ABSTRACT
This study compared mandibular distraction and vertical ramus osteotomy in terms of their effectiveness at increasing access to the cranial base and distal internal carotid artery. Five fresh–frozen cadavers were used to obtain a total of ten cranial base exposures. The following two techniques were evaluated on each of the ten exposures: (1) anterior distraction of the mandible without violation of the temporomandibular joint capsule, and (2) vertical ramus osteotomy of the mandible with distraction of the proximal and distal segment. The neutrally positioned mandible with the condyle seated in the glenoid fossa served as the control. The area of surgical access defined by bony and cartilaginous landmarks was determined for each technique using the nondistracted control as a baseline.
The vertical ramus osteotomy group provided greater increase in surgical access with approximately a 99.64 % increase compared with the control and a mean area of exposure of 14.653 cm2. Mandibular distraction provided only a 28.32 % increase with a mean area of 9.252 cm2. The control or nondistracted baseline mean area of exposure was 7.214 cm2. Vertical ramus osteotomy significantly increased access to cranial base vascular lesions with minimal morbidity. It afforded greater and more reliable access than that achieved by the mandibular distraction technique. The procedure can be completed rapidly with no additional skin incisions.
Keywords: Mandibular osteotomy, closed carotid artery trauma, carotid artery aneurysm, reconstructive arterial surgery, endarterectomy
Surgical treatment of vascular lesions in Zone III, specifically those involving the distal internal carotid artery (ICA), are exceptionally challenging because exposure is limited. Zone III is defined as the area from the angle of the mandible to the tip of the mastoid process. Common vascular lesions include penetrating or blunt trauma, aneurysms, atherosclerosis, and fibromuscular dysplasia. Although surgical exposure may be adequate to visualize the pathology, the access is insufficient for the surgical manipulation needed for optimal repair due to the bony interference of the angle of the mandible and the mastoid process (Fig. 1). The angle of the mandible further interferes with adequate visualization of the cranial nerves in this region.
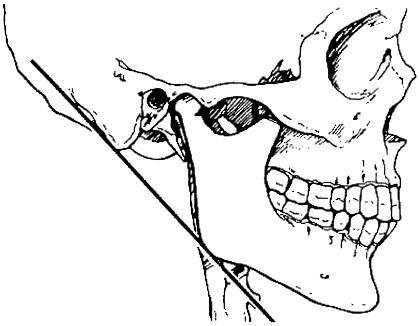
Figure 1.
Highlighted area represents the area of surgical access as defined by bony and cartilaginous landmarks and a line drawn from the tip of the mastoid to the angle of the mandible. The ramus of the mandible overlies most of the distal internal carotid artery.
Various techniques designed to minimize these bony restrictions have been described. However, many of these techniques involve significant surgical morbidity, such as transection of the inferior alveolar nerve, facial nerve paralysis, and oral contamination. The two most widely used techniques, namely mandibular subluxation and mandibular vertical ramus osteotomy (VRO), have been associated with low rates of surgical morbidity. The effectiveness of these techniques has been detailed in case reports, but no quantitative data are available for comparisons. The purpose of this study was to quantitate the area of surgical access to the cranial base in Zone III afforded by mandibular subluxation (distraction) and VRO.
METHODS AND MATERIALS
Five fresh–frozen cadavers were used to obtain a total of ten cranial base/ICA exposures. Two techniques for exposure of the cranial base were evaluated on each of the ten sides: (1) anterior distraction of the mandible without violation of the temporomandibular joint (TMJ) capsule, and (2) VRO of the mandible with distraction of the distal segment and rotation of the condylar segment. The neutrally positioned condyle served as the control.
Quantitation of the surgical access was determined using foil templates with bony and cartilaginous boundaries. The superior boundary was formed by the external auditory canal, posterior articular eminence, and posterior aspect of the mandibular condyle. The inferior boundary was a tangential line extending from the anterior–inferior to the posterior–inferior prominence of the mandibular angle. The anterior boundary was the posterior border of the mandible. Finally, the posterior boundary was formed by the external auditory canal and the anterior portion of the mastoid process.
The overlying soft tissue structures were dissected down to the level of the TMJ capsule leaving the masseter, temporalis, and buccinator muscles intact. The sternocleidomastoid muscle was separated from the mastoid process to facilitate the fabrication of the foil templates.
In the nondistracted control group, the condyles were seated into the glenoid fossa and the mandible was placed into occlusion. When no dentition or dentures were available, the interarch distance was maintained at 25 mm. Outlines of the baseline area were recorded using acetate transparencies over the previously described landmarks.
In the mandibular distraction group, the mandible was distracted anteriorly into maximal protrusion while the integrity of the TMJ capsule was preserved. The area was outlined and recorded as described above.
In the VRO group, the masseter muscle was elevated from the ramus. An osteotomy was completed using a reciprocating saw from the midsigmoid notch (with a slight curvature) to a point about 4 mm posterior to the antilingular prominence, which curved anteriorly to the inferior border of the mandible (Fig. 2). The medial pterygoid muscle was elevated from the proximal segment, allowing the condylar segment to be rotated laterally, anteriorly, and superiorly over the lateral surface of the ramus while the condyle was maintained in the glenoid fossa. The distal segment of the ramus was distracted anteriorly (Figs. 3, 4, and 5), and an acetate transparency was used to record the exposure area.
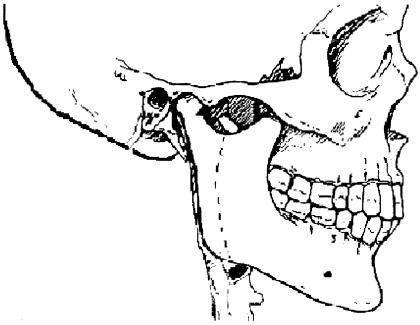
Figure 2.
The broken line indicates where the vertical ramus osteotomy is made. It extends from the depth of the sigmoid notch to the angle of the mandible.
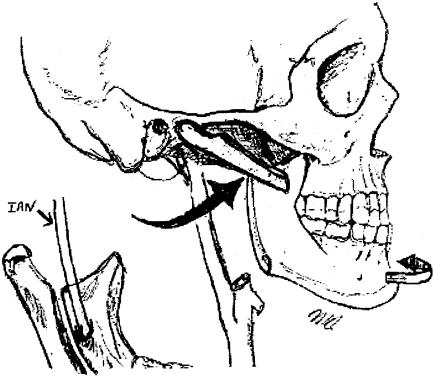
Figure 3.
The vertical ramus osteotomy and the distal segment retracted anteriorly and to the contralateral side (open arrow). The proximal segment is retracted anteriorly and superiorly (solid arrow). The inferior alveolar nerve (IAN) remains intact in the distal segment.
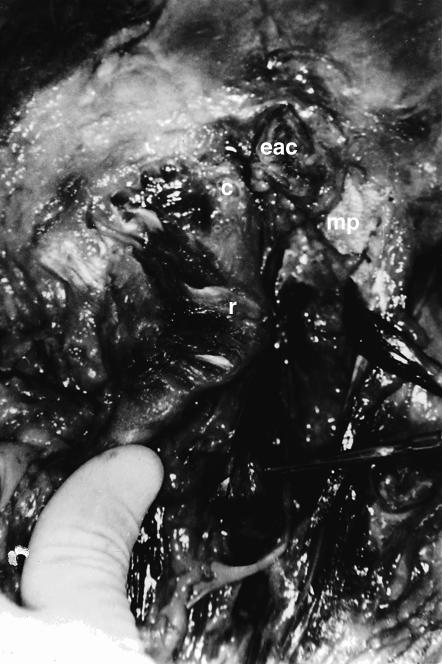
Figure 4.
Cadaveric specimen demonstrating anatomical relationship of the mandibular condyle (c) and ramus (r), the external auditory canal (eac), and the mastoid process (mp).
Figure 5.
Cadaveric specimen demonstrating the increase in access obtained with the VRO technique. The mandibular condyle (c) has been separated and swung forward from the ramus (r). eac, external auditory canal; a, internal carotid artery; b, carotid bifurcation.
All acetate tracings of the exposure area were scanned into a computer using a Hewlett–Packard ScanJet 6300Cxi. The area (cm2) of the digitized image was determined with a custom mathematical program created specifically for this task (created by Owen Murphy, Ph.D., Chairman, Computer Science Department, California State University, San Bernardino).
RESULTS
Table 1 shows the area of access in cm2 obtained for each of the cranial base exposures. The mean area of access for the control group was 7.214 cm2 (S.D.= 0.451, std. error = 0.143, range = 6.503 to 7.773). The mean area for the distraction group was 9.252 cm2 (S.D. = 0.734, std. error = 0.232, range = 7.896 to 10.541). The area of surgical access was greater in the VRO group with a mean area of 14.653 cm2 (S.D. = 1.251, std. error = .370, range = 12.489 to 16.705). Student's t–tests were used to compare the groups (control to test groups and distraction to osteotomy group), and all comparisons were significant (p < 0.01).
Table 1.
Area of Surgical Access in cm2
| Specimen | Side | Control | Distraction | Vertical Ramus Osteotomy |
| 1 | Right | 7.065 | 8.662 | 15.032 |
| Left | 7.508 | 9.726 | 16.705 | |
| 2 | Right | 7.03 | 8.814 | 14.765 |
| Left | 7.525 | 10.541 | 15.295 | |
| 3 | Right | 6.503 | 9.037 | 14.765 |
| Left | 6.643 | 7.896 | 12.489 | |
| 4 | Right | 7.773 | 9.158 | 13.523 |
| Left | 7.659 | 9.897 | 14.372 | |
| 5 | Right | 7.565 | 9.207 | 13.825 |
| Left | 6.865 | 9.585 | 14.039 | |
| Mean | 7.214 | 9.252 | 14.653 | |
| Standard Deviation | 0.451 | 0.734 | 1.251 | |
| Standard Error | 0.143 | 0.232 | 0.37 | |
| Range | 6.053–7.773 | 7.896–10.541 | 12.489–16.705 |
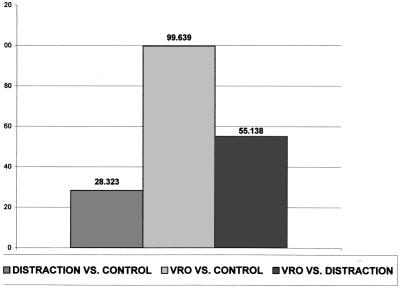
Table 2 illustrates the mean percentage increase in area of surgical access among the groups. The mean increase in area relative to the control was 28.32 % for the distraction group and 99.64 % for the VRO group. The VRO group demonstrated a mean increase in surgical access of 55.14 % relative to the distraction group (Fig. 6).
Table 2.
Percent Increase in Surgical Exposure
| Specimen | Side | Distraction vs. Control | Vertical Ramus Osteotomy vs. Control | Vertical Ramus Osteotomy vs. Distraction |
| 1 | Right | 22.038 | 112.77 | 73.539 |
| Left | 29.542 | 122.5 | 65.022 | |
| 2 | Right | 25.377 | 110.21 | 67.517 |
| Left | 40.079 | 103.26 | 45.1 | |
| 3 | Right | 18.862 | 88.002 | 58.169 |
| Left | 38.966 | 129.06 | 64.833 | |
| 4 | Right | 29.22 | 87.649 | 45.216 |
| Left | 17.818 | 70.269 | 45.518 | |
| 5 | Right | 21.705 | 82.749 | 50.157 |
| Left | 39.621 | 89.934 | 36.305 | |
| Mean | 28.232 | 99.639 | 55.138 | |
| Standard Deviation | 2.735 | 5.969 | 3.893 | |
| Standard Error | 8.649 | 18.867 | 12.311 |
Figure 6.
Bar graph illustrating the percentage increase in surgical access for the distraction and VRO groups versus the control group and for the VRO group versus the distraction group.
DISCUSSION
High ICA lesions (Zone III) require increased distal exposure to a level at or near the cranial base. Various techniques to gain additional exposure have been described, but quantitative data are lacking. Furthermore, many of these techniques are associated with significant rates of surgical morbidity.
Pellegrini and associates,1 Purdue and colleagues,2 and Fisch et al3 advocate radical mastoidectomy via preauricular and posterior auricular incisions in addition to the incision described by De Palma4 (an incision from behind the ear lobe into the neck lines inferiorly). The removal of a portion of the mastoid bone and release of the facial nerve to the stylomastoid foramen allow distal exposure of the ICA in the petrous portion of the temporal bone. This technique, however, is associated with facial nerve paralysis and, in the technique described by Fisch, sacrifice of middle ear function.3
As described by Dichtel and colleagues5 and McGregor and MacDonald,6 lateral mandibulotomy requires an additional facial incision so that the mandible can be sectioned anterior to the mental foramen. The mylohyoid muscle is incised so that the mandible can be retracted anteriorly and superiorly. The major drawback to this technique is the inevitable oral contamination, which presents a significant risk when repair of the lesion involves vascular grafts.
As advocated by Batzdorf and Gregarious,7 combined horizontal ramus and vertical body mandibular osteotomies result in trans–section of the inferior alveolar nerve (IAN). The authors state that the anesthesia of the lower lip and chin associated with trans–section of the IAN almost always recovers within 3 months. However, this statement has been shown to be inaccurate, especially in the elderly who are disproportionately afflicted with vascular lesions.8
As proposed by Shaha and associates,9 the posterolateral approach is quite time consuming. It requires sacrifice of the sternocleidomastoid and posterior belly of the digastric muscles, as well as the sublingual gland. Furthermore, the angle and ramus of the mandible still interfere with access and retraction is required.
As described by Fry and Fry10 and Fischer and associates,11 mandibular subluxation (anterior and contralateral distraction) increases exposure to the cranial base by transforming the triangular operating field into a rectangular field. Fry and Fry also state that an additional 1.5 to 2 cm of distal exposure can be achieved with this technique.9 However, the increase in exposure is variable and unpredictable.7, 11, 12, 13 Fischer and associates11 incorrectly state that distraction of the mandibular condyle 10 to 5 mm anteriorly displaces the mandibular ramus 20 to 30 mm. The technique of subluxation requires the placement of arch bars,10 transnasal and circum–mandibular wiring,11, 14 diagonal interdental wiring,14, 15 or use of Steinmann pins and jaw wiring15 to maintain the distraction position forward and to the contralateral side.
Disadvantages of mandibular subluxation include the possibility of passing beyond a physiologic translation of the condyle resulting in a pathologic dislocation associated with the potential for long–term TMJ pain and dysfunction.11, 16 In addition, rare cases of contralateral vocal cord paralysis and cerebral infarction caused by impingement of the recurrent laryngeal nerve and carotid artery between the angle of the mandible and the transverse vertebral process have been reported.11
VROs have been used by oral and maxillo–facial surgeons17 for many years and are associated with minimal surgical morbidity. Mandibular VRO for access to Zone III vascular lesions was first described by Welsh et al18 in 1981 and was further advocated by Larsen and Smead16 in 1992. The incidence of IAN paresthesia is less than 1 to 2 %.19, 20
The VRO has several advantages compared with other mandibular osteotomies (i.e., horizontal ramus,7 lateral mandibular,5, 6 and vertical body7). First, it uses the same surgical incision for carotid artery exploration. Second, there is no intraoral contamination. Third, it does not require postoperative intermaxillary fixation. In addition, there is little risk of damaging the IAN whereas the incidence approaches 100 % with other osteotomies.16 Finally, it can be performed in less time than the other osteotomies.
As described by Boyne,21 free condylar graft technique involves a VRO followed by disarticulation of the condyle. This technique affords excellent access but is more radical and potentially is associated with greater surgical morbidity than VRO with retraction of the osteotomized segments.
Of all the techniques described for increasing access to distal ICA lesions, mandibular subluxation and VRO are effective and associated with little surgical morbidity. VRO has been hailed as affording superior access.16, 17, 22 To date, however, no quantitative data were available to support this claim.
In this study, anterior distraction of the mandible without violation of the TMJ yielded an average of 28 % more surgical exposure than no surgical manipulation. VRO with retraction of the osteotomized segments provided an average of 99.7 % more surgical exposure than no surgical manipulation and more than 55 % more surgical access than mandibular distraction.
One reason that mandibular distraction yields less surgical access may be attributable to existing TMJ pathology. Restricted range of motion from an internal derangement limits translation and lateral excursion and therefore the extent of distraction. If the articular eminence is steep, the translation of the condyle is mostly in a vertical direction limiting the amount of forward distraction. Aggressive distraction may yield a pathologic dislocation of the condyle with the potential for long–term morbidity.
CLINICAL APPLICATION
The surgical technique of VRO may be accomplished with either oral or nasotracheal intubation; there is no need for a tracheostomy. The patient is positioned supine with a small roll under the shoulder to provide mild extension. Using a standard carotid endarterectomy (medial sternocleidomastoid) incision, the angle of the mandible may be adequately reached.4, 11, 16, 23
In some circumstances, the standard parotid–type incision, which incorporates a pre– and postauricular incision with the sternocleidomastoid (SCM), or a horizontal ramus incision may be used.1, 2, 24 Alternatively, the standard horizontal ramus incision (which begins at the tragus and progresses two finger–breadths below the posterior angle of the mandible and forward parallel to the inferior border of the mandible) may be used with or without extension downward along the SCM.3, 9, 18 Incisions behind the tragus place the facial nerve at less risk, with the exception of the horizontal ramus incision where the marginal mandibular branch of the facial nerve is manipulated. With extensive dissection of the mandibular angle, the facial trunk also may need to be dissected free and gently retracted. The IAN is ventral to the VRO and is at little risk of injury (Figs. 2 and 3). At the conclusion of surgery, the osteotomy is secured with standard craniofacial microplate fixation.
CONCLUSION
VRO with retraction of both proximal and distal mandibular segments affords superior surgical access to ICA pathology in Zone III than can be achieved by mandibular distraction techniques. VRO also is much less dependent on variations in TMJ anatomy and pathology than mandibular distraction techniques. VRO has a long–standing record of low surgical morbidity and can be accomplished with little additional surgical time. This technique may be considered when contemplating surgical treatment of lesions in Zone III.
REFERENCES
- Pellegrini RV, Manzetti GW, DiMarco RF, Bekoe S, Arena SA, Marrangoni AG. The direct surgical management of lesions of the high internal carotid artery. J Cardiovasc Surg (Torino) 1984;25:29–35. [PubMed] [Google Scholar]
- Purdue GF, Pellegrini RV, Arena S. Aneurysms of the high internal carotid artery: a new approach. Surgery. 1981;89:268–270. [PubMed] [Google Scholar]
- Fisch UP, Oldring DJ, Senning A. Surgical therapy of internal carotid artery lesions of the skull base and temporal bone. Otolaryngol Head Neck Surg. 1980;88:548–554. doi: 10.1177/019459988008800507. [DOI] [PubMed] [Google Scholar]
- DePalma RG. Optimal exposure of the internal carotid artery for endarterectomy. Surg Gynecol Obstet. 1977;144:249–250. [PubMed] [Google Scholar]
- Dichtel WJ, Miller RH, Feliciano DV, Woodson GE, Hurt J. Lateral mandibulotomy: a technique of exposure for penetrating injuries of the internal carotid artery at the base of the skull. Laryngoscope. 1984;94:1140–1144. doi: 10.1288/00005537-198409000-00002. [DOI] [PubMed] [Google Scholar]
- McGregor IA, MacDonald DG. Mandibular osteotomy in the surgical approach to the oral cavity. Head Neck Surg. 1983;5:457–462. doi: 10.1002/hed.2890050512. [DOI] [PubMed] [Google Scholar]
- Batzdorf U, Gregorius FK. Surgical exposure of the high cervical carotid artery: experimental study and review. Neurosurgery. 1983;13:657. doi: 10.1227/00006123-198312000-00007. [DOI] [PubMed] [Google Scholar]
- Cooper BY, Sessle GJ. Anatomy, physiology, and pathophysiology of trigeminal system paresthesias and dysesthesias. Oral Maxillofac Surg Clin N Am. 1992;4:297–322. [Google Scholar]
- Shaha A, Phillips T, Scalea T, et al. Exposure of the internal carotid artery near the skull base: the posterolateral anatomic approach. J Vasc Surg. 1988;8:618–622. doi: 10.1067/mva.1988.avs0080618. [DOI] [PubMed] [Google Scholar]
- Fry RE, Fry WJ. Extracranial carotid artery injuries. Surgery. 1980;88:581–587. [PubMed] [Google Scholar]
- Fisher DF Jr, Clagett GP, Parker JI, et al. Mandibular subluxation for high carotid exposure. J Vasc Surg. 1984;1:727–733. [PubMed] [Google Scholar]
- Goldsmith MM 3rd, Postma DS, Jones FD. The surgical exposure of penetrating injuries to the carotid artery at the skull base. Otolaryngol Head Neck Surg. 1986;95(3 Pt 1):278–284. doi: 10.1177/01945998860953P103. [DOI] [PubMed] [Google Scholar]
- Balagura S, Carter JB, Bossett DL. Surgical approach to the high subcranial internal carotid artery. Neurosurgery. 1985;16:402–405. doi: 10.1227/00006123-198503000-00022. [DOI] [PubMed] [Google Scholar]
- Frim DM, Padwa B, Buckley D, Crowell RM, Ogilvy CS. Mandibular subluxation as an adjunct to exposure of the distal internal carotid artery in endarterectomy surgery [technical note]. J Neurosurg. 1995;83:926–928. doi: 10.3171/jns.1995.83.5.0926. [DOI] [PubMed] [Google Scholar]
- Dossa C, Shepard AD, Wolford DG, Reddy DJ, Ernst CB. Distal internal carotid exposure: a simplified technique for temporary mandibular subluxation. J Vasc Surg. 1990;12:319–325. [PubMed] [Google Scholar]
- Larsen P, Smead WL. Vertical ramus osteotomy for improved exposure of the distal internal carotid artery: a new technique. J Vasc Surg. 1992;15:226–231. doi: 10.1067/mva.1992.30620. [DOI] [PubMed] [Google Scholar]
- Caldwell JB, Letterman GS. Vertical osteotomy in the mandibular rami for correction of prognathism. J Oral Surg. 1954;12:185–202. [PubMed] [Google Scholar]
- Welsh P, Pradier R, Repetto R. Fibromuscular dysplasia of the distal cervical internal carotid artery. J Cardiovasc Surg (Torino) 1981;22:321–326. [PubMed] [Google Scholar]
- Hall HD, Chase DC, Payor LG. Evaluation and refinement of the vertical subcondylar osteotomy. J Oral Surg. 1975;33:333–341. [PubMed] [Google Scholar]
- Akin RK, Walters PJ. Experience with the intraoral vertical subcondylar osteotomy. J Oral Surg. 1975;33:342–345. [PubMed] [Google Scholar]
- Boyne PJ. Free grafting of traumatically displaced or resected mandibular condyles. J Oral Maxillofac Surg. 1989;47:228–332. doi: 10.1016/0278-2391(89)90223-1. [DOI] [PubMed] [Google Scholar]
- Nelson SR, Schow SR, Stein SM, Read LA, Talkington CM. Enhanced surgical exposure for high extracranial internal carotid artery. Ann Vasc Surg. 1992;6:467–472. doi: 10.1007/BF02007006. [DOI] [PubMed] [Google Scholar]
- Sandmann W, Hennerici M, Aulich A, Kniemeyer H, Kremer KW. Progress in carotid artery surgery at the base of the skull. J Vasc Surg. 1984;1:734–743. [PubMed] [Google Scholar]
- Baker DC, Conley J. Treatment of massive deep lobe parotid tumors. Am J Surg. 1979;138:572–575. doi: 10.1016/0002-9610(79)90421-5. [DOI] [PubMed] [Google Scholar]