Abstract
Background
Since no specific environmental cleaning instructions and methods have been developed for schools to tackle pandemics, and cleaning methods, this study aims to investigate the feasibility of a new effective school cleaning protocol in reducing the environmental contamination in kindergarten and primary school settings.
Methods
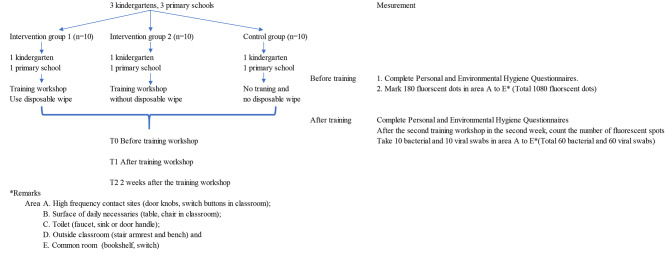
This study implemented a cluster randomized controlled trial with three-arms, namely two intervention arms - groups A and B, and one control arm – group C. The first intervention arm included the cleaning staff who would participate in an educational workshop and be equipped with disposable wipes, while the second arm, group B, participated in the educational workshop only. The third arm, group C, received no treatments.
Results
1080 sample points were collected from pre-determined sites in the study within the 6 schools. At the 2-week follow-up post-intervention assessment, all sites were found to be clean for group A that used disposable wipes, while group B, without disposable wipes, were found to have left more sites contaminated. Staphylococcus aureus was found in the sites cleaned by group C.
Conclusion
Based on the findings in this pilot study, a further study at a larger scale focusing on the education program with enhancement and use of the cleaning protocol can be conducted to train cleaning staff for effective environmental cleaning in a school setting.
Keywords: School health, Cleaning method, Disposable wipes, Cleaning staff, Fluorescent mark
Background
Non-pharmaceutical interventions, including hand hygiene and environmental cleansing, are recommended by the World Health Organization and Centers for Disease Control and Prevention (CDC) to prevent the spread of infectious diseases. Viruses such as COVID-19 virus can persist on different kind of surfaces like metal, wood, plastics, and stainless steel for a few days [1]. Studies found, e.g., influenza virus favored non-porous surfaces [2] and Staphylococcus aureus bacteria, a gram-positive, round-shaped bacterium in the respiratory tract and on the skin [3]. Cleaning with products containing soap or detergent reduces pathogens on surfaces and objects and may damage some of the pathogen particles, which decreases the risk of infection from surfaces [4]. If a contaminated surface is not cleaned properly, it may contaminate a single hand through contact with a varying degree of pathogen transfer. Contaminated hands will eventually become the source of contamination. Apart from hand hygiene, thorough cleaning and disinfection of contaminated surfaces can help break the chain of pathogen transfer in schools.
Due to non-compliance of hand hygiene, the risk from contaminated surfaces cannot be overlooked even though these practices have become increasingly a part of daily life [5]. Schools have a responsibility to provide a safe and healthy environment by implementing school health policies and practices. Infection control interventions require active collaboration among school administrators, teachers, cleaning staff, and health care professionals. COVID-19 cases during the study period in May, June, and July 2021 were 67, 82, and 61 respectively for a population of 7.4 million [6]. Children aged below 10 only accounted for less than 10% of the cases. Nonetheless, there was a peak in influenza detected (Centre for Health Protection, 2022) [7]. Moreover, laboratory studies have confirmed the ability of human influenza virus to survive in a health care setting, but few studies have attempted to investigate the presence of influenza virus, Staphylococcus aureus bacteria or other pathogens in a school setting [8]. Most studies used only self-report and observation measures, and generally lacked control-group and follow-up interventions. Therefore, this study would investigate the effectiveness of a new school cleaning protocol in reducing the environmental contamination of influenza virus and Staphylococcus aureus bacteria in kindergarten and primary school settings. A randomized, controlled pilot study was conducted.
Methods
Study design and setting
A cluster randomized controlled three-arm (2 intervention and 1 control groups) trial was implemented to assess the effectiveness of an environmental cleaning protocol in a school setting. Schools were the unit of recruitment and all cleaners within schools enrolled and consented.
The participating schools were selected according to the inclusion criterion that they had not conducted any infection control talks in the two months before the study. Schools were excluded if the schools have allowed other organization to use their school campus during weekends. The building and design of local schools have to follow the Education Regulations (Cap. 279, Sect. 84). The regular classroom size is 500–1000 ft². All participating schools have followed the general guidelines on prevention of communicable diseases in schools/kindergartens on environmental hygiene. All recruited schools used rags and buckets of water with disinfectant for cleaning and there was no training on cleaning before the study. They were then assigned randomly to the intervention Group A (new protocol and used disposable wipes), intervention Group B (new protocol with rags and buckets), and the wait-list control Group C (used the existing protocol with rags and buckets). Randomization was implemented by putting the sealed codes of schools for selection inside a paper bag. The random number sequence based on a table of random numbers, which is generated by computer. For confidentiality, computer generated numbers were used as codes to recruit 6 schools from the local kindergartens and primary schools, as clusters, to the two intervention and one control groups (Fig. 1). The schools were then drawn randomly by an individual who was not associated with the study for allocation to prevent selection and confounding biases. Single blinding was applied to the researcher that performs the assessment as well as those in charge of the statistical analyses. Thus, code identification was used for the three groups, ensuring that correspondence between codes and group characteristics (i.e. intervention or control) was not known by the aforementioned individuals. The data collection period is from 1 June 2021 to 31 September 2021. The date range for participant recruitment is from 2 April 2021 to 1 May 2021 and follow-up period from 2 May to 31 May 2021. This study did not register before enrolment of participants because researcher considered this study may not fulfill all requirements of health care research. It is confirmed that all ongoing and related trials for this intervention are registered with Registration number (ChiCTR2200066239), 29/11/2022.
Fig. 1.
Environmental swabs and fluorscent markers
Procedures
The intervention education program consisted of a Training Protocol including two 45-minute training sessions, cleaning procedures and school cleaning checklists. Training protocol involved behavior change interventions, included passive communication: lecture, demonstration cleaning procedures; active communication: discussion; group goal to clean environment effectively; response consequence: individual reward. The training protocol have designed education, feedback, reminder, commitment, incentive and reward strategies for proper cleaning method and the use of disposable wipe. The training workshop has 2 weeks program and one session per week in each school. Lecture content of the first training session: (1) what is infectious disease; (2) transmission mode of infectious disease and (3) importance of environmental cleaning. Lecture content with demonstration of the second session were: (1) cleaning skills and disinfection; (2) cleansing of cleaning tools and (3) how to use the cleaning and disinfection checklist. Discussion with scripts were held in both sessions and individual reward was given to participant with response. The same trainer used across all groups of workshops. All training content including self-made videos were put into PowerPoint and the same PowerPoint was used across workshops. Cleaning skills were used pictures to illustrate the proper direction such as from top to bottom, clean to dirty. Only intervention group A was using disposable wipes. A direct internet link on how to use the disposable wipes https://gamahealthcare.com/universal-range was used in all training workshops for intervention group A.
For group A, the cleaning staff were trained with skills to perform school cleaning according to the new protocol and use disposable detergent wipes [from A.R. Medicom Inc. (Asia) Limited] to clean their school environment. For the research team’s analysis, used detergent wipes were put into sterilized containers and collected every week from the schools by the team to assess adherence to the protocol. For group B, the cleaning staff were also trained to perform their school cleaning according to the same new protocol, but they were not provided with disposable detergent wipes to do their cleaning, they use rags and buckets. As for group C, neither workshop nor disposable wipes were provided, the cleaning staff just did their daily routines without extra support during the intervention period. The schools of group C joined the wait-list workshop, one week after all the data were collected from the two intervention groups.
Before the start of the training workshop in the first week, all cleaning staff in the schools completed 14 items “Personal and Environmental Hygiene Questionnaires” as pretest. After the training workshop in the second week, the cleaning staff in the schools completed the “Personal and Environmental Hygiene Questionnaires” as post-test. The control group will not receive any training workshops and disposable cleaning wipes. The participants in group A were required to complete the 10 items “Perception on Disposable Wipes Questionnaire at the 2-week follow-up on disposable wipes as well. Questionnaires included items such as the background information of the participants and questions on hand hygiene and cleaning knowledge and skills of the participants.
To assess the cleaning effectiveness of the cleaning staff, a school environment was divided into 5 categories (A to E) covering 10 sites as follows: (A) high-touch classroom surface (1. doorknob, 2. electrical switch); (B) classroom furniture surface (3. table, 4. chair); (C) toilet (5. faucet, 6. sink or door handle); (D) outside classroom (7. stair armrest, 8. bench), and (E) common area (9. bookshelf, 10. switch). A fluorescent marker system (Clinell evaluclean, fluorescent pen, Gama Healthcare Ltd., UK) was adopted to measure the cleanliness of the environmental surfaces. One day before each assessment, six dots were marked on each pre-determined site, at a size of 1 cm x 1 cm each. A total of 180 dots were marked in each school one day before and after the 2 weekly workshop sessions, and at the 2-week follow-up, resulting in a grand total of 1080 fluorescent dots on the designated surfaces for 6 schools. The cleaning effectiveness was assessed by the research team one day before and after the workshop and at the 2-week follow-up.
To overcome the shortcomings of the fluorescent marker system for monitoring cleaning practices as mentioned above, 10 bacterial swabs and 10 viral swabs (TransPorter) were collected from the surfaces of the 10 sites mentioned before at the 2-week follow-up after the workshop in each school [9].
Ethical approval for the study was obtained from the Human Research Ethics Committee of The Education University of Hong Kong (REF 2020-21-0278), and all participants had provided their written informed consent before the study. The participants were informed that their withdrawal at any time would not result in any negative consequences. To ensure confidentiality of research data, information that could reveal the identity of participants will be kept in confidential and entered data will be stored on a password-protected computer, only researcher and her team had access to the datasets to prevent any leakage of sensitive information. All methods were carried out in accordance with relevant guidelines and regulations.
Outcome measures
One questionnaire was used to assess the knowledge and the level of the participants’ understanding of hand hygiene and cleaning skills before and after the workshop. It was a survey with 14 questions to assess the knowledge of personal and environmental hygiene of the participants using a 5-point Likert scale ranging from “strongly disagree” to “strongly agree”. The questionnaire was validated for its content validity by a panel of 3 experts. Its test-retest reliability was confirmed by 5 school cleaning staff who were not involved in this study. The scale-level content validity index was found to be 0.88 and the content validity was established. Pearson correlation was used to measure the test-retest reliability of the questions, and the Pearson correlation coefficient was 0.75. Besides, at the 2-week follow-up only participants in group A were required to complete the “Perception on Disposable Wipes Questionnaire, a 10-question survey comparing the perception of using disposable wipes and previous disinfection methods applying a 5-point Likert scale. The range of the scale was from “strongly disagree” to “strongly agree”. Vaccination record on COVID-19 and influenza of cleaners from recruited schools were collected.
For the fluorescent marker system, checking of residual fluorescent dots was used to assess the cleaning effect on the pre-determined surfaces before, after the training workshop and at 2 weeks after the training to evaluate the effectiveness of the workshop between and within the intervention and control groups. For the assessments before and after the 2 weekly workshop sessions, and at the 2-week follow-up, the pre-marked dots on surfaces in each site from A to E (the 5 categories covering 10 sites) were checked with the findings recorded as number of dots from 0 to 6, which would be divided into three levels: (1) Removed = 0 fluorescent dot left; (2) Partial = 1–5 partial fluorescent dots left; and (3) Present = 6 full fluorescent dots left [10, 11].
To supplement the fluorescent marker system, bacterial and viral loads in the classroom environment were measured and compared between the intervention and control groups. Swabs were moistened with 1 ml viral transport medium or bacterial transport medium. A pre-moistened-only swab would be tested as a negative control. Each swab was rubbed across an area of approximately 100 cm2 in three different directions while applying even pressure [12]. All swabs were then collected by the research team and sent to a University microbiology laboratory for determining the total virus or bacteria count. Swabs of the environmental surfaces were evaluated by polymerase chain reaction (PCR) for influenza A and B, and enteroviruses for hand-foot-and-mouth disease two weeks after the training program (from June to July, 2021). The presence of viruses and the total viral colony counts on the pre-determined surfaces was compared between the intervention and control groups. Microbiology culture techniques were used to identify the bacteria (Sandora, et al., 2008). The medium used for bacterial growth and swabs was tryptic soy agar. The bacterial count was measured as the median total bacterial count in colony-forming units (CFUs) per millilitre on the pre-determined surfaces. Specific organism Staphylococcus aureus was also assessed [13].
Statistical analysis
Descriptive statistics were used to summarize the characteristics of the participating schools and cleaning staff in the intervention and control groups. Cluster-level analyses was used to compare the outcomes between clusters. ANOVA was used to test for significant differences in each of the outcome variables like cleaning effectiveness across groups A, B, and C.
Results
As regards the demographic characteristics, a total of 30 cleaning staff from six schools, including 11 from group A, 8 from group B, and 11 from group C, participated in the program with no dropouts. They aged from 31 to 56, with 19 (63.4%) older than 51. On the whole, no significant differences were found across the three groups (Table 1). Total 30 (100%) cleaning staff had taken the COVID-19 vaccination and 26 (86%) cleaning staff were vaccinated against influenza.
Table 1.
Demographic characteristics of the participants (N = 30)
| Group A count (%) (n = 11) | Group B count (%) (n = 8) | Group C count (%) (n = 11) | p value (α = 0.05) | |
|---|---|---|---|---|
| Gender | ||||
| Male | 1 (10.0) | 2 (15.0) | 0 | 0.52 |
| Female | 10 (90.0) | 6 (75.0) | 11 (100%) | |
| Age | ||||
| 35–40 | 1 (9.2) | 0 | 0 | 0.43 |
| 41–45 | 1 (9.2) | 1 (12.5) | 1 (9.2) | |
| 46–50 | 2 (18.5) | 2 (25.0) | 3 (27.1) | |
| 51–55 | 3 (26.5) | 2 (25.0) | 3 (27.1) | |
| 56 or above | 4 (36.6) | 3 (37.5) | 4 (36.6) | |
| Marital status | ||||
| Married | 10 (90.8) | 8 (100) | 10 (90.8) | 0.62 |
| Divorced | 1 (9.2) | 0 | 1 (9.2) | |
| Education | ||||
| Primary | 3 (26.5) | 2 (25) | 3 (27.2) | 0.73 |
| Secondary | 8 (73.5) | 6 (75.0) | 7 (63.6) | |
| Post-secondary | 0 | 0 | 1 (9.2) |
Personal and environmental hygiene questionnaire and perception on disposable wipes
All participants were required to complete questionnaires on personal and environmental hygiene to assess the change in their hygiene knowledge and cleaning skills before and after the training workshop, while those in group C were required to do the same as well. The findings showed that the knowledge level of the participants in groups A and B had improved after the workshops. Significant differences were found in 5 questions as follow: in Question 3 “I know the 7-steps of proper hand hygiene” with p = 0.02; Question 4 “When hands are not visibly soiled, they could be cleaned with 70–80% alcohol based handrub” with p = 0.04; Question 8 “Work from top to bottom is one of the cleaning skills” with p = 0.02; Question 9 “Work from clean to dirty is correct” with p = 0.02; Question 12 “I know when I need to wear personal protective equipment (PPE) for cleaning and disinfection work”; and Question 14 “I have been taught how to clean and disinfect the environment properly” with p = 0.03. The knowledge level of the participants in group C, however, improved significantly just in 2 questions as follows: Question 6 “Surgical mask should not be reused” and Question 7 “Contact transmission is one of the modes of transmission” with p = 0.02 and 0.01 respectively. The participating cleaning staff in group A completed the questionnaire on disposable wipes at the 2-week follow-up time. The findings showed that most of them (90.9%) agreed and strongly agreed to Question 1 “No pungent or unpleasant smell, no uncomfortable feeling”, and over 80% of them agreed to Question 6 " No need to wring out the wipe or rinse it every time. Increase work efficiency.” However, half of them (54.6%) disagreed and strongly disagreed to Question 9 “You would like to use the wipes to do the cleaning work”.
Fluorescent marker system
Of all the sites, the findings showed that the fluorescent dots on high-touch surfaces like school gates and classroom doorknobs were all removed after the training workshop only in the intervention group A. At the 2-week follow-up, the fluorescent dots were mostly removed, particularly for those outside classroom sites; group A was better than group B, followed by group C. However, the fluorescent dots on bookshelves for both the intervention and control groups were all “Present” as before, after, and at the 2-week follow-up after the program (Table 2).
Table 2.
Fluorescent dots on areas a to E
| Category | Site | Group | Pretest count (%) (n = 6) | Posttest count (%) (n = 6) | 2-week follow-up count (%) (n = 6) |
|---|---|---|---|---|---|
| A. High-touch surface | 1. School gate (e.g. gate, door handle) | A | 2 (33.3) | 0 | 2 (33.3) |
| B | 6 (100) | 0 | 6 (100) | ||
| C | 3 (50) | 0 | 1 (16.7) | ||
| 2. Classroom doorknob (front, back) | A | 2(33.3) | 1(16.7) | 0 | |
| B | 2(33.3) | 1(16.7) | 3(50) | ||
| C | 2(33.3) | 2 (33.3) | 2 (33.3) | ||
| B. Surface of daily necessaries | 3. Student desk (e.g. library, visual art room) | A | 3 (50) | 6 (100) | 3 (50) |
| B | 6 (100) | 6 (100) | 6 (100) | ||
| C | 6 (100) | 0 | 5 (83.3) | ||
| 4. Teacher desk (e.g. computer room, classroom) | A | 6 (100) | 5 (83.3) | 1 (16.7) | |
| B | 6 (100) | 6 (100) | 6 (100) | ||
| C | 5 (83.3) | 5 (83.3) | 5 (83.3) | ||
| C. Toilet | 5. Female toilet faucet | A | 6 (100) | 2 (33.3) | 0 |
| B | 4 (66.7) | 1 (16.7) | 5 (83.3) | ||
| C | 6 (100) | 0 | 5 (83.3) | ||
| 6. Male toilet compartment door handle | A | 5 (83.3) | 0 | 3 (50) | |
| B | 4 (66.7) | 4 (66.7) | 6 (100) | ||
| C | 5 (83.3) | 1 (16.7) | 3 (50) | ||
| D. Outside classroom | 7. Stair handrail, G/F to 1/F | A | 0 | 0 | 0 |
| B | 0 | 0 | 5 (83.3) | ||
| C | 3 (50) | 0 | 0 | ||
| 8. Chair (e.g. student chair, corridor bench, hall bench) | A | 0 | 0 | 0 | |
| B | 3 (50) | 3 (50) | 0 | ||
| C | 6 (100) | 3 (50) | 3 (50) | ||
| E. Common utensil | 9. Bookshelf (e.g. library) | A | 6 (100) | 6 (100) | 6 (100) |
| B | 6 (100) | 6 (100) | 6 (100) | ||
| C | 6 (100) | 6 (100) | 6 (100) | ||
| 10. Switch (e.g. staff room, hall) | A | 6 (100) | 3 | 1 (16.7) | |
| B | 3 (50) | 4 (66.7) | 6 (100) | ||
| C | 0 | 0 | 0 |
Level 1 Removed: 0 fluorescent dot left
Level 2 Partial: 1–5 partial fluorescent dots left
Level 3 Present: 6 all full fluorescent dots left
Environmental swabs
One paired bacterial and viral swab was collected from each site at the 2-week follow-up. A total of 60 paired swabs were collected. The virus count test was zero, virus could not be detected in the environment for all three groups. However, the bacteria count test showed that significantly more sites with 0 bacteria count occurred in the intervention than the control group, and the control group had significantly more bacteria count on areas such as teacher computer desks (1960 CFU/ml in group C; 216 CFU/ml in group B; 90 CFU/ml in group A); F (2, 27) = 1568.51, p < 0.01 and student chairs in the classrooms (1528 CFU/ml in control group; 1060 CFU/ml in group B; 210 CFU/ml in group A); F (2, 27) = 549.00, p < 0.01). Bacterial count was found to be insignificant on classroom doorknobs F (2, 27) = 3.20, p = 0.06. (Table 3). Additionally, Staphylococcus aureus was found on teacher computer desks and student chairs in the classrooms under group C but not under the two intervention groups.
Table 3.
Bacterial count (CFU/ml) on school environmental surfaces
| Category | Site | Group A (mean ± SD) | Group B (mean ± SD) | Group C (mean ± SD) | ANOVA F ratio | p value (α = 0.05) |
|---|---|---|---|---|---|---|
| n = 20 | n = 20 | n = 20 | ||||
| A. High-touch surfaces | 1. School gates (e.g., gate, door handles) | 1.00 ± 0.66 | 2.00 ± 2.58 | 38.4 ± 28.50 | 16.62 | < 0.01 |
| 2. Classroom doorknobs | 0.10 ± 0.01 | 0.80 ± 0.63 | 1.60 ± 2.36 | 3.20 | 0.06 | |
| B. Surfaces of daily necessaries | 3. Student desks (e.g., library, visual art room) | 77.00 ± 53.13 | 4.00 ± 4.59 | 3.60 ± 2.50 | 18.79 | < 0.01 |
| 4. Teacher desks (e.g., computer rooms, classrooms) | 9.00 ± 7.37 | 21.60 ± 12.42 | 196.00 ± 0.00 | 1568.51 | < 0.01 | |
| C. Toilets | 5. Female toilet faucets | 3.00 ± 4.83 | 200.00 ± 0.00 | 27.20 ± 29.41 | 389.77 | < 0.01 |
| 6. Male toilet compartment door handles | 28.00 ± 34.25 | 5.60 ± 2.45 | 0.01 ± 0.01 | 5.58 | 0.01 | |
| D. Outside classroom | 7. Stair handrails from G/F to 1/F | 2.00 ± 3.49 | 1.20 ± 1.47 | 6.40 ± 4.78 | 6.30 | 0.01 |
| 8. Chairs (e.g., student chairs, corridor benches, hall benches) | 21.00 ± 12.86 | 106.00 ± 0.00 | 152.80 ± 8.85 | 549.00 | < 0.01 | |
| E. Common utensils | 9. Bookshelves | 5.00 ± 4.08 | 238.40 ± 156.03 | 75.60 ± 25.78 | 17.17 | < 0.01 |
| 10. Switches in communal areas (e.g., staff room, hall) | 0.00 ± 0.00 | 4.00 ± 3.16 | 5.20 ± 1.93 | 16.19 | < 0.01 |
Discussion
In case of an outbreak of infectious diseases at schools, schools may have to be closed to prevent the rapid transmission of the diseases among the children for safety reasons. However, class suspensions will affect children’s learning and development adversely, and schools will have to spend even more time and effort on cleaning and counselling activities to children, teachers, and parents as a result. Hence, maintaining a clean school environment can help children to thrive; not just because healthy students are better learners and can attain higher academic achievement, but they will bear a lifetime of benefits for themselves and their communities [14].
The results from the questionnaires indicated that the participants showed a significant increase in their knowledge of personal and environmental hygiene after the training workshop. The results were similar to a previous study [15], in which training was found to be essential in improving the technical skills and knowledge of the cleaning staff, particularly in the learning of procedural skills. The use of the fluorescent marker system was to evaluate the physical removal and thoroughness of cleaning before and after the training workshop. The results showed that in the high-touch surfaces category, the back of the classroom doorknobs had more fluorescent dots left than at the front of the doorknobs at the inspection visits. Only group A had removed all of the fluorescent dots on the back of the doorknobs at the 2-week follow-up inspection visit. Another piece of evidence came from the toilet areas where the number of fluorescent dots significantly reduced after the training (Forrest, 2017) [16]. This was especially the case with group A where no fluorescent dots were found on the female toilet faucets at the 2-week follow-up visit.
Outside classrooms, no fluorescent dots were found on the handrails of the school staircase for all three groups. It indicated that these areas had been well attended to and had been cleaned well. The number of fluorescent dots on the bookshelves of the libraries, nevertheless, remained unchanged for all three groups before, after, and at the 2-week follow-up. This might be due to the low usage of the common areas in the libraries during the pandemic and therefore, cleaning was less frequent than the student classrooms and toilets. Besides, the bookshelves were full of books which made it difficult or impracticable to clean the surfaces there. In general, intervention group A was found to perform much better than group B and group C. It is transpired that this group did thorough and effective cleaning which could have been attributed to disposable wipes being used because fluorescent dots could be wiped with a wet surface more easily [17] as compared with reusable cloths used by groups B and C [18].
The fluorescent marker system alone is not sufficient to measure the cleaning effectiveness. This method could reveal the physical cleaning of the fluorescent dots through visualization of the dots left after cleaning using ultraviolet (UV) light. It has to be supplemented with the environmental culture swab test which is a more reliable tool to provide data on the bioburden of environmental surfaces to evaluate cleaning effectiveness [18]. Luick et al. (2013) [19] suggested that only surfaces that were totally wiped off should be considered clean. In the findings, although no fluorescent dots were found on the front of the doorknobs of the intervention and control groups, yet residual bacteria were found on the front of the doorknob surfaces of groups B and C. The fluorescent dots on chairs (e.g., corridor benches, hall benches) outside the classrooms under groups A and B were removed, whilst some fluorescent dots were found on those of group C’s. Even so, residual bacteria were present in group A’s test, and thousands were counted on areas in the tests of groups B and C. A point to note is that Staphylococcus aureus were found on the pre-determined surfaces of group C only but not those of groups A or B. Study results show no fluorescent marks on the switches of Group C schools in Table 2 and the difference among the three Groups, the 0 (zero) counts were likely to be brought by either the cleaners’ thorough cleaning or the cleaners’ presses on the switches to “on”/“off” when getting in and out of the venues after their cleaning duties. The switches with “0” counts were all considered properly cleaned in this study. This, nevertheless, did not provide information on viral or bacterial presence which was a shortcoming of the marker system. We have therefore supplemented the system with viral and bacterial swabs on the 10 sites at the 2-week follow-up. From the above observations, although the surfaces were visibly clean, residual bacteria might repopulate on these surfaces, thus the results of the fluorescent marker method did not directly correlate with the bioburden debris on the environmental surfaces, which was different from previous studies [19–21]. While virus could not be easily detected on the surfaces because virus present in low amounts [22, 23].
The above findings supported the value of disposable wipes in cleaning. Also this study tested and found that using disposable wipes with correct cleaning methods could improve environmental cleanliness. For groups B and C, the reusable cloths were washed with detergent and rinsed with water at the end of the working task to remove the remaining sodium hypochlorite solution before they were dried and stored [13]. These cloths were not changed routinely. This coupled with the fact that water was not changed frequent enough to prevent bacteria accumulation resulted in contaminated cloths.
The school cleaning staff of groups A and B had been given a new cleaning protocol and in the case of group A, a new cleaning tool - disposal wipes. The cleaning effectiveness depends very much on the compliance of the cleaning staff which was affected by their perception of the cleaning protocol and the newly introduced cleaning material. From the literature, this perception might become a barrier and could affect the cleaning staff’s cleaning effectiveness [15]. This study results show that the cleaning staff agreed to the merits of using disposable wipes in cleaning. Some cleaning staff disagreed to using wipes to do the cleaning work because they were worried about the higher long-term costs of such materials (however, these costs are borne by their school authorities). It is worthwhile for the school management to collect cleaning staff’s feedback, and provide insights for educating cleaning staff.
The training protocol describes a randomized controlled study (RCT) to test whether a new school cleaning protocol in reducing the environmental contamination of influenza virus and Staphylococcus aureus bacteria in kindergarten and primary school settings. This protocol has four key strengths. Firstly, it will be the first study that analyses the effectiveness of a school-based protocol for environmental cleaning and disinfection during a pandemic. Secondly, it will be a single-blind RCT to avoid biases. Thirdly, a new school cleaning protocol together with 2 weeks training workshop exerts a positive effect on school. Finally, the new school cleaning protocol with introducing new cleaning tool - disposal wipes.
Despite the insights described above, limitations did exist with this study. First, the educational intervention period (2 weeks) might not be sufficiently long to improve the environmental cleanliness significantly. Second, cultural swabs were only taken from the environmental surfaces, future studies can include cultural swabs taken from reusable cleaning cloths and waste water for cloth-rinsing for bacterial analyses. Third, this study did not address the barrier to environmental cleaning. Forth, this study did not account for other confounding variables such as length of time cleaners had been employed at school, student absences with respiratory illnesses during the study period. Further studies may focus on organizational and work environment factors, communication of cleaning staff as well as their soft-skills that may affect their job performance in environmental cleaning.
Conclusion
This pilot study yielded the preliminary results that a school-based environmental cleaning and disinfection protocol can be effective during a pandemic. With proper guidance, cleaning staff can use it to improve their environmental hygiene knowledge, attitude, and performance. Through suitable training, they can learn various cleaning skills and are willing to use modern hygiene products for efficient environmental cleaning and disinfection. Based on the findings in this pilot, it is feasible and worthwhile to carry out a full-scale study with enhancement of the education program and cleaning protocol to help environmental cleaning in a school setting to combat the spread of infectious diseases.
Acknowledgements
The authors would like to thank participating schools for their support and help for the pilot study.
Abbreviations
- PCR
Polymerase chain reaction
- CFUs
Colony-forming units
Author contributions
These two authors contributed equally to this work. PO was a contributor in generating the research idea, collecting data and she has analyzed and interpreted the data, as well as written and edited the manuscript. All authors have reviewed and approved the final version of the manuscript.
Funding
This study was funded through A.R. Medicom Inc. (Asia) Limited. The funder has no role in study design, data collection and analysis, or preparation of manuscript.
Data availability
Derived data supporting the findings of the study is available from the corresponding author on request.
Declarations
Ethics approval and consent to participate
The ethical approval for the study was obtained from the Human Research Ethics Committee of The Education University of Hong Kong, and participants have provided written consent before taking part in the study.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Institutes of Health. New coronavirus stable for hours on surfaces. U.S. Department of Health & Human Services; 2020 [cited 2021 January 17]. https://www.nih.gov/news-events/news-releases/new-coronavirus-stable-hours-surfaces
- 2.Dublineau A, Batéjat C, Pinon A, Burguière A, Leclercq I, Manuguerr J. Persistence of the 2009 pandemic influenza A (H1N1) virus in water and on non-porous surface. PLoS ONE. 2011;6(11):1–10. 10.1371/journal.pone.0028043 10.1371/journal.pone.0028043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sandora T, Shih M, Goldmann D. Reducing absenteeism from gastrointestinal and respiratory illness in elementary school students: a randomized, controlled trial of an infection-control intervention. Pediatr 2008 121(6); e1555-62. https://doi.10.1542/peds.2007-2597. [DOI] [PubMed]
- 4.Centers for Disease Control and Prevention. Cleaning, disinfection, and hand hygiene in schools – a toolkit for school administrators. U.S.: Centers for Disease Prevention and Control. 2021. [cited 2021 Feb 15] https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/clean-disinfect-hygiene.html
- 5.Kramer A, Schwebke I, Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect Dis. 2006;6(130):1–8. 10.1186/1471-2334-6-130 10.1186/1471-2334-6-130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hon K, Leung K, Pediatric. COVID-19: what disease is this? World J Pediatr. 2020;16:323–5.C 10.1007/s12519-020-00375-z 10.1007/s12519-020-00375-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centre for Health Protection. Epidemiology of seasonal influenza in Hong Kong and use of seasonal influenza vaccines. Hong Kong: Centre for Health Protection. 2022. [cited 2022 Sept 2] chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/ https://www.chp.gov.hk/files/pdf/epidemiology_of_seasonal_influenza_in_hong_kong_and_use_of_seasonal_influenza_vaccines_sep_2022.pdf
- 8.Willmott M, Nicholson A, Busse H, et al. Effectiveness of hand hygiene interventions in reducing illness absence among children in educational settings: a systematic review and meta-analysis. Arch Dis Child. 2015;0:1–9. 10.1136/archdischild-2015-308875 10.1136/archdischild-2015-308875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kneison L, et al. Self-monitoring by environmental services may not accurately measure thoroughness of hospital room cleaning. Infect Control Hosp Epidemiol. 2017;38(11):1371–3. 10.1017/ice.2017.205 10.1017/ice.2017.205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bender L. Key messages and actions for COVID-19 prevention and control in schools. New York: UNICEF, 2020. [cited 2021 Feb 15] file: file:///D:/Research/Infection%20control/Environmental/Medicom/Article/key-messages-and-actions-for-covid-19-prevention-and-control-in-schools-march-2020.pdf
- 11.Killingley B, Greatorex J, Digard P, et al. The environmental deposition of influenza virus from patients infected with influenza A (H1N1) pdm09: implications for infection prevention and control. J Infect Public Health. 2016;9:278–88. 10.1016/j.jiph.2015.10.009 10.1016/j.jiph.2015.10.009 [DOI] [PubMed] [Google Scholar]
- 12.Hung C, et al. Application of a fluorescent marker with quantitative bioburden methods to assess cleanliness. Infect Control Hosp Epidemiol. 2018;39:1296–300. 10.1017/ice.2018.222 10.1017/ice.2018.222 [DOI] [PubMed] [Google Scholar]
- 13.Carling P. Methods for assessing the adequacy of practice and improving room disinfection. Am J Infect Control. 2013;41:S20–5. 10.1016/j.ajic.2013.01.003 [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. About CDC Healthy Schools. U.S.: Centers Disease Prev Control, 2019. [cited 2021 Aug 5] https://www.cdc.gov/healthyschools/about.htm
- 15.Hewage S, Cao L, Jones R, Fraser A. Factors associated with environmental service worker cleaning practices in health care settings: a systematic review of the literature. Am J Infect Control. 2021;49:919–27. 10.1016/j.ajic.2021.01.001 10.1016/j.ajic.2021.01.001 [DOI] [PubMed] [Google Scholar]
- 16.Forrest H. Joining up the dots – A pilot study on the use of ultraviolet marking to identify opportunities to improve cleaning effectiveness. Oral presentation. J Infect Prevent. 2017;18(1S).
- 17.Hung I, Chang H, Cheng A, Chen A, Ting L, Chen M, Lai Y, Sheng W. Application of a fluorescent marker with quantitative bioburden methods to assess cleanliness. Infect Control Hosp Epidemiol. 2018;39:1296–300. 10.1017/ice.2018.222 10.1017/ice.2018.222 [DOI] [PubMed] [Google Scholar]
- 18.Wong S, Huang C, Yang C, Hsieh Y, Kuo C, Chen Y, Chen L. Reducing health care-associated infections by implementing separated environmental cleaning management measures by using disposable wipes of four colors. Antimicrob Resist Infect Control. 2018;734. 10.1186/s13756-018-0320-6 [DOI] [PMC free article] [PubMed]
- 19.Luick L, Thompson PA, Loock MH, Vetter SL, Cook J, Guerrero DM. Diagnostic assessment of different environmental cleaning monitoring methods. Am J Infect Control. 2013;41:751–2. 10.1016/j.ajic.2012.09.019 10.1016/j.ajic.2012.09.019 [DOI] [PubMed] [Google Scholar]
- 20.Boyce JM, Havill NL, Havill HL, Mangione E, Dumigan DG, Moore BA. Comparison of fluorescent marker systems with 2 quantitative methods of assessing terminal cleaning practices. Infect Control Hosp Epidemiol. 2011;32:1187–93. 10.1086/662626 10.1086/662626 [DOI] [PubMed] [Google Scholar]
- 21.Snyder GM, Holyoak AD, Leary KE, Sullivan BF, Davis RB, Wright SB. Effectiveness of visual inspection compared with non-microbiologic methods to determine the thoroughness of post-discharge cleaning. Antimicrob Resist Infect Control. 2013. 10.1186/2047-2994-2-26. 2,26. 10.1186/2047-2994-2-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Breshears L, Nguyen B, Robles S, Wu L, Yoon JY. Biosensor detection of airborne respiratory virus sch as SARS-Co V-2. SLAS Tech. 2022;27(1):4–17. 10.1016/j.slast.2021.12.004 10.1016/j.slast.2021.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greatorex J, Digard P, Curran M, Moynihan R, Wensley H, Wreghitt T, Varsani H, Garcia F, Enstone J, Nguyen-Van-Tam J. Survival of influenza A (H1N1) on materials found in households: implications for infection control. PLoS ONE. 2011. 10.1371/journal.pone.0027932 10.1371/journal.pone.0027932 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Derived data supporting the findings of the study is available from the corresponding author on request.