Abstract
Background
This study aimed to clarify medical-nonmedical difference on the relationship between social capital, mental health and digital health literacy of university students in China, and furtherly provide evidence-based suggestions on the improvement of the digital health literacy for the university students.
Methods
The snowball sampling method was used to collect data from the university students (including medical students and nonmedical students) through online questionnaires, and finally 1472 university students were included for the data analysis, of whom, 665 (45.18%) were medical students, 807 (54.82%) were nonmedical students; 462 (31.39%) were male, 1010 (68.61%) were female. Mean value of the age was 21.34 ± 2.33 for medical students vs. 20.96 ± 2.16 for nonmedical students. Descriptive analysis, chi-square test analysis, one-way Analysis of Variance (conducted by SPSS) and structural equation modeling (conducted by AMOS) were employed to explore the difference on the relationship between social capital, mental health and digital health literacy between the medical students and nonmedical students.
Results
The mean value of the digital health literacy was 36.27 (37.33 for medical students vs. 35.39 for nonmedical students). The SEM analysis showed that there was a statistically positive correlation between social capital and digital health literacy (stronger among the nonmedical students (0.317) than medical students (0.184)). Mental health had a statistically positive impact on the digital health literacy among medical students (0.242), but statistically significant correlation was not observed in nonmedical students (0.017). Social capital was negatively correlated with the mental health for both medical students and NMS (stronger among the nonmedical students (0.366) than medical students (0.255)). And the fitness indices of SEM were same between medical students and nonmedical students (GFI = 0.911, AGFI = 0.859, CFI = 0.922, RMSEA = 0.074).
Conclusion
The digital health literacy of the university student was relatively high. Both social capital and mental health could exert a positive effect on digital health literacy, while social capital was found to be positively associated with mental health. Statistical difference was found between medical students and nonmedical students on the above correlations. Implications were given on the improvement of the digital health literacy among university students in China.
Keywords: Digital health literacy, Social capital, Mental health, University students
Introduction
As the development of the science and technology, the number of internet users had reached 1.067 billion by the end of 2023 in China [1], which made the internet become an important and useful source of health information [2]. However, previous literature reported that up to 1/3 of the medical misinformation were prevalent on the social media account [3], leading to incorrect healthcare behaviors and treatment [4, 5], which further lead to the aggravation and higher incidence of negative health outcomes of the individual [6]. Digital health literacy (DHL) refers to the skills to search, select, evaluate, and apply online health information and healthcare related digital applications [7, 8]. The difference of DHL between individuals could affect the health related behaviors (such as exercise and diets), and contributed to health inequalities [9, 10]. Sufficient level of DHL could improve the health status by promoting access and utilization of digital health information [11]. However, the previous studies about DHL mainly focused on the medical students (MS) or hadn't clarify the difference between MS and nonmedical students (NMS) [12, 13].
Social capital was divided into cognitive (e.g. reciprocity and support) and structural components (e.g. participation and connection) [14, 15]. Many researchers had demonstrated the relationship between social capital and eHealth literacy [16]. Cui et al. clarified the direct and positive association between social capital and eHealth literacy among Chinese elderly people [17], and Stellefson et al. found a significant relationship of social support on eHealth literacy among patients living with chronic obstructive pulmonary disease [18]. Moreover, Arcury et al. also clarified the potential benefits of social support in improving low eHealth literacy [19]. However, few existed studies had explored the relationship between social capital and digital health literacy.
Mental health is a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community [20]. There is no unanimous conclusion on the relationship between mental health and eHealth literacy. Previous researches mainly showed the positive association between mental health and DHL [21]. However, the university students who had mental health problems sought health information more frequently online in Ethiopia [22], and the mental health were found to be improved by higher DHL in Vietnam [23]. There were few studies explored the impact of mental health on DHL by SEM.
Many researches demonstrated a positive relationship between social capital and mental health [24, 25], that is, individuals with lower social capital were less likely to be able to deal with psychological problems and were more likely to suffer from mental illnesses [26]. Backhaus et al. reported that students with lower social capital were at greater risk of developing symptoms of clinically relevant mental problems in 12 countries [27]. Moreover, higher social capital could lower the depression symptoms by relieving stress among multicultural adolescents in Korea [28], as well as improve the mental condition of Chinese university students [29].
Some previous studies have explored the association between mental health and DHL, social capital and DHL, social capital and mental health, yet no research has ever clarified the relationship between social capital, mental health and DHL by using (SEM) among the university students in China. Thus, this study aimed to identify the relationship and further investigate whether there was medical-nonmedical difference between social capital, mental health and DHL among the university students in China. According to the research purpose above, three hypotheses were proposed to construct the hypothetical model for this study (as shown in Fig. 1). First, it was hypothesized that DHL was positively associated with social capital in university students(H1). Second, DHL was correlated with mental health among the university students(H2). Third, mental health was positively associated with social capital in university students(H3).
Fig. 1.
Conceptual model of the association between social capital and mental health and DHL
Methods
Study participants
Sample selection
The snowball sampling method was used to collect the data via an online platform (Wenjuan.com) among the university students in China. The content of questionnaire was verified through the pilot survey by using snowball sampling among 304 university students to ensure that the questions were understandable and appropriate. A total of 1527 samples were collected online from September 20 to October 24,2022. Of these, 1472 university students were finally included for analysis, of which 665 were MS, 807 were NMS. All respondents expressed their willingness to participate and understand the background and purpose of the study.
Sample characteristics
Table 1 summarized the general demographic characteristics of university students in this study. 1472 participants were included in the data analysis, of whom 462 (31.39%) were male, 1010 (68.61%) were female. There were more female than male in both MS (219 for male and 446 for female) and NMS (243 for male and 564 for female), as well as more university students lived in the urban (1019) than in the rural areas (453). The mean value of the age was 21.34 ± 2.33 for MS vs. 20.96 ± 2.16 for NMS, showing that MS were older than NMS. In terms of average monthly household income, about 2/5 of the subjects belonged to the group of 5000–10000 RMB (570, 38.72%). Regarding the average monthly spending, about 2/3 of the participants belonged to the group of 1000–2000 RMB (970, 65.90%). In terms of health status compared to last year, about 2/5 of the participants belonged to the same health status compared to the last year. Regarding to the health status compared to peers, more than half of the participants belonged to the same health status compared to peers. The mean value of the DHL was 36.27 (37.33 for MS vs. 35.39 for NMS), showing a high level of DHL among university students.
Table 1.
Participants' descriptive characteristics
| Variable | Major | χ2 Test/ANOVA | |
|---|---|---|---|
| MS | NMS | ||
| n(%)/Mean ± SD | n(%)/Mean ± SD | ||
| Total | 665(45.18%) | 807(54.82%) | |
| Gender | |||
| Male | 219(47.40%) | 243(52.60%) |
1.347a P = 0.246 |
| Female | 446(44.16%) | 564(52.84%) | |
| Residence | |||
| Urban | 456(44.75%) | 563(55.25%) |
0.244a P = 0.622 |
| Rural | 209(46.14%) | 244(53.86%) | |
| Age | 21.34 ± 2.33 | 20.96 ± 2.16 |
10.742b P = 0.001 |
| Average Monthly Household Income (RMB) | |||
| 0–3000 | 71(43.03%) | 94(56.97%) |
0.727a P = 0.867 |
| 3000–5000 | 159(45.30%) | 192(54.70%) | |
| 5000–10000 | 264(46.32%) | 306(53.68%) | |
| > 10,000 | 171(44.30%) | 215(55.70%) | |
| Average Monthly Spending (RMB) | |||
| 0–1000 | 82(38.32%) | 132(61.68%) |
6.366a P = 0.095 |
| 1000–2000 | 458(47.22%) | 512(52.78%) | |
| 2000–5000 | 108(44.08%) | 137(55.92%) | |
| > 5000 | 17(39.53%) | 26(60.47%) | |
| Health Compared to Last Year | |||
| Much Worse | 29(35.37%) | 53(64.63%) |
14.456a P = 0.006 |
| Worse | 185(41.76%) | 258(58.24%) | |
| About Same | 320(49.92%) | 321(50.08%) | |
| Better | 102(40.64%) | 149(59.36%) | |
| Much Better | 29(52.73%) | 26(47.27%) | |
| Health Compared to Peers | |||
| Much Worse | 16(34.04%) | 31(65.96%) |
10.531a P = 0.032 |
| Worse | 129(40.19%) | 192(59.81%) | |
| About Same | 385(48.61%) | 407(51.39%) | |
| Better | 107(42.13%) | 147(57.87%) | |
| Much Better | 28(48.28%) | 30(51.72%) | |
| DHL | 37.33 ± 7.11 | 35.39 ± 7.21 |
26.807b P < 0.001 |
MS Medical students, NMS Nonmedical students, SD Standard deviation, DHL Digital health literacy
ameans χ2 Test
bmeans ANOVA
Measurements
General demographics
In this study, general demographics included gender, residence, age, major, average monthly household income, average monthly spending, health status compare to peers, and health status compare to last year. The options for hukou were urban and rural, and the major were divided into medical and nonmedical university students. Average monthly household income was divided into below 3000 RMB, 3000–5000 RMB, 5000–10000 RMB, and more than 10,000 RMB. Average monthly spending were divided in below 1000 RMB,1000–2000 RMB, 2000–5000 RMB, and more than 5000 RMB. health status compared to peers and health status compared to last year were both categorized in five classes as much worse / worse / about same / better / much better.
DHL
DHL was measured by digital health literacy assessment (DHLA), which was designed by Peggy Liu in Taiwan China [30] and tested its reliability and validity in Mainland China by Nie et al. [31]. DHL was divided into two sections, named self-rated of digital health literacy (questions 1 to 6) and trust degree of online health information (questions 7 to 10) separately. The Cronbach's α of the questionnaire was 0.923 and show the good internal consistency. The total score of DHLA is between 10 to 50, with a higher score indicating a better DHL.
Social capital
Social capital was assessed by Chinese Shortened Social Capital Scale (CSSCS) designed by Xu et al. [32], which had been validated and used widely among Chinese population [32, 33]. The CSSCS includes two subscales: structural social capital and cognitive social capital. The structural social capital includes three dimensions: social participation (questions 1, 2, 3 and 4), social support (questions 5, 6, 7 and 8), and social connection (questions 9,10 and 11); the cognitive social capital includes three dimensions: trust (questions 12, 13 and 14), cohesion (questions 15, 16, 17, 18 and 19), and reciprocity (questions 20 21 and 22). The total score of CSSCS is between 22 to 110, with a higher score shows the better social capital. Considering the social fact of the university students (having no children), the 9th questions related to children was deleted from the original scale for this study. The Cronbach's α of the questionnaire was 0.882 after the deletion of the 9th question, while the Cronbach's α of each dimension (social participation, social support, social connection, trust, cohesion, and reciprocity) were 0.882, 0.719, 0.671,0.697, 0.851 and 0.796 separately, suggesting that the scale after deleting the 9th question had good internal consistency [34, 35]. Construct validity was tested to estimate the validity of CSSCS by correlation coefficient of each item of each dimension (social participation, social support, social connection, trust, cohesion, and reciprocity) respectively. Large effect sizes were observed in all dimensions (correlation coefficient ≥ 0.50) [35], indicating the feasibility of using CSSCS among the university students in this study.
Mental health
Mental health was assessed by Chinese version of Depression Anxiety Stress Scale (DASS-21), which had been validated by Wang et al. among Chinese university students and showed high reliability and validity [36]. Three dimensions (depression, anxiety and stress) were included in DASS-21. The depression scale included questions 3, 5, 10, 16, and 17, the anxiety scale included questions 2, 4, 7,9,15, 19 and 20, and the stress scale included questions 1, 6, 8, 11, 12, 14, 18 and 21. The DASS-21 is determined using a 4-point Likert scale: 1 = never, 2 = often, 3 = sometimes, 4 = always. The total score of DASS-21 is 21–84, and the higher scores indicating worse mental health. The Cronbach's α of DASS-21 was 0.962, of which show the good internal consistency.
Statistical analysis
Descriptive statistics were used to show the general distribution of the basic demographics of the participants. The chi-square was used to compare the major difference in general demographics, and one-way Analysis of Variance (ANOVA) were used to compare the difference in social capital, mental health and DHL among MS and NMS in China. A P value < 0.05 denotes statistical significance, and all the analysis were executed using the Statistical Package for Social Science for Windows (SPSS, version 25.0, IBM, Armonk, New York, USA).
Structural Equation Modeling (SEM) was used to explore the association between the social capital, mental health and DHL of the university students in China. The maximum-likelihood estimation was used to predict the best-fitting model in the study. The SEM model consists two types of latent variables: exogenous variable and endogenous variable. The exogenous variable was social capital, and the endogenous variables were mental health and DHL. In the diagrams, regression and coefficients between variables were focused on standardized regression coefficients performed to interpret and compare. Assessment of the model fitness calculates how the theoretical model might be consistent with the empirical data. The chi-square test, goodness of fit index (GFI), adjusted goodness of fit index (AGFI), normed fit index (NFI), incremental fit index (IFI), comparative fitness index (CFI), root mean square error of approximation (RMSEA) and the Hoelter’s critical N (CN) were reported for analysis of model fitness, as in many previous studies. When sample sizes are large (as in the present study), a non-significant chi-square is rarely obtained [37–39]. GFI, AGFI, NFI, IFI, CFI, and RMSEA were instead adopted as the fitness indices in this study. The hypothetical models are regarded to be well fitted to the data when P > 0.05; GFI > 0.90, AGFI > 0.80, NFI > 0.90, IFI > 0.90,CFI > 0.90, and RMSEA < 0.08 [40, 41]. The CN values is higher than 200, indicating multi- group restriction models have the property of constancy and can be estimated across group categories [42].The change in RMSEA was used to assess the measurement invariance for the comparison of the less restricted model with the more constrained model. With a sample of more than 300, the change of CFI is less than 0.010 and the change of RMSEA (ΔRMSEA) is less than 0.015 implies that measurement invariance has been successfully established [43, 44]. The AMOS (version 28.0, IBM, Armonk, New York, USA) statistical software package for Windows was executed to measure the model's fitness indexes, and obtain the maximum-likelihood estimates of model parameters.
Ethics approval and consent to participate
The survey and data were obtained with informed consent from all participants. The Ethics Committee of Shandong University reviewed and approved this study (task no. LL20220425) and was in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Results
Structural model
Model fitness indices
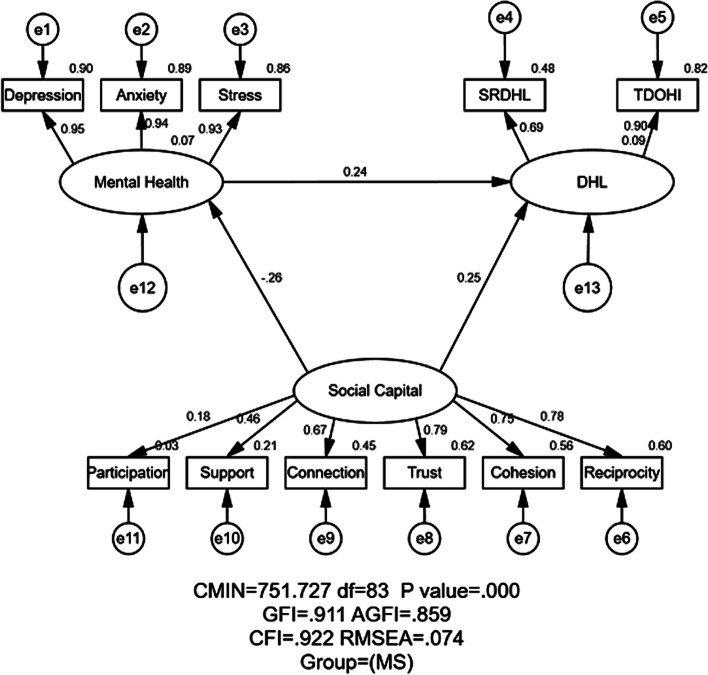
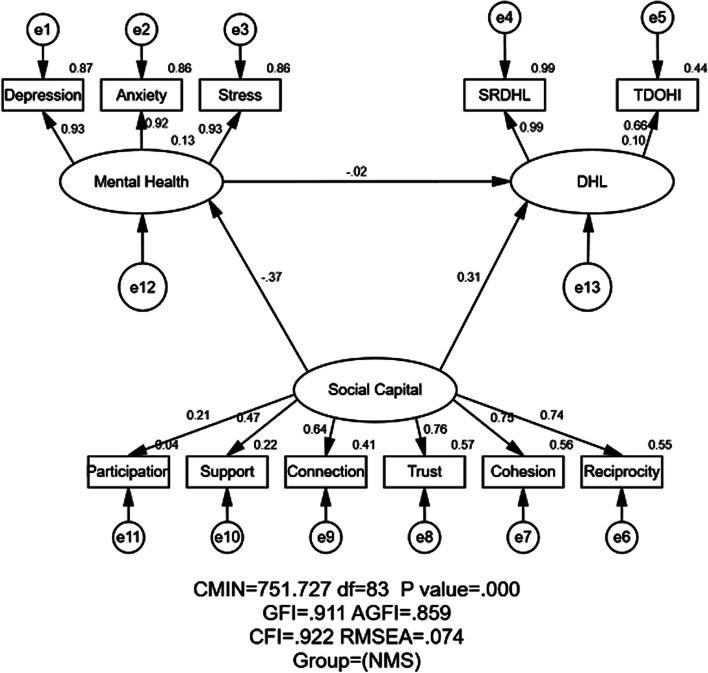
Figures 2 and 3 displayed the unconstrained model of MS and NMS groups, respectively. As shown in Figs. 2 and 3, the estimates of model fitness were the same for the two groups in M1 and M2: GFI = 0.911 > 0.90, AGFI = 0.859 > 0.80, NFI = 0.913, IFI = 0.922, CFI = 0.922 > 0.90, and RMSEA = 0.074 < 0.08, indicating the proposed model fit the empirical data well for both MS and NMS. The chi-square in AMOS was called CMIN and it was significant (P < 0.001) in this study. However, the CMIN was not applied to appraise the fitness index in the current study due to it is sensitive to the sample size [45].
Fig. 2.
Structural equation modeling analysis of the association between social capital, mental health and DHL (digital health literacy) of the MS (n = 665). Employing the data, association between social capital, mental health and DHL were analyzed. The arrows indicate the associations and directions between variables. All parameter estimates were statistically significant (P < 0.001). Note: CMIN = Chi Square; df = Degrees of Freedom; GFI = Goodness of Fit Index; AGFI = Adjusted Goodness of Fit Index; CFI = Comparative Fitness Index; RMSEA = Root-mean Square; MS = Medical Students; SRDHL = Self-rated of Digital Health Literacy; TDOHI = Trust Degree of Online Health Information
Fig. 3.
Structural equation modeling analysis of the association between social capital, mental health and DHL (digital health literacy) of the NMS (n = 807). Employing the data, association between social capital, mental health and DHL were analyzed. The arrows indicate the associations and directions between variables. All parameter estimates were statistically significant (P < 0.001), except for the impact of mental health on DHL. Note: CMIN = Chi Square; df = Degrees of Freedom; GFI = Goodness of Fit Index; AGFI = Adjusted Goodness of Fit Index; CFI = Comparative Fitness Index; RMSEA = Root-mean Square; NMS = Nonmedical Students; SRDHL = Self-rated of Digital Health Literacy; TDOHI = Trust Degree of Online Health Information
Association between social capital, mental health and DHL assessed by SEM
Table 2, Figs. 2 and 3 illustrated the association of standardized effects between social capital, mental health and DHL. The total effects in the path mode consisted of direct and indirect. In Figs. 2 and 3, social capital → DHL showed the direct effect from social capital to DHL. And social capital → mental health → DHL showed the indirect effect of social capital on DHL via mental health.
Table 2.
Standardized effects between social capital, mental health and DHL by major
| Variable | Direct | Indirect | Total | |||
|---|---|---|---|---|---|---|
| MS | NMS | MS | NMS | MS | NMS | |
| Social Capital → DHL | 0.245 | 0.311 | -0.062 | 0.060 | 0.184 | 0.371 |
| Mental Health → DHL | 0.242 | -0.017 | - | - | 0.242 | -0.017 |
| Social Capital → Mental Health | -0.255 | -0.366 | - | - | -0.255 | -0.366 |
MS Medical students, NMS Nonmedical students, DHL Digital health literacy
Relationship between social capital and DHL
As shown in Table 2, Figs. 2 and 3, social capital exerted both direct and indirect (through mental health) impact on DHL. The positive and direct effect of social capital on DHL were reported in both MS (standardized direct effects = 0.245) and NMS (standardized direct effects = 0.311). Meanwhile, the indirect effect of social capital on DHL through mental health in MS was negative (standardized indirect effects = − 0.062) but in NMS was no statically significance (standardized indirect effects = 0.060). Eventually, social capital exerted a stronger positive effect on DHL for NMS than MS (standardized total effects = 0.371 for NMS; standardized total effects = 0.184 for MS), implying that the higher social capital groups would have higher DHL.
Relationship between mental health and DHL
Mental health exerted positive indirect effect among MS (standardized total effects = 0.242) and negatively indirect effect (standardized total effects = − 0.017) among NMS on DHL, yet none statistical significance was found for NMS. As motioned in the method, the higher score of mental health implied the poorer mental health. In this study, the poorer mental health status of MS would indicate the higher DHL of MS, yet the correlation for NMS had no statistical significance.
Relationship between social capital and mental health
Social capital exerted negative and direct impact on mental health for both the MS and NMS (standardized total effect = − 0.255 for MS; standardized total effect = − 0.236 for NMS). Taking the higher score of mental health implied the poorer mental health, the higher level of social capital would indicate the better mental health for both MS and NMS in this study.
Measurement invariance across major
The authors used Harman's single-factor test for Common Method bias(CMB) [46], and the results showed that a total of 8 factors with eigenvalues > 1 were extracted, and the explanation rate of the first factor was 25.60%, which was lower than the 40% critical value, indicating that there was no common method bias in the data of this study [47].
Table 3 showed the results of related fitness indicators regarding the measurement invariance across majors and the fitness indexes in eight different models. To check whether the major was suitable for group comparison, the fitness indexes between MS and NMS should be compared first.
Table 3.
Model invariance test using multi-group nested analysis
| Model | χ2 | df | χ2 /df | GFI | AGFI | NFI | IFI | CFI | RMSEA | ΔCFI | ΔRMSEA | CN |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M1 | 751.727a | 83 | 9.057 | 0.911 | 0.859 | 0.913 | 0.922 | 0.922 | 0.074 | - | - | 207 |
| M2 | 751.727a | 83 | 9.057 | 0.911 | 0.859 | 0.913 | 0.922 | 0.922 | 0.074 | 0 | 0 | 207 |
| M3 | 751.727a | 83 | 9.057 | 0.911 | 0.859 | 0.913 | 0.922 | 0.922 | 0.074 | 0 | 0 | 207 |
| M4 | 755.970a | 90 | 8.400 | 0.911 | 0.869 | 0.909 | 0.923 | 0.922 | 0.071 | 0 | 0.003 | 222 |
| M5 | 793.876a | 93 | 8.536 | 0.907 | 0.868 | 0.909 | 0.918 | 0.918 | 0.072 | 0.004 | 0.001 | 217 |
| M6 | 793.877a | 94 | 8.445 | 0.907 | 0.870 | 0.908 | 0.919 | 0.918 | 0.071 | 0 | 0.001 | 219 |
| M7 | 800.877a | 96 | 8.342 | 0.907 | 0.872 | 0.901 | 0.918 | 0.918 | 0.071 | 0 | 0 | 222 |
M1 Medical students, M2 Nonmedical students, M3 Unconstrained, M4 Measurement weights, M5 Structural weights, M6 Structural covariance, M7 Structural residuals, χ2 Chi square, df Degrees of freedom, GFI Goodness of fit index, AGFI Adjusted goodness of fit index, NFI Normed fit index, IFI Incremental fit index, CFI Comparative fitness index, RMSEA Root-mean square error of approximation, ∆CFI Change of CFI, ∆RMSEA Change of RMSEA, CN Hoelter’s critical N
As illustrated in Table 3, the fitness indices of MS and NMS were same (GFI = 0.911, AGFI = 0.859, NFI = 0.913, IFI = 0.922, CFI = 0.922, RMSEA = 0.074 for both M1 and M2). The GFI, NFI, IFI and CFI were higher than 0.9, the AGFI was more than 0.8, and the RMSEA values were less than 0.08, implying the measurement invariance between two groups on the other models could be furtherly explored.
Then the ΔCFI and ΔRMSEA between M3 (unconstrained model), M4 (measurement weights model), M5 (structural weights model), M6 (structural covariance model) and M7 (structural residuals model) were used to evaluate the measurement invariance. The M3 does not restrict any model coefficient, the M4 assumes that the indicator loadings for the corresponding construct of each group are equal, while M5 constrains both the indicator loadings of the corresponding construct and the structural coefficients between two groups. Instead, M6 assumes the indicator loadings of the corresponding construct and the structural coefficients between two groups are equal. In addition, the indicator loadings, structural coefficients, endogenous variables' covariance, and variance of the exogenous variable between the groups are assumed equal in M7.
In Table 3, the ΔCFI was 0.004 between M4 and M5, and 0 between M3 and M4, M5 and M6, M6 and M7; the ΔRMSEA between M3 and M4, M4 and M5, M5 and M6, and M6 and M7, are 0.003, 0.001, 0.001 and 0, respectively. All the ΔCFI values were less than 0.010, implying that the measurement invariance of each model was established. Regarding ΔRMSEA, the value less than 0.015 established the measurement invariance between the M1, M2, M3, M4, M5, M6 and M7 models across the group of medical and NMS. In terms of the CN at the 0.05 significance level, all models had CN values greater than 200. Therefore, the above multi- group restriction models have the property of constancy and can be estimated across group categories.
Discussion
Principal findings
Using SEM, this study clarified the status and determinants of DHL among the university students in China, and investigated the major difference in social capital, mental health and DHL between MS and NMS. The findings of this study confirmed the first hypothesis, which hypothesized that DHL was positively associated with social capital in university students(H1). As for the second hypothesis, which hypothesized the DHL was correlated with mental health among the university students(H2) was only partially confirmed. Mental health was positively associated with social capital in university students(H3) was also confirmed in this study.
Major difference in demographic characteristics
In terms of influencing effects of major among demographic characteristics, there were significant major difference among age, health compared to last year, and health compared to peers. MS were older than NMS in this study, which may due to the fact that the duration for most medical professions in China were longer than non-medical professions, which was similar with the research in United States and Canada [48, 49]. Regarding the health compared to last year and peers, MS suggested their health status become worse than last year and peers. It was similar with previous studies that MS have more negative attitudes towards their health status than NMS because of academic pressure [50, 51].
DHL of the participants
The mean value of DHL was 36.27 for university students, implying the levels of DHL to be satisfactory. There was limited literature regarding levels of DHL and number of assessments used to measure DHL, which made it difficult to compare studies directly. Compared to peers, a study showed a similar result among university students in Denmark and Australia [52, 53], and findings from the Portuguese survey also reported the adequate DHL [54]. In this study, MS had higher scores of DHL than NMS, which contradicted previous research undertaken in university students in England [55] and Taiwan province of China [56].
Social capital and DHL
Consistent with the first hypothesis(H1), positive effect of social capital on DHL was found in this study, which was similar with Paige's study conducted among the university students in America [57], and Wu et al. also clarified the positive association between social support and eHealth literacy [58]. However, Wang et al. proposed the self-realization of benefits of online information was more effective than social capital [59]. As for major difference, NMS exerted stronger effect than MS in this study, this may due to the fact that MS generally have better health knowledge than NMS and the social capital is not the main access to health information for them [60, 61]. Lee suggested that social capital was a resource, which had a positive effect in improving the efficiency of health information dissemination [62]. And Tsahi Zack Hayat clarified that social capital could help bridge the gap for individuals with lower levels of DHL [63]. Therefore, it will be important for university students, especially NMS, to improve the social capital to enhance the DHL.
Mental health and DHL
Negative association between mental health and DHL was clarified among MS in present study (higher mental health score means lower mental health status by using DASS-21), which contradicted with the findings of Ning et al. [64]. And the relationship for NMS had no statistical significance. In other words, the lower mental health status would generally indicate the higher DHL. The second hypothesis(H2) was only partially confirmed. Previous studies showed MS had worse mental health than NMS [65–67].This might because MS mainly have a deeper perception and understanding of changes in mental health [68–70], they were more proactive in accessing health information and have higher DHL when they feel their mental health deteriorates. On the contrary, NMS were not able to detect and accurately describe the changes of mental health status to search this information online which may explain why the relationship between mental health and DHL for the NMS had no statistical significance. Moreover, MS might be worried about jeopardizing their expertise, which pushed them to search the informal sources (such as Internet) for health information when needed rather than formal healthcare-seeking behavior [71–74]. Young people with high knowledge were more likely to seek professional and useful mental health information online [75]. As for NMS with poor health knowledge, they were more willing to seek formal professional health services offline [76], rather than searching online. This implies the importance of improving basic medical language for NMS should be addressed. Existing studies and European initiatives advocated the digital health on education implementation among university students [77]. On the contrast of this study, Martin Baumgartner et al. focus on the improvement of digital health education in MS [78]. In a word, policymakers should add common digital health information in general health education among university students.
Social capital and mental health
The third hypothesis(H3) regarded that positive correlation was determined in present study between social capital and mental health score both for MS and NMS, which was confirmed by the findings. It was in accordance with previous studies [79, 80]. That is to say, the higher social capital would generally imply the higher mental health status (higher mental health score means lower mental health status by using DASS-21). Social capital might protect mental health by playing a buffering role against mental health problems [81]. Meanwhile, social capital may enhance resilience to maintain better mental health [82]. Regarding the major difference between social capital and mental health, MS have stronger correlation than NMS. MS faced heavy academic schedules, disrupted work-life balance [83], while NMS had more spare time to socialise and relax. That is to say, NMS may have more opportunities to release negative emotions and stress through the buffering effect of social support and other entertainment ways. This suggested that the improvement of social support capital would be beneficial to mental health among university students.
Implications
Firstly, the effect of social capital on mental health and DHL implied more attention should be paid to university students' social network, especially for the NMS with less health knowledge. Secondly, the statistical correlation between mental health and DHL highlighted the importance of maintenance and promotion of mental health for the university students, particularly in health consulting services and health education. Thirdly, mental health, a mediator of social capital and DHL, could affect the correlation between social capital and mental health. Therefore, the importance of mental health promotion among university students should be addressed. It is essential to accommodate the diversity of major and improve the health condition by enhancing the DHL of university students. The results of the current study on the empirical relationship between social capital, mental health and DHL could be useful in the development of fostering DHL among university students. These findings may provide evidence-based reference for improving DHL of university students in China.
Limitations
There were several limitations of the present study should be addressed. First, information was collected by processing a self-assessment typical for online questionnaires, which may cause issues such as the uncertainty of the respondents' attitude and seriousness when completing it. Second, the cross-sectional nature of the data limits the study of causal relationships between these factors. Third, the total number of the female were almost twice as male may affect the results of the study. Forth, the 9th question of CSSCS scale was deleted. Despite the good results of the scale's reliability, the appropriateness of using the scale's original scoring method to calculate the total score of CSSCS needs to be further explored. Finally, although the snowball sampling could be utilized to reach the participants who may not be easily accessible, it may also bring potential bias stemming from the non-random selection of participants and the risk of oversampling certain subgroups within the population. Combining snowball sampling with other sampling methods or employing rigorous data analysis techniques to mitigate potential bias and fully representative of the target population are needed for the future researches.
Conclusion
Despite the limitations above, the present study clarified the empirical association between social capital, mental health, and DHL among university students in China and highlight the major difference between MS and NMS. Social capital was found to be significantly and positively associated with mental health and DHL, with NMS slightly stronger than MS. Statistically significant positive association between mental health and DHL was found among MS, but not found among the NMS. The current study was a cross-sectional survey and future longitudinal studies should also be conducted to explore causal relationships. In addition, health includes physical health and social health in addition to mental health, and more research in the future will explore health and social capital and DHL in these categories. Since only the major difference were explored in this study, more researches focusing in difference of rural, other majors (engineering and non-engineering) etc. are worth to explore. Additionally, MS perceived themselves to be in poorer health than NMS. Therefore, a future study is planned to clarify the association between physical health, mental health, and the DHL among MS and NMS.
Acknowledgements
The research team greatly appreciates the funding support, and the research participants for their cooperation and support.
Abbreviations
- DHL
Digital Health Literacy
- MS
Medical Students
- NMS
Nonmedical Students
- CSSCS
Chinese Shortened Social Capital Scale
- DASS-21
Depression Anxiety Stress Scale
- DHLA
Digital Health Literacy Assessment
- ANOVA
One-way Analysis of Variance
- SEM
Structural equation modeling
- SRDHL
Self-rated Digital Health Literacy
- TDOHI
Trust Degree of Online Health Information
- CMIN
Chi square
- RMSEA
Root mean square error of approximation
- GFI
Goodness-of-fit index
- AGFI
Adjusted goodness of fit Index
- CFI
Comparative fit index
- NFI
Normed Fit Index
- IFI
Incremental Fit Index
- CN
Hoelter’s critical N
- CMB
Common Method bias
Authors’ contributions
Jiajia Zhao performed the experiments, analyzed the data, drafted the manuscript; Limei Nie performed the experiments, analyzed the data and provided several valuable comments on the draft. Fanlei Kong applied the fund to support this study, designed the study, completed the questionnaire design, supervised and combined the data collected, instructed the writing, statistical analysis, data processing and provided comments on the modification of the manuscript; Lutong Pan, Mingli Pang, Jieru Wang, Yue Zhou, Rui Chen, Hui Liu, Xixing Xu, Chengchao Zhou and Shixue Li gave many valuable comments on the manuscript and polished it. All authors read and approved the final manuscript.
Funding
This study was supported and funded by the National Natural Science Foundation of China (No. 71804094).
Availability of data and materials
Under reasonable requirements, the data and material of this study can be obtained from the corresponding author. The data are not publicly available due to privacy restrictions.
Declarations
Consent for publication
All authors consent to the publication of this research.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.CNNIC: The 51st Statistical Report on China's Internet Development. China Internet. 2023. http://www.199it.com/archives/1573087.html.
- 2.Zhou X-F, Chen L. Digital health care in China and access for older people. Lancet Public Health. 2021;6(12):e873–4. 10.1016/S2468-2667(21)00051-7 [DOI] [PubMed] [Google Scholar]
- 3.do Borges Nascimento IJ, Pizarro AB, Almeida JM, Azzopardi-Muscat N, Gonçalves MA, Björklund M, Novillo-Ortiz D. Infodemics and health misinformation: a systematic review of reviews. Bull World Health Organ. 2022;100(9):544–61. 10.2471/BLT.21.287654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sefidbakht S, Lotfi M, Jalli R, Moghadami M, Sabetian G, Iranpour P. Methanol toxicity outbreak: when fear of COVID-19 goes viral. Emerg Med J. 2020;37(7):416. 10.1136/emermed-2020-209886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hassanian-Moghaddam H, Zamani N, Kolahi A-A, McDonald R, Hovda KE. Double trouble: methanol outbreak in the wake of the COVID-19 pandemic in Iran—a cross-sectional assessment. Crit Care. 2020;24(1):402. 10.1186/s13054-020-03140-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.During this coronavirus pandemic, ‘fake news’ is putting lives at risk. https://news.un.org/en/story/2020/04/1061592.
- 7.Lee J-A, Choi M, Lee SA, Jiang N. Effective behavioral intervention strategies using mobile health applications for chronic disease management: a systematic review. BMC Med Inform Decis Mak. 2018;18(1):12. 10.1186/s12911-018-0591-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Vaart R, Drossaert C. Development of the digital health literacy instrument: measuring a broad spectrum of health 1.0 and Health 2.0 skills. J Med Internet Res. 2017;19(1):e27. 10.2196/jmir.6709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim K, Shin S, Kim S, Lee E. The relation between eHealth literacy and health-related behaviors: systematic review and meta-analysis. J Med Internet Res. 2023;25:e40778. 10.2196/40778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davis SLM, Pham T, Kpodo I, Imalingat T, Muthui AK, Mjwana N, Sandset T, Ayeh E, Dong DD, Large K, et al. Digital health and human rights of young adults in Ghana, Kenya and Vietnam: a qualitative participatory action research study. BMJ Glob Health. 2023;8(5):e011254. 10.1136/bmjgh-2022-011254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spexoto MCB, Serrano SV, Halliday V, Maroco J, Wilcock A, Campos JADB. Cross-cultural psychometric assessment of an appetite questionnaire for patients with cancer. Trends Psychiatry Psychother. 2018;40(2):152–9. 10.1590/2237-6089-2017-0093 [DOI] [PubMed] [Google Scholar]
- 12.Sun H, Qian L, Xue M, Zhou T, Qu J, Zhou J, Qu J, Ji S, Bu Y, Hu Y, et al. The relationship between eHealth literacy, social media self-efficacy and health communication intention among Chinese nursing undergraduates: a cross-sectional study. Front Public Health. 2022;10:1030887. 10.3389/fpubh.2022.1030887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bao X, Chen D, Shi L, Xia Y, Shi Z, Wang D. The relationship between COVID-19-related prevention cognition and healthy lifestyle behaviors among university students: mediated by e-health literacy and self-efficacy. J Affect Disord. 2022;309:236–41. 10.1016/j.jad.2022.04.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McKenzie K, Whitley R, Weich S. Social capital and mental health. Br J Psychiatry. 2002;181:280–3. 10.1192/bjp.181.4.280 [DOI] [PubMed] [Google Scholar]
- 15.Almedom AM. Social capital and mental health: an interdisciplinary review of primary evidence. Soc Sci Med. 2005;61(5):943–64. 10.1016/j.socscimed.2004.12.025 [DOI] [PubMed] [Google Scholar]
- 16.Cao C, Cao W, Zheng X, Ji K, Wu Y, Hu Z, Chen R, Bai Z. Association of social capital with self-perceived eHealth literacy among community-dwelling older people: age and gender differences. Front Public Health. 2023;11:1088863. 10.3389/fpubh.2023.1088863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cui G-H, Li S-J, Yin Y-T, Chen L-J, Li J-Q, Liang F-Y, Liu X-Y, Chen L. The relationship among social capital, eHealth literacy and health behaviours in Chinese elderly people: a cross-sectional study. BMC Public Health. 2021;21(1):45. 10.1186/s12889-020-10037-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stellefson ML, Shuster JJ, Chaney BH, Paige SR, Alber JM, Chaney JD, Sriram PS. Web-based Health Information Seeking and eHealth Literacy among Patients Living with Chronic Obstructive Pulmonary Disease (COPD). Health Commun. 2018;33(12):1410–24. 10.1080/10410236.2017.1353868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arcury TA, Sandberg JC, Melius KP, Quandt SA, Leng X, Latulipe C, Miller DP, Smith DA, Bertoni AG. Older adult internet use and eHealth literacy. J Appl Gerontol. 2020;39(2):141–50. 10.1177/0733464818807468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO.Mental Health Report 2022. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response.
- 21.Yang BX, Xia L, Huang R, Chen P, Luo D, Liu Q, Kang LJ, Zhang ZJ, Liu Z, Yu S, et al. Relationship between eHealth literacy and psychological status during COVID-19 pandemic: a survey of Chinese residents. J Nurs Manag. 2021;29(4):805–12. 10.1111/jonm.13221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tariku Seboka B, Hailegebreal S, Negash M, Mamo TT, Ali Ewune H, Gilano G, Yehualashet DE, Gizachew G, Demeke AD, Worku A, et al. Predictors of mental health literacy and information seeking behavior toward mental health among university students in resource-limited settings. Int J Gen Med. 2022;15:8159–72. 10.2147/IJGM.S377791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nguyen TT, Nguyen MH, Pham TTM, Le V-TT, Nguyen TT, Luong TC, Do BN, Dao HK, Nguyen HC, Ha TH, et al. Negative impacts of COVID-19 induced lockdown on changes in eating behavior, physical activity, and mental health as modified by digital healthy diet literacy and eHealth literacy. Front Nutr. 2021;8:774328. 10.3389/fnut.2021.774328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gu N. The effects of neighborhood social ties and networks on mental health and well-being: a qualitative case study of women residents in a middle-class Korean urban neighborhood. Soc Sci Med. 2020;265:113336. 10.1016/j.socscimed.2020.113336 [DOI] [PubMed] [Google Scholar]
- 25.Cao D, Zhou Z, Liu G, Shen C, Ren Y, Zhao D, Zhao Y, Deng Q, Zhai X. Does social capital buffer or exacerbate mental health inequality? Evidence from the China Family Panel Study (CFPS). Int J Equity Health. 2022;21(1):75. 10.1186/s12939-022-01642-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu X, Zhang L, Lin Z, Zhou Z, Hazer-Rau D, Li P, Ji W, Zhang H, Wu T. Ostracism, psychological capital, perceived social support and depression among economically disadvantaged youths: a moderated mediation model. Int J Environ Res Public Health. 2021;18:11282. 10.3390/ijerph182111282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Backhaus I, Varela AR, Khoo S, Siefken K, Crozier A, Begotaraj E, Fischer F, Wiehn J, Lanning BA, Lin PH, et al. Associations between social capital and depressive symptoms among college students in 12 countries: results of a cross-national study. Front Psychol. 2020;11:644. 10.3389/fpsyg.2020.00644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim E, Song MK. Profiles of social capital and the association with depressive symptoms among multicultural adolescents in Korea: a latent profile analysis. Front Public Health. 2022;10:794729. 10.3389/fpubh.2022.794729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chu H, Yang Y, Zhou J, Wang W, Qiu X, Yang X, Qiao Z, Song X, Zhao E. Social support and suicide risk among Chinese university students: a mental health perspective. Front Public Health. 2021;9:566993. 10.3389/fpubh.2021.566993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu P, Yeh L-L, Wang J-Y, Lee S-T. relationship between levels of digital health literacy based on the Taiwan digital health literacy assessment and accurate assessment of online health information: cross-sectional questionnaire study. J Med Internet Res. 2020;22(12):e19767. 10.2196/19767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nie L, Zhao J, Pan L, Pang M, Wang J, Zhou Y, Chen R, Liu H, Xu X, Su B, et al. Validation of the digital health literacy assessment among the university students in China. Front Public Health. 2023;11:1294183. 10.3389/fpubh.2023.1294183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bai Z, Xu Z, Xu X, Qin X, Hu W, Hu Z. Association between social capital and depression among older people: evidence from Anhui Province, China. BMC Public Health. 2020;20(1):1560. 10.1186/s12889-020-09657-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu F, Niu L, Chen R, Ma Y, Qin X, Hu Z. The association between social capital and quality of life among type 2 diabetes patients in Anhui province, China: a cross-sectional study. BMC Public Health. 2015;15:786. 10.1186/s12889-015-2138-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jago R, Fox KR, Page AS, Brockman R, Thompson JL. Development of scales to assess children’s perceptions of friend and parental influences on physical activity. Int J Behav Nutr Phys Act. 2009;6:67. 10.1186/1479-5868-6-67. 10.1186/1479-5868-6-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gupta M, Gupta V, Nagar Buckshee R, Sharma V. Validity and reliability of hindi translated version of Montreal cognitive assessment in older adults. Asian J Psychiatr. 2019;45:125–8. 10.1016/j.ajp.2019.09.022 [DOI] [PubMed] [Google Scholar]
- 36.Wang K, Shi H-S, Geng F-L, Zou L-Q, Tan S-P, Wang Y, Neumann DL, Shum DHK, Chan RCK. Cross-cultural validation of the depression anxiety stress scale-21 in China. Psychol Assess. 2016;28(5):e88. 10.1037/pas0000207 [DOI] [PubMed] [Google Scholar]
- 37.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. 10.1037/0033-2909.88.3.588 [DOI] [Google Scholar]
- 38.Jöreskog KGA, E.B.; Laake, P.; Cox, D.; Schweder, T. Analysis of covariance structures[with discussion and reply]. Scand J Stat. 1981;8:65–92.
- 39.Hu LT, Bentler P. M: cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- 40.Rong T. Amos and research method. 2nd ed. Chongqing: Chongqing University Press; 2010. [Google Scholar]
- 41.Kline RB. Principles and practice of structural equation modeling. 4th ed. New York: The Guilford Press; 2016. [Google Scholar]
- 42.Haibo X. Research on the Psychological Capital and Its Influence on Management Effectiveness of Universities' Middle-level Administrators in China. China University of Mining and Technology; 2022.
- 43.Zhao BH: Measurement equivalence test and implementation of AMOS. China Health Stat. 2007;24.
- 44.Cheung GWR, Roger B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Modeling. 2002;9(2):233–55. 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- 45.Jiang S, Liang Z. Mediator of school belongingness and moderator of migration status in the relationship between peer victimization and depression among Chinese children: a multi-group structural equation modeling approach. J Affect Disord. 2021;278:382–9. 10.1016/j.jad.2020.09.075 [DOI] [PubMed] [Google Scholar]
- 46.Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879–903. 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- 47.Dandan Tang LW. Common methodology bias testing: issues and recommendations. Psychol Sci. 2020;43(1):215–23. [Google Scholar]
- 48.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354–73. 10.1097/00001888-200604000-00009 [DOI] [PubMed] [Google Scholar]
- 49.Goebert D, Thompson D, Takeshita J, Beach C, Bryson P, Ephgrave K, Kent A, Kunkel M, Schechter J, Tate J. Depressive symptoms in medical students and residents: a multischool study. Acad Med. 2009;84(2):236–41. 10.1097/ACM.0b013e31819391bb [DOI] [PubMed] [Google Scholar]
- 50.Porru F, Schuring M, Bültmann U, Portoghese I, Burdorf A, Robroek SJW. Associations of university student life challenges with mental health and self-rated health: a longitudinal study with 6 months follow-up. J Affect Disord. 2022;296:250–7. 10.1016/j.jad.2021.09.057 [DOI] [PubMed] [Google Scholar]
- 51.Martin SD, Urban RW, Johnson AH, Magner D, Wilson JE, Zhang Y. Health-related behaviors, self-rated health, and predictors of stress and well-being in nursing students. J Prof Nurs. 2022;38:45–53. 10.1016/j.profnurs.2021.11.008 [DOI] [PubMed] [Google Scholar]
- 52.Bak CK, Krammer JØ, Dadaczynski K, Orkan O, von Seelen J, Prinds C, Søbjerg LM, Klakk H. Digital health literacy and information-seeking behavior among university college students during the COVID-19 pandemic: a cross-sectional study from Denmark. Int J Environ Res Public Health. 2022;19(6):3676. 10.3390/ijerph19063676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taba M, Allen TB, Caldwell PHY, Skinner SR, Kang M, McCaffery K, Scott KM. Adolescents’ self-efficacy and digital health literacy: a cross-sectional mixed methods study. BMC Public Health. 2022;22(1):1223. 10.1186/s12889-022-13599-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rosário R, Martins MRO, Augusto C, Silva MJ, Martins S, Duarte A, Fronteira I, Ramos N, Okan O, Dadaczynski K. Associations between COVID-19-related digital health literacy and online information-seeking behavior among portuguese university students. Int J Environ Res Public Health. 2020;17(23):8987. 10.3390/ijerph17238987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Frings D, Sykes S, Ojo A, Rowlands G, Trasolini A, Dadaczynski K, Okan O, Wills J. Differences in digital health literacy and future anxiety between health care and other university students in England during the COVID-19 pandemic. BMC Public Health. 2022;22(1):658. 10.1186/s12889-022-13087-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen S-C, Hong Nguyen NT, Lin C-Y, Huy LD, Lai C-F, Dang LT, Truong NLT, Hoang NY, Nguyen TTP, Phaṇ TN, et al. Digital health literacy and well-being among university students: Mediating roles of fear of COVID-19, information satisfaction, and internet information search. Digit Health. 2023;9:20552076231165970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Paige SR, Stellefson M, Chaney BH, Chaney JD, Alber JM, Chappell C, Barry AE. Examining the relationship between online social capital and eHealth literacy: implications for instagram use for chronic disease prevention among college students. Am J Health Educ. 2017;48(4):264–77. 10.1080/19325037.2017.1316693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu Y, Wen J, Wang X, Wang Q, Wang W, Wang X, Xie J, Cong L. Chinese community home-based aging institution elders’ self-management of chronic non-communicable diseases and its interrelationships with social support, e-Health literacy, and self efficacy: a serial multiple mediation model. Patient Prefer Adherence. 2023;17:1311–21. 10.2147/PPA.S412125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang X, Yue T, Mo PK-h. The associations among cognitive social factors, eHealth literacy and health-promoting behaviors in Chinese adolescents. Health Promot Int. 2022;37(6):daac143. 10.1093/heapro/daac143 [DOI] [PubMed] [Google Scholar]
- 60.Huang Y, Gu J, Zhang M, Ren Z, Yang W, Chen Y, Fu Y, Chen X, Cals JWL, Zhang F. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ. 2013;13(1):163. 10.1186/1472-6920-13-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jamshed SQ, Elkalmi R, Rajiah K, Al-Shami AK, Shamsudin SH, Siddiqui MJA, Abdul Aziz MAB, Hanafi MBB, Mohammad Shariff NIB, Ramlan NHB, et al. Understanding of antibiotic use and resistance among final-year pharmacy and medical students: a pilot study. J Infect Dev Ctries. 2014;8(6):780–5. 10.3855/jidc.3833 [DOI] [PubMed] [Google Scholar]
- 62.Lee S-YD, Arozullah AM, Cho YI. Health literacy, social support, and health: a research agenda. Soc Sci Med. 2004;58(7):1309–21. 10.1016/S0277-9536(03)00329-0 [DOI] [PubMed] [Google Scholar]
- 63.Hayat TZ, Brainin E, Neter E. With some help from my network: supplementing eHealth literacy with social ties. J Med Internet Res. 2017;19(3):e98. 10.2196/jmir.6472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ning L, Zheng Z, Liu M, Gao S, Yang X, Bi J, Yu X, Yi D. Profiles of digital health literacy among university students and its association with mental health during the COVID-19 pandemic: a latent profile analysis. Digit Health. 2024;10:20552076231224596. 10.1177/20552076231224596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yang Shuzhen GS, Bai Dongmei, An Guihua, Huang Mi, Wu Pengxia. A study on the correlation between sleep quality and depression in college students: taking a university in Gansu Province as an Example. J Hexi Univ. 2022;38(2):32-38
- 66.Li S, Cheng J, Li YP, Zhao GJ, Wang Y. Association between circadian rhythm disorder with depressive and anxiety symptoms of college students in Jinzhou City. Chin J School Health. 2022;43(5):731–5. [Google Scholar]
- 67.Zhang Y, Tao S, Qu Y, Mou X, Gan H, Zhou P, Zhu Z, Wu X, Tao F. The correlation between lifestyle health behaviors, coping style, and mental health during the COVID-19 pandemic among college students: Two rounds of a web-based study. Front Public Health. 2022;10:1031560. 10.3389/fpubh.2022.1031560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Walter G. Soh NL-W, Norgren Jaconelli S, Lampe L, Malhi GS, Hunt G: Medical students’ subjective ratings of stress levels and awareness of student support services about mental health. Postgrad Med J. 2013;89(1052):311–5. 10.1136/postgradmedj-2012-131343 [DOI] [PubMed] [Google Scholar]
- 69.Hsu W, Chiang C, Yang S. The effect of individual factors on health behaviors among college students: the mediating effects of eHealth literacy. J Med Internet Res. 2014;16(12):e287. 10.2196/jmir.3542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Broks VMA, Stegers-Jager KM, van der Waal J, van den Broek WW, Woltman AM. Medical students’ crisis-induced stress and the association with social support. PLoS One. 2022;17(12):e0278577. 10.1371/journal.pone.0278577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Roberts LW, Hardee JT, Franchini G, Stidley CA, Siegler M. Medical students as patients: a pilot study of their health care needs, practices, and concerns. Acad Med. 1996;71(11):1225–32. 10.1097/00001888-199611000-00019 [DOI] [PubMed] [Google Scholar]
- 72.Strawbridge L, Mackie S, Bharath N, Shahaf-Oren B, Madan I, Henderson C. Development of decision aid on health help-seeking for medical students. Occup Med (Lond). 2022;72(3):191–9. 10.1093/occmed/kqab188 [DOI] [PubMed] [Google Scholar]
- 73.Dyrbye LN, Eacker A, Durning SJ, Brazeau C, Moutier C, Massie FS, Satele D, Sloan JA, Shanafelt TD. The impact of stigma and personal experiences on the help-seeking behaviors of medical students with burnout. Acad Med. 2015;90(7):961–9. 10.1097/ACM.0000000000000655 [DOI] [PubMed] [Google Scholar]
- 74.Umami A, Zsiros V, Maróti-Nagy Á, Máté Z, Sudalhar S, Molnár R, Paulik E. Healthcare-seeking of medical students: the effect of socio-demographic factors, health behaviour and health status - a cross-sectional study in Hungary. BMC Public Health. 2023;23(1):2126. 10.1186/s12889-023-17041-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xu RH, Bao XL, Shi LSB, Wang D. Associations between eHealth literacy, mental health-seeking attitude, and mental wellbeing among young electronic media users in China during the COVID-19 pandemic. Front Public Health. 2023;11:1139786. 10.3389/fpubh.2023.1139786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Amarasuriya SD, Jorm AF, Reavley NJ. Perceptions and intentions relating to seeking help for depression among medical undergraduates in Sri Lanka: a cross-sectional comparison with non-medical undergraduates. BMC Med Educ. 2015;15(1):162. 10.1186/s12909-015-0453-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Commission E. EU health policy platform - proposal for a thematic network on digital skills for future-proof doctors (digital doc). 2019. https://health.ec.europa.eu/system/files/2019-10/ev_20191017_co12_en_0.pdf.
- 78.Baumgartner M, Sauer C, Blagec K, Dorffner G. Digital health understanding and preparedness of medical students: a cross-sectional study. Med Educ Online. 2022;27(1):2114851. 10.1080/10872981.2022.2114851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sotaquirá L, Backhaus I, Sotaquirá P, Pinilla-Roncancio M, González-Uribe C, Bernal R, Galeano JJ, Mejia N, La Torre G, Trujillo-Maza EM, et al. Social capital and lifestyle impacts on mental health in university students in Colombia: an observational study. Front Public Health. 2022;10:840292. 10.3389/fpubh.2022.840292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sweet D, Byng R, Webber M, Enki DG, Porter I, Larsen J, Huxley P, Pinfold V. Personal well-being networks, social capital and severe mental illness: exploratory study. Br J Psychiatry. 2018;212(5):308–17. 10.1192/bjp.bp.117.203950 [DOI] [PubMed] [Google Scholar]
- 81.Hunduma G, Deyessa N, Dessie Y, Geda B, Yadeta TA. High social capital is associated with decreased mental health problem among in-school adolescents in Eastern Ethiopia: a cross-sectional study. Psychol Res Behav Manag. 2022;15:503–16. 10.2147/PRBM.S347261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Duren R, Yalçın Ö. Social capital and mental health problems among Syrian refugee adolescents: the mediating roles of perceived social support and post-traumatic symptoms. Int J Soc Psychiatry. 2020;67(3):243–50. 10.1177/0020764020945355 [DOI] [PubMed] [Google Scholar]
- 83.Lu C-P, Dijk SW, Pandit A, Kranenburg L, Luik AI, Hunink MGM. The effect of mindfulness-based interventions on reducing stress in future health professionals: A systematic review and meta-analysis of randomized controlled trials. Appl Psychol Health Well Being. 2024;16(2):765–92. 10.1111/aphw.12472 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Under reasonable requirements, the data and material of this study can be obtained from the corresponding author. The data are not publicly available due to privacy restrictions.