Abstract
Background
Due to the incomplete standardization of the etiology and diagnostic criteria for fetal growth restriction (FGR), there has been uncertainty in the early prediction of FGR. The comprehensive estimation of FGR was mainly based on various factors, such as maternal characteristics and medical history, nuchal translucency (NT), and serum biochemical markers [pregnancy-associated plasma protein-A (PAPP-A) and free beta human chorionic gonadotropin (free β-hCG)]. Herein, we performed a retrospective cohort study to investigate the correlation and diagnostic value of maternal markers such as PAPP-A, free β-hCG, and NT in the first trimester with maternal characteristics, so as to provide theoretical basis for perinatal care and the application of low-dose aspirin.
Methods
A retrospective cohort study was conducted to analyze the data of an FGR group and a non-FGR group. Chi-square test and Mann-Whitney U test were used for univariate analysis of qualitative or quantitative data, respectively. Modified Poisson regression calculated the relative risk (RR) and 95% confidence interval (CI) of perinatal variables; P<0.05 was considered statistically significant.
Results
The multiple of median (MoM) of PAPP-A level and NT in the FGR group were lower than those of the non-FGR group [0.63 (0.12–2.08) vs. 1.01 (0.28–2.41) MoM, 1.30 (0.80–2.07) vs. 1.40 (0.80–2.20) cm, P<0.05]. The weight, score, and length of newborns in the FGR group were lower than those in the non-FGR group (all P<0.001). Modified Poisson regression analysis showed that gestational hypertension (GH) [RR =1.836 (95% CI: 1.188–2.836)], oligohydramnios [1.420 (95% CI: 1.022–1.973)], premature rupture of membranes (PROM) [0.641 (95% CI: 0.425–0.969)], female infant [1.539 (95% CI: 1.098–2.157)], low infant length [5.700 (95% CI: 3.416–9.509)], low birth weight [1.609 (95% CI: 1.012–2.559), and increased PAPP-A MoM [0.533 (95% CI: 0.369–0.769)] were associated with FGR. The cut-off value of PAPP-A + free β-hCG + NT for predicting FGR was 0.190, with a sensitivity of 0.547 and a specificity of 0.778.
Conclusions
Early screening markers combined with perinatal characteristics have better diagnostic value in predicting FGR and provide a scientific basis for the clinical use of low-dose aspirin to prevent FGR.
Keywords: Fetal growth restriction (FGR), screening marker, perinatal characteristics, pregnancy-associated plasma protein-A (PAPP-A), low birth weight
Highlight box.
Key findings
• The decrease of serum pregnancy-associated plasma protein-A (PAPP-A) level in early pregnancy can predict fetal growth restriction (FGR), and maternal serum free beta human chorionic gonadotropin (free β-hCG) or nuchal translucency (NT) combined with PAPP-A could improve the diagnostic sensitivity of FGR. Pregnant women with FGR were more likely to have decreased body mass index (BMI) and placental disease such as gestational hypertension (GH); low birth weight and low infant length might also occur in this circumstance.
What is known and what is new?
• The definition of FGR is usually manifested as fetal ultrasonographic estimated weight or abdominal circumference below the 10th percentile for gestational age (GA). According to the survey, about 10% of pregnant women have intrauterine growth restriction (IUGR).
• As the etiology and diagnostic criteria of FGR have not been completely unified, and there are no clear defining parameters, uncertainties remain for the early prediction of FGR and the optimal delivery time. Subsequently, the comprehensive estimation of FGR is mainly based on multiple factors.
What is the implication, and what should change now?
• Prenatal screening markers in early pregnancy combined with perinatal characteristics can predict FGR, which can enable early intervention against the occurrence of FGR in pregnant women and provide a theoretical basis for perinatal health care and the clinical use of low-dose aspirin.
Introduction
Background
The definition of fetal growth restriction (FGR) in the American College of Obstetricians and Gynecologists (ACOG) bulletin refers to the fetal growth that does not reach its due genetic potential due to the influence of maternal, fetal, placental, and other pathological factors. FGR usually manifests as fetal ultrasonographic estimated weight or abdominal circumference below the 10th percentile for gestational age (GA) (1). According to a survey (2), about 10% of pregnant women have intrauterine growth restriction (IUGR). However, the majority of healthy women without underlying diseases can deliver physiologically healthy fetuses, defined as small for gestational age (SGA). The other class of SGA fetuses with pathological FGR, which is characterized by the failure of the fetus to achieve its normal growth process, is associated with perinatal morbidity and mortality and a series of problems in adulthood, including short stature, metabolic syndrome, type 2 diabetes, insulin resistance, and cardiovascular disease (2,3), and is also closely associated with iatrogenic preterm birth and pregnancy complications such as preeclampsia (PE) (4). Normal fetal growth predominantly relies on the placenta to provide adequate oxygen and nutrition, so the causes of FGR include placental factors, as well as maternal and fetal factors (5,6).
Rationale and knowledge gap
Secretion of placental markers is affected by trophoblast invasion and structure, and impairment of trophoblast circulation leads to changes in the concentration of some markers. Thus, in the case of placental hypoperfusion, serum markers such as pregnancy-associated plasma protein-A (PAPP-A) levels are reduced and IUGR occurs simultaneously (7). In addition, it has been reported that according to Doppler analysis, the mean uterine artery pulsatility index and uterine resistance index were higher, and PAPP-A level was 0.42 times lower in FGR fetuses (all P<0.05) (8). A large retrospective study reported that decreased levels of maternal serum PAPP-A and free beta human chorionic gonadotropin (free β-hCG) at 11–13 weeks of gestation could predict SGA newborns (9). In contrast, a comprehensive screening method (2), including maternal characteristics and medical history, body mass index (BMI), nuchal translucency (NT), and serum biochemical markers such as PAPP-A, has been described with higher accuracy in predicting FGR and PE.
Objective
As the etiology and diagnostic criteria of FGR have not been completely unified, and there are no clear parameters to define, there are still uncertainties for the early prediction of FGR and the optimal delivery time, so the comprehensive estimation of FGR is mainly based on multiple factors (10). Therefore, we performed this retrospective cohort study. On the basis of prenatal diagnosis in early pregnancy, pregnant women who gave birth to healthy fetuses and pregnant women with clinical diagnosis of FGR were selected as the research participants to investigate the correlation with maternal characteristics and diagnostic value of maternal markers PAPP-A, free β-hCG, and NT in early pregnancy, and to provide theoretical basis for clinical diagnosis and rational drug use. We present this article in accordance with the STARD reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-24-58/rc).
Methods
Participants
The data of pregnant women who underwent prenatal diagnosis during the first trimester and were hospitalized for delivery in late pregnancy from January 2018 to December 2020 were collected. Excel data were derived from the hospital information system (HIS) and prenatal screening system of Hangzhou Women’s Hospital (Hangzhou Maternal and Child Health Care Hospital) according to the principle of unique matching. After eliminating repeated test results, 440 pregnant women were randomly selected according to the ratio of 1:4 and divided into two groups: FGR group (n=90) and non-FGR group (n=350). All cases were singleton pregnancies; informed consent and signature were obtained before the study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Human Research Ethics Committee of the Hangzhou Women’s Hospital (No. Medical Ethics Review 2023-032).
Diagnostic and exclusion criteria
Diagnostic criteria
Ultrasound can be used to evaluate the fetal growth status by measuring abdominal circumference, head circumference, biparietal diameter, and femoral length. It is suggested that if the fetal weight or abdominal circumference estimated by ultrasound is lower than the 10th percentile of GA, further umbilical artery Doppler flow imaging and amniotic fluid evaluation should be considered (11). Pregnancy complications include hypertensive disorders of pregnancy (HDP), gestational diabetes mellitus (GDM), intrahepatic cholestasis of pregnancy (ICP), thrombocytopenia, hyperlipidemia, uterine scar, arrhythmias, and hypothyroidism/hyperthyroidism during pregnancy. Other factors include premature rupture of membranes (PROM), fetal distress, placental abruption, oligohydramnios, nuchal umbilical cord, premature delivery, and low birth weight infants (12-15).
PROM refers to the rupture of the membrane before the onset of uterine contraction, also known as the rupture of the membrane before labor (15). Fetal distress refers to acute or chronic hypoxia of the fetus in utero; the commonly used clinical indicators include intrapartum fetal heart rate monitoring, meconium contamination of amniotic fluid, and low Apgar score (16). Preterm birth is defined as a fetus born at 28–37 weeks of gestation or birth weight ≥1,000 g (17). Oligohydramnios was defined as amniotic fluid index (AFI) <5 cm, and polyhydramnios as AFI ≥25 cm (18).
Advanced maternal age refers to pregnant women with a pre-delivery age ≥35 years; young maternal age refers to pregnant women with a pre-delivery age <35 years. According to the Chinese health industry standard WS/T 800-2022 on “Growth evaluation standards for neonates with different gestational ages at birth”, birth weight percentiles (<P3 & >P97) of different infant gender with a GA of 24–42 weeks combined with clinical diagnosis were used to define low birth weight and macrosomia (19).
Exclusion criteria
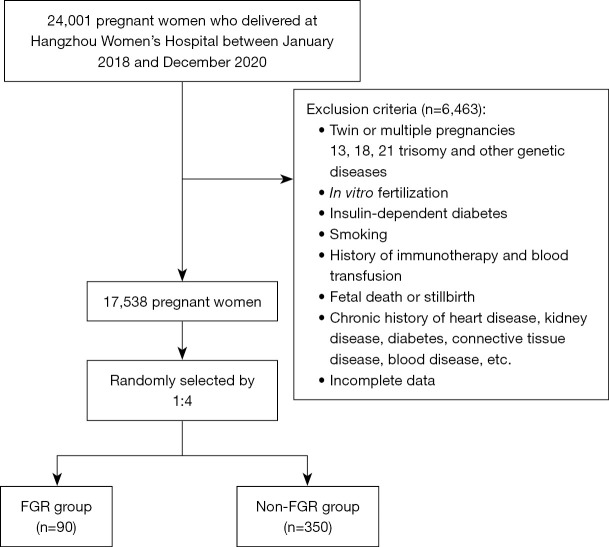
Exclusion criteria included: twin or multiple pregnancies; 13, 18, 21 trisomy and other genetic diseases; in vitro fertilization; insulin-dependent diabetes; smoking; history of immunotherapy and blood transfusion; fetal death or stillbirth; chronic history of heart disease, kidney disease, diabetes, connective tissue disease, blood disease, and so on; incomplete data (20) (see Figure 1).
Figure 1.
Flow chart of the study population. FGR, fetal growth restriction.
Study methods
Sampling and screening
Fasting venous blood samples (2–3 mL) were taken from pregnant women (9–13+6 weeks of gestation), separated for serum samples after 30 minutes, stored at 2–8 ℃, and submitted for examination in the prenatal screening laboratory of the hospital within 1 week. Screening markers and schemes were as follows: only maternal serum PAPP-A and free β-hCG were detected, or the levels of PAPP-A and free β-hCG were detected and then combined with the fetal NT thickness, which was measured by ultrasound.
Instruments and reagents
1235 Auto automatic time-resolved fluorescence immunoassay analyzer (PerkinElmer, Shelton, CT, USA), PAPP-A reagent, free β-hCG single kit, enhancer, lotion, quality control (PerkinElmer), and standard (WallacOy, Turku, Finland). The detection procedure was carried out according to the instructions. Ultrasound instrument (VolusonE8; GE, Boston, MA, USA).
NT thickness measurement method and screening criteria
During 11–13+6 weeks of gestation, ultrasound examination was performed by specially trained ultrasound doctors according to many industry standards and national standards (21) and was used to measure at the widest transparency between the skin and soft tissue on the cervical spine. NT thickness <3.50 mm was considered normal, ≥3.50 mm was considered abnormal.
Color Doppler ultrasound examination
The fetal chromosome index and preliminary morphology were screened with the pregnant women in a supine position. Transabdominal ultrasound was performed to examine the fetal heart; the length of the head and rump, the length of the head, the development of the limbs, the fetal heart, and the NT value and the condition of the nasal bone were monitored.
Quality control
All testing and follow-up personnel received pre-service training and obtained qualification certificates from health authorities. Low-value, median-value, and high-value, representing three different quality control serum specimens, were conducted as a part of internal quality control in the laboratories. External quality auditors participated in external quality assessment activities organized by the Clinical Laboratory Center of Ministry of Health twice a year and obtained certificates of qualification.
Expression of PAPP-A, free β-hCG, and NT level
Multiple of median (MoM) values were used to replace the original concentrations of serum indicators, which were calibrated by weight and GA. The algorithm of MoM (20): (Original Conj. was the original concentration value of PAPP-A, free β-hCG, or NT; Median indicated the median of the original concentration value).
Statistical analysis
Statistical analysis was performed using the software SPSS 21.0 (IBM Corp., Armonk, NY, USA). One-sample Kolmogorov-Smirnov test was used to test the data normality. The skewed distribution was expressed as median and percentile [M (P2.5–P97.5)], and the normal distribution was expressed as mean ± standard deviation (). Quantitative data were analyzed by Mann-Whitney test of independent samples, chi-square test was used for univariate analysis of qualitative data; P<0.05 was chosen as the selection criteria for modified Poisson regression analysis. Potential confounding variables were adjusted by relative risks (RRs) and 95% confidence interval (CI) of each related factor (all the independent variables that meet the requirements were inserted into the regression equation, and then gradually eliminated), with the following input indicators in the first step: parity, mode of delivery, infant gender, PE, gestational hypertension (GH), fetal distress, premature delivery, PROM, oligohydramnios, low birth weight, infant Apgar scores, infant length, PAPP-A, and MoM. Finally, FGR was assessed by RR. Cut-off and area under the curve (AUC) were determined via a receiver operating characteristic (ROC) curve to evaluate the diagnostic value of FGR, and the optimal cut-off, AUC, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (+LR), negative likelihood ratio (−LR), and Youden index were calculated. When P<0.05, the difference was statistically significant, and the risk model with the largest AUC and higher sensitivity had better diagnostic value.
Results
Demographic comparison between the FGR and Non-FGR groups of pregnant women
The maternal weight, height, age, and BMI in the first trimester of the FGR group were lower than those in the non-FGR group (63.00 vs. 67.00 kg, 158.00 vs. 160.00 cm, 28.00 vs. 29.00 years, 24.84 vs. 25.78 kg/m2), and the different results were statistically significant (Z=3.464, Z=2.987, Z=1.989, Z=2.108, all P<0.05). Maternal diastolic blood pressure (75.50 vs. 72.00 mmHg), mean arterial pressure (MAP; 90.00 vs. 87.00 mmHg), and gestational day (263.50 vs. 273.00 days) could affect the occurrence of FGR during pregnancy, and these were also statistically significant (Z=2.652, Z=2.492, Z=7.533, all P<0.05). In addition, there was also a statistical difference between the two groups in the parity and mode of delivery (χ2=4.818, χ2=33.463, both P<0.05). However, systolic blood pressure, gravidity, and advanced maternal age of pregnant women were not significantly different (P>0.05) (see Table 1 for details).
Table 1. Univariate demographic analysis of FGR group and non-FGR group.
| Indicators | Groups | Z/χ2 | P value | |
|---|---|---|---|---|
| Non-FGR (n=350) | FGR (n=90) | |||
| Maternal age (years) | 29.00 (24.00–34.00) | 28.00 (22.28–34.00) | 1.989 | 0.047** |
| Maternal weight (kg) | 67.00 (53.00–88.00) | 63.00 (49.00–91.73) | 3.464 | 0.001** |
| Body height (cm) | 160.00 (150.68–171.00) | 158.00 (151.00–171.80) | 2.987 | 0.003** |
| BMI (kg/m2) | 25.78 (21.17–32.91) | 24.84 (19.67–33.56) | 2.108 | 0.04** |
| SBP (mmHg) | 118.00 (99.00–139.48) | 118.00 (100.40–160.00) | 1.438 | 0.15 |
| DBP (mmHg) | 72.00 (59.00–94.48) | 75.50 (59.65–113.35) | 2.652 | 0.008** |
| MAP (mmHg) | 87.00 (74.68–108.98) | 90.00 (76.38–127.69) | 2.492 | 0.01** |
| Gestational age (days) | 273.00 (245.00–287.00) | 263.50 (207.03–280.00) | 7.553 | <0.001* |
| Gravidity | 0.459 | 0.50 | ||
| 1 | 204 (58.29) | 56 (62.22) | ||
| ≥2 | 146 (41.71) | 34 (37.78) | ||
| Parity | 4.818 | 0.03** | ||
| 0 | 252 (72.00) | 75 (83.33) | ||
| ≥1 | 98 (28.00) | 15 (16.67) | ||
| Mode of delivery | 33.463 | <0.001* | ||
| Natural childbirth | 249 (71.14) | 35 (38.89) | ||
| Cesarean section | 101 (28.86) | 55 (61.11) | ||
| Advanced maternal age | 1.038 | 0.31 | ||
| No | 346 (98.86) | 90 (100.00) | ||
| Yes | 4 (1.14) | 0 (0) | ||
The quantitative data were expressed by median and percentile [M (P2.5–P97.5)], while qualitative data were expressed by n (%). *, P<0.001; **, P<0.05. FGR, fetal growth restriction; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure [MAP =DBP + (SBP−DBP)/3].
Comparison of demographic details of the newborns between two groups
The birth weight, score, and length of the FGR group were lower than those of the non-FGR group (2,290 vs. 3,280 g, 10.00 vs. 10.00, 47.50 vs. 50.00 cm), indicating a statistically significant difference between the two groups (Z=13.492, Z=3.838, Z=12.991, all P<0.001). Female newborns were prone to FGR (65.56% vs. 34.44%; χ2=13.319, P<0.001), as shown in Table 2.
Table 2. Univariate demographic analysis of newborns in the FGR group and non-FGR group.
| Indicators | Groups | Z/χ2 | P value | |
|---|---|---|---|---|
| Non-FGR (n=350) | FGR (n=90) | |||
| Infant weight (g) | 3,280 (2,276–4,205) | 2,290 (960–2,980) | 13.492 | <0.001* |
| Infant length (cm) | 50.00 (46.78–52.00) | 47.50 (30.00–50.00) | 12.991 | <0.001* |
| Infant Apgar scores | 10.00 (9.00–10.00) | 10.00 (6.55–10.00) | 3.838 | <0.001* |
| Infant gender | 13.319 | <0.001* | ||
| Male | 196 (56.00) | 31 (34.44) | ||
| Female | 154 (44.00) | 59 (65.56) | ||
The quantitative data were expressed by median and percentile [M (P2.5–P97.5)], while qualitative data were expressed by n (%). *, P<0.001. FGR, fetal growth restriction.
Comparison of prenatal screening markers in early pregnancy
As shown in Table 3, the PAPP-A level and NT of the FGR group were lower than those of the non-FGR group [0.63 (0.12–2.08) vs. 1.01 (0.28–2.41) MoM, 1.30 (0.80–2.07) vs. 1.40 (0.80–2.20) cm], and the differences between the groups were statistically significant (Z=6.210 and 2.899, P<0.05). There were no significant differences in free β-hCG MoM and NT MoM between FGR group and non-FGR group in early pregnancy (all P>0.05). The concentrations of serum PAPP-A and free β-hCG were divided and subjected to the chi-square test, which revealed that in the FGR group, the PAPP-A level was less than 0.42 MoM, which was statistically significant (χ2=29.325, P<0.001).
Table 3. Comparison of early screening indicators in pregnant women in the FGR group and non-FGR group.
| Indicators | Groups | Z/χ2 | P value | |
|---|---|---|---|---|
| Non-FGR (n=350) | FGR (n=90) | |||
| PAPP-A (mU/L) | 4,175.00 (1,019.65–10,500.00) | 2,760.00 (354.00–4,295.00) | 4.921 | <0.001* |
| PAPP-A MoM | 1.01 (0.28–2.41) | 0.63 (0.12–2.08) | 6.210 | <0.001* |
| Free β-hCG (ng/mL) | 46.60 (18.31–226.25) | 54.30 (11.68–235.43) | 0.501 | 0.62 |
| Free β-hCG MoM | 0.98 (0.42–4.25) | 1.07 (0.23–3.77) | 0.178 | 0.86 |
| NT (cm) | 1.40 (0.80–2.20) | 1.30 (0.80–2.07) | 2.899 | 0.004** |
| NT MoM | 0.99 (0.59–1.61) | 0.95 (0.60–1.46) | 1.463 | 0.14 |
| PAPP-A (≤0.42 MoM) | 29.325 | <0.001* | ||
| No | 332 (94.86) | 69 (76.67) | ||
| Yes | 18 (5.14) | 21 (23.33) | ||
| Free β-hCG (≥2.50 MoM) | 0.272 | 0.60 | ||
| No | 172 (49.14) | 47 (52.22) | ||
| Yes | 178 (50.86) | 43 (47.78) | ||
| Free β-hCG (≤0.25 MoM) | 2.817 | 0.09 | ||
| No | 317 (90.57) | 76 (84.44) | ||
| Yes | 33 (9.43) | 14 (15.56) | ||
The quantitative data were expressed by median and percentile [M (P2.5–P97.5)], while qualitative data were expressed by n (%). *, P<0.001; **, P<0.05. FGR, fetal growth restriction; PAPP-A, pregnancy-associated plasma protein A; MoM, multiple of median; Free β-hCG, free beta subunit of human chorionic gonadotropin; NT, nuchal translucency.
Univariate analysis of perinatal characteristics and pregnancy outcomes
Table 4 shows that pregnancy complications and outcomes such as PE, GH, hyperlipidemia, fetal distress, premature delivery, oligohydramnios, and low birth weight in the FGR group and Non FGR group were related to FGR (all P<0.05); the other perinatal characteristics and pregnancy outcomes were not related to FGR (all P>0.05).
Table 4. Univariate analysis of pregnancy characteristics between the FGR group and non-FGR group.
| Pregnancy characteristics | Groups | χ2 | P value | |
|---|---|---|---|---|
| Non-FGR (n=350), n (%) | FGR (n=90), n (%) | |||
| Preeclampsia | 33.318 | <0.001* | ||
| No | 342 (98.57) | 74 (82.22) | ||
| Yes | 8 (1.43) | 16 (17.78) | ||
| Gestational hypertension | 10.001 | 0.002** | ||
| No | 339 (96.86) | 80 (88.89) | ||
| Yes | 11 (3.14) | 10 (11.11) | ||
| Intrahepatic cholestasis of pregnancy | 2.393 | 0.12 | ||
| No | 339 (96.86) | 84 (93.33) | ||
| Yes | 11 (3.14) | 6 (0.67) | ||
| Hyperlipidemia | 8.325 | 0.004** | ||
| No | 333 (95.14) | 88 (97.78) | ||
| Yes | 17 (4.86) | 2 (0.22) | ||
| Fetal distress | 11.752 | 0.001** | ||
| No | 318 (90.86) | 70 (77.78) | ||
| Yes | 32 (9.14) | 20 (22.22) | ||
| Premature delivery | 53.580 | <0.001* | ||
| No | 328 (93.71) | 59 (65.56) | ||
| Yes | 22 (6.29) | 31 (34.44) | ||
| GDM | <0.001 | 0.99 | ||
| No | 307 (87.71) | 79 (87.78) | ||
| Yes | 43 (12.29) | 11 (12.22) | ||
| Hypothyroidism | 0.267 | 0.61 | ||
| No | 321 (91.71) | 81 (90) | ||
| Yes | 29 (8.29) | 9 (10) | ||
| Anemia | 2.366 | 0.12 | ||
| No | 265 (75.71) | 75 (83.33) | ||
| Yes | 85 (24.29) | 15 (16.67) | ||
| Thrombocytopenia | 0.665 | 0.42 | ||
| No | 338 (96.57) | 89 (98.89) | ||
| Yes | 12 (3.43) | 1 (1.11) | ||
| Uterine inertia | 1.755 | 0.19 | ||
| No | 339 (96.86) | 90 (100) | ||
| Yes | 11 (3.14) | 0 (0) | ||
| Placenta previa | 2.713 | 0.10 | ||
| No | 348 (99.43) | 87 (96.67) | ||
| Yes | 2 (0.57) | 3 (3.33) | ||
| Polyhydramnios | <0.001 | >0.99 | ||
| No | 348 (99.43) | 90 (100) | ||
| Yes | 2 (0.57) | 0 (0) | ||
| Oligohydramnios | 37.112 | <0.001* | ||
| No | 333 (95.14) | 67 (74.44) | ||
| Yes | 17 (4.86) | 23 (25.56) | ||
| Low birth weight | 65.782 | <0.001* | ||
| No | 346 (98.86) | 69 (76.67) | ||
| Yes | 4 (1.14) | 21 (23.33) | ||
| Placental abruption | 0.027 | 0.87 | ||
| No | 347 (99.14) | 90 (100) | ||
| Yes | 53 (0.86) | 0 (0) | ||
*, P<0.001; **, P<0.05. FGR, fetal growth restriction; GDM, gestational diabetes mellitus.
Results of modified Poisson regression analysis
The results of modified Poisson regression analysis found that the RR of GH, PROM, oligohydramnios, low birth weight, female infant, infant length, and increased PAPP-A MoM were 1.836 (95% CI: 1.188–2.836), 0.641 (95% CI: 0.425–0.969), 1.420 (95% CI: 1.022–1.973), 1.609 (95% CI: 1.012–2.559), 1.539 (95% CI: 1.098–2.157), 5.700 (95% CI: 3.416–9.509), and 0.533 (95% CI: 0.369–0.769), respectively, all P<0.05, which were statistically associated with FGR (see Table 5).
Table 5. Modified Poisson regression analysis of maternal characteristics and pregnancy outcomes.
| Variables | β | SE | Wald | df | P value | RR (95% CI) |
|---|---|---|---|---|---|---|
| Parity | ||||||
| 0 | Reference | |||||
| ≥1 | 0.069 | 0.264 | 0.068 | 1 | 0.79 | 1.071 (0.639–1.796) |
| Mode of delivery | ||||||
| Natural childbirth | Reference | |||||
| Cesarean section | −0.222 | 0.206 | 1.161 | 1 | 0.28 | 0.801 (0.535–1.199) |
| Infant gender | ||||||
| Male | Reference | |||||
| Female | 0.431 | 0.172 | 6.267 | 1 | 0.01** | 1.539 (1.098–2.157) |
| Preeclampsia | ||||||
| No | Reference | |||||
| Yes | 0.296 | 0.244 | 1.469 | 1 | 0.23 | 1.344 (0.833–2.170) |
| Gestational hypertension | ||||||
| No | Reference | |||||
| Yes | 0.607 | 0.222 | 7.491 | 1 | 0.006** | 1.836 (1.188–2.836) |
| Fetal distress | ||||||
| No | Reference | |||||
| Yes | 0.253 | 0.198 | 1.631 | 1 | 0.20 | 1.287 (0.874–1.897) |
| Premature delivery | ||||||
| No | Reference | |||||
| Yes | 0.110 | 0.216 | 0.258 | 1 | 0.61 | 1.116 (0.730–1.705) |
| PROM | ||||||
| No | Reference | |||||
| Yes | -0.444 | 0.210 | 4.453 | 1 | 0.04** | 0.641 (0.425–0.969) |
| Oligohydramnios | ||||||
| No | Reference | |||||
| Yes | 0.351 | 0.168 | 4.365 | 1 | 0.04** | 1.420 (1.022–1.973) |
| Low birth weight | ||||||
| No | Reference | |||||
| Yes | 0.476 | 0.237 | 4.041 | 1 | 0.044** | 1.609 (1.012–2.559) |
| Infant Apgar scores | ||||||
| 10 | Reference | |||||
| <10 | 0.187 | 0.214 | 0.759 | 1 | 0.38 | 1.205 (0.792–1.833) |
| Infant length (cm) | ||||||
| ≥50 | Reference | |||||
| <50 | 1.740 | 0.261 | 44.407 | 1 | <0.001* | 5.700 (3.416–9.509) |
| PAPP-A MoM | −0.630 | 0.187 | 11.317 | 1 | 0.001** | 0.533 (0.369–0.769) |
Variable (s) entered on step 1: Parity; Mode of delivery; Infant gender; Preeclampsia; Gestational hypertension; Fetal distress; Premature delivery; PROM; Oligohydramnios; Low birth weight; Infant Apgar scores; Infant length (cm); PAPP-A MoM; *, P<0.001; **, P<0.05. SE, standard error; RR, relative risk; 95% CI, 95% confidence interval; PROM, premature rupture of membranes; PAPP-A, pregnancy-associated plasma protein A; MoM, multiple of median.
Diagnostic value of PAPP-A, free β-hCG, NT, or their combination in predicting FGR
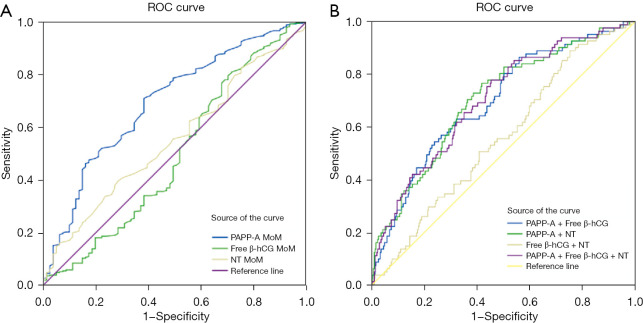
The ROC curves of PAPP-A MoM, PAPP-A + free β-hCG, PAPP-A + NT, and PAPP-A + free β-hCG + NT showed that the AUCs for FGR were 0.695 (95% CI: 0.630–0.760), 0.695 (95% CI: 0.631–0.759), 0.703 (95% CI: 0.639–0.767), and 0.702 (95% CI: 0.639–0.765), all P<0.05. When the cut off was MoM 0.745, 0.241, 0.201, and 0.190, the corresponding specificity was 0.617, 0.678, 0.582, and 0.547 respectively, and the sensitivity was 0.711, 0.630, 0.765, and 0.778, respectively. After increasing the free β-hCG, the PPV and NPV of PAPP-A + free β-hCG was 0.662 and 0.647, but the +LR was 1.957, and the −LR was 0.546 (see Table 6 and Figure 2).
Table 6. The value of PAPP-A, and combined above index screening for the FGR.
| Index | Youden | Sensitivity | Specificity | Cut-off | AUC | 95% CI | P value | PPV | NPV | FPR | FNR | +LR | −LR |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PAPP-A MoM | 0.328 | 0.711 | 0.617 | 0.745 | 0.695 | 0.630–0.760 | <0.001* | 0.650 | 0.681 | 0.383 | 0.289 | 1.856 | 0.468 |
| Free-β hCG MoM | 0.094 | 0.810 | 0.284 | 0.625 | 0.495 | 0.418–0.572 | 0.89 | 0.531 | 0.599 | 0.716 | 0.190 | 1.131 | 0.669 |
| NT MoM | 0.112 | 0.395 | 0.716 | 1.075 | 0.553 | 0.485–0.620 | 0.14 | 0.582 | 0.542 | 0.284 | 0.605 | 1.391 | 0.845 |
| PAPP-A + free-β hCG | 0.308 | 0.630 | 0.678 | 0.241 | 0.695 | 0.631–0.759 | <0.001* | 0.662 | 0.647 | 0.322 | 0.370 | 1.957 | 0.546 |
| PAPP-A + NT | 0.347 | 0.765 | 0.582 | 0.201 | 0.703 | 0.639–0.767 | <0.001* | 0.647 | 0.712 | 0.418 | 0.235 | 1.830 | 0.404 |
| Free-β hCG + NT | 0.136 | 0.889 | 0.248 | 0.181 | 0.558 | 0.491–0.625 | 0.11 | 0.542 | 0.691 | 0.752 | 0.111 | 1.182 | 0.448 |
| PAPP-A + free-β hCG + NT | 0.324 | 0.778 | 0.547 | 0.190 | 0.702 | 0.639–0.765 | <0.001* | 0.632 | 0.711 | 0.453 | 0.222 | 1.717 | 0.406 |
*, P<0.001. PAPP-A, pregnancy associated plasma protein A; FGR, fetal growth restriction; AUC, area under the curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value; FNR, false negative rate; FPR, false positive rate; +LR, positive likelihood ratio; −LR, negative likelihood ratio; MoM, multiple of median; Free β-hCG, free beta subunit of human chorionic gonadotropin; NT, nuchal translucency.
Figure 2.
Maternal markers alone or in combination predict the ROC curve of fetal growth restriction. (A) The ROC curves for PAPP-A MoM, free β-hCG MoM, or NT MoM, respectively. (B) ROC curves for combined prediction models of various associated PAPP-A, free β-hCG or NT. ROC, receiver operating characteristic; PAPP-A, pregnancy-associated plasma protein A; Free β-hCG, free beta subunit of human chorionic gonadotropin; NT, nuchal translucency; MoM, multiple of median.
Discussion
FGR is a common pregnancy complication, which poses a serious threat to the life and safety of the fetus. Currently, the etiology of FGR remains unknown, and there is no targeted intervention method available. The clinical diagnosis of FGR mostly depends on the ultrasonic detection of the fetus in the middle and late pregnancy, meaning that preventive measures against FGR could not be taken in the first trimester (22). Therefore, it is very important to explore the indicators that have predictive value for FGR in early pregnancy to facilitate early prediction and intervention. The main findings of this study were that serum PAPP-A levels were significantly decreased in pregnant women with FGR in the first trimester, and the following related characteristics appeared in late pregnancy: decreased BMI, placental diseases such as PE and PROM, and low birth weight and low infant length. Some risk models incorporating PAPP-A and PAPP-A + maternal serum indicators could predict FGR.
This study showed that serum PAPP-A was significantly lower in the FGR group (P<0.001), which was in the accordance with previous reports (23-25). Maternal serum PAPP-A was decreased in early pregnancy, but the risk of having a fetus with FGR was increased (RR =0.533). PAPP-A is a syncytial trophoblast-derived metalloproteinase, which splits the complex formed between insulin-like growth factor and insulin-like growth factor binding protein. The maternal serum PAPP-A level is related to various diseases, such as stillbirth, premature delivery, PE, and some chromosomal diseases (22). As shown in Table 3, the ratio of PAPP-A ≤0.42 MoM was 23.33% in the FGR group, higher than the 5.14% in the non-FGR group, P<0.001, indicating that low-concentration PAPP-A was prone to FGR, which aligned with the results of Mohamad et al. (26).
In this study, the qualitative classification of free β-hCG was analyzed. The results indicated that the proportion of free β-hCG ≤0.25 MoM in the FGR group was 15.56% higher than the 9.43% in the non-FGR group (P=0.093). Similarly, Goetzinger et al. (27) showed that free β-hCG MoM >90th percentile could well predict FGR among Black women (P=0.04). When free β-hCG MoM >95th percentile, only a small number of patients had FGR in the cohort (P=0.26). The poor value of free β-hCG in predicting FGR may be because low levels of hCG imply poor development of gestational trophoblast cells, fetal FGR, or in some populations, poor placental environment is the pathophysiological basis for elevated levels of free β-hCG, which also causes FGR. This requires continuous discussion and research in the future (28,29).
Table 6 shows that the AUC of PAPP-A in predicting FGR was 0.695, similar to the predictive value of PAPP-A <0.40 MoM (AUC was 0.705) as reported by Mohamad et al. (26). We assumed that the addition of maternal serum indicators such as free β-hCG and NT combined with PAPP-A could improve the diagnostic value of predicting FGR. The AUC of free β-hCG MoM or NT MoM alone for predicting FGR was 0.495 and 0.553, respectively, whereas the AUC of PAPP-A + free β-hCG + NT for predicting FGR was 0.702, but the specificity of the combined index was reduced. The +LR and −LR were both slightly decreased, the PPV was slightly decreased, and the NPV was slightly increased, so the value of maternal free β-hCG and NT combined with PAPP-A in predicting FGR was similar to that of PAPP-A alone.
This study also showed that the RR of low infant length and low birth weight were 5.700 and 1.609, respectively, so we interpreted that when FGR occurs, the changes of low birth weight are higher. In this paper, the RR of preterm birth was 1.116, P>0.05, but there were several reports indicating that preterm birth was significantly associated with FGR (30), which usually manifested as fetal ultrasonographic estimated weight or abdominal circumference below the 10th percentile for GA (1). In univariate analysis, there was a certain difference in the occurrence of FGR in pregnant women with different BMI (P=0.04). In other study of FGR, low BMI pregnant women had a 2.80-fold increased risk of giving birth to low weight infants (P=0.02), and low birth weight infants had a higher risk of obesity, diabetes, and cardiovascular disease in adulthood (31,32). However, Lewandowska et al. (33) reported that there was a U-shaped relationship between FGR and BMI, and too high or too low BMI could increase the risk of FGR. In addition, FGR could trigger the development of adaptive responses, including increased vascular tension and hyperinsulinemia, which further increased the occurrence of susceptible hypertension (34). This study also confirmed that hypertension during pregnancy was a risk factor for FGR (RR =1.836).
Placental-mediated FGR is caused by chronic fetal hypoxia resulting from poor placental perfusion, and its mechanisms are diverse. Researchers have also considered ischemic placenta and placental implantation to be related to IUGR, postpartum hemorrhage, PE (mainly premature delivery), and placental abruption (35,36).
The Society of Obstetricians and Gynaecologists of Canada (SOGC) clinical practice guidelines [2014] still list FGR as a placental adverse condition and consider it a serious complication of PE (37). In the current study, the incidence of PE in the FGR group was higher than that in the non-FGR group (17.78% vs. 1.43%, P<0.001), but Poisson regression analysis showed that there was no significant correlation between PE in pregnant women with FGR. We also found that maternal oligohydramnios (RR =1.420) was an exposure factor for FGR. According to the previous study of Spinillo et al. (38), in pregnant women with FGR, oligohydramnios was directly related to histological features such as placental hypoperfusion, fecal contamination of fetal membranes, and fetal blood vessel injury, which showed that oligohydramnios was also a placenta-related pregnancy disease. Balayla et al. (39) pointed out in multiple systematic reviews and meta-analyses of placenta previa that compared with cases with different placenta locations, placenta previa pregnancy had a slightly increased risk of FGR [odds ratio (OR) =1.190]. Therefore, the placental diseases found in these studies were related to FGR, similar to the results of placenta-related maternal complications in this study.
Compared with male fetuses (RR =1.539), female fetuses were more likely to develop FGR. A study reported that the gender dimorphic pattern of microRNA (miRNA) in the serum of pregnant women with FGR and the different susceptibility of male and female fetuses to intrauterine adverse conditions might make miRNA a biomarker for FGR and relative placental dysfunction (40).
According to the early perinatal characteristics of pregnant women and related serological indicators, combined with clinical Doppler indicators, it is possible to preliminarily determine whether a pregnant woman has FGR (41). However, aspirin could alleviate placenta-mediated pregnancy complications including PE and FGR. The most widely used strategy for aspirin has been clinical risk stratification according to the medical history, with women with a history of PE or underlying conditions considered to be at high risk. Women with placenta-related FGR such as that of PE pathology could use aspirin alleviate FGR (42). Studies have pointed out that before 16 weeks of pregnancy, taking low-dose aspirin can significantly reduce the risk of FGR (RR =0.56, 95% CI: 0.44–0.70, P<0.001) (43).
This study has some limitations: (I) there were only 90 cases of FGR, and the statistical heterogeneity between studies was also large. The characteristics of the population, or namely, the baseline data, vary greatly. (II) It was well known that smoking is the main predictive factor for FGR. However, the number of smoking pregnant women was low and there was no growth delay in this study, so it was difficult to verify the effect of smoking on pregnancy outcomes (44). (III) A low birth weight in a previous pregnancy was a major risk factor for FGR, but the data were not available in this study. (IV) This study involved a single center, and its causal relationship needs to be confirmed by further multi-center prospective studies.
Conclusions
The decrease of serum PAPP-A level in early pregnancy can predict FGR, and maternal serum free β-hCG or NT combined with PAPP-A could improve the diagnostic sensitivity of FGR. Pregnant women with FGR are more likely to have decreased BMI and placental disease such as GH. In addition, low birth weight and low infant length are prone to occur.
Prenatal screening markers in early pregnancy combined with perinatal characteristics can predict FGR, which can enable early intervention against the occurrence of FGR in pregnant women and provide a theoretical basis for perinatal health care, and provide a scientific basis for the clinical use of low-dose aspirin to prevent FGR.
Supplementary
The article’s supplementary files as
Acknowledgments
The authors are grateful to all of the participants and contributors. We would like to thank Songhe Chen from Hangzhou Women’s Hospital for helping to collect the data. We would also like to thank Xiao Lu of the Data Analysis Department, Zhejiang Biosan Biochemical Technologies Co., Ltd., for his contribution to data matching.
Funding: This study was supported by Hangzhou Medicine and Health Science and Technology Plan Project (No. A202301168).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Human Research Ethics Committee of the Hangzhou Women’s Hospital (No. Medical Ethics Review 2023-032) and informed consent was taken from all the patients.
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-24-58/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-24-58/coif). The authors have no conflicts of interest to declare.
(English Language Editor: J. Jones)
Data Sharing Statement
Available at https://tp.amegroups.com/article/view/10.21037/tp-24-58/dss
References
- 1.ACOG Practice Bulletin No . 204: Fetal Growth Restriction. Obstet Gynecol 2019;133:e97-e109. 10.1097/AOG.0000000000003070 [DOI] [PubMed] [Google Scholar]
- 2.Albu AR, Anca AF, Horhoianu VV, et al. Predictive factors for intrauterine growth restriction. J Med Life 2014;7:165-71. [PMC free article] [PubMed] [Google Scholar]
- 3.Darendeliler F. IUGR: Genetic influences, metabolic problems, environmental associations/triggers, current and future management. Best Pract Res Clin Endocrinol Metab 2019;33:101260. 10.1016/j.beem.2019.01.001 [DOI] [PubMed] [Google Scholar]
- 4.Audette MC, Kingdom JC. Screening for fetal growth restriction and placental insufficiency. Semin Fetal Neonatal Med 2018;23:119-25. 10.1016/j.siny.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 5.Saenger P, Czernichow P, Hughes I, et al. Small for gestational age: short stature and beyond. Endocr Rev 2007;28:219-51. 10.1210/er.2006-0039 [DOI] [PubMed] [Google Scholar]
- 6.Sharma D, Sharma P, Shastri S. Genetic, metabolic and endocrine aspect of intrauterine growth restriction: an update. J Matern Fetal Neonatal Med 2017;30:2263-75. 10.1080/14767058.2016.1245285 [DOI] [PubMed] [Google Scholar]
- 7.Ormesher L, Warrander L, Liu Y, et al. Risk stratification for early-onset fetal growth restriction in women with abnormal serum biomarkers: a retrospective cohort study. Sci Rep 2020;10:22259. 10.1038/s41598-020-78631-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.He B, Hu C, Zhou Y. First-trimester screening for fetal growth restriction using Doppler color flow analysis of the uterine artery and serum PAPP-A levels in unselected pregnancies. J Matern Fetal Neonatal Med 2021;34:3857-61. 10.1080/14767058.2019.1701646 [DOI] [PubMed] [Google Scholar]
- 9.Karagiannis G, Akolekar R, Sarquis R, et al. Prediction of small-for-gestation neonates from biophysical and biochemical markers at 11-13 weeks. Fetal Diagn Ther 2011;29:148-54. 10.1159/000321694 [DOI] [PubMed] [Google Scholar]
- 10.ACOG Practice bulletin no. 134: fetal growth restriction. Obstet Gynecol 2013;121:1122-33. 10.1097/01.AOG.0000429658.85846.f9 [DOI] [PubMed] [Google Scholar]
- 11.Fetal Growth Restriction : ACOG Practice Bulletin, Number 227. Obstet Gynecol 2021;137:e16-28. 10.1097/AOG.0000000000004251 [DOI] [PubMed] [Google Scholar]
- 12.Chinese Medical Association Obstetrics and Gynecology Branch Pregnancy Hypertension Disease Group . Guidelines for Diagnosis and Treatment of Hypertension during Pregnancy (2015). Chinese Journal of Obstetrics and Gynecology 2015;50:721-8. [Google Scholar]
- 13.Obstetrics Subgroup,Chinese Society of Obstetrics and Gynecology, Chinese Medical Association . Guidelines for diagnosis and treatment of intrahepatic cholestasis of pregnancy (2015). Zhonghua Fu Chan Ke Za Zhi 2015;50:481-5. [PubMed] [Google Scholar]
- 14.International Association of Diabetes and Pregnancy Study Groups Consensus Panel ; Metzger BE, Gabbe SG, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010;33:676-82. 10.2337/dc09-1848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Practice bulletins No. 139: premature rupture of membranes. Obstet Gynecol 2013;122:918-30. 10.1097/01.AOG.0000435415.21944.8f [DOI] [PubMed] [Google Scholar]
- 16.Committee on Obstetric Practice, American College of Obstetricians and Gynecologists . ACOG Committee Opinion. Number 326, December 2005. Inappropriate use of the terms fetal distress and birth asphyxia. Obstet Gynecol 2005;106:1469-70. 10.1097/00006250-200512000-00056 [DOI] [PubMed] [Google Scholar]
- 17.Chinese Society of Obstetrics and Gynecology, Chinese Medical Association . Guidelines for clinical diagnosis and treatment of preterm birth (2014). Chin J Perinatology 2015;18:241-5. [Google Scholar]
- 18.Whelan AR, Has P, Savitz DA, et al. Neonatal Outcomes Are Similar between Patients with Resolved and Those with Persistent Oligohydramnios. Am J Perinatol 2024;41:1285-9. 10.1055/a-2278-8948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Health industry standards of the People's Republic of China, WS/T 800-2022 Growth evaluation standards for neonates with different gestational ages at birth, Health Commission of China, 2022. [Google Scholar]
- 20.Dai X, Zhang H, Wu B, et al. Correlation between elevated maternal serum alpha-fetoprotein and ischemic placental disease: a retrospective cohort study. Clin Exp Hypertens 2023;45:2175848. 10.1080/10641963.2023.2175848 [DOI] [PubMed] [Google Scholar]
- 21.Huang J, Wu D, He JH, et al. Associations between genomic aberrations, increased nuchal translucency, and pregnancy outcomes: a comprehensive analysis of 2,272 singleton pregnancies in women under 35. Front Med (Lausanne) 2024;11:1376319. 10.3389/fmed.2024.1376319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Farzad Mohajeri Z, Aalipour S, Sheikh M, et al. Ultrasound measurement of fetal adrenal gland in fetuses with intrauterine growth restriction, an early predictive method for adverse outcomes. J Matern Fetal Neonatal Med 2019;32:1485-91. 10.1080/14767058.2017.1410125 [DOI] [PubMed] [Google Scholar]
- 23.Sifakis S, Androutsopoulos VP, Pontikaki A, et al. Placental expression of PAPPA, PAPPA-2 and PLAC-1 in pregnacies is associated with FGR. Mol Med Rep 2018;17:6435-40. 10.3892/mmr.2018.8721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Antsaklis P, Fasoulakis Z, Theodora M, et al. Association of Low Maternal Pregnancy-associated Plasma Protein A with Adverse Perinatal Outcome. Cureus 2019;11:e4912. 10.7759/cureus.4912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kirkegaard I, Uldbjerg N, Oxvig C. Biology of pregnancy-associated plasma protein-A in relation to prenatal diagnostics: an overview. Acta Obstet Gynecol Scand 2010;89:1118-25. 10.3109/00016349.2010.505639 [DOI] [PubMed] [Google Scholar]
- 26.Mohamad Jafari R, Masihi S, Barati M, et al. Value of Pregnancy-Associated Plasma Protein-A for Predicting Adverse Pregnancy Outcome. Arch Iran Med 2019;22:584-7. [PubMed] [Google Scholar]
- 27.Goetzinger KR, Singla A, Gerkowicz S, et al. The efficiency of first-trimester serum analytes and maternal characteristics in predicting fetal growth disorders. Am J Obstet Gynecol 2009;201:412.e1-6. 10.1016/j.ajog.2009.07.016 [DOI] [PubMed] [Google Scholar]
- 28.Hansen YB, Myrhøj V, Jørgensen FS, Oxvig C, Sørensen S. First trimester PAPP-A2, PAPP-A and hCGβ in small-for-gestational-age pregnancies. Clin Chem Lab Med 2016;54:117-23. 10.1515/cclm-2015-0230 [DOI] [PubMed] [Google Scholar]
- 29.Honarjoo M, Zarean E, Tarrahi MJ, et al. Role of pregnancy-associated plasma protein A (PAPP-A) and human-derived chorionic gonadotrophic hormone (free β-hCG) serum levels as a marker in predicting of Small for gestational age (SGA): A cohort study. J Res Med Sci 2021;26:104. 10.4103/jrms.JRMS_560_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jiang M, Mishu MM, Lu D, et al. A case control study of risk factors and neonatal outcomes of preterm birth. Taiwan J Obstet Gynecol 2018;57:814-8. 10.1016/j.tjog.2018.10.008 [DOI] [PubMed] [Google Scholar]
- 31.Johnson CD, Jones S, Paranjothy S. Reducing low birth weight: prioritizing action to address modifiable risk factors. J Public Health (Oxf) 2017;39:122-31. 10.1093/pubmed/fdv212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agnihotri B, Antonisamy B, Priya G, et al. Trends in human birth weight across two successive generations. Indian J Pediatr 2008;75:111-7. 10.1007/s12098-008-0066-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lewandowska M. Maternal Obesity and Risk of Low Birth Weight, Fetal Growth Restriction, and Macrosomia: Multiple Analyses. Nutrients 2021;13:1213. 10.3390/nu13041213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chatmethakul T, Roghair RD. Risk of hypertension following perinatal adversity: IUGR and prematurity. J Endocrinol 2019;242:T21-32. 10.1530/JOE-18-0687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berezowsky A, Pardo J, Ben-Zion M, et al. Second Trimester Biochemical Markers as Possible Predictors of Pathological Placentation: A Retrospective Case-Control Study. Fetal Diagn Ther 2019;46:187-92. 10.1159/000492829 [DOI] [PubMed] [Google Scholar]
- 36.Dinglas C, Afsar N, Cochrane E, et al. First-trimester maternal serum alpha fetoprotein is associated with ischemic placental disease. Am J Obstet Gynecol 2020;222:499.e1-6. 10.1016/j.ajog.2019.11.1264 [DOI] [PubMed] [Google Scholar]
- 37.Jain V. Letter to the Editor: Diagnosis, Evaluation, and Management of the Hypertensive Disorders of Pregnancy: Executive Summary. J Obstet Gynaecol Can 2015;37:774-5. [DOI] [PubMed] [Google Scholar]
- 38.Spinillo A, Cesari S, Bariselli S, et al. Placental lesions associated with oligohydramnios in fetal growth restricted (FGR) pregnancies. Placenta 2015;36:538-44. 10.1016/j.placenta.2015.02.007 [DOI] [PubMed] [Google Scholar]
- 39.Balayla J, Desilets J, Shrem G. Placenta previa and the risk of intrauterine growth restriction (IUGR): a systematic review and meta-analysis. J Perinat Med 2019;47:577-84. 10.1515/jpm-2019-0116 [DOI] [PubMed] [Google Scholar]
- 40.Baker BC, Lui S, Lorne I, et al. Sexually dimorphic patterns in maternal circulating microRNAs in pregnancies complicated by fetal growth restriction. Biol Sex Differ 2021;12:61. 10.1186/s13293-021-00405-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Loussert L, Vidal F, Parant O, et al. Aspirin for prevention of preeclampsia and fetal growth restriction. Prenat Diagn 2020;40:519-27. 10.1002/pd.5645 [DOI] [PubMed] [Google Scholar]
- 42.Burton GJ, Jauniaux E. Pathophysiology of placental-derived fetal growth restriction. Am J Obstet Gynecol 2018;218:S745-61. 10.1016/j.ajog.2017.11.577 [DOI] [PubMed] [Google Scholar]
- 43.Roberge S, Nicolaides K, Demers S, et al. The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis. Am J Obstet Gynecol 2017;216:110-120.e6. 10.1016/j.ajog.2016.09.076 [DOI] [PubMed] [Google Scholar]
- 44.Lewandowska M, Więckowska B, Sztorc L, et al. Smoking and Smoking Cessation in the Risk for Fetal Growth Restriction and Low Birth Weight and Additive Effect of Maternal Obesity. J Clin Med 2020;9:3504. 10.3390/jcm9113504 [DOI] [PMC free article] [PubMed] [Google Scholar]