Abstract
Purpose
The aim of this study is to investigate the effect of obesity on the results of laparoscopic adrenal surgery in patients with Cushing syndrome.
Methods
This retrospective study was performed in Department of General Surgery at Erciyes University School of Medicine between January 2010 and January 2023. Our analysis included Cushing syndrome patients who underwent unilateral laparoscopic adrenalectomy (LA) with the transabdominal lateral approach. All patients were evaluated in terms of age, sex, tumor diameter, body mass index (BMI), American Society of Anesthesiologists physical status classification, morbidities, surgery history, tumor side, operative time, conversion to open surgery, complications, and length of hospital stay.
Results
A total of 90 patients (75 females and 15 males) underwent a transperitoneal LA. Patients were divided into 2 groups according to their BMI: obese group (≥30 kg/m2; n = 53, 58.8%) and nonobese group (<30 kg/m2; n = 37, 41.2%). All patients were classified into 3 subgroups: obese patient group, BMI ≥30–39 kg/m2 (n = 23); morbidly obese patient group, BMI ≥40 kg/m2 (n = 14); and nonobese patient group, BMI <30 kg/m2 (n = 53). There was no significant difference in intraoperative complications, conversion to open surgery, operative time, or length of hospital stay between the groups. Only conversion to open surgery was a risk factor for postoperative complications in univariate and multivariate analyses (odds ratio, 15.4; 95% confidence interval, 1.277–185.599; P = 0.031).
Conclusion
Our results showed that LA is safe and effective in patients with Cushing syndrome with morbid obesity, allowing acceptable morbidity and length of hospital stay.
Keywords: Adrenalectomy, Adrenal glands, Cushing syndrome, Laparoscopic surgery, Morbid obesity
INTRODUCTION
Laparoscopic adrenalectomy (LA) has been the gold standard in the treatment of benign adrenal tumors [1]. The laparoscopic approach has advantages such as less postoperative pain, less bleeding, better cosmetic appearance for patients, and faster return to daily activities [2]. Current indications for LA are similar to open surgery and include all functional adrenal tumors; pheochromocytoma, aldosteronoma, cortisol-producing adenoma (Cushing syndrome), adrenal hyperplasia secondary to bilateral Cushing disease, or ectopic adrenocorticotropic hormone production [3]. The World Health Organization defines obesity as body mass index (BMI) of ≥30 kg/m2 [4]. Obesity is often considered a risk factor for longer operating time, increased blood loss, septic complications, and wound infection [5,6,7]. Additionally, obesity causes an increased risk of wound infection due to less perfusion of fatty tissue and less oxygen. Long-term hospital stay is due mainly to perioperative and postoperative complications [8].
There are some studies in the literature on minimally invasive surgery for the adrenal gland in obese patients; these studies have included all functional diseases. However, there are few studies investigating the impact of obesity on patients with Cushing syndrome [9]. This study aims to investigate the effect of obesity on the results of laparoscopic adrenal surgery in patients with Cushing syndrome.
METHODS
Ethics statement
The study protocol was approved by the Ethics Committee of the University of Erciyes University Faculty of Medicine, Kayseri, Turkiye (No. 2022/749).
Study design and participants
This retrospective study was performed in Department of General Surgery at Erciyes University School of Medicine between January 2010 and January 2023. During the study period, transperitoneal LA was conducted on 200 patients, among whom 185 cases were unilateral LA. Therefore, our analysis included 90 consecutive patients with Cushing syndrome who underwent laparoscopic unilateral LA with the transabdominal lateral approach. The endocrine unit evaluated each patient prior to surgery and decided on surgical indications at the endocrine tumor board. The preoperative evaluation measured serum cortisol levels, aldosterone-to-renin ratio, 24-hour urinary cortisol level, dexamethasone suppression test, dehydroepiandrosterone sulfate, 17-hydroxyprogesterone, testosterone, 24-hour urinary metanephrine, normetanephrine, and vanillylmandelic acid levels. Surgical indications were considered in patients with Cushing syndrome. Malignancies and other functional or non-functioning adrenal tumors were excluded from this study. Hemogram, coagulation profile, biochemical parameters, and serum electrolytes were analyzed in all cases. The location of the adrenal masses was determined using CT or MRI. The patients were divided into 2 groups according to BMI: nonobese group (<30 kg/m2) and obese group (≥30 kg/m2).
Data collection
Data were collected from the patient’s medical records. All patients were evaluated in terms of age, sex, tumor diameter, BMI (kg/m2), American Society of Anesthesiologists (ASA) physical status (PS) classification, accompanying morbidities, surgery history, surgery indication, tumor side and size, operative time, conversion to open surgery, dissection devices, adrenal vein ligation method, a need for additional trocar, complications, and length of hospital stay.
Surgical technique
All adrenalectomy procedures were conducted under general anesthesia by experienced endocrine surgeons with similar learning curves. All patients received antibiotic and antithrombotic prophylactic therapy. All laparoscopic bilateral adrenalectomies were performed concurrently using a lateral transperitoneal approach. Surgical procedures were performed using either the left or right lateral decubitus postures. Operation duration was defined as the period between surgical incision and wound dressing. During dissections, L-Hook monopolar cautery was used with the LigaSure vascular sealing device (Medtronic) or Harmonic ultrasonic scalpel (Ethicon Endo-Surgery). Two devices were used for adrenal vein ligation: a metal clip, the Hem-o-lok polymer ligation system.
After insufflation, a 10-mm camera trocar was placed in the anterior axillary line on both sides, 2–3 cm below the costal border for right and left adrenalectomy. On the right side, 10-mm and 5-mm working trocars were inserted through the midaxillary and midclavicular lines, respectively. The 5-mm and 10-mm working trocars were inserted for the left side through the midaxillary and midclavicular lines, respectively. Trocars were inserted in the subxiphoid in the epigastrium on the left side.
Outcomes
The primary outcome was to investigate the effect of obesity on the results of laparoscopic adrenal surgery in patients with Cushing syndrome. The secondary outcome was to compare the clinical outcomes of obese patients between BMI of >30 to <40 kg/m2 and ≥40 kg/m2. Postoperative complications in 30 days were classified according to the Clavien-Dindo classification [10].
Statistical analysis
The data were analyzed using JMP 16.2.0 software (SAS Institute Inc.). The data were analyzed using descriptive statistical techniques to determine the number, percentage, mean, and standard deviation. The Shapiro-Wilk test was used to determine the normal distribution. The data were represented as mean, standard deviation, or median, depending on the distribution (interquartile range, IQR). Categorical variables were compared using the chi-square or Fisher exact test. The t-test and Wilcoxon signed-rank test were used to compare quantitative and ordinal variables.
Otherwise, the Wilcoxon rank-sum test and t-test were used to compare ordinal and quantitative variables. Multiple comparisons are made using the Kruskal-Wallis test if a variable has 3 or more levels. Multiple logistic regression analyses were applied to identify the independent predictors of postoperative complications. The univariate analysis with a P-value of <0.20 was included in the multiple model for the logistic regression analysis to obtain adjusted odds ratios. The P-value of <0.05 was considered to be statistically significant.
RESULTS
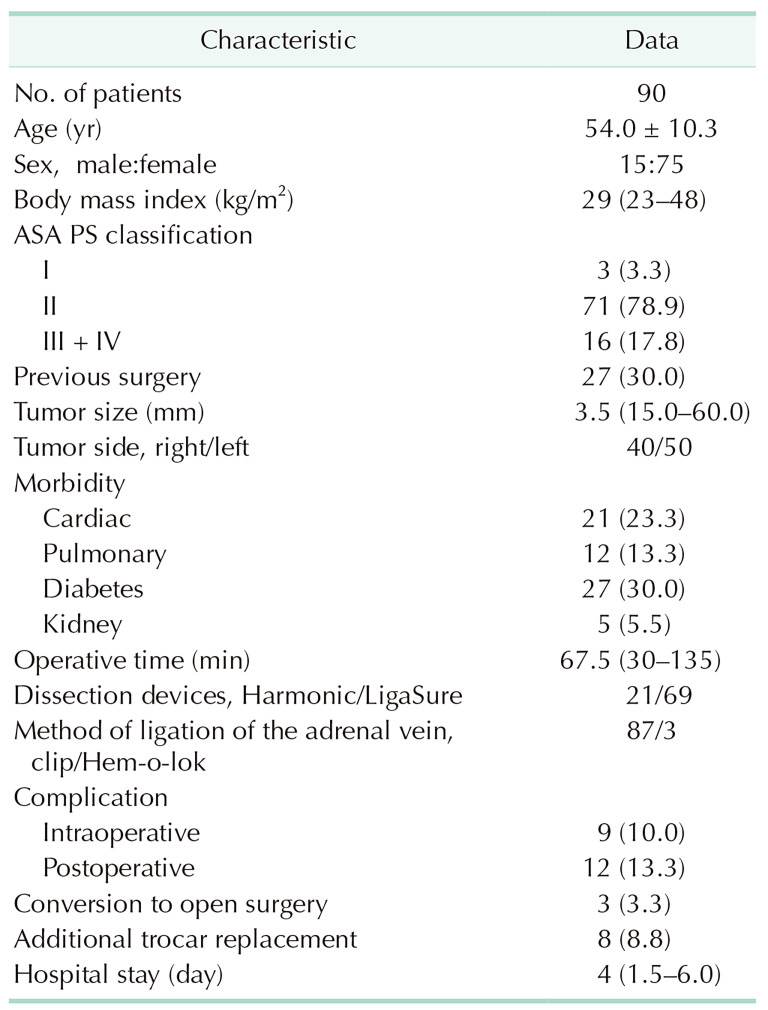
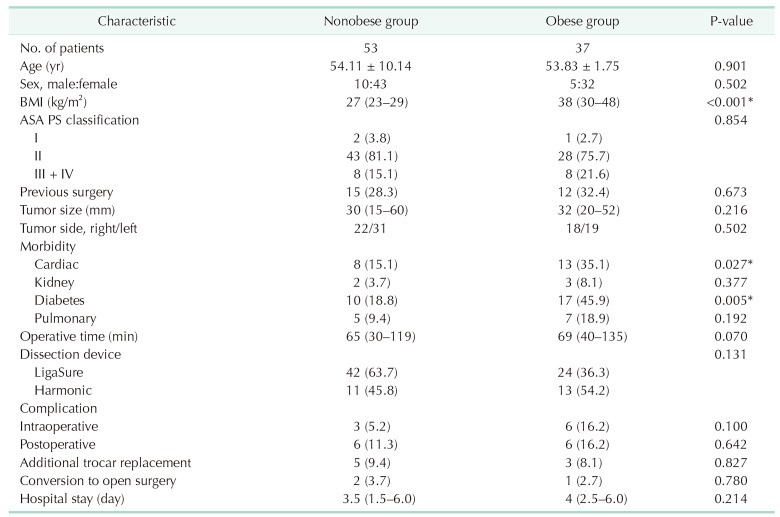
During the study period, unilateral LA was performed on 215 patients. Of these, 90 patients with Cushing syndrome were included in this study. The number of surgical procedures performed by 2 experienced surgeons was 43 and 47, respectively. A total of 90 patients (75 females and 15 males) underwent laparoscopic transperitoneal adrenalectomy. The demographic findings of all patients are shown in Table 1. The median BMI was 29 kg/m2 (IQR, 23–48 kg/m2). Patients were divided into 2 groups according to their BMI: obese (≥30 kg/m2) and nonobese (<30 kg/m2). The nonobese group included 53 patients (58.8%), and the obese group included 37 patients (41.2%). A comparison of the perioperative and postoperative outcomes of obese and nonobese patients is shown in Table 2. The mean age of the obese group was 53.83 ± 1.75 years, and the mean age of the nonobese group was 54.11 ± 10.14 years (P = 0.901). The median tumor size was 3.2 cm in the obese group and 3.0 cm in the nonobese group. All patients had Cushing syndrome in all preoperative diagnoses. The median operation time was 65 minutes (IQR, 30–119 minutes) in the nonobese group and 69 minutes (IQR, 40–135 minutes) in the obese group (P = 0.07). Intraoperative complications were seen in 6 (16.2%) and 3 patients (5.2%) in the obese and nonobese groups, respectively. These complications were liver laceration (n = 5), vascular injury (n = 3), and organ injury (n = 1). The conversion rate to laparotomy was 2.7% in the obese group and 3.7% in the nonobese group (P = 0.780). The reasons for conversion to open surgery were difficult dissection in 2 patients and uncontrolled bleeding in 1 patient. Surgery was completed without intraoperative mortality in patients who were converted to laparotomy.
Table 1. Demographic characteristics of patients.
Values are presented as number only, mean ± standard deviation, median (interquartile range), or number (%).
ASA, American Society of Anesthesiologists; PS, physical status.
Harmonic, Harmonic ultrasonic scalpel (Ethicon Endo-Surgery); LigaSure, LigaSure vascular sealing device (Medtronic).
Table 2. Comparison of perioperative and postoperative results between obese and nonobese patients.
Values are presented as number only, mean ± standard deviation, median (interquartile range), or number (%).
BMI, body mass index; ASA, American Society of Anesthesiologists; PS, physical status.
LigaSure, LigaSure vascular sealing device (Medtronic); Harmonic, Harmonic ultrasonic scalpel (Ethicon Endo-Surgery).
Nonobese group, BMI <30 kg/m2; obese group, BMI ≥30 kg/m2.
*P < 0.05, statistically significant.
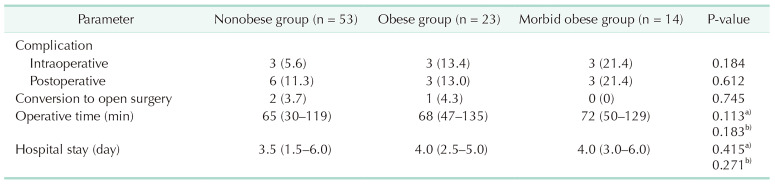
Also, all the patients were split into 3 groups: those with a BMI of 30–39 kg/m2 were considered obese (n = 23); those with a BMI of ≥40 kg/m2 were considered morbidly obese (n = 14); a nd t hose w ith a BMI of <30 kg/m2 (n = 53) were not obese. The results of surgery and after surgery were compared (Table 3). Three patients in the obese group (13.4%) with a BMI of 30–39 kg/m2, 3 patients in the obese group (21.4%) with a BMI of ≥40 kg/m2, and 6 patients in the nonobese group (11.3%) had problems after surgery. There was no statistically significant difference between the groups (P = 0.612). Postoperative complications included atelectasis (n = 5), respiratory failure (n = 1), incisional hernia (n = 1), arrhythmia (n = 3), and pleural effusion (n = 2). Also, among the above complications, incisional hernia (n = 1), atelectasis (n = 1), and respiratory failure (n = 1) were seen in patients who underwent open surgery. Incisional hernia appeared after 3 months postoperatively. There was no significant difference in intraoperative complications, conversion to open surgery, operative time, or length of hospital stay in these 3 patient groups categorized at the same time. Both groups used dissection instruments at similar rates. The median hospital stay was 4 days (IQR, 2.5–6.0 days) in the obese patient group and 3.5 days (IQR, 1.5–6.0 days) in the nonobese patient group.
Table 3. Comparison of perioperative results of the patient groups.
Nonobese group, body mass index (BMI) <30 kg/m2; obese group, BMI ≥30–39 kg/m2; morbid obese group, BMI ≥40 kg/m2.
a)Obese patient group with BMI <30 kg/m2 compared with obese patient group with BMI ≥40 kg/m2.
b)Obese patient group with BMI <30 kg/m2 compared with obese patient group with BMI ≥30–39 kg/m2.
Reference group, nonobese patient group with BMI <30 kg/m2.
There was no statistically significant difference between the 2 g roups (P = 0.214). All patients underwent deep vein thrombosis prophylaxis. Cardiac morbidity was seen in 21 patients (23.3%), renal morbidity in 5 patients (5.5%), diabetes in 27 patients (30.0%), and pulmonary morbidity in 12 patients (13.3%). Cardiac morbidity was present in 13 patients in the obese patient group (35.1%) and 8 patients in the nonobese patient group (15.1%). There was a statistically significant difference between the 2 groups for cardiac morbidity (P = 0.027). Diabetes-related morbidity was present in 17 patients in the obese patient group (45.9%) and 10 patients in the nonobese patient group (18.8%). There was a statistically significant difference between the 2 groups for diabetes-related morbidity (P = 0.005).
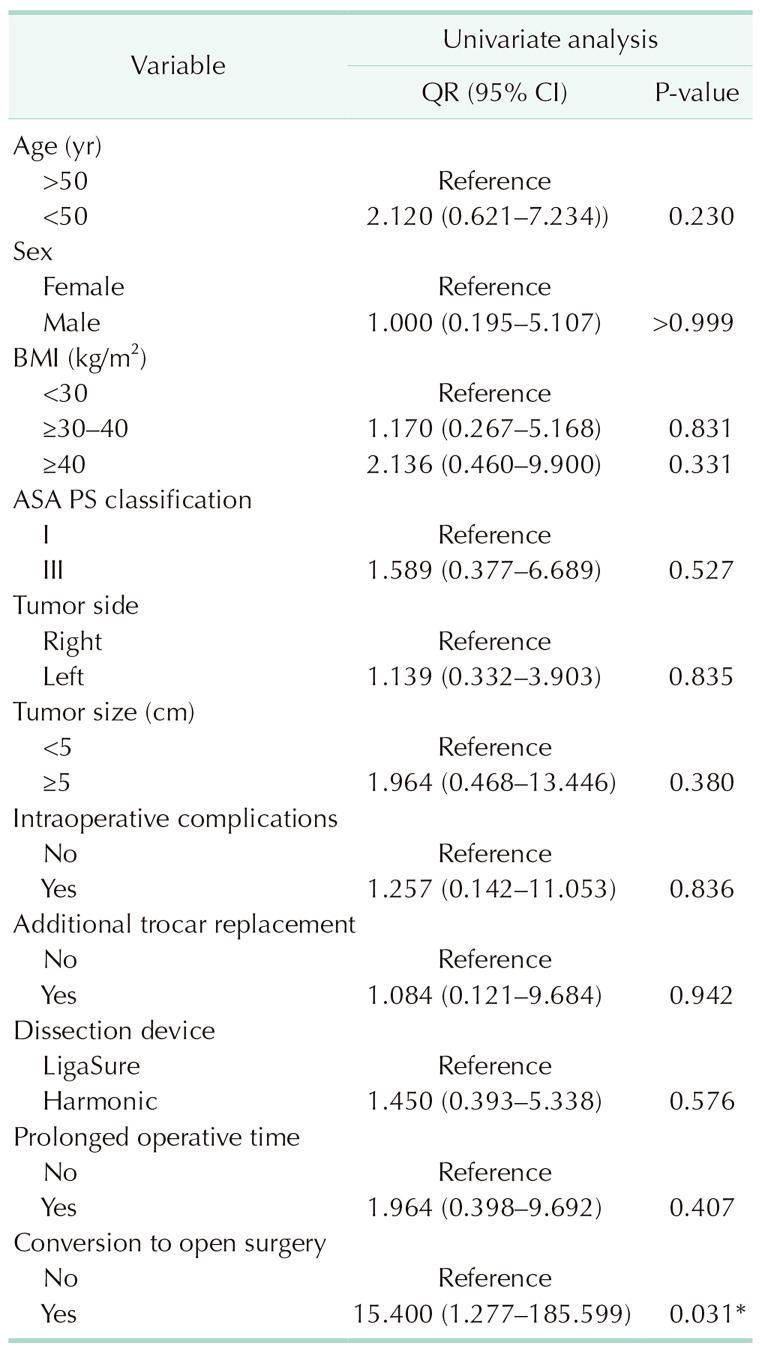
We performed a logistic regression analysis to determine postoperative complications (Table 4). In univariate analysis, age, sex, BMI, ASA PS classification, tumor side, tumor diameter, intraoperative complications, additional trocar, dissection instrument, and prolonged operative time were not found to be risk factors for postoperative complications. Only conversion to open surgery was a predictor of postoperative complications in univariate and multivariate analyses (odds ratio, 15.4; 95% confidence interval, 1.277–185.599; P = 0.031). Blood transfusion was not required in any patient, and mortality was not observed.
Table 4. Univariate and multiple regression analysis for postoperative complications in all patients.
OR, odds ratio; CI, confidence interval; BMI, body mass index; ASA, American Society of Anesthesiologists; PS, physical status.
LigaSure, LigaSure vascular sealing device (Medtronic); Harmonic, Harmonic ultrasonic scalpel (Ethicon Endo-Surgery).
*P < 0.05, statistically significant.
DISCUSSION
The aim of this study was to investigate the effect of obesity on the outcomes of laparoscopic adrenal surgery in patients with Cushing syndrome. This study shows that the complications, length of hospitalization, operative time, and exposure rates were similar in obese patients with BMI ≥30 kg/m2 compared to nonobese patients in LA. In addition, the complications, length of hospitalization, duration of operation, and exposure rates were similar in patients with morbid obesity above BMI ≥40 kg/m2 compared to patients with BMI <30 kg/m2. The ASA PS classification and morbid obesity, side of operation, tumor diameter, dissection instrument, and prolonged operation time were not found to be risk factors for postoperative complications. Only the conversion to open surgery was identified as a risk factor.
The difficulties of laparoscopic surgical procedures in obese patients have been previously described [7,11,12]. Increased central and visceral adiposity also leads to intraoperative technical difficulties during LA, which may be responsible for prolonged operative times and higher rates of conversion to open surgery [11,12,13]. In addition, obese patients have a higher rate of comorbid disease and a higher risk of perioperative complications for LA [11]. Based on the findings of numerous studies, LA is associated with a shorter postoperative hospital stay, early recovery, and shorter operative time compared to open surgery [14,15].
There are 4 approaches for LA: lateral and anterior transperitoneal and lateral and posterior retroperitoneal, and none of them is superior to the other [4]. The lateral transabdominal approach is the most commonly used laparoscopic approach for adrenal surgery [2]. More than 75% of laparoscopic adrenalectomies are performed using the lateral transperitoneal technique. The advantage of the lateral approach is that it allows the adrenal glands to be exposed to gravity [16,17]. We have already presented our experience with this approach [18,19,20].
The increase in obesity in the last 10 years, especially in developed countries, has caused new challenges for surgeons [11,13]. The adrenal gland is surrounded by fatty tissue surround. Adrenal tissue is difficult to see and the safety of adrenalectomy may be compromised in patients with a high BMI [12,21]. There are questions about LA in morbidly obese patients due to the limited study area and increased risk of postoperative complications [9]. In addition, the diagnosis of Cushing syndrome has been identified as an adverse prognostic factor, as both subclinical and symptomatic chronic hypercortisolism have been shown to adversely affect perioperative outcomes after various general surgical procedures, including LA [13]. Obese patients are at high surgical risk and may have adverse outcomes including perioperative and postoperative complications [7,13]. In some studies, obesity had no significant effect on the results of laparoscopic transperitoneal adrenalectomy in terms of complications, exposure, and length of hospital stay [9,19]; in other studies, there has been an increase in the risk of complications [11,20].
In our study, the rates of intraoperative and postoperative complications were 10% and 13.3% in all cases and were compatible with the studies in the literature. When Pędziwiatr et al. [19] compared obese patients with nonobese patients, hospitalization and complication rates were similar. Similarly, postoperative complications, duration of hospitalization, and intraoperative complications were similar for obese patients in our study. Although intraoperative complications were more common in obese patients, they were not statistically significant. Most of these complications did not require any life-threatening additional treatments or interventions.
The conversion rate to open surgery in LA is 1%–22% [16,21,22]. Conversion to open surgery is usually due to bleeding, tight adhesions, obesity, large masses, inexperienced surgeons, or malignant processes [16,23,24]. In our study, open surgery was preferred in 3 of LA (3.3%), and no difference was observed between nonobese patients and obese and morbidly obese patients.
Patient comorbidities (ASA PS classification III + IV, previous abdominal surgery, obesity, and diabetes), adrenal pathology (pheochromocytoma), tumor size (≥6 cm), and surgeon inexperience are associated with increased operative time, conversions, complications, and length of hospitalization [7,16,25,26,27,28].
The operative times and rates of conversion to open surgery were similar between the nonobese group and the morbidly obese group when compared with nonobese patients in our study. We evaluated the factors determining postoperative complications. In logistic regression analysis, conversion to open surgery was found to be a significant risk factor. This was not directly related to obesity. Differently, Kazaure et al. [7] also found that all complications, wound site and septic complications were higher in obese and morbidly obese patients.
The difficulty of good visualization of the surgical field in obese patients during LA has been reported to result in a significantly longer operative time [29,30]. We used an additional trocar in 8 patients to improve visualization of the surgical field, particularly in cases where the spleen could not be excluded on the left side or where there was too much periadrenal fat. The use of additional trocars was similar in both groups and was used in 5 patients in the group with BMI <30 kg/m2 (9.4%) and 3 patients in the group with BMI ≥30 kg/m2 (8.1%), with no statistical significance. In addition, the use of an extra trocar did not increase postoperative complications.
This retrospective study has some limitations. LA was performed by 2 competent endocrine surgeons with a similar learning curve. We used 2 different energy devices at similar rates in practice. We did not see an effect on the determinant of postoperative complications. We compared patients with Cushing syndrome and did not include other endocrine disorders. We believe this provides a more homogeneous study group for a comparative analysis.
Our results showed that LA is safe and effective in patients with Cushing syndrome with morbid obesity, allowing acceptable morbidity and length of hospital stay. The lateral transperitoneal approach provides an excellent anatomical view. ASA PS classification, dissection instruments, tumor side, use of additional trocar, sex, and prolonged operative time were not found to be determinants of postoperative complications. Conversion to open surgery was the only factor determining postoperative complications. Obesity was not a directly related risk factor. A multidisciplinary team, including anesthesiologists, intensive care specialists, and endocrinologists, is needed for adequate perioperative and postoperative management of patients.
Footnotes
Fund/Grant Support: None.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: BÖ, AA.
- Formal Analysis: AÖ, MK.
- Investigation: OÖ, BÖ.
- Methodology: BÖ, MK, FÖ.
- Project Administration: SD, FÖ.
- Writing – Original Draft: SÇ, MG, MK.
- Writing – Review & Editing: All authors.
References
- 1.Gagner M, Lacroix A, Bolté E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma. N Engl J Med. 1992;327:1033. doi: 10.1056/NEJM199210013271417. [DOI] [PubMed] [Google Scholar]
- 2.Raffaelli M, De Crea C, Bellantone R. Laparoscopic adrenalectomy. Gland Surg. 2019;8(Suppl 1):S41–S52. doi: 10.21037/gs.2019.06.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saunders BD, Wainess RM, Dimick JB, Upchurch GR, Doherty GM, Gauger PG. Trends in utilization of adrenalectomy in the United States: have indications changed? World J Surg. 2004;28:1169–1175. doi: 10.1007/s00268-004-7619-6. [DOI] [PubMed] [Google Scholar]
- 4.Stefanidis D, Goldfarb M, Kercher KW, Hope WW, Richardson W, Fanelli RD, et al. SAGES guidelines for minimally invasive treatment of adrenal pathology. Surg Endosc. 2013;27:3960–3980. doi: 10.1007/s00464-013-3169-z. [DOI] [PubMed] [Google Scholar]
- 5.Khoury W, Stocchi L, Geisler D. Outcomes after laparoscopic intestinal resection in obese versus non-obese patients. Br J Surg. 2011;98:293–298. doi: 10.1002/bjs.7313. [DOI] [PubMed] [Google Scholar]
- 6.Kamoun S, Alves A, Bretagnol F, Lefevre JH, Valleur P, Panis Y. Outcomes of laparoscopic colorectal surgery in obese and nonobese patients: a case-matched study of 180 patients. Am J Surg. 2009;198:450–455. doi: 10.1016/j.amjsurg.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 7.Kazaure HS, Roman SA, Sosa JA. Obesity is a predictor of morbidity in 1,629 patients who underwent adrenalectomy. World J Surg. 2011;35:1287–1295. doi: 10.1007/s00268-011-1070-2. [DOI] [PubMed] [Google Scholar]
- 8.Chand M, De'Ath HD, Siddiqui M, Mehta C, Rasheed S, Bromilow J, et al. Obese patients have similar short-term outcomes to non-obese in laparoscopic colorectal surgery. World J Gastrointest Surg. 2015;7:261–266. doi: 10.4240/wjgs.v7.i10.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ortenzi M, Balla A, Ghiselli R, Vergari R, Silecchia G, Guerrieri E, et al. Minimally invasive approach to the adrenal gland in obese patients with Cushing's syndrome. Minim Invasive Ther Allied Technol. 2019;28:285–291. doi: 10.1080/13645706.2018.1536669. [DOI] [PubMed] [Google Scholar]
- 10.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 11.Dancea HC, Obradovic V, Sartorius J, Woll N, Blansfield JA. Increased complication rate in obese patients undergoing laparoscopic adrenalectomy. JSLS. 2012;16:45–49. doi: 10.4293/108680812X13291597715862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erbil Y, Barbaros U, Sari S, Agcaoglu O, Salmaslioglu A, Ozarmagan S. The effect of retroperitoneal fat mass on surgical outcomes in patients performing laparoscopic adrenalectomy: the effect of fat tissue in adrenalectomy. Surg Innov. 2010;17:114–119. doi: 10.1177/1553350610365703. [DOI] [PubMed] [Google Scholar]
- 13.Shariq OA, Fruth KM, Hanson KT, Cronin PA, Richards ML, Farley DR, et al. Metabolic syndrome is associated with increased postoperative complications and use of hospital resources in patients undergoing laparoscopic adrenalectomy. Surgery. 2018;163:167–175. doi: 10.1016/j.surg.2017.06.023. [DOI] [PubMed] [Google Scholar]
- 14.Al-Jalabneh T, Al-Shawabkeh O, Al-Gwairy I, Abu-Zeitoun O, Al-Njadat I, Al-Soudi M, et al. Laparoscopic versus open adrenalectomy: a retrospective comparative study. Med Arch. 2021;75:41–44. doi: 10.5455/medarh.2021.75.41-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heger P, Probst P, Hüttner FJ, Gooßen K, Proctor T, Müller-Stich BP, et al. Evaluation of open and minimally invasive adrenalectomy: a systematic review and network meta-analysis. World J Surg. 2017;41:2746–2757. doi: 10.1007/s00268-017-4095-3. [DOI] [PubMed] [Google Scholar]
- 16.Vidal O, Saavedra-Perez D, Martos JM, de la Quintana A, Rodriguez JI, Villar J, et al. Risk factors for open conversion of lateral transperitoneal laparoscopic adrenalectomy: retrospective cohort study of the Spanish Adrenal Surgery Group (SASG) Surg Endosc. 2020;34:3690–3695. doi: 10.1007/s00464-019-07264-1. [DOI] [PubMed] [Google Scholar]
- 17.Rodríguez Hermosa JI, Roig García J, Font Pascual JA, Recasens Sala M, Ortuño Muro P, Pardina Badía B, et al. Evolution of laparoscopic adrenal surgery in a general surgery department. Cir Esp. 2008;83:205–210. doi: 10.1016/s0009-739x(08)70548-7. [DOI] [PubMed] [Google Scholar]
- 18.Gök M, Öz B, Akcan A, Sözüer E. Laparoscopic bilateral adrenalectomy with the transabdominal lateral approach. Iran Red Crescent Med J. 2023;25:e2527 [Google Scholar]
- 19.Pędziwiatr M, Major P, Pisarska M, Natkaniec M, Godlewska M, Przęczek K, et al. Laparoscopic transperitoneal adrenalectomy in morbidly obese patients is not associated with worse short-term outcomes. Int J Urol. 2017;24:59–63. doi: 10.1111/iju.13241. [DOI] [PubMed] [Google Scholar]
- 20.Altın Ö, Sarı R. The effect of obesity in laparoscopic transperitoneal adrenalectomy. Turk J Surg. 2021;37:126–132. doi: 10.47717/turkjsurg.2021.4901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Constantinides VA, Christakis I, Touska P, Palazzo FF. Systematic review and meta-analysis of retroperitoneoscopic versus laparoscopic adrenalectomy. Br J Surg. 2012;99:1639–1648. doi: 10.1002/bjs.8921. [DOI] [PubMed] [Google Scholar]
- 22.Zonča P, Bužga M, Ihnát P, Martínek L. Retroperitoneoscopic adrenalectomy in obese patients: is it suitable? Obes Surg. 2015;25:1203–1208. doi: 10.1007/s11695-014-1475-8. [DOI] [PubMed] [Google Scholar]
- 23.Aranceta-Bartrina J, Pérez-Rodrigo C, Alberdi-Aresti G, Ramos-Carrera N, Lázaro-Masedo S. Prevalence of general obesity and abdominal obesity in the Spanish adult population (aged 25-64 years) 2014-2015: the ENPE study. Rev Esp Cardiol (Engl Ed) 2016;69:579–587. doi: 10.1016/j.rec.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 24.Paun D, Petris R, Ganescu R, Paun S, Vartic M, Beuran M. Outcome of laparoscopic adrenalectomy in obese patients. Maedica (Bucur) 2015;10:231–236. [PMC free article] [PubMed] [Google Scholar]
- 25.Coste T, Caiazzo R, Torres F, Vantyghem MC, Carnaille B, Do Cao C, et al. Laparoscopic adrenalectomy by transabdominal lateral approach: 20 years of experience. Surg Endosc. 2017;31:2743–2751. doi: 10.1007/s00464-016-4830-0. [DOI] [PubMed] [Google Scholar]
- 26.Chen Y, Scholten A, Chomsky-Higgins K, Nwaogu I, Gosnell JE, Seib C, et al. Risk factors associated with perioperative complications and prolonged length of stay after laparoscopic adrenalectomy. JAMA Surg. 2018;153:1036–1041. doi: 10.1001/jamasurg.2018.2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Natkaniec M, Dworak J, Pędziwiatr M, Pisarska M, Major P, Dembiński M, et al. Patients criteria determining difficulty of the laparoscopic lateral transperitoneal adrenalectomy. A retrospective cohort study. Int J Surg. 2017;43:33–37. doi: 10.1016/j.ijsu.2017.05.032. [DOI] [PubMed] [Google Scholar]
- 28.Thompson LH, Nordenström E, Almquist M, Jacobsson H, Bergenfelz A. Risk factors for complications after adrenalectomy: results from a comprehensive national database. Langenbecks Arch Surg. 2017;402:315–322. doi: 10.1007/s00423-016-1535-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kazaryan AM, Marangos IP, Røsok BI, Rosseland AR, Edwin B. Impact of body mass index on outcomes of laparoscopic adrenal surgery. Surg Innov. 2011;18:358–367. doi: 10.1177/1553350611403772. [DOI] [PubMed] [Google Scholar]
- 30.Economopoulos KP, Phitayakorn R, Lubitz CC, Sadow PM, Parangi S, Stephen AE, et al. Should specific patient clinical characteristics discourage adrenal surgeons from performing laparoscopic transperitoneal adrenalectomy? Surgery. 2016;159:240–248. doi: 10.1016/j.surg.2015.07.045. [DOI] [PubMed] [Google Scholar]