Abstract
Achalasia, a rare esophageal motility disorder characterized by the inability of the lower esophageal sphincter to relax and loss of esophageal peristalsis, significantly impacts pediatric patient quality of life through symptoms like dysphagia, chest pain, and weight loss. This nationwide retrospective cohort study evaluates the efficacy and safety of peroral endoscopic myotomy (POEM) for pediatric achalasia in Mongolia, contributing to the limited global data on this minimally invasive treatment in children. Conducted between February 2020 and March 2022 at 2 tertiary centers, the study included symptomatic achalasia patients, treatment-naive or those with unsatisfactory outcomes from previous esophageal dilations. The POEM procedure was assessed for its impact on esophageal structure and function, symptom severity via the Eckardt score, and procedure-related safety, with outcomes measured at baseline, 3 days, and 12 months post-procedure. The study demonstrated notable post-procedure improvements across all measured outcomes: abnormal contraction length and esophageal width significantly reduced, underscoring the procedure’s effectiveness. More precisely, the integrated relaxation pressure showed a significant improvement from a mean of 26.8 mm Hg (standard deviation [SD], 5.4 mm Hg) pre-procedure to 10.8 mm Hg (SD, 1.1 mm Hg) 12 months (P < .001). Similarly, Eckardt scores, which assess symptom severity, improved significantly from a pre-procedure mean of 7.0 (SD, 1.0) to a substantially lower score post-procedure (P < .001), reflecting enhanced patient quality of life and symptom alleviation. This study underscores POEM’s role as an effective, minimally invasive option for pediatric achalasia management within the Mongolian population, offering significant symptomatic relief and improved esophageal function.
Keywords: pediatric achalasia, pediatric POEM, per oral endoscopic myotomy
1. Introduction
Achalasia is an infrequent disorder of esophageal motility, known by the lower esophageal sphincter’s (LES) inability to relax, coupled with the loss of peristaltic movements within the esophagus.[1,2] This disorder manifests through symptoms including dysphagia (difficulty swallowing), chest pain, regurgitation of undigested food, and weight loss, substantially affecting the life quality of those afflicted.[3,4] The etiology and pathophysiology of achalasia are attributed to the degeneration of esophageal inhibitory neurons, resulting in the inability of the lower esophageal sphincter to relax properly and abnormal motility.[5] Achalasia is a scarce disorder in pediatric populations, significantly rarer than in adults.[6–8]
Traditionally, treatment options for achalasia have included pharmacological interventions such as calcium channel blockers and endoscopic management techniques like local injections of botulinum toxin or esophageal dilation. For pediatric patients, Heller myotomy is a commonly employed surgical intervention for pediatric patients that demonstrates excellent clinical outcomes.[9–11] Nevertheless, per oral endoscopic myotomy (POEM) is the less invasive endoscopic management for children with achalasia, achieving favorable clinical outcomes.[10,12–17]
This nationwide study aims to evaluate the safety and efficacy of the POEM in pediatric patients with achalasia and report experience in Mongolia.
2. Materials and methods
This retrospective cohort study was conducted to evaluate the efficacy and safety of POEM in a total 12 pediatric patients with achalasia at 2 tertiary centers between February 2020 and March 2022 in Ulaanbaatar, Mongolia. Eligible participants were children (<18 years old) diagnosed with achalasia based on clinical, radiological, endoscopic findings and, patients were required to have the esophageal luminal capacity for a 9.2 mm gastroscope insertion. Inclusion criteria were patients who had symptomatic achalasia confirmed by contrast esophagram and upper gastrointestinal endoscopy, who were either treatment-naive or had previously undergone esophageal dilation without satisfactory symptom resolution.
Patient characteristics were collected, including age in months, gender, body weight, height, and body mass index. The below weight and height of the patients for their age were determined according to the World Health Organization Child Growth Standards.[18] Moreover, clinical history of the mean interval from the definitive diagnosis to the performance of the POEM procedure and prior esophageal dilation before POEM were collected.
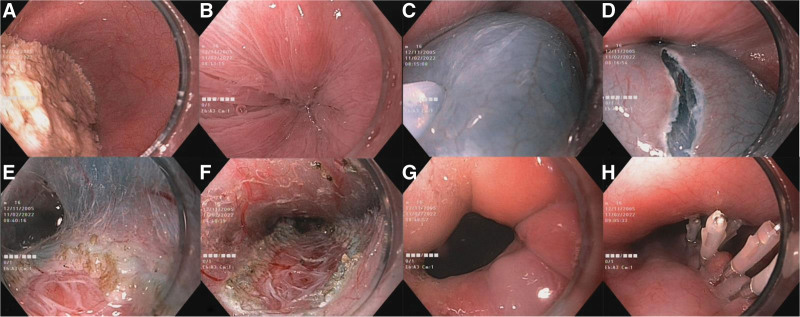
The POEM procedure was performed under general anesthesia and the carbon dioxide was utilized as the insufflation gas throughout the procedure. The Olympus Exera III (EVIS-190 system) paired with a GIF-H190 gastroscope of 9.2 mm diameter featuring a 2.8 mm working channel. Electrocoagulation was used with the ERBE VIO 200D unit and a Dual Jet knife with a 2.0 mm size for the procedure. The mucosal incision was achieved through the Endocut Q mode, utilized to effect level 1, a duration of 4, and an interval setting of 1. During the submucosal tunneling and myotomy phases, the forced coagulation mode was engaged at effect level 3 and a maximum wattage of 45. A submucosal tunnel was started 6 to 8 cm proximal to the esophagogastric junction. Elevation of the mucosa was done by injection of a solution mix of normal saline and indigo carmine. Subsequently, a mucosal incision of approximately 2 cm was performed, followed by tunneling extending to the gastric cardia. A selective myotomy of the inner circular muscle layer on the posterior side of the esophagus was performed. The extent of the myotomy was chosen according to the length of abnormal contractions in the preoperative LES. Upon completion, the esophagogastric junction opening and a thorough inspection for any intratunnel bleeding were assessed prior to closing the mucosal incision point with EZ reloadable hemoclips (Fig. 1). Postoperatively, patients were instructed to abstain from oral intake for 24 hours, after which a soft diet was initiated after a confirmatory contrast esophagram. All patients were initiated on intravenous proton pump inhibitors (PPIs) 1 day before the POEM procedure. The dosing regimen was meticulously calculated based on each patient’s age and weight. This regimen of on intravenous PPIs was maintained until the patients were discharged. Post-discharge, patients were transitioned to oral PPI therapy, which was continued for 1 month following the POEM procedure.
Figure 1.
Peroral endoscopic myotomy procedure stages. (A) Endoscopic visualization of the esophageal lumen with an obstructing food bolus indicating abnormal contraction. (B) Endoscopic detection of pathologic contractions. (C) Submucosal elevation via injection of a solution comprising normal saline and indigo carmine. (D) Creation of a longitudinal incision within the mucosal layer to access the submucosal space. (E) Establishment of a submucosal tunnel and initiation of targeted myotomy of the inner circular muscle layer. (F) Continuation of the selective myotomy extending through the inner circular layer down to the level of the gastric cardia. (G) Endoscopic assessment of the lower esophageal sphincter post-myotomy to ensure adequate opening and release of pressure. (H) Endoscopic application of clips to approximate the mucosal edges and secure closure of the initial access incision.
The procedure outcomes measured were abnormal contraction length and width of the esophagus, contrast delay above the abnormal contraction, integrated relaxation pressure (IRP), and the severity of achalasia symptoms quantified by the Eckardt score. These measurements were obtained at baseline (prior to the procedure), 3 days post-procedure, and at the 12-month follow-up after POEM, where applicable. The Wilcoxon signed-rank test was used to compare pre-POEM and post-POEM parameters within the same group. A P-value of <.001 was considered statistically significant, and statistical analysis was performed using SPSS 26.
3. Results
The baseline characteristics of the participants are presented in Table 1. The study comprised an equal distribution of female and male participants, each representing 50% of the total, with 6 participants in each group, and the mean age of the participants was 99.3 ± 63.9 months. The mean weight was 25.7 ± 14.0 kg, and the average percentage of underweight was 11.5% ± 5.6%. The average height was 119.2 ± 30.4 cm, and a percentage of 4.4% (±1.7%) was the mean percentage of underweight for their age. Body mass index across the population averaged 16.4 ± 1.8. Regarding the Chicago classification of achalasia version 3.0, most patients (91.7%) were classified as Type 2, with only one patient (8.3%) classified as Type 1, and no patients were classified as Type 3. The duration from diagnosis to POEM averaged 12.2 ± 8.5 months. Among the study participants, a substantial majority, 75% (n = 9), had previously received esophageal dilation, in contrast to 25% (n = 3) who had not. The mean duration of post-procedure hospitalization, expressed in bed days, was 9.0 ± 5.0 days.
Table 1.
Baseline characteristics.
| Parameter | Mean ± SD/percentage |
|---|---|
| Age | 99.3 ± 63.9 months |
| Gender | |
| Female | 6 (50%) |
| Male | 6 (50%) |
| Weight | 25.7 ± 14.0 kg |
| Percentage of underweight | 11.5%±5.6% |
| Height | 119.2 ± 30.4 cm |
| Percentage of under height | 4.4%±1.7% |
| Body mass index | 16.4 ± 1.8 |
| Chicago classification | |
| Type 1 | 1 (8.3%) |
| Type 2 | 11 (91.7%) |
| Type 3 | 0 (0%) |
| Duration of diagnosis to POEM | 12.2 ± 8.5 months |
| Previous dilation | |
| Yes | 9 (75%) |
| No | 3 (25%) |
| Bed day | 9.0 ± 5.0 days |
POEM = peroral endoscopic myotomy.
A comparative evaluation of patient characteristics, conducted before and after the POEM, is delineated in Table 2. This analysis revealed a statistically significant improvement in all assessed parameters from the pre-procedure baseline to the 3-day and 12-month post-procedure follow-up. The pre-POEM abnormal contraction length demonstrated a mean of 3.2 cm (standard deviation [SD] 0.4 cm), which showed a significant decrease to 0.2 cm (SD 0.5 cm) 3 days post-procedure and 0.3 cm (SD 0.6 cm) at the 12 months follow-up (P < .001), respectively. Similarly, the esophageal width reduced from a pre-POEM mean of 3.7 cm (SD 0.5 cm) to 2.2 cm (SD 0.4 cm) in the immediate post-procedure period and to 2.0 cm (SD 0.2 cm) after 12 months (P < .001). Furthermore, the pre-procedural IRP was 26.8 ± 5.4 mm Hg, significantly improving to 10.8 ± 1.1 mm Hg after 12 months.
Table 2.
Comparative evaluation of patient characteristics before and after peroral endoscopic myotomy (POEM).
| Before POEM | Post-POEM | P value | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre-procedure | 95% CI | 3 days post-POEM | 95% CI | 12 months post-POEM | 95% CI | Pre-POEM vs 3 days post-POEM | Pre-POEM vs 12 months post-POEM | |
| Abnormal contraction lenght | ||||||||
| 3.2 + 0.4 cm | [2.974–3.426] | 0.2 ± 0.5 cm | [0.083–0.483] | 0.3 ± 0.6 cm | [0.039–0.639] | 0.0001 | 0.0001 | |
| Width of esophagus | ||||||||
| 3.7 ± 0.5 cm | [3.417–3.983] | 2.2 ± 0.4 | [1.974–2.426] | 2.0 ± 0.2 | [1.887–2.113] | 0.0001 | 0.0001 | |
| Contrast delay | ||||||||
| 22.3 ± 7.0 sec | [18.339–26.261] | 1.7 ± .3.7 sec | [0.393–3.793] | 2.1 ± .4.7 sec | [0.559–4.759] | 0.0001 | 0.0001 | |
| High resolution-manometory (IRP) mm Hg | ||||||||
| 26.8 ± 5.4 | [21.508–32.092] | NA | NA | 10.8 ± 1.1 | [9.722–11.878] | NA | 0.0001 | |
| Eckardt score | ||||||||
| 7.0 ± 1.0 | [6.434–7.566] | 1.0 ± 1.7 | [0.0382–1.962] | 1.0 ± 1.7 | [0.0382–1.962] | 0.0001 | 0.0001 | |
Notwithstanding these improvements, the Eckardt score, which assesses the severity of achalasia symptoms, significantly improved from pre-procedure of 7.0 ± 1.0 to post-procedure, indicating a significant improvement of symptoms (P < .001). These findings suggest that POEM is an effective treatment for eliminating esophageal abnormal contraction and improving the Eckardt score in patients with achalasia. Two patients developed gas-related complications, specifically subcutaneous emphysema around the neck area. However, the subcutaneous emphysema resolved spontaneously after 2 days without the need for further intervention or specific treatment. Moreover, 3 patients developed symptomatic gastroesophageal reflux disease (GERD) during the 12-month follow-up period. These patients reported experiencing heartburn symptoms approximately 3 to 4 months after the intervention. A diagnostic gastroscopy revealed that both patients had developed Grade A esophagitis according to the Los Angeles classification. We initiated treatment with PPIs in response to these findings. There is no indication for further invasive intervention, as the symptoms are being managed medically. Moreover, 2 patients developed symptoms of occasional dysphagia and regurgitation after 12 months of follow-up.
4. Discussion
The findings from our nationwide study reveal the efficacy of POEM procedure as a formidable minimal invasive approach for achalasia in pediatric patients within the Mongolian population. Moreover, our findings show that POEM offers significant improvements in structural and functional parameters. The equal distribution of male and female participants and the inclusion of both treatment-naive patients and those with prior esophageal dilations broaden the applicability of the results. Additionally, the study shows that the annual incidence of pediatric achalasia in Mongolia is 0.14 cases per 100,000 individuals, highlighting the rarity of this disorder in the pediatric population.
The management of achalasia in pediatric populations poses significant challenges due to the rarity of the condition and the necessity for therapeutic modalities that are both efficacious and minimally invasive. Therefore, previously, the favored treatment options for pediatric patients were pneumatic dilation and Heller myotomy.[17] Nonetheless, in earlier studies over a 3-year follow-up period, the clinical success rates for Heller myotomy and pneumatic dilations stood at 78% and 45%, respectively.[10,19] In our study, myotomy was only performed on the posterior wall of the esophagus. This strategic choice is predicated on the possibility of necessitating an additional intervention should the initial POEM not produce the anticipated outcomes. Should further treatment be required, the options include either an anterior POEM or a surgical Hellers myotomy. Recent literature has demonstrated that POEM procedure achieves notable technical and clinical success, particularly in enhancing Eckardt scores and significantly reducing the IRP of the LES.[20–24] Additionally, these studies include both short-term and long-term follow-up assessments, with some even comparing the efficacy of POEM between pediatric and adult patients with achalasia, providing a comprehensive evaluation of its effectiveness across different age groups.[14,25–29]
In our study population, the POEM procedure demonstrated a favorable safety profile, 2 patients experienced gas-related complications, presenting as subcutaneous emphysema in the neck area. Remarkably, the subcutaneous emphysema resolved on its own within 2 days, requiring no additional intervention or specific treatment. The emergence of symptomatic GERD in a subset of 3 patients during the follow-up period is consistent with established post-POEM outcomes, highlighting the necessity for continuous monitoring and the development of effective management strategies to address post-procedural GERD. Out of these cases, 2 had not been subjected to prior dilation therapies, whereas 1 had, indicating no significant correlation between prior dilation procedures and the onset of GERD post-POEM. These observations concord with prior literature documenting the incidence of GERD following POEM procedures.[23,28,29] Moreover, the development of the occasional regurgitation and dysphagia in 2 patients during the 12-month follow-up. These findings suggest the possibility of either incomplete myotomy, fibrosis formation, or the natural progression of the disease in some patients. Furthermore, that the 2 individuals who did not benefit optimally from POEM had histories of multiple dilations before undergoing the endoscopic myotomy. This indicates a preference for selecting POEM as the initial treatment modality rather than esophageal dilation. This suggestion arises from observations within our study population where patients with previous dilation exhibited submucosal fibrosis during the POEM procedure. Furthermore, these patients were more likely to experience suboptimal outcomes, as evidenced by the persistence of achalasia symptoms post-POEM. It underscores the need for careful patient selection, precise surgical technique, and possibly longer follow-up to understand the long-term outcomes fully.
Despite the encouraging findings, our study acknowledges the limitations inherent in its retrospective design and the sample size, which may affect the generalizability of the results. Additionally, the lack of a control group precludes a direct comparison with other therapeutic modalities, such as Heller myotomy, thus limiting our ability to determine POEM’s relative efficacy conclusively. Furthermore, identifying the annual incidence rate of 0.14 cases per 100,000 individuals for pediatric achalasia in Mongolia, emphasizing the need for awareness and specialized care for this rare disorder.
In conclusion, POEM is a safe, effective, minimally invasive approach with acceptable clinical outcomes for pediatric patients with achalasia.
Author contributions
Conceptualization: Bayasgalan Luvsandagva, Ganbayar Luuzanbadam, Narantsatsralt Jalbuu, Davaadorj Duger, Xiaohua Hou.
Data curation: Bayasgalan Luvsandagva, Narantsatsralt Jalbuu.
Formal analysis: Bayasgalan Luvsandagva, Bayaraa Bagachoimbol.
Investigation: Bayaraa Bagachoimbol, Ganbayar Luuzanbadam.
Methodology: Bayasgalan Luvsandagva, Battulga Adyasuren, Ganbayar Luuzanbadam, Tao Bai.
Project administration: Davaadorj Duger.
Supervision: Bayasgalan Luvsandagva, Xiaohua Hou.
Validation: Bayasgalan Luvsandagva, Davaadorj Duger.
Writing – original draft: Bayasgalan Luvsandagva.
Writing – review & editing: Bayasgalan Luvsandagva, Battulga Adyasuren, Tao Bai, Narantsatsralt Jalbuu, Davaadorj Duger, Xiaohua Hou.
Abbreviations:
- GERD
- gastroesophageal reflux disease
- IRP
- integrated relaxation pressure
- LES
- lower esophageal sphincter
- POEM
- per oral endoscopic myotomy
- PPI
- proton pump inhibitor
- SD
- standard deviation
Informed consent was obtained from all subjects involved in the study.
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of UB Songdo Hospital (December 1st, 2023).
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Luvsandagva B, Adyasuren B, Bagachoimbol B, Luuzanbadam G, Bai T, Jalbuu N, Duger D, Hou X. Efficacy and safety of peroral endoscopic myotomy for pediatric achalasia: A nationwide study. Medicine 2024;103:32(e38970).
Contributor Information
Battulga Adyasuren, Email: battulgaadya@yahoo.com.
Bayaraa Bagachoimbol, Email: bayarbaga0609@gmail.com.
Ganbayar Luuzanbadam, Email: luuganba@gmail.com.
Tao Bai, Email: drbaitao@126.com.
Narantsatsralt Jalbuu, Email: tsatsaa.nj@gmail.com.
Davaadorj Duger, Email: davaadorj.duger@gmail.com.
Xiaohua Hou, Email: houxh@hust.edu.cn.
References
- [1].Vaezi MF, Pandolfino JE, Vela MF. ACG Clinical Guideline: Diagnosis and Management of Achalasia. Am J Gastroenterol. 2013;108:1238–49; quiz 1250. [DOI] [PubMed] [Google Scholar]
- [2].Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010;22:e256–261. [DOI] [PubMed] [Google Scholar]
- [3].Laurino-Neto RM, Herbella F, Schlottmann F, Patti M. Evaluation of esophageal achalasia: from symptoms to the Chicago classification. Arq Bras Cir Dig. 2018;31:e1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Khlevner J, Patel D, Rodriguez L. Pediatric neurogastroenterology and motility disorders: what role does endoscopy play? Gastrointest Endosc Clin N Am. 2023;33:379–99. [DOI] [PubMed] [Google Scholar]
- [5].Pressman A, Behar J. Etiology and pathogenesis of idiopathic achalasia. J Clin Gastroenterol. 2017;51:195–202. [DOI] [PubMed] [Google Scholar]
- [6].Meyer A, Catto-Smith A, Crameri J, et al. Achalasia: outcome in children. J Gastroenterol Hepatol. 2017;32:395–400. [DOI] [PubMed] [Google Scholar]
- [7].Sato H, Yokomichi H, Takahashi K, et al. Epidemiological analysis of achalasia in Japan using a large-scale claims database. J Gastroenterol. 2019;54:621–7. [DOI] [PubMed] [Google Scholar]
- [8].Miller J, Khlevner J, Rodriguez L. Upper gastrointestinal functional and motility disorders in children. Pediatr Clin North Am. 2021;68:1237–53. [DOI] [PubMed] [Google Scholar]
- [9].Franklin AL, Petrosyan M, Kane TD. Childhood achalasia: a comprehensive review of disease, diagnosis and therapeutic management. World J Gastrointest Endosc. 2014;6:105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg. 2009;249:45–57. [DOI] [PubMed] [Google Scholar]
- [11].Smits M, van Lennep M, Vrijlandt R, et al. Pediatric achalasia in the Netherlands: incidence, clinical course, and quality of life. J Pediatr. 2016;169:110–5.e3. [DOI] [PubMed] [Google Scholar]
- [12].Lee Y, Brar K, Doumouras AG, Hong D. Peroral endoscopic myotomy (POEM) for the treatment of pediatric achalasia: a systematic review and meta-analysis. Surg Endosc. 2019;33:1710–20. [DOI] [PubMed] [Google Scholar]
- [13].Mencin AA, Sethi A, Barakat MT, Lerner DG. Peroral endoscopic myotomy (POEM) in children: a state of the art review. J Pediatr Gastroenterol Nutr. 2022;75:231–6. [DOI] [PubMed] [Google Scholar]
- [14].Miao S, Wu J, Lu J, et al. Peroral endoscopic myotomy in children with achalasia: a relatively long-term single-center study. J Pediatr Gastroenterol Nutr. 2018;66:257–62. [DOI] [PubMed] [Google Scholar]
- [15].Tashiro J, Petrosyan M, Kane TD. Current management of pediatric achalasia. Transl Gastroenterol Hepatol. 2021;6:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Van Lennep M, Van Wijk MP, Omari TIM, Benninga MA, Singendonk MMJ. Clinical management of pediatric achalasia. Expert Rev Gastroenterol Hepatol. 2018;12:391–404. [DOI] [PubMed] [Google Scholar]
- [17].van Lennep M, van Wijk MP, Omari TIM, Salvatore S, Benninga MA, Singendonk MMJ. Clinical management of pediatric achalasia: a survey of current practice. J Pediatr Gastroenterol Nutr. 2019;68:521–6. [DOI] [PubMed] [Google Scholar]
- [18].de Onis M. WHO child growth Standards based on length/height, weight and age. Acta Paediatr. 2006;95:76–85. [DOI] [PubMed] [Google Scholar]
- [19].Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–16. [DOI] [PubMed] [Google Scholar]
- [20].Choné A, Familiari P, von Rahden B, et al. Multicenter evaluation of clinical efficacy and safety of per-oral endoscopic myotomy in children. J Pediatr Gastroenterol Nutr. 2019;69:523–7. [DOI] [PubMed] [Google Scholar]
- [21].Lee CW, Kays DW, Chen MK, Islam S. Outcomes of treatment of childhood achalasia. J Pediatr Surg. 2010;45:1173–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Nabi Z, Talukdar R, Chavan R, Basha J, Reddy DN. Outcomes of per-oral endoscopic myotomy in children: a systematic review and meta-analysis. Dysphagia. 2022;37:1468–81. [DOI] [PubMed] [Google Scholar]
- [23].Saez J, Mejia R, Pattillo JC, et al. Per oral endoscopic myotomy (POEM) in pediatric patients with esophageal achalasia: first Latin-American experience. J Pediatr Surg. 2021;56:706–10. [DOI] [PubMed] [Google Scholar]
- [24].Sbaraglia F, Familiari P, Maiellare F, et al. Pediatric anesthesia and achalasia: 10 years’ experience in peroral endoscopy myotomy management. J Anesth Analg Crit Care. 2022;2:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Bi Y-W, Lei X, Ru N, et al. Per-oral endoscopic myotomy is safe and effective for pediatric patients with achalasia: a long-term follow-up study. World J Gastroenterol. 2023;29:3497–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Liu Z, Wang Y, Fang Y, et al. Short-term safety and efficacy of peroral endoscopic myotomy for the treatment of achalasia in children. J Gastroenterol. 2020;55:159–68. [DOI] [PubMed] [Google Scholar]
- [27].Mejía R, Sáez J, Aranda F, et al. Per oral endoscopic myotomy in a pediatric patient with achalasia. Rev Chil Pediatr. 2019;90:88–93. [DOI] [PubMed] [Google Scholar]
- [28].Nabi Z, Ramchandani M, Basha J, Goud R, Darisetty S, Reddy DN. POEM is a durable treatment in children and adolescents with achalasia cardia. Front Pediatr. 2022;10:812201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Peng D, Tan Y, Li C, et al. Peroral endoscopic myotomy for pediatric achalasia: a retrospective analysis of 21 cases with a minimum follow-up of 5 years. Front Pediatr. 2022;10:845103. [DOI] [PMC free article] [PubMed] [Google Scholar]