Abstract
Introduction
Pregnant women can choose from different prenatal genetic tests throughout their maternity journey. We aim to investigate the clinical, societal, and economic determinants influencing the selection of different options (non-invasive, invasive, or both).
Methods
A systematic survey focusing on maternity pathways was launched by the Region of Tuscany, Italy, to collect data on pregnant women’s experience, outcomes and satisfaction levels. Drawing from this survey, we retrospectively analyzed data on women who filled out the second-trimester questionnaire between March 2019 and February 2023 (n = 27,337), providing complete data on relevant variables. Logistic regression models were applied to identify the factors contributing to a higher likelihood of opting for non-invasive prenatal testing (NIPT) and invasive testing.
Results
Among the participants, 42.7 % chose only NIPT, 3.8 % opted for invasive tests exclusively, 1.3 % underwent both tests, and 52.2 % did not pursue any genetic testing. NIPT was more often chosen by older, Italian, highly educated, nulliparous women, who perceived better health, were employed (versus unemployed), had higher economic status, planned pregnancy, received hospital-based care (versus counseling center), under gynecologist supervision (versus midwife), not opted for combined testing and received pregnancy vaccinations. Conversely, invasive testing was more prevalent among older women but less common among those who were nulliparous, had Italian nationality, and had a perceived better health status. This group also tended to experience unplanned and high-risk pregnancy, did not take folate during pregnancy, received public hospital-based assistance, less frequently chose combined tests or NIPT, and had frequent delays in examinations.
Conclusions
Various factors beyond clinical considerations influence the selection of a prenatal test. Therefore, NIPT pathways should include balanced, high-quality information about benefits and limitations, ensuring laboratory specialists' active and integrated involvement in decision-making.
Keywords: Prenatal testing, Value-based health care (VBHC), Patient-reported experience measures (PREMS), Non-invasive prenatal testing (NIPT), Survey
1. Introduction
According to value-based healthcare (VBHC) principles, outcomes that matter to patients should drive regulation, provision and funding. The selection of diagnostic tests is crucial for achieving this goal [1].
Non-invasive prenatal testing (NIPT) is based on the analysis of cell-free DNA derived from the placenta in maternal plasma to screen for fetal aneuploidies. The accuracy of the test, its non-invasiveness, and the possibility of performing it from the first weeks of pregnancy result in a quick global dissemination [2], [3], [4]. Many NIPT panels offer the opportunity to screen for specific conditions other than the common trisomy [5], [6], accurately identifying chromosomal anomalies of difficult interpretation and potentially complicating clinical strategies and sensitive decisions within the maternity pathway [7].
Prenatal tests may offer valuable care when they provide clinicians with important information on fetal conditions and support women's timely, informed decisions. Conversely, these tests can detract value if the results provide information not clear enough to affect clinical management by a) leaving physicians unable to determine the relevance of that information to the fetus’ health and b) preventing couples from clearly understanding whether such information matters for their child's health, even though they become aware of potential risks of severe health issues.
The technical quality of the healthcare performance provides limited information about its value for the patient’s well-being [8]. Thus, patient-reported information provided by pregnant women is crucial to understanding their experience and enhancing care impact and quality [9], [10]. The International Consortium for Health Outcome Measurement (ICHOM) also included the domains of “Shared decision-making and confidence in care providers” and “Health-related Quality of Life” in the Standard set dedicated to Pregnancy and Childbirth [11]. However, there is limited knowledge about the decision-making strategies used to choose a specific level of Non-Invasive Prenatal Tests (NIPT), considering the increased availability and complexity of NIPT options [12].
A systematic survey on patient-reported experiences (PREs), patient-reported outcomes (PROs) and satisfaction levels throughout the maternity care pathway was launched by the Region of Tuscany, Italy, in cooperation with the Scuola Superiore Sant’Anna of Pisa, in March 2019 [13], [14]. Based on this survey, this retrospective, observational study aims to investigate which determinants are associated with pregnant women’s decision to opt for a NIPT, an invasive diagnostic test or both. Understanding these determinants will aid healthcare professionals and policymakers in enhancing the diagnostic prenatal testing process to support informed, rational, and serene decision-making.
2. Methods
2.1. Study setting, design, and data source
The Italian National Health Service (NHS) provides free universal healthcare by making each Region accountable for meeting National coverage goals with National financial funds [15], [16]. The Regional Health Service (RHS) of Tuscany, in central Italy, is divided into three Local Health Authorities (LHAs) comprising 26 health districts, providing healthcare to 3.7 million citizens. Its comprehensive healthcare infrastructure includes 40 hospitals, 95 % of which are public and 25 of which provide maternity care services [17]. Notably, the annual childbirth rate in Tuscany is approximately 22 thousand deliveries.
The survey of the RHS of Tuscany has been embedded into the hAPPyMamma App, a digital platform containing the regional Digital Pregnancy Booklet. As part of this initiative, all pregnant women who receive the Pregnancy Booklet (digital or paper) receive an invitation to participate in the survey online, contingent upon consent. Eight questionnaires are administered at different stages, from the first trimester of pregnancy to one year postpartum, investigating women-reported information potentially relevant at each stage (https://www.regione.toscana.it/-/happymamma).
These data are anonymized. Approval for research use was granted by Tuscany's four ethics committees in late 2017, in compliance a) with the Decree of the President of Tuscany Region number 6/R/2013, b) with the 2011 Italian guidelines on processing personal data to perform customer satisfaction surveys in healthcare [17], [18], [19]. We used these data to explore the factors behind the decision to opt for non-invasive prenatal tests, invasive prenatal tests (amniocentesis or chorionic villus sampling) or both to understand how to improve the diagnostic test delivery in prenatal age (e.g., better communication between patient and healthcare professional, better information policies, better financial coverage). In Tuscany, the combined test (maternal serum pregnancy-associated plasma protein-A, free β-human chorionic gonadotropin and ultrasound fetal nuchal translucency thickness) is free to all pregnant women. In contrast, the cost of NIPT is 400 € out-of-pocket, providing about a 50 % discount to the benefit of those women who resulted positive for a previous combined test (risk score between 1/301 and 1/1000).
2.2. Participants and outcomes
We included all women who completed the questionnaire administered during the second trimester of pregnancy from March 2019 to February 2023. We used each woman's anonymous unique identifier to match the clinical, sociodemographic and maternity pathway-related variables (first trimester) with dichotomous variables (Yes/No) on the performance of NIPT and invasive tests during pregnancy (second trimester) (Table 1). We considered only women with no missing data in any variable of interest.
Table 1.
Baseline characteristics of women according to the performance of NIPT.
| Women’s characteristics | Total | No NIPT | NIPT | p-value |
|---|---|---|---|---|
| (n = 27,337) | (n = 15,305) | (n = 12,032) | ||
| Age class | < 0.001 | |||
| < 30 years | 5147 (18.8 %) | 3857 (25.2 %) | 1290 (10.7 %) | |
| < 40 years | 19224 (70.3 %) | 10513 (68.7 %) | 8711 (72.4 %) | |
| ≥ 40 years | 2966 (10.8 %) | 935 (6.1 %) | 2031 (16.9 %) | |
| Nationality | < 0.001 | |||
| Italian | 25533 (93.4 %) | 14012 (91.6 %) | 11521 (95.8 %) | |
| Non-Italian | 1804 (6.6 %) | 1293 (8.4 %) | 511 (4.2 %) | |
| Homeland migration pressure | < 0.001 | |||
| Italy | 25533 (93.4 %) | 14012 (91.6 %) | 11521 (95.8 %) | |
| High | 1608 (5.9 %) | 1184 (7.7 %) | 424 (3.5 %) | |
| Low | 196 (0.7 %) | 109 (0.7 %) | 87 (0.7 %) | |
| Education level | < 0.001 | |||
| Low | 2467 (9.0 %) | 1764 (11.5 %) | 703 (5.8 %) | |
| High school | 10856 (39.7 %) | 6592 (43.1 %) | 4264 (35.4 %) | |
| University | 14014 (51.3 %) | 6949 (45.4 %) | 7065 (58.7 %) | |
| Work condition | < 0.001 | |||
| Unemployed | 4015 (14.7 %) | 2812 (18.4 %) | 1203 (10.0 %) | |
| Employed | 23322 (85.3 %) | 12493 (81.6 %) | 10829 (90.0 %) | |
| Civil status | 0.004 | |||
| Without partner | 1002 (3.7 %) | 605 (4.0 %) | 397 (3.3 %) | |
| With partner | 26335 (96.3 %) | 14700 (96.0 %) | 11635 (96.7 %) | |
| Local Health Authority | < 0.001 | |||
| LHA1 | 9027 (33.0 %) | 5233 (34.2 %) | 3794 (31.5 %) | |
| LHA2 | 13052 (47.7 %) | 7646 (50.0 %) | 5406 (44.9 %) | |
| LHA3 | 5258 (19.2 %) | 2426 (15.9 %) | 2832 (23.5 %) | |
| Economic condition | < 0.001 | |||
| Not troubled | 6262 (22.9 %) | 3013 (19.7 %) | 3249 (27.0 %) | |
| Quite troubled | 15271 (55.9 %) | 8506 (55.6 %) | 6765 (56.2 %) | |
| Troubled | 5804 (21.2 %) | 3786 (24.7 %) | 2018 (16.8 %) | |
| BMI class | < 0.001 | |||
| Underweight | 1911 (7.0 %) | 999 (6.5 %) | 912 (7.6 %) | |
| Normal | 19029 (69.6 %) | 10419 (68.1 %) | 8610 (71.6 %) | |
| Overweight | 4483 (16.4 %) | 2672 (17.5 %) | 1811 (15.1 %) | |
| Obesity | 1914 (7.0 %) | 1215 (7.9 %) | 699 (5.8 %) | |
| Perceived health, median (IQR) | 3.0 (3.0, 4.0) | 3.0 (3.0, 4.0) | 3.0 (3.0, 4.0) | 0.53 |
| Parity | < 0.001 | |||
| Multiparous | 10278 (37.6 %) | 5941 (38.8 %) | 4337 (36.0 %) | |
| Primigravidae | 17059 (62.4 %) | 9364 (61.2 %) | 7695 (64.0 %) | |
| Pregnancy planning | < 0.001 | |||
| Planned pregnancy | 15743 (57.6 %) | 8358 (54.6 %) | 7385 (61.4 %) | |
| Not excluded | 8964 (32.8 %) | 5330 (34.8 %) | 3634 (30.2 %) | |
| Unplanned | 2630 (9.6 %) | 1617 (10.6 %) | 1013 (8.4 %) | |
| Close people during pregnancy | < 0.001 | |||
| No one | 510 (1.9 %) | 300 (2.0 %) | 210 (1.7 %) | |
| Less than 5 | 22668 (82.9 %) | 12575 (82.2 %) | 10093 (83.9 %) | |
| 6 or more | 4159 (15.2 %) | 2430 (15.9 %) | 1729 (14.4 %) | |
| Folate intake | < 0.001 | |||
| Yes | 26221 (95.9 %) | 14545 (95.0 %) | 11676 (97.0 %) | |
| No | 1116 (4.1 %) | 760 (5.0 %) | 356 (3.0 %) | |
| Smoking in pregnancy | < 0.001 | |||
| No | 25653 (93.8 %) | 14250 (93.1 %) | 11403 (94.8 %) | |
| Yes | 1684 (6.2 %) | 1055 (6.9 %) | 629 (5.2 %) | |
| Alcohol intake | 0.037 | |||
| Never | 19174 (70.1 %) | 10815 (70.7 %) | 8359 (69.5 %) | |
| < 5 times a month | 7739 (28.3 %) | 4271 (27.9 %) | 3468 (28.8 %) | |
| ≥ 5 times a month | 424 (1.6 %) | 219 (1.4 %) | 205 (1.7 %) | |
| High-risk pregnancy | < 0.001 | |||
| No | 22192 (81.2 %) | 12564 (82.1 %) | 9628 (80.0 %) | |
| Yes | 5145 (18.8 %) | 2741 (17.9 %) | 2404 (20.0 %) | |
| Discomfort in pregnancy | 0.10 | |||
| No | 19439 (71.1 %) | 10944 (71.5 %) | 8495 (70.6 %) | |
| Yes | 7898 (28.9 %) | 4361 (28.5 %) | 3537 (29.4 %) | |
| Setting of pregnancy care | < 0.001 | |||
| Counselling centre | 7089 (25.9 %) | 4922 (32.2 %) | 2167 (18.0 %) | |
| Public hospital | 6833 (25.0 %) | 3597 (23.5 %) | 3236 (26.9 %) | |
| Private | 13415 (49.1 %) | 6786 (44.3 %) | 6629 (55.1 %) | |
| Pregnancy assisting professional | < 0.001 | |||
| Midwife | 2746 (10.0 %) | 2034 (13.3 %) | 712 (5.9 %) | |
| Gynecologist | 19178 (70.2 %) | 9989 (65.3 %) | 9189 (76.4 %) | |
| Midwife + gynecologist | 5358 (19.6 %) | 3249 (21.2 %) | 2109 (17.5 %) | |
| Others | 55 (0.2 %) | 33 (0.2 %) | 22 (0.2 %) | |
| Pregnancy exam booking | < 0.001 | |||
| By the woman | 15291 (55.9 %) | 8212 (53.7 %) | 7079 (58.8 %) | |
| By public professionals | 11544 (42.2 %) | 6872 (44.9 %) | 4672 (38.8 %) | |
| By private professionals | 502 (1.8 %) | 221 (1.4 %) | 281 (2.3 %) | |
| Combined screening test | < 0.001 | |||
| No | 783 (2.9 %) | 111 (0.7 %) | 672 (5.6 %) | |
| Yes | 26554 (97.1 %) | 15194 (99.3 %) | 11360 (94.4 %) | |
| Pregnancy examination knowledge, median (IQR) | 4.0 (3.0, 4.0) | 4.0 (3.0, 4.0) | 4.0 (3.0, 5.0) | 0.050 |
| Access to pregnancy services | 0.004 | |||
| Very easy | 22398 (81.9 %) | 12639 (82.6 %) | 9759 (81.1 %) | |
| Quite easy | 3784 (13.8 %) | 2025 (13.2 %) | 1759 (14.6 %) | |
| Not easy | 1155 (4.2 %) | 641 (4.2 %) | 514 (4.3 %) | |
| Delays due to waiting | 0.032 | |||
| No | 18811 (68.8 %) | 10620 (69.4 %) | 8191 (68.1 %) | |
| Few | 7732 (28.3 %) | 4265 (27.9 %) | 3467 (28.8 %) | |
| Frequent | 794 (2.9 %) | 420 (2.7 %) | 374 (3.1 %) | |
| Involvement in choices | < 0.001 | |||
| Low | 7192 (26.3 %) | 3911 (25.6 %) | 3281 (27.3 %) | |
| Average | 10207 (37.3 %) | 5637 (36.8 %) | 4570 (38.0 %) | |
| High | 9938 (36.4 %) | 5757 (37.6 %) | 4181 (34.7 %) | |
| Influenza or pertussis vaccination | < 0.001 | |||
| No | 10439 (38.2 %) | 6431 (42.0 %) | 4008 (33.3 %) | |
| Yes | 16898 (61.8 %) | 8874 (58.0 %) | 8024 (66.7 %) |
2.3. Statistical analyses
First, we reconstructed the diagnostic journey experienced by women during the maternity pathway by analyzing the patterns of diagnostic tests performed by them (no test, NIPT only, invasive test only, both), as well as the related PRE-measures derived from the diverse array of diagnostic tests. We computed the mean scores for each PRE-measure (expressed as 1-to-5 Likert scale) associated with any step of the diagnostic journey.
Then, we described the characteristics of participants by reporting continuous variables as median and interquartile range (IQR) and categorical variables as counts and proportions (%). We compared such characteristics between women undergoing NIPT vs. not and between women undergoing invasive tests vs. not by performing the Mann-Whitney and the χ2 tests, respectively.
Finally, we performed logistic regression models using the three outcomes as dependent variables: 1) NIPT, 2) invasive test, and 3) NIPT + invasive test. We adjusted these models for the women’s characteristics, as shown in Table 1.
Statistical analyses were conducted using Stata Software version 17.0 (Stata-Corp, LLC, College Station, Texas, USA), with statistical significance set at a p-value below 0.05.
3. Results
3.1. Women’s experiences
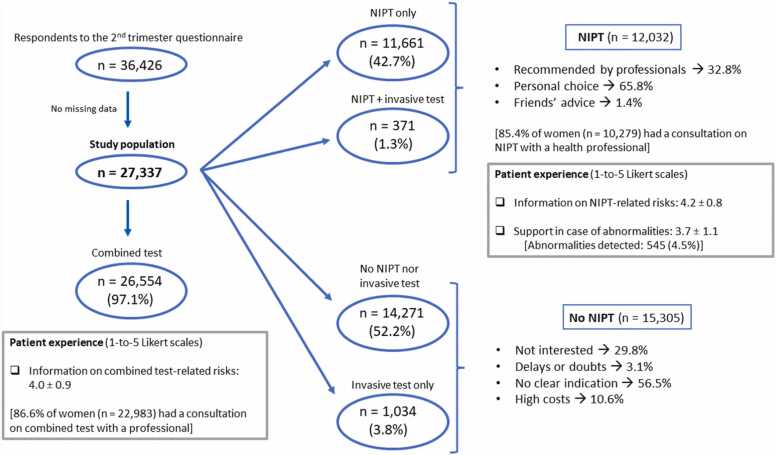
We obtained a study population of 27,337 respondents (Fig. 1). 44 % of women underwent NIPT (n = 12,032), among which 1.3 % (of the total) women chose subsequent invasive testing. 66 % of those who decided on NIPT took such a decision autonomously, while the remaining 33 % followed the recommendation of a healthcare professional. Their perceived level of information concerning the NIPT-associated risks averaged 4.2 on a 1-to-5 scale. NIPT detected possible abnormalities in 4.5 % of cases, in which the interested women reported an average support score of 3.7 on the same scale. Most women (56 %) who decided against NIPT cited a lack of clear recommendation (56 %) or a simple lack of interest (30 %) as their reasons.
Fig. 1.
Study flowchart.
In addition, women who opted for invasive tests were 5 % (n = 1405), with 3.8 % (n = 1034) of the study population directly undergoing invasive testing (no previous screening). The interested women felt informed about the possible risks of invasive testing, with a mean score of 4.2. Most women reported choosing an invasive test for personal choice (n = 481), followed by a recommendation from a healthcare professional (n = 420).
3.2. Characteristics of respondents
Women aged 30–39 years were 70 % (Table 1, Supplementary Table S1). Half of the women had a college degree, and 93 % were Italian. Most women were employed and lived with a partner, but 56 % reported a somewhat troubled economic status. 62 % were primipara, and 70 % had an average weight. On a 1-to-5 Likert scale, the median score of perceived health status was 3.0. Most women who took folates during pregnancy did not smoke or consume alcohol. Only 62 % were vaccinated against influenza, a non-compulsory vaccination that can be considered an indicator of attention towards health.
Moreover, 58 % of women planned their pregnancy, only 36 % of women felt utterly involved in choices about pregnancy, and 83 % claimed to have 1 to 5 helping people during pregnancy. The percentage of high-risk pregnancies was 19 %, with 29 % of pregnant women experiencing some discomfort. Half women were assisted privately, 70 % by a gynecologist; however, 56 % had to book examinations independently. Almost all women underwent combined testing. Most women accessed pregnancy services very quickly and did not have delays in examinations.
All these characteristics (except health status and discomfort in pregnancy) differed significantly between women who underwent NIPT vs. those who did not. Indeed, women in the NIPT group were older, more frequently graduated, Italian, primiparous, and of average-to-low weight. They were also more commonly employed in a relationship, enjoyed a better economic status, and had a higher rate of planned pregnancy. They took folates more frequently and refrained from smoking but consumed alcohol more regularly. Also, their pregnancies were more commonly reported as high-risk. These women were followed more frequently by a gynecologist (vs midwife) and privately, scheduling examinations more regularly.
Women who did not undergo NIPT had less frequent experience with combined testing. These women faced more significant challenges in accessing maternity care, had limited involvement in decisions but experienced fewer delays due to waiting lists, and received vaccinations more frequently.
3.3. Testing patterns
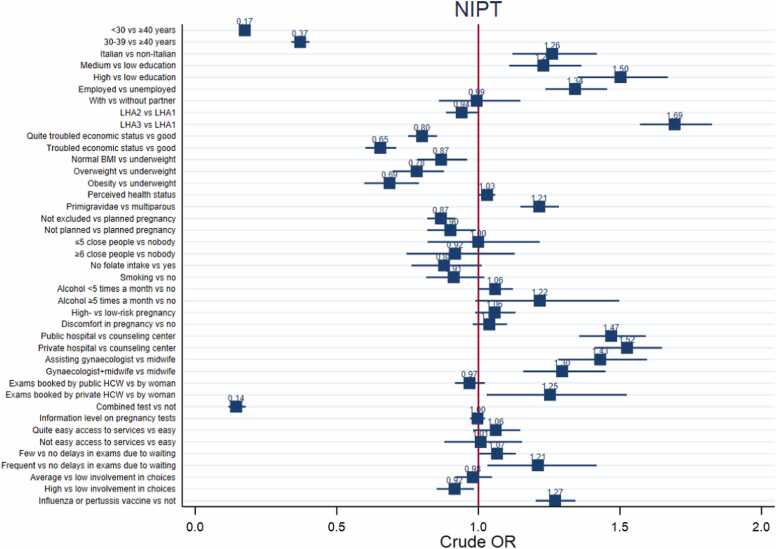
The main determinants for undergoing NIPT that emerged from the weighted analysis (Fig. 2, Supplementary Table S2) were older age, higher education, nulliparity, low weight, and employment. Women who opted for NIPT had better perceived health status, superior economic status and planned pregnancy more frequently. Being assisted by hospitals (either public or private) rather than counseling centers and by gynecologists rather than midwives was associated with higher odds of choosing NIPT. Not having undergone combined testing and being vaccinated during pregnancy were factors favoring NIPT. Women experiencing delays in pregnancy examinations due to waiting opted for NIPT more frequently, while women feeling highly involved in choices about pregnancy less frequently.
Fig. 2.
Logistic regression models for non-invasive prenatal test (NIPT) performance.
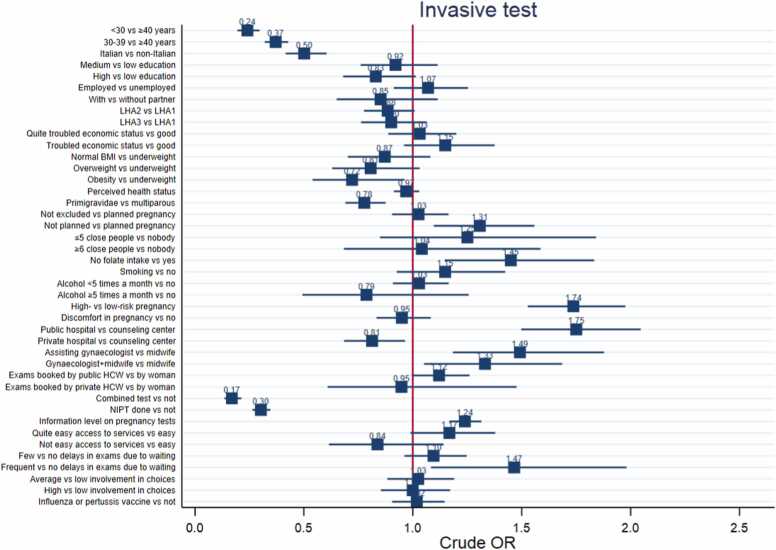
Women who underwent invasive testing were older, less often primiparous and Italian (Fig. 3, Supplementary Table S3). Obesity was negatively associated with invasive test choice. More frequently, these women did not plan pregnancy, took no folate, and had a high-risk pregnancy. These women received more often maternity care from public hospitals than from counseling centers and even less from private hospitals. Women opting for invasive testing were more often followed by gynecologists, had not done either combined tests or NIPT and reported higher levels of information about pregnancy exams. Finally, women choosing invasive test were more likely to experience delays in pregnancy exams.
Fig. 3.
Logistic regression models for the performance of invasive prenatal tests.
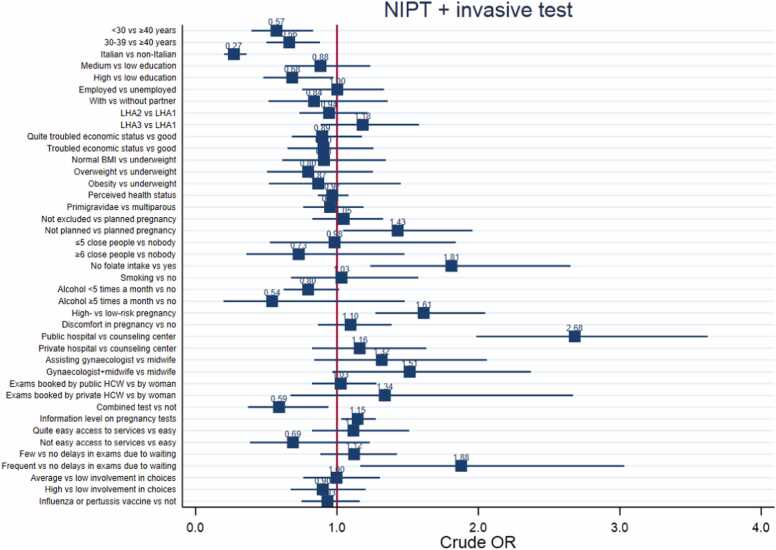
In addition, factors associated with higher odds of undergoing both tests (NIPT and invasive test) were older age, non-Italian nationality, lower education, not having planned pregnancy, not having taken folates during pregnancy, having a high-risk pregnancy, and being assisted in public hospitals rather than in counseling centers (Fig. 4, Supplementary Table S4). Also, women undergoing both tests did not opt for combined test more frequently and experienced frequent delays in examinations due to waiting.
Fig. 4.
Logistic regression models for the performance of both non-invasive and invasive prenatal tests.
4. Discussion
Since the introduction of NIPTs, there has been a continuous debate over their benefits and limitations. The main advantages are a) the increased insight into genetic disease risks for the unborn child and b) the subsequent possibility of making informed choices about whether to opt for subsequent invasive prenatal diagnostic tests. This holds as long as the decisions made are genuinely informed.
Otherwise, in the absence of adequate pre- and post-test counselling, there may be false expectations, misinterpretation of test results, iatrogenic stress and unwanted pregnancy terminations. To put it with the European Commission Expert Panel framework on value-based care [20], these tests could be detrimental in terms of personal value (worse health and decreased ability to make informed, relevant decisions); technical value (funding expensive tests of unclear benefits and controversial effects); allocative value (detrimental cost opportunity against other, more valuable investments); societal value (psychosocial harm to women and reduced birth rates).
Only 58.7 % of the women who underwent NIPT had a university degree, and only 33 % followed the recommendation of a healthcare professional. These findings suggest that the information provided by NIPT could be subject to misunderstanding. Straightforward advice from healthcare professionals and pregnant women’s expectations should be given more significant consideration, especially with the increasing availability of non-invasive prenatal tests. On the one hand, decreasing sequencing costs and technological advancements can enhance technical value [21]. On the other hand, Genome-wide (GW) NIPT methods can report additional findings, such as rare autosomal trisomies, structural aberrations, and sex chromosomal disorders [22]. However, these applications are not yet recommended due to insufficient evidence of their clinical validity and utility [23]. It could even be possible, in the future, to expand the scope of NIPT to include screening for fetal monogenic disorders and fetal-maternal risk factors, including preeclampsia, preterm birth and viral infections. As NIPT technology evolves, with the potential to screen for a broader range of conditions, ethical considerations and the impact on decision-making will become increasingly complex. This underscores the importance of ongoing research, ethical debate, and policy development to navigate these advancements responsibly.
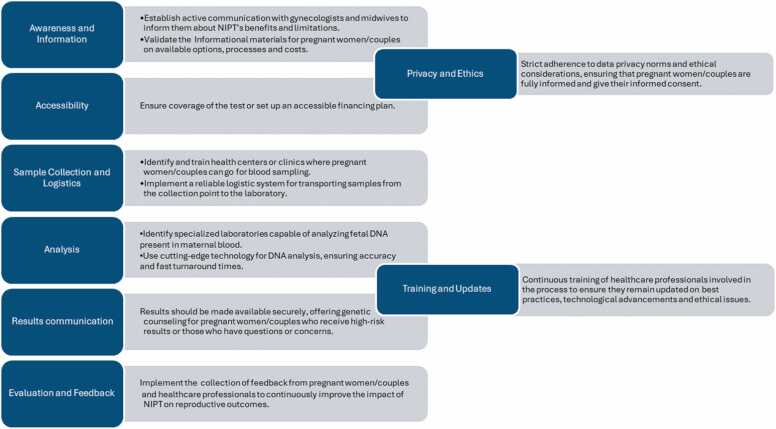
The findings that a significant portion of women undergoing NIPT do so following the recommendation of a healthcare professional, coupled with the fact that a notable percentage of women feel under-informed, highlight the crucial role of healthcare providers. There is a clear need for healthcare professionals to offer clear, straightforward advice and support women's expectations and understanding of NIPT, ultimately enhancing the quality of care and patient satisfaction. Implementing a safe, efficient, and accessible NIPT service requires several key steps involving multidisciplinary healthcare professionals, advanced technologies, and ethical evaluations to ensure pregnant women/couples receive the best possible outcome. The successful implementation of NIPT services requires the collaboration of various stakeholders, including healthcare professionals, genetic counselors, and ethicists. A multidisciplinary approach can ensure that ethical, technological, and patient-care considerations are adequately addressed, leading to safer, more efficient, and equitable prenatal testing services. Fig. 5 provides a general overview of what these key steps could entail.
Fig. 5.
A general overview of the significant points to be implemented.
Although the diagnostic phase is typically an intermediate step guiding medical decisions [24], its therapeutic impact on patient outcomes is often overlooked, as patients tend to give more importance to interventions than to the diagnoses which support them [25]. Our in-depth analysis of patient-reported experience related to diagnostic tests at prenatal age has revealed disparities in the baseline characteristics of women deciding whether or not to undergo NIPT. Given these concerns, it can be argued that the NIPT delivery pathways should include balanced and high-quality information about benefits and limitations and their implications for expectant mothers, healthcare professionals, and the broader healthcare system. There is a significant reliance on NIPT for gaining insights into genetic risks to the unborn child, which underscores its perceived value among pregnant women. However, the decision to undergo NIPT appears to be influenced by various sociodemographic factors, including age, education level, and economic status. This suggests a need for more inclusive education and counseling strategies that address the diverse needs and backgrounds of expectant mothers.
The main limitation of this study is its observational design, which prevents inferring causation despite extensive adjustment for confounding variables. Additionally, the data are patient-reported and, thus, susceptible to reporting bias. The study population was self-selected, as participation in the survey is voluntary, so the study population was not representative of the general population of women giving birth in Tuscany. Moreover, the details provided by obstetricians or midwives about NIPT were unknown, preventing us from determining whether all women had the same information to make uniform decisions. Finally, our results cannot be generalized nationally, as the study was conducted in a single Italian Region. The regional focus of the study suggests the potential value of extending similar research to other contexts and settings, enabling a more comprehensive understanding of NIPT's impact on prenatal care globally.
5. Conclusions
The study highlights the critical role of informed decision-making in prenatal testing. Adequate pre- and post-test counseling is essential to prevent misunderstandings, false expectations, and the potential stress associated with testing outcomes. This calls for a more integrated approach to patient education and support throughout decision-making.
Therefore, while NIPT offers significant benefits in prenatal care, its practical and equitable implementation requires careful consideration of informed decision-making, accessibility, healthcare professional involvement, and ethical considerations. Addressing these factors can enhance the value and impact of prenatal testing for all expecting mothers.
Ethics
As explained in a previous publication using the same data source [17], informed consent and ethics approval were unnecessary for using such data for research purposes, as established by the 2011 Italian guidelines on processing personal data to perform customer satisfaction surveys in the healthcare sector. Therefore, this study fully complies with the Italian law on privacy 101/2018, aligned with the European GDPR 2016/679.
Author contributions
-
•
A. Ferrari: design of the work; acquisition, analysis, and interpretation of data; drafting and reviewing the work; final approval of the version to be published; accountability for all aspects of the work.
-
•
F. Pennestrì : design of the work; drafting and reviewing the work; final approval of the version to be published; accountability for all aspects of the work.
-
•
M. Bonciani: acquisition and interpretation of data; drafting and reviewing the work; final approval of the version to be published; accountability for all aspects of the work.
-
•
G. Banfi: design of the work; draft and review; final approval of the version to be published; accountability for all aspects of the work.
-
•
M. Vainieri: design of the work; draft and review; final approval of the version to be published; accountability for all aspects of the work.
-
•
R. Tomaiuolo: design of the work; drafting and reviewing the work; final approval of the version to be published; accountability for all aspects of the work.
Funding
The data source and publication charges were funded as part of the MeS Lab of Scuola Superiore Sant’Anna research activities. The Tuscany Region Health Authority funded such activities under the collaboration agreement with Scuola Superiore Sant’Anna. Tuscany Region had no role in formulating the research question, study design, data collection and analysis, or writing and submitting the article for publication.
CRediT authorship contribution statement
Federico Pennestrì: Writing – review & editing, Writing – original draft, Methodology, Investigation, Conceptualization. Amerigo Ferrari: Writing – review & editing, Writing – original draft, Software, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Giuseppe Banfi: Writing – review & editing, Validation, Supervision, Project administration, Conceptualization. Manila Bonciani: Writing – review & editing, Supervision, Project administration, Conceptualization. Tomaiuolo Rossella: Writing – review & editing, Writing – original draft, Validation, Supervision, Project administration, Investigation, Data curation, Conceptualization. Milena Vainieri: Writing – review & editing, Validation, Supervision, Project administration.
Declaration of Competing Interest
None declared by the authors.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.eurox.2024.100327.
Appendix A. Supplementary material
Supplementary material
.
References
- 1.Tomaiuolo R., Banfi G. From volume to value: a watershed moment for the clinical laboratory. Clin Chem Lab Med (CCLM) 2023 doi: 10.1515/cclm-2023-0870. [DOI] [PubMed] [Google Scholar]
- 2.Chandrasekharan S., Minear M.A., Hung A., Allyse M. Noninvasive prenatal testing goes global. Sci Transl Med. 2014;6 doi: 10.1126/scitranslmed.3008704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gadsbøll K., Petersen O.B., Gatinois V., Strange H., Jacobsson B., Wapner R., et al. Current use of noninvasive prenatal testing in Europe, Australia and the USA: a graphical presentation. Acta Obstet Gynecol Scand. 2020;99:722–730. doi: 10.1111/aogs.13841. [DOI] [PubMed] [Google Scholar]
- 4.Ravitsky V., Roy M.-C., Haidar H., Henneman L., Marshall J., Newson A.J., et al. The emergence and global spread of noninvasive prenatal testing. Annu Rev Genom Hum Genet. 2021;22:309–338. doi: 10.1146/annurev-genom-083118-015053. [DOI] [PubMed] [Google Scholar]
- 5.Christiaens L., Chitty L.S., Langlois S. Current controversies in prenatal diagnosis: expanded NIPT that includes conditions other than trisomies 13, 18, and 21 should be offered. Prenat Diagn. 2021;41:1316–1323. doi: 10.1002/pd.5943. [DOI] [PubMed] [Google Scholar]
- 6.Chitty L.S., Hudgins L., Norton M.E. Current controversies in prenatal diagnosis 2: Cell‐free DNA prenatal screening should be used to identify all chromosome abnormalities. Prenat Diagn. 2018;38:160–165. doi: 10.1002/pd.5216. [DOI] [PubMed] [Google Scholar]
- 7.Labonté V., Alsaid D., Lang B., Meerpohl J.J. Psychological and social consequences of non-invasive prenatal testing (NIPT): a scoping review. BMC Pregnancy Childbirth. 2019;19:385. doi: 10.1186/s12884-019-2518-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anhang Price R., Elliott M.N., Cleary P.D., Zaslavsky A.M., Hays R.D. Should health care providers be accountable for patients’ care experiences? J Gen Intern Med. 2015;30:253–256. doi: 10.1007/s11606-014-3111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dickinson F., McCauley M., Smith H., van den Broek N. Patient reported outcome measures for use in pregnancy and childbirth: a systematic review. BMC Pregnancy Childbirth. 2019;19:155. doi: 10.1186/s12884-019-2318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Depla A.L., Lamain-de Ruiter M., Laureij L.T., Ernst-Smelt H.E., Hazelzet J.A., Franx A., et al. Patient-reported outcome and experience measures in perinatal care to guide clinical practice: prospective observational study. J Med Internet Res. 2022;24 doi: 10.2196/37725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ICHOM (International Consortium for Health Outcomes Measurement) n.d. 〈https://www.ichom.org/portfolio/pregnancy-and-childbirth/?_gl=1*3ax〉.
- 12.Oliveri S., Ongaro G., Cutica I., Menicucci G., Belperio D., Spinella F., et al. Decision-making process about prenatal genetic screening: how deeply do moms-to-be want to know from Non-Invasive Prenatal Testing? BMC Pregnancy Childbirth. 2023;23:1–10. doi: 10.1186/s12884-022-05272-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonciani M., De Rosis S.V.M. Mobile health intervention in the maternal care pathway: protocol for the impact evaluation of hAPPyMamma. JMIR Res Protoc. 2021;10(1) doi: 10.2196/19073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lungu D.A., Pennucci F., De Rosis S., Romano G., Melfi F. Implementing successful systematic patient reported outcome and experience measures (PROMs and PREMs) in robotic oncological surgery—the role of physicians. Int J Health Plan Manag. 2019:1–15. doi: 10.1002/hpm.2959. [DOI] [PubMed] [Google Scholar]
- 15.Ferre F., de Belvis A.G. iulio, Valerio L., Longhi S., Lazzari A., Fattore G., et al. Italy: health system review. Health Syst Transit. 2014;16:1–168. [PubMed] [Google Scholar]
- 16.Ricciardi W., Tarricone R. The evolution of the Italian National Health Service. Lancet. 2021;398:2193–2206. doi: 10.1016/S0140-6736(21)01733-5. [DOI] [PubMed] [Google Scholar]
- 17.Ferrari A., Mannella P., Caputo A., Simoncini T., Bonciani M. Risk and protective factors for pregnancy-related urinary incontinence until 1 year postpartum: A cohort study using reported outcome measures in Italy 2023:1–10. 10.1002/ijgo.15003. [DOI] [PubMed]
- 18.De Rosis S., Pennucci F., Lungu D.A., Manca M., Nuti S. A continuous PREMs and PROMs observatory for elective hip and knee arthroplasty: study protocol. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-049826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferrari A., Corazza I., Mannella P., Simoncini T., Bonciani M. Influence of COVID-19 pandemic on self-reported urinary incontinence during pregnancy and postpartum: a prospective study. Int J Gynecol Obstet. 2022:1–8. doi: 10.1002/ijgo.14522. [DOI] [PubMed] [Google Scholar]
- 20.Expert Panel on effective ways of investing in Health (EXPH). Defining value in “Value-based healthcare.” 2019. 10.2875/35471. [DOI]
- 21.Bianchi D.W., Chiu R.W.K. Sequencing of circulating cell-free DNA during pregnancy. N Engl J Med. 2018;379:464–473. doi: 10.1056/NEJMra1705345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van der Meij K.R.M., Sistermans E.A., Macville M.V.E., Stevens S.J.C., Bax C.J., Bekker M.N., et al. TRIDENT-2: national implementation of genome-wide non-invasive prenatal testing as a first-tier screening test in the Netherlands. Am J Hum Genet. 2019;105:1091–1101. doi: 10.1016/j.ajhg.2019.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Prooyen Schuurman L., Sistermans E.A., Van Opstal D., Henneman L., Bekker M.N., Bax C.J., et al. Clinical impact of additional findings detected by genome-wide non-invasive prenatal testing: Follow-up results of the TRIDENT-2 study. Am J Hum Genet. 2022;109:1140–1152. doi: 10.1016/j.ajhg.2022.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hallworth M.J. The “70% claim”: what is the evidence base? Ann Clin Biochem. 2011;48:487–488. doi: 10.1258/acb.2011.011177. [DOI] [PubMed] [Google Scholar]
- 25.Plebani M. Quality and future of clinical laboratories: the Vico’s whole cyclical theory of the recurring cycles. Clin Chem Lab Med. 2018;56:901–908. doi: 10.1515/cclm-2018-0009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material