Abstract

Nanoparticles (NPs) have been widely used to improve the pharmacokinetic properties and tissue distribution of small molecules such as targeting to a specific tissue of interest, enhancing their systemic circulation, and enlarging their therapeutic properties. NPs have unique and complicated in vivo disposition properties compared to small molecule drugs due to their complex multifunctionality. Physiologically based pharmacokinetic (PBPK) modeling has been a powerful tool in the simulation of the absorption, distribution, metabolism, and elimination (ADME) characteristics of the materials, and it can be used in the characterization and prediction of the systemic disposition, toxicity, efficacy, and target exposure of various types of nanoparticles. In this review, recent advances in PBPK model applications related to the nanoparticles with unique properties, and dispositional features in the biological systems, ADME characteristics, the description of transport processes of nanoparticles in the PBPK model, and the challenges in PBPK model development of nanoparticles are delineated and juxtaposed with those encountered in small molecule models. Nanoparticle related, non-nanoparticle-related, and interspecies-scaling methods applied in PBPK modeling are reviewed. In vitro to in vivo extrapolation (IVIVE) methods being a promising computational tool to provide in vivo predictions from the results of in vitro and in silico studies are discussed. Finally, as a recent advancement ML/AI-based approaches and challenges in PBPK modeling in the estimation of ADME parameters and pharmacokinetic (PK) analysis results are introduced.
Keywords: physiologically based pharmacokinetic (PBPK) model, nanoparticles (NPs), absorption, distribution, metabolism, excretion (ADME), interspecies scaling, in vitro to in vivo extrapolation (IVIVE), artificial intelligence (AI)
With the expanding interest in the discovery and development of drug delivery systems containing nanoparticles, the need for effective quantitative tools to determine the safety, efficacy, and possible toxicity of these materials has emerged. Physiologically based pharmacokinetic (PBPK) modeling is a computational tool to simulate the absorption, distribution, metabolism, and elimination (ADME) characteristics of the materials that are administered inside the body of living organisms. PBPK models have the ability to simulate the drug concentration profile in the targeted site of action such as specific organs or tissues that facilitates the adjustment of a dosage strategy and helps to attain maximum safety and efficacy profiles.1 PBPK models are comprised of a series of differential mass balance equations which stand for the physiological processes that occur in the biological tissues or fluids of an organism.
PBPK modeling serves as a valuable tool for forecasting and unraveling the dynamics of drug behavior by both mechanistically figuring out the disposition of the drug and empirically by parameter estimation.2 The major requirements in the formation of a PBPK model are the species-specific anatomical and physiological data and also the compound-specific pharmacokinetic data and partition coefficients in different tissues.3 Once the substance-specific and species-specific parameters are obtained, PBPK models can be developed for organic and inorganic compounds. The building blocks or the compartments in the construction of PBPK models are tissues in the body such as the heart, liver, kidney, brain, gut, spleen, lung, muscle, and adipose tissues. Unless they are not related to the organ of interest, the other tissues in the body may be grouped in a remainder compartment, or they may be neglected if they are not important concerning mass balance. For simplification, tissues that have comparable kinetic properties can be lumped together.4 In PBPK models, all the tissue compartments are linked to the circulating blood system and occasionally by the lymphatic system. The drug-metabolizing tissue compartments such as the liver and kidney are selected to define drug clearance. Species extrapolation, dose–response prediction, risk assessment, and individual variability prediction can be mentioned among the advantages of PBPK models. Integrating genetic and physiological variations with physicochemical properties, PBPK models can predict individual differences in response to toxicants, aiding personalized risk assessments and interventions.
The discovery and the development of nanoparticle-based drug delivery systems have been a research subject of major interest owing to their various advantages in the field of targeted drug delivery. Nanoparticle-based drug delivery systems have been considered promising agents in the treatment of various pathologies such as cancer, diabetes, neurodegenerative, cardiovascular, and respiratory and infectious diseases5−7 and also have been widely used as diagnostic and imaging agents for the early diagnosis of disease.5,8−10 Nanoparticles which have various sizes, surface charges, and functionalization can exhibit different pharmacokinetic behaviors that may limit the preclinical assessments when compared with conventional therapeutics.11 In this aspect, the use of computational and mathematical modeling that are discrete such as quantum mechanics, molecular dynamics, or continuous models like physiologically based pharmacokinetic (PBPK) modeling and pharmacokinetic/pharmacodynamic (PK/PD) modeling stands as promising tools to predict the pharmacokinetic properties of nanoparticles.
In this review, recent advances in PBPK model applications focusing on nanoparticles and considering their unique characteristics, their dispositional features in the biological systems, ADME characteristics, the description of transport processes of nanoparticles in the PBPK model, and the challenges in PBPK model development of nanoparticles are summarized and compared with those of the small molecules. PBPK modeling and simulation have been widely used to predict the pharmacokinetics (PK) and disposition of small molecules and biologics; however, these practices to nanoparticles are bounded and challenging because of the complicated in vivo transport mechanisms, for instance, opsonization and uptake by mononuclear phagocyte system (MPS), recognition and internalization by the cells, enhanced permeability and retention (EPR) effect, lymphatic transfer, enzymatic degradation and structural property changes in biological systems.12
This review provides an overview of the ADME characteristics of nanoparticles and parameters used in PBPK modeling including interspecies scaling techniques, and gives brief summary on the recent developments regarding the PBPK modeling of nanoparticles. The use of in vitro to in vivo extrapolation (IVIVE) techniques integrated with PBPK models to determine the safety, efficacy, and potential toxicity of a rapidly increasing number of nanoparticle-based products is presented. These techniques are considered as promising approaches in the risk estimation of nanoparticles owing to being nonanimal alternative techniques to the traditional methods. The major challenges in the model development and validation of nanoparticle based PBPK models are also discussed. Finally, as a novel technique in PBPK modeling, AI (Artificial Intelligence)-Assisted PBPK modeling and related literature studies are introduced. With the considerable progression in the field of nanotechnology and nanomedicine over the past few decades, efficient development of modeling frameworks using novel applications that facilitate the prediction of species-specific physiological disposition has been emerging to extrapolate both from in vitro to in vivo as well as from animals to humans. This paper outlines the advancements and challenges and points out the future prospects in the PBPK modeling of nanomaterials.
ADME Characteristics of Nanoparticles
Unlike the PBPK modeling of small molecules, the unique interaction of the nanoparticles with physiological systems should be considered when constructing PBPK models for nanoparticles.12 The limitations in the development and the validation of the PBPK models of NPs are regarded as a deficiency in the reliable and rapid analytical approaches for NP models.13 This situation arises from the much more complex ADME properties of NPs compared to the small molecules and also the difficulty in the NP isolation from the tissues compared to isolating from the plasma samples.13 In this aspect, it is crucial to incorporate the ADME properties of the nanoparticles specifically according to their features into the PBPK models, to enhance the predictability and performance of these models. A schematic representation of the adsorption, distribution, metabolism, and excretion (ADME) of drugs and nanoparticles is shown in Figure 1.
Figure 1.

Adsorption, distribution, metabolism, and excretion (ADME) of drugs and/or nanoparticles. Reproduced with permission from ref (26) with no modifications. Open Access. CC-BY 4.0 license. Copyright: © 2022 by the authors. Licensee MDPI, Basel, Switzerland. URL: https://www.mdpi.com/2075-4426/12/5/673. No endorsement.
Absorption
Most of the nanoparticles designed for drug targeting have been intended to be administered by intravenous (IV) injection, and many of them have been developed to extend the circulation time or target the organ specific to that disease through the circulation system.4 When the nanoparticles are administered via nonintravenous injection methods, they go through two competitive processes that are preabsorption clearance and absorption.4 In preabsorption clearance, nanoparticles encounter local degradation and direct removal by different excretion routes upon oral, pulmonary, and nasal administration.4 In the local degradation of NPs, the release of an active pharmaceutical ingredient (API) from an encapsulated form of NP can take place at the administration site, and APIs are disposed like small molecules.4 After oral administration, the nanoparticles that do not encounter preabsorption clearance can participate in the bloodstream and lymphatic system by crossing the unstirred water layer and the epithelium of the gastrointestinal (GI) tract.4 After pulmonary exposure, nanoparticles deposited in the lungs can be exhaled, discharged via mucociliary clearance to the GI tract, or kept apart and degraded by macrophages.4 The nanoparticles left from these discharge mechanisms can be absorbed after crossing the mucus and lung epithelium cells.4 After subcutaneous, intramuscular, intradermal, or intraperitoneal injections, NPs are mostly absorbed via highly permeable lymph vessels or via macrophages and transferred into regional lymph nodes.4
Distribution
Nanoparticles pass to the vascular system after intravenous administration and are then distributed to the tissues and organs of the body.3 After the NP administration via inhalation, NPs are placed in the alveolar region and taken up by the alveolar macrophages.3 These alveolar macrophages then move to the tracheobronchial region with the aim of mucociliary clearance or to the mediastinal lymph nodes.3 Some of the nanoparticles may enter to epithelium via the process of endocytosis.3 The region-specific placement information on the nanoparticles obtained from the model can be useful in the determination of the multicompartmental parameters in PBPK modeling.3 When the nanoparticles arrive at the vascular system, they come across blood cells, plasma proteins, platelets, and coagulation factors.3 The proteins present in the vascular system are adsorbed on the surface of these nanoparticles, and as a result, NP-protein complex and dynamic corona formation occur.3 The NP-protein corona affects the internalization and the distribution of the nanoparticles into different tissues.3 It is imperative to incorporate the formation of NP-protein complexes and their dynamic processes when constructing a PBPK model.3 Since the mechanism inside the NP-protein formation process has not been fully revealed,14 it is significant to carry out further studies on this topic.
Metabolism
The enzymatically degradable nanoparticles (such as protein, lipid, and poly(lactic-co-glycolic) acid (PLGA) based NPs) can be metabolized inside the system of the organism, whereas inorganic nanoparticles (nondegradable in general) are not metabolized.3 On the other hand, the ligands that are used as a surface modification of these inorganic nanoparticles and organic coatings can be degraded enzymatically.3 Most of the xenobiotics are metabolized in the liver (the main organ responsible for the metabolism), and the enzymes that participate in the metabolism belong to the transferase, esterase, monooxygenase and epoxide hydrolase families.3 However, the nanoparticles which are hard to degrade by intracellular processes like inert Au NPs remain inside the cells and are located in the liver for a very long time.15 Au nanoparticles, which were administered intravenously, were reported to accumulate in the liver of the mouse, and the duration of the elimination of the nanoparticles lasted more than 6 months.16 Also, according to toxicological studies, if the dose of the nanoparticles is higher than the hepatic biodegradation capacity, the residual nanoparticles accumulate in the organ for a long period.15 The in vivo clearance values of most of the compounds are found by scaling up the in vitro metabolic clearance data obtained from human liver microsomes or hepatocytes.3 In PBPK modeling, the equations related to the metabolism of compounds are usually described by a combination of linear and Michaelis–Menten kinetic equations.3 The kinetic constants of the Michaelis–Menten equation, which are Km and Vmax are obtained by in vitro or in vivo empirical experiments.3
Some of the previous studies discarded the pharmacokinetics regarding the metabolism of the nanoparticles that have protein ligands on their surface or include organic coatings since the process is not fully understood.17 Hence, in PBPK modeling of NPs, the metabolism term is sometimes described by the processes of dissolution, corona formation, and aggregation/agglomeration.3 Since the mathematical description of the dissolution kinetics of nanomaterials has not been fully identified, this process is included in some of the PBPK models and neglected in others. For example, in a study on the PBPK modeling Ag nanoparticles, the metabolic pathway of NPs was first described by the extracellular and intracellular dissolution followed by the release of the soluble silver species and then by the storage of Ag nanoparticles directly as in the form of silver sulfide particles.18 In some other studies on the nanoparticles that have low dissolution rates inside the body, e.g., AuNPs, the metabolism process was neglected during the construction of PBPK models.17 Moreover, the dissolution of Ag nanoparticles was excluded in the PBPK model of another study, and the results indicated an accurate simulation of nanoparticles.19
When the nanoparticles form aggregates or agglomerates, which are regarded as secondary entities, they show more complicated physicochemical properties compared to the single nanoparticles since their properties such as size, surface area, morphology, and effective density change and depend on additional factors.20 However, the information on the interaction of the aggregates or agglomerates of the nanoparticles in the biological system has been limited. In a previous article that reviewed the interaction of nanoparticle aggregates with biological systems, the critical threshold particle size for the tissue uptake and clearance was reported to be between 200 and 250 nm, and hence particles larger than this threshold may tend to accumulate.21 Compared to larger sized Au nanoparticles (20 nm), smaller sized ones (7 nm) that form aggregates with a maximum diameter of 45 nm showed higher translocation and a wider distribution to secondary organs in rats following 15 days of inhalation exposure.22 However, further studies are needed to shed a light on the topic of differences between single particles and aggregated particles at the mechanistic level, and the mechanisms of interaction of the aggregates with the biological system should be identified.
Excretion
The major organs that are responsible for the excretion process of the nanoparticles are the liver and kidney through feces and urine, respectively.3 The nanoparticles can also be excreted from the body through lungs, sweat, and breast milk.3 In PBPK models, generally, renal and hepatic clearances of the nanoparticles are considered.23 The size of the nanoparticles is significant in renal clearance. For example, quantum dot (QD) nanoparticles smaller than 5.5 nm have been effectively and rapidly excreted from the body via urinary clearance,24 whereas for Au nanoparticles with a particle diameter larger than 10 nm the renal excretion process has been neglected.25 The pore size of the liver capillaries is much larger than that of kidneys, and hence for nanoparticles the degree of urinary excretion is much smaller than of the biliary excretion.3 In this aspect, the hepatobiliary excretion system that includes hepatocytes followed by excretion into the bile is considered as the major clearance route for the larger-sized nanoparticles.3 Apart from the size of the nanoparticles, their surface functionalization has been reported to play an important role in biliary excretion; however there is limited knowledge about the effect of surface functionalization of nanoparticles on the excretion process.3 Further investigations both based on in vitro and in vivo assays are significant for the development of accurate PBPK models that represent the excretion process of the nanoparticles.
Parameters Used in PBPK Modeling
To predict the absorption, distribution, metabolism, and excretion (ADME) of chemical compounds in living organisms, PBPK models integrate physiological, biochemical, and physicochemical parameters to provide quantitative insights into the kinetic processes of drugs and other substances within the body. The key physiological parameters in PBPK models are the organ volumes (sizes of organs and tissues), the blood flow rates at which blood circulates through various tissues and organs, and the partition coefficients (the ratios of a compound’s concentration between blood and tissue). These parameters along with the enzymatic activities are incorporated into the PBPK models (Figure 2). These parameters are often species-specific, allowing the model to be tailored to different animal species or humans.27
Figure 2.
Schematic diagram for PBPK model parameters and application areas.
The key physicochemical characteristics of toxicants are molecular weight and size influencing the ability of the toxicant to pass through biological membranes and barriers, solubility and lipophilicity showing the compound’s tendency to dissolve in fats, affecting its distribution, ionization (pKa), and permeability. Water solubility affects how well a toxicant can dissolve in bodily fluids, impacting absorption and excretion, whereas lipid solubility (lipophilicity) determines how readily a toxicant can cross cell membranes and distribute into fatty tissues. The degree of ionization of a toxicant at physiological pH affects its solubility and permeability across cell membranes. Nonionized forms usually permeate cell membranes more readily than ionized forms. The partition coefficients describe the distribution of a toxicant between aqueous and lipid phases, informing its distribution in the body. Higher partition coefficients generally indicate higher lipophilicity, leading to greater accumulation in fatty tissues. The ability of a toxicant to penetrate biological membranes depends on its size, lipophilicity, and degree of ionization.27
PBPK models incorporate the physiological aspects of animals as well as the physicochemical properties of toxicants to simulate their absorption through different routes such as oral, inhalation, dermal, or intravenous. For oral absorption, parameters like solubility and permeability through the gastrointestinal (GI) tract are considered. The model simulates the dissolution of the toxicant in the GI fluids and its permeation through the GI lining. For inhalation, factors such as volatility and particle size are integrated to predict the deposition and absorption in the respiratory tract.27
The PBPK models predict how the compound distributes across different tissues based on blood flow rates and tissue-specific partition coefficients. This helps in understanding the drug’s or NP’s tissue accumulation and potential target sites. Physicochemical properties are used to determine the distribution of toxicants between blood and tissues. Lipophilic toxicants with high partition coefficients tend to accumulate in fatty tissues, while hydrophilic toxicants remain more in the aqueous compartments. The model accounts for tissue-specific blood flow rates and tissue-to-blood partition coefficients to predict the concentration of toxicants in different tissues over time. PBPK models include metabolic pathways, informed by the physicochemical properties of the toxicant, to predict its biotransformation. The levels and activities of metabolic enzymes help metabolize the compound. Lipophilicity and molecular structure can influence which enzymes metabolize the toxicant and the rate of metabolism. The model can simulate phase I (e.g., oxidation, reduction) and phase II (e.g., conjugation) metabolic processes, taking into account enzyme kinetics and tissue-specific enzyme expression.27
The excretion of toxicants is influenced by their solubility and molecular size. Hydrophilic toxicants are typically excreted via the kidneys, while lipophilic ones may undergo biliary excretion. PBPK models simulate renal filtration, reabsorption, and secretion, as well as biliary excretion, based on the physicochemical properties of the toxicant.27,2
Based on data acquired from in vitro studies, literature reports, or estimates derived from simulations, the initial model parameters are determined. In vitro to in vivo extrapolation (IVIVE) is used in PBPK systems to predict the concentration–time profiles of the drugs within the plasma or tissue of an organism without the need for in vivo data, and that correlation-based method is beneficial in the field of drug discovery where a large number of drug candidates are required to be analyzed.4 After the model is constructed, the verification of the optimized parameters can be carried out by comparing it with an independent data set.
Nanoparticle-Specific Parameters in the PBPK Modeling of NPs
When constructing PBPK models for the nanoparticles, nanoparticle-specific parameters such as the Hill coefficient, maximum uptake rate in phagocytic cells (PCs), nanoparticle release constant, phagocytic cells (PCs) release constant, partition coefficient, and permeability coefficient between blood and tissue should be included in the model.2
Endocytosis of the nanoparticles by phagocytic cells (PCs) is elucidated using both a linear equation and the Hill function, and according to the simulation results in the literature, the Hill function provides more accurate predictions.17 The Hill function is described by the following equation:17
where Kup_t is the uptake rate parameter of NPs by PCs in the organ t at time T, in 1/h, Kmax_t is the maximum uptake rate constant of phagocytic cells, in 1/h, K50_t is the time to reach the half of Kmax_t, in h, T is the simulation time, in h, nt is the Hill coefficient (unitless).
To attain simulated in vivo data in PBPK modeling of nanoparticles, some of the parameters such as permeability data, transporter-mediated uptake, liver transporter kinetic data, and metabolic enzymes (CYPs) can be obtained by in vitro experiments, and the resultant data can be used in different stages of ADME processes of the PBPK model.2 Nanoparticle-specific descriptions and exemplary values of nanoparticle-specific parameters used in PBPK modeling including Hill coefficient (n), tissue/plasma partition coefficient (P), permeability coefficient (χa), maximum uptake rate constant (Kmax), release rate constant (Kout), time for reaching half-maximum uptake rate (K50), and elimination rates for the bile or kidney (Clbile or Clkidney) in various compartments in body, depending on their availability in the published literature, are shown in Table 1. Further detailed information on the NP related parameters is given under the section Physiologically Based Pharmacokinetic (PBPK) Modeling Applications of Nanoparticles.
Table 1. NP-Specific Descriptions and Exemplary Values of Parameters Used in PBPK Modeling.
| parameter (unit) | description | nanoparticle and size | lung | liver | spleen | kidney | tumor | heart | brain | rest of body | reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n (unitless) | Hill coefficient | mPEG5k-9.09%-80 nma | 0.001 | 0.001 | 1.62 | 0.04 | 0.005 | 0.07 | N/A | 0.5 | Li et al., 202113 |
| mPEG5k-28.57%-80 nma | 0.001 | 0.001 | 1.6 | 0.04 | 0.005 | 0.07 | N/A | 1 | |||
| mPEG5k-9.09%-200 nma | 0.002 | 0.02 | 1.6 | 0.04 | 0.2 | 0.07 | N/A | 0.5 | |||
| mPEG5k-28.57%-200 nma | 0.0002 | 0.5 | 0.4 | 0.04 | 0.2 | 0.07 | N/A | 1 | |||
| mPEG2k-28.57%-200 nma | 0.0002 | 0.9 | 0.01 | 0.04 | 0.2 | 0.07 | N/A | 1 | |||
| Superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs)- 38.3 nm | 2 | 0.1 | 0.1 | 0.1 | N/A | N/A | N/A | N/A | Chen et al. 202228 | ||
| Water-dispersible cadmium telluride/cadmium sulfide (CdTe/CdS) QDs-4.2 nm | 5 | 7 | 2 | 3 | N/A | N/A | N/A | 5 | Liang et al., 201629 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-13 nm | 5 | 5 | 5 | 5 | N/A | N/A | N/A | N/A | Lin et al., 201617 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-100 nm | 0.1 | 0.1 | 0.1 | 0.1 | N/A | N/A | N/A | N/A | |||
| P (unitless) | Tissue/plasma partition coefficient | mPEG5k-9.09%-80 nma | 0.15 | 0.08 | 0.15 | 0.15 | 0.15 | 0.15 | N/A | 0.15 | Li et al., 202113 |
| mPEG5k-28.57%-80 nma | 0.15 | 0.08 | 0.15 | 0.15 | 0.15 | 0.15 | N/A | 0.15 | |||
| mPEG5k-9.09%-200 nma | 0.15 | 0.08 | 0.15 | 0.15 | 0.15 | 0.15 | N/A | 0.15 | |||
| mPEG5k-28.57%-200 nma | 0.15 | 0.08 | 0.15 | 0.15 | 0.15 | 0.15 | N/A | 0.15 | |||
| mPEG2k-28.57%-200 nma | 0.15 | 0.08 | 0.15 | 0.15 | 0.15 | 0.15 | N/A | 0.15 | |||
| Cerium oxide (CeO2) NPs-25 and 90 nm | 0.209 | 0.209 | 0.209 | 0.209 | N/A | 0.209 | 0.209 | 0.209 | Li et al., 201630 | ||
| Polyethylene on glycol-coated polyacrylamide (PAA–PEG) NPs-35 nm | 0.147 | 0.147 | 0.147 | 0.147 | N/A | 0.147 | 0.147 | 0.147 | Li et al., 201431 | ||
| Stavudine-AuNP (40 nm) | N/A | 0.55 | 0.77 | N/A | N/A | N/A | 0.46 | N/A | Zazo et al., 202211 | ||
| Superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs)- 38.3 nm | 0.15 | 0.08 | 0.15 | 0.15 | N/A | N/A | 0.15 | 0.15 | Chen et al. 202228 | ||
| Water-dispersible cadmium telluride/cadmium sulfide (CdTe/CdS) QDs-4.2 nm | 0.015 | 0.15 | 0.15 | 0.015 | N/A | N/A | N/A | 0.15 | Liang et al., 201629 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-13 nm | 0.15 | 0.08 | 0.15 | 0.15 | N/A | N/A | 0.15 | 0.15 | Lin et al., 201617 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-100 nm | 0.15 | 0.08 | 0.15 | 0.15 | N/A | N/A | 0.15 | 0.15 | |||
| χa (unitless) | Permeability coefficient | mPEG5k-9.09%-80 nma | 0.001 | 0.001 | 0.03 | 0.001 | 0.001 | 0.001 | N/A | 0.001 | Li et al., 202113 |
| mPEG5k-28.57%-80 nma | 0.001 | 0.001 | 0.03 | 0.001 | 0.001 | 0.001 | N/A | 0.001 | |||
| mPEG5k-9.09%-200 nma | 0.001 | 0.001 | 0.03 | 0.001 | 0.001 | 0.001 | N/A | 0.001 | |||
| mPEG5k-28.57%-200 nma | 0.001 | 0.001 | 0.03 | 0.001 | 0.001 | 0.001 | N/A | 0.001 | |||
| mPEG2k-28.57%-200 nma | 0.001 | 0.001 | 0.03 | 0.001 | 0.001 | 0.001 | N/A | 0.001 | |||
| Cerium oxide (CeO2) NPs-25 and 90 nm | 0.776 | 0.776 | 0.776 | 0.776 | N/A | 0.776 | 6.75 × 10–7 | 0.0171 | Li et al., 201630 | ||
| Polyethylene on glycol-coated polyacrylamide (PAA-PEG) NPs - 35 nm | 1.06 × 10–3 | 1.06 × 10–3 | 1.06 × 10–3 | 1.06 × 10–3 | N/A | 1.06 × 10–3 | 0 | 8.25 × 10–5 | Li et al., 201431 | ||
| Superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs)- 38.3 nm | 10–3 | 10–3 | 10–3 | 10–3 | N/A | N/A | 1.32 × 10–4 (MF-)a3.51 × 10–4 (SMF)a | 10–6 | Chen et al. 202228 | ||
| Water-dispersible cadmium telluride/cadmium sulfide (CdTe/CdS) QDs-4.2 nm | 0.0001 | 0.001 | 0.001 | 0.0001 | N/A | N/A | N/A | 0.001 | Liang et al., 201629 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-13 nm | 0.001 | 0.001 | 0.03 | 0.001 | N/A | N/A | 0.000001 | 0.000001 | Lin et al., 201617 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-100 nm | 0.001 | 0.001 | 0.001 | 0.001 | N/A | N/A | 0.000001 | 0.000001 | |||
| Kmax (h–1) | Maximum uptake rate constant | mPEG5k-9.09%-80 nma | 1.04 | 132 | 65 | 0.52 | 15 | 0.9 | N/A | 4 | Li et al., 202113 |
| mPEG5k-28.57%-80 nma | 0.05 | 151 | 83 | 0.05 | 15 | 0.16 | N/A | 2 | |||
| mPEG5k-9.09%-200 nma | 10 | 560 | 350 | 2.2 | 32 | 2.57 | N/A | 51 | |||
| mPEG5k-28.57%-200 nma | 1 | 100 | 130 | 0.7 | 16 | 0.4 | N/A | 21 | |||
| mPEG2k-28.57%-200 nma | 0.1 | 280 | 140 | 1.5 | 16 | 6.94 | N/A | 28 | |||
| Cerium oxide (CeO2) NPs-25 and 90 nm | 1.45 | 1.45 | 0.518 | 1.45 | N/A | 1.45 | 1.45 | 1.45 | Li et al., 201630 | ||
| Polyethylene on glycol-coated polyacrylamide (PAA-PEG) NPs-35 nm | 16.1 | 16.1 | 0.112 | 16.1 | N/A | 16.1 | 16.1 | 16.1 | Li et al., 201431 | ||
| Stavudine-AuNP (40 nm) | N/A | 0.15 | 0.03 | N/A | N/A | N/A | 7.9 × 10–3 | N/A | Zazo et al., 202211 | ||
| Superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs)- 38.3 nm | 0.1 | 4 | 10 | 0.1 | N/A | N/A | N/A | N/A | Chen et al. 202228 | ||
| water-dispersible cadmium telluride/cadmium sulfide (CdTe/CdS) QDs-4.2 nm | 0.0026 | 0.15 | 0.09 | 0.07 | N/A | N/A | N/A | 0.2 | Liang et al., 201629 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-13 nm | 0.075 | 20 | 40 | 0.075 | N/A | N/A | N/A | N/A | Lin et al., 201617 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-100 nm | 0.1 | 4 | 10 | 0.1 | N/A | N/A | N/A | N/A | |||
| Kout (h–1) | Release rate constant | mPEG5k-9.09%-80 nma | 0.92 | 5 | 3 | 0.085 | 0.27 | 0.075 | N/A | 0.1 | Li et al., 202113 |
| mPEG5k-28.57%-80 nma | 4 | 12 | 7.2 | 0.085 | 1.1 | 0.075 | N/A | 0.17 | |||
| mPEG5k-9.09%-200 nma | 2 | 7 | 3.6 | 0.085 | 0.53 | 0.075 | N/A | 0.41 | |||
| mPEG5k-28.57%-200 nma | 1 | 9 | 1.6 | 0.085 | 0.53 | 0.075 | N/A | 0.94 | |||
| mPEG2k-28.57%-200 nma | 1 | 11 | 1.4 | 0.085 | 0.53 | 0.4 | N/A | 0.32 | |||
| Cerium oxide (CeO2) NPs-25 and 90 nm | 5.30 × 10–19 | 5.30 × 10–19 | 5.30 × 10–19 | 5.30 × 10–19 | N/A | 5.30 × 10–19 | 5.30 × 10–19 | 5.30 × 10–19 | Li et al., 201630 | ||
| Polyethylene on glycol-coated polyacrylamide (PAA-PEG) NPs- 35 nm | 4.90 × 10–19 | 4.90 × 10–19 | 4.90 × 10–19 | 4.90 × 10–19 | N/A | 4.90 × 10–19 | 4.90 × 10–19 | 4.90 × 10–19 | Li et al., 201431 | ||
| Superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs)- 38.3 nm | 0.005 | 0.0075 | 0.003 | 0.01 | N/A | N/A | N/A | N/A | Chen et al. 202228 | ||
| Water-dispersible cadmium telluride/cadmium sulfide (CdTe/CdS) QDs-4.2 nm | 0.0061 | 0.011 | 0.0072 | 0.002 | N/A | N/A | N/A | 0.0121 | Liang et al., 201629 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-13 nm | 0.003 | 0.001 | 0.001 | 0.0004 | N/A | N/A | N/A | N/A | Lin et al., 201617 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-100 nm | 0.005 | 0.0075 | 0.003 | 0.01 | N/A | N/A | N/A | N/A | |||
| K50 (h) | Time for reaching half-maximum uptake rate | mPEG5k-9.09%-80 nma | 0.006 | 0.001 | 0.003 | 0.04 | 0.02 | 0.4 | N/A | 0.5 | Li et al., 202113 |
| mPEG5k-28.57%-80 nma | 0.006 | 0.001 | 0.003 | 0.04 | 0.02 | 0.4 | N/A | 1 | |||
| mPEG5k-9.09%-200 nma | 0.0052 | 0.0008 | 0.003 | 0.04 | 0.3 | 0.4 | N/A | 0.09 | |||
| mPEG5k-28.57%-200 nma | 0.0002 | 0.46 | 0.0056 | 0.012 | 0.3 | 0.4 | N/A | 10 | |||
| mPEG2k-28.57%-200 nma | 0.0002 | 0.04 | 0.01 | 0.012 | 0.3 | 0.4 | N/A | 0.4 | |||
| Superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs)- 38.3 nm | 24 | 24 | 24 | 24 | N/A | N/A | N/A | N/A | Chen et al. 202228 | ||
| Water-dispersible cadmium telluride/cadmium sulfide (CdTe/CdS) QDs-4.2 nm | 7.5 | 2.78 | 1.5 | 6.82 | N/A | N/A | N/A | 7.5 | Liang et al., 201629 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-13 nm | 24 | 48 | 48 | 24 | N/A | N/A | N/A | N/A | Lin et al., 201617 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-100 nm | 24 | 24 | 24 | 24 | N/A | N/A | N/A | N/A | |||
| Clbile or Clkidney (L/h) | Elimination rates for the bile or kidney | mPEG5k-9.09%-80 nma | NA | 0.0012 | NA | 0.00012 | NA | NA | NA | NA | Li et al., 202113 |
| mPEG5k-28.57%-80 nma | NA | 0.0012 | NA | 0.00012 | NA | NA | NA | NA | |||
| mPEG5k-9.09%-200 nma | NA | 0.0012 | NA | 0.00012 | NA | NA | NA | NA | |||
| mPEG5k-28.57%-200 nma | NA | 0.0012 | NA | 0.00012 | NA | NA | NA | NA | |||
| mPEG2k-28.57%-200 nma | NA | 0.0012 | NA | 0.00012 | NA | NA | NA | NA | |||
| Superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs)- 38.3 nm | N/A | 0.0012 | N/A | 0.00012 | N/A | N/A | N/A | N/A | Chen et al. 202228 | ||
| Water-dispersible cadmium telluride/cadmium sulfide (CdTe/CdS) QDs-4.2 nm | N/A | 0.000000001 | N/A | 0.000000001 | N/A | N/A | N/A | N/A | Liang et al., 201629 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-13 nm | N/A | 0.00003 | N/A | 0.000003 | N/A | N/A | N/A | N/A | Lin et al., 201617 | ||
| Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs)-100 nm | N/A | 0.0012 | N/A | 0.00012 | N/A | N/A | N/A | N/A |
MF-: No magnetic field; SMF: external static magnetic field; methoxy poly (ethylene glycol)-poly (″ε-caprolactone) (mPEG–PCL).
Non-Nanoparticle Specific Parameters in the PBPK Modeling of NPs
The input parameters in PBPK models can be divided into different categories: physicochemical properties; drug-biological properties; and anatomic and physiological properties (organ-specific).2 Physicochemical properties can be regarded as drug-dependent parameters including the molecular weight, partition coefficient, equilibrium constants, solubility, pH-dependent partition coefficient, and membrane affinity.2 Drug-biological properties refer to the properties that are related to both the drug and the organism.2 Some examples of these properties are the fraction unbound value of the drug, Michaelis–Menten kinetic parameter constants (Km and Vmax), and dissociation constant.2 The drug-specific parameters are obtained from different in vitro studies by extrapolation or by model fitting to the available experimental data.4 Organ-specific parameters include organ volumes, blood flow rates, surface areas, tissue composition and expression levels.2 For these physiological parameters, a standardized set of values commonly employed in such contexts is utilized. The pharmacokinetic disposition for different populations can be predicted by using some of these above-mentioned properties; for instance expression level information can be predictive information on the determination of gene expression for some of the metabolizing enzymes in different organs for various populations.2 The parameters utilized in PBPK modeling along with the application areas are presented in Figure 2.
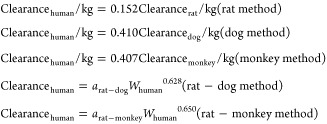
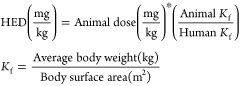
Interspecies Scaling Parameters based on Clearance and Human Equivalent Dose
Interspecies scaling techniques have been commonly used in the prediction of pharmacokinetic parameters of different species.32 Allometric scaling is an empirical method that is used in interspecies scale-up based on the similarities in the anatomy, physiology and biochemistry of the cross-species in terms of power functions that correlate the physiological parameters with body size. This method has been used in the projection of the human pharmacokinetics for small molecule drugs and also for therapeutic proteins. Allometric scaling has also been widely used in the pharmaceutical industry for the initial decision-making for the various stages in drug discovery and development. The main equation used in the allometric scaling is described as follows:33
where Y is the parameter of interest, BW is the body weight, and a and b are the coefficient and exponent of the allometric equation, respectively.
Allometric scaling of clearance using a single species to obtain human clearance was carried out in various ways such as based on the body weight of the species or in terms of the physiological factor of the species using different physiological parameters, i.e. liver weight (LW), kidney weight (KW), liver blood flow (LBF), kidney blood flow (KBF), and lymph flow rate (LFR). Some of the allometric scaling to predict human clearance described in the literature studies are shown in Table 2.
Table 2. Allometric Scaling to Predict Human Clearance.
| allometric scaling equation | allometric scaling method | notes | reference | |
|---|---|---|---|---|
| Single species scaling | BW is the body weight, b is the allometry exponent. Value of the allometry exponent is 0.60, 0.65, 0.70, 0.75, 0.80, 0.85, or 0.9033 | (33, 34) | ||
| Single species scaling | BW is the body weight | (35) | ||
|
One- or two-species scaling by Tang method | arat-dog is the coefficient for rat-dog method; arat-monkey is the coefficient for rat-monkey method | (36) | |
|
Single species scaling using hepatic blood flow | HBF is the hepatic blood flow | (35) | |
| Scaling using liver blood flow | LBF is the liver blood flow, the value of LBF (mL/min/kg) should be multiplied by the corresponding body weight of the species | (33, 36) | ||
| Multiple species scaling by simple allometry (SA) | BW is the body weight, a is the coefficient, and b is the allometry exponent | (33, 34) | ||
| Multiple species scaling by exponent rule-corrected allometry (ROE) | MLP is the maximum life-span potential and BRW is the brain weight of the organism, BW is the body weight, a is the coefficient, and b is the allometry exponent | (33, 34) | ||
| If b < 0.71 in simple allometry, no correction factor is applied; if 0.71 ≤ b < 1, MLP is used as a correction factor; if 1 ≤ b, BRW is used as an correction factor33 If 0.56 < b < 0.70, simple allometry is used, 0.71 < b < 0.99 or 1.0 ≤ b ≤ 1.3 MLP or BRW is used for small molecules34 | ||||
| Product of MLP and Clearance (MLP × Clearance) | MLP is the maximum life-span potential and BW is the body weight, a is the coefficient, b is the allometry exponent, 93.4 is the human MLP in years, and this relation is predicted for the human clearance of Antibody–drug conjugates (ADCs) | (34) | ||
| Product of Brain Weight and Clearance (BRW × Clearance) | BRW is the brain weight, BW is the body weight, a is the coefficient, b is the allometry exponent, 1400 is the human brain weight in grams, and this relation is predicted for the human clearance of Antibody–drug conjugates (ADCs) | (34) | ||
|
Multiple species scaling by multiexponential allometry (MA) | BW is the body weight, a is the coefficient and b is the allometry exponent determined from the simple allometry analysis. | (33) | |
|
Multiple species scaling by exponent rule-corrected multiexponential allometry (SA+MA) | BW is the body weight, a is the coefficient and b is the allometry exponent. If b < 0.71, simple allometry method is applied with no correction factor; if b ≥ 0.71, the multiexponential allometry equation is used. | (33) | |
|
Single species scaling using different physiological parameters | LW is the liver weight, KW is the kidney weight, LBF is the liver blood flow, KBF is the kidney blood flow, and LFR is the lymph flow rate | (37) |
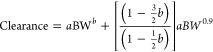
Human Equivalent Dose (HED) prediction can be carried out by a variety of methods, as shown in Table 3: linear method based on clearance values, exponential method based on clearance values, the method based on body weight, the method based on predicted human clearance and the method based on correction factor.
Table 3. Human Equivalent Dose (HED) Prediction Methods.
| HED prediction equation | HED prediction method | notes | reference | |
|---|---|---|---|---|
| Dose prediction by linear method based on clearance values | Dose and clearance values are in absolute numbers, not normalized to body weight | (37) | ||
| Dose prediction by exponential method based on clearance values | Dose and clearance values are in absolute numbers, not normalized to body weight | (37) | ||
| Dose prediction based on body weight | Dose values are normalized to body weight | (37−39) | ||
|
Dose prediction based on predicted human clearance | Dose values are normalized to body weight | (37) | |
|
Dose prediction based on correction factor | Kf is the correction factor; dose values are normalized to body weight | (38−40) |
Benefits and Drawbacks of Allometric Scaling Approach in Predicting Drug and Nanomaterial Clearance
Clearance is regarded as the most important pharmacokinetic parameter that affects the distribution of the drug. The prediction of human clearance is very crucial in early drug discovery and development, but there is a conflict on the most suitable method to attain the clearance data.35
Among different pharmacokinetic parameters belonging to a drug or a nanoparticle, systemic clearance is the most scaled parameter from preclinical data using allometry. The implementation of statistical analyses of allometric scaling functions and variables for the pharmacokinetic parameter of nanoparticles has not been possible due to the limited number of nanoparticle-based clinical investigations and also the difficulty of attaining appropriate multispecies pharmacokinetic data from the literature.41 In contrast to small molecule drugs, limited studies on the multispecies data of nanoparticles prevent the identification of correlations between nanoparticle-specific properties and biases in allometric relationships.41 Furthermore, studies have shown that despite having similar physicochemical characteristics, certain nanoparticles, for example, three types of PEGylated liposomal NPs loaded with anticancer drugs, exhibit different allometric coefficients and exponents. This discrepancy arises due to their varying pharmacokinetic profiles within the same species, even when administered at comparable doses.42
Making generalizations based on interspecies allometric relationships of nanoparticles even with similar physicochemical characteristics is not effective due to showing different dispositions and pharmacokinetic profiles.41 It should be also stated that the simple allometry approach carried out for drugs and nanoparticles can cause predictive errors when applying interspecies scaling to humans since scaling up the physicochemical, anatomical, physiological, and biochemical properties based on body weight does not always show accurate results.41 The possible reasons that result in predictive errors in allometric scaling to humans can be regarded as the differences in interspecies hepatic metabolism, species-dependent pharmacokinetic profiles for nanoparticles or nanoparticles showing a nonlinear relationship with the dosage, species-specific differences in protein interactions with nanoparticles and drugs, and the requirement of at least three or more species of animals to obtain robust correlation.41
To improve the predictive performance of the interspecies allometric scaling in terms of clearance of the drug or nanoparticles, some modifications have been carried out to the standard power-law function by the inclusion of different factors such as maximum life-span potential (MLP), organ weights (e.g., brain weight, liver weight, etc.), in vitro metabolic data (e.g., from liver hepatocyte or microsome assays), blood flows (e.g., liver blood flow of monkey), and correction for protein binding (differences in fraction unbound values), etc. Each of the allometric scaling methods used for the prediction of the clearance has their benefits and drawbacks in terms of different aspects as the summary table is provided in Table 4.
Table 4. Benefits and Drawbacks of Several Allometric Scaling Methods Employed for the Prediction of Clearance (CL).
| allometric scaling methods based on clearance | benefits | drawbacks |
|---|---|---|
| Simple Allometry (SA) | Frequently used, simple, and fast method32 | Poor for the drugs that are significantly eliminated by biliary excretion, renally eliminated with significant reabsorption, drugs with extensive metabolism, and combination of hepatic metabolism and renal excretion32 |
| Least successful in predicting clearance for the drugs metabolized in the liver with a low extraction rate32 | ||
| Good for the drugs that are renally excreted drugs and low-protein bound drugs32 | ||
| Product of CL and Maximal Life Potential (CL × MLP) or CL and brain weight (CL × BRW) | Improves the predictive performance of scaling compared to SA32 | Not suitable for large animals because of higher prediction errors32 |
| Enhances the prediction for the drugs that are hepatic metabolized and renally eliminated32 | Mathematical manipulation; does not have any physiological relevance32 | |
| Scaling by rule of exponents (ROE) | Enhances the prediction greatly compared to SA, CL × MLP and CL × BRW32 | Results in prediction errors in larger preclinical animals (and humans)42 |
| Improves the predictive power for the drugs and nanoparticles with extensive hepatic metabolism42 | The accuracy of the prediction depends on the type of species used32 | |
| Unable to be used for renally excreted drugs32 | ||
| At least three animal species are needed to correctly apply ROE34 | ||
| Scaling by multiexponential allometry (MA) | Successful in predicting human clearance46 | When used with preclinical data from more than 3 species accuracy improves47 |
| Prediction accuracy is higher than SA but lower than ROE48 | ||
| Monkey Hepatic Blood Flow Approach | Successful method to predict human clearance compared to SA47 | Least successful for renally excreted drugs32 |
| Only requires CL of monkey48 | Not a commonly used method; the prediction is based on an empirical assumption48 | |
| Successful in the prediction for the biliary excreted drugs32 | ||
| Scaling from one or two animal species | Requires only clearance from one or two species48 | Neglects interspecies differences in metabolism and protein binding48 |
| Vertical allometry and fraction unbound (FU) corrected intercept method (FCIM) | Improved accuracy due to taking into account the interspecies differences in protein binding48 | Requires the data for the fraction unbound value in plasma48 |
| Prediction accuracy is enhanced for the drugs having high extraction rate32 | ||
| Incorporation with physicochemical properties of a drug | Predicts clearance from molecular weight, clogP, and the number of hydrogen bond acceptors49 | Requires comprehensive computational effort |
| Predicts human clearance using regression methods, multiple linear regression (MLR) analysis, partial least-squares (PLS) method, and artificial neural network (ANN)49 | ||
| Incorporation of IVIVE by using in vitro data (hepatocytes, microsomes, etc.) and interspacing scaling | Improved prediction of in vivo CL in different species by adjusting CL for relative metabolism rates obtained in vitro(32) | Can only be applied to the drugs that are metabolized in liver; not suitable for the drugs that are renally eliminated or eliminated both by hepatic and renal excretion32 |
| Requires only in vitro data;48 provides the inclusion of interspecies differences in hepatic metabolism in predicting CL32 |
Some of the allometric scaling methods are regarded as impractical due to different aspects; for example, although improving the predictive performance of the scaling compared to simple allometry, the product of clearance and maximal life potential (CL × MLP) or clearance and brain weight (CL × BRW) methods are regarded as providing only mathematical adjustments without physiological significance.32 Pure in vitro to in vivo extrapolation (IVIVE) methods may yield inaccurate results when extrapolating drug-specific parameters such as Km and Vmax, derived from cellular components (e.g., hepatocytes) and subcellular components (e.g., microsomes) of organs. This inaccuracy arises because these methods often neglect the effects of physiological processes and the interactions between the drug and both the intracellular and extracellular environments.43 Additionally, when incorporating in vitro data from components like hepatocytes and microsomes to obtain in vivo clearance values, the predicted clearance can be misleading for drugs that are renally eliminated or eliminated by both hepatic and renal excretion. This method is valid only for drugs that are metabolized only in the liver.32
The scaling method of rule of exponents (ROE) proposed by Mahmood and Balian in 199644 was applied in allometric scaling studies based on nanoparticle pharmacokinetics and resulted in successful outcomes for PEGylated liposomal anticancer drugs.42 In the study of pharmacokinetics using the allometry on PEGylated liposomal anticancer drugs with the addition of MLP to the standard allometric equation, the linear correlation of the allometric scaling function in preclinical animal models was enhanced.42 In a previous pharmacokinetic study, the clearance data of colloidal tumor necrosis factor-alpha (TNF)-gold nanoparticles in rabbit, rat, and oncology patients were scaled by allometric scaling using a power model and were not found predictive for the human clearance.45 To improve the predictability of the human clearance, Mahmood’s ROE model with the inclusion of brain weight as a multiplication factor to clearance was applied, and hence the correlation coefficient for the interspecies clearance model was improved significantly.45 The ROE method has been reported to significantly improve the predictive power of the allometric relations for drugs and nanoparticles with extensive hepatic metabolism; however, this method resulted in predictive errors in larger preclinical animals and humans contingent on the types of species used in fitting.41
In Vivo Conditions of Nanoparticles and Their Challenges on ADME and Scaling
Since the measured physicochemical properties of nanoparticles such as size, surface charge, and surface chemistry are not the only factors in the determination of in vivo disposition properties of nanoparticles, the correlation of in vitro nanoparticle properties with in vivo disposition is a compelling issue.4 Also, other than particle properties there are other determinants to account for the in vivo conditions of nanoparticles such as aggregation and biocorona formation.4 When the nanoparticles are introduced into biological fluids, biomolecular corona formation occurs, where the process consists of the spontaneous adsorption of proteins, lipids, metabolites, nucleic acids, and sugar moieties on the surface of the nanoparticles.50 The biomolecular corona formation of the nanoparticle surfaces changes the physiochemical properties and influences their subsequent interactions with the biosystems, and hence the content of the biomolecular corona determines the effects of the nanoparticles on the biological systems.50 Most of the studies focus on the adsorption of the proteins regarding the formation of protein-corona on the nanoparticle surfaces.50 Protein-corona formation may provide beneficial outcomes for disease diagnosis and personalized nanomedicine when desired adjustments are done for the optimization of cell internalization or for the improvement of in vivo biodistribution.50 However, by affecting the disposition and pharmacokinetic profiles of nanoparticles, the protein-corona formation may limit the access and distribution of nanomaterials to their targeted sites of action and excretion.41
The formation and stabilization of biomolecular coronas within the body are generally directed by the thermodynamics and the biological environment; these corona formation processes are independent of the physiological rates within the organism including the basal metabolic rate (BMR). This situation makes the prediction of pharmacokinetic parameters and simple extrapolations of the nanoparticles debatable.32 To attain better nanoparticle characteristics in vivo, the allometric scaling approaches (allometric extrapolation of pharmacokinetic parameters) should be improved.41
A pharmacokinetic model on the potential fate of NPs in vivo took the rate processes dependent on basal metabolic rate and the dynamics of protein corona into account.51 The time scales on which metabolic and physiological processes occur and the protein-corona formation kinetics differing from each other that consequently result in mismatches were assumed to contribute significant differences in interspecies extrapolations of nanoparticle biodistribution.51 Across two species, the effect of corona formation on nanoparticle biodistribution was highest when the half-life of the corona transition is similar to the geometric average of NP half-lives of the two species.51 The interspecies differences in the blood proteomes can bring about different compositions of protein-coronas which may lead to inaccuracies in the extrapolation results.52 Consequently, since allometric power-law functions are not adequate to describe the effect of protein-corona formation on the surface of the nanoparticles, novel strategies that combine experimental in vitro and in vivo data and in silico modeling methods by taking into account biocorona dynamics are crucial to extrapolate the pharmacokinetics of nanoparticles.
The pharmacokinetics of tumor necrosis factor-alpha (TNF)-gold nanoparticles that were predicted for rats and rabbits were scaled to humans by an allometric scaling approach.45 The allometric correlation between the clearance value and the body weight was found to be moderately predictive in humans.45 Following adjustments on the simple allometric equation in the determination of clearance by using the multiplication factor as brain weight, the scaling prediction was significantly improved.45 However, since preclinical data from at least three species were required to predict the exponent of powers in model scaling to determine the clearance by regression analysis, better predictions can be obtained when the number of species is increased in the model for TNF-gold nanoparticles. A study carried out a simple allometric scaling approach to deferoxamine-based nanochelator (DFO-NP) in rats to predict pharmacokinetic parameters in mice and humans.53 This method predicted the serum concentration–time profile of DFO-NPs to be very close to the experimentally determined values in mice, and nonlinear disposition and absorption models were validated for DFO-NPs for multiple doses across the species.53 The pharmacokinetic profile of DFO-NPs in humans was predicted by carrying out allometric scaling by applying clinically meaningful dosages, and pharmacokinetic simulations were carried out demonstrating improved pharmacokinetics by a nanochelator compared to PK profiles after typical infusion protocols of DFO.53 However, some limitations have been reported such as the requirement of setting up DFO-NP-specific allometric exponents for all the mechanisms incorporated in the pharmacokinetic model to increase the accuracy of the prediction.53 Another constraint in the model was explained as using simple allometry in the scaling of nonlinear pharmacokinetics may be unreliable.53
In the allometric scaling of nanomaterial pharmacokinetics, another challenge encountered for many of the intravenously administered nanoparticles is the nonlinear or dose-independent disposition and pharmacokinetic profiles.41 There is no theoretical framework to scale nonlinear pharmacokinetic parameters by carrying out allometric approaches because the pharmacokinetic parameters display relationships with various independent variables, such as dosage and body weight, that can be described by multiple linear regression analysis rather than the power-law function.41 These nonlinearities generally stem from the saturation of elimination mechanisms associated with the phagocytic cells of the mononuclear phagocyte system (MPS) organs, such as spleen, liver, bone marrow, and lungs, within the framework of the nanoparticles cleared by hepatic elimination after intravenous administration.41 A previous study compared the disposition of pegylated liposomal anticancer drugs across species of male and female mice, rats, dogs, and patients with refractory solid tumors, by substituting the physiological parameters of body weight in the allometric equation to predict clearance by the factors related to the mononuclear phagocyte system (MPS).42 The parameter that showed the strongest correlation to liposomal clearance was found as the total monocyte count, and this parameter was attributed as a better physiological variable for the allometric scaling of pegylated liposomes in animals and humans.42 Hence, it was interpreted that MPS-associated factors such as monocyte count may enhance the clearance prediction in humans.42
To sum up, although substantial efforts have been spent on the improvement of nanoparticle interspecies allometric scaling in terms of their pharmacokinetic parameters, there are some restrictions to derive such correlations across species. The protein-corona formation on the surface of the nanoparticles when introduced into biological fluids, the nonlinear disposition and pharmacokinetic profiles with prolonged circulation time of nanoparticles, and their comprehensive interactions with MPS organs especially the liver can be regarded as outstanding challenges for scaling nanomaterial pharmacokinetics. Moreover, different physicochemical properties such as size, shape, surface modification of the nanoparticles and distinct pharmacokinetic profiles make the development of generalized allometric relationships difficult for different types of nanoparticles. Investigating different allometric scaling methods by analyzing multispecies data and determining the advantages and disadvantages of these relationships is crucial. With careful consideration of the requirements of each method, improvements in these correlations play a critical role in developing enhanced scaling approaches for nanoparticle pharmacokinetics.
In Vitro to In Vivo Extrapolation (IVIVE) Studies and Challenges
The use of in vitro and in silico methods in the determination of the pharmacokinetic properties or toxicology levels of the compounds has attracted great attention when the scientific, ethical, and practical issues considered in in vivo methods are taken into account. While in vitro experiments facilitate fast application across large chemical sets, elucidation of the data obtained from these methods is sometimes challenging because of the mechanistic nature of many assays.54 In this aspect, in vitro to in vivo extrapolation (IVIVE) has become a promising computational tool to provide in vivo predictions from results obtained by in vitro and in silico studies. The term IVIVE was traditionally used in the literature to refer to the estimation of in vivo whole-organ ADME properties by scaling from the properties obtained from in vitro methods whose results were used in the construction of bottom-up pharmacokinetic (PK) and PBPK models.55 The ADME parameters that are commonly determined via in vitro analysis methods are plasma protein binding fraction, hepatic metabolism, and intestinal absorption.55 Current in vitro methods also facilitate the calculation of the parameters such as, glucuronidation, renal clearance, extrahepatic clearance, and tissue or blood partition coefficients.55 Lately, IVIVE methods have been used to describe the conversion of in vitro concentration of the molecule related to its bioactivity into an external exposure level.55 This procedure, also referred to as reverse dosimetry, includes the determination of the required drug exposure level that results in the plasma or tissue concentration equivalent to the in vitro concentration by carrying out PK modeling.55 At this point, some important factors should be examined while conducting IVIVE approaches such as the selection of the kinetic model and parametrization of exposure, the modeling technique of the test article, and the selection of in vitro assays.56 Although IVIVE methods for dosimetry generally consider that the chemicals in in vitro systems behave the same way as in the blood or tissue of an organism, the presence of various kinetic factors in in vivo studies such as chemical binding to proteins and lipids in the culture medium, degradation processes, internalization processes in the cultured cells, etc. make this assumption inappropriate.55 Hence, the in vitro bioactivity concentration of the drug needs to be adjusted according to these kinetic factors.
For the characterization of the metabolism, literature data are generally used to obtain metabolic clearance data.57 In most of the published data, subcellular fractions such as microsomes, cytosol, or primary cell monoculture systems have been used in in vitro determination of the clearance values.57 The major challenge encountered when using literature data in the parametrization of IVIVE models is that in vivo metabolism processes include integrated systems that contain interaction and competing reactions, and these may not be fully ensured by the simplified systems used in the in vitro studies.57 For example, when microsomal fractions are used in the determination of metabolic data of a compound via in vitro studies, this method is limited only to specific processes such as phase I cytochrome-P450-mediated oxidative reactions, epoxide hydrolases, carboxylesterases, and phase II metabolism via glucuronide conjugation.57 However, some of the enzymes such as soluble phase II enzymes including glutathione S-transferases and sulfotransferases are neglected.57 In this aspect, comprehensive research has shown that freshly isolated primary hepatocytes, which express most of the proteins in the human liver including the proteins related to the membrane transport, metabolism, and receptor-mediated processes are promising systems both for the determination of hepatic metabolism and metabolite mediated effects of compounds.57 However, this system has also drawbacks such as a limited time of viability in suspension form, and a rapid change in enzyme activity in the plated form of primary hepatocytes.57 Novel techniques should be developed to overcome these limitations to stabilize the hepatic phenotype for longer durations.
While pharmacokinetic (PK) modeling has been generally used to estimate plasma or tissue concentrations following in vivo exposure, recently PK models have been used for reverse dosimetry approaches, which refer to the exposure dosage prediction, that provides specific plasma or tissue concentrations equal to the bioactive concentrations resulting from in vitro assays.56 In this aspect, several parameters such as metabolic pathways, exposure routes, tissue compartments, systemic clearance, plasma protein binding, and the dosage regimen should be carefully taken into account. Research has shown that one-compartmental models that provide rough estimates with minimal input parameters are not sufficient to differentiate between various exposure routes.56 Hence complex multiple-compartment and PBPK models have been shown to describe complex biological processes of in vivo systems better, but with requirements of more specific input parameters such as tissue-specific physiological and metabolic parameters and tissue-to-plasma partitioning coefficients.56 In a study that has used an (IVIVE)-linked mechanistic PBPK framework for modeling liver transporters and their interaction with liver metabolizing enzymes, area under the plasma concentration–time curve (AUC), maximum concentration (Cmax), and the time to reach Cmax (tmax) values were obtained within 2-fold of the observed data between the dose range of 10–80 mg of rosuvastatin, and the validated model was shown to be satisfactory for integration of wide range of in vitro and in vivo data.58
One of the challenges in the applications of IVIVE approaches arises from the in vitro toxicity testing. It is very important in in vitro toxicity testing to differentiate between the specific disruption of biomolecular targets or pathways and the generalized disruption of cellular machinery which results in cell stress and cytotoxicity.55 Investigations on the general cell stress response and cytotoxicity analyses are significant to distinguish cytotoxic bursts of nonspecific mechanisms such as necrosis and regenerative proliferation from the specific effects on the particular molecular targets.55 A recent study developed a Bayesian multispecies PBPK model for interspecies extrapolation and IVIVE, and incorporated toxicogenomic dose–response data into the PBPK model to determine chemical risk assessment.59 In that study, perfluorooctanesulfonate (PFOS) was used in the determination of risk assessment, and results showed reference doses (RfDs) for the most sensitive pathways and diseases were found similar to the recent European Food Safety Authority’s guidance values.59 These results show that for human health risk assessment of the chemicals, the usage of toxicogenomic dose–response data in combination with PBPK modeling is a promising tool, being a nonanimal alternative to traditional risk assessment.59
In the case of nanomaterials, the quantification of an in vivo toxicokinetic (TK) profile from in vitro studies is challenging unless appropriate IVIVE methods are applied due to the dosimetry consideration between in vitro and in vivo experimental designs.60 In in vitro studies, the exposed dose of the nanomaterials to the cell medium is not equal to the dose that is delivered to the cell because of the agglomeration, aggregation, diffusion, and sedimentation properties of the nanomaterials.60 Moreover, protein-nanoparticle corona formation should also be considered due to the differences in the type of proteins present in the cell culture media in vitro and the proteins present in the plasma in vivo.60 The delivered dose of the nanomaterials to the target organ in in vivo testing is affected by the physiochemical properties such as size, zeta potential, surface functionalization, and agglomeration state.60 Also, these properties affect the cellular uptake mechanism and degree of internalization of the nanomaterials inside the cell. To sum up, the determination of target organ exposure to the nanomaterials is challenging due to different physicochemical factors dominating in vitro cell culture and in vivo conditions resulting in differences in nanomaterial properties. Thus, the application of proper IVIVE methods is significant when using in vitro dosimetry and toxicity data to determine the in vivo toxicity and TK profiles. In this regard, PBPK modeling can be a promising approach in the determination of TK profiles of nanomaterials, and it facilitates the prediction of target organ dosimetry by correlating external doses administered through various routes of administration. Moreover, it allows for extrapolation across species exposure paradigms and from in vitro to in vivo settings.60 A recent study has used nanomaterial IVIVE for cellular uptake and toxicity data and incorporated it into the PBPK model for the toxicity assessment of gold nanoparticles (AuNPs).61
While many PBPK modeling approaches like IVIVE, interspecies extrapolation, and route-to-route extrapolation have been carried out for small molecules, their applicability for nanomaterials has been debated due to various factors related to nanomaterials such as nanoparticle–protein corona formation in different biological fluids. Hence, systematic and appropriate methodologies of PBPK modeling should be developed for nanoparticles.
Physiologically Based Pharmacokinetic (PBPK) Modeling Applications of Nanoparticles
The use of nanoparticle-based drug delivery systems facilitates the development of therapeutics with enhanced solubility, improved therapeutic index, and improved targeting of the diseased cells.5 Among the various advantages of encapsulating drugs into nanoparticles are better control of pharmacokinetic properties of therapeutic substances such as circulation half-life and release characteristics, and restricting the drug interactions with the healthy tissues.62 Physiologically based pharmacokinetic modeling has risen to prominence as a robust quantitative tool, owing to its capability to precisely simulate the disposition of nanoparticle or nanoparticle-drug hybrid systems within the body. Such precise modeling holds paramount importance in advancing the development of nanoparticle-based drug delivery systems as well as in assessing the safety, efficacy, and quality of nanoparticle-drug systems. In addition to providing a more mechanistic approach to the determination of drug disposition for individual tissues and organs, PBPK modeling and simulation also facilitate the prediction of human pharmacokinetics from preclinical investigations.11 PBPK modeling enables the study of the biokinetics of nanoparticle-drug systems to model past experimental data and also to figure out the suitable drug dosage by carrying out simulations.2
Different from the traditional one-compartment pharmacokinetic modeling, PBPK modeling allows the inclusion of more physiological processes. Each compartment in PBPK models is explained as a permeability-limited model (diffusion-limited or membrane-limited model) or perfusion-limited model (flow-limited model).3,17,62−64 In the PBPK model structure of NPs, both permeability-limited (membrane-limited) and perfusion-limited (flow-limited) models can be used to explain the transfer of NPs from the blood to the tissue compartments.17 In the permeability-limited model the main barrier of the nanodrug complex is regarded as tissue cell membranes, whereas in the perfusion-limited model, the only limiting factor of nanodrug complex penetration through tissue cell membrane is regarded as blood perfusion. In the perfusion-limited model, it is assumed that the transportation of the nanoparticles into tissues is very fast, and the equilibrium between blood and tissue can be obtained instantly.62 In this model, nanoparticle transportation into the tissues depends on its blood supply.62 In the permeability-limited model, a membrane is assumed at the capillary or cellular membrane, or both.62 In this model, NP transportation across cellular membranes depends on endocytic uptake mechanisms (i.e., phagocytosis, macropinocytosis, and receptor-mediated endocytosis) and exocytic release.62 Perfusion-limited and permeability-limited tissue models are represented in Figure 3.
Figure 3.
Perfusion-limited and permeability-limited tissue models. Reproduced with permission from ref (62) with minor modifications in the scheme (figure was redrawn and the wordings were paraphrased). Open Access. CC-BY 4.0 license. Copyright: © 2022 by the authors. Licensee MDPI, Basel, Switzerland. URL: https://www.mdpi.com/1422-0067/23/20/12560. No endorsement.
While the exchange of small molecules between tissue and blood is governed by perfusion (flow), the transfer of nanoparticles between blood and tissue is mainly constrained by permeability. Hence, while constructing nanoparticle-based PBPK models, the consideration of permeability (diffusion) limited processes is crucial to obtain accurate results. In the literature, the membrane-limited models were well described for the smaller-sized nanoparticles, e.g. 13 nm of PEG-coated gold NPs (AuNPs),17 whereas the perfusion-limited models were more suitable for the larger-sized nanoparticles, such as 100 nm of PEG-coated gold NPs (AuNPs).17 The biodistribution of AuNPs was assumed to be controlled by two main processes; the first was the capability of the nanoparticles to cross the capillary membrane of the organs, and the latter was the internalization of the nanoparticles by the process of endocytosis.17 The rate of change of the number of NPs in PCs was assumed to be equal to the internalization rate from the tissue (or blood) minus the release rate from the PCs back to the tissue (or blood). The actual uptake rate of the NPs by PCs depended on the uptake rate parameter and the amount of NP for uptake. The equations describing the rate of uptake, release, and mass transfer of small-sized AuNPs in the PCs are shown below:17
 |
where Rup_t is the uptake rate of the NPs from tissue to PCs in organ t, in mg/h, Atissue_t is the amount of NPs in the tissue subcompartment in organ t, in mg, Rrelease_t is the release rate of the NPs from the PCs to the tissue in organ t, in mg/h, Krelease_t is the release rate parameter of NPs in the organ t, in 1/h, APC_t is the is the amount of NPs in the PCs in organ t, in mg, RPC_t is the rate of change in the mass of NPs in the PCs, in mg/h.
In the permeability-limited (membrane-limited) model, each of the compartments contained vascular and tissue spaces and the kinetics of the NPs in the capillary blood, and the tissue of each organ should be described separately. Two kinetic parameters were considered in the modeling of mass transfer between two subcompartments: the ability of AuNPs to diffuse through the capillary wall of the organs and the degree of endocytosis process from the tissue or blood to PCs. The kinetics of the nanoparticles (13 nm AuNPs) in the subcompartments is described as follows:17
where, Rblood_t is the rate of change of the amount of AuNPs in the capillary blood subcompartment of the organ t, in mg/h, Rtissue_t is the rate of change of the amount of AuNPs in the tissue subcompartment of the organ t, in mg/h, is the blood flow rate to the organ t in L/h, Ca is the AuNP concentration in the arterial blood of organ t in mg/L, CVt is the AuNP concentration in the venous blood of organ t in mg/L, PAt permeability area cross product between the capillary blood and the tissue of the organ t, in L/h, Ctissue_t is the AuNP concentration in the tissue subcompartment, in mg/L, Pt is the tissue to plasma distribution coefficient for the organ t, unitless.
The PBPK model development scheme of nanoparticles is represented in Figure 4. The previously published PBPK models for nanoparticles are summarized in Table 5, with selected notable examples detailed below. In the PBPK model constructed for methoxy poly(ethylene glycol)-poly(″ε-caprolactone) (mPEG-PCL) NPs which were intravenously administered to mice, while using quantification data and direct visualization of specific organs, the PBPK model was focused on the phagocytosis process to reveal nanoparticle kinetics within and among the organs in mice.13 The developed model integrated the cellular processes such as phagocytosis and the enhanced permeability and retention (EPR) effects. Both permeability-limited and membrane-limited models were incorporated within the PBPK model, and the results showed that the membrane-limited model was more appropriate to characterize the experimental data. The phagocytic cells (PCs)-PBPK model showed better performance than the enhanced permeability and retention (EPR)-PBPK model, and this model enabled the quantitative representation and prediction of concentration–time profiles and degree of exposure for the mPEG-PCL NPs in blood and different organs.13
Figure 4.
PBPK model development scheme of nanoparticles.
Table 5. Summary of Previously Published PBPK Models for Nanoparticles.
| type of the nanoparticle | nanoparticle name and physicochemical properties (if available) | modeling species | administration route | data available for model development and validation and software for simulation | PBPK model description | reference |
|---|---|---|---|---|---|---|
| Metal-Oxide NPs | 15–150 nm of nano-TiO2 NPs | Mice and Rats | Intravenous (IV), oral, and dermal administration | • Organ titanium concentration from toxicokinetic data | • Permeability (membrane) limited model included | Bachler et al., 201577 |
| • Modified from the literature model18 | • Two processes are simultaneously considered: NPs to cross the capillary wall of the organs and to transport from blood to tissues by phagocytosis in the mononuclear phagocyte system (MPS). | |||||
| • Model was validated by comparing simulated organ levels with independent in vivo experimental data.75,76 | • The size and crystalline structure of nano-TiO2 had a minor effect on the biodistribution; NPs agglomerate at high internal exposure in vivo and are internalized by macrophages in the MPS. | |||||
| Metal-Oxide NPs | 25 and 90 nm Cerium oxide (CeO2) NPs | Rats | Inhalation | • Amount of CeO2 in lungs, accumulated feces, extrapulmonary organs, gastrointestinal (GI) tract data | • Model was based on PBPK of previously the published version of the study for intravenously injected nanoparticles.31,78 Deposition in the respiratory system and transfer to the gastrointestinal (GI) tract was involved for the inhalation exposure. | Li et al., 201630 |
| •The PBPK model was carried out in Berkeley Madonna version 8.3.18 (Berkeley, CA) and acslX version 3.0.2.1. | • In the model, both permeability and perfusion limited models were used. | |||||
| •The PBPK model successfully predicted biodistribution of CeO2 in various organs and identified that most of the nanoparticles that were not eliminated by feces were internalized by the phagocytizing cells (PCs) in the pulmonary region. | ||||||
| Inorganic NPs | Cerium oxide (CeO2) NPs | Rats | Intravenous (IV) | • Various organs (liver, kidneys, brain, spleen, lungs, blood, heart, GIT, rest) concentration of NP data from experimental study was used for calibration and optimization of the model.79 | • PBPK model was constructed based on the model introduced by the previous literature study.30 | Kasyanova et al., 202069 |
| • Model was validated using independent biodistribution study.80 | • Model included the nanoparticles uptake by phagocytes, as well as different ways of NP removal from the body. | |||||
| • PBPK simulations of CeO2 NPs were carried out using Matlab Simbiology R2018b software. | • PBPK model sufficiently described and predicted the biokinetics of intravenously administered CeO2 NPs in the body of rats. | |||||
| NP-drug or NP-biochemical conjugates | 110 nm of Dexamethasone-loaded block copolymer nanoparticles (Dex-NPs) | BALB/c mice | Intravenous (IV) | • Plasma, liver, spleen and kidney concentration data | • Perfusion-limited model applied to tissue compartments and an additional theoretical “other” organ compartment which is connected to the liver, spleen, and kidney included. This compartment stood for the loss of the administered dose injected. | Gilkey et al., 201582 |
| • Simulations were produced using the experimental data of the previously published in vivo study.81 | • Simulation results were in line with the literature data.81 | |||||
| • Simulations were conducted via MATLAB. | ||||||
| NP-drug or NP-biochemical conjugates | 25 nm of AuNPs capped with epigallocatechin gallate (EGCG-AuNP) or 19.62 nm of AuNPs capped with curcumin Curc-AuNP | Mice and Rats | Intraperitoneal (IP) Injection | • Amount of NP in heart, kidney, liver, lung, spleen, stomach data | • MPS and whole lymphatic system was included in the model. | Aborig et al., 201925 |
| • The PBPK model was built and evaluated in MATLAB R2017a using the Intiquan toolbox (IQMTools v1.2.2.2) by Henning Schmidt | • Model evaluation was carried in order to extrapolate biodistribution to other species using experimental data of previous studies.83,84 | |||||
| • Model parametrization was done using PK-Sim | • In the model, organism-specific parameters were adapted to represent rats, and the rat PBPK model was obtained. | |||||
| • Strong uptake was observed in the liver and spleen in which extravasation and phagocytosis were major mechanisms. | ||||||
| Organic NPs | Methoxy poly(ethylene glycol)-poly(″ε-caprolactone) (mPEG-PCL) NPs | Mice | Intravenous (IV) | • Blood, heart, liver, spleen, lung, kidney, and tumors concentration of NP data | • Both blood-flow- and membrane-limited models were applied, and the membrane-limited model was found to be the most suitable model to describe their experimental data. | Li et al., 202113 |
| * The PBPK model of NPs was simulated using Berkeley Madonna v.8.3.23. | • Subcompartment of phagocytic cells (PCs) in the blood compartments was not included since its effect was found to be insignificant in terms of the model fitting. | |||||
| • Enhanced permeability and retention (EPR) effects were integrated into a tumor subcompartment. | ||||||
| • Both the PCs-PBPK model and EPR-PBPK model were generated, and the PCs-PBPK model showed better performance. | ||||||
| Organic NPs | 121.8 nm of Poly(alkyl cyanoacrylate) (PACA) loaded with cabazitaxel (PACA-Cbz), and 52.2 nm of LipImage 815 | Rats | Intravenous (IV) | • Blood plasma, liver, spleen, lung, brain, heart, and kidney concentration data of cabazitaxel and LipImage 815. | • The model framework was based on a PBPK model developed previously to describe distribution of CeO2 nanoparticles.30 | Minnema et al., 202285 |
| * Analyses were performed in R using the packages mrgSolve and adaptMCMC. | • Parameter estimation of the PBPK model was carried out by the Bayesian parameter estimation approach. | |||||
| • Results showed that the PBPK model can be adequately parametrized using biodistribution data. | ||||||
| • The estimated kinetic parameters may be beneficial to set up a more comprehensive database on kinetic information specific to nanobiomateirals. | ||||||
| Inorganic NPs | 13–20 nm and 80–100 nm of Polyethylene glycol-coated gold nanoparticles (PEG-coated AuNPs) | BALB/c mice | Intravenous (IV) | • Plasma, liver, spleen, kidney, lung concentration data | • Model was calibrated with the literature experimental data.86 | Lin et al., 201617 |
| • PBPK model was coded using the acslX | • Transfer of AuNPs from the blood to tissue compartments explained both by perfusion-limited and permeability (membrane) limited models. | |||||
| version 3.0.2.1. | • Both models were successful to simulate 100 nm AuNPs, but the permeability limited model showed better results for 13 nm AuNPs than the perfusion-limited model. | |||||
| • Final model was determined as the permeability limited model to stand for the varied sizes of AuNPs and validated with multiple independent data sets for the NPs of similar sizes. | ||||||
| Inorganic NPs | 1.4–200 nm of AuNPs | Rats | Intravenous (IV), oral gavage, intratracheal instillation, and endotracheal inhalation | • A mechanistic-based PBPK model was calibrated with experimental data sets. | • Tissue distribution of AuNPs was described by taking into account the permeability (membrane) limited transcapillary transport, different distribution of NPs between blood and tissue, endocytosis/phagocytosis using nonlinear functions and exocytic release. | Chou et al., 202265 |
| • Model was optimized using a Bayesian hierarchical approach with Markov chain Monte Carlo simulations. | • Route-specific approach: a multiroute PBPK model for different sizes of AuNPs | |||||
| • A multiple-linear regression-based quantitative structure–activity relationships (QSAR) model was developed and integrated into the PBPK model | • New route-specific approach had superior performance than the traditional approach. | |||||
| • Model was validated with independent data. | • The size and surface area of AuNPs were the main factors in the determination of endocytic/phagocytic uptake rates irrespective of the administration route. | |||||
| • Web-based nanoparticle interactive physiologically based pharmacokinetic (Nano-iPBPK) interface was developed. | • Zeta potential was a significant parameter to predict the exocytic release rates following IV administration. | |||||
| Inorganic NPs | 40 nm of AuNPs | Rats | intraperitoneal administration | • Plasma, liver, spleen, thymus, and brain concentration data | • The permeability (membrane) limited model was used in all tissues in the model. | Zazo et al., 202211 |
| • Simulations were conducted via with Phoenix WinNonlin 64. | • Two tissue compartments: vascular and extravascular which were separated by a cell membrane barrier. | |||||
| Inorganic NPs | 46, 69, 113, and 162 nm of mesoporous silica NPs | Rats | Intravenous (IV) | • Organ NP concentration data | • Whole-body disposition kinetics was simulated by constructing the PBPK model (without the tumor compartment), and tumor deliverability of NPs was investigated. | Dogra et al., 202068 |
| • The model was validated with the in vivo data from the previous literature study.87 | • MPS and lymphatic system were included in the model. | |||||
| • The analyses were performed in MATLAB R2018a. | • NP size, degradation rate, tumor blood viscosity, tumor vascular fraction, and tumor vascular porosity are the major factors affecting NP kinetics in the tumor interstitium. | |||||
| Inorganic NPs | 50 nm of gold NPs (AuNPs) attached with polyethylene glycol (PEG) | Rats | Intravenous (IV) | • Amount of AuNP in blood plasma, liver, spleen, lung, brain, heart, and kidney data | • Physiologically based kinetic (PBK) model framework initially proposed by a previous study was used.30 | Minnema et al., 202388 |
| • To parametrize the model, the model parameters were fitted to the in vivo biodistribution data. | • The model parameters were compared with PBK parameters for poly(alkyl cyanoacrylate) NPs loaded with cabazitaxel and for LipImage 815 which were studied in a previous work.85 | |||||
| • Analyses were performed via open-source software R using the program packages mrgSolve and adaptMCMC. | ||||||
| Inorganic NPs | 38.3 nm of Superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs) | Mice | Intraperitoneal (IP) injection | • Blood, liver, lung, and brain concentration of NP data | • Permeability (membrane) limited model was included. | Chen et al. 202228 |
| • PBPK model was calibrated and validated using the data of in vivo experimental results. | • To predict in vivo biodistribution of SPIO-Au-PEG NPs, the PBPK model was developed and the dynamic BBB crossing behavior of these NPs was investigated. | |||||
| • Set of ordinary differential equations (ODEs) were numerically solved using COMSOL Multiphysics. | • PBPK model results after incorporating the brain permeability displayed a good agreement with the in vivo results | |||||
| Inorganic NPs | 13 nm of Polyethylene glycol-coated gold NPs (PEG-AuNPs) | Rats | Injection via tail vein | • Blood, liver, spleen, kidney, and lungs concentration of NP data | • The perfusion rate-limited model was used with neglecting active uptake of NPs by phagocytes. | Dubaj et al., 202290 |
| • The biodistribution curves obtained from simulation were compared with the data in the previous study.89 | • The membrane permeability coefficient was set to 1 and the absorption rate of nanoparticles by phagocytes was set to 0 for all organs. | |||||
| • The PBPK model was carried out using the SimBiology toolbox (Matlab R2018b). | ||||||
| Inorganic NPs | 168.9 ± 1.1 nm of superparamagnetic iron oxide NPs (SPIONs) | Mice | Intravenous (IV) | • The murine PBPK model validation was carried out by comparing the simulated results with the in vivo pharmacokinetic data. | • Novel approach was performed in the integration of in vitro experimental data into the PBPK model identifying the uptake of SPIONs in murine macrophage cell line and primary human monocyte-derived macrophages. | Henrique Silva et al., 201791 |
| Human | • After validation, similar PBPK model for the simulation and distribution SPIONs in human was constructed. | • The modeling of NP penetration into the tissues was carried out by considering passive diffusion of NPs through the capillary endothelium and the active internalization of NPs by the macrophages in the liver, spleen, and lung. | ||||
| * The PBPK model was carried out in Matlab version 2014a using the Simbiology toolbox. | • The murine PBPK model accurately described accumulation of SPIONs in liver, spleen, and lungs. | |||||
| • Human PBPK model showed similar distribution results compared to the murine model with higher NP accumulation in liver and spleen. | ||||||
| Inorganic NPs | 4.2 nm of water-dispersible cadmium telluride/cadmium sulfide (CdTe/CdS) QDs | Mice | Intravenous (IV) and subcutaneous injection | • Blood, liver, spleen and kidney concentration of NP data | • Applicability of the model was evaluated by comparing the PBPK model with the experimental data with 3.5 nm of long-circulating and similar type of QDs.92 | Liang et al., 201629 |
| • The PBPK Model of NPs was simulated using Berkeley Madonna version 8.3.18. | • The predictability of the PBPK model for larger QDs (18.5 nm) was evaluated by using the experimental data.93 | |||||
| • PBPK model was validated using multiple external data sets and under various conditions and in different species. | • The interspecies predictability of the PBPK model was evaluated by comparing the results with the experimental data of 21.2 nm PEG-QDs from rats.94 | |||||
| Inorganic NPs | 34 ± 5 nm of Argovit-S Ag NPs | mice | Oral administration | • Brain, lungs, liver, testicles, and blood concentration of NP data.95 | • A mathematical chamber model describing the biokinetics of Ag NPs in the body of mice was developed based on the previously developed chamber model96 and experimental data.95 | Antsiferova et al., 202397 |
| • A program in Python was written to solve and visualize the PBPK model of NPs. The integrate.odeint function from the SciPy library was used. | • The obtained numerical parameters were compared with the previous study.96 | |||||
| • The chamber model described the biokinetics of Ag NPs in a living organism well; numerical differences found with the compared model were attributed to the different dosages of Ag NPs and species differences in model mammals. |
The permeability (membrane) limited approach was considered in the PBPK model developed for 38.3 nm superparamagnetic iron oxide nanoparticles coated by gold and conjugated with poly(ethylene glycol) (PEG) (SPIO-Au-PEG NPs) which were administered to mice via intraperitoneal (IP) injection.28 This model predicted in vivo biodistribution of SPIO-Au-PEG NPs, and the dynamic blood-brain-barrier (BBB) crossing behavior of these NPs was also incorporated into the model.28 After the integration of brain permeability, the PBPK model showed a strong correlation with the in vivo data, revealing that the propped model can anticipate in vivo biodistribution of SPIO-Au-PEG NPs under an external static magnetic field (SMF).
The traditional route-to-route extrapolation method that is applied for small molecules may not be suitable for the case of nanoparticles. A multiroute (intravenous (IV) injection, oral, intratracheal instillation, and endotracheal inhalation) PBPK model for various sizes (1.4–200 nm) of AuNPs has been constructed for rats.65 In the proposed model, the distribution of AuNPs in tissues was elaborated by considering the permeability-limited transcapillary transport, dynamic distribution of NPs between blood and tissue, processes like endocytosis/phagocytosis using nonlinear functions and exocytic release.65 Among the two approaches utilized, the novel route-specific approach showed enhanced efficiency compared to the traditional route-to-route extrapolation approach (mainly used for small molecules) implying that the traditional approach was inappropriate for NPs in the development of multiroute PBPK models for NPs.65
It has been reported that the physical and chemical characteristics of nanoparticles including size, surface area, and zeta potential have significant impacts on the pharmacokinetics and biodistribution within the body.65 Moreover, the size of the nanoparticles is closely linked to their renal clearance or excretion, predominantly because of the limitation on the pore size of glomerular filtration in the kidney.65 A particle size-dependent PBPK model for zinc oxide nanoparticles (ZnO NPs) has been developed in mice in order to assess the tissue accumulation characteristics of different sizes of ZnO NPs and zinc nitrate (Zn(NO3)2).66 It was determined that the physicochemical parameters of 10 and 71 nm ZnO NPs and Zn(NO3)2 in the PBPK modeling played a predictive role in the biodistribution and accumulative levels in living organisms.66 The proposed PBPK model in which time-dependent partition coefficients and excretion or elimination rates were used, predicted the ZnO NP and Zn(NO3)2 distribution in the targeted tissues.66 Smaller sized nanoparticles, i.e. 10 nm of ZnO NPs, tended to accumulate in the body for longer periods compared to 71 nm of ZnO NPs and Zn(NO3)2.66 Hence, this study effectively developed a dynamic model that shows promising results in predicting the behavior of slowly decomposed nanoparticles.66 A multiroute PBPK model proposed for AuNPs of different sizes ranging from 1.4 to 200 nm showed that the size and the surface area of AuNPs were the primary factors affecting the rates of internalization by endocytosis/phagocytosis irrespective of the administration route.65
Nanoparticles that are introduced into the bloodstream are quickly internalized by the phagocytic cells present in organs such as the liver and spleen based on their different physiochemical properties such as size, charge, shape, surface structure, coating, and aggregation status.67 Since the most important transportation method for many intravenously administered nanoparticles is regarded as the uptake by the MPS organs such as the liver, spleen, kidneys, lungs, and lymph nodes, more accurate results in pharmacokinetic studies of nanoparticles can be achieved when MPS and the lymphatic system are included in the modeling studies. A recent study developed a mathematical framework to predict whole-body nanoparticle pharmacokinetics and tumor delivery in vivo.68 The pharmacokinetics of 46, 69, 113, and 162 nm of mesoporous silica NPs was investigated following their intravenous administration to rats. In this model MPS and the lymphatic system were integrated. The size of NPs, the degradation rate, the viscosity of tumor blood, the vascular fraction within the tumor, and the porosity of tumor blood vessels were found to be prevailing factors influencing the NP kinetics within the tumor interstitial space.68 Another study investigated the biodistribution of 25 nm AuNPs capped with epigallocatechin gallate (EGCG-AuNP) and 19.62 nm AuNPs capped with curcumin Curc-AuNP via administration of intraperitoneal (IP) injection to mice by carrying out PBPK modeling including MPS and the whole lymphatic system.25 Organism-specific parameters in the model were adjusted to reflect those of rats to evaluate the possibility of interspecies extrapolation, and the PBPK model for rats was assessed using the data of citrate-capped AuNPs from the literature.25 Successful results were obtained in the prediction of organs by interspecies extrapolation to rats administered by citrate-capped AuNPs.25 NPs were strongly internalized by the liver and spleen which indicated the extravasation and phagocytosis were the primary factors contributing to NP uptake.
Another PBPK model was constructed for cerium oxide (CeO2) NPs administered intravenously to rats and incorporated the internalization of nanoparticles by phagocytic cells along with the various mechanisms for nanoparticle removal from the body.69 The model sufficiently depicted the CeO2 biokinetics, and their absorption by phagocytic cells was found a key factor for nanoparticle biokinetics. The results demonstrated that the kinetics of CeO2 nanoparticles varied among the tissues in different organs, and CeO2 accumulation was primarily observed in liver and spleen. Sensitivity analyses revealed that the partition coefficient between the blood and tissue, the permeability coefficient between capillary blood and tissues, the maximum rate of phagocytic cells, and the maximum capacity for internalization in individual phagocytic cells were the most significant parameters that affect the nanoparticle biokinetics.
One of the limitations in the PBPK modeling of nanoparticles is that the composed model is valid for only that nanoparticle because of the specific physicochemical properties of the nanoparticles and change in parameters such as permeability and macrophage uptake rate according to the type of the nanoparticle.2 The investigations in the disposition of the nanoparticle-drug systems have been challenging due to the complexity of their structure and function, and their different characteristics such as size, shape, composition, charge, and surface functionalization which influence the interactions with the biological systems.4 This limitation may be overcome by carrying out reparametrization in PBPK modeling of nanoparticles.2 As a result, the systematic development of nanoparticle-drug PBPK modeling in a uniting manner is significant and should take the physiological properties, major parameters, and model compartments into account (Figure 4). Since there have been substantial differences in the structure of small molecule drugs and the nanoparticles, some variations arise in the development of PBPK for nanoparticles compared to small molecules. Table 6 presents a brief summary on the differences between PBPK modeling of small molecules and nanoparticles.
Table 6. Comparison between the PBPK Modeling of Small Molecules and Nanoparticles.
| small molecules | nanoparticles | |
|---|---|---|
| Modeled molecules | Active ingredient and/or metabolite (s) | Nanoparticle or nanoparticle-drug hybrid system and released drug |
| Model development | Perfusion (flow)-limited models are more suitable.3 | Permeability (diffusion)-limited models are more suitable.3 |
| Preferred modeling software | Simcyp Simulator, GastroPlus, PKSim/MoBi62 | MATLAB/SimBiology, Berkeley Madonna, The R Language, acslX, BioUML, PKSim/MoBi62 |
| Absorption and uptake by cells | Diffusion and/or active transport by transporters12 | Paracellular transport,12 transcytosis,12 M cell uptake,12 macrophage uptake and diffusion,12 lymphatic uptake,12 internalization by phagocytic cells (PCs) by endocytosis/phagocytosis67 |
| Biodistribution | Distribute into tissues based on membrane permeability by passive diffusion and active transport via membrane transporters at the blood-to-organ or organ-to-excretion interfaces98 | Encounter mononuclear phagocyte system (MPS) in the circulatory system that is involved in the biodistribution,3 opsonization,12 target-mediated disposition,12 EPR effect,12 lymphatic transport12 |
| Metabolism | CYP enzymes and non-CYP enzymes12 | Extracellular degradation, endocytosis, phagocytosis12 |
| Commonly metabolized in the hepatocytes (parenchymal cells in the liver)4 | Metabolism primarily occurs in the lysosomes of the MPS4 | |
| Elimination | Mainly excreted either through hepatic metabolism (liver) or through renal/biliary excretion99 | Liver and kidney are the organs that are primarily responsible for excretion.3 |
| Slower or very limited renal excretion compared to small molecules due to the larger size.4 | ||
| Protein binding | Binds to plasma proteins after the absorption into systemic circulation | Protein-corona formation on their surface50 |
| Extrapolation | Traditional route-to-route extrapolation approaches of PBPK models65 | Route-specific approach of PBPK models65 |
| Allometric scaling | Applicable | Difficult to apply because of nonlinear or dose-independent disposition and pharmacokinetic profiles41 |
| Tumor accumulation | Can penetrate normal tissues freely and have no selectivity toward tumor cells4 | Improved tumor accumulation and tumor selectivity by enhanced permeation and retention (EPR) effect compared to small molecules4 |
Physiologically Based Toxicokinetic (PBTK) Modeling and Risk Assessment
Toxicokinetics is essential in evaluating the health risks associated with xenobiotics by integrating the principles and approaches in pharmacokinetics and toxicology.70 Physiologically Based Toxicokinetic (PBTK) models provide a more comprehensive approach in identifying the chemical concentrations in specific organs or tissues compared to the classical compartmental models.70 PBTK models serve as valuable tools for extrapolating data and providing a theoretical foundation for health risk assessment and management.70 The internal kinetics of nine chemicals (three endocrine disrupters, three liver steatosis inducers, and three developmental toxicants) were anticipated by using PBTK modeling in data-rich and data-poor conditions, and higher degrees of parametrization complexity were applied.71 The results revealed that the parametrization significantly influences the outputs of the model since it can alter the prioritization of chemicals based on internal concentration factors.71 A Physiologically Based Toxicokinetic and Toxicodynamic (PBTK-TD) model constructed for the prediction of accumulation and toxicity of Cd and Pb after exposure to zebrafish revealed that the uptake, distribution, and disposition kinetics of Cd and Pb in zebrafish was anticipated accurately.72 The toxicodynamic (TD) submodel studies demonstrated that the concentrations of metal in the gill can be a more appropriate indicator of the toxic effect for Cd and Pb than the whole body or other organs. The PBTK-TD model quantitatively predicted the metal toxicity and revealed primary processes by which the uptake and disposition of metals in zebrafish were controlled.
PBPK modeling approaches have been used for the risk assessment of nanoparticles. A PBPK model was developed for 99mtechnetium-labeled carbon nanoparticles (Technegas) following its administration to humans by inhalation.73 This PBPK model, which used imaging data to explain the absorption and distribution of nanoparticles, provided a reasonable explanation on the inhalation and distribution of Techngas in humans using Bayesian and MCMC techniques.73 To carry out an integrated and probabilistic risk assessment, a PBPK model was developed for AuNPs administered to humans intravenously.74 Cell viability assays were used to identify the dose–response relationships in different human cell types. Internal concentrations of AuNPs in the liver, kidney, skin, and venous plasma were quantified by a human PBPK model that was thoroughly validated previously.74 Bayesian-based probabilistic risk assessment technique integrated with Monte Carlo simulation was used to depict the probable fractions of human cell death. External exposure levels for AuNPs which induced minimum toxicity were predicted by IVIVE approaches and interspecies extrapolation techniques. The intravenously administered AuNPs at different dosages, determined by allometric scaling or nonscaled values used in rodent studies, possibly exert none to mild nanotoxicity to humans.74 Moreover, the importance of adequately deriving human equivalent doses (HED) from doses in rodents was emphasized for future clinical and risk assessment studies.74 These types of computational approaches are significant in providing a novel understanding of the safety evaluation and toxicity estimation of nanoparticles.
By integrating physiological aspects of animals with biochemical and physicochemical data, these models offer quantitative insights that are crucial for drug development, toxicology, and personalized medicine. By incorporating the physicochemical characteristics of toxicants, PBPK models provide detailed quantitative predictions of ADME processes. This integration allows for a comprehensive understanding of how toxicants behave in biological systems, supporting risk assessments, regulatory decisions, and the design of safer chemicals and pharmaceuticals.
Simulation Tools for PBPK Modeling of Nanoparticles
For the description of in vivo transport of nanoparticles, there have been several general integration algorithms and programming languages that allow for the coding and solving of the differential equations related to the process.12 However, since nanoparticles have complex ADME processes, some of the precoded PBPK modeling tools do not provide adequate flexibility and capability to work with the complex nature of nanoparticles.
The primary used modeling and simulation tools for the PBPK modeling of the nanoparticles are Matlab-Simulink, ACSL/acslXtreme, Berkeley Madonna, and Simbiology MCSim. These software packages have been commonly used for parameter estimation and optimization processes, sensitivity analysis, simulation, and data plotting purposes. Matlab-Simulink, ACSL/acslXtreme, and Berkeley Madonna have integrated specific equation libraries, PBPK modules, and visual graphical interface into the packages. Also, there are other modeling and simulation tools such as ADAPT, Stella, and SAAM II to construct PBPK models of small molecules and therapeutic proteins; however, there is no information available for these tools to be used in the PBPK modeling of nanoparticles.12 The built-in algorithms of Simcyp and GastroPlus are not sufficient for NP complexity when working with their free versions.
Comparing the software packages commonly used for the PBPK modeling of nanoparticles in terms of strengths and their limitations, Matlab-Simulink is the most powerful tool and provides graphical representation with Simulink; however, it is expensive and requires more programming skills. ACSL/acslXtreme was also a powerful tool, mainly used in the toxicology area, the upgrading of this tool is no longer provided, and it requires more skills in programming. Berkeley Madonna offers high flexibility to the user, requires fewer skills for programming, and is not expensive and is user-friendly; however, the incorporation of the population variability is hard in this tool. Simbiology MCSim is a free simulation tool that enables one to carry out Bayesian analysis using Markov chain Monte Carlo approach; however, its drawback lies in the absence of a graphical interface.12
Model-Based Methodologies for the Advancement of Disease-Specific Delivery of Nanomaterials
The tumor microenvironment (TME) presents a challenging obstacle to attaining effective nanotherapy-mediated drug delivery to solid tumors.100 The drug molecules should overcome various barriers to show therapeutic responses in solid tumors across different physical scales.100 TME contains multiple scales such as molecular (nano-) scale (up- and down-regulation of various proteins influencing tumor growth and drug-efflux mechanisms), nano- to microscale (integrating gradients of cell nutrients and oxygen, growth factors and other factors that are crucial for cell-to-cell interaction), microscale (interactions within the acellular stroma section of the tumor), and micro to macro scale (blood supply, lymphatics, organ architecture, and other physiological processes).100 Hence the TME becomes heterogeneous regarding the solutes and nutrients (nano- to microscale) as well as the variations in pH levels and cell viability resulting from hypoxia (microscale). Hypoxia has effects on the interactions between cells at the microscale by stimulating the recruitment of immune cells to the tissue and inducing the secretion of cytokines and chemokines at the nanoscale. This heterogeneity in the TME structure strongly influences the therapeutic outcomes. For example, its complexity and three-dimensional structure cause substantial barriers to the systemically administered therapeutics including nanotherapeutics. Also, the cells in the TME including immune cells, macrophages, fibroblasts/myofibroblasts, and endothelial cells actively interface with the tumor cells in most solid tumors and influence cancer cell growth, survival, polarity, and ability to invade surrounding tissues.100 The outcomes resulting from the heterogeneity of the TME should be well understood and investigated in the research area of the disease-specific delivery of therapeutics including the nanomaterials, and the development of model-based methodologies is crucial to predict the distribution and site-specific delivery of the substances considering the heterogeneous TME.
The studies on PBPK models of cancer-specific delivery of nanomaterials through heterogeneous tumor microenvironments are very limited. One study investigated the effects of TME heterogeneity on the disposition of nonliposomal doxorubicin (NL-doxo) or polyethylene glycol tagged (PEGylated) liposomal doxorubicin (PLD) nanoparticles and the efficacy on the tumors of the breast.101 Genomically validated basal-like C3(1)-T-Antigen genetically engineered mouse model (C3-TAg) and claudin-low T11/TP53Null orthotopic syngeneic murine transplant model (T11), which represent human breast tumor subtypes, were used to analyze whether the heterogeneity of the tumor cells and the TME between breast tumor subtypes have an impact on the tumor delivery and therapeutic effects of NPs.101 NL-doxo and PLD were administered intravenously to mice after the tumor size reached a certain level. The area under the curve (AUC) values in plasma for NL-doxo and PLD encapsulated and released doxorubicin were found comparable for the two models, whereas the encapsulated and released doxorubicin AUC value in tumor for PLD was higher in C3-TAg compared to T11. T11 tumors exhibited remarkably higher expression of CC chemokine ligand (CCL) 2 and vascular endothelial growth factor (VEGF)-a, larger vascular quantity and lowered VEGF-c expression compared to C3-TAg. When the two models were compared, PLD was found more efficient than NL-doxo. The results revealed that TME and tumor cell properties in breast cancer influence the efficiency and the tumor delivery of nanoparticles.101
Attaining uniform delivery of sufficient quantities of drugs and nanoparticles to the tumors is challenging due to barriers such as antigen expression, the heterogeneous nature of the tumor environment, and its permeability.102 The distribution of the nanoparticles in solid tumors has been analyzed by developing computational approaches that investigate drug delivery restrictions stemming from the perivascular areas limiting access to the majority of distant tumor cells. A spatial model of tumor distribution was constructed to simulate the geometric arrangement of tumor vessels and the surrounding tumor cells, and the model was incorporated with a systemic pharmacokinetics model for nanoparticles.103 Doxil which is a nanodrug with liposome formulation that encapsulates the chemotherapeutic drug, doxorubicin was used as a model drug. The effects of various factors including systemic clearance of nanoparticles, tumor blood perfusion, vascular permeability of nanoparticles, diffusion coefficient and nanoparticle release constant in the tumor extracellular matrix, tumor delivery efficacy (ID%), enhanced permeability and retention (EPR) and the magnitude of heterogeneous distribution (H index) were investigated.103 The spatial distribution of nanoparticles and their free-form counterparts in the tumors were compared, where high degrees of distributional heterogeneity were obtained for both nanoparticles and free-drug counterparts.103 The diffusion coefficient of nanoparticles was determined as the most important factor in decreasing the nanoparticle H index; however, this factor was not prominent on the H index of free payloads; the most effective factor in decreasing the H index for free payloads was the payload diffusion coefficient.103 The factors that increased the free payload distribution were strongly related to the higher drug effectiveness, but the factors that enhanced nanoparticle spatial distributions did not always lead to increased antitumor effects of the administered drug.103
In the drug delivery applications of nanoparticles for tumor therapy, the penetration process is challenging due to the complex tumor microenvironments.104 A recent study aimed to design nanoparticles and to investigate their transvascular transport in two abnormal tumor microenvironments through a 2-D simulation for drug delivery purposes.104 The Computational Fluid Dynamics (CFD) approach was applied to simulate tumor vascular-interstitial models in pancreatic and hepatic tumors, and the influence of the nanoparticles on the velocity profile and pressure gradient in TME was observed.104 The findings demonstrated that the nanoparticle velocity in the blood vessels of hepatic tumors was higher compared to the pancreatic tumors because of the smaller diameter of blood vessels in pancreatic tumors.104 This result indicated faster delivery of the nanoparticles to the hepatic tumors than to the pancreatic tumors.104 Nevertheless, as benign tumors translate into malignant tumors, the diameter of the blood vessel increases, which shows faster delivery of nanoparticle-based drugs to malignant tumors compared to benign tumors.104 This study assessed the effect of different TME on the transport of therapeutic agents by carrying out simulations for both pancreatic and hepatic tumors, which have different fluid flow patterns.104
Pharmacokinetic Studies for Specialized Cases
The development of PBPK modeling to predict the pharmacokinetic properties of various drug-like compounds is highly significant for investigating and anticipating the safety of these drugs/nanoparticles under specific individual conditions, such as pregnancy and lactation, as well as assessing their safety for fetuses. Besides the determination of drug safety during drug development, the extrapolation of the administration dosage from nonpregnant subjects is also important considering the physiological changes that take place during pregnancy. The modifications of the body composition in different compartments/organs during the pregnancy influence the digestive, cardiovascular, and renal systems within the body, and this results in the altered pharmacokinetic properties of the API (active pharmaceutical ingredients).105 The excretion of the API from the body usually takes place through renal mechanisms after metabolic processes or as an unchanged drug.105 Glomerular filtration rate (GFR), fraction unbound (plasma free fraction), and kidney volume are some of the altered physiological parameters that affect the renal excretion of the drug during pregnancy.106,107 The variations in the blood flow rates, enzyme expression levels, size of tissues, plasma protein binding, glomerular filtration rates, and other parameters that are affected during the pregnancy were considered by carrying out investigations for both fetal and maternal PBPK models.105 A PBPK model was developed to predict the maternal and fetal pharmacokinetics during different stages of the pregnancy, and the model was validated by using the clinical data for the antibiotics excreted via the renal route and commonly used during the pregnancy, which are cefuroxime (CFX) and cefazolin (CZ).105
The nanomaterials can cross the placenta and reach the fetus.3,108−110 The exposure to nanoparticles in pregnancy may cause damage and fetotoxicity.111 The primary factor that leads to the nanoparticle-induced cytotoxicity is the direct translocation of nanoparticles from maternal circulation across the placental barrier into the fetus that is growing.112 The stage of embryonic or placental maturation and the nanoparticle surface functionalizations (ferritin, PEG, and citrate) affected the fetal exposure to 13 nm gold nanoparticles during murine pregnancy.111 Surface functionality also influences the transfer and accumulation of the nanoparticles in fetus.111 The size of the nanoparticles also affects the maternal-fetal transfer and fetal developmental toxicity.113 For instance, ZnO nanoparticles with small diameters (13 nm) were able to cross the intestinal and placental barrier and reached the fetus following oral administration to mice.113 13 nm ZnO nanoparticles caused fetal developmental toxicity; however, 57 nm ZnO nanoparticles and bulk nanoparticles did not cross these barriers and show toxic effects.113 Similarly, silver nanoparticles (AgNPs) with a size range of 4–20 nm were rapidly absorbed in the gastrointestinal tract following their oral administration to pregnant rats.114 The cumulative excretion values of AgNPs showed a renal excretion level of 8.25%, which was higher than the fecal excretion level of 4.77% after 24 h.114 The results showed that AgNPs accumulated within the body of pregnant rats and also transferred to the fetus which may lead to adverse effects.114 Despite numerous studies that have been conducted to investigate and predict the effects of nanoparticles on pregnant subjects, there appears to be no NP-PBPK model that has been developed for such specific cases.
Recent Advances in PBPK Modeling: Artificial Intelligence (AI)-Assisted PBPK Modeling
The prediction of input parameters such as absorption, distribution, metabolism, and excretion (ADME) parameters of new compounds can sometimes be challenging in PBPK model development. This situation raises the requirement of computational models to estimate the input parameter values; hence, integrating PBPK modeling with machine learning (ML) or artificial intelligence (AI)-based computational methods has been considered promising for this purpose. In a recent study, this approach consisted of three stages; the first one is obtaining pharmacokinetic (PK) data consisting of a concentration versus time profile and/or ADME parameters from various databases, the second step is to build ML/AI-based methods to estimate ADME parameters, and the last one is to incorporate ML/AI approaches into PBPK models for the prediction of results of PK analysis such as area under the curve (AUC) and maximum plasma concentration (Cmax), etc.115
There are several challenges that can be encountered in the application of ML/AI-based methods in PBPK modeling. One of these can be regarded as the limited number of data available in the literature, in which more data points help extend the training set by providing the existence of structural diversity of the compounds in the model, and the prediction accuracy of the model can thus be increased.115 Another limitation is that the black box nature of many ML approaches in the decision-making process makes the interpretability of the model inadequate.115 Also, although neural-ODE is a promising tool to generate time-series of PK profiles for the new compounds that have limited ADME knowledge, its application requires further research.115
One of the challenges encountered in the field of nanomedicine has been considered as the inefficient delivery of the nanoparticles to the particular target in the body where tumors are present. There are a number of PBPK models that have been developed for various types of nanoparticles that are loaded with or without cancer drugs.116 However, these studies do not use PBPK modeling methods to analyze the NP disposition in tumor-bearing animals using hundreds of disparate data sets to comprehensively investigate the major factors of NP delivery efficiency to tumors.116
A previous literature study identified 200 pharmacokinetic studies (376 data sets in total) for PBPK modeling and simulations for tumor-bearing mice intravenously administered with gold nanoparticles (AuNPs) and various inorganic and organic nanoparticles.116 The PBPK model was used to estimate the maximum delivery efficiency of the nanoparticles, and the delivery efficiency at 24 and 168 h post-IV administration of the nanoparticles for different time points, different tumor types, and different types of nanoparticles.116 However, the limitation of this model was that it was difficult to experimentally measure some critical kinetic parameters of NPs such as Hill coefficient, maximum uptake rate constant, release rate constant, and time reaching 50% maximum uptake rate in the model, and these parameters were usually obtained by fitting to in vivo experimental data.117 Hence, this method was also dependent on animal studies, and the PBPK model simulation still corresponded to one specific type of NP based on each training data set, so the model could not be efficiently extrapolated from one nanoparticle to the other type of nanoparticles.117 Another PBPK model was developed generating data from a recently published Nano-Tumor Database containing 376 data sets, and using multiple machine learning and artificial intelligence methods the prediction of the delivery efficiency of nanoparticles in tumor-bearing mice was performed.118 According to this study, the deep neural network sufficiently predicted the delivery efficiency of various nanoparticles to different tumor types, and the type of cancer was an important parameter in the deep neural network model to estimate the tumor delivery efficiency.118 Among the different physicochemical properties of nanoparticles, the zeta potential and the type of core material were found to be the most effective ones in the process of delivery efficiency.118
Recent developments in computational methods, machine learning (ML), and artificial intelligence (AI) approaches offer novel tools to resolve the issues in targeted drug delivery applications. Machine learning methods have been implemented to predict some rat and human pharmacokinetic parameters such as Cmax and AUC and concentration versus time pharmacokinetic profiles by using their chemical structure and administration dosage119,120 and were also used to estimate the ADME properties for small molecule drugs.115,121 A previous study has focused on the AI-assisted PBPK modeling via integration of an AI-based quantitative structure–activity relationship (QSAR) model with the PBPK model with the aim of simulation of the tumor-targeted delivery efficiency and biodistribution of different nanoparticles.117 The model results correlated well (R2 ≥ 0.70 for 133 out of 288 data sets) with the experimentally determined pharmacokinetic profiles of various nanoparticles in tumors following intravenous injection.117 The AI-assisted PBPK model provided an efficient screening tool to predict tumor delivery efficiency of nanoparticles based on the physicochemical properties of NPs without depending on an animal training data set.117 These types of quantitative approaches that integrate machine learning and artificial intelligence methods with PBPK modeling serve as promising studies to predict the tumor delivery efficiency and tumor disposition profile in the field of cancer nanomedicine.
Concluding Remarks and Future Aspects
Nanoparticles have been found in extensive applications across various domains, particularly in nanomedicine. Accurately determining tissue and blood dosimetry, as well as concentration profiles of nanoparticles, holds paramount importance in evaluating their safety, efficacy, and potential toxicity. There has been an emerging need for the development of novel methods to evaluate nanoparticle safety and efficacy. Moreover, interspecies and in vitro to in vivo extrapolations of toxicology and pharmacokinetics data play a pivotal role in the effective development of laboratory studies for humans and appropriate risk assessment of nanoparticles. Thus, this review article aims to consolidate the current state-of-the-art and delineate the research challenges in the field of PBPK modeling of nanoparticles. Recent advancements in computational techniques, along with the emergence of machine learning (ML) and artificial intelligence (AI) methodologies, provide innovative solutions for addressing challenges in targeted drug delivery applications. ML techniques have been utilized to forecast certain pharmacokinetic parameters in rats and humans, as well as to generate concentration versus time pharmacokinetic profiles based on chemical structure and dosage information. Some of these PBPK models are validated and show superior concurrence with the predicted and observed data. However, with further understanding of the pharmacokinetics and the biological effects of nanoparticles on humans and other species, more exact PBPK models can be developed.
Author Contributions
K.O.U. and O.O.: Conceptualization, methodology. O.O. and D.G.: formal analysis, writing- original draft. K.O.U.: Supervision, writing- review and editing.
This work was supported by the Bogazici University Research Fund project no. 19764D.
The authors declare no competing financial interest.
References
- Mystridis G. A.; Batzias G. C.; Vizirianakis I. S. Physiologically Based Pharmacokinetic Modelling and Simulation to Predict the Plasma Concentration Profile of Doxorubicin. Pharmaceutics 2022, 14, 541. 10.3390/pharmaceutics14030541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le A.-D.; Wearing H. J.; Li D. Streamlining Physiologically-Based Pharmacokinetic Model Design for Intravenous Delivery of Nanoparticle Drugs. CPT Pharmacometrics Syst. Pharmacol. 2022, 11 (4), 409–424. 10.1002/psp4.12762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utembe W.; Clewell H.; Sanabria N.; Doganis P.; Gulumian M. Current Approaches and Techniques in Physiologically Based Pharmacokinetic (PBPK) Modelling of Nanomaterials. Nanomaterials 2020, 10, 1267. 10.3390/nano10071267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan D.; He H.; Wu Y.; Fan J.; Cao Y. Physiologically Based Pharmacokinetic Modeling of Nanoparticles. J. Pharm. Sci. 2019, 108 (1), 58–72. 10.1016/j.xphs.2018.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamsi M.; Mohammadi A.; Manshadi M. K. D.; Sanati-Nezhad A. Mathematical and Computational Modeling of Nano-Engineered Drug Delivery Systems. J. Controlled Release 2019, 307, 150–165. 10.1016/j.jconrel.2019.06.014. [DOI] [PubMed] [Google Scholar]
- Afzal O.; Altamimi A. S. A.; Nadeem M. S.; Alzarea S. I.; Almalki W. H.; Tariq A.; Mubeen B.; Murtaza B. N.; Iftikhar S.; Riaz N.; Kazmi I. Nanoparticles in Drug Delivery: From History to Therapeutic Applications. Nanomaterials 2022, 12 (24), 4494. 10.3390/nano12244494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad M.; Lambe U. P.; Brar B.; Shah I.; J M.; Ranjan K.; Rao R.; Kumar S.; Mahant S.; Khurana S. K.; Iqbal H. M. N.; Dhama K.; Misri J.; Prasad G. Nanotherapeutics: An Insight into Healthcare and Multi-Dimensional Applications in Medical Sector of the Modern World. Biomed. Pharmacother. 2018, 97, 1521–1537. 10.1016/j.biopha.2017.11.026. [DOI] [PubMed] [Google Scholar]
- Yusuf A.; Almotairy A. R. Z.; Henidi H.; Alshehri O. Y.; Aldughaim M. S. Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems. Polymers (Basel). 2023, 15 (7), 1596. 10.3390/polym15071596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patra J. K.; Das G.; Fraceto L. F.; Campos E. V. R.; Rodriguez-Torres M. d. P.; Acosta-Torres L. S.; Diaz-Torres L. A.; Grillo R.; Swamy M. K.; Sharma S.; Habtemariam S.; Shin H.-S. Nano Based Drug Delivery Systems: Recent Developments and Future Prospects. J. Nanobiotechnology 2018, 16 (1), 71. 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A.; Amiji M. M. Application of Nanotechnology in Medical Diagnosis and Imaging. Curr. Opin. Biotechnol. 2022, 74, 241–246. 10.1016/j.copbio.2021.12.011. [DOI] [PubMed] [Google Scholar]
- Zazo H.; Colino C. I.; Gutiérrez-Millán C.; Cordero A. A.; Bartneck M.; Lanao J. M. Physiologically Based Pharmacokinetic (PBPK) Model of Gold Nanoparticle-Based Drug Delivery System for Stavudine Biodistribution. Pharmaceutics 2022, 14, 406. 10.3390/pharmaceutics14020406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M.; Zou P.; Tyner K.; Lee S. Physiologically Based Pharmacokinetic (PBPK) Modeling of Pharmaceutical Nanoparticles. AAPS J. 2017, 19 (1), 26–42. 10.1208/s12248-016-0010-3. [DOI] [PubMed] [Google Scholar]
- Li L.; He H.; Jiang S.; Qi J.; Lu Y.; Ding N.; Lin H.-S.; Wu W.; Xiang X. Simulation of the In Vivo Fate of Polymeric Nanoparticles Traced by Environment-Responsive Near-Infrared Dye: A Physiologically Based Pharmacokinetic Modelling Approach. Molecules 2021, 26, 1271. 10.3390/molecules26051271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Docter D.; Westmeier D.; Markiewicz M.; Stolte S.; Knauer S. K.; Stauber R. H. The Nanoparticle Biomolecule Corona: Lessons Learned - Challenge Accepted?. Chem. Soc. Rev. 2015, 44 (17), 6094–6121. 10.1039/C5CS00217F. [DOI] [PubMed] [Google Scholar]
- Wang B.; He X.; Zhang Z.; Zhao Y.; Feng W. Metabolism of Nanomaterials in Vivo: Blood Circulation and Organ Clearance. Acc. Chem. Res. 2013, 46 (3), 761–769. 10.1021/ar2003336. [DOI] [PubMed] [Google Scholar]
- Sadauskas E.; Danscher G.; Stoltenberg M.; Vogel U.; Larsen A.; Wallin H. Protracted Elimination of Gold Nanoparticles from Mouse Liver. Nanomedicine Nanotechnology, Biol. Med. 2009, 5 (2), 162–169. 10.1016/j.nano.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Lin Z.; Monteiro-Riviere N. A.; Riviere J. E. A Physiologically Based Pharmacokinetic Model for Polyethylene Glycol-Coated Gold Nanoparticles of Different Sizes in Adult Mice. Nanotoxicology 2016, 10 (2), 162–172. 10.3109/17435390.2015.1027314. [DOI] [PubMed] [Google Scholar]
- Bachler G.; von Goetz N.; Hungerbühler K. A Physiologically Based Pharmacokinetic Model for Ionic Silver and Silver Nanoparticles. Int. J. Nanomedicine 2013, 8, 3365–3382. 10.2147/IJN.S46624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankveld D. P. K.; Oomen A. G.; Krystek P.; Neigh A.; Troost - de Jong A.; Noorlander C. W.; Van Eijkeren J. C. H.; Geertsma R. E.; De Jong W. H. The Kinetics of the Tissue Distribution of Silver Nanoparticles of Different Sizes. Biomaterials 2010, 31 (32), 8350–8361. 10.1016/j.biomaterials.2010.07.045. [DOI] [PubMed] [Google Scholar]
- Durantie E.; Vanhecke D.; Rodriguez-Lorenzo L.; Delhaes F.; Balog S.; Septiadi D.; Bourquin J.; Petri-Fink A.; Rothen-Rutishauser B. Biodistribution of Single and Aggregated Gold Nanoparticles Exposed to the Human Lung Epithelial Tissue Barrier at the Air-Liquid Interface. Part. Fibre Toxicol. 2017, 14 (1), 49. 10.1186/s12989-017-0231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruinink A.; Wang J.; Wick P. Effect of Particle Agglomeration in Nanotoxicology. Arch. Toxicol. 2015, 89 (5), 659–675. 10.1007/s00204-015-1460-6. [DOI] [PubMed] [Google Scholar]
- Balasubramanian S. K.; Poh K.-W.; Ong C.-N.; Kreyling W. G.; Ong W.-Y.; Yu L. E. The Effect of Primary Particle Size on Biodistribution of Inhaled Gold Nano-Agglomerates. Biomaterials 2013, 34 (22), 5439–5452. 10.1016/j.biomaterials.2013.03.080. [DOI] [PubMed] [Google Scholar]
- Carlander U.; Moto T. P.; Desalegn A. A.; Yokel R. A.; Johanson G. Physiologically Based Pharmacokinetic Modeling of Nanoceria Systemic Distribution in Rats Suggests Dose- and Route-Dependent Biokinetics. Int. J. Nanomedicine 2018, 13, 2631–2646. 10.2147/IJN.S157210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soo Choi H.; Liu W.; Misra P.; Tanaka E.; Zimmer J. P.; Itty Ipe B.; Bawendi M. G.; Frangioni J. V. Renal Clearance of Quantum Dots. Nat. Biotechnol. 2007, 25 (10), 1165–1170. 10.1038/nbt1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aborig M.; Malik P. R. V; Nambiar S.; Chelle P.; Darko J.; Mutsaers A.; Edginton A. N.; Fleck A.; Osei E.; Wettig S. Biodistribution and Physiologically-Based Pharmacokinetic Modeling of Gold Nanoparticles in Mice with Interspecies Extrapolation. Pharmaceutics 2019, 11, 179. 10.3390/pharmaceutics11040179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alghamdi M. A.; Fallica A. N.; Virzì N.; Kesharwani P.; Pittalà V.; Greish K. The Promise of Nanotechnology in Personalized Medicine. J. Pers. Med. 2022, 12 (5), 673. 10.3390/jpm12050673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shargel L.; Yu A. B. C.. Applied Biopharmaceutics & Pharmacokinetics. In Applied Biopharmaceutics & Pharmacokinetics, 7th ed.; McGraw-Hill Education: New York, NY, 2016. [Google Scholar]
- Chen J.; Yuan M.; Madison C. A.; Eitan S.; Wang Y. Blood-Brain Barrier Crossing Using Magnetic Stimulated Nanoparticles. J. Controlled Release 2022, 345, 557–571. 10.1016/j.jconrel.2022.03.007. [DOI] [PubMed] [Google Scholar]
- Liang X.; Wang H.; Grice J. E.; Li L.; Liu X.; Xu Z. P.; Roberts M. S. Physiologically Based Pharmacokinetic Model for Long-Circulating Inorganic Nanoparticles. Nano Lett. 2016, 16 (2), 939–945. 10.1021/acs.nanolett.5b03854. [DOI] [PubMed] [Google Scholar]
- Li D.; Morishita M.; Wagner J. G.; Fatouraie M.; Wooldridge M.; Eagle W. E.; Barres J.; Carlander U.; Emond C.; Jolliet O. In Vivo Biodistribution and Physiologically Based Pharmacokinetic Modeling of Inhaled Fresh and Aged Cerium Oxide Nanoparticles in Rats. Part. Fibre Toxicol. 2015, 13 (1), 45. 10.1186/s12989-016-0156-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D.; Johanson G.; Emond C.; Carlander U.; Philbert M.; Jolliet O. Physiologically Based Pharmacokinetic Modeling of Polyethylene Glycol-Coated Polyacrylamide Nanoparticles in Rats. Nanotoxicology 2014, 8 (sup1), 128–137. 10.3109/17435390.2013.863406. [DOI] [PubMed] [Google Scholar]
- Huang Q.; Riviere J. E. The Application of Allometric Scaling Principles to Predict Pharmacokinetic Parameters across Species. Expert Opin. Drug Metab. Toxicol. 2014, 10 (9), 1241–1253. 10.1517/17425255.2014.934671. [DOI] [PubMed] [Google Scholar]
- Huh Y.; Smith D.; Feng M. Interspecies Scaling and Prediction of Human Clearance: Comparison of Small- and Macro-Molecule Drugs. Xenobiotica 2011, 41, 972–987. 10.3109/00498254.2011.598582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood I. Interspecies Scaling of Antibody-Drug Conjugates (ADC) for the Prediction of Human Clearance. Antibodies 2021, 10 (1), 1. 10.3390/antib10010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaumont K.; Gardner I.; Chapman K.; Hall M.; Rowland M. Toward an Integrated Human Clearance Prediction Strategy That Minimizes Animal Use. J. Pharm. Sci. 2011, 100 (10), 4518–4535. 10.1002/jps.22635. [DOI] [PubMed] [Google Scholar]
- Tang H.; Hussain A.; Leal M.; Mayersohn M.; Fluhler E. Interspecies Prediction of Human Drug Clearance Based on Scaling Data from One or Two Animal Species. Drug Metab. Dispos. 2007, 35 (10), 1886–1893. 10.1124/dmd.107.016188. [DOI] [PubMed] [Google Scholar]
- Mahmood I. A Single Animal Species-Based Prediction of Human Clearance and First-in-Human Dose of Monoclonal Antibodies: Beyond Monkey. Antibodies 2021, 10, 35. 10.3390/antib10030035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair A.; Jacob S. A Simple Practice Guide for Dose Conversion between Animals and Human. J. Basic Clin. Pharm. 2016, 7, 27–31. 10.4103/0976-0105.177703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair A.; Morsy M. A.; Jacob S. Dose Translation between Laboratory Animals and Human in Preclinical and Clinical Phases of Drug Development. Drug Dev. Res. 2018, 79 (8), 373–382. 10.1002/ddr.21461. [DOI] [PubMed] [Google Scholar]
- Jacob S.; Nair A.; Morsy M. Dose Conversion Between Animals and Humans: A Practical Solution. Indian J. Pharm. Educ. Res. 2022, 56, 600–607. 10.5530/ijper.56.3.108. [DOI] [Google Scholar]
- Valic M.; Zheng G. Research Tools for Extrapolating the Disposition and Pharmacokinetics of Nanomaterials from Preclinical Animals to Humans. Theranostics 2019, 9, 3365–3387. 10.7150/thno.34509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caron W.; Clewell H.; Dedrick R.; Ramanathan R.; Davis W.; Yu N.; Tonda M.; Schellens J.; Beijnen J.; Zamboni W. Allometric Scaling of Pegylated Liposomal Anticancer Drugs. J. Pharmacokinet. Pharmacodyn. 2011, 38, 653–669. 10.1007/s10928-011-9213-5. [DOI] [PubMed] [Google Scholar]
- Espié P.; Tytgat D.; Sargentini-Maier M.-L.; Poggesi I.; Watelet J.-B. Physiologically Based Pharmacokinetics (PBPK). Drug Metab. Rev. 2009, 41 (3), 391–407. 10.1080/10837450902891360. [DOI] [PubMed] [Google Scholar]
- Mahmood I.; Balian J. D. Interspecies Scaling: Predicting Pharmacokinetic Parameters of Antiepileptic Drugs in Humans from Animals with Special Emphasis on Clearance. J. Pharm. Sci. 1996, 85 (4), 411–414. 10.1021/js950400y. [DOI] [PubMed] [Google Scholar]
- Stern S. T.; Hall J. B.; Yu L. L.; Wood L. J.; Paciotti G. F.; Tamarkin L.; Long S. E.; McNeil S. E. Translational Considerations for Cancer Nanomedicine. J. Controlled Release 2010, 146 (2), 164–174. 10.1016/j.jconrel.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi G.-W.; Lee Y.-B.; Cho H.-Y. Interpretation of Non-Clinical Data for Prediction of Human Pharmacokinetic Parameters: In Vitro-In Vivo Extrapolation and Allometric Scaling. Pharmaceutics 2019, 11, 168. 10.3390/pharmaceutics11040168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goteti K.; Brassil P.; Good S.; Garner C. Estimation of Human Drug Clearance Using Multiexponential Techniques. J. Clin. Pharmacol. 2008, 48, 1226–1236. 10.1177/0091270008320369. [DOI] [PubMed] [Google Scholar]
- Zou P.; Yu Y.; Zheng N.; Yang Y.; Paholak H.; Yu L.; Sun D. Applications of Human Pharmacokinetic Prediction in First-in-Human Dose Estimation. AAPS J. 2012, 14, 262–281. 10.1208/s12248-012-9332-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wajima T.; Fukumura K.; Yano Y.; Oguma T. Prediction of Human Clearance from Animal Data and Molecular Structural Parameters Using Multivariate Regression Analysis. J. Pharm. Sci. 2002, 91 (12), 2489–2499. 10.1002/jps.10242. [DOI] [PubMed] [Google Scholar]
- Mahmoudi M.; Landry M. P.; Moore A.; Coreas R. The Protein Corona from Nanomedicine to Environmental Science. Nat. Rev. Mater. 2023, 8 (7), 422–438. 10.1038/s41578-023-00552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahneh F. D.; Scoglio C. M.; Monteiro-Riviere N. A.; Riviere J. E. Predicting the Impact of Biocorona Formation Kinetics on Interspecies Extrapolations of Nanoparticle Biodistribution Modeling. Nanomedicine 2015, 10 (1), 25–33. 10.2217/nnm.14.60. [DOI] [PubMed] [Google Scholar]
- Riviere J. E. Of Mice, Men and Nanoparticle Biocoronas: Are In Vitro to In Vivo Correlations and Interspecies Extrapolations Realistic?. Nanomedicine 2013, 8 (9), 1357–1359. 10.2217/nnm.13.129. [DOI] [PubMed] [Google Scholar]
- Jones G.; Zeng L.; Kim J. Application of Allometric Scaling to Nanochelator Pharmacokinetics. ACS Omega 2023, 8 (30), 27256–27263. 10.1021/acsomega.3c02570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines D. E.; Bell S.; Chang X.; Mansouri K.; Allen D.; Kleinstreuer N.. Application of an Accessible Interface for Pharmacokinetic Modeling and In Vitro to In Vivo Extrapolation. Front. Pharmacol. 2022, 13. 10.3389/fphar.2022.864742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang X.; Tan Y.-M.; Allen D. G.; Bell S.; Brown P. C.; Browning L.; Ceger P.; Gearhart J.; Hakkinen P. J.; Kabadi S. V.; Kleinstreuer N. C.; Lumen A.; Matheson J.; Paini A.; Pangburn H. A.; Petersen E. J.; Reinke E. N.; Ribeiro A. J. S.; Sipes N.; Sweeney L. M.; Wambaugh J. F.; Wange R.; Wetmore B. A.; Mumtaz M. IVIVE: Facilitating the Use of In Vitro Toxicity Data in Risk Assessment and Decision Making. Toxics 2022, 10, 232. 10.3390/toxics10050232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang X.; Abedini J.; Bell S.; Lee K. M. Exploring in Vitro to in Vivo Extrapolation for Exposure and Health Impacts of E-Cigarette Flavor Mixtures. Toxicol. Vitr. 2021, 72, 105090. 10.1016/j.tiv.2021.105090. [DOI] [PubMed] [Google Scholar]
- Moreau M.; Mallick P.; Smeltz M.; Haider S.; Nicolas C. I.; Pendse S. N.; Leonard J. A.; Linakis M. W.; McMullen P. D.; Clewell R. A.; Clewell H. J.; Yoon M.. Considerations for Improving Metabolism Predictions for In Vitro to In Vivo Extrapolation. Front. Toxicol. 2022, 4. 10.3389/ftox.2022.894569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamei M.; Bajot F.; Neuhoff S.; Barter Z.; Yang J.; Rostami-Hodjegan A.; Rowland-Yeo K. A Mechanistic Framework for In Vitro-In Vivo Extrapolation of Liver Membrane Transporters: Prediction of Drug-Drug Interaction Between Rosuvastatin and Cyclosporine. Clin. Pharmacokinet. 2014, 53, 73–87. 10.1007/s40262-013-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q.; Chou W.-C.; Lin Z. Integration of Toxicogenomics and Physiologically Based Pharmacokinetic Modeling in Human Health Risk Assessment of Perfluorooctane Sulfonate. Environ. Sci. Technol. 2022, 56 (6), 3623–3633. 10.1021/acs.est.1c06479. [DOI] [PubMed] [Google Scholar]
- Chen Q.; Riviere J. E.; Lin Z.. Toxicokinetics, Dose-Response, and Risk Assessment of Nanomaterials: Methodology, Challenges, and Future Perspectives. WIREs Nanomed. Nanobiotechnol. 2022, 14 ( (6), ). 10.1002/wnan.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Z.; Monteiro-Riviere N. A.; Kannan R.; Riviere J. E. A Computational Framework for Interspecies Pharmacokinetics, Exposure and Toxicity Assessment of Gold Nanoparticles. Nanomedicine 2016, 11 (2), 107–119. 10.2217/nnm.15.177. [DOI] [PubMed] [Google Scholar]
- Kutumova E. O.; Akberdin I. R.; Kiselev I. N.; Sharipov R. N.; Egorova V. S.; Syrocheva A. O.; Parodi A.; Zamyatnin A. A.; Kolpakov F. A. Physiologically Based Pharmacokinetic Modeling of Nanoparticle Biodistribution: A Review of Existing Models, Simulation Software, and Data Analysis Tools. International Journal of Molecular Sciences 2022, 23, 12560. 10.3390/ijms232012560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korzekwa K.; Radice C.; Nagar S. A Permeability- and Perfusion-based PBPK Model for Improved Prediction of Concentration-time Profiles. Clin. Transl. Sci. 2022, 15 (8), 2035–2052. 10.1111/cts.13314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson M. D.; Beard D. A. Development of Appropriate Equations for Physiologically Based Pharmacokinetic Modeling of Permeability-Limited and Flow-Limited Transport. J. Pharmacokinet. Pharmacodyn. 2011, 38 (4), 405–421. 10.1007/s10928-011-9200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou W.-C.; Cheng Y.-H.; Riviere J. E.; Monteiro-Riviere N. A.; Kreyling W. G.; Lin Z. Development of a Multi-Route Physiologically Based Pharmacokinetic (PBPK) Model for Nanomaterials: A Comparison between a Traditional versus a New Route-Specific Approach Using Gold Nanoparticles in Rats. Part. Fibre Toxicol. 2022, 19 (1), 47. 10.1186/s12989-022-00489-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.-Y.; Cheng Y.-H.; Hsieh N.-H.; Wu B.-C.; Chou W.-C.; Ho C.-C.; Chen J.-K.; Liao C.-M.; Lin P. Physiologically Based Pharmacokinetic Modeling of Zinc Oxide Nanoparticles and Zinc Nitrate in Mice. Int. J. Nanomedicine 2015, 10 (null), 6277–6292. 10.2147/IJN.S86785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haripriyaa M.; Suthindhiran K. Pharmacokinetics of Nanoparticles: Current Knowledge, Future Directions and Its Implications in Drug Delivery. Futur. J. Pharm. Sci. 2023, 9 (1), 113. 10.1186/s43094-023-00569-y. [DOI] [Google Scholar]
- Dogra P.; Butner J. D.; Ruiz Ramírez J.; Chuang Y.; Noureddine A.; Jeffrey Brinker C.; Cristini V.; Wang Z. A Mathematical Model to Predict Nanomedicine Pharmacokinetics and Tumor Delivery. Comput. Struct. Biotechnol. J. 2020, 18, 518–531. 10.1016/j.csbj.2020.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasyanova V. V.; Bazhukova I. N. Modeling of Cerium Oxide Nanoparticles Pharmacokinetics. AIP Conf. Proc. 2020, 2313 (1), 80015. 10.1063/5.0032208. [DOI] [Google Scholar]
- Chen M.; Du R.; Zhang T.; Li C.; Bao W.; Xin F.; Hou S.; Yang Q.; Chen L.; Wang Q.; Zhu A. The Application of a Physiologically Based Toxicokinetic Model in Health Risk Assessment. Toxics 2023, 11, 874. 10.3390/toxics11100874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebby C.; van der Voet H.; de Sousa G.; Rorije E.; Kumar V.; de Boer W.; Kruisselbrink J. W.; Bois F. Y.; Faniband M.; Moretto A.; Brochot C. A Generic PBTK Model Implemented in the MCRA Platform: Predictive Performance and Uses in Risk Assessment of Chemicals. Food Chem. Toxicol. 2020, 142, 111440. 10.1016/j.fct.2020.111440. [DOI] [PubMed] [Google Scholar]
- Zhang Y.; Feng J.; Gao Y.; Liu X.; Qu L.; Zhu L. Physiologically Based Toxicokinetic and Toxicodynamic (PBTK-TD) Modelling of Cd and Pb Exposure in Adult Zebrafish Danio Rerio: Accumulation and Toxicity. Environ. Pollut. 2019, 249, 959–968. 10.1016/j.envpol.2019.03.115. [DOI] [PubMed] [Google Scholar]
- Péry A. R. R.; Brochot C.; Hoet P. H. M.; Nemmar A.; Bois F. Y. Development of a Physiologically Based Kinetic Model for 99m-Technetium-Labelled Carbon Nanoparticles Inhaled by Humans. Inhal. Toxicol. 2009, 21 (13), 1099–1107. 10.3109/08958370902748542. [DOI] [PubMed] [Google Scholar]
- Cheng Y.-H.; Riviere J. E.; Monteiro-Riviere N. A.; Lin Z. Probabilistic Risk Assessment of Gold Nanoparticles after Intravenous Administration by Integrating in Vitro and in Vivo Toxicity with Physiologically Based Pharmacokinetic Modeling. Nanotoxicology 2018, 12 (5), 453–469. 10.1080/17435390.2018.1459922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J.; Zhou G.; Chen C.; Yu H.; Wang T.-C.; Ma Y.; Jia G.; Gao Y.; Li B.; Sun J.; Li Y.; Jiao F.; Zhao Y.; Chai Z. Acute Toxicity and Biodistribution of Different Sized Titanium Dioxide Particles in Mice after Oral Administration. Toxicol. Lett. 2007, 168, 176–185. 10.1016/j.toxlet.2006.12.001. [DOI] [PubMed] [Google Scholar]
- Wu J.; Liu W.; Xue C.; Zhou S.; Lan F.; Bi L.; Xu H.; Yang X.; Zeng F.-D. Toxicity and Penetration of TiO2 Nanoparticles in Hairless Mice and Porcine Skin after Subchronic Dermal Exposure. Toxicol. Lett. 2009, 191 (1), 1–8. 10.1016/j.toxlet.2009.05.020. [DOI] [PubMed] [Google Scholar]
- Bachler G.; von Goetz N.; Hungerbuhler K. Using Physiologically Based Pharmacokinetic (PBPK) Modeling for Dietary Risk Assessment of Titanium Dioxide (TiO2) Nanoparticles. Nanotoxicology 2015, 9 (3), 373–380. 10.3109/17435390.2014.940404. [DOI] [PubMed] [Google Scholar]
- Carlander U.; Li D.; Jolliet O.; Emond C.; Johanson G. Toward a General Physiologically-Based Pharmacokinetic Model for Intravenously Injected Nanoparticles. Int. J. Nanomedicine 2016, 11, 625. 10.2147/IJN.S94370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yokel R. A.; Au T. C.; MacPhail R.; Hardas S. S.; Butterfield D. A.; Sultana R.; Goodman M.; Tseng M. T.; Dan M.; Haghnazar H.; Unrine J. M.; Graham U. M.; Wu P.; Grulke E. A. Distribution, Elimination, and Biopersistence to 90 Days of a Systemically Introduced 30 Nm Ceria-Engineered Nanomaterial in Rats. Toxicol. Sci. 2012, 127 (1), 256–268. 10.1093/toxsci/kfs067. [DOI] [PubMed] [Google Scholar]
- Yokel R. A.; Tseng M. T.; Dan M.; Unrine J. M.; Graham U. M.; Wu P.; Grulke E. A. Biodistribution and Biopersistence of Ceria Engineered Nanomaterials: Size Dependence. Nanomedicine Nanotechnology, Biol. Med. 2013, 9 (3), 398–407. 10.1016/j.nano.2012.08.002. [DOI] [PubMed] [Google Scholar]
- Krishnan V.; Xu X.; Barwe S. P.; Yang X.; Czymmek K.; Waldman S. A.; Mason R. W.; Jia X.; Rajasekaran A. K. Dexamethasone-Loaded Block Copolymer Nanoparticles Induce Leukemia Cell Death and Enhance Therapeutic Efficacy: A Novel Application in Pediatric Nanomedicine. Mol. Pharmaceutics 2013, 10 (6), 2199–2210. 10.1021/mp300350e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheetz L.; Gilkey M.; Krishnan V.; Jia X.; Rajasekaran A.; Dhurjati P. Physiologically Based Pharmacokinetic Modeling of Fluorescently Labeled Block Copolymer Nanoparticles for Controlled Drug Delivery in Leukemia Therapy. CPT Pharmacometrics Syst. Pharmacol. 2015, 4, 167. 10.1002/psp4.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasubramanian S. K.; Jittiwat J.; Manikandan J.; Ong C.-N.; Yu L. E.; Ong W.-Y. Biodistribution of Gold Nanoparticles and Gene Expression Changes in the Liver and Spleen after Intravenous Administration in Rats. Biomaterials 2010, 31 (8), 2034–2042. 10.1016/j.biomaterials.2009.11.079. [DOI] [PubMed] [Google Scholar]
- Fraga S.; Brandão A.; Soares M. E.; Morais T.; Duarte J. A.; Pereira L.; Soares L.; Neves C.; Pereira E.; Bastos M. de L.; Carmo H. Short- and Long-Term Distribution and Toxicity of Gold Nanoparticles in the Rat after a Single-Dose Intravenous Administration. Nanomedicine Nanotechnology, Biol. Med. 2014, 10 (8), 1757–1766. 10.1016/j.nano.2014.06.005. [DOI] [PubMed] [Google Scholar]
- Minnema J.; Borgos S. E. F.; Liptrott N.; Vandebriel R.; Delmaar C. Physiologically Based Pharmacokinetic Modeling of Intravenously Administered Nanoformulated Substances. Drug Delivery Transl. Res. 2022, 12 (9), 2132–2144. 10.1007/s13346-022-01159-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho W.-S.; Cho M.; Jeong J.; Choi M.; Han B. S.; Shin H.-S.; Hong J.; Chung B. H.; Jeong J.; Cho M.-H. Size-Dependent Tissue Kinetics of PEG-Coated Gold Nanoparticles. Toxicol. Appl. Pharmacol. 2010, 245 (1), 116–123. 10.1016/j.taap.2010.02.013. [DOI] [PubMed] [Google Scholar]
- Dogra P.; Adolphi N. L.; Wang Z.; Lin Y.-S.; Butler K. S.; Durfee P. N.; Croissant J. G.; Noureddine A.; Coker E. N.; Bearer E. L.; Cristini V.; Brinker C. J. Establishing the Effects of Mesoporous Silica Nanoparticle Properties on in Vivo Disposition Using Imaging-Based Pharmacokinetics. Nat. Commun. 2018, 9 (1), 4551. 10.1038/s41467-018-06730-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnema J.; Vandebriel R. J.; Boer K.; Klerx W.; De Jong W. H.; Delmaar C. J. E. Physiologically-Based Kinetic Modeling of Intravenously Administered Gold (Au) Nanoparticles. Small 2023, 19 (21), 2207326. 10.1002/smll.202207326. [DOI] [PubMed] [Google Scholar]
- Kozics K.; Sramkova M.; Kopecka K.; Begerova P.; Manova A.; Krivosikova Z.; Sevcikova Z.; Liskova A.; Rollerova E.; Dubaj T.; Puntes V.; Wsolova L.; Simon P.; Tulinska J.; Gabelova A. Pharmacokinetics, Biodistribution, and Biosafety of PEGylated Gold Nanoparticles In Vivo. Nanomaterials 2021, 11, 1702. 10.3390/nano11071702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubaj T.; Kozics K.; Sramkova M.; Manova A.; Bastús N. G.; Moriones O. H.; Kohl Y.; Dusinska M.; Runden-Pran E.; Puntes V.; Nelson A.; Gabelova A.; Simon P. Pharmacokinetics of PEGylated Gold Nanoparticles: In Vitro—In Vivo Correlation. Nanomaterials 2022, 12, 511. 10.3390/nano12030511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrique Silva A.; Lima Jr E.; Vasquez Mansilla M.; Zysler R. D.; Mojica Pisciotti M. L.; Locatelli C.; Kumar Reddy Rajoli R.; Owen A.; Creczynski-Pasa T. B.; Siccardi M.. A Physiologically Based Pharmacokinetic Model to Predict the Superparamagnetic Iron Oxide Nanoparticles (SPIONs) Accumulation in Vivo. Eur. J. Nanomedicine 2017, 9. 10.1515/ejnm-2017-0001. [DOI] [Google Scholar]
- Su Y.; Peng F.; Jiang Z.; Zhong Y.; Lu Y.; Jiang X.; Huang Q.; Fan C.; Lee S.-T.; He Y. In Vivo Distribution, Pharmacokinetics, and Toxicity of Aqueous Synthesized Cadmium-Containing Quantum Dots. Biomaterials 2011, 32 (25), 5855–5862. 10.1016/j.biomaterials.2011.04.063. [DOI] [PubMed] [Google Scholar]
- Lin P.; Chen J.-W.; Chang L. W.; Wu J.-P.; Redding L.; Chang H.; Yeh T.-K.; Yang C. S.; Tsai M.-H.; Wang H.-J.; Kuo Y.-C.; Yang R. S. H. Computational and Ultrastructural Toxicology of a Nanoparticle, Quantum Dot 705, in Mice. Environ. Sci. Technol. 2008, 42 (16), 6264–6270. 10.1021/es800254a. [DOI] [PubMed] [Google Scholar]
- Hauck T. S.; Anderson R. E.; Fischer H. C.; Newbigging S.; Chan W. C. W. In Vivo Quantum-Dot Toxicity Assessment. Small 2010, 6 (1), 138–144. 10.1002/smll.200900626. [DOI] [PubMed] [Google Scholar]
- Antsiferova A. A.; Kopaeva M. Y.; Kochkin V. N.; Kashkarov P. K. Kinetics of Silver Accumulation in Tissues of Laboratory Mice after Long-Term Oral Administration of Silver Nanoparticles. Nanomaterials 2021, 11, 3204. 10.3390/nano11123204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demin V. A.; Gmoshinsky I. V.; Demin V. F.; Anciferova A. A.; Buzulukov Y. P.; Khotimchenko S. A.; Tutelyan V. A. Modeling Interorgan Distribution and Bioaccumulation of Engineered Nanoparticles (Using the Example of Silver Nanoparticles). Nanotechnologies Russ. 2015, 10 (3–4), 288–296. 10.1134/S1995078015020081. [DOI] [Google Scholar]
- Antsiferova A. A.; Loginova M. A.; Kashkarov P. K. Physiologically Based Pharmacokinetic Modelling of Accumulation Kinetics of Silver Nanoparticles in a Mammalian Organism. Nanobiotechnology Reports 2023, 18 (6), 927–935. 10.1134/S2635167623601201. [DOI] [Google Scholar]
- Cannady E.; Katyayan K.; Patel N.. Chapter 3 - ADME Principles in Small Molecule Drug Discovery and Development: An Industrial Perspective. In Haschek and Rousseaux’s Handbook of Toxicologic Pathology, 4th ed.; Haschek W. M.; Rousseaux C. G.; Wallig M. A.; Bolon B. B., Eds.; Academic Press, 2022; pp 51–76. 10.1016/B978-0-12-821044-4.00003-0. [DOI] [Google Scholar]
- Zhao L.; Ren T.; Wang D. D. Clinical Pharmacology Considerations in Biologics Development. Acta Pharmacol. Sin. 2012, 33 (11), 1339–1347. 10.1038/aps.2012.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frieboes H. B.; Raghavan S.; Godin B.. Modeling of Nanotherapy Response as a Function of the Tumor Microenvironment: Focus on Liver Metastasis. Front. Bioeng. Biotechnol. 2020, 8. 10.3389/fbioe.2020.01011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song G.; Darr D. B.; Santos C. M.; Ross M.; Valdivia A.; Jordan J. L.; Midkiff B. R.; Cohen S.; Nikolaishvili-Feinberg N.; Miller C. R.; Tarrant T. K.; Rogers A. B.; Dudley A. C.; Perou C. M.; Zamboni W. C. Effects of Tumor Microenvironment Heterogeneity on Nanoparticle Disposition and Efficacy in Breast Cancer Tumor Models. Clin. Cancer Res. 2014, 20 (23), 6083–6095. 10.1158/1078-0432.CCR-14-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari H.; Rai N.; Singh S.; Gupta P.; Verma A.; Singh A. K.; Kajal; Salvi P.; Singh S. K.; Gautam V. Recent Advances in Nanomaterials-Based Targeted Drug Delivery for Preclinical Cancer Diagnosis and Therapeutics. Bioengineering 2023, 10, 760. 10.3390/bioengineering10070760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He H.; Liu C.; Liu Y.; Liu X.; Wu Y.; Fan J.; Zhao L.; Cao Y. Mathematical Modeling of the Heterogeneous Distributions of Nanomedicines in Solid Tumors. Eur. J. Pharm. Biopharm. 2019, 142, 153–164. 10.1016/j.ejpb.2019.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shabbir F.; Mujeeb A. A.; Jawed S. F.; Khan A. H.; Shakeel C. S. Simulation of Transvascular Transport of Nanoparticles in Tumor Microenvironments for Drug Delivery Applications. Sci. Rep. 2024, 14 (1), 1764. 10.1038/s41598-024-52292-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szeto K. X.; Le Merdy M.; Dupont B.; Bolger M. B.; Lukacova V. PBPK Modeling Approach to Predict the Behavior of Drugs Cleared by Kidney in Pregnant Subjects and Fetus. AAPS J. 2021, 23 (4), 89. 10.1208/s12248-021-00603-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallmann A.; Ince I.; Meyer M.; Willmann S.; Eissing T.; Hempel G. Gestation-Specific Changes in the Anatomy and Physiology of Healthy Pregnant Women: An Extended Repository of Model Parameters for Physiologically Based Pharmacokinetic Modeling in Pregnancy. Clin. Pharmacokinet. 2017, 56, 1303–1330. 10.1007/s40262-017-0539-z. [DOI] [PubMed] [Google Scholar]
- Abduljalil K.; Furness P.; Johnson T. N.; Rostami-Hodjegan A.; Soltani H. Anatomical, Physiological and Metabolic Changes with Gestational Age during Normal Pregnancy. Clin. Pharmacokinet. 2012, 51 (6), 365–396. 10.2165/11597440-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Huang J.-P.; Hsieh P. C. H.; Chen C.-Y.; Wang T.-Y.; Chen P.-C.; Liu C.-C.; Chen C.-C.; Chen C.-P. Nanoparticles Can Cross Mouse Placenta and Induce Trophoblast Apoptosis. Placenta 2015, 36 (12), 1433–1441. 10.1016/j.placenta.2015.10.007. [DOI] [PubMed] [Google Scholar]
- Teng C.; Jiang C.; Gao S.; Liu X.; Zhai S. Fetotoxicity of Nanoparticles: Causes and Mechanisms. Nanomaterials 2021, 11, 791. 10.3390/nano11030791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bongaerts E.; Nawrot T. S.; Van Pee T.; Ameloot M.; Bové H. Translocation of (Ultra)Fine Particles and Nanoparticles across the Placenta; a Systematic Review on the Evidence of in Vitro, Ex Vivo, and in Vivo Studies. Part. Fibre Toxicol. 2020, 17 (1), 56. 10.1186/s12989-020-00386-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H.; Sun C.; Fan Z.; Tian X.; Yan L.; Du L.; Liu Y.; Chen C.; Liang X.-J.; Anderson G.; Keelan J.; Zhao Y.; Nie G. Effects of Gestational Age and Surface Modification on Materno-Fetal Transfer of Nanoparticles in Murine Pregnancy. Sci. Rep. 2012, 2, 847. 10.1038/srep00847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqi N. J.; Fatima S.; Sharma B.; Elrobh M. S.. In-Utero Neurotoxicity of Nanoparticles. In Neurotoxicity - New Advances; Sabuncuoglu S., Ed.; IntechOpen: Rijeka, 2022; Ch. 1. 10.5772/intechopen.101452. [DOI] [Google Scholar]
- Teng C.; Jia J.; Wang Z.; Sharma V. K.; Yan B. Size-Dependent Maternal-Fetal Transfer and Fetal Developmental Toxicity of ZnO Nanoparticles after Oral Exposures in Pregnant Mice. Ecotoxicol. Environ. Saf. 2019, 182, 109439. 10.1016/j.ecoenv.2019.109439. [DOI] [PubMed] [Google Scholar]
- Abdel-Halim K.; Salim E.; Abdel-Latif A.; Abu-Risha S. Tissue Distribution, Placental Transfer and Excretion of Silver Nanoparticles in Pregnant Rats after a Single Oral Dose. Environ. Anal. Heal. Toxicol. 2023, 38, e2023023 10.5620/eaht.2023023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou W.-C.; Lin Z. Machine Learning and Artificial Intelligence in Physiologically Based Pharmacokinetic Modeling. Toxicol. Sci. 2023, 191 (1), 1–14. 10.1093/toxsci/kfac101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y.-H.; He C.; Riviere J. E.; Monteiro-Riviere N. A.; Lin Z. Meta-Analysis of Nanoparticle Delivery to Tumors Using a Physiologically Based Pharmacokinetic Modeling and Simulation Approach. ACS Nano 2020, 14 (3), 3075–3095. 10.1021/acsnano.9b08142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou W.-C.; Chen Q.; Yuan L.; Cheng Y.-H.; He C.; Monteiro-Riviere N. A.; Riviere J. E.; Lin Z. An Artificial Intelligence-Assisted Physiologically-Based Pharmacokinetic Model to Predict Nanoparticle Delivery to Tumors in Mice. J. Controlled Release 2023, 361, 53–63. 10.1016/j.jconrel.2023.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Z.; Chou W.-C.; Cheng Y.-H.; He C.; Monteiro-Riviere N. A.; Riviere J. E. Predicting Nanoparticle Delivery to Tumors Using Machine Learning and Artificial Intelligence Approaches. Int. J. Nanomedicine 2022, 17, 1365–1379. 10.2147/IJN.S344208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obrezanova O.; Martinsson A.; Whitehead T.; Mahmoud S.; Bender A.; Miljković F.; Grabowski P.; Irwin B.; Oprisiu I.; Conduit G.; Segall M.; Smith G. F.; Williamson B.; Winiwarter S.; Greene N. Prediction of In Vivo Pharmacokinetic Parameters and Time-Exposure Curves in Rats Using Machine Learning from the Chemical Structure. Mol. Pharmaceutics 2022, 19 (5), 1488–1504. 10.1021/acs.molpharmaceut.2c00027. [DOI] [PubMed] [Google Scholar]
- Miljković F.; Martinsson A.; Obrezanova O.; Williamson B.; Johnson M.; Sykes A.; Bender A.; Greene N. Machine Learning Models for Human In Vivo Pharmacokinetic Parameters with In-House Validation. Mol. Pharmaceutics 2021, 18 (12), 4520–4530. 10.1021/acs.molpharmaceut.1c00718. [DOI] [PubMed] [Google Scholar]
- Lin Z.; Chou W.-C. Machine Learning and Artificial Intelligence in Toxicological Sciences. Toxicol. Sci. 2022, 189 (1), 7–19. 10.1093/toxsci/kfac075. [DOI] [PMC free article] [PubMed] [Google Scholar]