Abstract
Background
Model for end-stage liver disease (MELD) is an effective predictive marker for renal, hepatic, and cardiac dysfunctions. In this study, we explore the correlation between MELD scores and the outcomes of patients undergoing cardiac valve surgery.
Methods
We conducted a retrospective analysis of clinical data from patients who underwent cardiac valve surgery, encompassing procedures on the aortic valve, mitral valve, and tricuspid valve, using the Informative Surgical Patient dataset for Innovative Research Environment (INSPIRE) database, we conducted receiver operating characteristic (ROC) analyses on the study participants and chose MELD as the primary scoring tool for our study due to its optimal area under the curve (AUC), patients were stratified into high (MELD ≥18) and low (MELD <18) groups based on the determined cutoff value. The perioperative clinical data of the two groups were compared.
Results
The analysis revealed 751 patients in the low MELD group (75.5%) and 244 patients (24.5%) in the high MELD group. Patients in the high MELD group exhibited a lower body mass index (BMI) compared to those in the low MELD group. In comparison to the low MELD group, the high MELD group exhibited a higher rate of emergency surgery (10.66% vs. 5.99%, P=0.01), along with prolonged anesthesia time, surgery time, and cardiopulmonary bypass (CPB) time. Regarding clinical prognosis, the high MELD group demonstrated a higher 28-day mortality rate (10.66% vs. 0.8%, P<0.001), as also observed in the analysis of three valve subgroups. Additionally, the high MELD group experienced longer hospitalization and intensive care unit (ICU) stay, and a higher proportion of patients requiring mechanical circulatory support, including intra-aortic balloon pump (IABP) assist (14.75% vs. 3.86%, P<0.001), extracorporeal membrane oxygenation (ECMO) assist (7.38% vs. 0.8%, P<0.001), and continuous renal replacement therapy (CRRT) (27.87% vs. 1.46%, P<0.001) post-surgery. The Kaplan-Meier survival curves illustrated a significantly lower mortality rate in the low MELD group compared to the high MELD group, with highly significant statistical differences (P<0.001).
Conclusions
The MELD score demonstrates a robust predictive value for clinical outcomes following cardiac valve surgery, underscoring its utility as a viable metric for disease stratification research.
Keywords: Model for end-stage liver disease (MELD), disease classification, cardiac valve surgery
Highlight box.
Key findings
• Model for end-stage liver disease (MELD) score demonstrates a robust predictive value for clinical outcomes following cardiac valve surgery, underscoring its utility as a viable metric for disease stratification research.
What is known and what is new?
• MELD score serves as indicators of multisystem dysfunction and coagulopathy and play a pivotal role in identifying individuals at an elevated risk of experiencing renal failure and hepatic dysfunction, particularly during the perioperative period of heart transplantation and aortic dissection.
• In this study, we explore the correlation between MELD score and the outcomes of patients undergoing cardiac valve surgery.
What is the implication, and what should change now?
• MELD score plays an important predictive value in perioperative cardiac valve surgery and can effectively guide disease stratification. Dynamic MELD score during perioperative period may bring positive clinical results.
Introduction
Over the past three decades, the primary gauge of hepatic dysfunction (HD) has been the Child-Turcotte-Pugh (CTP) classification (1). However, the CTP score incorporates subjective indicators, thereby limiting its applicability in medical studies. Recently, the model for end-stage liver disease (MELD) has emerged as the predominant scoring system for prioritizing patients on the liver transplantation waiting list. The MELD score, encompassing both liver and renal function, has become a widely used prognostic tool for individuals with liver disease (2). Calculated using baseline serum creatinine, serum total bilirubin, and international normalized ratio (INR) for prothrombin time, the MELD score, initially designed for end-stage liver disease patients, has also been proposed as an effective predictive marker for renal, hepatic, and cardiac dysfunctions (3,4).
The variables composing the MELD score serve as indicators of multisystem dysfunction and coagulopathy. They play a pivotal role in identifying individuals at an elevated risk of experiencing renal failure and right ventricular failure (5), particularly during the perioperative period of heart transplantation and aortic dissection (6-8). In this study, we explore the correlation between MELD scores and the outcomes of patients undergoing cardiac valve surgery. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-242/rc).
Methods
Study design
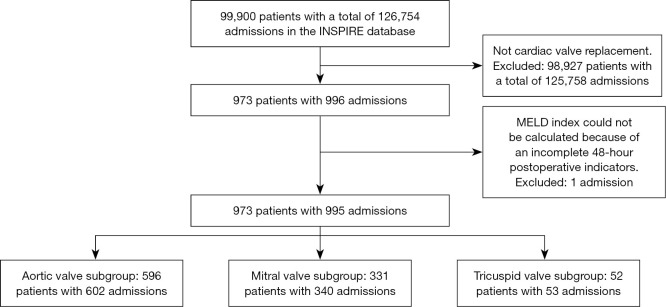
We conducted a retrospective analysis of clinical data from patients who underwent cardiac valve surgery, encompassing procedures on the aortic valve, mitral valve, and tricuspid valve, using the Informative Surgical Patient dataset for Innovative Research Environment (INSPIRE) database (9). This database comprises records of all individuals undergoing systemic, intraspinal, and regional anesthesia surgeries at Seoul National University Hospital from January 2011 to December 2020. The study’s inclusion criteria were as follows: (I) patients who underwent open-heart valve replacement surgery (aortic valve, mitral valve, tricuspid valve); (II) patients aged 18 years or older. Exclusion criteria were defined as: patients with incomplete clinical data. The flow chart illustrating the patient screening process is depicted in Figure 1. At the initiation of our study, the INSPIRE database contained a total of 99,900 patients with 126,754 hospitalizations. In our approach, the same patient with different admissions was considered as two cases, while the same hospitalization with multiple surgeries is considered as one case. After excluding patients who underwent non-heart valve replacement surgery and one patient with incomplete clinical data, our study included a total of 973 patients with 995 hospitalizations. This encompassed 596 patients with 602 admissions for aortic valve surgery, 331 patients with 340 admissions for mitral valve surgery, and 52 patients with 53 admissions for tricuspid valve surgery. There were 6 patients who had two different procedures in two hospitalizations, so they overlapped in the subgroup, so the sum was greater than the total above.
Figure 1.
The flowchart of study. INSPIRE, Informative Surgical Patient dataset for Innovative Research Environment; MELD, model for end-stage liver disease.
Ethical statement
Approval for this study was obtained from the Committee on Ethics of Biomedical Research at Shanghai East Hospital, Tongji University School of Medicine, Shanghai (No. TJUSM2023-010), with a waiver for individual patient consent. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Data collection
We gathered comprehensive data on patients, encompassing demographic details such as age, sex, body mass index (BMI), and an array of laboratory test results including albumin, leukocytes, troponin, alanine transaminase (ALT), aspartate transaminase (AST), oxygen partial pressure (PaO2), partial pressure of carbon dioxide (PaCO2), base excess, C-reactive protein (CRP), among others. Surgical conditions, such as the method of anesthesia, emergency surgery status, operation time, extracorporeal circulation time, and more, were also documented as part of the study.
The postoperative clinical outcomes recorded included parameters such as postoperative 28-day mortality, occurrences of pneumonia, duration of stay in the intensive care unit (ICU), and the necessity for interventions like continuous renal replacement therapy (CRRT), extracorporeal membrane oxygenation (ECMO), intra-aortic balloon pump (IABP), and others.
Definitions and grouping
Currently, there exist various MELD scores and their modified versions, detailed as follows:
| [1] |
| [2] |
| [3] |
| [4] |
These equations represent different formulations of the MELD score, each designed to assess liver function and predict outcomes in patients with liver disease.
We conducted receiver operating characteristic (ROC) analyses using the four scores on the study participants, and the specific results are depicted in Figure 2. Prognostic assessment and area under the curve (AUC) comparison of the four scores, MELD emerged as the primary scoring tool for our study due to its optimal AUC. Using the optimal cut-off point of 18 obtained from its ROC analysis, patients were categorized into two groups. Biochemical indicators (bilirubin, creatinine, INR) within 48 hours of admission to the ICU were utilized for scoring. Patients were then stratified into high (MELD ≥18) and low (MELD <18) groups based on the determined cutoff value. Subsequently, we conducted an in-depth analysis of the clinical baseline data and perioperative clinical prognosis outcomes for the two patient groups.
Figure 2.
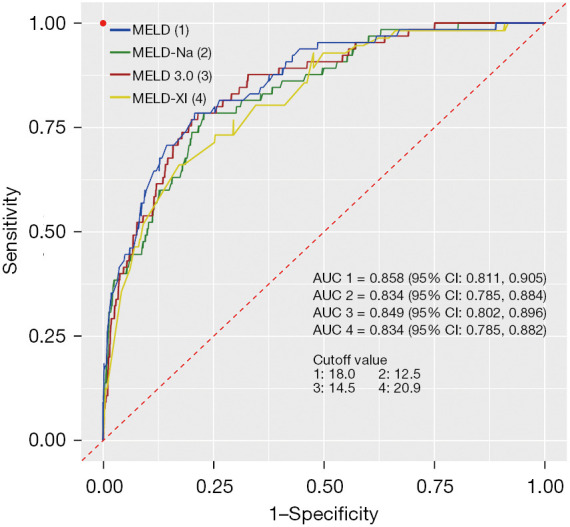
The ROC analyses of four scores. MELD, model for end-stage liver disease; AUC, area under the curve; ROC, receiver operating characteristic.
Statistical analysis
All data were subjected to statistical analysis using Statistical Package for the Social Science (SPSS) 29.0 software. ROC curve was employed to determine the optimal critical value of the MELD score for predicting the prognosis of patients undergoing open cardiac valve surgery. Additionally, survival curves for the two patient groups were generated and analyzed. For normally distributed measurement data, values were presented as mean ± standard deviation, and comparisons were performed using independent sample t-tests. For non-normally distributed measurement data, a description was provided using quartiles [median (P25, P75)], and statistical calculations were performed using non-parametric tests. Counting data were expressed as rates, and comparisons were conducted using χ2 tests or Fisher’s exact test, as appropriate. The overall survival rate between the two groups was calculated using the Kaplan-Meier method. A significance level of P<0.05 was used to denote statistical significance.
Results
Baseline demographic and clinical data of patients included in primary analysis
As previously outlined in the “definitions and grouping” section, MELD was chosen as the research indicator for grouping. The analysis revealed 751 patients in the low MELD group (75.5%) and 244 patients (24.5%) in the high MELD group.
A comprehensive analysis of baseline data is presented in Table 1. Notably, patients in the high MELD group exhibited a lower BMI compared to those in the low MELD group. Statistically significant differences were observed in preoperative laboratory tests, including albumin, troponin, neutrophil percentage, platelet count, aspartate aminotransferase, activated partial thromboplastin time (APTT), urea nitrogen, CRP, and INR (P<0.05).
Table 1. Preoperative baseline data of two groups of patients.
| Variables | All | MELD <18 group (n=751) | MELD ≥18 group (n=244) | Statistical value | P |
|---|---|---|---|---|---|
| Gender (male) | 540 (54.27) | 397 (52.86) | 143 (58.61) | 2.448 | 0.12 |
| Age (years) | 65 [55, 75] | 65 [50, 70] | 70 [60, 75] | 4.960 | <0.001 |
| Weight (kg) | 60 [51, 68] | 60 [53, 68] | 56 [49, 64.5] | −3.190 | <0.001 |
| Height (cm) | 161 [154, 167] | 160 [154, 167] | 162 [154, 167] | 0.098 | 0.92 |
| BMI (kg/m2) | 23.0 [20.5, 25.3] | 23.3 [21.0, 25.6] | 21.7 [19.6, 24.4] | −5.010 | <0.001 |
| Albumin (g/dL) | 3.9 [3.4, 4.2] | 4.0 [3.6, 4.3] | 3.5 [3.0, 4.1] | −5.320 | <0.001 |
| Troponin I (μg/L) | 0.03 [0.01, 0.13] | 0.02 [0.01, 0.06] | 0.11 [0.03, 0.44] | 5.045 | <0.001 |
| Fibrinogen (mg/dL) | 302 [263, 360] | 293 [263, 343] | 314 [257, 360] | 1.234 | 0.22 |
| PO2 (mmHg) | 107 [92, 143] | 107 [92, 143] | 108 [92, 147] | 1.237 | 0.22 |
| PCO2 (mmHg) | 39.6 [37.0, 42.1] | 40.0 [37.0, 42.5] | 38.8 [36.0, 41.6] | −2.255 | 0.02 |
| Base surplus (mmol/L) | 0.4 [−0.9, 1.7] | 0.4 [−0.9, 1.3] | 0 [−1.5, 1.8] | −1.607 | 0.11 |
| White blood cell count (/nL) | 6.26 [4.71, 7.84] | 6.26 [5.14, 7.62] | 5.52 [4.19, 8.31] | −1.522 | 0.13 |
| Neutrophil percentage (%) | 63.0 [55.9, 72.6] | 60.9 [52.9, 69.5] | 67.4 [60.1, 77.7] | 5.214 | <0.001 |
| Platelet count (/nL) | 176 [134, 216] | 198 [164, 231] | 150 [114, 188] | −7.134 | <0.001 |
| Alanine aminotransferase (IU/L) | 20 [13, 30] | 20 [13, 28] | 19 [12, 35] | 0.249 | 0.80 |
| Aspartate aminotransferase (IU/L) | 25 [19, 35] | 23 [18, 31] | 31 [23, 49] | 5.008 | <0.001 |
| APTT (s) | 34.8 [31.2, 43.1] | 33.8 [30.7, 38.4] | 38.4 [33.0, 56.5] | 5.191 | <0.001 |
| Urea nitrogen (mg/dL) | 16 [13, 24] | 15 [13, 20] | 23.5 [15, 37] | 7.579 | <0.001 |
| Creatine kinase (IU/L) | 64 [47, 99] | 64 [49, 99] | 49.5 [39, 99] | −2.201 | 0.03 |
| CRP (mg/dL) | 0.19 [0.06, 1.64] | 0.11 [0.06, 0.57] | 0.78 [0.19, 4.60] | 5.905 | <0.001 |
| INR | 1.10 [1.00, 1.27] | 1.05 [0.98, 1.19] | 1.21 [1.08, 1.54] | 6.098 | <0.001 |
| MELD | 5.74 [2.83, 11.02] | 4.67 [2.16, 7.96] | 13.42 [8.68, 18.66] | 13.468 | <0.001 |
Data are presented as median [P25, P75] or n (%). MELD, model for end-stage liver disease; BMI, body mass index; PO2, oxygen partial pressure; PCO2, partial pressure of carbon dioxide; APTT, activated partial thromboplastin time; CRP, C-reactive protein; INR, international normalized ratio.
Intraoperative data and postoperative data between the groups
Intraoperative and postoperative data for the two groups included in the final analysis are compared in Tables 2,3. In comparison to the low MELD group, the high MELD group exhibited a higher rate of emergency surgery (10.66% vs. 5.99%, P=0.01), along with prolonged anesthesia time, surgery time, and cardiopulmonary bypass (CPB) time. Regarding clinical prognosis, the high MELD group demonstrated a higher 28-day mortality rate (10.66% vs. 0.8%, P<0.001), as also observed in the analysis of three valve subgroups. Additionally, the high MELD group experienced longer hospitalization and ICU stay, and a higher proportion of patients requiring mechanical circulatory support, including IABP assist (14.75% vs. 3.86%, P<0.001), ECMO assist (7.38% vs. 0.8%, P<0.001), and CRRT (27.87% vs. 1.46%, P<0.001) post-surgery. The postoperative laboratory test comparison outcomes were shown in Table S1.
Table 2. Clinical data of the two groups during operation.
| Variables | All | MELD <18 group (n=751) | MELD ≥18 group (n=244) | Statistical value | P |
|---|---|---|---|---|---|
| Emergency operation | 71 (7.14) | 45 (5.99) | 26 (10.66) | 6.045 | 0.01 |
| Duration of anesthesia (min) | 425 [350, 510] | 410 [340, 485] | 467.5 [396, 599] | 7.271 | <0.001 |
| Operating room time (min) | 445 [370, 530] | 435 [360, 510] | 495 [420, 619] | 7.311 | <0.001 |
| Operation time (min) | 360 [285, 440] | 345 [275, 420] | 403 [335, 524] | 7.397 | <0.001 |
| CPB time (min) | 200 [160, 250] | 195 [150, 240] | 230 [185, 270] | 7.362 | <0.001 |
| Invasive MAP (mmHg) | 66 [64, 68] | 66 [64, 68] | 64 [60, 68] | −4.839 | <0.001 |
| BIS | 37 [31, 41] | 38 [33, 41] | 35 [29, 40] | −4.972 | <0.001 |
| CI (L/min/m2) | 2.3 [2.0, 2.7] | 2.3 [2.0, 2.7] | 2.4 [2.0, 2.8] | 1.443 | 0.15 |
| CVP (mmHg) | 6 [4, 7] | 6 [2, 7] | 6 [4, 7] | 2.264 | 0.02 |
| PEEP (cmH2O) | 0 [0, 2.5] | 0.5 [0, 2.0] | 0 [0, 3.0] | −0.425 | 0.67 |
| Respiratory rate (/min) | 11 [10, 12] | 11 [10, 12] | 11 [10, 12] | −1.341 | 0.18 |
| Intraoperative tidal volume (mL) | 432 [384, 472] | 440 [384, 472] | 424 [368, 472] | −1.957 | 0.05 |
Data are presented as median [P25, P75] or n (%). MELD, model for end-stage liver disease; CPB, cardiopulmonary bypass; MAP, mean arterial pressure; BIS, bispectral index score; CI, cardiac index; CVP, central venous pressure; PEEP, positive end-respiratory pressure.
Table 3. Clinical results of the two groups.
| Variables | All | MELD <18 group (n=751) | MELD ≥18 group (n=244) | Statistical value | P |
|---|---|---|---|---|---|
| In-hospital time (h) | 432 [312, 672] | 408 [312, 576] | 600 [408, 1,002] | 9.441 | <0.001 |
| ICU stay time (h) | 48 [26, 97] | 47 [25, 83] | 100 [46, 170] | 9.541 | <0.001 |
| Number of patients in subgroups | |||||
| Subgroup 1 (aortic valve) | 602 | 480 (79.7) | 122 (20.3) | – | – |
| Subgroup 2 (mitral valve) | 340 | 239 (70.3) | 101 (29.7) | – | – |
| Subgroup 3 (tricuspid valve) | 53 | 32 (60.4) | 21 (39.6) | – | – |
| Postoperative 28 d mortality | 32 (3.22) | 6 (0.8) | 26 (10.66) | 57.484 | <0.001 |
| Subgroup 1 (aortic valve) | 15 (2.49) | 3 (0.63) | 12 (9.84) | 33.969 | <0.001 |
| Subgroup 2 (mitral valve) | 13 (3.82) | 3 (1.26) | 10 (9.9) | 14.432 | <0.001 |
| Subgroup 3 (tricuspid valve) | 4 (7.55) | 0 | 4 (19.05) | 6.593 | 0.01 |
| Receiving reoperation | 8 (0.8) | 2 (0.27) | 6 (2.46) | 11.102 | 0.001 |
| Receiving CRRT | 79 (7.94) | 11 (1.46) | 68 (27.87) | 175.661 | <0.001 |
| ECMO assist | 24 (2.41) | 6 (0.8) | 18 (7.38) | 33.855 | <0.001 |
| IABP assist | 65 (6.53) | 29 (3.86) | 36 (14.75) | 35.786 | <0.001 |
| Atrial fibrillation and flutter | 46 (4.62) | 32 (4.26) | 14 (5.74) | 0.911 | 0.34 |
| Heart failure | 12 (1.21) | 8 (1.07) | 4 (1.64) | 0.509 | 0.48 |
| Arterial embolism and thrombosis | 1 (0.1) | 1 (0.13) | 0 | 0.325 | 0.57 |
| Bacterial pneumonia, not elsewhere classified | 1 (0.1) | 1 (0.13) | 0 | 0.325 | 0.57 |
| Pneumonia, unspecified organism | 5 (0.5) | 4 (0.53) | 1 (0.41) | 0.056 | 0.81 |
| Complications of cardiac and vascular prosthetic devices, implants and grafts | 19 (1.91) | 10 (1.33) | 9 (3.69) | 5.462 | 0.02 |
Data are presented as median [P25, P75] or n (%). MELD, model for end-stage liver disease; ICU, intensive care unit; CRRT, continuous renal replacement therapy; ECMO, extracorporeal membrane oxygenation; IABP, intra-aortic balloon pump.
Survival Kaplan-Meier survival curves
The Kaplan-Meier survival curves illustrated a significantly lower mortality rate in the low MELD group compared to the high MELD group, with highly significant statistical differences (P<0.001) evident in the results (Figure 3). ROC analysis of three different valves showed that cutoff (sensitivity: 0.706, specificity: 0.833) for aortic valve surgery was 18.2, AUC =0.831 [95% confidence interval (CI): 0.759, 0.903], cutoff (sensitivity: 0.760, specificity: 0.844) for mitral valve surgery was 19.4, AUC =0.875 (95% CI: 0.818, 0.933), and cutoff (sensitivity: 0.833, specificity: 0.979) for tricuspid valve surgery was 22.6, AUC =0.961 (95% CI: 0.900, 1.000) (cause of low mortality) (Figure 4).
Figure 3.
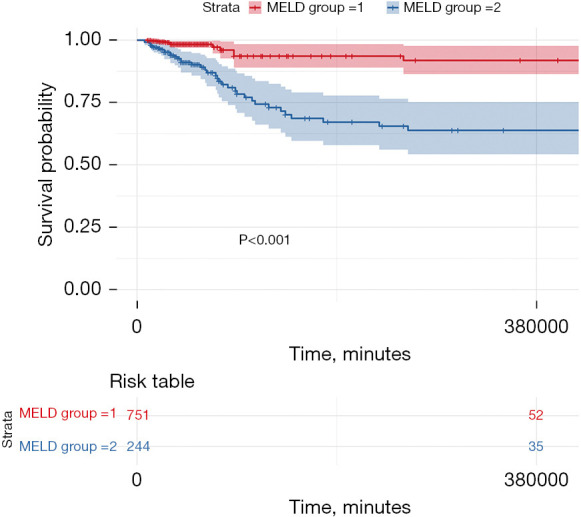
The Kaplan-Meier survival curves. MELD group =1: MELD <18 group; MELD group =2: MELD ≥18 group. MELD, model for end-stage liver disease.
Figure 4.
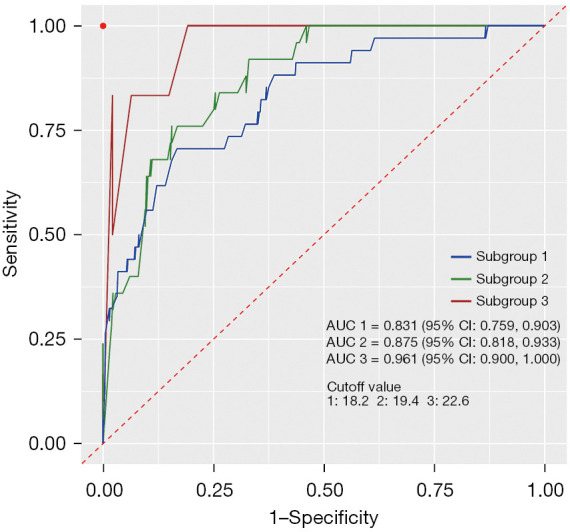
ROC analysis of three different valves—subgroup 1: aortic valve group; subgroup 2: mitral valve group; subgroup 3: tricuspid valve group. AUC, area under the curve; ROC, receiver operating characteristic.
Discussion
Cardiac valve surgery, a staple in managing heart valve diseases such as mitral and aortic valve stenosis, carries inherent risks of complications like renal and liver dysfunction (10,11). The MELD score emerges as a robust, non-invasive tool, leveraging accessible laboratory metrics for its computation. Its reliance on objective, non-respiratory parameters streamline its use in clinical settings, making it particularly invaluable in assessing perioperative liver function among cardiac surgery patients (12,13).
A previous study corroborates the utility of MELD for predicting liver dysfunction post-acute type A aortic dissection surgeries, with its early application facilitating the identification of at-risk patients (14). The score’s sensitivity and effectiveness in disease stratification have been affirmed in coronary artery bypass and heart transplantation cases (15-17). Our study extends these findings, demonstrating the efficacy of early MELD scoring post-heart valve surgery as a stratification tool. High preoperative levels of clinical indicators such as aspartate aminotransferase, APTT, urea nitrogen, CRP, and INR, in conjunction with extended surgical and CPB duration, are predictors of elevated postoperative MELD scores. Notably, patients with higher early postoperative scores typically face poorer prognoses, including higher in-hospital mortality rates and increased dependency on mechanical circulatory support and CRRT for acute kidney injury (AKI).
While the inclusion of INR as a coagulation indicator in the MELD score and the requirement for CPB assistance during smooth heart valve surgery have some impact on the score. Although previous studies have suggested that MELD-XI may have better practical applications (15), our research has found that MELD is more suitable in this type of surgery. Our study not only highlights the diagnostic value of the MELD score but also demonstrates its superiority over the MELD-XI and other modified MELD scores in predicting mortality risk. This may be attributed to the fact that all our scores were evaluated within 48 hours after surgery, which eliminates the impact of postoperative warfarin anticoagulation on INR. However, further research is needed to confirm this. The underlying mechanism is that venous congestion and hyperthyroidism can contribute to elevated liver enzymes and other factors, leading to cardiovascular renal hepatic syndrome (18). The progression of liver dysfunction in patients with acute hepatic failure (AHF) is complex and may follow various paths.
The optimal MELD threshold for cardiac surgery has historically been debated, with previous literature advocating for a 14–15 range (19,20). Contrarily, our analysis supports a threshold of 18, balancing sensitivity and specificity to avoid diluting disease stratification efficacy. It is pertinent to consider variable thresholds across different surgical interventions. The assessment of organ function becomes paramount for patients with multiple preoperative risks undergoing complex procedures. The MELD score, thus, serves as a critical barometer for clinical guidance, highlighting patients necessitating focused care to potentially enhance clinical outcomes. In conclusion, while the MELD score is a valuable prognostic tool for postoperative complications, it is incumbent upon us to refine its application post-heart valve surgery through continued research, aiming to optimize patient prognosis.
Limitations
This study is subject to several limitations that merit consideration. Primarily, it is based on a single-center database, and the cohort is predominantly from the Korean population. Consequently, the applicability of our findings to other ethnic or demographic groups may be limited. Moreover, the reliance on data extracted from the INSPIRE database introduces the possibility of compromised data integrity, which could be attributed to incomplete medical records, data entry inaccuracies, or instances of omitted information. These factors collectively could impact the robustness of our conclusions. In light of these limitations, it is imperative that future studies, especially larger-scale randomized controlled trials (RCTs), are undertaken to corroborate and extend our findings across more diverse and representative populations.
Conclusions
The MELD score demonstrates a robust predictive value for clinical outcomes following cardiac valve surgery, underscoring its utility as a viable metric for disease stratification research. This score, by quantifying the severity of organ dysfunction, provides a reliable gauge for prognostic assessments in the postoperative phase of cardiac interventions.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This study was supported by the Pudong New Area Health Commission Clinical Peak Discipline Construction (Emergency and Critical Care Unit) (No. PWYgf2021-03).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Approval for this study was obtained from the Committee on Ethics of Biomedical Research at Shanghai East Hospital, Tongji University School of Medicine, Shanghai (No. TJUSM2023-010), with a waiver for individual patient consent.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-242/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-242/coif). The authors have no conflicts of interest to declare.
References
- 1.Ziser A, Plevak DJ. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Curr Opin Anaesthesiol 2001;14:707-11. 10.1097/00001503-200112000-00018 [DOI] [PubMed] [Google Scholar]
- 2.Khurram M, Qayyum W, Umar M, et al. Evaluation of model for end-stage liver disease score cut off values in patients with hepatic encephalopathy. J Ayub Med Coll Abbottabad 2015;27:886-9. [PubMed] [Google Scholar]
- 3.Matthews JC, Pagani FD, Haft JW, et al. Model for end-stage liver disease score predicts left ventricular assist device operative transfusion requirements, morbidity, and mortality. Circulation 2010;121:214-20. 10.1161/CIRCULATIONAHA.108.838656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nwakanma LU, Williams JA, Weiss ES, et al. Influence of pretransplant panel-reactive antibody on outcomes in 8,160 heart transplant recipients in recent era. Ann Thorac Surg 2007;84:1556-62; discussion 1562-3. 10.1016/j.athoracsur.2007.05.095 [DOI] [PubMed] [Google Scholar]
- 5.Kamath PS, Kim WR, Advanced Liver Disease Study Group . The model for end-stage liver disease (MELD). Hepatology 2007;45:797-805. 10.1002/hep.21563 [DOI] [PubMed] [Google Scholar]
- 6.Liu J, Wu M, Xie E, et al. Assessment of Liver Function for Evaluation of Short- and Long-Term Outcomes in Type B Aortic Dissection Patients Undergoing Thoracic Endovascular Aortic Repair. Front Cardiovasc Med 2021;8:643127. 10.3389/fcvm.2021.643127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin X, Xie L, Jiang D, et al. Hepatic dysfunction and adverse outcomes after total arch repair of acute type a aortic dissection: application of the MELD-XI score. BMC Cardiovasc Disord 2022;22:491. 10.1186/s12872-022-02934-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirani R, Okumura K, Isath A, et al. Utilization of hepatitis C virus infected donors in heart transplant recipients with elevated MELD-XI score. Clin Transplant 2023;37:e15124. 10.1111/ctr.15124 [DOI] [PubMed] [Google Scholar]
- 9.Lim L, Lee H, Jung CW, et al. INSPIRE, a publicly available research dataset for perioperative medicine. Sci Data 2024;11:655. 10.1038/s41597-024-03517-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rasmussen SB, Boyko Y, Ranucci M, et al. Cardiac surgery-Associated acute kidney injury - A narrative review. Perfusion 2023. [Epub ahead of print]. doi: . 10.1177/02676591231211503 [DOI] [PubMed] [Google Scholar]
- 11.Chen X, Bai M, Zhao L, et al. Time to peak bilirubin concentration and advanced AKI were associated with increased mortality in rheumatic heart valve replacement surgery patients with severe postoperative hyperbilirubinemia: a retrospective cohort study. BMC Cardiovasc Disord 2021;21:16. 10.1186/s12872-020-01830-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Z, Chen T, Ge M, et al. The risk factors and outcomes of preoperative hepatic dysfunction in patients who receive surgical repair for acute type A aortic dissection. J Thorac Dis 2021;13:5638-48. 10.21037/jtd-21-1051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farr M, Mitchell J, Lippel M, et al. Combination of liver biopsy with MELD-XI scores for post-transplant outcome prediction in patients with advanced heart failure and suspected liver dysfunction. J Heart Lung Transplant 2015;34:873-82. 10.1016/j.healun.2014.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou W, Wang G, Liu Y, et al. Outcomes and risk factors of postoperative hepatic dysfunction in patients undergoing acute type A aortic dissection surgery. J Thorac Dis 2019;11:3225-33. 10.21037/jtd.2019.08.72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deo SV, Al-Kindi SG, Altarabsheh SE, et al. Model for end-stage liver disease excluding international normalized ratio (MELD-XI) score predicts heart transplant outcomes: Evidence from the registry of the United Network for Organ Sharing. J Heart Lung Transplant 2016;35:222-7. 10.1016/j.healun.2015.10.008 [DOI] [PubMed] [Google Scholar]
- 16.Grimm JC, Magruder JT, Do N, et al. Modified Model for End-Stage Liver Disease eXcluding INR (MELD-XI) Score Predicts Early Death After Pediatric Heart Transplantation. Ann Thorac Surg 2016;101:730-5. 10.1016/j.athoracsur.2015.06.063 [DOI] [PubMed] [Google Scholar]
- 17.Dolapoglu A, Avci E, Argan O, et al. Impact of model for end-stage liver disease (MELD) score for mortality in patients undergoing coronary bypass surgery. Bratisl Lek Listy 2021;122:125-31. 10.4149/BLL_2021_019 [DOI] [PubMed] [Google Scholar]
- 18.Harjola VP, Mullens W, Banaszewski M, et al. Organ dysfunction, injury and failure in acute heart failure: from pathophysiology to diagnosis and management. A review on behalf of the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail 2017;19:821-36. 10.1002/ejhf.872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ailawadi G, Lapar DJ, Swenson BR, et al. Model for end-stage liver disease predicts mortality for tricuspid valve surgery. Ann Thorac Surg 2009;87:1460-7; discussion 1467-8. 10.1016/j.athoracsur.2009.01.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Z, Ge M, Chen C, et al. Hepatic dysfunction in patients who received acute DeBakey type I aortic dissection repair surgery: incidence, risk factors, and long-term outcomes. J Cardiothorac Surg 2021;16:296. 10.1186/s13019-021-01676-8 [DOI] [PMC free article] [PubMed] [Google Scholar]