Abstract
Purpose
Although experimental psychopathology using PET, EEG, and fMRI is at the forefront of understanding the underlying mechanisms of sleep inertia, many questions concerning causality remain unanswerable due to ethical constraints and the use of small and heterogeneous samples in experimental methods. There is a pressing need for a novel perspective in a large and relatively homogeneous population to fully capture and elucidate longitudinal processes and dynamic causality that culminate in episodes of sleep inertia over time. Therefore, this study aimed to reveal the causal relationships between symptoms of sleep inertia across its distinct patterns.
Patients and Methods
A total of 1636 intern nurses participated in the first survey (94.1% validity rate), then 1277 intern nurses were followed up (82.9% tracing rate). Symptoms of sleep inertia were self-reported using the Sleep Inertia Questionnaire. The cross-lagged panel network models were used to examine unique longitudinal relationships between symptoms of sleep inertia across distinct trajectories.
Results
Four distinct trajectories of sleep inertia were established. Additionally, we found differences in those symptoms with the highest influence on other symptoms at the subsequent point across the networks of four trajectories, particularly, “Difficulty in concentrating” in the persistent-high group and “Feeling tense” in the deteriorating groups.
Conclusion
The current study highlights changes in sleep inertia based on the long-term course over time. Notably, symptoms of “Difficulty in concentrating” and “Feeling tense” are imperative to address these specific symptoms within subpopulations.
Keywords: sleep inertia, change patterns, network structures, intern nurse, shift work
Introduction
Sleep inertia, characterized by temporarily degraded vigilance, impaired neurobehavioral cognitive performance, worsened mood, and sleepiness, is the unavoidable transitional state from sleep to wakefulness.1–3 Individuals with sleep inertia while performing safety-critical tasks are at greater risk of performance errors or accidents, posing threats to the safety of themselves and those around them.1,4,5 For example, on May 29, 2010, the 3252gt Norwegian-registered platform supply vessel (Skandi Foula) made heavy contact with the moored Panamanian-registered supply vessel (OMS Resolution) in Victoria Dock, Aberdeen.4 Analysis of the chief officer’s hours of rest suggested that he was suffering from sleep inertia at the time of the accident, which may have impaired his ability to control Skandi Foula effectively.4 Furthermore, the prevalence rates of severe sleep inertia increased from 2.9% in 2000 to 15.2% in 2014 among the general population.6,7 Notably, a sample of 92 employed and volunteer Australian emergency service personnel completed an online survey to determine whether sleep inertia is perceived as a concern among emergency service personnel.8 Results found that 25% of shift workers reported that, despite having the opportunity to nap or rest while on shift, they chose not to nap to avoid sleep inertia.8 Given the increasing prevalence of severe sleep inertia and the extensive demands of 24/7 service, it is essential to deepen our understanding of sleep inertia to minimize its potential risks for emergency service personnel.
Decades of research using PET, EEG, and/or fMRI have investigated the neurophysiological mechanisms of sleep inertia.9–13 To illustrate, a simultaneous EEG-fMRI study has revealed that sleep-like features such as slow EEG power and reduced BOLD activity persist during sleep inertia.9 Vallat et al found that awakening in deep sleep is characterized by a global loss of brain functional segregation between task-negative (default mode) and task-positive (dorsal attention, salience, sensorimotor) networks.10 Although experimental psychopathology using PET, EEG, and fMRI is at the forefront of understanding the underlying mechanisms of sleep inertia, many questions concerning causality remain unanswerable due to ethical constraints and the use of small and heterogeneous samples in experimental methods. Notably, as a complement to experimental approaches, network analysis aims to clarify the causal processes among symptoms that culminate in episodes of psychological phenomena or disease using data from large-scale self-report surveys.14,15
Recently, the network analysis based on network theory has emerged as an alternative framework for conceptualizing mental disorders and psychological phenomena.16,17 Network theory posits that symptoms of psychopathology are causally connected through various biological, psychological, and societal mechanisms. When these causal associations are sufficiently strong, symptoms may generate feedback loops that sustain themselves.17 While undirected networks with cross-sectional data have involved correlational analyses,15 the cross-lagged panel network (CLPN) could illuminate longitudinal processes and dynamic causality occurring within and across constructs over time.18,19 This approach is well-suitable for elucidating the causal associations between symptoms proposed by the network theory.18,20 Network parameters, such as edges and thresholds, are statistical representations of psychological and biological processes, derived from material referents in the real world.14 In brief, network analysis could identify connections that appear consistently across many people, which may provide some leverage for thinking about innovative prevention strategies in the real word.14
In summary, by using longitudinal data, we would like to employ CLPN to uncover the temporal and causal relationships between symptoms of sleep inertia. Notably, several studies have highlighted significant individual differences in people’s responses and adaptation processes to sleep inertia,2,8,21,22 indicating that there may be distinct change patterns of sleep inertia over time. Therefore, the current study aimed to deepen our understanding of sleep inertia across these varied change patterns.
Materials and Methods
Participants
Participants were recruited from a nursing school in Huizhou, China. The sample size was calculated according to established formula:23
 |
In the above formula, p, d, and Z1-α/2 represents the expected minimum rate by a previous study,6 allowable error, and statistic for significance test.23 Specifically, p = 0.152, q = 1 – p = 1–0.152 = 0.848, d = 0.2p = 0.2 * 0.152 = 0.0304, Z1-α/2 = 1.96. According to this formula, the minimum required sample size for this study is 536 people. To accommodate potential missed responses, refusals, and dropout risks during a longitudinal study, the sample size was adjusted to a ratio of 1:2.
This study included two surveys: the first survey (Time 1, T1) was conducted half a month after their clinical internship from June 28 to July 5, 2022) and the second wave (Time 2, T2) occurred three and a half months later from October 11 to 31, 2022. In the first survey, 1636 intern nurses participated, with 1540 providing valid questionnaires (94.1% validity rate). For the second survey, 1277 intern nurses were followed up (82.9% tracing rate), and, 1156 successfully completed all measurements. After excluding 77 individuals with day work, the current study included 1079 intern nurses with shift work.
Procedure
An electronic invitation letter including a QR code for the questionnaire, was initially sent to the target population via their teachers. The participants volunteered to complete the online questionnaires via their phones or computers with the assistance of trained staff from the nursing school. All participants were free to withdraw from the study at any time. If they feel uncomfortable during or after participating in this study, they could get psychological counseling services from South China Normal University (SCNU) according to the contact information we provided. We assessed various variables in both surveys, including demographic characteristics, willingness to continue working as a nurse, circadian rhythm, sleep inertia, sleep problems, and emotional problems. Electronic informed consent was obtained from all participants or their guardians (if necessary) before starting this survey. Our study was approved by the Human Research Ethics Committees of SCNU and carried out in line with the Helsinki Declaration as revised in 1989.
Measures
The subjective sleep inertia over the past week was assessed by the Chinese version of the Sleep Inertia Questionnaire (SIQ) in both surveys.24 Previous studies demonstrated that the SIQ has robust reliability and validity among different populations.24,25 Each item of the SIQ is rated on a 5-point Likert scale (1 = Not at all, 2 = A little, 3 = Somewhat, 4 = Often, 5 = All the time). With a total of 21 items, the SIQ yields scores ranging from 21 to 105, where higher scores indicate more severe sleep inertia. The cut-off score of 69 indicates severe sleep inertia in the current sample. Another study, currently under review in the Journal of Sleep Research, offers a more detailed analysis of the cut-off score of 69 used to classify severe sleep inertia among intern nurses. The Cronbach’s α for the SIQ in this study were 0.95 at T1 and 0.96 at T2, respectively.
Sex, subjective sleep quality at T1, and sleep duration at T1 were evaluated separately using single items. The morningness–eveningness type was determined at T2 through the Chinese version of the 5-item Morningness/Eveningness Questionnaire (MEQ-5).26 The two dimensions (flexibility and languid) of the Chinese Version of the Circadian Type Inventory (CTI) were used to measure the flexibility of the rhythm (items 1–6) and the ability to overcome drowsy (items 7–11), respectively.27
Statistical Analyses
Change Patterns of Sleep Inertia
The change patterns of sleep inertia were disentangled based on the following two steps. Firstly, participants were classified into non- or severe sleep inertia with a cut-off value of 69 at T1 and T2, respectively. Second, the change patterns of sleep inertia from T1 to T2 after their clinical internship were revealed according to the methodology of previous research.28,29 We further summarized four patterns of sleep inertia: persistent-low, alleviating, deteriorating, and persistent-high. More specifically, individuals in the persistent-high group showed severe sleep inertia at both time points. Intern nurses who reported no severe sleep inertia at T1 but symptoms at T2 were assigned to the deteriorating group. Participants with severe sleep inertia at T1 but without symptoms at T2 were included in the alleviating group. For the persistent-low group, severe sleep inertia was absent at both time points.
The Cross-Lagged Panel Network Models
The CLPN models were constructed using a series of regularized regression models to estimate both the autoregressive and cross-lagged coefficients. The autoregressive coefficients depict a variable’s influence on itself at the subsequent measurement after controlling for covariates, while the cross-lagged coefficients illustrate the influence of one variable on another variable at the subsequent measurement.19 Demographic and sleep-related factors (see Supplementary Table 1) were incorporated as covariates in all CLPN models, as recommended by Funkhouser et al.18 All models were estimated using the R-package glmnet, and all network graphs were visualized using the Fruchterman-Reingold algorithm in R-package qgraph. In a network graph, nodes represent the symptoms, edges depict the relationships between two symptoms, and the thickness of the edges represents the strength of associations between symptoms.30
Centrality indices, namely the in-expected influence (in-EI) and out-expected influence (out-EI), were computed using the R-package qgraph.30 The in-EI quantifies the proportion of variance for a given variable at follow-up that is accounted for by nodes at baseline, whereas the out-EI signifies the effect a given node at baseline has on nodes at follow-up.18,31,32 As in previous studies,33,34 the threshold for identifying key symptoms was set at in-EI > 1 and out-EI > 1.
The bootstrapping function in the R-package boonet was utilized to evaluate the accuracy and stability of all networks.35 First, we employed nonparametric bootstrapping to examine the edge-weight accuracy and the significance between edge-weights, with 95% confidence intervals (CIs) based on 1000 bootstrap iterations. Then, we calculated the correlation stability coefficient (CS-C) using the case-dropping bootstrap procedure. The CS-C quantifies the maximum proportion of cases that can be dropped while maintaining a correlation above 0.7 between the centrality indices of the sample with and without dropouts with 95% possibility. The CS-C values ≥0.25 were considered acceptable, whereas CS-C values ≥0.50 were regarded as good.
Results
Change Patterns of Sleep Inertia
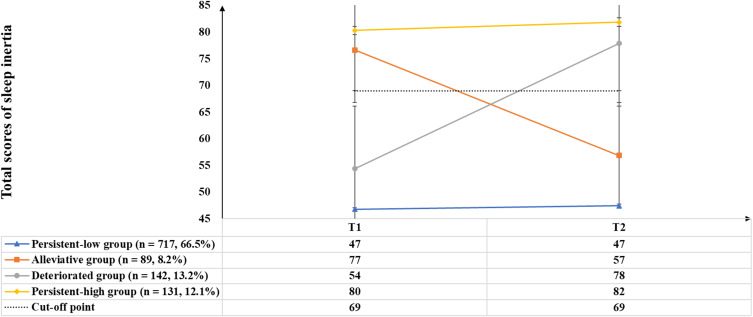
As shown in Figure 1, four distinct patterns of sleep inertia were established: persistent-low group, alleviating group, deteriorating group, and persistent-high group. The persistent-low group, characterized by SIQ total scores below the cut-off value of 69 at both T1 and T2, comprised 717 (66.5%) participants. The alleviating group (n = 89, 8.2%) was characterized by SIQ scores being equal or above the cut-off value at T1 but below at T2; while the deteriorating group (n = 142, 13.2%) was characterized by SIQ scores being below the cut-off value at T1 but equal or above at T2. Additionally, the persistent-high group comprised 131 participants (12.1%) who had SIQ scores equal or above the cut-off value at two waves. More detailed information on the four patterns of sleep inertia is shown in Table 1.
Figure 1.
The four SI’s trajectories from half a month to three and half months after their clinical internship among 1079 intern nurses.
Abbreviations: SI, sleep inertia; T1, Time 1; T2, time 2.
Table 1.
Differences on Demographic and Sleep-Related Factors Between the Four Change Patterns of Sleep Inertia
| Variable | n | % | Persistent-Low Group (n = 717) | Alleviative Group (n = 89) | Deteriorated Group (n = 142) | Persistent-High Group (n = 131) | χ2 | η2 |
|---|---|---|---|---|---|---|---|---|
| Sexa | 0.433 | 0.013 | ||||||
| 60 | 5.6 | 42 | 4 | 7 | 7 | |||
| 1019 | 94.4 | 675 | 85 | 135 | 124 | |||
| Morningness–eveningness typeb | 101.812*** | 0.292 | ||||||
| 99 | 9.2 | 85 | 8 | 5 | 1 | |||
| 702 | 65.1 | 509 | 44 | 86 | 63 | |||
| 278 | 25.8 | 123 | 37 | 51 | 67 | |||
| Flexibility of the rhythmb | 17.567** | 0.102 | ||||||
| 238 | 22.1 | 153 | 19 | 27 | 39 | |||
| 593 | 55.0 | 379 | 49 | 94 | 71 | |||
| 248 | 23.0 | 185 | 21 | 21 | 21 | |||
| Ability to overcome drowsyb | 213.291*** | 0.436 | ||||||
| 230 | 21.3 | 201 | 13 | 8 | 8 | |||
| 582 | 53.9 | 420 | 55 | 68 | 39 | |||
| 267 | 24.7 | 96 | 21 | 66 | 84 | |||
| Subjective sleep qualitya | 105.677*** | 0.271 | ||||||
| 498 | 46.2 | 389 | 22 | 59 | 28 | |||
| 501 | 46.4 | 305 | 50 | 68 | 78 | |||
| 80 | 7.4 | 23 | 17 | 15 | 25 | |||
| Sleep durationa | 66.732*** | 0.224 | ||||||
| 47 | 4.4 | 33 | 4 | 7 | 3 | |||
| 707 | 65.5 | 520 | 44 | 86 | 57 | |||
| 325 | 30.1 | 164 | 41 | 49 | 71 |
Notes: aVariables were assessed at T1; bVariables were assessed at T2. **p < 0.01, ***p < 0.001.
Temporal Networks Across Four Distinct Change Patterns of Sleep Inertia
Network Structure
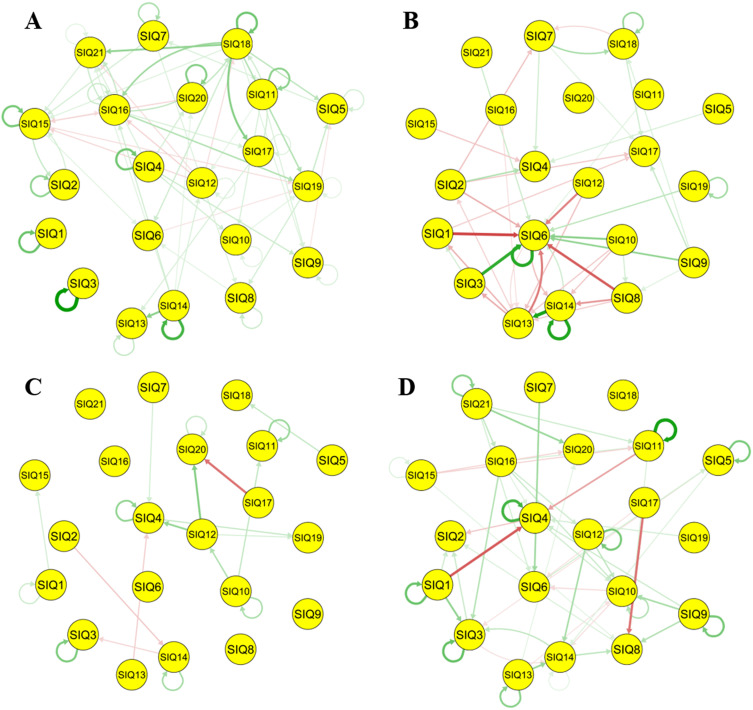
The CLPN network structures of four distinct change patterns of sleep inertia are depicted in Figure 2. Overall, the persistent-low group exhibited the highest number of estimated edges (n = 181), followed by the persistent-high (n = 94), alleviating (n = 62), and deteriorating (n = 40) groups. As shown in Table 2, all estimated edges and autoregressive edges showed no significant differences among four networks, while the cross-lagged edges were significantly different (F = 3.121, p < 0.05, η2 = 0.028). Furthermore, we applied the Bonferroni correction to adjust the significance levels for multiple comparisons. The results found a significant difference in the cross-lagged edges between the persistent-low and alleviating groups (Difference of mean = 0.03, p < 0.05). Notably, the strongest cross-lagged edges were observed: “React more slowly (SIQ18) - Think more slowly (SIQ17)” in the persistent-low group (edge-weighted value =0.20), “Dread starting your day (SIQ14) - Anxious about the upcoming day (SIQ13)” in the alleviating group (edge-weighted value =0.38), “Feeling tense (SIQ12) - Resist to wake up (SIQ20)” in the deteriorating group (edge-weighted value =0.20), and “Difficulty in getting up (SIQ1) - Hit the snooze button on the alarm (SIQ3)” in the persistent-high group (edge-weighted value =0.19). More detailed information for edge-weighted values can be found in Supplementary Tables 1–4.
Figure 2.
Cross-lagged panel networks across four distinct SI’s trajectories. A threshold of all edge weights was manually set to 0.05 to make the figures more interpretable.
Notes: Each curved arrow “loop” reflects an autoregressive association; White nodes indicate depressive symptoms; Blue lines indicate positive relations, whereas red lines signal negative relations, and line thickness and boldness reflect the strength of associations. (A) Persistent-low group; (B) Alleviative group; (C) Deteriorated group; (D) Persistent-high group; SIQ, Sleep Inertia Questionnaire; SIQ1, Difficulty in getting up; SIQ2, Need an alarm to wake up; SIQ3, Hit the snooze button on the alarm; SIQ4, Bump into and drop things; SIQ5, Move more slowly; SIQ6, Feel sleepy; SIQ7, Heavy, sore, or itchy eyes; SIQ8, Tired or heavy arms and/or legs; SIQ9, Groggy, fuzzy or hazy mind; SIQ10, Get winded more easily; SIQ11, Difficulty in keeping balance; SIQ12, Feel tense; SIQ13, Anxious about the upcoming day; SIQ14, Dread starting your day; SIQ15, Wish to sleep more; SIQ16, Difficulty in concentrating; SIQ17, Think more slowly; SIQ18, React more slowly; SIQ19, Make more mistakes/errors; SIQ20, Resist to wake up; SIQ21, Difficulty in getting your thoughts together.
Table 2.
Comparison on Edge Weights and Centrality Indicators in Four Networks of Distinct Change Patterns of Sleep Inertia
| Persistent-Low Group (n = 717) | Alleviative Group (n = 89) | Deteriorated Group (n = 142) | Persistent-High Group (n = 131) | F | η2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| M±SD | N | M±SD | N | M±SD | N | M±SD | N | |||
| Edge weights | ||||||||||
| All estimated edges | 0.04±0.07 | 181 | 0.01±0.14 | 62 | 0.04±0.09 | 40 | 0.05±0.10 | 94 | 2.503 | 0.02 |
| All autoregressive edges | 0.15±0.10 | 21 | 0.26±0.12 | 4 | 0.15±0.04 | 7 | 0.20±0.10 | 13 | 1.929 | 0.124 |
| All cross-lagged edges | 0.03±0.05 | 160 | −0.01±0.13 | 58 | 0.02±0.08 | 33 | 0.03±0.08 | 81 | 3.121* | 0.028 |
| Centrality indicators | ||||||||||
| In-EI | 0.20±0.11 | 0.02±0.12 | 0.03±0.08 | 0.11±0.13 | 15.973*** | 0.375 | ||||
| Out-EI | 0.20±0.30 | 0.02±0.30 | 0.03±0.14 | 0.11±0.20 | 3.382* | 0.113 | ||||
Note: *p < 0.05, ***p < 0.001.
Abbreviations: M, mean; SD, standard deviation; in-EI, in expected influence; out-EI, out expected influence.
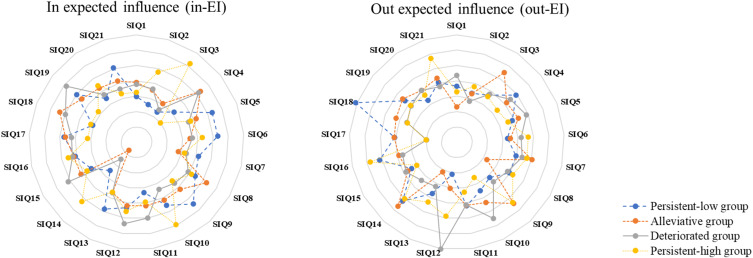
Network Inference
More specifically, symptoms with the high out-EI in the persistent-high group included “Difficulty in concentrating” (SIQ16; out-EI = 1.80), “Difficulty in getting your thoughts together” (SIQ21; out-EI = 1.71), and “Groggy fuzzy or hazy mind” (SIQ9; out-EI = 1.34); while symptoms in the deteriorating groups were “Feeling tense” (SIQ12; out-EI = 3.02) and “Get winded more easily” (SIQ10; out-EI = 1.49). Figure 3 shows further details regarding the standardized values of in-EI and out-EI. Table 3 provides the results of multiple comparisons using the Bonferroni correction between in EI and out EI.
Figure 3.
Centrality estimates of in-EI (Left) and out-EI (Right) using z values between four distinct SI’s trajectories.
Notes: Higher values indicate more centrality. SIQ, Sleep Inertia Questionnaire; SIQ1, Difficulty in getting up; SIQ2, Need an alarm to wake up; SIQ3, Hit the snooze button on the alarm; SIQ4, Bump into and drop things; SIQ5, Move more slowly; SIQ6, Feel sleepy; SIQ7, Heavy, sore, or itchy eyes; SIQ8, Tired or heavy arms and/or legs; SIQ9, Groggy, fuzzy or hazy mind; SIQ10, Get winded more easily; SIQ11, Difficulty in keeping balance; SIQ12, Feel tense; SIQ13, Anxious about the upcoming day; SIQ14, Dread starting your day; SIQ15, Wish to sleep more; SIQ16, Difficulty in concentrating; SIQ17, Think more slowly; SIQ18, React more slowly; SIQ19, Make more mistakes/errors; SIQ20, Resist to wake up; SIQ21, Difficulty in getting your thoughts together.
Table 3.
The Results of Multiple Comparisons Using the Bonferroni Correction Between in EI and Out EI
| Group (I) | Group (J) | Mean(I) - Mean(J) | p | 95% CI | |
|---|---|---|---|---|---|
| In-EI | Persistent-low | Alleviative | 0.22* | <0.001 | [0.13, 0.32] |
| Deteriorated | 0.17* | <0.001 | [0.08, 0.27] | ||
| Persistent-high | 0.10* | 0.042 | [0.00, 0.19] | ||
| Alleviative | Persistent-low | −0.22* | <0.001 | [−0.32, −0.13] | |
| Deteriorated | −0.05 | 0.940 | [−0.14, 0.04] | ||
| Persistent-high | −0.13* | 0.002 | [−0.22, −0.03] | ||
| Deteriorated | Persistent-low | −0.17* | <0.001 | [−0.27, −0.08] | |
| Alleviative | 0.05 | 0.940 | [−0.04, 0.14] | ||
| Persistent-high | −0.08 | 0.153 | [−0.17, 0.01] | ||
| Persistent-high | Persistent-low | −0.10* | 0.042 | [−0.19, 0.00] | |
| Alleviative | 0.13* | 0.002 | [0.03, 0.22] | ||
| Deteriorated | 0.08 | 0.153 | [−0.01, 0.17] | ||
| Out-EI | Persistent-low | Alleviative | 0.22* | 0.023 | [0.02, 0.43] |
| Deteriorated | 0.17 | 0.137 | [−0.03, 0.38] | ||
| Persistent-high | 0.10 | 1.000 | [−0.11, 0.30] | ||
| Alleviative | Persistent-low | −0.22* | 0.023 | [−0.43, −0.02] | |
| Deteriorated | −0.05 | 1.000 | [−0.25, 0.15] | ||
| Persistent-high | −0.13 | 0.555 | [−0.33, 0.08] | ||
| Deteriorated | Persistent-low | −0.17 | 0.137 | [−0.38, 0.03] | |
| Alleviative | 0.05 | 1.000 | [−0.15, 0.25] | ||
| Persistent-high | −0.08 | 1.000 | [−0.28, 0.12] | ||
| Persistent-high | Persistent-low | −0.10 | 1.000 | [−0.30, 0.11] | |
| Alleviative | 0.13 | 0.555 | [−0.08, 0.33] | ||
| Deteriorated | 0.08 | 1.000 | [−0.12, 0.28] |
Note: *p < 0.05.
Abbreviation: 95% CI, 95% confidence interval.
Network Stability and Accuracy
The bootstrapped 95% CIs tests indicated that 95% CIs of all edges were small to moderate (Supplementary Figure 1). Statistical significance was observed in the results of the bootstrap difference test for edges and centrality indicators Supplementary Figures 2–4 Stability analyses for in-EI and out-EI centrality suggested partial stability (Supplementary Figure 5). Specifically, in-EI centrality is 0.51 in the persistent-low group, 0.11 in the alleviating group, 0.11 in the deteriorating group, and 0.05 in the persistent-high group, and out-EI centrality is 0.34 in the persistent-low group, 0.07 in the alleviating group, 0.18 in the deteriorating group, and 0.15 in the persistent-high group.
Discussion
To the best of our knowledge, this study is the first to uncover temporal networks of sleep inertia across its distinct change patterns using longitudinal data. We have two main findings in this study. On the one hand, we established four distinct patterns of sleep inertia. On the other hand, we found differences in those symptoms with the highest influence on other symptoms at the subsequent point across the networks of four change patterns. Particularly, “Difficulty in concentrating” in the persistent-high group and “Feeling tense” in the deteriorating groups should be prioritized for attention in interventions targeting sleep inertia.
In the current study, we established four change patterns for long-term sleep inertia among intern nurses with shift work: persistent-low (66.5%), alleviating (8.2%), deteriorating (13.2%), and persistent-high (12.1%) groups. This finding is partially consistent with our prior investigation,21 indicating distinct latent profiles of sleep inertia among Chinese college students. Additionally, according to previous research regarding change patterns in sleep-related problems,28,29,36 we could postulate that sleep inertia has large individual differences in people’s responses and adaptation processes to shift work. Several plausible explanations can elucidate this finding. First, sleep inertia, as the third process of sleep regulation, reflects the interplay between a homeostatic drive or pressure for sleep and a circadian rhythm of arousal.37 Given that shift work has a profound impact on the pressure for sleep over time,38 sleep inertia might consequently display a different pattern in the long-term period. Second, people perceive the world differently, leading to individual differences in vulnerability to sleep inertia.39 Further studies are needed to validate the specific explanations mentioned above.
Our findings suggest that central symptoms with the highest out-EI values vary across the four heterogeneous networks of sleep inertia. Due to the lack of network analysis results for sleep inertia subgroups, there is no reference basis for the current findings. However, previous network analysis studies on subgroups of depression or posttraumatic stress symptoms have shown that the key symptoms across subgroups are different.20,32,33 These studies can partially support the current finding. Taken together, sleep inertia exhibits significant individual differences, highlighting the importance of future research to further explore its long-term heterogeneity.
Evidence has suggested that symptoms with the highest out-EI play a role in the onset or development of psychological symptoms.15,40 Given the availability and effectiveness of clinical interventions,15,29,40 priority should be given to focusing on those symptoms with the highest out-EI in the deteriorating d and persistent-high groups. More specifically, our study reveals firstly that “Difficulty in concentrating” exhibited the greatest influence on other symptoms within the network with the persistent-high sleep inertia among intern nurses with shift work. Several experimental studies provide partial support for significant impairment of vigilance due to sleep inertia.41–44 For example, Santhi et al found that alertness was most strongly affected by sleep inertia followed by other cognitive functions.44 Notably, shift work involves exposure to light and eating during the biological night while sleeping during the biological day, causing misalignment with the endogenous circadian system,45 which may contribute to persistent-high sleep inertia. Alertness has emerged as a fundamental and crucial component of human performance in many work environments.46 Consequently, the aforementioned evidence helps explain why “Difficulty in concentrating” could strongly predict other symptoms three and a half months after the clinical internship among intern nurses with shift work. A recent study indicated that mindfulness-based interventions can help individuals feel less stressed improve their ability to concentrate.47 Therefore, these interventions should be employed to enhance concentration in individuals experiencing persistent high sleep inertia.
Furthermore, “Feeling tense” exhibited the most significant influence on other symptoms within the network characterized by deteriorating sleep inertia. Similar to our previous published study,48 “Dread starting your day” emerged as a central symptom within the cross-sectional network of sleep inertia among Chinese college students. These findings indicate that negative effects such as irritability and anxiety tend to manifest during the sleep-wake transitional state sleep inertia.25,48,49 It is noteworthy that the desire to return to sleep is one of the characteristics of sleep inertia,3 potentially indicating that individuals with more severe sleep inertia might endure insufficient sleep. Sleep loss is closely associated with worsened mood and decreased ability to regulate negative emotions, even exhibiting somatic symptoms.50 Further, nurses with shift work report frequently poorer sleep quality and reduced sleep duration, which could impact an individual’s positive effects.45 Therefore, we thought that “Feeling tense” may activate and maintain other symptoms within the network with the deteriorating sleep inertia among intern nurses with shift work. According previous studies,47,51 techniques such as deep breathing exercises, progressive muscle relaxation, and mindfulness meditation have been shown to reduce anxiety and tension. Therefore, these techniques can be beneficial for individuals experiencing worsening sleep inertia.
Notably, this study made a unique contribution to the underlying mechanisms of sleep inertia at the symptom level across distinct change patterns over time. However, it is crucial to acknowledge several limitations. First, the sample only consisted of intern nurses with shift work, potentially limiting the generalizability of findings to other populations such as firefighters, police officers, or pilots due to sex, workplace stability, anticipating a stressful task, frequency of on call.8,52 Second, the reliance on subjective self-reports of sleep inertia may introduce potential biases into our findings. Therefore, future studies need reliable and objective measures (eg, psychomotor vigilance task) to measure sleep inertia. The emergency services sectors can prioritize The possible reason is that the temporal nature of symptoms remains unresolved, which is a crucial consideration when selecting a sampling scheme for within-subject studies14 (ie, How many time points per day or week should be planned?). Fourth, we considered only a limited range of variables and omitted other important information, such as details about the clinical internship and the participants’ shift work schedules (ie, nights per week, rotation direction/speed, days off, or work days). Fifth, similar to previous studies,53–55 categorizing individuals into groups based on whether they have a disease or not will inevitably lead to an imbalance in the number of people in each group. Finally, due to the low stability and accuracy of the estimated network for the three small sample groups, the results should be interpreted with caution. Future research should prioritize expanding the sample size to validate the these results.
Conclusions
The current study highlights changes in sleep inertia based on the long-term course over time. Notably, symptoms of “Difficulty in concentrating” in the persistent-high group and “Feeling tense” in the deteriorating groups were most predictive of other symptoms at follow-up. Taken together, it is imperative to address these specific symptoms within subpopulations.
Acknowledgments
We thank all the participants of the study.
Funding Statement
This work was supported by the National Natural Science Foundation of China (Grant No.31871129, 32271135), Natural Science Foundation of Guangdong Province, China (Grant No. 2023A1515012200), Young Talent Support Project of Guangzhou Association for Science and Technology (Grant No. QT-2023-025), and the 2023 Young Teacher Research and Training Fund Project of South China Normal University: Humanities and Social Sciences (23SK16).
Data Sharing Statement
The data that support the findings in the current study are available from the corresponding author upon reasonable request.
Ethics Approval
Our study was approved by the Human Research Ethics Committees of SCNU and carried out in line with the Helsinki Declaration as revised in 1989.
Disclosure
The authors report no other conflicts of interest in this work.
References
- 1.Kovac K, Vincent GE, Paterson JL, Hilditch CJ, Ferguson SA. A preliminary framework for managing sleep inertia in occupational settings. Sleep Adv. 2023;2023:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hilditch CJ, Pradhan S, Costedoat G, et al. Sex differences in perceptions of sleep inertia following nighttime awakenings. Sleep Adv. 2022;2022:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trotti LM. Waking up is the hardest thing I do all day: sleep inertia and sleep drunkenness. Sleep Med Rev. 2017;35:76–84. doi: 10.1016/j.smrv.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Branch MAI. Heavy Contact by Skandi Foula with OMS Resolution, Aberdeen Harbour 29 May 2010. London: UK Department for Transport; 2011. [Google Scholar]
- 5.Armentrout JJ, Holland DA, O’Toole KJ, Ercoline WR. Fatigue and related human factors in the near crash of a large military aircraft. Aviat Space Environ Med. 2006;77:963–970. [PubMed] [Google Scholar]
- 6.Ohayon MM, Mahowald MW, Leger D. Are confusional arousals pathological? Neurology. 2014;83:834–841. doi: 10.1212/WNL.0000000000000727 [DOI] [PubMed] [Google Scholar]
- 7.Ohayon MM, Priest RG, Zulley J, Smirne S. The place of confusional arousals in sleep and mental disorders: findings in a general population sample of 13,057 subjects. J Nerv Ment Dis. 2000;188:340–348. doi: 10.1097/00005053-200006000-00004 [DOI] [PubMed] [Google Scholar]
- 8.Kovac K, Vincent GE, Paterson JL, Ferguson SA. “I want to be safe and not still half asleep”: exploring practical countermeasures to manage the risk of sleep inertia for emergency service personnel using a mixed methods approach. Nat Sci Sleep. 2022;14:1493–1510. doi: 10.2147/NSS.S370488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen X, Hsu C-F, Xu D, Yu J, Lei X. Loss of frontal regulator of vigilance during sleep inertia: a simultaneous EEG-fMRI study. Hum Brain Mapp. 2020;41:4288–4298. doi: 10.1002/hbm.25125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vallat R, Meunier D, Nicolas A, Ruby P. Hard to wake up? The cerebral correlates of sleep inertia assessed using combined behavioral, EEG and fMRI measures. NeuroImage. 2019;184:266–278. doi: 10.1016/j.neuroimage.2018.09.033 [DOI] [PubMed] [Google Scholar]
- 11.Gorgoni M, Ferrara M, D’Atri A, et al. EEG topography during sleep inertia upon awakening after a period of increased homeostatic sleep pressure. Sleep Med. 2015;16:883–890. doi: 10.1016/j.sleep.2015.03.009 [DOI] [PubMed] [Google Scholar]
- 12.Marzano C, Ferrara M, Moroni F, De Gennaro L. Electroencephalographic sleep inertia of the awakening brain. Neuroscience. 2011;176:308–317. doi: 10.1016/j.neuroscience.2010.12.014 [DOI] [PubMed] [Google Scholar]
- 13.Balkin TJ, Braun AR, Wesensten NJ, et al. The process of awakening: a PET study of regional brain activity patterns mediating the re-establishment of alertness and consciousness. Brain. 2002;125:2308–2319. doi: 10.1093/brain/awf228 [DOI] [PubMed] [Google Scholar]
- 14.Fried EI, Cramer AOJ. Moving forward: challenges and directions for psychopathological network theory and methodology. Perspect Psychol Sci. 2017;12:999–1020. doi: 10.1177/1745691617705892 [DOI] [PubMed] [Google Scholar]
- 15.McNally RJ. Can network analysis transform psychopathology? Behav Res Ther. 2016;86:95–104. doi: 10.1016/j.brat.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 16.Haslbeck JMB, Waldorp LJ. How well do network models predict observations? On the importance of predictability in network models. Behav Res Methods. 2018;50:853–861. doi: 10.3758/s13428-017-0910-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16:5–13. doi: 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Funkhouser CJ, Chacko AA, Correa KA, Kaiser AJE, Shankman SA. Unique longitudinal relationships between symptoms of psychopathology in youth: a cross‐lagged panel network analysis in the ABCD study. J Child Psychol Psyc. 2021;62:184–194. doi: 10.1111/jcpp.13256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rhemtulla M, Bork RV, Cramer AOJ. Cross-lagged network models. Multivar Behav Res. 2017;2017:1. [Google Scholar]
- 20.Ma Z, Wang D, Fu X, et al. Prospective network of post-traumatic stress disorder (PTSD) symptoms across adolescent survivors with distinct trajectories of PTSD: a cohort study of the Wenchuan earthquake. J Anxiety Disord. 2023;99:102767. doi: 10.1016/j.janxdis.2023.102767 [DOI] [PubMed] [Google Scholar]
- 21.Ma Z, Chen XY, Wang D, et al. Who is the hardest to wake up from sleep? An investigation of self‐reported sleep inertia using a latent profile analysis. J Sleep Res. 2022;31. doi: 10.1111/jsr.13552 [DOI] [PubMed] [Google Scholar]
- 22.Lundholm KR, Honn KA, Skeiky L, Muck RA, Van Dongen HPA. Trait interindividual differences in the magnitude of subjective sleepiness from sleep inertia. Clocks Sleep. 2021;3:298–311. doi: 10.3390/clockssleep3020019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Serdar CC, Cihan M, Yücel D, Serdar MA. Sample size, power and effect size revisited: simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem Med. 2021;31:010502. doi: 10.11613/BM.2021.010502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma Z, Wang D, Zhu Z, et al. Reliability and validity of the Chinese vision of sleep inertia questionnaire. Chinese J Clin Psychol. 2023;31(1):102–106. [Google Scholar]
- 25.Kanady JC, Harvey AG. Development and validation of the sleep inertia questionnaire (SIQ) and assessment of sleep inertia in analogue and clinical depression. Cognitive Ther Res. 2015;39:601–612. doi: 10.1007/s10608-015-9686-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei-Xia L, Aizezi M, XZ-TLW-hZ B. Validity and reliability of the Chinese version of Morningness/Eveningness Questionnaire-5 items (MEQ-5) in students of technical schools. Chinese Ment Heal J. 2016;30:406–412. [Google Scholar]
- 27.H-y Q, X-l S, Li L, Yang L, Fan F. Reliability and validity of the Chinese version of circadian type inventory in nurses on shifts. Chinese J Clin Psychol. 2019;27:258–262. [Google Scholar]
- 28.Chen XY, Shi X, Zhou Y, et al. Change patterns of sleep problems predict mental health problems among adolescents: a 10-year cohort study of Chinese Wenchuan earthquake. J Affect Disord. 2021;287:138–144. doi: 10.1016/j.jad.2021.02.080 [DOI] [PubMed] [Google Scholar]
- 29.Wang D, Zhao J, Zhai S, et al. Longitudinal trajectories of insomnia symptoms among college students during the COVID-19 lockdown in China. J Psychosom Res. 2022;157:110795. doi: 10.1016/j.jpsychores.2022.110795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.qgraph. Network visualizations of relationships in psychometric data [computer program]; 2012.
- 31.Savelieva K, Komulainen K, Elovainio M, Jokela M. Longitudinal associations between specific symptoms of depression: network analysis in a prospective cohort study. J Affect Disord. 2021;278:99–106. doi: 10.1016/j.jad.2020.09.024 [DOI] [PubMed] [Google Scholar]
- 32.Rubin M, Bicki A, Papini S, Smits JAJ, Telch MJ, Gray JS. Distinct trajectories of depression symptoms in early and middle adolescence: preliminary evidence from longitudinal network analysis. J Psychiatr Res. 2021;142:198–203. doi: 10.1016/j.jpsychires.2021.07.053 [DOI] [PubMed] [Google Scholar]
- 33.Ma Z, Zhao J, Chen H, Tao Y, Zhang Y, Fan F. Temporal network of depressive symptoms across college students with distinct depressive trajectories during the COVID-19 pandemic. Depress Anxiety. 2023;2023:1–11. doi: 10.1155/2023/8469620 [DOI] [Google Scholar]
- 34.Sánchez Hernández MO, Carrasco MA, Holgado-Tello FP. Anxiety and depression symptoms in Spanish children and adolescents: an exploration of comorbidity from the network perspective. Child Psychiat Hum D. 2021;2021:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper [computer program]. Version 2017/03/28; 2018. [DOI] [PMC free article] [PubMed]
- 36.Tomfohr LM, Buliga E, Letourneau NL, Campbell TS, Giesbrecht GF. Trajectories of sleep quality and associations with mood during the perinatal period. Sleep. 2015;38(8):1237–1245. doi: 10.5665/sleep.4900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hilditch CJ, McHill AW. Sleep inertia: current insights. Nat Sci Sleep. 2019;11:155–165. doi: 10.2147/NSS.S188911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. BMJ. 2016;355:i5210. doi: 10.1136/bmj.i5210 [DOI] [PubMed] [Google Scholar]
- 39.Saksvik IB, Bjorvatn B, Hetland H, Sandal GM, Pallesen S. Individual differences in tolerance to shift work--a systematic review. Sleep Med Rev. 2011;15:221–235. doi: 10.1016/j.smrv.2010.07.002 [DOI] [PubMed] [Google Scholar]
- 40.Liang Y, Yang L, Xi J, Liu Z. The unique role of sleep problems among symptoms of posttraumatic stress disorder: a cross-lagged panel network analysis. Acta Psychologica Sinica. 2022;54:1206. doi: 10.3724/SP.J.1041.2022.01206 [DOI] [Google Scholar]
- 41.Hilditch CJ, Dorrian J, Centofanti SA, Van Dongen HP, Banks S. Sleep inertia associated with a 10-min nap before the commute home following a night shift: a laboratory simulation study. Accident Anal Prev. 2017;99:411–415. doi: 10.1016/j.aap.2015.11.010 [DOI] [PubMed] [Google Scholar]
- 42.Mulrine HM, Signal TL, van den Berg MJ, Gander PH. Post-sleep inertia performance benefits of longer naps in simulated nightwork and extended operations. Chronobiol Int. 2012;29:1249–1257. doi: 10.3109/07420528.2012.719957 [DOI] [PubMed] [Google Scholar]
- 43.Kubo T, Takahashi M, Takeyama H, et al. How do the timing and length of a night-shift nap affect sleep inertia? Chronobiol Int. 2010;27:1031–1044. doi: 10.3109/07420528.2010.489502 [DOI] [PubMed] [Google Scholar]
- 44.Santhi N, Groeger JA, Archer SN, Gimenez M, Schlangen LJ, Dijk DJ. Morning sleep inertia in alertness and performance: effect of cognitive domain and white light conditions. PLoS One. 2013;8:e79688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Querstret D, O’Brien K, Skene DJ, Maben J. Improving fatigue risk management in healthcare: a scoping review of sleep-related/ fatigue-management interventions for nurses and midwives (reprint). Int J Nurs Stud. 2020;112:103745. doi: 10.1016/j.ijnurstu.2020.103745 [DOI] [PubMed] [Google Scholar]
- 46.Warm JS, Parasuraman R, Matthews G. Vigilance requires hard mental work and is stressful. Hum Fac Ergon Soc. 2008;50:433–441. doi: 10.1518/001872008X312152 [DOI] [PubMed] [Google Scholar]
- 47.Simpson S, Mercer S, Simpson R, Lawrence M, Wyke S. Mindfulness-based interventions for young offenders: a scoping review. Mindfulness. 2018;9:1330–1343. doi: 10.1007/s12671-018-0892-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ma Z, Tao Y, Chen H, et al. An exploration of self-reported sleep inertia symptoms using network analysis. Nat Sci Sleep. 2022;14:661–674. doi: 10.2147/NSS.S347419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hou Y, Huangfu E, Zhang L, Miao D. Changes in cognition and mood due to sleep inertia after 30-hour sleep deprivation. Int J Ment Health. 2007;4:1–11. [Google Scholar]
- 50.Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. J Child Psychol Psyc. 2014;55:180–190. doi: 10.1111/jcpp.12125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsitsi T, Charalambous A, Papastavrou E, Raftopoulos V. Effectiveness of a relaxation intervention (progressive muscle relaxation and guided imagery techniques) to reduce anxiety and improve mood of parents of hospitalized children with malignancies: a randomized controlled trial in Republic of Cyprus and Greece. Eur J Oncol Nurs. 2017;26:9–18. doi: 10.1016/j.ejon.2016.10.007 [DOI] [PubMed] [Google Scholar]
- 52.Kovac K, Vincent GE, Jay SM, et al. The impact of anticipating a stressful task on sleep inertia when on-call. Appl Ergon. 2020;82:102942. doi: 10.1016/j.apergo.2019.102942 [DOI] [PubMed] [Google Scholar]
- 53.Wang D, Zhao J, Ross B, et al. Longitudinal trajectories of depression and anxiety among adolescents during COVID-19 lockdown in China. J Affect Disord. 2022;299:628–635. doi: 10.1016/j.jad.2021.12.086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen XY, Zhou Y, Shi X, Ma Z, Fan F. Longitudinal associations between adolescents’ trajectory membership of depressive symptoms and suicidality in young adulthood: a 10-year cohort of Chinese Wenchuan earthquake survivors. Epidemiol Psychiatr Sci. 2020;29:e175. doi: 10.1017/S2045796020000827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fan F, Long K, Zhou Y, Zheng Y, Liu X. Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychol Med. 2015;45:2885–2896. doi: 10.1017/S0033291715000884 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings in the current study are available from the corresponding author upon reasonable request.