Abstract
Background:
Dimensional frameworks of psychopathology call for multivariate approaches to map co-occurring disorders to index what symptoms emerge when and for whom. Ecological momentary assessment (EMA) offers a method for assessing and differentiating the dynamics of co-occurring symptoms with greater temporal granularity and naturalistic context. The present study used multivariate mixed effects location-scale modeling to characterize the time-varying dynamics of depressed mood and anxiety for women diagnosed with social anxiety disorder (SAD) and major depression (MDD).
Methods:
Women completed five daily EMA surveys over 30 days (150 EMA surveys/woman, T ≈ 5,250 total observations) and two clinical diagnostic and retrospective self-report measures administered approximately two months apart.
Results:
There was evidence of same-symptom lagged effects (bs = .08-.09), but not cross-symptom lagged effects (bs < .01) during EMA. Symptoms co-varied such that momentary spikes from one’s typical level of anxiety were associated with increases in momentary depressed mood (b = .19) and greater variability of depressed mood (b = .06). Similarly, spikes from one’s typical levels of depressed mood were associated with increases in momentary anxiety (b = .19). Furthermore, the presence and magnitude of effects demonstrated person-specific heterogeneity.
Limitations:
Our findings are constrained to the dynamics of depressed and anxious mood among cisgender women with primary SAD and current or past MDD.
Conclusions:
Findings from this work help to characterize how daily experiences of co-occurring mood and anxiety fluctuate and offer insight to aid the development of momentary, person-specific interventions designed to regulate symptom fluctuations.
Keywords: Internalizing, HiTOP, affective dynamics, ecological momentary assessment, heterogeneity
Increasing scientific investment in theoretical models of psychopathology can more thoroughly characterize why and how psychological disorders co-occur (see Hierarchical Topographical Organization of Psychopathology, HiTOP; Kotov et al., 2017). For example, social anxiety disorder (SAD) and major depressive disorder (MDD) are two of the most commonly reported adult psychiatric disorders (Kessler et al., 2005) and women are at increased risk for developing both disorders (Breslau et al., 1995; Kessler et al., 2012). Results from longitudinal research suggest that SAD often precedes the onset of MDD (Kessler et al., 1999; Parker et al., 1999). Furthermore, individuals who go on to develop MDD experience more frequent and more severe episodes of depression (Kessler et al., 1999; Stein et al., 2001) and women are at increased risk for negative consequences resulting from internalizing symptoms (Foster et al., 2015, 2016; Miranda-Mendizabal et al., 2019).
SAD and MDD have traditionally been conceptualized separately (Abramson et al., 1989; Heimberg et al., 2014). Transdiagnostic frameworks (e.g., HiTOP, Kotov et al., 2017) help explain the high co-occurrence rates between single disorders by classifying DSM-5 psychiatric disorders into different spectra, unified by shared cognitive, affective, and behavioral processes. Within the ‘internalizing’ spectra, SAD and MDD are disorders consisting of symptoms characterized by fear and distress (Kotov et al., 2017). Overlap in symptoms and co-occurrence of disorders within the broader internalizing spectra may signal meaningful links in underlying etiology and maintenance processes that undermines the distinctiveness and relevance of DSM-5 diagnostic categories. Consequently, characterizing covariation among symptoms improves our understanding of how disorders within the internalizing spectra are maintained.
Transdiagnostic frameworks of psychopathology reflect an important shift in efforts to model why certain disorders co-vary. However, the HiTOP framework remain largely focused on modeling trait-level (i.e., singular metric, static in time) vulnerabilities with limited examination of state-level relationships between momentary experiences of internalizing symptoms. Intensive longitudinal methods (e.g., ecological momentary assessment; EMA) can be used to examine how co-occurring SAD and MDD symptoms fluctuate with closer proximity to the time-scale with which they are experienced and regulated. Thus, modeling the dynamics of co-occurring symptoms can strengthen characterization of transdiagnostic processes. Analyses of real-time (i.e., dynamic) data can demonstrate the degree to which symptoms predict themselves over time (i.e., inertia) or exhibit instability over time (e.g., momentary deviations from one’s typical level of a given symptom) (Jahng et al., 2008). Results from dynamic models can characterize how symptoms within a given disorder are maintained over time (e.g., how depressed mood maintains itself), as well as how symptoms across disorders co-occur or are co-maintained over time (e.g., how depressed mood maintains anxiety). Overall, collecting and analyzing EMA data can strengthen the current HiTOP framework by providing evidence of within-disorder patterns, as well as cross-disorder patterns that result from naturalistic interactions between co-occurring symptoms in everyday life.
Methods for measuring and analyzing symptom dynamics also align with measurement-based care initiatives that call for repeated symptom monitoring to increase standards of care (e.g., within national healthcare systems; Lemke et al., 2017) and can inform the design of momentary interventions for co-occurring symptoms. For example, charting symptom dynamics for a client with SAD-MDD may help guide a therapist to use behavioral activation to help disrupt inertia in their client’s mood, behavioral exposure to reduce instability in their client’s anxiety, or emotion regulation skills to reduce covariation in depressed mood and anxiety over time. Furthermore, symptom dynamics may offer predictive utility for identifying risk for future psychopathology. For example, some research has demonstrated that inertia (i.e., stability) of depressed mood predicts future depression (Elmer et al., 2020), even after accounting for depressogenic factors and baseline depression (Koval et al., 2012; Kuppens et al., 2012). Preliminary evidence has demonstrated that changes in emotional inertia may also precede relapse into major depressive episodes (Tonge et al., 2024; van de Leemput et al., 2014a; Wichers & Groot, 2016). Finally, a recent study examining symptom dynamics during psychotherapy demonstrated that greater symptom variability was associated with reduced treatment gains (Brose et al., 2024).
In this study, we aimed to test how hallmark affective symptoms of MDD and SAD (i.e., ‘depressed mood’ and ‘anxiety’) fluctuated in association with one another. We hypothesized that there would be meaningful variation within disorder (i.e., levels of anxiety varying over time) and across disorders (i.e., levels of anxiety at one timepoint varying with levels of depression). Additionally, we hypothesized that there would be significant individual-level variation in symptom dynamics given previous work demonstrating person-specific heterogeneity within internalizing symptoms (Piccirillo & Rodebaugh, 2022) and affect (Bosley & Fisher, 2020; Foster & Beltz, 2021). Finally, we aimed to further characterize the nature of SAD and MDD symptom (co-) variation by examining the extent to which between-person differences in symptoms assessed using retrospective symptom self-report are associated with within-person differences in momentary symptom co-variation. Results test the potential clinical utility of using within-person dynamic metrics to identify individuals with greater clinical severity or more stable symptom patterns over time.
To test these aims, we constructed two multivariate mixed-effects location-scale models (MELSM; see Table 1). MELSM is a statistical approach that allows researchers to simultaneously estimate predictors of the momentary ratings of a symptom for a given person in an average moment (i.e., location), as well as the average degree of variability of a given symptom from one moment to the next (i.e., scale) releasing assumptions regarding homogeneity in variance (Hedeker et al., 2008). We also extracted personalized estimates of SAD and MDD dynamic indices and examined the association with traditional, retrospective, self-report measures of SAD and MDD symptoms assessed at baseline, as well as pre-/post- change (i.e., before and after dynamic assessment). Taken together, results characterize how daily experiences of co-occurring mood and anxiety fluctuate and offer insight to aid the development of momentary, person-specific interventions designed to regulate symptom fluctuations.
Table 1.
Description of model parameters for Model 1 and Model 2
| Depressed mood | |||
|---|---|---|---|
|
| |||
| Model 1a | Model 1b | ||
|
| |||
| Location parameter | M (SD) [90% CI] | Scale parameter | M (SD) [90% CI] |
|
| |||
| Fixed effects estimates | |||
|
| |||
| β0 | Level of depressed mood at the start of EMA on average for the sample, accounting for one’s average level of co-occurring anxiety | η0 | Degree of variability of depressed mood at the start of EMA on average for the sample, accounting for one’s average level of co-occurring anxiety |
| β1 Dayij | Linear effect of time (i.e., day) on level of depressed mood on average | η1 Dayij | Linear effect of time (i.e., day) on degree of variability of depressed mood |
| β2 Surveyij | Linear effect of time (i.e., survey) of depressed mood on average | η2 Surveyij | Linear effect of time (i.e., survey) on degree of variability of depressed mood |
| β3 DownLag1,ij | Effect of depressed mood at the previous timepoint on levels of future depressed mood | η3 DownLag1,ij | Effect of depressed mood at the previous timepoint on degree of variability of future depressed mood |
| β4 AnxietyLag1,ij | Effect of anxiety at the previous timepoint on levels of future depressed mood | η4 AnxietyLag1,ij | Effect of anxiety at the previous timepoint on degree of variability of depressed mood |
| β5 Anxietyi | Effect of an individual’s average level of anxiety on levels of depressed mood | η5 Anxietyi | Effect of an individual’s average level of anxiety on degree of variability of depressed mood |
| β6 Anxietyij | Effect of an individual’s momentary deviations of anxiety on levels of depressed mood | η6 Anxietyij | Effect of an individual’s momentary deviations of anxiety on degree of variability of depressed mood |
|
| |||
| Anxiety | |||
|
| |||
| Model 2a | Model 2b | ||
|
| |||
| Location parameter | M (SD) [90% CI] | Scale parameter | M (SD) [90% CI] |
|
| |||
| Fixed effects estimates | |||
|
| |||
| β0 | Level of anxiety at the start of EMA on average for the sample, accounting for one’s average level of co-occurring depressed mood | η0 | Degree of variability of anxiety at the start of EMA on average for the sample, accounting for one’s average level of co-occurring depressed mood |
| β1 Dayij | Linear effect of time (i.e., day) on level of anxiety on average | η1 Dayij | Linear effect of time (i.e., day) on degree of variability of anxiety |
| β2 Surveyij | Linear effect of time (i.e., survey) on level of anxiety on average | η2 Surveyij | Linear effect of time (i.e., survey) on degree of variability of anxiety |
| β3 DownLag1,ij | Effect of depressed mood at the previous timepoint on levels of future anxiety | η3 DownLag1,ij | Effect of depressed mood at the previous timepoint on degree of variability of future anxiety |
| β4 AnxietyLag1,ij | Effect of anxiety at the previous timepoint on levels of future anxiety | η4 AnxietyLag1,ij | Effect of anxiety at the previous timepoint on degree of variability of future anxiety |
| β5 Downi | Effect of an individual’s average level of depressed mood on levels of anxiety | η5 Downi | Effect of an individual’s average level of depressed mood on degree of variability of anxiety |
| β6 Downij | Effect of an individual’s momentary deviations of depressed mood on levels of anxiety | η6 Downij | Effect of an individual’s momentary deviations of depressed mood on degree of variability of anxiety |
Note. Location sub-models estimated predictors of momentary ratings of feeling down or feeling anxious for a given individual in a given moment. Scale sub-models estimated the momentary degree of variability of depressed mood or anxiety for individual in moment. Lagged variables were person-mean-centered (Hamaker et al., 2015) so that a lagged parameter measures the effect of momentary deviations from one’s typical level of that symptom on the level or degree of variability of a given symptom at the next timepoint. Individual-level variation was measured by including random effects around all time-varying effects.
Methods
Participants
Cisgender women (N = 35) diagnosed with SAD and history of MDD completed intensive longitudinal assessments five times a day for approximately 30 days (T = 5,250 observations; Mt = 125 observations). Women were recruited from the university community into a larger study examining cognitive-affective predictors of mood over time (Piccirillo & Rodebaugh, 2022). Our sample size and decision to recruit cisgender women was constrained by resources available, which were insufficient to examine the effects of sex or gender with adequate statistical power. Women mostly identified as White (51.43%); however, 28.57% identified as East Asian, 17.14% identified as Black, and 5.71% identified as Hispanic or Latinx. The average age was 21.37 years (range 18–37 years). Most women (n =19, 54.29%) identified as straight or heterosexual, although 12 women (34.29%) identified as bisexual and four women (11.43%) reported questioning their sexual orientation. A majority of women (n = 28, 80%) reported that English was their native language.
Measures
A structured clinical interview (Mini International Neuropsychiatric Interview 6.0 (MINI; (Lecrubier et al., 1997) was used to assess psychiatric symptoms for SAD and MDD at baseline. MDD was assessed again approximately two months later. Blinded independent assessors rated randomly assigned interviews from the larger study, which included 18 interviews from this sample (51.4%). Inter-rater reliability was assessed for MDD (K = .83) and SAD (K = .73).
Depression, social anxiety, and social avoidance symptoms were assessed at baseline interview prior to starting EMA and approximately one month after completing EMA. Self-reported depressive symptoms during the past two weeks were assessed using the Beck Depression Inventory (BDI-II; (Beck et al., 1996). The BDI-II is a routinely used self-report measure with excellent internal reliability and good validity (Beck et al., 1996). Clinician-rated social anxiety and social avoidance symptoms during the past week were assessed using the Liebowitz Social Anxiety Scale (LSAS; (Liebowitz, 1987). The LSAS is a clinician-rated interview with excellent internal reliability and good validity (Heimberg et al., 1999).
A brief battery of 14 EMA items were created for this study to assess symptoms of MDD and SAD (American Psychiatric Association, 2013) in the present moment. In this study, we analyzed two items that corresponded to hallmark symptoms of MDD (i.e., feeling down) and SAD (i.e., feeling anxious). Notably, we believed that experiences of anxiety were likely to fluctuate every few hours (i.e., similar to depressed mood); whereas fluctuations in ‘social-related anxiety’ were more likely to be influenced by external factors, such as engagement to social interactions or avoidance. Thus, we selected the broader term, ‘anxiety’, instead of ‘social-related anxiety’ to ensure adequate observational power. Items were rated using a scale from 0 (Not at all) to 10 (A lot).
Procedure
Participants completed a brief phone screen to determine preliminary study eligibility, followed by a lab-based diagnostic interview. Women completed five EMA surveys during a self-selected 12-hour time for approximately 30 days. Participants returned to the laboratory for a second diagnostic interview approximately one month after completing EMA (i.e., two months after the baseline interview).
Scientific transparency and openness
The university’s Institutional Review Board approved this research (IRB #201710016, 201712134) and all participants provided informed consent before beginning study procedures. The study methods and measures are described further in previous work (Piccirillo & Rodebaugh, 2022). Hypotheses and analyses presented here were pre-registered (https://osf.io/s8jzb) and analyzed using R, version 4.3.1 (R Core Team, 2023) and packages dplyr (Wickham et al., 2023), brms (Bürkner, 2017), and ggplot (Wickham, 2016). Code is included in the supplementary material. Data are not currently openly available and may be requested by emailing the corresponding author.
Data Analytic Plan
To model the dynamics of depressed mood, anxiety, and their co-occurrence, we constructed two multivariate mixed-effects location-scale models (MELSM) using the terms described in Table 1 and specified further in our pre-registration (https://osf.io/s8jzb). Location and scale sub-models were estimated simultaneously using Stan, a probabilistic programming language accessed through the brms R package (Bürkner, 2017). We measured individual-level variation around the average-level estimate of a given model parameter using random effect terms for all time-varying parameters and further characterized the nature of individual-level variation within model effects using a descriptive approach presented in Williams et al. (2020). Specifically, we calculated personalized estimates for each parameter by adding the predicted random effect for each person (i.e., each person’s predicted deviation from the fixed effect) to the fixed effect estimate for that parameter. We assessed individual-level variation around each fixed effect by counting the number of individuals who demonstrated a personalized estimate with a 90% CI that did not include 0 (suggestive of a non-zero estimate for that parameter) (see Table 3, Figures 1, 2). For example, if the fixed effect for a model parameter was statistically significant but only a few individuals demonstrated personalized estimates that were statistically significant, we concluded that the fixed effect described only a minority of individuals within the group. We also compared the magnitude of personalized estimates to the magnitude of the fixed effect by counting the number of individuals who exhibited a 90% CI around their personalized estimate that did not include the fixed effect estimate. This allowed us to assess the number of individuals who demonstrated an estimate that was significantly stronger or weaker in magnitude compared to the fixed effect (see Table 3, Figures 1, 2).
Table 3.
Examining person-specific heterogeneity within parameter estimates from Models 1 and 2
| Model 1a | Model 1b | ||||
|---|---|---|---|---|---|
|
| |||||
| Location parameter | 90% CI around personalized estimates ∉ FE (n) | 90% CI around personalized estimates ∉ 0 (n) | Scale parameter | 90% CI around personalized estimates ∉ FE (n) | 90% CI around personalized estimates ∉ 0 (n) |
|
| |||||
| Intercept | 0 | 34 | Intercept | 2 | 27 |
| Dayij | 0 | 24 | Dayij | 4 | 4 |
| Surveyij | 0 | 0 | Surveyij | 1 | 2 |
| Lag1, Downij | 6 | 23 | Lag1, Downij | 3 | 8 |
| Lag1, Anxietyij | 0 | 0 | Lag1, Anxietyij | 1 | 1 |
| Anxietyij | 11 | 35 | Anxietyij | 8 | 13 |
|
| |||||
| Model 2a | Model 2b | ||||
|
| |||||
| Location parameter | 90% CI around personalized estimates ∉ FE (n) | 90% CI around personalized estimates ∉ 0 (n) | Scale parameter | 90% CI around personalized estimates ∉ FE (n) | 90% CI around personalized estimates ∉ 0 (n) |
|
| |||||
| Intercept | 0 | 5 | Intercept | 0 | 13 |
| Dayij | 1 | 1 | Dayij | 5 | 6 |
| Surveyij | 0 | 4 | Surveyij | 2 | 2 |
| Lag1, Downij | 0 | 0 | Lag1, Downij | 0 | 0 |
| Lag1, Anxietyij | 1 | 31 | Lag1, Anxietyij | 1 | 1 |
| Downij | 12 | 35 | Downij | 8 | 8 |
Note. FE = Fixed effect; ∉ = does not include; Personalized estimates refers to the predicted personalized estimate (fixed effect + random effect). 90% CI refers to the credible interval (CI) around the posterior distribution. The 90% CI denotes the interval that the associated estimate lies within, with 90% certainty. If the 90% CI does not include 0, the estimate is likely to be non-zero, with 95% certainty. Subscript i refers to a person-mean value; ij refers to a person-mean centered variable.
Figure 1: Modeling personalized estimates for parameters reflecting the dynamics of depressed mood.
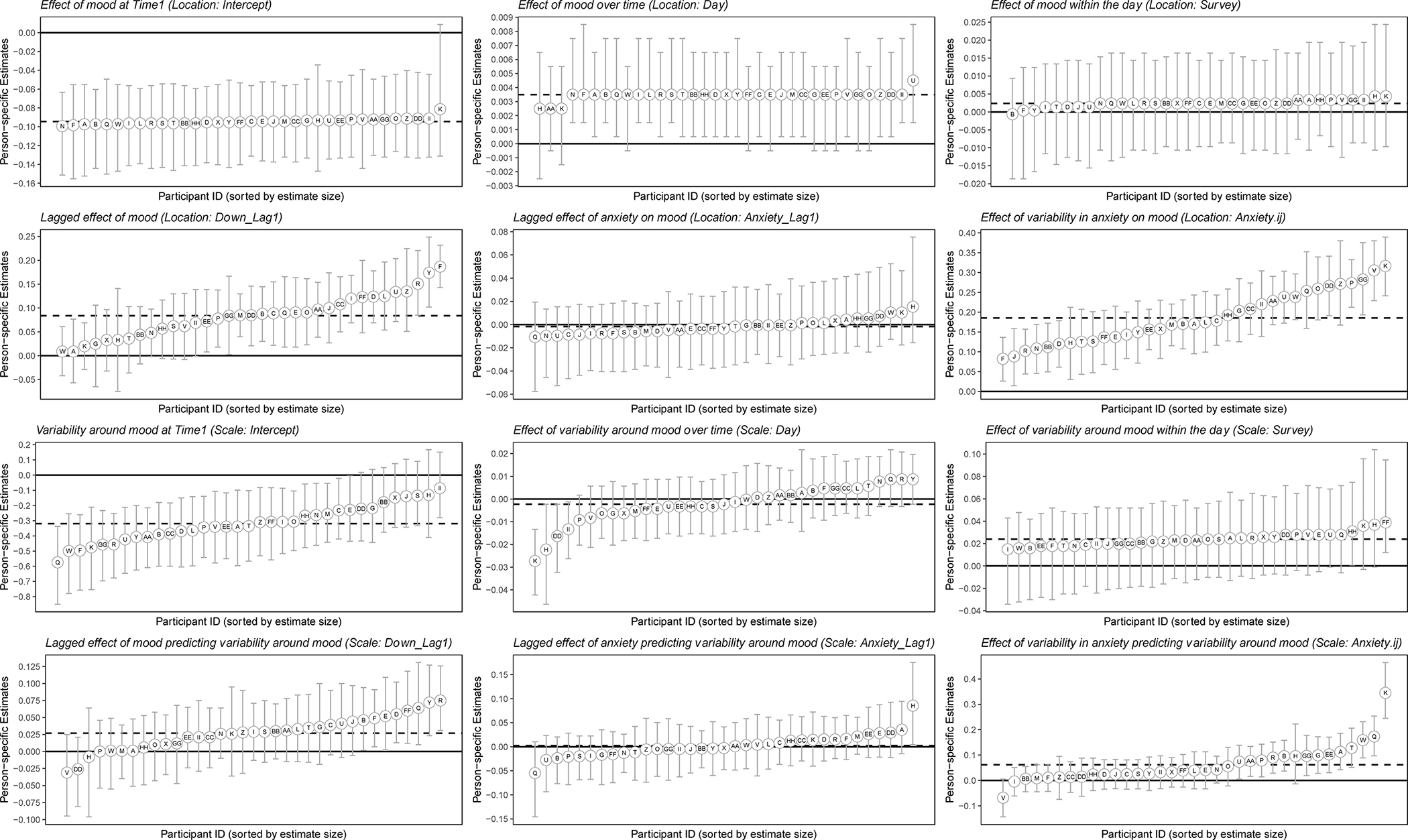
Note. Error bars represent the 90% credible interval around each predicted personalized estimate (fixed effect plus random effect). 90% CI refers to the credible interval (CI) around the posterior distribution. The 90% CI denotes the interval that the associated estimate lies within, with 90% certainty. If the 90% CI does not include 0, the estimate is likely to be non-zero, with 95% certainty. The fixed effect is represented with a hashed line.
Figure 2: Modeling personalized estimates for parameters reflecting the dynamics of anxiety.
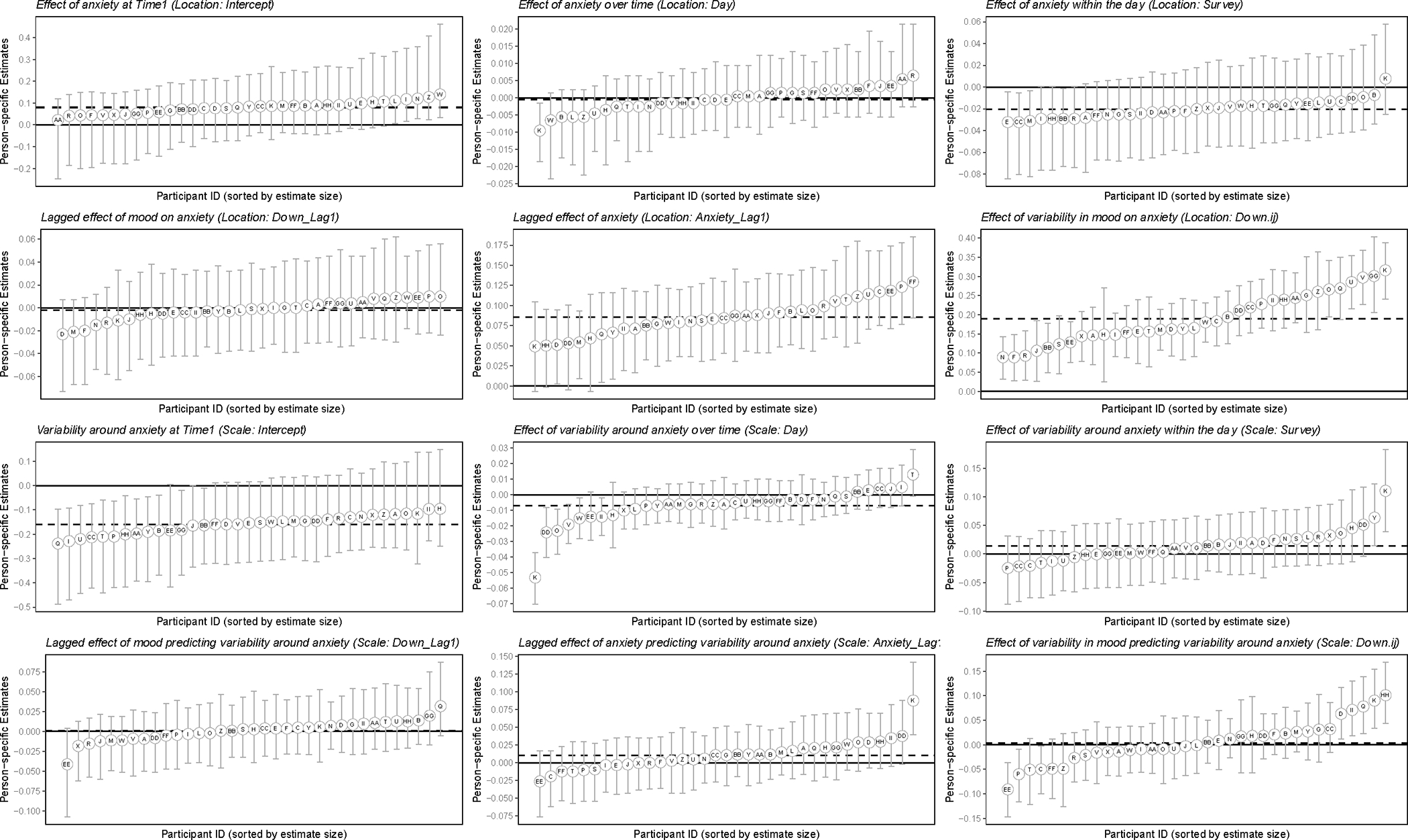
Note. Error bars represent the 90% credible interval around each predicted personalized estimate (fixed effect plus random effect). 90% CI refers to the credible interval (CI) around the posterior distribution. The 90% CI denotes the interval that the associated estimate lies within, with 90% certainty. If the 90% CI does not include 0, the estimate is likely to be non-zero, with 95% certainty. The fixed effect is represented with a hashed line.
MELSM models were fit with non-informative priors that included four chains with at least 1,000 iterations (and an equally sized warm-up period). We evaluated each model for convergence by examining the R-hat metric, which is an estimate of convergence of between- and within-chain estimates for model parameters. We assessed model fit by examining whether each parameter was associated with a R-hat value < 1.01. We also examined whether parameters were associated with bulk and tail effective sample sizes of at least 400 (Gelman, 2006). Bulk and tail effective sample sizes reflect the level of sampling efficiency in the bulk and tails of the distribution, respectively and are used to assess reliability. All parameters exhibited R-hat values of 1.00 and bulk and tail effective sample sizes > 400.1 We examined posterior distributions for each parameter and reported the mean, standard deviation, and a 90% equal tailed credible interval (90% CI), which corresponds to upper and lower bounds at the 5th and 95th percentiles, respectively.
To model the associations between baseline levels of SAD and MDD symptoms and dynamic indices, we calculated the zero-order correlations between personalized estimates and scores from clinical measures of depression, social anxiety, and social avoidance symptoms assessed at baseline (Table 4). We also calculated the zero-order correlations between personalized estimates and change in SAD or MDD symptoms over a 2-month period (i.e., symptom score assessed 1–2 months after ending EMA minus symptom score assessed at baseline) to determine whether symptom dynamics were associated with symptom change over time (Table 4).
Table 4.
Associations (r) between personalized estimates of dynamic features of depressed mood and anxiety and self-reported mood and anxiety symptoms at baseline and follow-up
| Associations at baseline | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Model 1a | Model 1b | |||||
|
| ||||||
| Location parameters | Scale parameters | |||||
|
| ||||||
| BDI-II | LSAS, Anx | LSAS, Avoid | BDI-II | LSAS, Anx | LSAS, Avoid | |
|
| ||||||
| Intercept | −.29 | −.06 | −.03 | −.15 | −.16 | −.15 |
| Dayij | .25 | .20 | .15 | .26 | .17 | .14 |
| Surveyij | −.25 | −.15 | −.06 | .12 | .06 | .05 |
| Lag1, Downij | .47** | .15 | .05 | .24 | .15 | .08 |
| Lag1, Anxietyij | −.20 | −.22 | −.18 | .10 | −.20 | −.32 |
| Anxietyij | −.22 | .12 | .22 | −.29 | .03 | .06 |
| Model 2a | Model 2b | |||||
| Location parameters | Scale parameters | |||||
| BDI-II | LSAS, Anx | LSAS, Avoid | BDI-II | LSAS, Anx | LSAS, Avoid | |
| Intercept | .20 | .22 | .00 | −.16 | −.13 | −.12 |
| Dayij | −.02 | −.24 | .00 | .25 | .13 | .06 |
| Surveyij | −.27 | −.02 | −.09 | −.12 | −.10 | −.09 |
| Lag1, Downij | −.28 | −.15 | .05 | .14 | .36* | .28 |
| Lag1, Anxietyij | −.03 | −.10 | −.11 | −.03 | .16 | .13 |
| Downij | −.18 | .20 | .27 | .13 | .19 | .15 |
|
| ||||||
| Associations at follow-up | ||||||
|
| ||||||
| Model 1a | Model 1b | |||||
|
| ||||||
| Location parameters | Scale parameters | |||||
|
| ||||||
| BDI-II | LSAS, Anx | LSAS, Avoid | BDI-II | LSAS, Anx | LSAS, Avoid | |
|
| ||||||
| Intercept | −.03 | −.32 | −.15 | −.06 | −.02 | −.02 |
| Dayij | −.01 | .03 | −.10 | .06 | .35 | .07 |
| Surveyij | −.04 | −.46** | −.27 | −.23 | −.30 | −.08 |
| Lag1, Downij | −.29 | .08 | .05 | −.17 | .27 | .12 |
| Lag1, Anxietyij | .04 | −.14 | −.04 | −.22 | −.12 | .11 |
| Anxietyij | .13 | −.42* | −.36* | .06 | −.02 | −.01 |
|
| ||||||
| Model 2a | Model 2b | |||||
|
| ||||||
| Location parameters | Scale parameters | |||||
|
| ||||||
| BDI-II | LSAS, Anx | LSAS, Avoid | BDI-II | LSAS, Anx | LSAS, Avoid | |
|
| ||||||
| Intercept | −.01 | .08 | .29 | −.14 | −.01 | .07 |
| Dayij | .02 | .05 | −.26 | −.03 | .33 | .09 |
| Surveyij | −.04 | −.13 | .10 | −.12 | −.09 | .02 |
| Lag1, Downij | .15 | −.17 | −.24 | −.23 | −.23 | −.27 |
| Lag1, Anxietyij | −.04 | .15 | .19 | .07 | −.28 | −.10 |
| Downij | .09 | −.47** | −.43* | −.02 | −.25 | −.19 |
Note. Parameters refer to the predicted personalized estimates (fixed effect + random effect). BDI-II = Score on the Beck Depression Inventory – II; LSAS = Liebowitz Social Anxiety Scale; Anx = Anxiety subscale; Avoid = Avoidance subscale. BDI-II and LSAS were administered at baseline. Follow-up assessments were administered approximately 1–2 months after finishing EMA.
reflects p < .05
reflects p < .001.
Results
On average, participants completed 78.13% of the 150 administered assessments (Mt = 125, Ranget = 59 – 147).
Model 1a. Examining predictors of momentary ratings of depressed mood
Estimates from the model examining predictors of momentary depressed mood are included in Table 1. On average (i.e., across people), depressed mood was relatively stable from one timepoint to the next such that, previous levels of depressed mood predicted future levels of depressed mood. Additionally, momentary spikes in anxiety (i.e., deviations from one’s typical level of anxiety) were associated with higher momentary levels of depressed mood on average.
Model 1b. Examining predictors of momentary variability of depressed mood
A negative intercept was observed, suggesting that – on average and given an individual’s typical level of anxiety – the expected residual degree of variability of depressed mood was lower when starting EMA, and degree of variability significantly increased within the day. Additionally, lagged levels of depressed mood predicted greater degree of variability of future depressed mood. Finally, momentary spikes in anxiety (i.e., deviation from one’s typical levels of anxiety) were associated with greater degree of variability of depressed mood from one time point to the next.
Examination of random effects and individual-level variation across Models 1a, 1b
Some dynamic predictors of depressed mood demonstrated significant individual-level variation (Table 2). We examined individual-level variation further by reviewing the statistical significance and magnitude of personalized estimates (Table 3, Figure 1). We describe heterogeneity in two statistically significant effects from the location sub-model below. First, although depressed mood on average demonstrated significant lagged effects from one timepoint to the next, there were 12 individuals (34.3%) for whom lagged levels of depressed mood were not significant predictors of their future depressed mood. Furthermore, among individuals for whom this effect was statistically significant, there was heterogeneity in the magnitude of personalized effects, such that three individuals (8.6%) demonstrated personalized estimates of lagged mood that were significantly stronger than the fixed effect. Consequently, depressed mood appears to change in an especially predictable manner for three individuals. Secondly, the effect between momentary spikes in anxiety and momentary levels of depressed mood was statistically significant for all individuals in the sample. However, six individuals (17.1%) demonstrated personalized effects that were significantly weaker in magnitude than the fixed effect and five individuals (14.3%) who demonstrated personalized effects that were significantly stronger in magnitude than the fixed effect. These results suggest that co-occurring increases in momentary levels of depressed mood and anxiety appear to be particularly strong for some individuals, but not others.
Table 2.
Modeling dynamic features of depressed mood (Model 1) and anxiety (Model 2)
| Depressed mood | |||
|---|---|---|---|
|
| |||
| Model 1a | Model 1b | ||
|
| |||
| Location parameter | M (SD) [90% CI] | Scale parameter | M (SD) [90% CI] |
|
| |||
| Fixed effects estimates | |||
|
| |||
| β0 | −0.09 (0.06) [−0.21, 0.02] | η0 | −0.32 (0.09) [−0.50, −0.14] |
| β1 Dayij | 0.00 (0.00) [0.00, 0.01] | η1 Dayij | 0.00 (0.00) [−0.01, 0.00] |
| β2 Surveyij | 0.00 (0.01) [−0.01, 0.02] | η2 Surveyij | 0.02 (0.01) [0.01, 0.04] |
| β3 DownLag1,ij | 0.08 (0.01) [0.06, 0.11] | η3 DownLag1,ij | 0.03 (0.01) [0.01, 0.04] |
| β4 AnxietyLag1,ij | 0.00 (0.01) [−0.02, 0.01] | η4 AnxietyLag1,ij | 0.00 (0.01) [−0.02, 0.02] |
| β5 Anxietyi | 0.01 (0.01) [−0.01, 0.03] | η5 Anxietyi | 0.01 (0.02) [−0.02, 0.05] |
| β6 Anxietyij | 0.19 (0.01) [0.16, 0.22] | η6 Anxietyij | 0.06 (0.02) [0.03, 0.09] |
|
| |||
| Random effects estimates | |||
|
| |||
| μ0 | 0.02 (0.01) [0.00, 0.05] | μ0 | 0.16 (0.04) [0.09, 0.24] |
| μ1 Dayij | 0.00 (0.00) [0.00, 0.00] | μ1 Dayij | 0.01 (0.00) [0.01, 0.02] |
| μ2 Surveyij | 0.01 (0.00) [0.00, 0.02] | μ2 Surveyij | 0.02 (0.01) [0.00, 0.04] |
| μ3 DownLag1,ij | 0.06 (0.01) [0.04, 0.08] | μ3 DownLag1,ij | 0.04 (0.01) [0.02, 0.06] |
| μ4 AnxietyLag1,ij | 0.01 (0.01) [0.00, 0.04] | μ4 AnxietyLag1,ij | 0.04 (0.01) [0.01, 0.06] |
| μ5 Anxietyij | 0.08 (0.01) [0.06, 0.11] | μ5 Anxietyij | 0.08 (0.01) [0.06, 0.11] |
|
| |||
| Anxiety | |||
|
| |||
| Model 2a | Model 2b | ||
|
| |||
| Location parameter | M (SD) [90% CI] | Scale parameter | M (SD) [90% CI] |
|
| |||
| Fixed effects estimates | |||
|
| |||
| β0 | 0.08 (0.06) [−0.05, 0.21] | η0 | −0.16 (0.08) [−0.31, −0.01] |
| β1 Dayij | 0.00 (0.00) [0.00, 0.00] | η1 Dayij | −0.01 (0.00) [−0.01, 0.00] |
| β2 Surveyij | −0.02 (0.01) [−0.04, 0.00] | η2 Surveyij | 0.01 (0.01) [−0.01, 0.04] |
| β3 DownLag1,ij | 0.00 (0.01) [−0.02, 0.02] | η3 DownLag1,ij | 0.00 (0.01) [−0.01, 0.02] |
| β4 AnxietyLag1,ij | 0.09 (0.01) [0.07, 0.10] | η4 AnxietyLag1,ij | 0.01 (0.01) [0.00, 0.03] |
| β5 Downi | 0.00 (0.01) [−0.03, 0.03] | η5 Downi | 0.01 (0.02) [−0.03, 0.05] |
| β6 Downij | 0.19 (0.02) [0.16, 0.22] | η6 Downij | 0.00 (0.01) [−0.02, 0.03] |
|
| |||
| Random effects estimates | |||
|
| |||
| μ0 | 0.06 (0.05) [0.00, 0.19] | μ0 | 0.08 (0.05) [0.01, 0.19] |
| μ1 Dayij | 0.01 (0.00) [0.00, 0.01] | μ1 Dayij | 0.01 (0.00) [0.01, 0.02] |
| μ2 Surveyij | 0.02 (0.01) [0.00, 0.04] | μ2 Surveyij | 0.04 (0.01) [0.02, 0.06] |
| μ3 DownLag1,ij | 0.02 (0.01) [0.00, 0.04] | μ3 DownLag1,ij | 0.02 (0.01) [0.00, 0.04] |
| μ4 AnxietyLag1,ij | 0.03 (0.01) [0.01, 0.05] | μ4 AnxietyLag1,ij | 0.03 (0.01) [0.01, 0.04] |
| μ5 Downij | 0.08 (0.01) [0.06, 0.11] | μ5 Downij | 0.05 (0.01) [0.03, 0.07] |
Note. 90% CI refers to the credible interval (CI) around the posterior distribution. The 90% CI denotes the interval that the associated estimate lies within, with 90% certainty. If the 90% CI does not include 0, the estimate is likely to be non-zero, with 95% certainty; these estimates are bolded. Subscript i refers to a person-mean value; ij refers to a person-mean centered variable.
Predictors of variability of depressed mood also varied on the individual-level (Table 2). We reviewed the personalized estimates for each parameter in the scale sub-model (Table 3, Figure 1). Among the parameters associated with a statistically significant fixed effect, we found that a majority of individuals did not demonstrate corresponding personalized estimates that were statistically significant. Therefore, we concluded that the strength of the fixed effects for the scale sub-model was likely driven by the magnitude of the personalized estimates from a minority of individuals in the sample.
Overall, results from Model 1 suggested that depressed mood demonstrated consistent patterns over time for the majority – but not all – individuals, and, for a small subset of individuals, lagged effects between previous levels of depressed mood and degree of variability of future depressed mood were especially pronounced. Additionally, momentary spikes in anxiety were often associated with higher momentary levels of depressed mood, as well as a greater degree of variability of depressed mood, although there was individual-level variation in the presence and direction of these associations.
Model 2a. Examining predictors of momentary levels of anxiety
Estimates from the model examining predictors of momentary anxiety are included in Table 2. Similar to Model 1, on average, anxiety demonstrated significant lagged effects from one timepoint to the next. Additionally, on average, momentary spikes in depressed mood (i.e., deviations from one’s typical level of depressed mood) were associated with higher levels of anxiety.
Model 2b. Examining predictors of momentary variability of anxiety
A negative intercept was observed, suggesting that – on average and given an individual’s typical level of depressed mood – the expected residual degree of variability of anxiety was lower when starting EMA.
Examination of random effects and individual-level variation across Models 2a, 2b
Some dynamic predictors of anxiety demonstrated significant individual-level variation (Table 2) and review of personalized estimates revealed further heterogeneity (Table 3, Figure 2). For example, we reviewed personalized estimates for the association between momentary deviations in depressed mood and momentary levels of anxiety. Although this effect was statistically significant for all individuals in the sample, there were six individuals (17.1%) who demonstrated a personalized estimate that was significantly larger than the fixed effect and six individuals (17.1%) who exhibited a personalized estimate that was significantly weaker than the fixed (i.e., average-level) effect. Consequently, the presence of this effect appears homogenous, although its magnitude tends to vary from one person to another.
Furthermore, nearly all predictors of variability of anxiety demonstrated significant random effects (i.e., individual-level variation around the fixed effect; Table 2) and there was some evidence of individual-level variation in model effects. First, although the fixed effect for the intercept from the scale sub-model was statistically significant on average, we found that 62.9% of individuals did not demonstrate a personalized estimate that was statistically significant. Therefore, we conclude that the strength of the fixed effect is likely driven by the magnitude of the personalized estimates from a minority of individuals in the sample. Second, we found that a small minority of individuals (n = 8, 22.9%) demonstrated a statistically significant association between momentary deviations in depressed mood and degree of variability of anxiety, even though the fixed effect was not statistically significant on average. Furthermore, within this subgroup, five individuals (14.3%) demonstrated a personalized estimate that was considerably higher-than-average and three individuals (8.6%) demonstrated a personalized estimate that was considerably lower-than-average. Consequently, we conclude that a small minority of individuals exhibited significant associations between momentary deviations in depressed mood and degree of variability of anxiety; however, the magnitude and valence of this effect varies from person to person.
Taken together, results from Model 2 suggest that anxiety demonstrated consistent patterns over time (although we demonstrated individual-level variation in the magnitude of this effect) and that momentary spikes in depressed mood (i.e., deviations from one’s typical level of depressed mood) were associated with higher momentary levels of anxiety (again, individual-level variation was evident in the magnitude of this effect). Additionally, the association between momentary deviations in depressed mood and degree of variability of anxiety was statistically significant for a minority of individuals in the sample.
Examining associations between dynamic indices and baseline SAD and MDD symptoms
We calculated the associations between clinical scores of depressive and social anxiety symptoms at baseline and personalized estimates to better characterize person- or trait-level differences in symptom dynamics (Table 4). We found that individuals with higher baseline BDI-II scores were more likely to exhibit a stronger lagged effect in levels of depressed mood during EMA. Likewise, individuals with higher baseline LSAS social anxiety scores were more likely to exhibit a stronger association between lagged levels of depressed mood and degree of variability of future anxiety during EMA.
Examining associations between dynamic indices and change in SAD and MDD symptoms
We examined the correlations between personalized estimates and change in depression, social anxiety, and social avoidance symptoms to examine how symptom dynamics were associated with symptom change over time (see Table 4). We demonstrated that individuals who experienced higher depressed mood in the evenings reported greater change in LSAS social anxiety symptoms during EMA. Additionally, those with stronger same-moment associations between depressed mood and anxiety reported greater change in LSAS social anxiety and avoidance symptoms across the 2-month period.
Overall, those with higher baseline SAD and MDD symptom severity exhibited stronger lagged effects of depressed mood on future levels of depressed mood, as well as stronger associations between lagged levels of depressed mood and degree of variability of future anxiety. There was some evidence to suggest that symptom dynamics were significantly associated with change in social anxiety and avoidance symptoms over the 2-month period.
Discussion
Examining (co-)variation in symptoms using dynamic data can improve our understanding of how psychopathology is maintained over time and strengthen transdiagnostic frameworks that have largely modeled psychopathology using trait-level measures. We applied an innovative modeling approach to examine dynamics of depressed mood and anxiety and person-specific heterogeneity within dynamic indicators of SAD and MDD. We found evidence of within-disorder, but not cross-disorder, inertia during EMA. We also found evidence of significant co-variation such that spikes from one’s typical level of depressed mood or anxiety were associated with increased levels of the respective symptom; although there was individual-level variation within the presence and magnitude of these effects. Efforts to characterize fluctuations and co-variation within daily experiences of mood and anxiety strengthens our understanding of dynamic patterns of psychopathology, individual-level variation within these dynamic patterns and may help to direct the use of clinical strategies to regulate momentary symptom fluctuations for vulnerable women.
Previous research has consistently demonstrated inertia in mood (i.e., lagged effects of mood; van de Leemput et al., 2014; Wichers et al., 2020) within individuals diagnosed with depression; however, there is limited evidence to detail how one affective experience (e.g., depressed mood) impacts the level (or degree of variability) around a co-occurring experience (e.g., anxiety). We demonstrated that lagged effects of depressed mood (or anxiety) were significantly associated with higher levels of (and, to some extent, greater variability of) the same symptom on average at the following timepoint. Additionally, women with higher levels of depressive symptoms at baseline demonstrated stronger lagged (i.e., autoregressive) effects of depressed mood during EMA. However, there was no evidence of cross-symptom lagged effects. That is, previous levels of anxiety were not significantly associated with future levels of (or variability of) depressed mood, nor were previous levels of depressed mood associated with future levels of (or degree of variability of) anxiety. Results from this sample of women with co-occurring SAD-MDD help to advance our theoretical understanding of how internalizing symptoms are maintained across moments in time. Specifically, these symptoms appear distinct over time, with little evidence of cross-disorder variation, Future work is needed to articulate the timescale over which these symptoms influence each other (e.g., weeks, months, or years).
Additionally, we found minimal evidence of trait-level differences in dynamics of depressed mood or anxiety during EMA. Specifically, a person’s average level of depressed mood or anxiety during EMA was not significantly associated with the level or degree of variability of their anxiety or depressed mood, respectively. Furthermore, baseline levels of depression or social anxiety symptoms were not significantly associated with personalized estimates of dynamic indices. That is, on average, differences in dynamic experiences of depressed mood or anxiety were not clearly a function of one’s baseline or typical level of symptoms. These findings contrast with previous literature which has demonstrated trait-level differences among symptom dynamics from the same disorder (e.g., individuals with MDD; Thompson et al., 2012). Results suggest that baseline or average-levels of depressed mood or anxiety show little correspondence with momentary levels of depressed mood and anxiety. These results strengthen our conceptualization of trait-versus state-level metrics as potentially distinct, with limited linkages within or between symptoms of fear and distress.
Instead, results provided clear evidence for momentary co-variation between hallmark symptoms of MDD and SAD and help to characterize the dynamic relationships within the internalizing spectra. For example, momentary spikes from one’s typical level of anxiety were associated with higher concurrent ratings of depressed mood and variability of depressed mood. Likewise, momentary spikes from one’s typical level of depressed mood were associated with higher concurrent ratings of anxiety. These results provide evidence of cross-disorder co-variation in depressed mood and anxiety that seem most likely to occur during periods of high symptom intensity. Additionally, individuals who exhibited stronger associations between momentary co-variation in their depressed mood and anxiety (i.e., personalized estimates that were larger in magnitude) reported lower change in social anxiety symptoms across EMA. Thus, tracking the momentary fluctuations in depressed mood (or anxiety) may help detect concurrent increases in anxiety (or depressed mood), suggestive of a lower emotion differentiation or a more persistent pattern of social anxiety and avoidance.
We examined individual-level variation within co-occurring symptom dynamics by modeling random effects and reviewing personalized estimates for each parameter. We found that although fixed effect estimates demonstrated that previous levels of depressed mood were significantly associated with future levels of depressed mood, approximately one-third of women did not demonstrate a significant lagged effect. Additionally, careful examination of personalized estimates demonstrated that significant fixed effects regarding the association between previous levels of depressed mood and degree of variability of future depressed mood were likely driven by a small subset of women (e.g., as over 75% of women in the sample did not demonstrate a significant effect). Examining heterogeneity provides helpful insight into person-specific differences. For example, designing momentary interventions based solely on review of fixed effects may result in limited efficacy for specific individuals within the sample. Future research is needed to examine whether these person-specific differences are associated with differential responses to relevant interventions (e.g., are women who lack strong temporal associations in depressed mood less responsive to interventions that target inert mood, such as intense physical activity)?
Likewise, there was evidence of person-specific heterogeneity around the magnitude and valence of model effects (despite homogeneity in the presence of an effect). For example, the association between momentary spikes in anxiety and levels of momentary co-occurring depressed mood was significant for all women in the sample; however, approximately 15% of women in the sample exhibited an association that was significantly stronger than the fixed effect and approximately 15% of women demonstrated an association that was significantly weaker than the fixed effect. Similarly, nearly one-quarter of women demonstrated a significant association between momentary spikes in depressed mood and degree of variability of co-occurring anxiety; however, within this subsample of women, some women’s degree of variability of anxiety was higher during periods of above-average mood; whereas, other women’s degree of variability of anxiety was higher during periods of below-average mood.
Several limitations are evident in this work. First, our findings are constrained to cisgender women with primary SAD and current or past MDD and so dynamic indices may yield different information or predictive value when modeling symptom dynamics for other affective disorders or in non-cisgender female populations. At the same time, individual-level generalizability in affective science may be broadly limited overall (see Foster & Beltz, 2021). Second, we used single-items to measure depressed mood and anxiety to increase the ease of completing EMA and maximize the number of person-specific observations, which is critical for maximizing stability in personalized estimates (Mansueto et al., 2022). However, single-item measurement decreases construct validity by restricting our definitions of depressed mood and anxiety and increases measurement error (see Dejonckheere et al., 2022 for design-related solution to assess measurement error for single-items). Future work is needed to model dynamics of additional symptoms associated with mood and anxiety disorders, as well as symptom-symptom interactions that define disorder given the significant symptom-level heterogeneity within internalizing disorders (e.g., Fried et al., 2016).
There are relevant clinical implications stemming from this work, particularly linked to measurement-based care initiatives that call for increased symptom monitoring to increase standards of care (e.g., within national healthcare systems; Lemke et al., 2017). Findings from our work underscore the utility of tracking momentary affective experiences to understand co-variation within daily experiences of mood and anxiety disorders and to account for person-specific heterogeneity when modeling changes in momentary mood and anxiety. Measuring the momentary links between co-occurring depressed mood and anxiety may improve our assessment of clinical severity for an individual with comorbid SAD-MDD. Moreover, findings highlight the utility of strategies to help women regulate symptoms on the momentary level (versus interventions based on broad diagnostic profiles). For example, using psychoeducation to build awareness around coping with momentary spikes in depressed mood (or anxiety) may better support women’s use of emotion regulation strategies, as these occasions are likely to also reflect momentary spikes in anxiety (or depressed mood). Alternatively, symptom-specific emotion regulation strategies (e.g., increasing pleasant experiences or approaching anxious situations) may be more useful in decreasing the inertia in depressed mood (or anxiety), as opposed to broader, cross-disorder, emotion-regulation strategies (e.g., cognitive restructuring).
Findings also illustrate the utility of accounting for differences in the valence of an effect. For example, distress tolerance skills may be more useful for women who exhibited increased variability of anxiety during periods of above-average levels of depressed mood; whereas a skill that is more targeted for anxiety specifically may be more effective for women who exhibited increased variability of anxiety during periods of below-average levels of depressed mood. However, future research is needed to determine the extent to which dynamic metrics correspond to future symptoms among individuals with co-occurring clinical presentations (see criticisms of predicting future psychopathology using affective dynamics; Bos et al., 2019; Dejonckheere et al., 2019).
Results highlight the utility of repeated symptom monitoring to measure within-day symptom fluctuations, which can assist treatment planning and prediction of treatment outcomes (Torous et al., 2020). However, the question of how to best incorporate dynamic measures into clinical practice requires continued discussion and evaluation. Our findings advance our conceptualization of the dynamic interplay between internalizing symptoms and offer insight to those working at the intersection of mental health, measurement-based care, and digital technology.
Supplementary Material
Acknowledgments
Research reported here was supported by grants from the National Institutes of Health (NIH): F31MH115641 (PI: Piccirillo). Marilyn Piccirillo was supported by NIH grants: K99AA029459 (PI: Piccirillo) and T32AA007455 (PI: Larimer). Madelyn Frumkin was supported by a NIH grant: F31MH124291 (PI: Frumkin). Katie Malloy Spink was supported by a Graduate Research Fellowship from the National Science Foundation. The analytic plan was pre-registered https://osf.io/s8jzb) and analytic code is included in supplementary material. Data are not openly available and may be requested by emailing the corresponding author.
We wish to thank Dr. Tom Rodebaugh who provided mentorship during the data collection process. We also wish to acknowledge Drs. Anna Karam, Elizabeth Hawkey, Patrick Cruitt, Zoë Hawks, Erin Bondy, Alison Moreau, and Jason Grossman who assisted with data collection for this study.
Footnotes
Declarations of interest
None
Random effects for intercept and day parameters from Model 2, location sub-model demonstrated R-hat = 1.01.
References
- Abramso LY, Metalsk GI, & Allo LB (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96, 358–372. 10.1037/0033-295X.96.2.358 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders : DSM-5 (5th ed.). American Psychiatric Association. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory - II. Psychological Corporation. [Google Scholar]
- Bos EH, Jonge P, & Cox RFA (2019). Affective variability in depression: Revisiting the inertia–instability paradox. British Journal of Psychology, 110(4), 814–827. 10.1111/bjop.12372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosley HG, & Fisher AJ (2020). Mapping the idiographic dynamics of emotion. 32nd Annual Meeting of the Association for Psychological Science. [Google Scholar]
- Breslau N, Schultz L, & Peterson E (1995). Sex differences in depression: a role for preexisting anxiety. Psychiatry Research, 58(1), 1–12. 10.1016/0165-1781(95)02765-O [DOI] [PubMed] [Google Scholar]
- Brose A, Koval P, Heinrich M, Zagorscak P, Bohn J, & Knaevelsrud C (2024). Location-scale modeling as an integrative approach to symptom dynamics during psychotherapy: An illustration with depressive symptoms. Journal of Consulting and Clinical Psychology. 10.1037/ccp0000892 [DOI] [PubMed] [Google Scholar]
- Bürkner P-C (2017). brms: An R Package for Bayesian Multilevel Models using Stan. Journal of Statistical Software, 80(1), 1–28. 10.18637/jss.v080.i01 [DOI] [Google Scholar]
- Dejonckheere E, Demeyer F, Geusens B, Piot M, Tuerlinckx F, Verdonck S, & Mestdagh M (2022). Assessing the reliability of single-item momentary affective measurements in experience sampling. Psychological Assessment, 34(12), 1138–1154. 10.1037/pas0001178 [DOI] [PubMed] [Google Scholar]
- Dejonckheere E, Mestdagh M, Houben M, Rutten I, Sels L, Kuppens P, & Tuerlinckx F (2019). Complex affect dynamics add limited information to the prediction of psychological well-being. Nature Human Behavior, 3, 478–491. 10.1038/s41562-019-0555-0 [DOI] [PubMed] [Google Scholar]
- Elmer T, Geschwind N, Peeters F, Wichers M, & Bringmann L (2020). Getting stuck in social isolation: Solitude inertia and depressive symptoms. Journal of Abnormal Psychology, 129(7), 713–723. 10.1037/abn0000588 [DOI] [PubMed] [Google Scholar]
- Foster KT, & Beltz AM (2021). Emotion heterogeneity in affective complexity among men and women. Emotion. 10.1037/emo0000956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster KT, Hicks BM, Iacono WG, & McGue M (2015). Gender differences in the structure of risk for alcohol use disorder in adolescence and young adulthood. Psychological Medicine, 45(14), 3047–3058. 10.1017/S0033291715001014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster KT, Li N, McClure EA, Sonne SC, & Gray KM (2016). Gender differences in internalizing symptoms and suicide risk among men and women seeking treatment for cannabis use disorder from late adolescence to middle adulthood. Journal of Substance Abuse Treatment, 66, 16–22. 10.1016/j.jsat.2016.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Epskamp S, Schoevers RA, Tuerlinckx F, & Borsboom D (2016). Measuring depression over time...or not? lack of unidimensionality and longitudinal measurement invariance in four common rating scales of depression. Psychological Assessment, 28(11), 1354–1367. 10.1037/pas0000275 [DOI] [PubMed] [Google Scholar]
- Gelman Andrew. (2006). Prior distributions for variance parameters in hierarchical models. Bayesian Analysis, 1(3), 515–534. 10.1214/06-BA117A. [DOI] [Google Scholar]
- Hamaker EL, Grasman RPPP, Cipresso P, Italiano IA, & Zhang J (2015). To center or not to center? Investigating inertia with a multilevel autoregressive model. 5. 10.3389/fpsyg.2014.01492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedeker D, Mermelstein RJ, & Demirtas H (2008). An application of a mixed-effects location scale model for analysis of ecological momentary assessment (EMA) data. Biometrics, 64(2), 627–634. 10.1111/j.1541-0420.2007.00924.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heimberg RG, Brozovich FA, & Rapee RM (2014). A cognitive-behavioral model of social anxiety disorder. In Hofmann PM, DiBartolo SG(Ed.), Social Anxiety: Clinical, Developmental, and Social Perspectives (3rd ed., pp. 705–728). Elsevier. 10.1016/B978-0-12-394427-6.00024-8 [DOI] [Google Scholar]
- Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR, & Liebowitz MR (1999). Psychometric properties of the Liebowitz Social Anxiety Scale. Psychological Medicine, 29(1), 199–212. 10.1017/S0033291798007879 [DOI] [PubMed] [Google Scholar]
- Jahng S, Wood PK, & Trull TJ (2008). Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychological Methods, 13, 354–375. 10.1037/a0014173 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen H-U (2012). Twelve-month and lifetime prevalence morbid risk of anxiety and mood disorder in the US. International Journal of Methods in Psychiatric Research, 21, 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Stang P, Wittchen H-U, Stein M, & Walters EE (1999). Lifetime co-morbidities between social phobia and mood disorders in the US National Comorbidity Survey. Psychological Medicine, 29, 555–567. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, Brown TA, Carpenter WT, Caspi A, Clark LA, Eaton NR, Forbes MK, Forbush KT, Goldberg D, Hasin D, Hyman SE, Ivanova MY, Lynam DR, Markon K, … Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Koval P, Kuppens P, Allen NB, & Sheeber L (2012). Getting stuck in depression: The roles of rumination and emotional inertia. Cognition and Emotion, 26(8), 1412–1427. 10.1080/02699931.2012.667392 [DOI] [PubMed] [Google Scholar]
- Kuppens P, Sheeber LB, Yap MBH, Whittle S, Simmons JG, & Allen NB (2012). Emotional inertia prospectively predicts the onset of depressive disorder in adolescence. Emotion, 12(2), 283–289. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, & Dunbar GC (1997). The Mini International Neuropsychiatric Interview (MINI): A short diagnostic structured interview. European Psychiatry, 12, 224–231. 10.1016/S0924-9338(97)83296-8 [DOI] [Google Scholar]
- Lemke S, Boden MT, Kearney LK, Krahn DD, Neuman MJ, Schmidt EM, Trafton JA, & Operations H (2017). Measurement-based management of mental health quality and access in VHA: SAIL mental health domain. Psychological Services , 14(1), 1–12. 10.1037/ser0000097 [DOI] [PubMed] [Google Scholar]
- Liebowitz MR (1987). Social phobia. Modern Problems in Pharmacopsychiatry, 22, 141–173. [DOI] [PubMed] [Google Scholar]
- Mansueto AC, Wiers RW, van Weert JCM, Schouten BC, & Epskamp S (2022). Investigating the feasibility of idiographic network models. Psychological Methods. 10.1037/met0000466 [DOI] [PubMed] [Google Scholar]
- Miranda-Mendizabal A, Castellví P, Parés-Badell O, Alayo I, Almenara J, Alonso I, Blasco MJ, Cebrià A, Gabilondo A, Gili M, Lagares C, Piqueras JA, Rodríguez-Jiménez T, Rodríguez-Marín J, Roca M, Soto-Sanz V, Vilagut G, & Alonso J (2019). Gender differences in suicidal behavior in adolescents and young adults: Systematic review and meta-analysis of longitudinal studies. International Journal of Public Health, 64(2), 265–283. 10.1007/s00038-018-1196-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker G, Wilhelm K, Mitchell P, Austin MP, Roussos J, & Gladstone G (1999). The influence of anxiety as a risk to early onset major depression. Journal of Affective Disorders, 52(1–3), 11–17. 10.1016/S0165-0327(98)00084-6 [DOI] [PubMed] [Google Scholar]
- Piccirillo ML, & Rodebaugh TL (2022). Personalized models of internalizing symptoms for women with social anxiety disorder and depression. Journal of Affective Disorders, 298, 262–276. 10.31234/osf.io/yjq65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2023). R: A language and environment for statistical computing (4.3.1) R Foundation for Statistical Computing. [Google Scholar]
- Stein MB, Fuetsch M, Müller N, Höfler M, Lieb R, & Wittchen H-U (2001). Social anxiety disorder and the risk of depression: A prospective community study of adolescents and young adults. Archives of General Psychiatry, 58(3), 251–256. 10.1001/archpsyc.58.3.251 [DOI] [PubMed] [Google Scholar]
- Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, & Gotlib IH (2012). The everyday emotional experience of adults with major depressive disorder: Examining emotional instability, inertia, and reactivity. Journal of Abnormal Psychology, 121(4), 819–829. 10.1037/a0027978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonge NA, Miller JP, Kharasch ED, Lenze EJ, & Rodebaugh TL (2024). An investigation of the potential clinical utility of critical slowing down as an early warning sign for recurrence of depression. Journal of Behavior Therapy and Experimental Psychiatry, 82. 10.1016/j.jbtep.2023.101922 [DOI] [PubMed] [Google Scholar]
- Torous J, Powell AC, & Rodriguez-Villa E (2020). Health information technology resources to support measurement-based care. Child and Adolescent Psychiatric Clinics of North America. 10.1016/j.chc.2020.06.011 [DOI] [PubMed] [Google Scholar]
- van de Leemput IA, Wichers M, Cramer AOJ, Borsboom D, Tuerlinckx F, Kuppens P, van Nes EH, Viechtbauer W, Giltay EJ, Aggen SH, Derom C, Jacobs N, Kendler KS, van der Maas HLJ, Neale MC, Peeters F, Thiery E, Zachar P, & Scheffer M (2014a). Critical slowing down as early warning for the onset and termination of depression. Proceedings of the National Academy of Science of the United States of America, 111, 87–92. 10.1073/pnas.1312114110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichers M, & Groot PC (2016). Critical slowing down as a personalized early warning signal for depression. Psychotherapy and Psychosomatics, 85, 114–116. 10.1159/000441458 [DOI] [PubMed] [Google Scholar]
- Wichers M, Smit AC, & Snippe E (2020). Early warning signals based on momentary affect dynamics can expose nearby transitions in depression: A confirmatory single-subject time-series study. Journal for Person-Oriented Research, 6(1), 1–15. 10.17505/jpor.2020.22042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham H (2016). ggplot2: Elegant Graphics for Data Analysis. Springer-Verlag New York. [Google Scholar]
- Wickham H, François R, Henry L, Müller K, & Vaughan D (2023). dplyr: A grammar of data manipulation (1.1.4). https://cran.r-project.org/package=dplyr [Google Scholar]
- Williams DR, Martin SR, Liu S, & Rast P (2020). Bayesian multivariate mixed-effects location scale modeling of longitudinal relations among affective traits, states, and physical activity. European Journal of Psychological Assessment, 36(6), 981–997. 10.1027/1015-5759/a000624 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


