Abstract
Clinical presentation A 12-year-old spayed domestic crossbred cat presented because she would not walk down stairs. A firm swelling on the medial aspect of the elbow was detected during physical examination. The lesion was not hot or painful on palpation and the lameness was mild, but the elbow had a reduced range of motion compared with the contralateral limb.
Diagnosis and treatment Plain radiographs, physical findings, the appearance of the lesion at surgery and histopathological examination of biopsy specimens suggested the mass was a synovial osteochondroma arising from synovial membrane near the medial portion of the elbow joint. Resection of the lesion improved the cat's mobility and overall clinical status. At the time of writing, the cat continued to do well 18 months following surgery and was receiving standard doses of meloxicam for the concurrent elbow osteoarthritis.
Practical relevance Practitioners should be alert to the possibility of this benign entity. Misdiagnosis as a chondrosarcoma, for example, might conceivably lead to radical and unnecessary amputation.
Periarticular mineralised masses can present a diagnostic challenge in the cat because radiology alone is often insufficiently characteristic to provide a definitive diagnosis. 1 Signalment, history, physical findings, radiographic features, histological examination of representative biopsy specimens and the subsequent clinical course are best considered together when attempting to differentiate between possible aetiologies. Diet, lifestyle (indoors versus outdoors), obesity, degenerative joint disease (DJD), feline leukaemia virus (FeLV) status and neoplasia may potentially play a role in the development of periarticular mineralised masses. All these contributing factors must be considered in the investigation of cats with such lesions.
Case history
History, physical findings and radiography
A 12-year-old, neutered female domestic shorthair cat was presented with a 2-month history of reluctance to walk down stairs. Occasionally, the left foreleg was ‘held up’ when the cat was at rest. The patient had been eating and drinking normally and her owner had not noticed any changes in urination or defecation. The cat resided exclusively indoors in a three-cat household and had not been vaccinated since her initial inoculations against respiratory viruses and panleukopenia as a kitten. She had been fed a diet consisting largely of fresh fish and red meat, with some dry food given occasionally. In addition, she had been given chopped sheep's liver about three times weekly. When observed in her home environment, the cat would still jump on and off the owner's bed, and lameness during locomotion in the house was too subtle to be easily appreciated by one of the authors during a home visit (RM).
On physical examination, the cat was in good body condition (body condition score 5/9). She had a grade 1/5 lameness of the left fore leg. A firm swelling on the medial aspect of the distal left humerus could be palpated. The lesion was neither hot nor painful to the touch, and there was no obvious associated soft tissue swelling. Some discomfort was elicited on flexion and, in particular, attempted extension of the left elbow. No other pertinent physical findings were evident.
The presence of a similar but less dramatic lesion at a similar position in the contralateral elbow emphasises the importance of taking radiographs of the contralateral limb in cases with unusual bone lesion (s).
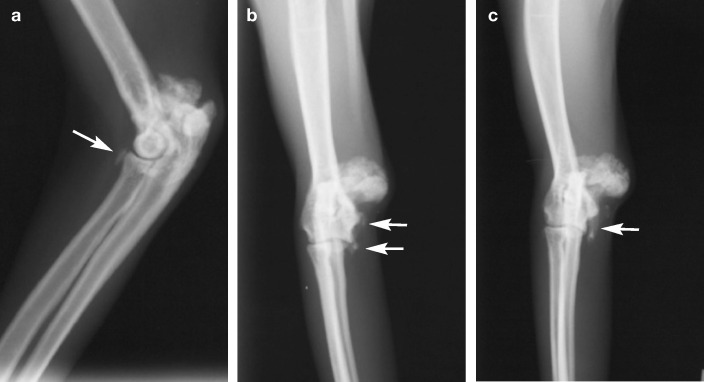
The cat was sedated with a combination of ketamine (5 mg/kg) and midazolam (0.3 mg/kg) mixed together and given subcutaneously. Radiographs of the affected elbow (Fig 1a,b), contralateral elbow (Fig 2a,b) and thorax were taken. The views of the affected limb demonstrated a focal, sessile, mineralised lesion with smoothly irregular margination adjacent to the medial epicondylar crest of the left humerus. There was no obvious associated soft tissue swelling, consistent with the physical findings. The lesion appeared well demarcated from surrounding tissues, although there was a conical-shaped mineralised structure extending from the joint to the proliferative mass. It was not possible to determine if this structure was contiguous with the synovial membrane. The cortical bone and medullary cavity of the humerus adjacent to this lesion appeared uninvolved in the underlying disease process and there was no evidence of lysis within the mass. As well as this obvious lesion, there was evidence of chronic DJD of the left elbow, with enthesiophytes at sites of attachment of the collateral ligaments, increased radiodensity of subchrondral bone in the ulna, and new bone on the distal edge of the articular margin of the humerus and the medial coronoid process of the ulna (Fig 1b).
FIG 1.
Mediolateral (a), craniocaudal (b) and craniocaudal oblique (c) radiographs of the left elbow of an elderly cat with left forelimb lameness. There is a well-circumscribed mineralised lesion adjacent to the medial epicondylar ridge of the left humerus. There is also a conical-shaped bony structure (arrow; c) extending from the joint to the proliferative mass, which was speculated to be a mineralised ‘outpocketing’ of synovial membrane. There is no lytic component to the lesion, or the adjacent humerus. As well as these lesions, there is evidence of chronic osteoarthritis of the left elbow (eg, the supinator sesamoid bone [arrow; a] adjacent to the radius is more obvious than normal), increased radiodensity of the subchrondral bone in the ulna (a), and mineralised structures on the medial humeral epicondyle and medial extent of the articular surface (arrows; b), which could be enthesiophytes, further osteochondromas or mineralised free bodies
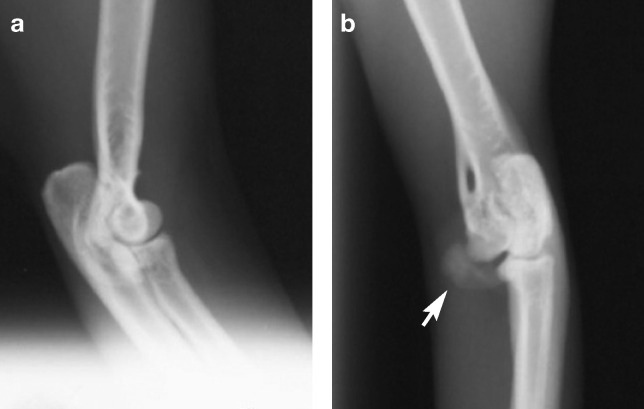
FIG 2.
Lateral (a) and craniocaudal (b) radiographs of the right elbow of an elderly cat with a left forelimb lameness. A mineralised mass (arrow; b) was evident on the medial aspect of the right humeral condyle
There was also a mineralised lesion on the medial aspect of the distal right humerus, smaller and ‘smoother’ than the lesion medial to the left elbow. The thoracic radiograph demonstrated no evidence of metastatic disease, although the heart had shifted forward on its axis, as is quite common in older cats.
Our assessment was that the mineralised lesion explained much of the cat's presenting complaint and physical examination findings, and that this lesion was most likely a synovial osteochondroma, or perhaps an atypical bone neoplasm (osteoma, osteosarcoma, chondroma, chrondrosarcoma, parosteal osteosarcoma). The presence of a similar but less dramatic lesion at a similar position in the contralateral elbow suggested that both lesions were reflective of the same disease process, and emphasises the importance of taking radio graphs of the contralateral limb in cases with unusual bone lesion(s).
Surgical management
A decision was made to obtain a tissue sample for histological assessment, and simultaneously to debulk the lesion as much as possible in an attempt to improve mobility of the affected elbow joint. Cefazolin sodium (22 mg/kg) was administered by slow intravenous infusion immediately following induction of general anaesthesia.
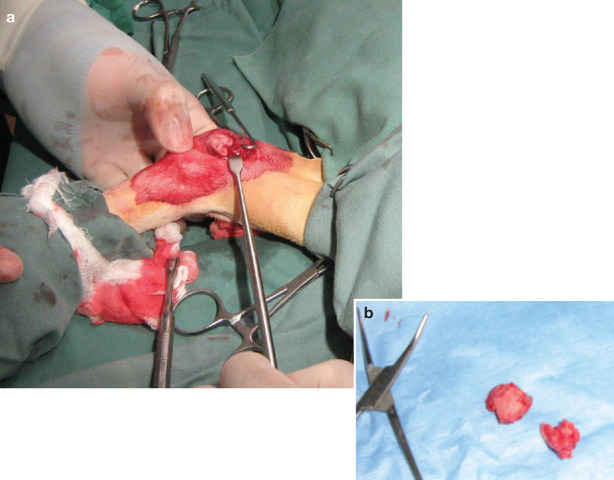
A standard medial approach to the left elbow was made. 2 Following dissection of the subcutaneous tissues and retraction of the ulnar nerve, a smooth proliferative mass was identified (Fig 3). The mass appeared to be completely extra-articular. It was not possible to determine with certainty whether there was any communication with the articular cavity of the elbow joint. The mass was gently separated from the underlying bone using a periosteal elevator, and dissected free from its soft tissue attachments. Rongeurs were used subsequently to remove residual mineralised material from the humerus. The wound was closed in a routine fashion with 30 polydioxanone sutures in a simple continuous pattern. Skin was opposed using monofilament non-absorbable sutures in a simple interrupted pattern.
FIG 3.
Intraoperative view (a) demonstrating the gross appearance of the lesion — a smooth proliferative mass. The resected bone specimens, submitted subsequently for histological assessment, are shown in (b)
Immediately postoperatively, an improved range of motion of the elbow was noted, particularly with respect to full extension. An additional dose of methadone (0.2 mg/kg) was given postoperatively to provide further analgesia.
Histology
Sections were prepared from the extra-osseous masses associated with the distal end of the humerus and the elbow joint. Two microscopic patterns were apparent within the two biopsy specimens. First, broad osseous trabeculae of lamellar bone with a relatively uniform scattering of osteocytic lacunae containing single osteocytes were present. Most trabecular surfaces were covered by a single layer of plump osteoblasts. The inter-trabecular spaces were filled with a mixture of fatty and haematopoietic marrow. In several of these spaces, there was some periarterial fibrosis. An occasional island of cartilage, with a single chondrocyte per lacuna, was evident.
Secondly, the larger piece of tissue had osseous trabeculae of uneven thickness, often covered with plump osteoblasts. There were large tracts of fibrocartilage with a few large foci of hyaline chondrocytes. The cartilage was mostly just below the apparent surface and the outer margins were coated with a thick layer of bone. Some of the cartilaginous areas displayed endochondral vascular invasion, often preceded by a multinucleated chondroclast. Occasional foci of hyaline cartilage were apparent. The bands of bone and cartilage were separated by well-vascularised, predominantly mature, fibrous tissue. The cellularity of these fibrous regions was moderate but with limited anisokaryosis. The amount of fibrillary collagen was variable. A few intertrabecular spaces contained a mixture of fatty and haematopoietic marrow. Often cells lining the osseous trabeculae were osteoblasts.
The radiological and histopathological patterns were consistent with a feline osteochondroma or synovial chondromatosis/osteochondromatosis. The latter usually has considerable cartilage but in cats this may occasionally be replaced by remodelling osteogenesis, as in this case.
A diagnosis that was considered, but rejected, was parosteal osteosarcoma.3–5 These surface osseous neoplasms are distinctly less malignant than other osteosarcomas and are often heavily ossified and somewhat lobulated. They are distinctly attached to the corticalis of the underlying bone, the sessile base being in contrast to the pedunculated appearance of the osteochondroma. The general pathology involves trabeculae of lamellar bone separated by slightly atypical spindle cell stroma of varying cellular numbers. Haematopoietic and fatty marrow in the intertrabecular spaces is not characteristic and then only foci or islands are enclosed by spindle cells. There may be a cartilaginous cap. The bone trabeculae are classed as abnormal, with irregularity and multiple cement lines. 6
Outcome and long-term follow-up
Following surgery, the cat's lameness was improved, with no recurrence of the mass on palpation after 18 months. Continued close monitoring was recommended to the owner. The owner was also advised to completely discontinue the practice of feeding fresh liver to the patient and to administer meloxicam (Metacam; Boehringer Ingelheim) at recommended doses to treat the underlying DJD;7,8 this drug appeared to contribute to the cat's improved mobility.
Discussion
This report describes a well-circumscribed, proliferative, periarticular mineralised lesion in close proximity to the elbow joint of an aged cat with osteoarthritis. Prior to biopsy, the diagnostic possibilities included osteoarthritis, synovial osteochondroma, osteochondroma (either solitary, or as part of multiple cartilaginous exostosis) or an atypical bone neoplasm. However, in the light of the clinical features (especially the absence of substantial pain, lameness, heat or soft tissue swelling) and, in particular, the radiographic and histologic findings, and the postoperative clinical course, the most likely diagnosis was synovial osteochondroma or feline osteochondroma. The presence of a proliferative bony lesion in close proximity to a joint affected by osteoarthritis should always suggest the possibility of synovial osteochondroma,9–12 especially if, as in the present case, there is a comparable lesion in another joint (or joints).
The suspicion that the lesion was connected to the elbow joint by a pedunculated structure that may have been mineralised synovial membrane, added support to the possibility that this was a synovial osteochondroma. Its origin was uncertain, however, and as it may have arisen from bone, an osteochondroma was also a possibility. The mineralised lesion medial to the right elbow may be a smaller synovial osteochondroma, an osteochondroma or an osteophyte.
Our impression from the veterinary literature is that synovial osteochondromas may occur as a primary entity, but more commonly they represent a degenerative condition of synovial epithelium near joints affected by osteoarthritis. Nodules form in the synovial tissue of a joint, tendon sheaths or bursae. 1 Proliferative lesions arise from nodules of cartilage formed by synovial metaplasia, and these nodules undergo endochondral ossification, eventually giving rise to mineralised periarticular masses. 10 Other radiographic features of DJD, such as enthesiophytes, increased subchondral bone opacity and bone remodelling, are often seen concurrently with the synovial mass. In young cats, the presence of multiple osteochrondromas associated with an adverse clinical course has been strongly associated with FeLV infection, but these arise from bone or growth plates rather than synovial membranes.
In small animals, synovial osteochondromatosis usually affects a single joint, such as the shoulder, stifle, elbow or tarsus.
In small animals, synovial osteochondromatosis usually affects a single joint, such as the shoulder, stifle, elbow or tarsus. Nodules may be single (as in the present case) or multiple,10,11 and may become pedunculated or break off, forming loose bodies within the joint space. The radiographic appearance of the affected joint varies according to the stage of the condition (Fig 4), although typically single or multiple mineralised bodies are visible within or adjacent to the joint, in addition to varying degrees of DJD. In the future, computed tomographic constructs will likely provide a better three-dimensional representation of the new bone formation in relation to other anatomical landmarks.
FIG 4.
Further radiographic examples of synovial osteochondromas in cats with osteoarthritis. (a) Lesions in a geriatric cat with DJD of both shoulders. Courtesy of Randolph Baral and Melissa Catt. (b) Lesions in a cat with DJD of both elbows. Courtesy of Richard Gowan. (c) Multiple synovial osteochondromas adjacent to the elbow joint of an aged cat with severe elbow osteoarthritis. (d) Stifle of a cat with DJD secondary to mucopolysaccharidosis type VI, a lysosomal storage disease caused by a deficiency of N-acetylgalactosamine-4-sulfatase 13
Hypervitaminosis A is typically associated with cats fed a diet consisting exclusively of liver. Enthesiophytes develop in periarticular locations as smoothly marginated and homogeneously textured growths, which gradually ankylose joints. Changes are most obvious on the cervical and cranial thoracic vertebrae but can also develop around the shoulder and elbow joints. 10 The pathomechanism of this change is said to be increased bone production at points of tension, such as the insertions of tendons and ligaments, in regions subjected to a wide range of motion and stress, such as the neck and thoracic limbs. Although cats that consume a liver-only diet are most susceptible, hypervitaminosis A can also occur in cats that eat liver on a regular basis for a protracted period. 14 It is conceivable that the lesions in the present cat were due, in part, to the effect of mild chronic vitamin A excess. However, lesions typical of hypervitaminosis A were not evident elsewhere (eg, cervical vertebrae) on survey radiography.
Elbow osteoarthritis appears over-represented when the distribution of radiographically affected joints is examined. 15 This likely reflects the fact that when cats land after jumping from a height, the elbows bear the greatest amount of biomechanical stress. Elbow dysplasia, chronic low grade trauma or subtle malarticulations have also been suggested as causes of elbow DJD.16,17
Primary bone tumours in cats are uncommon,18,19 representing 5% of feline neoplasms. Osteosarcoma is by far the most prevalent, comprising 70–80% of feline bone tumours, with medullary or central osteosarcomas being most common. 20 Osteosarcomas may also arise from the outer surface of the bone (parosteal osteosarcoma) or from extraskeletal sites, such as subcutaneous areas used for vaccination. 21 Other primary bone tumours include osteoma, chondroma, chondrosarcoma and fibrosarcoma. In this case, these conditions were excluded on the basis of histopathology. The absence of pain, heat and soft tissue swelling made a diagnosis of osteosarcoma unlikely. Radiographically the absence of bone destruction made this diagnosis even less likely.
In people, the term synovial osteochondromatosis refers to a benign condition in which synovial membrane proliferation and metaplasia result in cartilaginous/ossified synovial fragments in the joint space. The degree of calcification can vary from a few calcific specks to frankly ossified bodies. Free fragments may exist within the joint cavity or be embedded within the proliferating synovium and can extend to the surrounding soft tissues. This disorder nearly always occurs within joints but occasionally arises within bursa and tendon sheaths. It is monoarticular and typically affects large joints, such as the knee, hip, elbow and shoulder. It is more common in men than women and generally affects patients between 20 and 50 years old. The natural history of synovial osteochondromatosis entails gradual progression of disease, joint deterioration, and secondary osteoarthritis. On radiographs, the multiple lesions (typically more than five) appear as calcified or osseous bodies within the joint or bursa. The differential diagnosis includes pigmented villonodular synovitis, synovial haemangiomatosis, synovial sarcoma and secondary chondromatosis (eg, associated with joint surface disintegration as may be caused by osteo- or rheumatoid arthritis, osteochondral fracture, osteochondritis dissecans). Solitary synovial osteochondroma is an uncommon entity, representing a rare variant of synovial osteochondromatosis; this solitary manifestation is not connected to bone and occurs almost exclusively near joints in the hands and feet. 22
It is clear from these descriptions that the entities in cats and people are not quite the same. The semantics and precise pathogenesis of the lesion in the cat of the present report are therefore somewhat unclear, although we favour the notion that it is secondary to DJD. Readers interested in this entity can find further information elsewhere. 23
A proliferative bony lesion in close proximity to a joint affected by osteoarthritis should always suggest the possibility of synovial osteochondroma, especially if there is a comparable lesion in one or more other joints.
The main purpose of this report is to alert feline practitioners to this benign entity. To quote a similar case report concerning a human patient: ‘Synovial osteochondromatosis should always be considered as a differential diagnosis whenever a patient presents with pain, swelling, and loss of function at or around a joint. Chondrosarcoma has been misdiagnosed, leading to radical and unnecessary amputation, because synovial osteochondromatosis has not been considered.’ 24 These words seem just as pertinent in the veterinary context — it would be tragic if this were to occur in a feline patient.
Acknowledgements
Richard Malik is supported by the Valentine Charlton Bequest of the Centre for Veterinary Education of The University of Sydney.
References
- 1.Mahoney PN, Lamb CR. Articular, periarticular and juxtaarticular mineralised bodies in the dog and cat: a radiologic review. Vet Radiol Ultrasound 1996; 37: 3–19. [Google Scholar]
- 2.Piermattei DL, Johnson KA. The forelimb. In: An atlas of surgical approaches to the bones and joints of the dog and cat, 4th edn. Saunders, Philadelphia, 2004: 149–276. [Google Scholar]
- 3.Banks WC. Paraosteal osteosarcoma in a dog and a cat. J Am Vet Med Assoc 1971; 158: 1412–15. [PubMed] [Google Scholar]
- 4.Campanacci M, Picci P, Gherlinzoni F, Guerra A, Bertoni F, Neff JR. Parosteal osteosarcoma. J Bone Joint Surg Br 1984; 66: 313–21. [DOI] [PubMed] [Google Scholar]
- 5.Griffith JW, Dubielzig RR, Riser WH, Jezyk P. Paraosteal osteosarcoma with pulmonary metastases in a cat. Vet Pathol 1984; 21: 123–25. [DOI] [PubMed] [Google Scholar]
- 6.Thompson KG, Pool RR. Tumors in bones. In: Meuten DJ, ed. Tumors in domestic animals. 4th edn. Iowa State Press, Ames, USA, 2002: 245–318. [Google Scholar]
- 7.Lascelles BDX, Henderson AJ, Hackett IJ. Evaluation of the clinical efficacy of meloxicam in cats with painful locomotor disorders. J Small Anim Pract 2001; 42: 587–93. [DOI] [PubMed] [Google Scholar]
- 8.Gunew MN, Menrath VH, Marshall RD. Long-term safety, efficacy and palatability of oral meloxicam at 0.01–0.03 mg/kg for treatment of osteoarthritic pain in cats. J Feline Med Surg 2008; 10: 235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hubler M, Johnson KA, Burling RT, Francis DF, Ratcliffe RCC. Lesions resembling osteochondromatosis in two cats. J Small Anim Pract 1986; 27: 181–87. [Google Scholar]
- 10.Allan GS. Radiographic features of feline joint disease. Vet Clin North Am Small Anim Pract 2000; 30: 281–302. [PubMed] [Google Scholar]
- 11.Wood BC, Grant DC, McKlveen TL. What is your diagnosis? J Am Vet Med Assoc 2002; 221: 939–940. [DOI] [PubMed] [Google Scholar]
- 12.Langley-Hobbs SJ. Humeral osteochondromas in cats [abstract]. Vet Surg 2001; 30: 296. [Google Scholar]
- 13.Crawley AC, Yogalingam G, Muller VJ, Hopwood JJ. Two mutations within a feline mucopolysaccharidosis type VI colony cause three different clinical phenotypes. J Clin Invest 1998; 101: 109–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watson ADJ. An old, lame cat with a reduced food intake and stiff neck. Aust Vet J 1998; 76: 792–801. [DOI] [PubMed] [Google Scholar]
- 15.Godfrey DR. Osteoarthritis in cats: a retrospective radiological study. J Small Anim Pract 2005; 46: 425–29. [DOI] [PubMed] [Google Scholar]
- 16.Hardie EM, Roe SC, Martin FR. Radiographic evidence of degenerative joint disease in geriatric cats: 100 cases (1994–1997). J Am Vet Med Assoc 2002; 220: 628–32. [DOI] [PubMed] [Google Scholar]
- 17.Clarke SP, Mellor D, Clements DN. Prevalence of radiographic signs of degenerative joint disease in a hospital population of cats. Vet Rec 2005: 157: 793–99. [DOI] [PubMed] [Google Scholar]
- 18.Engle GC, Brodey RS. A retrospective study of 395 feline neoplasms. J Am Anim Hosp Assoc 1969; 5: 21–31. [Google Scholar]
- 19.Turrel JM, Pool RR. Primary bone tumors in the cat: a retrosprective study of 15 cats and a literature review. Vet Radiol 1982; 23: 152–66. [Google Scholar]
- 20.Liu S, Dorfman HD, Patnik AK. Primary and secondary bone tumours in the cat. J Small Anim Pract 1974; 15: 141–56. [DOI] [PubMed] [Google Scholar]
- 21.Heldmann E, Anderson MA, Wagner-Mann C. Feline osteosarcoma: 145 cases (1990–1995). J Am Anim Hosp Assoc 2000; 36: 518–21. [DOI] [PubMed] [Google Scholar]
- 22.Crotty JM, Monu JU, Pope TL., Jr Synovial osteochondromatosis. Radiol Clin North Am 1996: 34: 327–42. [PubMed] [Google Scholar]
- 23.Bennett D. The musculoskeletal system. In: Chandler EA, Gaskell RM, Gaskell CJ. (eds) Feline medicine and therapeutics. 3rd edn. Wiley Blackwell, Oxford, 2004: 203–4, 211. [Google Scholar]
- 24.Valmassy R, Ferguson H. Synovial osteochondromatosis. A brief review. J Am Podiatr Med Assoc 1992; 82: 427–31. [DOI] [PubMed] [Google Scholar]