Abstract
Background
Despite being high-achieving students, many medical students face academic challenges, particularly during their first year of study. Research indicates that self-regulated learning, involving metacognitive processes and adaptive strategies, can positively influence academic achievement. This study aimed to assess the early learning and study skills of first-year medical students in an international medical school with the goal of developing a learner-centered educational intervention to promote self-regulated learning.
Methods
We conducted a retrospective analysis of the Learning and Study Skills Inventory (LASSI) questionnaire that was administered annually each August to first-year medical students from 2019 to 2022. The distribution of students across different percentile ranges for each selected variable was determined for each year and all years collectively. Students were counted within distinct percentile brackets (50th and below, between 51st and 75th, and above 75th ) for each variable.
Results
A total of 147 students completed the LASSI questionnaire over the 4-year time period. Using academic resources was the greatest concern, with 67% of students in the 50th or below percentile, followed by selecting the main idea (56%), motivation (51%), and concentration (50%). Attitude scored highest across all cohorts, scoring between 21.55 ± 0.73 and 26.49 ± 0.34. In comparing mean scores of LASSI variables across all cohorts, attitude, motivation, test-taking strategies, time management, and the use of academic resources differed significantly (p < 0.05).
Conclusion
LASSI data can provide an early picture of students’ support needs. We posit that early identification of student learning and study skills and areas of struggle can inform personalized educational interventions and programs to support first-year medical students.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-05850-z.
Keywords: Self-regulation, Study strategies, Medical students, Cognitive load, Anxiety
Background
Applicants to medical schools are historically high-achieving students. Acceptance is based on traditional markers of academic success, including high grade point averages (GPA) and scores on the Medical College Admission Test (MCAT), as well as attitudinal and behavioral fit as determined through interviews. The collected data feed into a rigorous selection process designed to ensure that the incoming students are well-equipped to navigate the challenges of medical education. Despite meeting these criteria, many students still underperform when faced with the demands of the first-year curriculum. As the pace of medical school studies ramps up, some students develop serious academic deficits [1]. Research on attrition rates in medical school show that students most often drop out in their first year, primarily due to academic difficulty and failure [1]. Like other educational transitions, entry into medical training presents a unique learning adjustment, which can be stressful. The shift from the predictable, didactic teaching in undergraduate education to the constructivist reality of the medical school “fire hose” of information is challenging for students worldwide [2–4]. Medical curricula employ compressed, volume-intensive coverage over limited time frames, providing little opportunity for repetition, revisitation, and consolidation [5]. Substantial time is spent acquiring facts, which are subsequently examined in multiple-choice style tests. Students can feel overwhelmed by the excessive amounts of factual knowledge that they are expected to retain and may realize that the study techniques used in undergraduate courses may be ineffective in medical school, often resulting in increased anxiety and frustration [6, 7]. Systematic reviews have identified high rates of anxiety, depression, and stress among medical students [8–11].
International students appear to have higher attrition rates, with one study citing the highest drop-out rate among students from the Middle East [1], which has been attributed to academic difficulty, absenteeism, social isolation, and English fluency problems [8–11]. In recent years, researchers have tried to identify the factors that contribute to underperformance in medical school. Several studies have explored the role of learning and study skills - the skills that assist students in processing and organizing academic information for effective learning [12], in predicting academic performance among students. These factors include information processing, test-taking strategies, attitude, motivation, and anxiety [3, 13, 14]. The majority of research was carried out in Western settings, but the significance of identified factors may vary across different populations. Cultural stressors, such as managing study during Ramadan fasting and committing to attending Friday prayers, may also impact study skills and academic performance for Middle Eastern students.
Self-regulated learning (SRL) is defined as a metacognitively guided proactive process “that students use to acquire academic skills, such as setting goals, selecting and developing learning strategies, and self-monitoring one’s effectiveness” [15, 16]. Self-regulated students have cyclical control of their learning process, whereby learning starts with motivation and preparation for the task to be performed, followed by adapting their behavior through learning strategies, such as re-reading, summarizing information, and developing concept maps [17]. To consolidate learning, the final steps involve self-reflection and self-evaluation, which inform a willingness to modify the cycle for future tasks [18]. This cycle allows learners to recognize that time and effort spent studying do not always translate into effective learning, such that accurate self-monitoring and regulation of effort are essential components of the learning process. The development of SRL in medical education is associated with higher academic achievement, improved clinical skills, and better mental health outcomes [13, 19]. Research demonstrates that shortcomings in learning and study skills contribute to academic difficulties during medical training. These studies also highlight the relationship between students’ study skills and their performance in both internal and external examinations [7, 20]. Time management and self-testing were observed to be strong predictors of academic performance, particularly in the first year of medical school [13]. Thus far, the literature offers limited insight into the exact learning skills students use and how they use them during their first year [21]. Gaining a better understanding of how students navigate the challenges of medical school can help educators pinpoint key learning skills for academic success. The purpose of this study was to understand the learning and study challenges faced by first-year medical students in an international medical school in the United Arab Emirates (UAE), with the goal of developing a learner-centered educational intervention to promote SRL [22].
Methods
Theoretical framework
This research is rooted in the theory of SRL, a proactive process through which students become masters of their own learning and academic performance and which is required for the successful acquisition of complex conceptual understanding [23, 24]. While several models of SRL exist, they all share fundamental assumptions concerning student learning [15]. Learners do not passively receive information but actively create their understanding through various skills and information sources [15, 16]. Control of the learning process promotes independence and responsibility. Self-regulated activities, such as time management and the judicious use of academic resources, serve as mediators influencing students’ overall performance [25].
Setting and participants
The UAE is a high-income country in the Middle East. Like many of its Gulf neighbors, the UAE has relied on expatriate medical professionals to meet population health needs [26]. It is estimated that almost 90% of the healthcare workforce is comprised of expatriates [27]. As such, national health systems strategies include increasing physician training capacity at both the undergraduate and postgraduate levels [28].
Participants in the study included first-year medical students at Khalifa University College of Medicine and Health Sciences, a post-graduate entry medical school established in 2019 in the UAE. Students completed bachelor’s degrees from countries worldwide and have varied cultural and educational backgrounds.
Survey instrument
The Learning and Study Skills Inventory (LASSI) questionnaire (3rd edition) is composed of 60 multiple-choice questions on a 5-point Likert scale (1 = not at all typical of me, 2 = not very typical of me, 3 = somewhat typical of me, 4 = fairly typical of me, and 5 = very much like me) and takes approximately 10 min to complete. It measures three latent factors of self-regulated learning: skill (subgroups of information processing, selecting the main idea and test strategies); will (subgroups of anxiety, attitude, and motivation); and self-regulation (subgroups of self-testing, concentration, time management, and using academic resources).
Table 1 includes the LASSI subscales. A score below the 50th percentile on any scale raises concern about that domain and indicates a need for a learning or behavioral intervention. A score above the 75th percentile on a scale is reassuring that this domain is not a source of academic concern (except for anxiety).
Table 1.
LASSI subscales and sample questions.
(adapted from Weinstein et al., 2002) [29]
| LASSI subscale | Description | Sample questions |
|---|---|---|
| Anxiety (ANX) | Degree of worry about coursework. |
I feel very panicky when I take a test. My mind wanders a lot when I study. |
| Attitude (ATT) | Students’ interests, goals and opinions about college and academic success. | I have a positive attitude about attending classes |
| Concentration (CON) | Strategies to stay focused and engagement in academic tasks. | My mind wanders a lot when I study. |
| Information processing (INP) | Students’ ability to organize information into meaningful pieces and bridge previous knowledge with new knowledge. | I try to find relationships between what I am learning and what I already know |
| Motivation (MOT) | Effort and self-discipline put into doing work and the ability to set academic goals and achieve them. | When work is difficult I either give up or study only the easy parts. |
| Selecting main ideas (SMI) | Students’ thinking skills for identifying important information. | When studying, I seem to get lost in the details and miss the important information. |
| Self-testing (SFT) | Strategies used to test knowledge acquired, one’s level of understanding and application of knowledge. | I try to think of possible test questions when studying my class material |
| Using Academic Resources (UAR) | Willingness to use academic resources, including tutors, that support meaningful learning and understanding. | When they are available, I go to study or review sessions |
| Test strategies (TST) | Strategies used to prepare for examinations | I have difficulty adapting my studying to different types of subjects |
| Time management (TMT) | How I manage my time and academic tasks | I set aside more time to study the subjects that are difficult for me. |
Data collection
From 2019 to 2022, an online version of the LASSI questionnaire was administered annually each August to first-year medical students at the beginning of the academic year as a routine part of the orientation process. The study was deemed exempt from institutional review board review with a waiver of informed consent by the Khalifa University Research Ethics Committee [H24-011] as all data were retrospective and de-identified.
Data analysis
Statistical analyses were carried out using R version 4.2.3. The distribution of students across different percentile ranges for each selected variable was determined for each year and all years collectively. Students were counted within distinct percentile brackets for each variable. Categories were the 50th percentile and below, between the 51st-75th percentiles, and above the 75th percentile. A descriptive table was generated with R to explore the distribution of variables across the different cohorts, and data was presented as the mean (standard error) and median (range) statistics for each variable. Probability values were generated using ANOVA tests to determine if the means of the variables differed significantly across the cohorts. Tukey’s post hoc test was used to determine the significance between specific years. A p-value of < 0.05 was considered statistically significant. The reliability of the instrument was tested using the Cronbach alpha coefficient.
Results
A total of 147 students completed the LASSI questionnaire over the 4-year time period (S1 Table). The mean age of participants was 24 years (SD = 3.2) and the majority of students were female (n = 106; 72%). The reliability of the LASSI subscales as a survey instrument was tested on the sample from 2019 (N = 26) and 2020 (N = 31) using Cronbach’s alpha. Alpha coefficients were between (0.72–0.78), which is acceptable in the social sciences domain [30, 31].
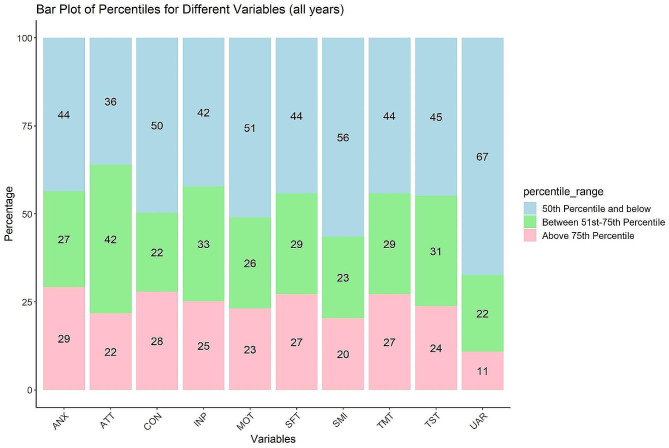
Figure 1 displays the distribution of students across different percentiles for various cognitive and behavioral variables. S1 Figure includes LASSI reports for individual cohorts. Overall, there were deficiencies in many of the scales. Several areas of concern were consistent across all cohorts. Using academic resources was the greatest concern, with 67% of students in the 50th or below percentile, followed by selecting the main idea (56%), motivation (51%), and concentration (50%). The S2 Table shows the number of students in each percentile category.
Fig. 1.
Aggregate percentile distribution of LASSI scores for all cohorts (2019–2022). The figure describes the aggregate scores for each of the LASSI domains for all cohorts combined. The Learning and Study Skills Inventory (LASSI) is a self-report questionnaire designed to assess students’ awareness of and use of learning and study skills. The LASSI provides scores across various domains (ANX- anxiety; ATT- attention; CON- concentration; INP- information processing; MOT- motivation; SFT- self-testing; SMI- selecting main ideas; TMT- time management; TST- test-taking strategies; UAR- using academic resources), each reflecting a specific aspect of a student’s approach to learning. Above the 75th percentile: Strengths are evident, and the student demonstrates a high level of competence in the assessed learning and study strategy. Between the 51st and 75th percentile: Competence is above average but may not reach the highest levels. There is room for improvement but also areas of strength. Below the 50th percentile: Indicates performance below the average level of the normative group. This may highlight areas where the student could benefit from enhancing their learning and study skills
Within the 75% percentile and above, 29% of the students reported anxiety- which corresponds with increased anxiety in these students. Notably, the cohort that started medical school in August 2020 during the peak of the COVID-19 pandemic scored lower in all domains. Specifically, there was a dramatic increase in students in the 50th percentile and lower, particularly in using academic resources (87%). High percentages of students were also in the 50th percentile or lower for motivation (77%), selecting main ideas (71%), attitude (68%), and concentration (68%).
Table 2 shows the mean scores and standard deviation across the studied variables. Attitude, concentration, time management, and using academic resources were the highest in the 2021 cohort, with means of 26.49 ± 0.34 (p < 0.001), 21.49 ± 0.73 (p = 0.001), 20.42 ± 0.68 (p = 0.002), and 19.64 ± 0.63 (p = 0.007), respectively. In contrast, motivation and test-taking strategies were highest in the 2022 cohort, with mean scores of 25.49 ± 0.46 (p < 0.001) and 23.36 ± 0.54 (p = 0.002), respectively.
Table 2.
Distribution of LASSI variables across different years
| 2019 (N = 26) | 2020 (N = 31) | 2021 (N = 45) | 2022 (N = 45) | Total N= (147) | p value | |
|---|---|---|---|---|---|---|
| 1. ANXIETY (ANX) | 0.098 | |||||
| Mean (SE) | 17.27 (1.22) | 18.58 (1.08) | 19.16 (0.92) | 20.89 (0.88) | 19.23 (0.51) | |
| Median (Range) | 17.00 (6.00, 29.00) | 19.00 (7.00, 30.00) | 19.00 (6.00, 30.00) | 21.00 (6.00, 30.00) | 19.00 (6.00, 30.00) | |
| 2. ATTITUDE (ATT) | < 0.001 | |||||
| Mean (SE) | 24.35 (0.70) | 21.55 (0.73) | 26.49 (0.34) | 25.67 (0.42) | 24.82 (0.30) | |
| Median (Range) | 25.00 (15.00, 28.00) | 21.00 (12.00, 28.00) | 26.00 (21.00, 30.00) | 26.00 (14.00, 30.00) | 26.00 (12.00, 30.00) | |
| 3. CONCENTRATION (CON) | 0.001 | |||||
| Mean (SE) | 18.92 (0.90) | 17.52 (0.89) | 21.49 (0.73) | 21.00 (0.68) | 20.05 (0.41) | |
| Median (Range) | 19.50 (9.00, 28.00) | 18.00 (7.00, 26.00) | 23.00 (6.00, 30.00) | 21.00 (8.00, 28.00) | 21.00 (6.00, 30.00) | |
| 4. INFORMATION PROCESSING (INP) | 0.31 | |||||
| Mean (SE) | 22.42 (0.94) | 21.61 (0.73) | 23.40 (0.58) | 23.00 (0.64) | 22.73 (0.35) | |
| Median (Range) | 23.50 (12.00, 30.00) | 21.00 (12.00, 28.00) | 23.00 (15.00, 30.00) | 24.00 (12.00, 30.00) | 23.00 (12.00, 30.00) | |
| 5. MOTIVATION (MOT) | < 0.001 | |||||
| Mean (SE) | 22.77 (0.81) | 22.48 (0.71) | 25.33 (0.48) | 25.49 (0.46) | 24.33 (0.31) | |
| Median (Range) | 22.50 (14.00, 29.00) | 23.00 (11.00, 29.00) | 25.00 (18.00, 30.00) | 26.00 (19.00, 30.00) | 24.00 (11.00, 30.00) | |
| 6. SELECTING MAIN IDEAS (SMI) | 0.103 | |||||
| Mean (SE) | 19.38 (1.02) | 19.84 (0.67) | 21.80 (0.60) | 20.87 (0.71) | 20.67 (0.37) | |
| Median (Range) | 18.50 (10.00, 29.00) | 20.00 (10.00, 25.00) | 22.00 (13.00, 30.00) | 21.00 (9.00, 29.00) | 21.00 (9.00, 30.00) | |
| 7. SELF-TESTING (SFT) | 0.075 | |||||
| Mean (SE) | 18.69 (0.91) | 17.84 (0.80) | 20.33 (0.76) | 20.24 (0.70) | 19.49 (0.40) | |
| Median (Range) | 18.00 (9.00, 28.00) | 17.00 (7.00, 28.00) | 21.00 (10.00, 30.00) | 21.00 (9.00, 29.00) | 20.00 (7.00, 30.00) | |
| 8. TEST TAKING STRATEGIES (TST) | 0.002 | |||||
| Mean (SE) | 20.65 (0.81) | 20.35 (0.65) | 22.02 (0.49) | 23.36 (0.54) | 21.84 (0.31) | |
| Median (Range) | 21.00 (14.00, 28.00) | 20.00 (11.00, 28.00) | 22.00 (14.00, 30.00) | 24.00 (15.00, 30.00) | 22.00 (11.00, 30.00) | |
| 9. TIME MANAGEMENT (TMT) | 0.002 | |||||
| Mean (SE) | 18.58 (0.94) | 16.55 (0.80) | 20.42 (0.68) | 19.87 (0.64) | 19.11 (0.39) | |
| Median (Range) | 18.00 (9.00, 29.00) | 17.00 (8.00, 25.00) | 20.00 (9.00, 30.00) | 20.00 (11.00, 28.00) | 19.00 (8.00, 30.00) | |
| 10. USING ACADEMIC RESOURCES (UAR) | 0.007 | |||||
| Mean (SE) | 17.81 (0.97) | 16.23 (0.70) | 19.64 (0.63) | 19.31 (0.76) | 18.50 (0.39) | |
| Median (Range) | 17.50 (11.00, 30.00) | 16.00 (9.00, 26.00) | 19.00 (7.00, 27.00) | 19.00 (7.00, 30.00) | 18.00 (7.00, 30.00) |
Data are expressed as mean (standard error) and median (range). p-values were generated with ANOVA
When comparing genders across all cohorts (females = 106 and males = 41), significant differences were found in anxiety, selecting main ideas, and test-taking strategies between sexes (p < 0.01) (Table 3). Males performed better in selecting main ideas and test-taking strategies and had less anxiety than their female counterparts.
Table 3.
Distribution of LASSI variables according to gender
| FEMALE (106) | MALE (41) | TOTAL (147) | p value | |
|---|---|---|---|---|
| Anxiety (ANX) | < 0.001 | |||
| Mean (SE) | 18.05 (0.61) | 22.29 (0.74) | 19.23 (0.51) | |
| Median (Range) | 18.00 (6.00, 30.00) | 23.00 (12.00, 30.00) | 19.00 (6.00, 30.00) | |
| Attitude (ATT) | 0.346 | |||
| Mean (SE) | 24.99 (0.35) | 24.37 (0.57) | 24.82 (0.30) | |
| Median (Range) | 26.00 (12.00, 30.00) | 25.00 (15.00, 29.00) | 26.00 (12.00, 30.00) | |
| Concentration (CON) | 0.319 | |||
| Mean (SE) | 20.30 (0.47) | 19.39 (0.82) | 20.05 (0.41) | |
| Median (Range) | 20.50 (8.00, 30.00) | 21.00 (6.00, 28.00) | 21.00 (6.00, 30.00) | |
| Information processing (INP) | 0.192 | |||
| Mean (SE) | 22.44 (0.42) | 23.46 (0.61) | 22.73 (0.35) | |
| Median (Range) | 23.00 (12.00, 30.00) | 24.00 (12.00, 30.00) | 23.00 (12.00, 30.00) | |
| Motivation (MOT) | 0.674 | |||
| Mean (SE) | 24.25 (0.37) | 24.54 (0.56) | 24.33 (0.31) | |
| Median (Range) | 24.00 (11.00, 30.00) | 25.00 (13.00, 30.00) | 24.00 (11.00, 30.00) | |
| Selecting main ideas (SMI) | 0.001 | |||
| Mean (SE) | 19.93 (0.44) | 22.59 (0.58) | 20.67 (0.37) | |
| Median (Range) | 20.00 (9.00, 30.00) | 23.00 (13.00, 29.00) | 21.00 (9.00, 30.00) | |
| Self-testing (SFT) | 0.592 | |||
| Mean (SE) | 19.62 (0.50) | 19.15 (0.61) | 19.49 (0.40) | |
| Median (Range) | 20.00 (7.00, 30.00) | 19.00 (10.00, 25.00) | 20.00 (7.00, 30.00) | |
| Test strategies (TST) | 0.002 | |||
| Mean (SE) | 21.25 (0.38) | 23.34 (0.49) | 21.84 (0.31) | |
| Median (Range) | 21.00 (11.00, 30.00) | 24.00 (18.00, 30.00) | 22.00 (11.00, 30.00) | |
| Time management (TMT) | 0.921 | |||
| Mean (SE) | 19.08 (0.43) | 19.17 (0.83) | 19.11 (0.39) | |
| Median (Range) | 19.00 (8.00, 30.00) | 20.00 (9.00, 29.00) | 19.00 (8.00, 30.00) | |
| Using Academic Resources (UAR) | 0.015 | |||
| Mean (SE) | 19.08 (0.47) | 16.98 (0.65) | 18.50 (0.39) | |
| Median (Range) | 18.50 (9.00, 30.00) | 18.00 (7.00, 24.00) | 18.00 (7.00, 30.00) |
Data are expressed as mean (standard error) and median (range). p-values were generated with ANOVA
Discussion
In this four-year long study exploring the learning and study skills of first-year medical students, data from LASSI helped identify key learning challenges. Overall, students struggled with using academic resources, selecting main topics, test-taking strategies, attitudes, and motivation. Many students were in the 50th percentile and below for all ten variables, suggesting the need for a multi-pronged intervention to support their learning. Our findings are consistent with research that shows that even high-achieving students can face new academic challenges when facing the demands of a rigorous medical school curriculum and may need interventions to support self-regulated learning skills [1, 2, 6]. In our study, the second cohort started medical school during the COVID-19 pandemic, which profoundly impacted every aspect of their educational experience. The rapid transition to online classes negatively impacted the socialization process and the availability of peer support [32–34]. For the remaining cohorts (2021 and 2022), there is a shift, with more students performing better and scoring above the 75th percentile. A possible explanation is that each new cohort had a more advanced peer group that could offer guidance and support before and during the orientation process, particularly around managing the cognitive load.
The use of academic resources persisted as an area of concern across all cohorts. We relate this issue to students having access to multiple and varying teaching materials, including textbooks, journal articles, PowerPoint presentations, question banks, videos, and online study aids, while still underinformed about how best to manage these resources or determine the best resource for specific study needs. This echoes findings from a recent study where medical students reported that the lack of guidance on the utilization of academic resources led to uncertainty, rumors, and a constant fear of missing out on important information among the student body [35]. Course directors play an important role in guiding students regarding the appropriate study aids. This will likely help ease anxiety as well as improve time management and academic performance. The confusion around resource management likely contributed to increased anxiety, another common variable across the cohorts. Compared to university students in non-medical majors, research has shown that medical students in their basic science academic years report alarmingly high rates of negative mental health conditions, such as anxiety, depression, and imposter syndrome [11, 36, 37]. Increased medical student anxiety during the COVID-19 pandemic is well documented in the medical literature [38–40].
Low scores in motivation and attitude among medical students, as seen in our surveys, have also been linked to stress and anxiety [42]. While a certain amount of stress may be helpful, excessive stress can cause amotivation and hinder learning [41]. Several studies have looked at the relationship between stress, motivation, and performance during medical school [42]. Stress, motivation, and poor academic performance can become part of a vicious cycle, whereby increasing stress leads to decreasing performance, which, in turn, increases stress [42, 43]. Learners who feel that they are unable to succeed academically perceive a lack of competence, driving them toward amotivation [41]. This suggests that learning activities that encourage intrinsic motivation and make learning more enjoyable, such as gamification or game-based learning interventions, can provide students with a sense of progress and accomplishment, thereby breaking the cycle [44].
Moreover, students can enter medical school with feelings of insecurity and inadequacy [45]. The term imposter syndrome (IS) was coined to describe a psychological state of inadequacy, whereby individuals dismiss their achievements and are unable to internalize success [46]. The prevalence of IS is high among medical students, residents, and practicing physicians, with some studies showing a prevalence of up to 60% [47]. IS can inhibit motivation and is associated with mental health problems, including anxiety, depression, and burnout [47]. IS tends to occur in times of transition [45], such as first-year medical school and may help to explain the low scores in the attitude, anxiety, and motivation domains among our student population. Given the high rates of IS in medical students, awareness and preventive strategies are needed, along with early interventions to prevent initial feelings of imposterism from progressing.
There is a large body of literature exploring gender differences in academic achievement, with inconclusive results [48, 49]. In our students, analysis of LASSI scores showed that male students outperformed females in the domains of selecting the main idea and test-taking strategies. Male students also exhibited significantly lower levels of anxiety. Several studies have shown that female medical students have higher anxiety than male medical students but tend to perform better on high-stakes examinations [48, 49]. Research suggests that females with high anxiety are more aware of their knowledge gaps and more motivated to study, whereas male students with high anxiety may be less aware of their knowledge limitations [49]. The differential responses to anxiety observed between male and female students suggest the need to develop individualized support strategies.
Through taking the LASSI, students acquired an insight into the attributes of self-regulation and learning. We taught the students how to interpret their scores and identify areas of strength and weakness to help tailor their study techniques to attain the desired learning outcomes. Students were also encouraged to discuss their results and create individualized learning plans with their academic advisors. Moreover, the findings were used to develop a longitudinal orientation program personalized to our students, first offered in 2022. In addition to sessions on time management, high-yield study skills, and test-taking strategies, a workshop for recognizing and dealing with IS is offered during orientation. Also, course directors are encouraged to identify the optimal academic resources early in the semester and to implement gamification or game-based learning into their courses when possible. Finally, a comprehensive well-being program was developed.
SRL is a proactive process through which students take control of and evaluate their own learning and academic performance. Design guidelines are needed to develop educational interventions to promote SRL in medical students. This could encompass structured training programs that explicitly teach SRL strategies, such as goal setting, self-monitoring, and self-reflection. Integration into the medical curriculum provides students with ongoing opportunities for practical application to reinforce these skills. Technology and digital tools can also be leveraged to support personalized learning. For example, digital platforms can provide real-time feedback, enabling students to set goals, monitor progress, and identify areas for improvement. Using e-portfolios can be an effective way for students to document their learning, reflect on their progress, and receive feedback from educators, fostering a personalized and self-regulated approach to learning. Lastly, incorporating assessment methods that provide students with feedback on their SRL practices can help them identify areas for improvement and refine their learning skills, ultimately enhancing their overall learning experience.
Limitations
This research has some limitations and these were acknowledged and addressed throughout the study. The LASSI is a self-report tool. Students can overestimate their strengths and underestimate their weaknesses, leading to inaccurate assessments. They may also provide answers they believe to be socially desirable rather than wholly accurate, particularly when discussing their study habits and motivation. Considering these limitations, efforts were undertaken to reduce the potential sources of bias. Students were provided with explanations regarding the purpose of administering the LASSI and how individual scores were not used to evaluate performance or ability; the data was used to support and enhance the overall student learning experience. The cross-sectional survey prevents the identification of any causal relationships. Further, to maintain anonymity and confidentiality, we did not link LASSI scores with performance in medical school coursework. The LASSI scores are based on norms derived from Western educational systems, primarily in the United States, and may not reflect the cultural and educational context of students in the Middle East. Finally, many factors beyond LASSI data can impact student learning and study skills and should be considered when designing educational interventions.
Conclusion
First-year medical students face multiple challenges. Student success courses are commonplace interventions designed to improve academic performance. However, one size does not fit all, and if we wish to improve student outcomes, we first need to understand our student population and the challenges they face. Gaining early insight into students’ learning habits, such as test-taking strategies, information processing, and self-regulatory tools like time management, self-testing, and concentration, can help inform customized interventions and provide individualized support. LASSI data can provide this early picture of students’ support needs. In adopting this comprehensive and student-centric approach, we create a more effective educational environment that addresses the individual needs of our diverse student body.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: S1 Table: Datasets.
Supplementary Material 2: S2 Table: Number of students within each percentile category (N = 147).
Supplementary Material 3: S1 Figure: Percentile distribution of LASSI scores for each cohort (2019–2022).
Acknowledgements
Not applicable.
Abbreviations
- LASSI
Learning and Study Skills Inventory
- SRL
Self regulated learning
- GPA
Grade point averages
- MCAT
Medical College Admission Test
- UAE
United Arab Emirates
- IS
Imposter syndrome
Author contributions
SO- Conceptualization, Supervision, Data Curation, Writing- original draft, Writing- reviewing and editing; CAH- Methodology, Writing- reviewing and editing; ZD- Writing- reviewing and editing; LOA- Writing- reviewing and editing; DP- Writing- reviewing and editing; HI- Conceptualization, Writing- original draft, Writing- reviewing and editing.
Funding
The authors received no internal/external funding for this project.
Data availability
Data is provided within the manuscript or supplementary information files.
Declarations
Ethics approval and consent to participate
The study was deemed exempt from institutional review board review by the Khalifa University Research Ethics Committee [H24-011] with waiver of informed consent as all data were retrospective and de-identified. All methods were performed following all relevant guidelines and regulations of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Authors’ information
SO is an Assistant Professor Department of Biological Sciences, Khalifa University College of Medicine and Health Sciences, Abu Dhabi, UAE. CAH is a ost-doctoral fellow, Department of Medical Sciences, Khalifa University College of Medicine and Health Sciences, Abu Dhabi, UAE. ZD is an Assistant Professor, Department of Medical Sciences, Khalifa University College of Medicine and Health Sciences, Abu Dhabi, UAE. LOA is a research associate, Department of Medical Sciences, Khalifa University College of Medicine and Health Sciences, Abu Dhabi, UAE. DP is Director of Operations, Khalifa University College of Medicine and Health Sciences, Abu Dhabi, UAE. HI is an Associate Professor, Department of Medical Sciences, Khalifa University College of Medicine and Health Sciences, Abu Dhabi, UAE.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Maher BM, Hynes H, Sweeney C, Khashan AS, O’Rourke M, Doran K, et al. Medical school attrition-beyond the statistics a ten year retrospective study. BMC Med Educ. 2013;13:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aaron S, Skakun E. Correlation of students’ characteristics with their learning styles as they begin medical school. Acad Med. 1999;74(3):260–2. [DOI] [PubMed] [Google Scholar]
- 3.Barbosa J, Silva Á, Ferreira MA, Severo M. Transition from Secondary School to Medical School: the role of self-study and self-regulated learning skills in freshman burnout. Acta Med Port. 2016;29(12):803–8. [DOI] [PubMed] [Google Scholar]
- 4.de Bruin ABH, Dunlosky J, Cavalcanti RB. Monitoring and regulation of learning in medical education: the need for predictive cues. Med Educ. 2017;51(6):575–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hernández-Torrano D, Ali S, Chan CK. First year medical students’ learning style preferences and their correlation with performance in different subjects within the medical course. BMC Med Educ. 2017;17(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sayer M, Chaput De Saintonge M, Evans D, Wood D. Support for students with academic difficulties. Med Educ. 2002;36(7):643–50. [DOI] [PubMed] [Google Scholar]
- 7.Cleland J, Arnold R, Chesser A. Failing finals is often a surprise for the student but not the teacher: identifying difficulties and supporting students with academic difficulties. Med Teach. 2005;27(6):504–8. [DOI] [PubMed] [Google Scholar]
- 8.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354–73. [DOI] [PubMed] [Google Scholar]
- 9.Picton A. Work-life balance in medical students: self-care in a culture of self-sacrifice. BMC Med Educ. 2021;21(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Healy C, Ryan Á, Moran CN, Harkin DW, Doyle F, Hickey A. Medical students, mental health and the role of resilience - A cross-sectional study. Med Teach. 2023;45(1):40–8. [DOI] [PubMed] [Google Scholar]
- 11.Thompson G, McBride RB, Hosford CC, Halaas G. Resilience among medical students: the role of coping style and social support. Teach Learn Med. 2016;28(2):174–82. [DOI] [PubMed] [Google Scholar]
- 12.Opperman I, Mason HD. Structure and norms of the Learning and Study Strategy Inventory: a comparison of South African and American samples. J Psychol Afr. 2020;30(3):187–91. [Google Scholar]
- 13.West C, Sadoski M. Do study strategies predict academic performance in medical school? Med Educ. 2011;45(7):696–703. [DOI] [PubMed] [Google Scholar]
- 14.Augustin M. How to learn effectively in medical school: test yourself, learn actively, and repeat in intervals. Yale J Biol Med. 2014;87(2):207–12. [PMC free article] [PubMed] [Google Scholar]
- 15.Zimmerman BJ. Becoming a self-regulated learner: an overview. Theory into Pract. 2002;41(2):64–70. [Google Scholar]
- 16.Zimmerman BJ. Investigating self-regulation and motivation: historical background, methodological developments, and future prospects. Am Educ Res J. 2008;45(1):166–83. [Google Scholar]
- 17.Boyd T, Besche H, Goldhammer R, Alblooshi A, Coleman BI. First-year medical students’ perceptions of a self-regulated learning-informed intervention: an exploratory study. BMC Med Educ. 2022;22(1):821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siqueira MAM, Gonçalves JP, Mendonça VS, Kobayasi R, Arantes-Costa FM, Tempski PZ, et al. Relationship between metacognitive awareness and motivation to learn in medical students. BMC Med Educ. 2020;20(1):393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tseng AS, Edwards C, Rawls M, McGinn M, Wieghard N, Santen SA, et al. A mixed methods exploration of the emergence of goal orientation in medical students’ individualized learning plans. Med Teach. 2023;45(6):588–95. [DOI] [PubMed] [Google Scholar]
- 20.Cleland J, Mackenzie RK, Ross S, Sinclair HK, Lee AJ. A remedial intervention linked to a formative assessment is effective in terms of improving student performance in subsequent degree examinations. Med Teach. 2010;32(4):e185–90. [DOI] [PubMed] [Google Scholar]
- 21.Greenberg A, Olvet DM, Brenner J, Zheng B, Chess A, Schlegel EF et al. Strategies to support self-regulated learning in integrated, student-centered curricula. Med Teach. 2023:1–8. [DOI] [PubMed]
- 22.Durning SJ, Cleary TJ, Sandars J, Hemmer P, Kokotailo P, Artino AR. Perspective: viewing strugglers through a different lens: how a self-regulated learning perspective can help medical educators with assessment and remediation. Acad Med. 2011;86(4):488–95. [DOI] [PubMed] [Google Scholar]
- 23.Greene JA, Azevedo R. A macro-level analysis of SRL processes and their relations to the acquisition of a sophisticated mental model of a complex system. Contemp Educ Psychol. 2009;34(1):18–29. [Google Scholar]
- 24.Panadero E. A review of self-regulated learning: six models and four directions for research. Front Psychol. 2017;8:422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cutrer WB, Miller B, Pusic MV, Mejicano G, Mangrulkar RS, Gruppen LD, et al. Fostering the development of master adaptive learners: a conceptual model to guide skill acquisition in medical education. Acad Med. 2017;92(1):70–5. [DOI] [PubMed] [Google Scholar]
- 26.Alameri H, Hamdy H, Sims D. Medical education in the United Arab Emirates: challenges and opportunities. Med Teach. 2021;43(6):625–32. [DOI] [PubMed] [Google Scholar]
- 27.Ibrahim H, Nair SC, Shaban S, El-Zubeir M. Reducing the physician workforce crisis: Career choice and graduate medical education reform in an emerging arab country. Educ Health (Abingdon). 2016;29(2):82–8. [DOI] [PubMed] [Google Scholar]
- 28.Awamleh R. Perspective—UAE Future Government: the emerging pillars. Future Governments: Emerald Publishing Limited; 2019. pp. 43–50. [Google Scholar]
- 29.Weinstein CE, Palmer DR. User’s manual for those administering the learning and study strategies Inventory. Clearwater, FL: H&H Publishing; 2002. [Google Scholar]
- 30.Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Connelly LM. Cronbach’s Alpha. MedSurg Nursing. 2011 2011 January-February:45+. [PubMed]
- 32.O’Sullivan S, Campos LA, Baltatu OC, Involve Me, Learn I. Active learning in a Hybrid Medical Biochemistry First Year Course on an american-style MD program in the UAE. Med Sci Educ. 2022;32(3):703–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dimassi Z, Chaiban L, Zgheib NK, Sabra R. Re-conceptualizing medical education in the post-COVID era. Med Teach. 2023:1–8. [DOI] [PubMed]
- 34.O’Sullivan SM, Khraibi AA, Chen W, Corridon PR. Lessons learned transitioning from traditional premedical and medical education to E-learning platforms during the COVID-19 pandemic within the United Arab Emirates. J Med Educ Curric Dev. 2021;8:23821205211025861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weber J, Skodda S, Muth T, Angerer P, Loerbroks A. Stressors and resources related to academic studies and improvements suggested by medical students: a qualitative study. BMC Med Educ. 2019;19:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazurkiewicz R, Korenstein D, Fallar R, Ripp J. The prevalence and correlations of medical student burnout in the pre-clinical years: a cross-sectional study. Psychol Health Med. 2012;17(2):188–95. [DOI] [PubMed] [Google Scholar]
- 37.Salana K, Maty S, Hage R. Alive and well: Encouraging Long Term Health Habits through Implementation of Student Driven Wellness Programs in Medical Schools. Glob Adv Health Med. 2020;9:2164956120973622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alshehri A, Alshehri B, Alghadir O, Basamh A, Alzeer M, Alshehri M, et al. The prevalence of depressive and anxiety symptoms among first-year and fifth-year medical students during the COVID-19 pandemic: a cross-sectional study. BMC Med Educ. 2023;23(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jupina M, Sidle MW, Rehmeyer Caudill CJ. Medical student mental health during the COVID-19 pandemic. Clin Teach. 2022;19(5):e13518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mittal R, Su L, Jain R. COVID-19 mental health consequences on medical students worldwide. J Community Hosp Intern Med Perspect. 2021;11(3):296–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schumacher DJ, Englander R, Carraccio C. Developing the master learner: applying learning theory to the learner, the teacher, and the learning environment. Acad Med. 2013;88(11):1635–45. [DOI] [PubMed] [Google Scholar]
- 42.Dyrbye LN, Thomas MR, Shanafelt TD, editors. Medical student distress: causes, consequences, and proposed solutions. Mayo Clinic Proceedings; 2005: Elsevier. [DOI] [PubMed]
- 43.Kötter T, Wagner J, Brüheim L, Voltmer E. Perceived medical school stress of undergraduate medical students predicts academic performance: an observational study. BMC Med Educ. 2017;17(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chang TP, Doughty CB, Mitchell D, Rutledge C, Auerbach MA, Frisell K, et al. Leveraging quick response code technology to facilitate simulation-based leaderboard competition. Simul Healthc. 2018;13(1):64–71. [DOI] [PubMed] [Google Scholar]
- 45.LaDonna KA, Ginsburg S, Watling C. Rising to the level of your incompetence: what physicians’ self-assessment of their performance reveals about the imposter syndrome in medicine. Acad Med. 2018;93(5):763–8. [DOI] [PubMed] [Google Scholar]
- 46.Clance PR, Imes SA. The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention. Psychotherapy: Theory Res Pract. 1978;15(3):241. [Google Scholar]
- 47.Gottlieb M, Chung A, Battaglioli N, Sebok-Syer SS, Kalantari A. Impostor syndrome among physicians and physicians in training: a scoping review. Med Educ. 2020;54(2):116–24. [DOI] [PubMed] [Google Scholar]
- 48.Cassady JC, Johnson RE. Cognitive test anxiety and academic performance. Contemp Educ Psychol. 2002;27(2):270–95. [Google Scholar]
- 49.Colbert-Getz JM, Fleishman C, Jung J, Shilkofski N. How do gender and anxiety affect students’ self-assessment and actual performance on a high-stakes clinical skills examination? Acad Med. 2013;88(1):44–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: S1 Table: Datasets.
Supplementary Material 2: S2 Table: Number of students within each percentile category (N = 147).
Supplementary Material 3: S1 Figure: Percentile distribution of LASSI scores for each cohort (2019–2022).
Data Availability Statement
Data is provided within the manuscript or supplementary information files.