ABSTRACT
This retrospective study evaluated the safety and efficacy of submental intubation not only for trauma treatment but also for oncological cranial base surgery. The medical records of 24 patients who underwent submental intubation from 1996 to 2002 were reviewed. There were 6 procedures for craniofacial trauma, 12 transmaxillary approaches to the clivus for clivus chordomas, and 6 transmaxillary approaches to the cranial base for chondrosarcomas. Time required for intubation, accidental extubation, postoperative complications, and the healing of intraoral and submental scars were evaluated. The submental orotracheal intubation was completed successfully in all patients. No accidental extubations or tube injuries occurred. The mean time required for intubation was 5 minutes. The only complication was one case of superficial infection of the submental wound. The intraoral and submental accesses healed with minimal scarring in all patients. Submental orotracheal intubation is a useful and safe technique for airway management of craniomaxillofacial traumas and during transfacial approaches to the cranial base. It avoids the complications associated with tracheostomy. It also permits considerable downward retraction of the maxilla after a Le Fort I osteotomy and is associated with good clival exposure. Furthermore, it does not interfere with maxillomandibular fixation at the end of the surgery.
Keywords: Intubation, submental intubation, chordoma
Airway management in complex craniomaxillofacial traumas and in oncological cranial base surgery is often difficult. The choice of intubation technique requires good assessment from a multidisciplinary team that includes maxillofacial surgeons and neurosurgeons as well as good communication between the surgeons and anaesthetist.1 In many conditions such as craniomaxillofacial trauma, neither nasal nor orotracheal intubation is possible. In fact, nasotracheal intubation precludes the treatment of nasal fractures. It can result in meningitis or the tube can be passed intracranially in patients with frontobasilar fractures.2, 3, 4, 5, 6 Conversely, an orotracheal tube interferes with maxillomandibular fixation, compromising the reduction and stabilization of maxillary and mandibular fractures.7 Often neither nasal nor orothracheal intubation is suitable for transfacial approaches to the cranial base.8 In fact, during transmaxillary approaches the orotracheal tube can obstruct the downward retraction of the maxilla after a Le Fort I osteotomy, limiting the exposure of the cranial base.6, 8 The tube can also be clamped between the teeth, reducing the airway lumen.6, 8 At the end of surgery, restoring an individual occlusion may not be tested and, if needed, intermaxillary fixation cannot be performed. In these situations, which require teamwork from several disciplines,8 tracheostomy is considered the technique of choice for airway control by many anaesthetists and surgeons.1, 9
An alternative for tracheostomy was first described by Hernandez Altemir in 1986.10 The submental route for endotracheal intubation10 consists of pulling the free end of an endotracheal tube (universal connector removed) through a submental incision, after a usual orotracheal intubation has been performed.7, 10 The use of submental intubation with Altemir's technique and its modifications has been used in a large number of patients with maxillofacial injuries.1, 7, 10, 11, 12, 13 Many studies have compared the disadvantages and risks of tracheostomy and submental intubation for the treatment of facial fractures.1, 7, 12 However, the use of Altemir's technique in cranial base surgery has not been adequately assessed. This retrospective study therefore evaluated the experience of our multidisciplinary team using submental intubation not only during the treatment of craniomaxillofacial trauma but also during transfacial approaches to the cranial base.
CLINICAL MATERIALS AND METHODS
The medical records of 24 adults who underwent submental intubation at the Neurosurgical Department of San Raffaele Hospital in Milan and at the Maxillo–Facial Surgery Department of San Paolo Hospital in Milan from December 1996 to November 2002 were reviewed. Six patients were treated for craniofacial trauma, 12 underwent transmaxillary approaches to the clivus for clival chordomas (Figs. 1, 2, 3, 4, 5, 6, 7), and 6 underwent transmaxillary approaches to the cranial base for chondrosarcomas.
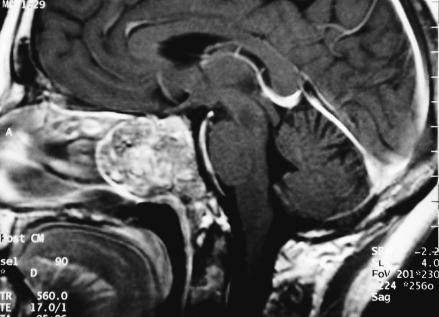
Figure 1.
Preoperative Magnetic Resonance (MR).
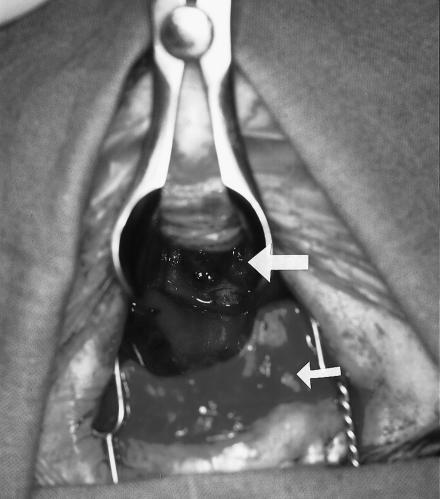
Figure 2.
Intraoperative view of the submental intubation.
Figure 3.
Surgical access to the clivus. Large arrow: exposure of the lesion. Small arrow: maxilla dislocated downward.
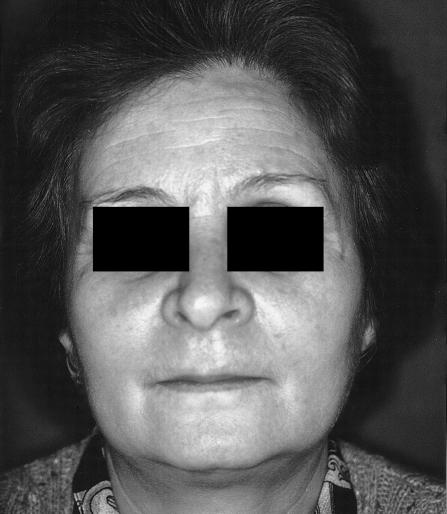
Figure 4.
Postoperative view of patient.
Figure 5.
Surgical scar.
Figure 6.
Postoperative dental occlusion.
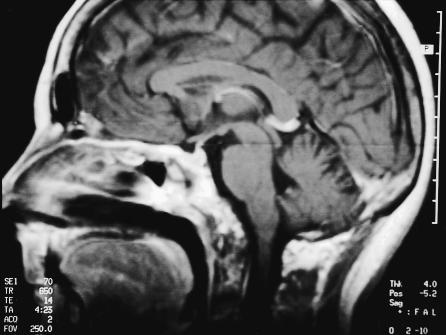
Figure 7.
Postoperative MR.
The following variables were evaluated to assess the results of Altemir's intubation technique: (1) time required for intubation, (2) accidental extubation, (3) postoperative complications (hemorrhage; injury to the sublingual glands, Wharton's duct, or lingual nerve; orotracheal fistula; and infection), and (4) healing of intraoral and submental scars. The time required for submental intubation was calculated starting from the completion of the orotracheal intubation to the fixation of the submental tube.
Surgical Technique
After a normal orotracheal intubation was performed with a reinforced (spiral embedded) 7.5 or 8.5 mm diameter tube, a 2–cm skin incision was made in the paramedian region, about 1 cm from the lower mandibular margin and parallel to it on the midline. Using a curved hemostat, a passage was created by blunt dissection near the lingual surface of the mandible. While the tongue was pushed backward, the tip of the hemostat was visible just below the mucosa of the floor of the mouth, anterior to Wharton's duct papillae. A mucosal incision was made parallel with the gingival margin on top of the tips. A passage for the tube was created from the mouth, through the mylohyoid muscle to the submental incision (Fig. 8). The orotracheal tube was secured in the mouth to avoid accidental extubation. It was then disconnected from the breathing circuit. The end was grasped with the hemostat and withdrawn through the submental tunnel and reconnected. When capnography and lungs auscultation confirm the correct tracheal position of the tube, the tube is fixed at the submental level with 2–0 silk suture, in a similar fashion as a drainage tube.
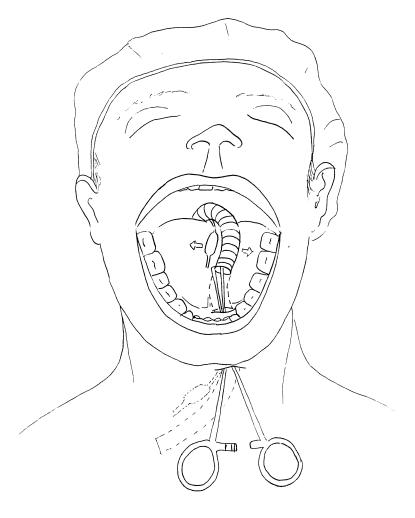
Figure 8A.
Illustration showing anterior view of submental intubation.
At the end of the procedure, anesthesia is discontinued and the patient is extubated in the operating room. The submental access is sutured after extubation using sutures inserted in advance or under local anesthesia. In case of maxillomandibular fixation, release of the incision at the end of surgery is unnecessary. In fact, the intraoral incision can be left to heal by second intention, and the extubation can be performed from the submental access.
RESULTS
Submental orotracheal intubation was completed successfully in all 24 patients. No accidental extubations or tube injuries occurred. The mean time required to place the tube was 5 minutes. No major complications (hemorrhage; injury to the sublingual glands, Wharton's duct or lingual nerve; or orotracheal fistula) were observed during the mean follow–up period of 48 months. Only one minor complication occurred. One case of superficial infection of the submental wound cleared after four days of washing with a saline solution and drainage. The submental incisions healed in all of the patients with minimal scarring.
DISCUSSION
The treatment of oncological and traumatic diseases through craniomaxillofacial surgery often implies problems with intraoperative airway management. When neither nasotracheal nor orotrachel intubation is suitable, temporary tracheostomy is frequently the option of choice.7 This technique, however, is associated with significant morbidity.12 Complications include hemorrhage, recurrent laryngeal nerve damage, subcutaneous emphysema, tracheal stenosis, and a cosmetically undesirable scar.1, 12, 14, 15, 16, 17
Different solutions have been proposed as an alternative to tracheostomy. In panmaxillofacial trauma, which requires maxillomandibular fixation and nasal fracture reduction, switching an endotracheal tube from the nasal route to the oral route without extubation can be a good option.1, 18, 19 This maneuver can be completed in less than 10 minutes.18, 19 The conversion can also be completed more rapidly with the use of tube exchangers.12, 20 Nevertheless, in patients with frontobasilar fractures associated with maxillofacial trauma, the nasotracheal intubation can lead to major complications such as meningitis, sepsis, and cerebrospinal fluid leakage. Furthermore, the nasal tube can be introduced intracranially, causing significant brain damage.1, 2, 3, 4, 5
In 1998 Martinez–Lage et al proposed an alternative to nasotracheal intubation and tracheostomy during treatment of craniofacial traumas and cranial base approaches.6 In this technique, called retromolar intubation, a semilunar osteotomy is made in the retromolar space.6 The orotracheal tube is then placed in the retromolar area, lying below the occlusal plane.6 This intubation technique offers an unobstructed intraoral surgical field with secure airway management, and intermaxillary fixation can be performed without any impediments.1 However bone anatomy must be destroyed to make space for the tube,19 and the procedure requires a mean of 25 minutes to perform.6 Besides, evaluation of the restoration of an individual occlusion can be partially impaired by the presence of the tube in the oral vestibule.
In contrast, the submental route for endotracheal intubation represents a fast and low–morbidity alternative to tracheostomy.7 The Altemir intubation procedure requires no more than 5 minutes to perform.7, 11 The technique is very easy, and the risk of damage to structures such as the sublingual and submaxillary glands, Wharton's duct, and the lingual nerve is very low. In fact, these major complications have never been reported. Our experience confirms that careful blunt dissection close to the medial border of the mandible and good knowledge of anatomy can help avoid damage to the structures of the floor of the mouth. In our experience, the one minor complication of the infected submental wound responded to local measures in 4 days.1 This result seems to confirm the experiences of other authors1, 7, 10 who have reported a low morbidity associated with submental intubation in the treatment of maxillofacial trauma. No episodes of accidental extubation, leaking cuff, submental orotracheal fistulae or anomalous scars have been reported.1
Some technical refinements can help minimize morbidity. After the normal orotracheal intubation, the tube must be firmly secured intraorally to prevent accidental extubation during the submental procedure.1
Choosing material and equipment can represent a technical problem. For example, some reinforced tracheal tubes are manufactured with no detachable connectors. To use these tubes, a modification of Altemir's techinique was proposed by Green and Moore in 1996.21 They described the insertion of a reinforced endotracheal tube from outside the submental incision after orotracheal intubation with a non–reinforced tube.7, 21 The initial orotracheal tube is then removed, and the reinforced tube is introduced into trachea during direct laryngoscopy. In 1997 Cooper proposed the use of tube exchangers.12, 20
In Altemir's original report, he suggested creating a subperiosteal passage for the tube in the lingual surface of the mandible.10 However, the passage can be created safely with an easier extraperiosteal blunt dissection near the lingual surface of the mandible. This dissection avoids lesions to the floor of the mouth structures and ensures good mobility of the mandibular segments.11
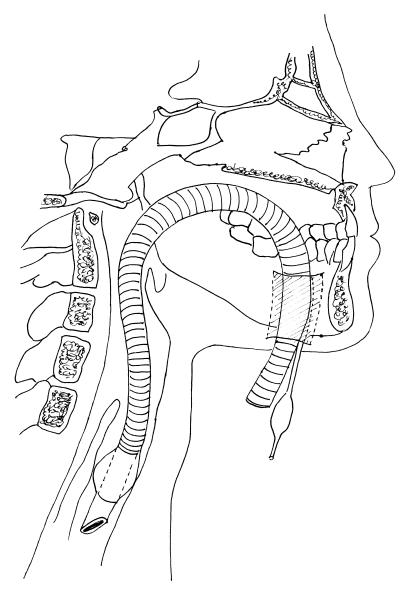
Figure 8B.
Illustration showing lateral view of submental intubation.
ACKNOWLEDGMENT
We thank anesthetist Dr. Tiziana Corino for her assistance.
REFERENCES
- Caron G, Pasquin R, Lessard M, Trepanier C, Landry PE. Submental endotracheal intubation: an alternative to tracheostomy in patients with midfacial and panfacial fractures. J Trauma. 2000;48:235–240. doi: 10.1097/00005373-200002000-00007. [DOI] [PubMed] [Google Scholar]
- Hall D. Nasotracheal intubation with facial fractures. JAMA. 1989;261:1198. [Google Scholar]
- Schultz RC. Nasotracheal intubation in the presence of facial fractures. Plast Reconstr Surg. 1990;86:1046. doi: 10.1097/00006534-199011000-00053. [DOI] [PubMed] [Google Scholar]
- Muzzi DM, Losasso TJ, Cucchiara RF. Complications from a nasopharyngeal airway in a patient with a basilar skull fractures. Anesthesiology. 1991;74:366–372. doi: 10.1097/00000542-199102000-00026. [DOI] [PubMed] [Google Scholar]
- Bahr W, Stoll P. Nasal intubation in the presence of frontobasal fractures. J Oral Maxillofac Surg. 1992;50:445–451. doi: 10.1016/s0278-2391(10)80312-x. [DOI] [PubMed] [Google Scholar]
- Martinez–Lage J, Esclava JM, Cebrecos AI, Marcos O. Retromolar intubation. J Oral Maxillofac Surg. 1998;56:302–306. doi: 10.1016/s0278-2391(98)90103-3. [DOI] [PubMed] [Google Scholar]
- Paetkau D, Strand M, Onc B. Submental orotracheal intubation for maxillofacial surgery. Anesthesiology. 2000;92:912–914. doi: 10.1097/00000542-200003000-00063. [DOI] [PubMed] [Google Scholar]
- Sekkar LN, Janeka IP. Surgery of the cranial base tumors. New York: Raven Press. 1993:235–240. [Google Scholar]
- James D, Crockord HA. Surgical access to the base of the skull and upper cervical spine by extended maxillectomy. Neurosurgery. 1991;29:411–416. doi: 10.1097/00006123-199109000-00012. [DOI] [PubMed] [Google Scholar]
- Altemir FH. The submental route for endotracheal intubation. J Maxillofac Surg. 1986;14:64–65. doi: 10.1016/s0301-0503(86)80261-2. [DOI] [PubMed] [Google Scholar]
- Biglioli F, Galioto S, Giannì AB, Autelitano L, Goisis M. Applicazione della tecnica di intubazione orotracheale con passaggio submentale nei traumi maxillo–facciali. Riv It Ch Maxillofac. 1999;10:19–21. [Google Scholar]
- Drolet P, Girard M, Poirier J, Grenier Y. Facilitating submental endotracheal intubation with an endotracheal tube exchanger. Anesth Analg. 2000;90:222–224. doi: 10.1097/00000539-200001000-00044. [DOI] [PubMed] [Google Scholar]
- Labbe D, Kaluinski A, Badie–Modiri B, et al. Submental oroendotracheal intubation in craniomaxillofacial trauma. Ann Chir Plast Esthet. 1998;43:248–251. [PubMed] [Google Scholar]
- Chew JY, Cantrell RW. Tracheostomy, complications and their management. Arch Otolaryngol. 1972;96:538–545. doi: 10.1001/archotol.1972.00770090816008. [DOI] [PubMed] [Google Scholar]
- Demas PN, Sotereanos GC. The use of tracheotomy in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1988;46:483–486. doi: 10.1016/0278-2391(88)90418-1. [DOI] [PubMed] [Google Scholar]
- Waldron J, Padgham ND, Hurley SE. Complications of emergency and elective tracheostomy: a retrospective study of 150 consecutives cases. Ann R Col Surg Engl. 1990;72:218–220. [PMC free article] [PubMed] [Google Scholar]
- Zeitouni AG, Kost KM. Tracheostomy: a retrospective review of 281 cases. J Otolaryngol. 1994;23:61–66. [PubMed] [Google Scholar]
- Werther JR, Richardson G, McIlwain MR. Nasal tube switch: converting from a nasal to an oral endotracheal tube without extubation. J Oral Maxillofac Surg. 1994;52(suppl 9):S994–S996. doi: 10.1016/s0278-2391(10)80090-4. [DOI] [PubMed] [Google Scholar]
- Martinez–Lage JL, Eslava JM, Cebrecos AI, Marcos O. Retromolar intubation. J Oral Maxillofac Surg. 1998;56:302–306. doi: 10.1016/s0278-2391(98)90103-3. [DOI] [PubMed] [Google Scholar]
- Cooper RM. Conversion of a nasal tube to an orotracheal intubation using an endotracheal tube exchanger. Anesthesiology. 1997;87:717–718. doi: 10.1097/00000542-199709000-00049. [DOI] [PubMed] [Google Scholar]
- Green JD, Moore UJ. A modification of sub–mental intubation. Br J Anaesth. 1996;77:789–791. doi: 10.1093/bja/77.6.789. [DOI] [PubMed] [Google Scholar]