Abstract
Background
Mentally disabled children have been found to have poor oral hygiene, a greater prevalence of periodontal disease, and higher caries prevalence. Flossing is an important oral hygiene skill adjacent to toothbrushing in plaque removal than brushing alone in children. GumChucks is a novel flossing device designed to assist children with easy and proper flossing techniques. To compare the efficacy of the GumChucks flossing system and string floss (SF) for plaque removal in mentally disabled children.
Materials and methods
Participants were randomly assigned to either GumChucks or SF. At baseline, a toothbrushing and flossing demonstration was given to all the participants. Gingival index (GI) and plaque index (PI) were recorded at baseline, 1 week, and 4 weeks postusage.
Results
Overall, there was a significant reduction in GI and PI after first use with children using GumChucks compared to SF floss. After 1 week and 4 weeks of postusage, children in the GumChucks group demonstrated significantly greater improvement in GI (1.03 ± 0.60), (1.12 ± 0.66), and PI (0.97 ± 0.53), (1.10 ± 0.54) from baseline p ≤ 0.05.
Conclusion
GumChucks was an effective alternative plaque removal, with recommended caretakers’ supervision for mentally disabled children.
How to cite this article
Takle TV, Vishwakarma PY, Dodamani AS, et al. Comparative Assessment of the Efficacy of the GumChucks Flossing System and String Floss for Plaque Removal in Mentally Disabled Children: A Randomized Clinical Trial. Int J Clin Pediatr Dent 2024;17(3):255–259.
Keywords: Flossing, Gingival index, Mentally disabled children, Plaque index
Introduction
Oral health is a key indicator of well-being! Dental plaque is an invisible, sticky film composed mainly of bacteria, starches, and sugars in food. This plaque that stays on the teeth becomes harder and is the most common cause of gingivitis. Gingivitis is a type of periodontal disease characterized by inflammation of the gums. Oral health is super important for all children, especially for those children who have special healthcare needs. It's sad to see that children with disabilities or sickness don't get the right amount of oral care that they need, even though there are a lot of dental diseases floating around them!1 “According to the American Association on Mental Retardation, mental retardation is defined as a disability characterized by significant limitations, both in intellectual functioning and in adaptive behavior, as expressed in conceptual, social, and practical adaptive skills, the disability originating before the age of 18 years.”2 The following are some of the risk factors that may contribute to gingivitis in mentally disabled children. The primary cause of gingivitis in this specific group is directly related to their poor oral hygiene practices. These children's oral health behaviors are primarily influenced by those around them, including their family, parents, or caregivers. It is their responsibility to educate and instill proper hygiene skills and effective oral hygiene habits in these children.3 When making a comparison between mentally disabled children and ordinary children of the same age-group, it is observed that the former have a higher incidence of caries, more teeth that have not received treatment and have been extracted, lower levels of oral hygiene maintenance, higher rates of gingival bleeding, calculus buildup, and reduced levels of periodontal health! Most mentally retarded children start their lives with teeth and gum as strong as normal children; however, their diet, medication, physical limitation, and lack of cleaning habits all contribute to the poor oral health of these children. Children with mental disabilities obviously do not make independent decisions; they need to rely on their parents or caregivers due to limitations, including insufficient manual dexterity and coordination. It has been reported that dental treatment is the most unattended health need of disabled people.4 It has been studied that in mentally challenged children, oral hygiene methods need to be simple and modified to suit the individual situation.
There are different methods for plaque control, including mechanical plaque control methods, such as toothbrushes, flosses, and interdental brushes. Toothbrushing alone cannot completely remove plaque. Flossing is advised as an adjustment to toothbrushing for plaque control and prevention of dental caries. Flossing is a technique-sensitive process, so it is mainly performed under parent's or caregivers’ supervision for children.
In flossing “C” shape is a proper flossing technique in which floss gently passes between the teeth and against the side of the teeth. Some investigations in children demonstrated that a combination of toothbrushing and conventional flossing products did not result in significant results in plaque reduction.5 This may be due to the use and design of these flossing methods, which are challenging for children's manual dexterity.
GumChucks is a totally modified flossing system. The finger wrap system around the two handles and the design of its curved shape facilitated the proper flossing technique. GumChucks required limited manual dexterity due to its handle. In mentally disabled children flossing may be reinforced along with toothbrushing to improve oral health. So, this modified GumChucks floss can be held by mentally challenged children using conventional floss. Hence, taking into consideration this study, it was performed to test the efficiency of two different flossing techniques that is GumChucks floss and string floss (SF) for plaque removal and reduction of gingivitis among mentally disabled children.
Materials and Methods
The study was registered at CTRL trial registration. The registration number for this trial is CTRL/2022/11/047032. This study was a randomized clinical trial. Shri Sanskar Matimand Residential School, Dhule, Maharashtra, India, was randomly selected for the study.
Participants were randomly recruited from Shri Sanskar Matimand Residential School, Dhule, Maharashtra, India. The residential school was randomly selected and assessed for eligibility. The written permission was obtained from the residential school. This study was approved by the institutional review board of ACPM Dental College, Dhule, Maharashtra, India. Participants were allotted based on the inclusion criteria given as (1) cooperative participants and (2) participants for whom informed consent was obtained. Participants were not included in the study if (1) participants were on any type of medication and (2) participants who received any type of oral prophylaxis within the previous month. This study was conducted between July and September 2022. A total of 80 mentally disabled children were selected for the study. Before the start of the study, the legal guardian of all participants signed written informed consent.
A randomized clinical study comparing the efficiency of GumChucks and SF. The study design and participants’ flowchart are shown (Flowchart 1). The participants were allotted randomly into two intervention groups. At the baseline visit, all participants demonstrated accurate flossing technique and GumChucks use. Children and caregivers were also demonstrated and supervised in using both the flossing product and the correct brushing technique. Clinical parameters were the gingival index (GI) and plaque index (PI), which were taken at baseline. Out of 80 participants, GumChucks floss was demonstrated to 40 participants, and SF was demonstrated to 40 participants, and ask to continue floss daily after toothbrushing for 4 weeks. The clinical parameters GI and PI scores were taken at 1 week and 4 weeks of postuse of the floss. Calculate the mean scores of GI and PI for each child by adding the scores of all surfaces and dividing by the total number of surfaces. The scores were measured at baseline, 1 week postusage, and 4 weeks postusage for both flossing products.
Flowchart 1:
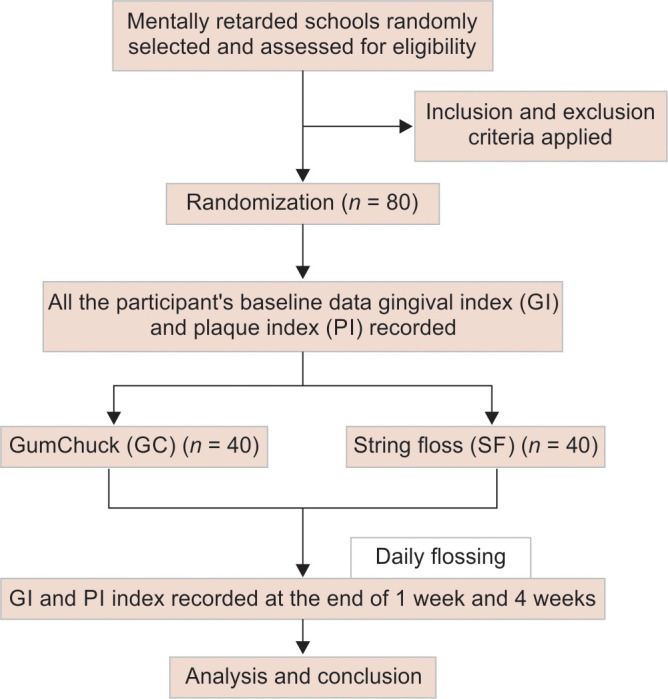
Study design and participants flowchart
Statistical Analysis
The intragroup comparison of GC and SF at baseline, 1 week, and 4 weeks was assessed by using a paired t-test. Intragroup comparison between GC and SF at baseline, 1 week, and 4 weeks was assessed by using an independent t-test. A statistically significant difference is p ≤ 0.05.
Results
The present study was conducted to compare means scores of GI and PI at baseline, 1 week, and 4 weeks of GumChucks and SF use.
The mean scores of the GI and PI of group I (participants who had used GumChucks floss) using an unpaired t-test. GI at baseline examination (1.33 ± 0.77), at the end of the 1-week significant difference, was observed (1.03 ± 0.60), and at the end of the 4-week significant difference was observed (1.12 ± 0.66) from the baseline examination but not significant compare to 1-week examination of daily flossing of the participants (Table 1).
Table 1:
A total of 80 participants compare GI and plaque scores at baseline, after 1 week, and 4 weeks postusage between GumChucks floss (group I) and SF (group II). Statistical significance was assessed using unpaired t-tests in treatment groups
| Group | No | Mean | Standard deviation | Mean difference | p-value | |
|---|---|---|---|---|---|---|
| Baseline GI | GumChucks (group I) SF (group II) |
40 40 |
1.33 1.52 |
0.77 0.73 |
0.43 | 0.51 |
| Baseline PI | GumChucks (group I) SF (group II) |
40 40 |
1.19 1.36 |
0.64 0.77 |
1.01 | 0.31 |
| 1 week GI | GumChucks (group I) SF (group II) |
40 40 |
1.03 1.45 |
0.60 0.68 |
0.19 | 0.05 |
| 1 week PI | GumChucks (group I) SF (group II) |
40 40 |
0.97 1.32 |
0.53 0.71 |
0.60 | 0.01 |
| 4 weeks GI | GumChucks (group I) SF (group II) |
40 40 |
1.12 1.52 |
0.60 0.69 |
0.42 | 0.02 |
| 4 weeks PI | GumChucks (group I) SF (group II) |
40 40 |
1.10 1.36 |
0.54 0.72 |
0.89 | 0.01 |
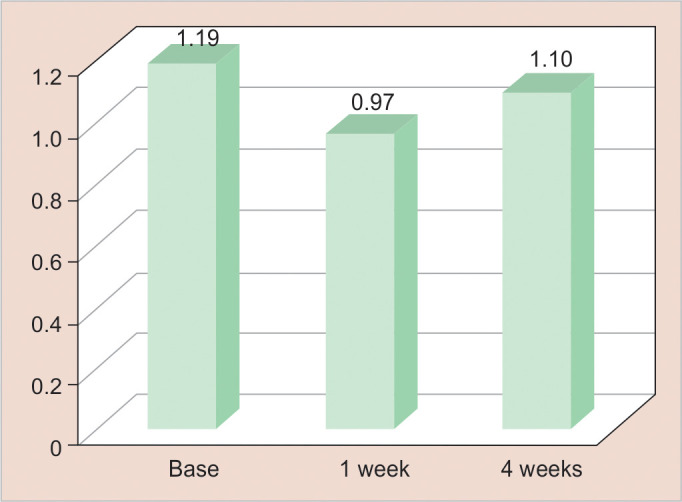
Similarly, for the PI of group I, there was a significant difference at the 1 week (0.97 ± 0.53) and at 4 weeks (1.1 ± 0.54) from the baseline examination (1.1 ± 0.64). There was a significant difference p ≤ 0.05 in the GI and PI scores from the baseline throughout the study duration for group I (Table 1).
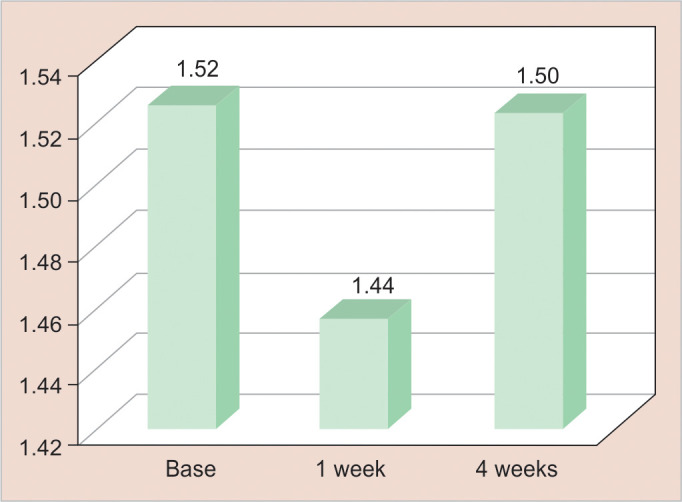
The mean scores of the GI and PI of group II (participants who had used SF) were assessed using an unpaired t-test. GI at baseline examination (1.5 ± 0.73), at the end of the 1 week's significant difference was observed (1.4 ± 0.68), and at the end of the 4-week significant difference was observed (1.5 ± 0.69) from the baseline examination, but no significant compare to 1-week examination of daily flossing of the participants (Table 1).
Similarly, for PI for group II, there was a significant difference at the 1 week (1.32 ± 0.71) and at 4 weeks (1.32 ± 0.72) from the baseline examination (1.36 ± 0.77). There was a significant difference p ≤ 0.05 in GI and PI scores from the baseline throughout the study duration (Table 1).
Intergroup group comparison between group I (participants who had used GumChucks floss) and group II (participants who had used SF) was analyzed using an independent t-test. Results show a significant difference in GI between group I (1.03 ± 0.60), (1.12 ± 0.66) at the end of the 1 week and 4 weeks compared to group II (1.45 ± 0.68), (1.52 ± 0.69) from the baseline, respectively (Table 1).
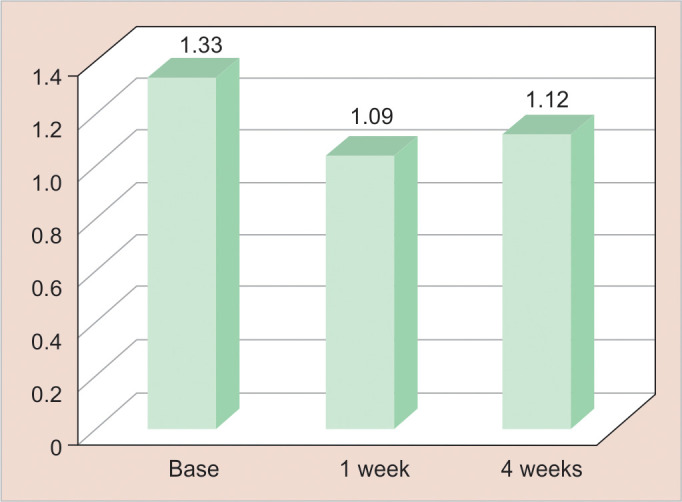
The comparison of gingival and PI scores for GumChucks floss at baseline, 1 week, and 4 weeks was shown in (Figs 1 and 2). It shows a significant reduction immediately after 1 week compared to 4 weeks. The comparison of gingival and PI scores for SF at baseline, 1 week, and 4 weeks was shown in (Figs 3 and 4). It shows a significant reduction after 1 week and 4 weeks from baseline. The comparison of gingival and PI scores for GumChucks floss and SF at baseline, 1 week, and 4 weeks was shown in (Figs 5 and 6). It shows a significant reduction in the scores that used GumChucks floss compared to SF in the participants.
Fig. 1:
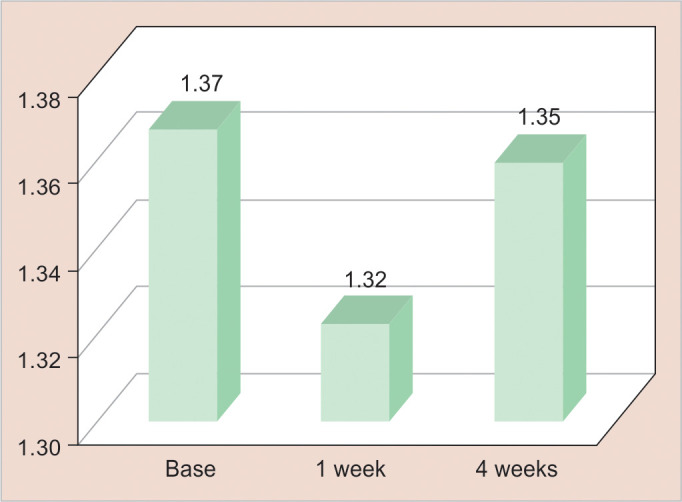
Comparison of GI scores at baseline, 1 week, and 4 weeks postusage of GumChucks floss of the total participants using paired t-test. Statistical significant at p ≤ 0.05
Fig. 2:
Comparison of PI scores baseline, 1 week, and 4 weeks of postusage of GumChucks floss of the total participants using paired t-test. Statistical significant at p ≤ 0.05
Fig. 3:
Comparison of GI at baseline, 1 week, and 4 weeks of postusage of SF of the total participants using paired t-test. Statistical significant at p ≤ 0.05
Fig. 4:
Comparison of PI at baseline, 1 week, and 4 weeks of postusage of SF of the total participants using paired t-test. Statistical significant at p ≤ 0.05
Fig. 5:
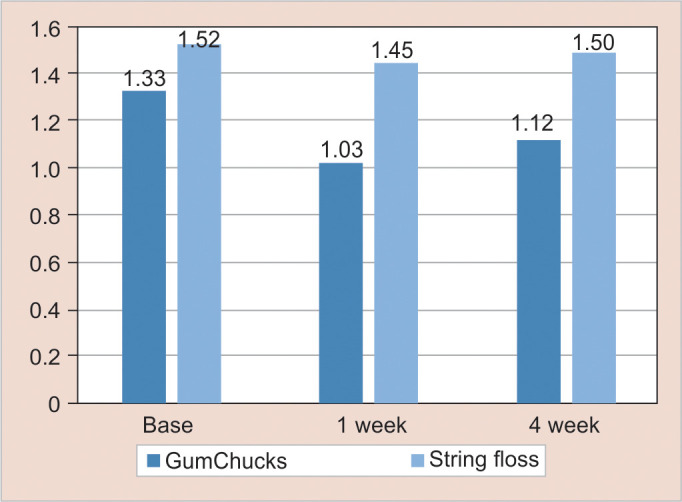
Comparison of GI scores at baseline, 1 week, and 4 weeks of postusage of GumChucks floss and SF of all the participants using independent t-test (p ≤ 0.05)
Fig. 6:
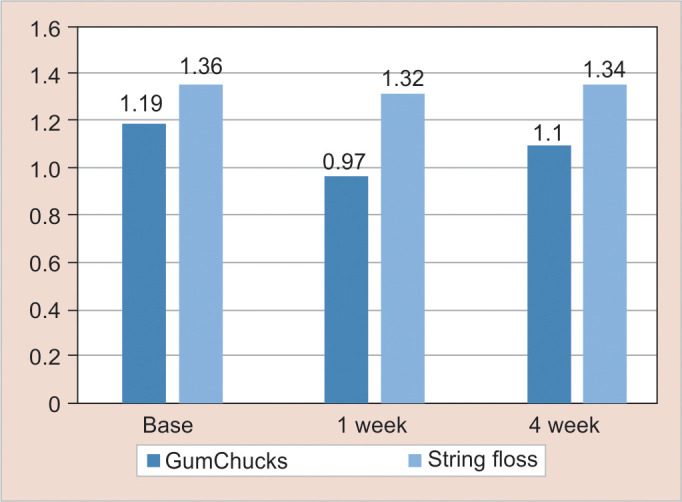
Comparison of PI scores at baseline, 1 week, and 4 weeks of postusage of GumChucks floss and SF of all the participants using independent t-test (p ≤ 0.05)
Discussion
The basic principle of preventive dentistry must be the preventive measures will have the most significant effect. Effective plaque control is essential for the successful implementation of preventive dentistry. Numerous studies have confirmed that professional prophylaxis, toothbrushes, dental floss, and various interdental devices are highly effective in eliminating interproximal plaque decreasing plaque buildup, gingival inflammation, and bleeding, ultimately resulting in enhanced gingival health. Maintenance of proper oral hygiene in handicapped individuals is known to be difficult because of psychological and physical limitations. A highly significant difference in oral hygiene habits between mentally disabled children and normal children has been observed in the studies conducted by Kumar et al. and Bennadi et al.1,4
Nicolaci and Tesini6 have observed the high frequency of poor oral hygiene among individuals with intellectual disabilities, suggesting a relationship between the level of oral care and the severity of the disability. Inadequate oral hygiene has been identified as the main cause of periodontal disease in people with disabilities. Prolonged retention of food particles in the mouth may lead to heightened gingival inflammation and, consequently, periodontal disease. Adequate knowledge and a positive mindset regarding oral health in caregivers and parents of mentally disabled children are crucial for promoting good oral health behaviors and encouraging better preventive habits related to oral health. The current research indicates that individuals with disabilities generally exhibit subpar gingival and plaque statuses. This agreed with studies conducted by Bhambal et al. and Shaw et al.7,8
Flossing is a critical component of oral care, demanding precision and presenting a challenge for youngsters. It effectively eliminates interdental plaque, acting as an early defense against dental caries and gingivitis, common problems in children's oral health. Developing this skill during childhood is vital, as it establishes lasting oral hygiene routines. This study shows that both the flossing products were effective in reducing plaque and gingivitis with regular toothbrushing, which agreed with the study conducted by Marchesan et al.9
Children with developing manual dexterity often find it difficult to master the proper flossing technique, especially with conventional floss. However, GumChucks floss offers a solution by providing a handle that gives children with limited dexterity better control. This handle also keeps the floss tight, ensuring painless and smooth entry while preventing any potential cutoff blood circulation from floss-wrapped fingertips. In a study conducted by Corby, it was discovered that toothbrushing combined with flossing was effective in reducing the microbial species linked to dental caries and periodontitis. This study involved a 2-week period and included matched twins aged between 12 and 21 years old.10
Children with mental disabilities demonstrated greater efficacy in plaque removal and reduction of gingival inflammation when utilizing GumChucks floss as opposed to traditional SF; nevertheless, GumChucks floss proved to be the superior option. Recommending proper instruction to this group of children can floss effectively using GumChucks.
The findings of this research align with a prior study carried out by Kiran et al.11 and Lin et al.,5 indicating that the utilization of GumChucks resulted in a decrease in plaque and an increase in the frequency of flossing, as opposed to conventional floss. This study shows that children prefer the usage of GumChucks floss after brushing than SF; this may be due to the fact that they easily adapted to GumChucks floss.
This study indicates that there was more reduction in gingivitis and plaque at the end of the 1 week compared to 4 weeks from the baseline. This may be due to factors like mood swings of participants, lack of continuous reinforcement, differences in self-esteem, acceptance, and understanding of the treatment
GumChucks resemble nunchucks, as they come with disposable tips containing an ¾-inch piece of dental floss. The notable decrease in PI and GI after 1 week and 4 weeks of flossing could be attributed to the unique two-handle design of GumChucks, which enhances control and dexterity. This feature allows even children with disabilities to effortlessly create a “C” shape with the floss and maintain regular flossing habits. Proper education and periodic reinforcement of GumChucks flossing in these mentally disabled children may help in improving their oral hygiene and oral hygiene habits.
Conclusion
Attitude and knowledge of oral health professionals are important while rendering oral healthcare to mentally disabled children. It was a call for attention toward these populations. GumChucks offers superior plaque removal efficacy and serves as a convenient substitute for traditional floss in helping mentally disabled children develop flossing routines and preserve their oral health. Enhancing the oral hygiene of mentally disabled children may pose challenges, but it can be accomplished through appropriate toothbrushing techniques, flossing practices, and the implementation of well-designed preventive programs. The research conducted revealed that both children and their caregivers favored GumChucks over traditional SF. GumChucks flossing is more effective than SF. It can be used for mentally disabled children after doing studies on large samples and long periods.
Strength and Limitation
The strength of the study was both the flossing system, that is, GumChucks floss and SF were efficient in reducing plaque and gingivitis in mentally disabled children. The limitation of the study was daily monitoring for flossing should have been done. This study sample did not have the same mental health intelligence quotient, which would have affected the result of the study.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Kumar S, Sharma J, Duraiswamy P, et al. Determinants for oral hygiene and periodontal status among mentally disabled children and adolescents. J Indian Soc Pedod Prevent Dent. 2009;27(3):151–157. doi: 10.4103/0970-4388.57095. [DOI] [PubMed] [Google Scholar]
- 2.Solanki J, Khetan J, Gupta S, et al. Oral rehabilitation and management of mentally retarded. J Clin Diagn Res. 2015;9(1):ZE01–ZE06. doi: 10.7860/JCDR/2015/11077.5415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu HY, Chen JR, Hsiao SY, et al. Caregivers’ oral health knowledge, attitude, and behavior toward their children with disabilities. J Dent Sci. 2017;12(4):388–389. doi: 10.1016/j.jds.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bennadi D, Konekeri V, Maurya M, et al. Oral hygiene negligence among institutionalized mentally disabled children in Mysore city—a call for attention. J Family Med Prim Care. 2020;9(4):2045–2051. doi: 10.4103/jfmpc.jfmpc_720_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin J, Dinis M, Tseng CH, et al. Effectiveness of the GumChucks flossing system compared to string floss for interdental plaque removal in children: a randomized clinical trial. Sci Rep. 2020;10(1):3052. doi: 10.1038/s41598-020-59705-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nicolaci AB, Tesini DA. Improvement in the oral hygiene of institutionalized mentally retarded individuals through training of direct care staff: a longitudinal study. Spec Care Dent. 1982;2(5):217–221. doi: 10.1111/j.1754-4505.1982.tb00059.x. [DOI] [PubMed] [Google Scholar]
- 7.Bhambal A, Jain M, Saxena S, et al. Oral health preventive protocol for mentally disabled subjects—a review. J Adv Oral Res. 2011;2(1):21–26. [Google Scholar]
- 8.Shaw L, Maclaurin ET, Foster TD. Dental study of handicapped children attending special schools in Birmingham, UK. Community Dent Oral Epidemiol. 1986;14(1):24–27. doi: 10.1111/j.1600-0528.1986.tb01488.x. [DOI] [PubMed] [Google Scholar]
- 9.Marchesan JT, Byrd KM, Moss K, et al. Flossing is associated with improved oral health in older adults. J Dent Res. 2020;99(9):1047–1053. doi: 10.1177/0022034520916151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corby PM, Biesbrock A, Bartizek R, et al. Treatment outcomes of dental flossing in twins: molecular analysis of the interproximal microflora. J Periodontal. 2008;79(8):1426–1433. doi: 10.1902/jop.2008.070585. [DOI] [PubMed] [Google Scholar]
- 11.Kiran SD, Ghiya K, Makwani D, et al. Comparison of plaque removal efficacy of a novel flossing agent with the conventional floss: a clinical study. Int J Clin Pediatr Dent. 2018;11(6):474–478. doi: 10.5005/jp-journals-10005-1560. [DOI] [PMC free article] [PubMed] [Google Scholar]


