Abstract
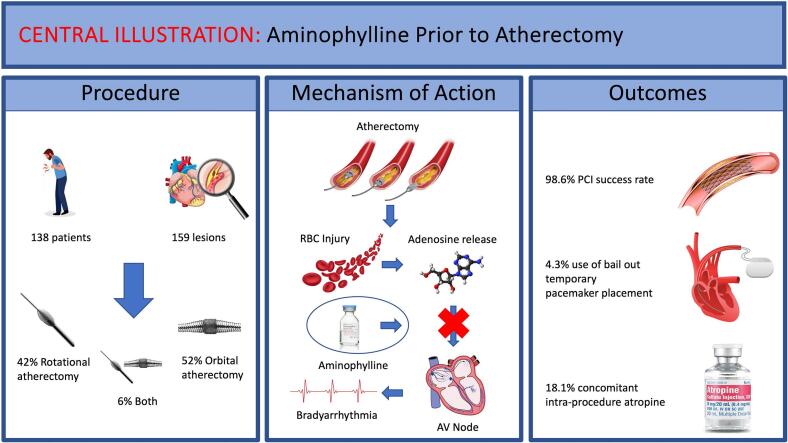
Coronary calcified lesions are commonly encountered and coronary atherectomy is commonly used for lesion modification during percutaneous coronary interventions (PCI). The release of adenosine during atherectomy can result in bradyarrhythmias and aminophylline is commonly used to prevent this reaction. We identified 138 patients to evaluate the safety and efficacy of intravenous (IV) aminophylline administration prior to coronary atherectomy. A total of 159 calcified lesions were treated, and the atherectomy device was orbital atherectomy, rotational atherectomy, and both in 52 %, 42 %, and 6 %; respectively. After administration of aminophylline, 4.3 % of patients required intraprocedural insertion of a transvenous pacer (TVP), and 18.1 % of patients required administration of IV atropine. Technical success was achieved in 98.6 % of patients, and no adverse reactions to aminophylline were reported. All patients survived to discharge. In conclusion, aminophylline administration prior to coronary atherectomy was safe and effective. No adverse effects of aminophylline were seen, and the rate of bailout TVP placement was low.
Keywords: Aminophylline, Atherectomy, Coronary artery disease, Bradyarrhythmia
Despite significant scientific advancements in the development of new drugs, current processes for drug approval are complex, lengthy, and costly. After identifying a chemical or genetic target, animal and clinical trials are conducted to assess safety, followed by a lengthy FDA approval process. On the other hand, therapeutic medicinal benefits of many so-called “historical drugs” were discovered in the past by simple observation and scientific serendipity. Some examples include aspirin, digoxin, and quinidine [1]. In this article, we aim to describe the use of another historical medication, namely aminophylline, for the prevention of bradyarrhythmias during atherectomy of calcified coronary lesions.
Severely calcified lesions are frequently encountered during percutaneous coronary intervention (PCI) and are associated with poor clinical outcomes [2]. Coronary atherectomy is utilized to modify such lesions and improve procedural success. A recent meta-analysis suggested the potential for increased complications and decreased success rates, even though not statistically significant, with rotational atherectomy (RA) during CTO PCI. There remains however a need for enhancement in procedural techniques, operator experience, and patient selection to further improve outcomes [3]. Within this analysis we demonstrate the possible benefits of utilizing an older, often overlooked drug, aminophylline, to improve the outcomes in patients undergoing atherectomy.
Bradyarrhythmia occurs during atherectomy due to the release of adenosine from red blood cells. Adenosine binds to type 1 (A1) receptors in the sinoatrial node and atrioventricular node, causing negative chronotropic and dromotropic effects. Aminophylline was extracted in the 1880s and was first used as a diuretic. After 20 years of its initial use, it was prescribed for asthma treatment due to its bronchodilatory effect although its utility for that indication has been questionable [4]. In the heart, it antagonizes the effects of adenosine by increasing cyclic adenosine monophosphate (cAMP) enhancing atrioventricular conduction and preventing adenosine-induced bradyarrhythmia [5]. This theory was proven in animal and human trials [6,7].
We identified all patients who received intravenous (IV) aminophylline and underwent coronary atherectomy in our cardiac catheterization laboratory between 10/1/2018 and 4/1/2021. Electronic medical records were retrospectively reviewed. Safety endpoints included intraprocedural use of atropine, vasopressors, mechanical circulatory support (MCS) device implantation, or transvenous pacemaker (TVP) placement. We also analyzed procedural complications related to urgent TVP, adverse reaction to aminophylline, and survival to discharge.
138 patients received IV aminophylline prior to coronary atherectomy in a total of 159 lesions. The mean age was 70.5 ± 10 and 76.1 % were male. Indications for PCI included stable angina (63.2 %), acute coronary syndrome (27.5 %), pre-operative revascularization (8 %), and ischemic cardiomyopathy (2.2 %). 86.3 % of patients had one lesion treated, 13 % had two lesions, and 0.7 % had three lesions treated during the procedure. Of 159 lesions, 39 % were in the right coronary artery, 25 % in the left circumflex artery, 18 % in the left anterior descending artery, and 16 % in the left main coronary artery. The average dose of aminophylline per case was 241.2 ± 77.2 administered over 10 min. Orbital atherectomy was used in 52 %, rotational atherectomy in 42 %, and in 6 % both technologies were used. After administration of IV aminophylline, 6 patients (4.3 %) had intraprocedural insertion of a TVP, and 25 patients (18.1 %) required intraprocedural administration of IV atropine (Fig. 1). All patients who required TVP placement were undergoing atherectomy for dominant right coronary artery lesions. 50 patients (36.2 %) were treated with intraprocedural vasopressors to support the procedure, procedural complications occurred in 23 (16.7 %) patients, and 3 of these patients (2.2 %) required urgent placement of MCS. All the above events were induced by procedural complexity and not due to bradyarrhythmia. Technical success was achieved in 136 patients (98.6 %), none of whom had adverse reactions to aminophylline. All patients survived to discharge.
Fig. 1.
Central illustration: aminophylline prior to atherectomy.
Bradyarrhythmia and atrioventricular block are commonly seen while performing atherectomy and occur in 27 % of cases [8], particularly in right coronary arteries or dominant left circumflex coronary arteries. Recently, atropine was reportedly used in 25 % of patients prior to atherectomy, and 15 % after atherectomy [9]. Although these events are usually transient, they can be associated with significant hypotension leading to discontinuation of atherectomy attempts, which may in turn lead to suboptimal lesion preparation.
Due to the high incidence of bradycardia, operators have utilized the placement of temporary pacemakers as a backup in the event significant bradycardia was to occur. This was reported in up to 50 % of cases where RA was used in a dominant RCA [10]. Although this is usually successful, placing a temporary pacing wire requires the addition of venous access, increases the bleeding risk, carries the risk of complications during placement, and adds to the overall cost of the procedure. On the other hand, pacing through coronary guidewires was described in small case series but had variable rates of ventricular capture, in addition to the concern for coronary vasospasm and perforations [11,12].
In conclusion, aminophylline was utilized safely and effectively during atherectomy. The incidence of concomitant atropine use was 18.1 %, and bailout use of TVP was 4.3 % which might be explained by the Bezold-Jarisch reflex as the cause of bradycardia. No patients had adverse reactions to aminophylline. Our study is limited to being a retrospective, single-center study. We were also limited due to our inability to identify intra-procedural steps to limit bradyarrhythmia such as stop times between atherectomy runs. However, this analysis evaluates and proves the safety and efficacy of aminophylline for the prevention of significant bradycardia during atherectomy.
Disclosures
Drs. Nakhle, Aqtash, Zakhour, Brice, and Arnautovic, have no disclosures. Parth Desai and Milan Kaushik have no disclosures. Dr. Kunkel has the following disclosures: Advisory panels, speaking fees, consulting: Abiomed, CSI, Medtronic, Shockwave; Advisor boards: Jansen, Bristol Myers Squibb. Dr. Ferdinand has the following disclosures: Consultant Novartis, Medtronic, Boehringer Ingelheim, Janssen, Eli Lilly. Dr. Alaswad has the following disclosures: Consultant and speaker: Boston Scientific, Abbott Cardiovascular, Teleflex, and CSI. Dr. Basir has the following disclosures: Consulting fees/honoraria: Abiomed, Cardiovascular Systems, Zoll, Abbott Cardiovascular, Cheisi, Saranas, Boston Scientific.
CRediT authorship contribution statement
Asaad Nakhle: Writing – review & editing, Writing – original draft. Katherine J. Kunkel: Writing – review & editing. Obadah Aqtash: Writing – review & editing. Samer Zakhour: Data curation. Lizbeth Brice: Writing – review & editing. Jelena Arnautovic: Writing – review & editing. Parth Desai: Data curation. Milan Kaushik: Data curation. Keith Ferdinand: Writing – review & editing. Khaldoon Alaswad: Writing – review & editing. Mir Babar Basir: Writing – review & editing, Writing – original draft, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
References
- 1.Smulyan H. The beat Goes on: the story of five ageless cardiac drugs. Am. J. Med. Sci. 2018;356:441–450. doi: 10.1016/j.amjms.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 2.Généreux P., Madhavan M.V., Mintz G.S., et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. Pooled analysis from the HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) and ACUITY (acute catheterization and urgent intervention triage strategy) TRIALS. J. Am. Coll. Cardiol. 2014;63:1845–1854. doi: 10.1016/j.jacc.2014.01.034. [DOI] [PubMed] [Google Scholar]
- 3.Devireddy R.R., Qaqish O., Pannikottu K., et al. Chronic total occlusion rotational atherectomy (CTO RA) versus non-CTO RA in coronary artery disease: a meta-analysis of clinical outcomes and complications. Am. Heart J. Plus: Cardiol. Res. Pract. 2023;36 doi: 10.1016/j.ahjo.2023.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hart S.P. Should aminophylline be abandoned in the treatment of acute asthma in adults? QJM. 2000;93:761–765. doi: 10.1093/qjmed/93.11.761. [DOI] [PubMed] [Google Scholar]
- 5.Mustafa S.J., Morrison R.R., Teng B., Pelleg A. Adenosine receptors and the heart: role in regulation of coronary blood flow and cardiac electrophysiology. Handb. Exp. Pharmacol. 2009:161–188. doi: 10.1007/978-3-540-89615-9_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murad B. Intracoronary aminophylline for heart block with AngioJet thrombectomy. J. Invasive Cardiol. 2005;17:A4. [PubMed] [Google Scholar]
- 7.Murad B. Intracoronary aminophylline for management of bradyarrhythmias during thrombectomy with the AngioJet catheter. J. Invasive Cardiol. 2008;20:12a–18a. [PubMed] [Google Scholar]
- 8.HIll A, Hajj ME, Staub S, Fernandes V, Maran A. 100.40 comparison of Intraprocedural hypotension and bradycardia in rotational versus orbital Atherectomy. JACC Cardiovasc. Interv. 2019;12:S12. [Google Scholar]
- 9.Knott J.D., Sabbah M.S., Lewis B.R., et al. Prophylactic intravenous aminophylline for preventing bradyarrhythmias during coronary atherectomy: a 10-year single-center experience. J. Soc. Cardiovasc. Angiogr. Intervent. 2023:2. [Google Scholar]
- 10.Mitar M.D., Ratner S., Lavi S. Heart block and temporary pacing during rotational atherectomy. Can. J. Cardiol. 2015;31:335–340. doi: 10.1016/j.cjca.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 11.Mixon T.A., Cross D.S., Lawrence M.E., Gantt D.S., Dehmer G.J. Temporary coronary guidewire pacing during percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 2004;61:494–500. doi: 10.1002/ccd.20009. (discussion 502-3) [DOI] [PubMed] [Google Scholar]
- 12.Kusumoto H., Ishibuchi K., Hasegawa K., Otsuji S. Trans-coronary pacing via Rota wire prevents bradycardia during rotational atherectomy: a case report. Eur. Heart J. Case Rep. 2022;6 doi: 10.1093/ehjcr/ytac013. [DOI] [PMC free article] [PubMed] [Google Scholar]