Abstract
Introduction
Empathy with the patient is one of the important factors in nursing care. This study aims to investigate the mediating role of self-compassion in the relationship between attachment styles and empathy in nurses.
Materials and methods
This correlational study was conducted using structural equation modeling (SEM) method. The statistical population included nurses working at public hospitals in Yazd City, Iran. A total of 308 nurses were selected by convenience sampling method. The data were collected using self-compassion scale, adult attachment styles scale, Jefferson scale of empathy and analyzed using structural equation analysis in AMOS software.
Results
Secure and anxious/ambivalent insecure attachment styles were positively and negatively correlated with empathy, respectively (p < .01). The path coefficient between avoidant and anxious/ambivalent insecure attachment styles and self-compassion was negative. On the contrary, the path coefficient between secure attachment style and self-compassion was positive. There was a positive correlation between self-compassion and empathy. The indirect path coefficient of secure and anxious/ambivalent insecure attachment styles to empathy through self-compassion. was significant (p < .01).
Conclusion
The results showed secure and anxious/ambivalent insecure attachment could directly and indirectly through influencing self-compassion predict empathy in nurses.
Keywords: Attachment styles, Empathy, Self-compassion, Nurses
Introduction
Care quality is among the most important indicators for measuring the quality of hospital services. Nurses play an important role in monitoring and evaluating patients and should perform appropriate interventions to reduce risks or prevent disease complications. Nurses play an essential role in improving hospital quality while providing comprehensive and patient-centered care [1]. Therefore, nurses as health care professionals who have constant and close contact with patients and their families should have empathy for them in order to ensure good nursing practice, obtain positive results and create an effective therapeutic relationship [2]. Empathy is an individual variable recognized by nursing personnel as a necessity to perform their professional work properly [3].
Empathy in nurses
Empathy is defined as an emotional ability to put oneself in the shoes of others, understand their state of mind and think about their emotions [4] and considered as a prosocial behavior [5]. Empathy consists of three main dimensions: (1) Cognitive empathy (knowing what others feel), (2) Emotional empathy (feeling what others feel), (3) Behavioral empathy (the ability to communicate and understand others’ viewpoints) [6]. Empathy is defined as a predominantly cognitive (rather than emotional) attribute that involves understanding (rather than feeling) patients’ experiences, concerns and perspectives along with the capacity to convey this understanding [7]. Empathy is effective in the nurse-patient relationship and healthcare outcomes; In addition to having positive outcomes for the patient [8], this concept is associated with factors such as respect, prosocial behavior, moral reasoning, positive attitude toward illness, ability to take a good medical history and improved clinical outcomes [9]. Therefore, empathic statements create cooperative relationship and trust among nurses and patients, which is considered important for maintaining patients’ adherence to nurses’ recommendations [10] and increasing their satisfaction with the care provided [11]. Therefore, an empathic relationship between nurses and patients leads to positive therapeutic outcomes, increases nurses’ adaptability in educational and therapeutic environments and affects their moral sensitivity [12]. Those with higher empathy could exhibit more social behaviors and better perceive others’ emotions and communicate with them [13]. Therefore, the concept of empathy, which seems to be very important in determining altruistic and social behavior, is strongly associated with individuals’ attachment styles. The strong association between empathy and attachment styles is well-supported by research. Studies have shown that secure attachment correlates with higher empathy levels [14], while theoretical models and neurobiological evidence further substantiate this link [15, 16]. Therefore, the conclusion is based on comprehensive empirical, theoretical, and neurobiological findings.
Attachment styles and empathy
In the past decades, attachment theory has become one of the most comprehensive and popular theories in modern psychology. Attachment theory provides a basic relational framework for understanding people’s experience in close relationships, interpreting others’ intentions and regulating their impacts and behaviors in the social environment [17]. Attachment theory is based on the idea that close personal relationships may have a profound influence on one’s performance in various interpersonal and social domains [18]. Attachment, as the human desire for emotional connection and understanding close relationships and intimacy, may facilitate or hinder development of empathic abilities among health professionals [19]. Healthcare providers’ attachment styles could affect their ability to understand and communicate patients’ emotions and experiences [20]. This ability is directly associated with empathy domains (cognitive and emotional), particularly cognitive one [21], and used to understand the patient’s suffering in order to make communication and provide help [22]. The three suggested attachment styles are secure, anxious and avoidant. Secure people could communicate and seek support from others when necessary and have a high level of care. They are more capable of establishing close relationships and discovering and responding to patients’ concerns [18]. They could communicate in a flexible and patient-centered manner [23]. In contrast, anxious individuals have less intimacy in relationships and may be less able to respond appropriately to patients’ emotions [24]. Finally, avoidant individuals show uncertainty about themselves and others and may avoid intimacy with others due to negative expectations [25]. Therefore, attachment styles could significantly contribute to our understanding of how people respond positively to stressful life events and their resilience to those events [18]. Attachment theorists argue that self-regulation skills such as self-compassion arise from positive social bonds, particularly with parents and important individuals [26].
Self-compassion and empathy
Self-compassion includes kindness and self-perception in times of personal hardship and failure [27] and is considered a protective factor that could be effective in the face of adversity [28]. Self-compassion is used as a useful strategy for coping with psychological distress by being aware of negative emotions, rather than avoiding them, and using self-kindness in the context of shared human experiences for reducing pain and suffering [29]. Neff [29] proposed that self-compassion consists of three components, each of which has two contrasting dimensions: (1) Kindness versus self-judgment, which includes kind and understanding attitudes towards oneself versus harsh criticism in times of trauma, (2) Common humanity versus isolation, which refers to recognizing suffering and failure as the shared human experience versus a separate experience that only happens to one, (3) Mindfulness versus overidentification, which involves a balanced approach to thoughts and feelings versus suppressing or exaggerating the painful experience. Accordingly, people could reduce self-blame, negative emotional states such as guilt and shame, and anxiety and depression symptoms [30]. Individuals with high levels of self-compassion are less likely to experience negative emotions when faced with negative life events [31] because they have a balanced view of suffering and are more objective in understanding negative life events. These individuals have more effective coping styles when faced with suffering [32]. Given that self-compassion involves directing compassion towards oneself, adopting a compassionate view towards oneself is similar to the way compassion is usually offered to others. Thus, individuals with higher levels of self-compassion would be expected to show a greater capacity for empathy. Furthermore, self-compassion improves interpersonal functioning, which is associated with attributes such as empathic concern, altruism, attitudinal perspective and forgiveness [33]. Evidence has demonstrated self-compassion improves one’s relationship with others and encourages more empathic care and altruism [34]. Since self-compassion trait is partially shaped by early family experiences [26], it is a mindset that could be taught through targeted interventions [35].
Proposed model
It seems that attachment styles not only directly affect nurses’ self-compassion, but also indirectly cause nurses’ empathic behaviors by influencing self-compassion. Self-compassion, defined as self-kindness and self-acceptance, could be useful for healthcare professionals, especially nurses; because it could play an important role in maintaining their mental health. Recent evidence has shown self-compassion is associated with compassion for others and has a significant impact on disease outcomes [36]. This concept has recently emerged as an important structure that is strongly associated with secure attachment. Individuals with secure attachment respond to others’ needs with more empathy and lower levels of personal distress. Moreover, secure attachment is mainly activated by interacting with empathy and affection for others and, consequently, a stable relationship is established between secure attachment and empathic thoughts and memories [37]. According to the presented evidence, it is assumed that self-compassion plays a mediating role in the relationship between attachment styles and empathy in nurses.
Present study
Empathy in nurses is one of the most important factors that affect the quality of care provided to patients, so investigating factors related to it can help hospital managers to have intervention programs to strengthen empathy in nurses. Although the importance of empathy in nursing care is understood, few studies have investigated its related factors. Based on the theories of attachment style and compassion, this study has assumed that these two variables can be related to empathy in nurses. If the proposed model in this study is confirmed, it can be suggested that compassion focused interventions and interventions based on improving attachment styles can be effective for improving empathy in nurses. Accordingly, the aim of this study was to evaluate the mediating role of self-compassion in the relationship between attachment styles and empathy in nurses. In this study, we explore the mediation pathways involving self-compassion, attachment styles, and empathy among nurses. Mediation analysis helps elucidate how self-compassion may act as a mechanism through which attachment styles influence nurses’ empathetic responses, offering insights into potential interventions to enhance patient care.
Method
This descriptive and correlational research was conducted using structural equation analysis. The statistical population included all nurses working at public hospitals in Yazd City, Iran. A total of 308 participants were selected by convenience and voluntary sampling method. The estimation of the sample size was based on the population size (approximately 1500 nurses) and Cochran’s formula. The sample size of 308 participants was determined to be adequate based on several methodological considerations for correlation and structural equation modeling (SEM). Kline [38] suggests that sample sizes between 200 and 400 are generally sufficient for SEM, depending on the complexity of the model. Given that our model includes the total scores of self-compassion, empathy, and the three subscales of attachment styles as observed variables, the chosen sample size ensures sufficient power and reliability for detecting meaningful relationships [39]. This sample size also aligns with the rule of thumb that recommends at least 10 participants per parameter estimated in the model, further validating its adequacy [39]. It was tried that the number of nurses selected from each hospital and its different wards should be proportional to the total number of nurses working in that hospital and its wards. The inclusion criteria were having at least two years of work experience and living with both parents during childhood, and the exclusion criteria included the death of one of the parents or the divorce of the parents during childhood. These criteria were chosen to ensure participants had sufficient professional experience and a consistent baseline for assessing attachment styles. Excluding significant early-life disruptions minimized confounding factors related to disorganized attachment, allowing for a clearer focus on the relationship between attachment styles, empathy, and self-compassion. The study emphasized primary caregiver influence, acknowledging sibling relationships but not including them to maintain focus and clarity. These criteria were designed to create a more homogeneous sample in terms of early family environment, which is relevant to our study variables (attachment styles, empathy, and self-compassion). We acknowledge that the use of convenience sampling may introduce sampling bias, as it relies on the availability and willingness of participants to volunteer. This method may not fully capture the diversity of the nursing population in Yazd City, potentially limiting the generalizability of the findings. To mitigate this risk, we employed proportional sampling across different hospitals and wards, which aimed to enhance the representativeness of our sample. Despite these efforts, there remains a possibility of self-selection bias, where nurses who chose to participate may differ systematically from those who did not, potentially affecting the study’s outcomes. While these limitations are inherent in convenience sampling, we believe that the proportional approach and the large sample size contribute to a reasonably representative sample, thus supporting the generalizability of our findings to similar nursing populations in comparable settings.
Measures
2.1.1. Self-Compassion Scale (SCS): The SCS has 26-item in six subscales, including self-kindness, self-judgment, human commonalities, isolation, mindfulness and over-identification [40]. Items were scored on a 5-point Likert scale, ranging from 1 = completely disagree to 5 = completely agree. Higher scores indicated a higher level of self-compassion. The reliability and validity for this scale were appropriate [40]. The SCS has demonstrated strong psychometric properties across multiple studies. For instance, a study by Neff [40] established the SCS’s internal consistency with Cronbach’s alpha coefficients ranging from 0.75 to 0.94 for the various subscales. Additionally, test-retest reliability over a three-week period yielded coefficients from 0.80 to 0.93, indicating stability over time. The scale’s validity is further supported by significant correlations with measures of mental health, including positive associations with psychological well-being and negative associations with depression and anxiety [41]. Cronbach’s alpha coefficient of the Persian version of the SCS was 0.70; the Construct validity was confirmed using confirmatory factor analyses. Convergent and divergent validity was confirmed using Rosenberg’s self-esteem scale and Beck depression and anxiety inventories, respectively [42]. In another study, Cronbach’s alpha for total score was 0.76. and for subscales of self-kindness, self-judgment, human commonalities, isolation, mindfulness and over-identification were 0.81, 0.79, 0.84, 0.85, 0.80 and 0.83, respectively [43].
2.1.2. Adult Attachment Styles Scale (AAS): The AAS was developed based on attachment scale items [44] and standardized on students at University of Tehran [45]. This 15-item scale measured three attachment styles, namely secure, avoidant and ambivalent, in a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s alpha coefficients of secure, avoidant and ambivalent subscales were calculated as 0.86, 0.84 and 0.85 respectively. Additionally, test-retest reliability was robust, with coefficients of 0.82, 0.78, and 0.75 for secure, avoidant, and ambivalent styles, respectively [45]. The AAS concurrent validity was confirmed by simultaneously implementing interpersonal problem inventory and self-esteem inventory. The factor analysis confirmed the AAS construct validity [45]. the AAS has shown good concurrent validity, with significant correlations between attachment styles and measures of emotional regulation and interpersonal problems [46].
2.1.3. The Jefferson Scale of Empathy (JSE): The 20-item JSE measured nursing students’ empathy for patients and comprised three subscales of perspective taking (10 items), compassionate care (7 items) and standing in the patient’s shoes (3 items). The items were scored based on a 7-point Likert scale [7]. Several studies have examined and confirmed the scale validity and reliability. The test-retest reliability and Cronbach’s alpha coefficient were 0.65 and 0.81, respectively [7]. Additionally, the JSE’s concurrent validity is supported by significant correlations with other empathy-related measures, such as the Empathy Construct Rating Scale and the Interpersonal Reactivity Index, indicating its robustness as a tool for assessing empathy in healthcare settings [22]. Cronbach’s alpha coefficient of The Persian version of the scale was 0.63 for total score and were 0.71, 0.63 and 0.62, for subscales of perspective taking, compassionate care and standing in the patient’s shoes, respectively. The content validity of the JSE was confirmed [47]. In another study, Cronbach’s alpha coefficient of the Persian version was 0.83 and the factor structure was confirmed [48].
Data analysis
Structural equation modeling (SEM) was conducted for analyzing the data. SEM was chosen due to its ability to concurrently assess direct and mediated relationships, aligning with the study’s focus on exploring the mediating role of self-compassion between attachment styles and empathy in nurses. Path analysis was employed to test the hypothesized relationships, with self-compassion serving as a mediator in the model. The normality of distributions was analyzed using Kolmogorov-Smirnov test. The variance inflation factor and tolerance test were used for evaluating the collinearity between independent variables. Independence of error variables from each other was analyzed using Durbin-Watson test. Linear relationship between the variables was examined using a scatter plot. Finally, indirect coefficients between variable were analyzed using bootstrapping method. The bootstrapping method was employed due to its robustness in estimating the sampling distribution of a statistic. This non-parametric approach allows for the computation of confidence intervals without assuming normality, which is particularly useful for small sample sizes or non-normally distributed data. By resampling the data with replacement and calculating the indirect effects repeatedly, bootstrapping provides more accurate and reliable estimates of mediation effects.
Results
In total, 122 participants were male (40%) and 186 were female (60%). The mean (± SD) age of the participants was 33.51 (± 7.11) years old. Moreover, 212 nurses were married (69%) and 96 were single (31%). The mean and standard deviation of work experience of the participants were 9.17 years and 6.29, respectively. Also, 92 nurses were working in internal and surgery wards (29.9%), 51 nurses in the ICU and CCU (16.5%), 43 nurses in the cardiac ward (14%), 64 nurses in obstetric, gynecologic and neonatal ward (20.8%), 46 nurses in the emergency department (14.9%) and 12 nurses in the radiology department (3.9%). Table 1 presents the mean, standard deviation and Pearson correlation between the studied variables.
Table 1.
Mean, standard deviation and Pearson correlation between variables
| Variables | 1 | 2 | 3 | 4 | Mean | SD |
|---|---|---|---|---|---|---|
| 1. Secure attachment | 1 | 13.97 | 3.99 | |||
| 2. Avoidant attachment | − 0.54* | 1 | 17.22 | 3.38 | ||
| 3. Anxiety/ambivalent Attachment | − 0.64* | 0.66* | 1 | 17.31 | 4.07 | |
| 4. Self-compassion | 0.75* | − 0.58* | − 0.66* | 1 | 70.08 | 18.73 |
| 5. Empathy | 0.77* | − 0.58* | − 0.67* | 0.87* | 72.85 | 24.87 |
* p < .001
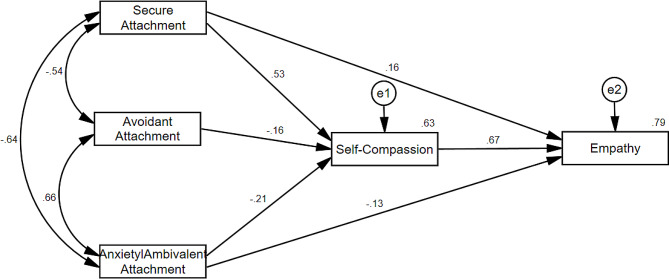
There were strong correlation coefficients greater than 0.5 between the variables, indicating a high covariance among the variables. Secure attachment style was significantly and positively correlated with empathy and self-compassion, while avoidant and ambivalent insecure attachment styles were significantly and negatively correlated with self-compassion and empathy. The proposed model was tested using path analysis. Before testing the model, path analysis assumptions were evaluated. The variable scores were normally distributed. This test compares the sample distribution to a normal distribution to determine if the data significantly deviates from normality. In our study, the results indicated that the data were normally distributed, as the Kolmogorov-Smirnov test did not show significant deviations from normality (p > .05 for all variables). To evaluate collinearity between independent variables, we calculated the Variance Inflation Factor (VIF) and performed the tolerance test. A VIF value greater than 10 and a tolerance value less than 0.1 indicate potential multicollinearity issues. All independent variables in our study showed VIF values below 10 and tolerance values above 0.1, indicating no significant collinearity concerns. Independence of error variables from each other was confirmed using Durbin-Watson test, with values close to 2 suggesting no autocorrelation. The linear relationship between the variables was examined using scatter plots, which displayed data points for each pair of variables. The scatter plots showed a consistent linear pattern without significant deviations, confirming the linearity assumption. The proposed model was tested by path analysis (Fig. 1). The path coefficients showed avoidant (β= − 0.16) and anxious/ambivalent (β= − 0.21) insecure attachment styles had a significant and negative effect on self-compassion, while secure attachment style had a significant and positive impact on self-compassion (β = 0.53). In terms of path coefficient strong, the path coefficient between secure attachment style and self-compassion was significantly higher than that between insecure attachment styles and self-compassion. Secure attachment style had a significant and positive effect on empathy (β = 0.16). The path coefficient between anxious/ambivalent insecure attachment style and empathy was significant and negative among nurses (β= − 0.13). The path coefficient between avoidant attachment style and empathy was not significant, so it was removed to fit the model.
Fig. 1.
Direct paths between variables
Table 2 presents the model fit indices. The Chi-square value was not significant (p = .11, df = 2, X2 = 4.46), which was considered desirable for model fitness. The ratio of Chi-square to degree of freedom (df) was 2.23 in the tested model, which was suitable for model fitness. Goodness of fit index (GFI), normal fit index (NFI), relative fit index (RFI), incremental fit index (IFI) and comparative fit index (CFI) were all greater than 0.90, which were considered favorable for model fitness. The root mean square error of approximation (RMSEA) was 0.06, which was considered favorable (the value under 0.08 is considered for model fitness). The results showed the data supported and confirmed the proposed model.
Table 2.
Fitness indices of tested model
| Index | CMIN | DF | Sig. | CMIN/DF | GFI | NFI | IFI | TLI | CFI | RMSEA |
|---|---|---|---|---|---|---|---|---|---|---|
| Statistics | 4.461 | 2 | 0.107 | 2.230 | 0.994 | 0.996 | 0.998 | 0.989 | 0.998 | 0.063 |
The mediating role of self-compassion in the relationship between attachment styles and nurses’ empathy was examined using bootstrapping method. Since the direct path between avoidant attachment style and empathy was insignificant, bootstrapping was not calculated for this attachment style. However, the indirect path coefficient between secure (β = 0.35) and anxious/ambivalent insecure (β= − 0.14) attachment styles and empathy through self-compassion was significant (p < .01). Thus, it could be concluded that self-compassion had a significant mediating role in the relationship between secure and anxious/ambivalent insecure attachment styles and empathy among nurses.
Discussion
This study investigated the mediating role of self-compassion in the relationship between attachment styles and empathy among nurses. The results showed a significant correlation between empathy and self-compassion among nurses, which was consistent with previous studies [49, 50]. The evidence showed that individuals with higher self-compassion had more empathy for others, leading to better interaction with them [50]. The importance of examining nurses’ self-compassion highlighted because nurses may not be sufficiently prepared to be compassionate to patients without self-compassion [49]. Although the concept of empathy encompasses different aspects, the person’s ability to understand others’ feelings represents its core [51]. Compassion is a fundamental component of the nursing care process, as even minimal self-compassion can enhance empathy and compassion towards patients. Therefore, the discomfort caused by others’ suffering may cause nurses to empathize and relieving this suffering boosts personal and professional satisfaction. Therefore, professional health cares with higher job satisfaction have more self-compassion [52].
The results revealed empathy was significantly and positively correlated with secure attachment and negatively correlated with anxious/ambivalent insecure attachment. These findings were in line with previous studies [53, 54]. The evidence showed attachment style could be an indicator of empathic behavior and nurses with the highest level of secure attachment had the highest level of empathy [54]. The attachment theory could be a useful theoretical framework for medical students who try to provide appropriate interventions for promoting empathy in interpersonal environments. Medical students with secure attachment demonstrate empathy without feeling emotional distress [53]. Therefore, having a secure attachment style is beneficial in terms of providing high-quality care to patients and their families and being an active and effective member of the healthcare team [19]. Empathy and attachment styles, which are among the most important elements of care, are necessary for paying empathic attention to patients’ needs, establishing a good relationship with other healthcare professionals, strengthening the work team and predicting nurses’ ability to cope with difficult situations and use effective coping methods for stress management [55, 56].
Self-compassion was significantly and positively correlated with secure attachment and negatively correlated with anxious/ambivalent insecure attachment among nurses. This finding was in line with previous studies [57, 58]. The findings showed people with a secure attachment style had more self-compassion, were more involved in activities effective in growth, had more meaningful life, showed more mastery of managing their life conditions and had more satisfying relationships with others [57]. The evidence showed anxious and avoidant attachment styles were associated with less self-compassion and more anxiety and depression simultaneously [58]. Previous studies have introduced self-compassion as a mediator between attachment styles and mental health and revealed people with an insecure attachment style (anxious and avoidant) have less attention to themselves, which could negatively affect their overall health and well-being [59]. Therefore, attachment styles and self-compassion are key factors in adapting to challenging situations. Both attachment styles and self-compassion are efficient in difficult experiences. Attachment behaviors are activated by threats (e.g., illness) [18], while self-compassion provides a way to connect to ourselves during difficult times [60]. Individuals with insecure attachment who have experienced unpredictable and less supportive environments have more difficulty accessing self-compassion and are more self-critical. However, individuals with a secure attachment may respond to life’s challenges with gentleness and understanding (e.g., self-compassion) [61]. Attachment theory could be a useful framework for examining nurses’ self-compassion.
Finally, the results showed self-compassion played a mediating role in the relationship between nurses’ attachment styles and empathy, which was in line with previous studies [62, 63]. The evidence showed empathy, secure attachment style and self-compassion are predictors of helping others [62]. Helpful people had a positive attitude towards helping those in need and had a more secure attachment style and greater self-compassion. Moreover, the results revealed strong empathy, secure attachment style and high self-compassion were psychological prerequisites for adopting positive attitudes and helpful behaviors towards others [62].
Self-compassion is among the reassurance sources that has preventive and promotional strengths and significantly maintains harmony with the internal and external realities of people’s lives [64]. According to self-compassion theory, self-compassion could be developed by early attachment experiences [65]. Attachment style could affect how nurses evaluate and cope with stressful situations and their response to patients’ needs. Individuals with secure attachment could manage stressful situations constructively without being influenced by negative emotions [66]. In general, secure attachment, as an internal resource, could facilitate stress and fear management by promoting people’s adaptation and helping them control negative emotions throughout life [67]. Secure attachment provides a stable foundation for empathy. The evidence shows secure attachment is associated with higher levels of emotion regulation, leading to empathy [68].
Self-compassion serves as a crucial mediator in understanding the relationship between attachment styles and empathy among nurses [29]. Attachment styles, which are formed through early interactions with caregivers, influence how individuals perceive and respond to social and emotional cues throughout their lives. Secure attachment styles are often associated with higher levels of empathy, as individuals with secure attachments tend to have greater emotional regulation skills and capacity for perspective-taking [18]. On the other hand, insecure attachment styles (such as avoidant or ambivalent) may hinder empathetic responses due to difficulties in managing one’s own emotions or connecting with others’ emotional experiences. Self-compassion, characterized by kindness toward oneself in times of suffering or failure, plays a pivotal role in mitigating the negative impact of insecure attachment styles on empathy.
Nurses who exhibit higher levels of self-compassion are more likely to approach patient interactions with empathy and understanding, regardless of their attachment styles. Self-compassion acts as an internal resource that buffers against the potential emotional barriers posed by insecure attachment patterns [32]. By cultivating self-compassion, nurses may enhance their ability to empathize with patients’ experiences, thereby fostering therapeutic relationships and improving patient outcomes.
Understanding the mediating role of self-compassion provides insights into interventions and strategies that can promote empathetic caregiving among nurses. By promoting self-compassion practices and addressing attachment-related challenges, healthcare organizations can support nurses in delivering compassionate and patient-centered care.
Conclusion
Self-compassion, which is an important indicator of mental health, has recently received attention as a factor in resisting stress, burnout and emotional exhaustion. This is a valuable coping resource for nurses who experience stressful working conditions, which may be beyond their direct control. From a theoretical perspective, self-compassion most likely mediates the relationship between attachment style and positive outcomes. Those with secure attachment could provide more effective care for others because feeling of security is closely associated with optimistic beliefs and self-efficacy when coping with distress. Nurses’ attachment styles could affect their communication and empathic relationship with patients. Empathic behaviors have positive effects on nurses, including providing more effective care and experiencing less psychological stress and burnout. Although empathy is a key component in the nurse-patient relationship, hyperalgesia and others’ suffering could have harmful effects on nurses’ mental health, which could limit their ability to provide effective care. This is especially true when nurses lack self-compassion skills. Therefore, training self-compassion may be valuable for preventing burnout and promoting job satisfaction. Some interventions are required for increasing self-compassion, as it has been confirmed that self-compassion could be learned. It is recommended to develop and implement training interventions focused on strengthening personal competencies related to empathy, such as communication skills or emotional competencies, for nurses and healthcare providers in order to create a safe environment and quality working conditions. On the other hand, the nurse’s awareness of attachment styles and its role on self-compassion and empathy can be increased in order to prevent the negative consequences of insecure attachment styles. Our findings underscore the significant mediating role of self-compassion in linking attachment styles to empathy among nurses. These results suggest that promoting self-compassion practices could enhance nurses’ empathetic capabilities, thereby improving patient care outcomes. Future research should explore tailored interventions that foster self-compassion in healthcare settings to further support compassionate caregiving.
Implications for practice
-
A.
Promoting Self-Compassion in Training Programs: Training programs should incorporate self-compassion training as a core component. Interventions that enhance self-compassion can help nurses manage stress and emotional exhaustion, potentially improving their empathetic engagement with patients. Programs such as mindfulness-based stress reduction (MBSR) or self-compassion training workshops could be integrated into nursing education and ongoing professional development.
-
B.
Addressing Attachment Styles in Clinical Training: Recognizing the impact of attachment styles on empathy, nursing training programs should include modules that help nurses understand their own attachment styles and how these influence their interactions with patients. Workshops or counseling sessions that explore attachment theory and its implications for patient care could enhance nurses’ self-awareness and interpersonal skills.
-
C.
Developing Supportive Work Environments: Healthcare organizations should foster a supportive work environment that encourages self-compassion and emotional well-being. This can be achieved by creating policies that reduce work-related stress, promote work-life balance, and provide access to psychological support and counseling services. Supportive supervision and peer support groups can also enhance nurses’ resilience and empathy.
-
D.
Incorporating Empathy Training into Routine Practice: Practical training sessions focused on empathy-building exercises, role-playing, and reflective practice should be a standard part of nursing curricula. Simulation-based training and real-life scenarios can help nurses develop and refine their empathetic skills, making them more effective in patient care.
-
E.
Research and Continuous Improvement: Future research should explore the long-term effects of self-compassion training on nursing performance and patient outcomes. Additionally, studies could investigate the best practices for integrating attachment-focused interventions into nursing education and clinical practice. Continuous evaluation and adaptation of training programs based on empirical evidence will ensure that they remain effective and relevant. By implementing these strategies, healthcare institutions can enhance the empathetic competencies of their nursing staff, ultimately improving patient care and satisfaction. The integration of self-compassion and attachment awareness into nursing practice is essential for fostering a compassionate, patient-centered care environment.
Limitation & future studies
Intervening variables such as the quality of relationship with colleagues, the atmosphere of the work environment and other demographic variables that might affect the results of the study were not controlled due to financial and time constraints. One limitation of this study is the use of a convenience sampling method, which may introduce sampling bias and affect the generalizability of the findings. While proportional sampling was employed to mitigate this risk, the voluntary nature of participation may still result in self-selection bias. The prevalence of the corona virus and fatigue caused by work pressure may have affected the responses of nurses to the questionnaires. The challenging work environment and stressors during the pandemic may have affected nurses’ perceptions of their empathetic abilities and self-compassion assessed in this study. Therefore, it is suggested to repeat this study in normal conditions where is less work pressure on nurses. To ensure the robustness of the results, future studies should consider controlling for potential confounding variables, including the quality of relationships with colleagues and the overall work environment atmosphere, which were not fully addressed in this study due to resource constraints. It is also suggested to examine the moderating role of demographic variables such as gender, work experience, and work environment in the proposed model presented in this study. This study employed a cross-sectional design due to time constraints and practical limitations. Data were collected at a single point in time, allowing for efficient gathering of information from participants. While this approach facilitated timely completion, it limits the ability to infer causality and observe changes over time. We acknowledge these limitations and consider them in the interpretation of our findings. Finally, the study’s findings may have limited generalizability due to the specific focus on nurses in public hospitals in Yazd, as well as the unique challenges posed by the COVID-19 pandemic and increased work pressures. Future research should consider replicating the study in diverse healthcare settings and populations to assess the broader applicability of the relationships among attachment styles, self-compassion, and empathy observed in this study.
Acknowledgements
The authors would like to thank all the nurses who participated in this research.
Author contributions
MHA participated in study design, data analysis and preparing the manuscript. Y R-M participated in gathering the theoretical framework and preparing the manuscript. FK participated in gathering and theoretical framework and revision of the manuscript. NA participated in data collection. All authors read and approved the final manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The research objectives were explained to the participants and they were assured of confidentiality of their information. Nurses participated in the study with informed consent and signed the consent form. Consent was obtained from the participants in a consent form to publish their identifiable data in an open access online journal. This study was approved by Ethics Committee of Yazd University of Medical Sciences in accordance with the Declaration of Helsinki (ID: IR.YAZD.REC.1400.056). This ethical approval can be viewed online at: https://ethics.research.ac.ir/form/tx5uwwr26azuzq92.pdf). All methods were performed in accordance with the relevant guidelines and regulations. Additionally, rigorous measures were implemented to maintain ethical standards throughout the study. These included continuous assurance of participant confidentiality, rigorous anonymization of data during analysis to protect privacy, and adherence to the Declaration of Helsinki guidelines. Participants were informed of their right to withdraw from the study at any time without repercussions, and steps were taken to minimize any potential risks or discomfort.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Draper DA, Felland LE, Liebhaber A, Melichar L. The role of nurses in hospital quality improvement. Res Brief. 2008;3:1–8. [PubMed] [Google Scholar]
- 2.Stavropoulou A, Rovithis M, Sigala E, Pantou S, Koukouli S. Greek nurses’ perceptions on empathy and empathic care in the Intensive Care Unit. Intensive Crit Care Nurs. 2020;58:102814. 10.1016/j.iccn.2020.102814 [DOI] [PubMed] [Google Scholar]
- 3.Wu Y. Empathy in nurse-patient interaction: a conversation analysis. BMC Nurs. 2021;20(1):1–6. 10.1186/s12912-021-00535-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev. 2004;3(2):71–100. 10.1177/1534582304267187 [DOI] [PubMed] [Google Scholar]
- 5.Kamas L, Preston A. Empathy, gender, and prosocial behavior. J Behav Exp Econ. 2021;92:101654. 10.1016/j.socec.2020.101654 [DOI] [Google Scholar]
- 6.Pérez-Fuentes MDC, Herrera-Peco I, Molero Jurado MDM, Oropesa Ruiz NF, Ayuso-Murillo D, Gázquez Linares JJ. A cross-sectional study of Empathy and emotion management: key to a work environment for Humanized Care in nursing. Front Psychol. 2020;11:706. 10.3389/fpsyg.2020.00706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159(9):1563–9. 10.1176/appi.ajp.159.9.1563 [DOI] [PubMed] [Google Scholar]
- 8.Dean S, Williams C, Balnaves M. Living dolls and nurses without empathy. J Adv Nurs. 2017;73(4):757–9. 10.1111/jan.12891 [DOI] [PubMed] [Google Scholar]
- 9.Yuguero O, Ramon Marsal J, Esquerda M, Vivanco L, Soler-González J. Association between low empathy and high burnout among primary care physicians and nurses in Lleida, Spain. Eur J Gen Pract. 2017;23(1):4–10. 10.1080/13814788.2016.1233173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97. 10.1056/NEJMra050100 [DOI] [PubMed] [Google Scholar]
- 11.Byrd J, Knowles H, Moore S, Acker V, Bell S, Alanis N, et al. Synergistic effects of emergency physician empathy and burnout on patient satisfaction: a prospective observational study. Emerg Med J. 2021;38(4):290–6. 10.1136/emermed-2019-209393 [DOI] [PubMed] [Google Scholar]
- 12.Mirzaei Maghsud A, Abazari F, Miri S, Sadat Nematollahi M. The effectiveness of empathy training on the empathy skills of nurses working in intensive care units. J Res Nurs. 2020;25(8):722–31. 10.1177/1744987120902827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van der Graaff J, Carlo G, Crocetti E, Koot HM, Branje S. Prosocial behavior in adolescence: gender differences in development and links with empathy. J Youth Adolesc. 2018;47(5):1086–99. 10.1007/s10964-017-0786-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mikulincer M, Shaver PR, Gillath O, Nitzberg RA. Attachment, caregiving, and altruism: boosting attachment security increases compassion and helping. J Pers Soc Psychol. 2005;89(5):817–39. 10.1037/0022-3514.89.5.817 [DOI] [PubMed] [Google Scholar]
- 15.Bowlby JA, Secure Base. Parent-child attachment and healthy Human Development. New York, NY: Basic Books; 1988. [Google Scholar]
- 16.Coan JA. Toward a neuroscience of attachment. In: Cassidy J, Shaver PR, editors. Handbook of attachment: theory, Research, and clinical applications. New York, NY: Guilford Press; 2008. pp. 241–65. [Google Scholar]
- 17.Fraley RC. Attachment in Adulthood: recent developments, emerging debates, and future directions. Annu Rev Psychol. 2019;70:401–22. 10.1146/annurev-psych-010418-102813 [DOI] [PubMed] [Google Scholar]
- 18.Mikulincer M, Shaver P. Attachment in adulthood: structure, dynamics, and change. New York: Guilford Press; 2007. [Google Scholar]
- 19.Tan A, Zimmermann C, Rodin G. Interpersonal processes in palliative care: an attachment perspective on the patient-clinician relationship. Palliat Med. 2005;19(2):143–50. 10.1191/0269216305pm994oa [DOI] [PubMed] [Google Scholar]
- 20.Cherry MG, Fletcher I, O’Sullivan H. The influence of medical students’ and doctors’ attachment style and emotional intelligence on their patient-provider communication. Patient Educ Couns. 2013;93(2):177–87. 10.1016/j.pec.2013.05.010 [DOI] [PubMed] [Google Scholar]
- 21.Davis MH. Empathy: a social psychological approach. Boulder, CO: Westview; 1996. [Google Scholar]
- 22.Fields SK, Mahan P, Tillman P, Harris J, Maxwell K, Hojat M. Measuring empathy in healthcare profession students using the Jefferson Scale of Physician Empathy: health provider–student version. J Interprof Care. 2011;25(4):287–93. 10.3109/13561820.2011.566648 [DOI] [PubMed] [Google Scholar]
- 23.Dozier M, Cue KL, Barnett L. Clinicians as caregivers: role of attachment organization in treatment. J Consult Clin Psychol. 1994;62(4):793–800. 10.1037/0022-006X.62.4.793 [DOI] [PubMed] [Google Scholar]
- 24.Georgi E, Petermann F, Schipper M. Are empathic abilities learnable? Implications for social neuroscientific research from psychometric assessments. Soc Neurosci. 2014;9(1):74–81. 10.1080/17470919.2013.855253 [DOI] [PubMed] [Google Scholar]
- 25.Daniel SI. Adult attachment patterns and individual psychotherapy: a review. Clin Psychol Rev. 2006;26(8):968–84. 10.1016/j.cpr.2006.02.001 [DOI] [PubMed] [Google Scholar]
- 26.Pepping CA, Davis PJ, O’Donovan A, Pal J. Individual differences in Self-Compassion: the role of attachment and experiences of parenting in Childhood. Self Identity. 2015;14(1):104–17. 10.1080/15298868.2014.955050 [DOI] [Google Scholar]
- 27.Neff KD. Self-compassion: the proven power of being kind to yourself. New York: William Morrow; 2011. [Google Scholar]
- 28.Játiva R, Cerezo MA. The mediating role of self-compassion in the relationship between victimization and psychological maladjustment in a sample of adolescents. Child Abuse Negl. 2014;38(7):1180–90. 10.1016/j.chiabu.2014.04.005 [DOI] [PubMed] [Google Scholar]
- 29.Neff KD. Self-Compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity. 2003;2(2):85–101. 10.1080/15298860309032 [DOI] [Google Scholar]
- 30.Galante J, Galante I, Bekkers MJ, Gallacher J. Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. J Consult Clin Psychol. 2014;82(6):1101–14. 10.1037/a0037249 [DOI] [PubMed] [Google Scholar]
- 31.Neff KD, Vonk R. Self-compassion versus global self-esteem: two different ways of relating to oneself. J Pers. 2009;77(1):23–50. 10.1111/j.1467-6494.2008.00537.x [DOI] [PubMed] [Google Scholar]
- 32.Leary MR, Tate EB, Adams CE, Allen AB, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. 2007;92(5):887–904. 10.1037/0022-3514.92.5.887 [DOI] [PubMed] [Google Scholar]
- 33.Neff KD, Pommier E. The relationship between self-compassion and other-focused concern among College undergraduates, Community adults, and practicing meditators. Self Identity. 2013;12(2):160–76. 10.1080/15298868.2011.649546 [DOI] [Google Scholar]
- 34.Upton KV. An investigation into compassion fatigue and self-compassion in acute medical care hospital nurses: a mixed methods study. J Compassionate Health Care. 2018;5(1):1–27. 10.1186/s40639-018-0050-x [DOI] [Google Scholar]
- 35.Ferrari M, Hunt C, Harrysunker A, Abbott MJ, Beath AP, Einstein DA. Self-compassion interventions and psychosocial outcomes: a meta-analysis of RCTs. Mindfulness. 2019;10:1455–73. 10.1007/s12671-019-01134-6 [DOI] [Google Scholar]
- 36.Wiklund Gustin L, Wagner L. The butterfly effect of caring - clinical nursing teachers’ understanding of self-compassion as a source to compassionate care. Scand J Caring Sci. 2013;27(1):175–83. 10.1111/j.1471-6712.2012.01033.x [DOI] [PubMed] [Google Scholar]
- 37.Mikulincer M, Gillath O, Halevy V, Avihou N, Avidan S, Eshkoli N. Attachment theory and reactions to others’ needs:’ evidence that activation of the sense of attachment security promotes empathic responses. J Pers Soc Psychol. 2001;81(6):1205–24. 10.1037/0022-3514.81.6.1205 [DOI] [PubMed] [Google Scholar]
- 38.Kline RB. Principles and practice of structural equation modeling. 4th ed. New York: Guilford Press; 2015. [Google Scholar]
- 39.Weston R, Gore PA. A brief guide to structural equation modeling. J Couns Psychol. 2006;34(5):719–51. 10.1177/0011000006286345 [DOI] [Google Scholar]
- 40.Neff KD. The Development and Validation of a scale to measure Self-Compassion. Self Identity. 2003;2(3):223–50. 10.1080/15298860309027 [DOI] [Google Scholar]
- 41.MacBeth A, Gumley A. Exploring compassion: a meta-analysis of the association between self-compassion and psychopathology. Clin Psychol Rev. 2012;32(6):545–52. 10.1016/j.cpr.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 42.Momeni F, Shahidi S, Mootabi F, Heydari M. Psychometric properties of a Farsi version of the Self-Compassion Scale (SCS). J Contemp Psychol. 2014;8(2):27–40. [Google Scholar]
- 43.Khosravani S, sadeghi M, Yabandeh M. Psychometric properties of Self-Compassion Scale(SCS). Psychol Methods Models. 2013;4(13):47–59. [Google Scholar]
- 44.Hazan C, Shaver PR. Romantic love conceptualized as an attachment process. J Pers Soc Psychol. 1987;52:511–24. 10.1037/0022-3514.52.3.511 [DOI] [PubMed] [Google Scholar]
- 45.Besharat MA. Development and validation of adult attachment inventory. Procedia Soc Behav Sci. 2011;30:475–9. 10.1016/j.sbspro.2011.10.093 [DOI] [Google Scholar]
- 46.Besharat MA, Naghshineh N, Ganji P, Tavalaeyan F. The moderating role of attachment styles on the relationship of alexithymia and fear of intimacy with marital satisfaction. Int J Psychol Stud. 2014;6(3):106–17. 10.5539/ijps.v6n3p106 [DOI] [Google Scholar]
- 47.Karimi FZ, Zarifnejad G, Abdolahi M, Taghipour A. Surveying the factor structure and reliability of the Persian version of the Jefferson scale of physician empathy-health care provider student version (JSE-HPS). Hayat. 2015;21(3):5–14. [Google Scholar]
- 48.Hashempor M, Karami M. Validity and reliability of the Persian version of JSPE-HP questionnaire (Jefferson scale of physician empathy-health professionals version). J Kerman Univ Med Sci. 2012;19(2):201–11. [Google Scholar]
- 49.Heffernan M, Quinn Griffin MT, Sister Rita M, Fitzpatrick JJ. Self-compassion and emotional intelligence in nurses. Int J Nurs Pract. 2010;16(4):366–73. 10.1111/j.1440-172X.2010.01853.x [DOI] [PubMed] [Google Scholar]
- 50.Tahir Raza Z. Self-compassion, empathy and helping attitudes in employees. University Lahore; 2021.
- 51.Wiseman T. Toward a holistic conceptualization of empathy for nursing practice. ANS Adv Nurs Sci. 2007;30(3):E61–72. 10.1097/01.ANS.0000286630.00011.e3 [DOI] [PubMed] [Google Scholar]
- 52.Gleichgerrcht E, Decety J. The relationship between different facets of empathy, pain perception and compassion fatigue among physicians. Front Behav Neurosci. 2014;8:243. 10.3389/fnbeh.2014.00243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ardenghi S, Rampoldi G, Bani M, Strepparava MG. Attachment styles as predictors of self-reported empathy in medical students during pre-clinical years. Patient Educ Couns. 2020;103(5):965–70. 10.1016/j.pec.2019.11.004 [DOI] [PubMed] [Google Scholar]
- 54.Williams B, Brown T, McKenna L, Beovich B, Etherington J. Attachment and empathy in Australian undergraduate paramedic, nursing and occupational therapy students: a cross-sectional study. Collegian. 2017;24(6):603–9. 10.1016/j.colegn.2016.11.004 [DOI] [Google Scholar]
- 55.Ayuso-Murillo D, Colomer-Sánchez A, Santiago-Magdalena CR, Lendínez-Mesa A, Gracia EB, López-Peláez A, Herrera-Peco I. Effect of anxiety on Empathy: an observational study among nurses. Healthc (Basel). 2020;8(2):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Franczak K. Attachment styles and the ways of coping with stress in Polish nurses. Adv Palliat Med. 2012;11(2):62–73. [Google Scholar]
- 57.Homan KJ. Secure attachment and eudaimonic well-being in late adulthood: the mediating role of self-compassion. Aging Ment Health. 2018;22(3):363–70. 10.1080/13607863.2016.1254597 [DOI] [PubMed] [Google Scholar]
- 58.Joeng JR, Turner SL, Kim EY, Choi SA, Lee YJ, Kim JK. Insecure attachment and emotional distress: fear of self-compassion and self-compassion as mediators. Pers Individ Dif. 2017;112:6–11. 10.1016/j.paid.2017.02.048 [DOI] [Google Scholar]
- 59.Raque-Bogdan TL, Ericson SK, Jackson J, Martin HM, Bryan NA. Attachment and mental and physical health: self-compassion and mattering as mediators. J Couns Psychol. 2011;58(2):272–8. 10.1037/a0023041 [DOI] [PubMed] [Google Scholar]
- 60.Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013;69(1):28–44. 10.1002/jclp.21923 [DOI] [PubMed] [Google Scholar]
- 61.Homan KJ, Sirois F. Self-compassion and physical health: exploring the roles of perceived stress and health-promoting behaviors. Health Psychol Open. 2017;4. [DOI] [PMC free article] [PubMed]
- 62.Hatami Varzaneh A, Fathi E, Khanipour H, Habibi N. Predicting helping attitude based on attachment styles, empathy, and self-compassion among volunteer and non-volunteer groups of public participation during COVID-19 outbreak. J Res Psychol Health. 2020;14(1):87–101. [Google Scholar]
- 63.Wei M, Liao KY, Ku TY, Shaffer PA. Attachment, self-compassion, empathy, and subjective well-being among college students and community adults. J Pers. 2011;79(1):191–221. 10.1111/j.1467-6494.2010.00677.x [DOI] [PubMed] [Google Scholar]
- 64.Tiwari GK, Pandey R, Rai PK, Pandey R, Verma Y, Parihar P, et al. Self-compassion as an intrapersonal resource of perceived positive mental health outcomes: a thematic analysis. Ment Health Relig Cult. 2020;23(7):550–69. 10.1080/13674676.2020.1774524 [DOI] [Google Scholar]
- 65.Neff KD, McGehee P. Self-compassion and psychological resilience among adolescents and young adults. Self Identity. 2010;9(3):225–40. 10.1080/15298860902979307 [DOI] [Google Scholar]
- 66.Shaver PR, Hazan C. Adult romantic attachment: theory and evidence. Adv Pers Relat. 1993;4:29–70. [Google Scholar]
- 67.Florian V, Mikulincer M. Symbolic immortality and the management of the terror of death: the moderating role of attachment style. J Pers Soc Psychol. 1998;74(3):725–34. 10.1037/0022-3514.74.3.725 [DOI] [PubMed] [Google Scholar]
- 68.Murphy TP, Laible DJ, Augustine M, Robeson L. Attachment’s links with adolescents’ social emotions: the roles of negative emotionality and emotion regulation. J Genet Psychol. 2015;176(5):315–29. 10.1080/00221325.2015.1072082 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.