kwae092. 10.1093/aje/kwae092 [DOI] [PubMed] [Google Scholar]
- 59.Heijboer AC, Blankenstein MA, Hoenderop J, de Borst MH, Vervloet MG, NIGRAM consortium. Laboratory aspects of circulating α-Klotho. Nephrol Dial Transpl. 2013;289:2283–7. 10.1093/ndt/gft236 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting the results of this study are available in NHANES database.Our analyses was conducted on the basis of publicly available data, and previous subjects signed an informed consent form. Thus, our research does not require renewed informed consent from participants or ethical approval from the NCHS Research Ethics Review Board. More detailed information can be obtained from the official NHANES website. (https://www.cdc.gov/nchs/nhanes/irba98.htm).