Abstract
Purpose
The summary presented herein covers recommendations on the early detection of prostate cancer and provides a framework to facilitate clinical decision-making in the implementation of prostate cancer screening, biopsy, and follow-up. This is Part II of a two-part series focusing on initial and repeat biopsies, and biopsy technique. Please refer to Part I for discussion of initial prostate cancer screening recommendations.
Materials and Methods
The systematic review utilized to inform this guideline was conducted by an independent methodological consultant. The systematic review was based on searches in Ovid MEDLINE and Embase and Cochrane Database of Systematic Reviews (January 1, 2000 – November 21, 2022). Searches were supplemented by reviewing reference lists of relevant articles.
Results
The Early Detection of Prostate Cancer Panel developed evidence- and consensus-based guideline statements to provide guidance in prostate cancer screening, initial and repeat biopsies, and biopsy technique.
Conclusions
The evaluation of prostate cancer risk should be focused on the detection of clinically significant prostate cancer (grade group 2 or higher [GG2+]). The use of laboratory biomarkers, prostate MRI, and biopsy techniques described herein may improve detection and safety when a prostate biopsy is deemed necessary following prostate cancer screening.
MeSh Terms: Early detection of prostate cancer, prostate cancer screening, prostate cancer biopsy, PSA, biopsy technique, MRI, imaging, biomarkers, HGPIN, ASAP, AIP, transrectal, transperineal, PI-RADS
Background
Part I of this guideline series presented recommendations on PSA-based prostate cancer screening, emphasizing shared decision-making (SDM) and tailored risk evaluations to guide the decision for a prostate biopsy. This summary presents those recommendations and associated algorithms (Figures 2 and 3) for persons having an initial prostate biopsy or with a prior negative biopsy, as well as technical recommendations regarding prostate biopsy. It also addresses the significance of non-cancerous, yet potentially significant, pathologic findings identified in biopsies. The Panel evaluated the current evidence to develop recommendations on how best to incorporate multi-parametric magnetic resonance imaging (mpMRI) and novel biomarkers into clinical practice. An abnormal MRI, for the purpose of this guideline, is defined as PI-RADS 3 to 5. However, given the local variation and expertise in performing and interpreting MRIs, some clinicians may opt to limit an abnormal MRI to PI-RADS 4 to 5.
FIGURE 2:
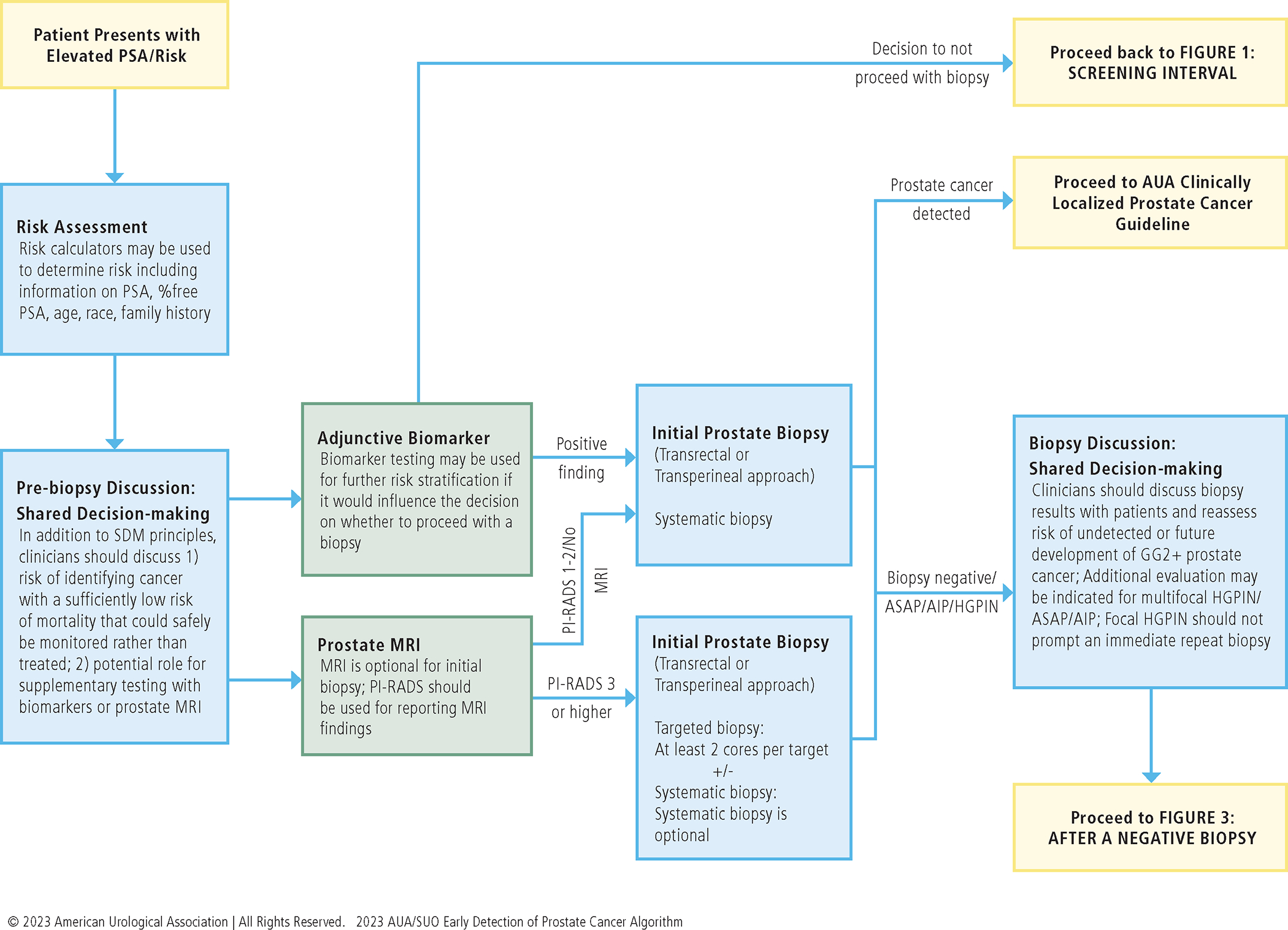
ELEVATED RISK EVALUATION
FIGURE 3:
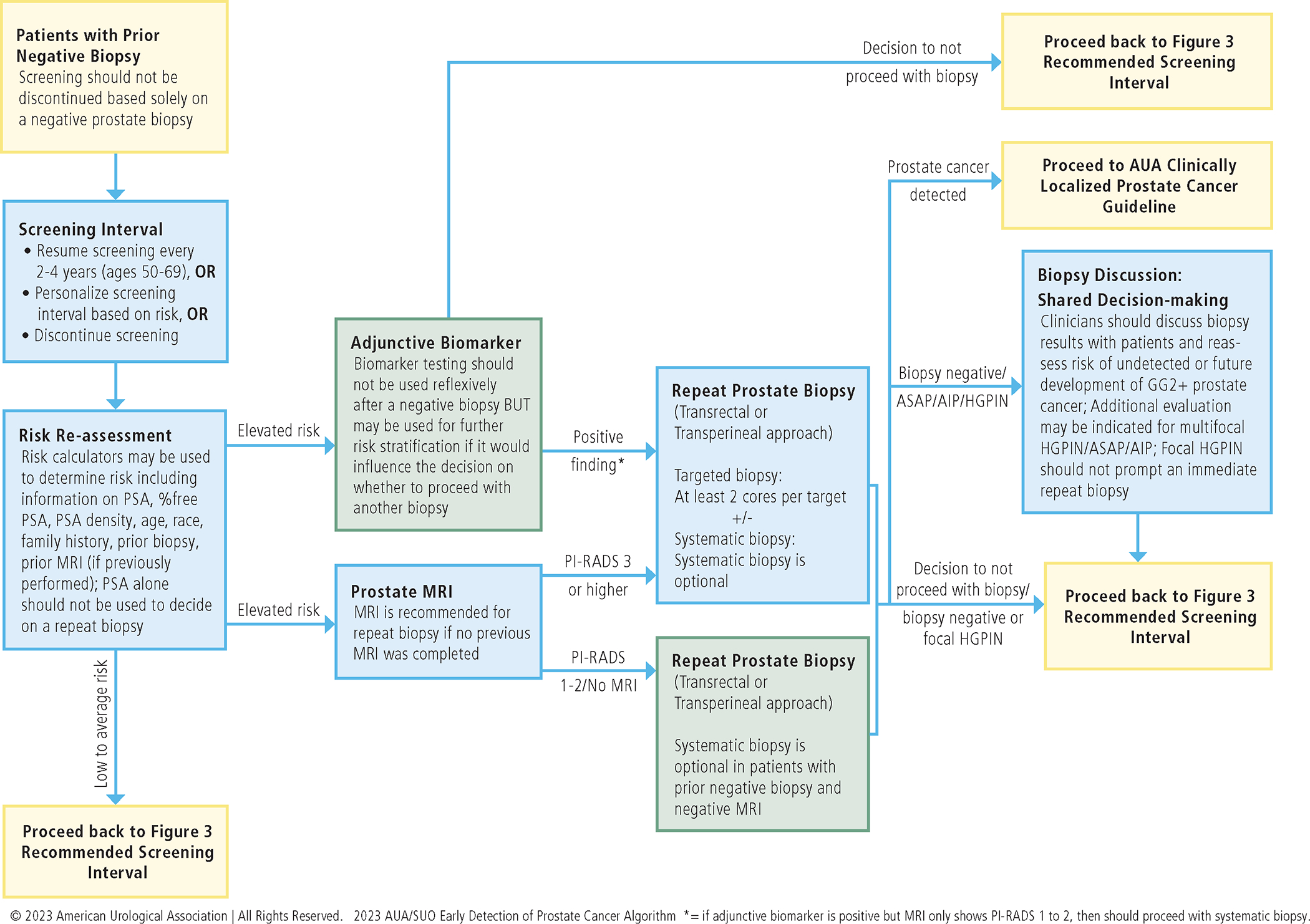
AFTER A NEGATIVE BIOPSY
Guideline Statements
Initial Biopsy
12. Clinicians should inform patients undergoing a prostate biopsy that there is a risk of identifying a cancer, with a sufficiently low risk of mortality, that could safely be monitored with active surveillance (AS) rather than treated. (Clinical Principle)
A brief pre-biopsy discussion about pathologic findings warranting AS is expected to increase subsequent acceptance of AS by patients and lower rates of treatment. In a multicenter study of patients undergoing a prostate biopsy, GG1 prostate cancer was found in 44% and 61% of initial and repeat positive biopsies, respectively.1 For low-risk prostate cancer, AS is the preferred management by the AUA and other international guidelines.2 The primary intent of screening and surveillance is to identify GG2+ prostate cancer that may prompt definitive treatment.
13. Clinicians may use MRI prior to initial biopsy to increase the detection of GG2+ prostate cancer. (Conditional Recommendation; Evidence Level: Grade B)
Studies have demonstrated that mpMRI increases the detection of clinically significant prostate cancer, while lowering the detection of insignificant disease. This is particularly true in patients with a prior negative prostate biopsy; data from patients who are biopsy-naïve are less definitive. The PRECISION trial (Prostate Evaluation for Clinically Important Disease: Sampling Using Image-guidance or Not?) was a randomized non-inferiority study that sought to compare the effectiveness of MRI-targeted versus systematic biopsy in detecting clinically significant prostate cancer in biopsy-naïve patients.3 Clinically significant prostate cancer was detected more often in patients undergoing mpMRI and patients undergoing MRI targeted biopsy had fewer insignificant cancers detected (9% versus 22%).
While some data suggest the benefit of a pre-biopsy MRI in biopsy-naïve patients, conflicting reports moderate the enthusiasm for a strong recommendation. A Cochrane review of data from 18 studies included biopsy-naïve patients and patients with prior negative prostate biopsy.4 Analysis suggests the sensitivity of a pre-biopsy MRI is 0.91 (95% CI: 0.83 to 0.95), and specificity is 0.37 (95% CI: 0.29 to 0.46) for GG2+ prostate cancer. The prostate cancer detection ratio for MRI prior to initial biopsy was 1.05 (95% CI: 0.95 to 1.16), which indicates prior MRI may have limited benefit in this setting.
In anticipation of more definitive data, it is reasonable to obtain an mpMRI in biopsy-naïve patients prior to their first biopsy, but such a practice cannot be regarded as the standard approach based on the currently available evidence.
14. Radiologists should utilize PI-RADS in the reporting of mpMRI imaging. (Moderate Recommendation; Evidence Level: Grade C)
Multiple studies have confirmed that the PI-RADS score, either on a per lesion or per patient basis, correlates with likelihood of detecting any cancer and GG2+ cancer (see supplementary references). Table 1 summarizes the detection prevalence for any prostate cancer and GG2+ prostate cancer based on the PI-RADS score when 23 studies identified by the systematic review were pooled. Clinicians should interpret PI-RADS scores in the context of known local experience and expertise. This statement applies to both initial and repeat biopsy situations.
Table 1:
Prevalence of Prostate Cancer Detection based on PI-RADS Score*
| PI-RADS Score | Any Prostate Cancer (% (95%CI)) | Clinically Significant Prostate Cancer (% (95%CI)) |
|---|---|---|
| 1 or 2 | 15% (95%CI: 8% to 22%) | 7% (95%CI: 4% to 11%) |
| 3 | 25% (95%CI: 22% to 29%) | 11% (95%CI: 8% to 14%) |
| 4 | 58% (95%CI: 53% to 63%) | 37% (95%CI: 33% to 40%) |
| 5 | 85% (95%CI: 80% to 90%) | 70% (95%CI: 62% to 79%) |
Detection prevalence for both any prostate cancer and clinically significant prostate cancer based on the PI-RADS score when 23 identified studies (see supplementary references) were pooled using a random-effects inverse-variance method. Due to the paucity of data using only PI-RADS version 2.1, pooled studies used version 1.0 through version 2.1.
15. For biopsy-naïve patients who have a suspicious lesion on MRI, clinicians should perform targeted biopsies of the suspicious lesion and may also perform a systematic template biopsy. (Moderate Recommendation [targeted biopsies]/Conditional Recommendation [systematic template biopsy]; Evidence Level: Grade C)
When a prostate MRI identifies a lesion suspicious for cancer (e.g., PI-RADS 3 to 5) among patients who are biopsy-naïve, clinicians need to decide whether to perform targeted biopsies along with systematic biopsies or perform targeted biopsies alone. Several observational studies have shown a higher detection of GG2+ prostate cancer when targeted and systematic biopsies are combined.5, 6 It has been hypothesized that systematic biopsies may improve detection of GG2+ cancer by sampling the target when the targeted cores may have missed the target.7, 8
In contrast, Kim et al. found little difference in detection between the combined approach and targeted cores.9 In reviewing the literature, the Panel found published studies have used a variety of fusion platforms, biopsy approaches, and systematic templates, making direct comparison prohibitive. The tradeoff for finding more GG2+ cancer, with adding a systematic biopsy to the target only approach, is that more GG1 cancer will also be diagnosed. In recent publications, this rate has been reported between 1.2% and 5% GG1.10, 11 Following the literature review window for these guidelines, a randomized trial comparing targeted biopsy alone versus targeted plus systematic biopsies among patients with PI-RADS 3 to 5 findings on MRI was published.11 This study demonstrated a 50% reduction in detection of GG1 cancers (absolute reduction from 1.2% to 0.6%), and a 27% reduction in findings of GG2+ cancers (absolute reduction from 1.1% to 0.8%), in the target-only arm. Although the decreased detection of GG2+ cancer detection was not statistically significant, (the study was not powered to detect this difference) it may well be clinically significant.11
16. For patients with both an absence of suspicious findings on MRI and an elevated risk for GG2+ prostate cancer, clinicians should proceed with a systematic biopsy. (Moderate Recommendation; Evidence Level: Grade C)
In a systematic review of 42 studies, the negative predictive value (NPV) of a “negative” MRI (defined as PI-RADS 1 to 2) to detect GG2+ prostate cancer among biopsy-naïve patients was 91%.12 Thus, approximately 1 in 10 patients who have a negative prostate MRI may have GG2+ cancer on biopsy, although rates widely vary by study and risk factors of the individual person. If the definition of a “negative” MRI was expanded to include PI-RADS 3, then NPV decreased to 87%.12 Multiple factors contribute to risk calculation, including race, age, total PSA, PSA density, percent free PSA, and family history of prostate cancer, as used in available risk calculators. Therefore, patients with elevated risk for GG2+ prostate cancer and a negative MRI should proceed with a systematic biopsy. SDM to omit systematic biopsy should include the risk of underdiagnosing clinically significant prostate cancer.
17. Clinicians may use adjunctive urine or serum markers when further risk stratification would influence the decision regarding whether to proceed with biopsy. (Conditional Recommendation; Evidence Level: Grade C)
There are several blood and urine markers available alone or in combination to further risk stratify patients with a mildly elevated PSA, typically between 2.5 ng/mL and 10 ng/mL. The intent is to improve upon the poor specificity of PSA and avoid the risks associated with unnecessary biopsies, including the risk of overdiagnosis of GG1 prostate cancer, in patients with a low probability of harboring GG2+ disease. Naturally, with avoidance of biopsies comes the risk of delaying the diagnosis of clinically significant prostate cancer (“false negatives”). Importantly, such biomarkers should not be used in situations in which, based on available clinical and laboratory data, the risk of GG2+ prostate cancer is so low or so high the result of adjunctive biomarkers would not influence the decision of whether to proceed with further testing (e.g., MRI and/or biopsy).
It is debatable which of the newer biomarkers (alone or in combination) is best, and comparative studies are sparse. Available tests for an initial biopsy cohort are summarized in Table 2. In general, the tests are calibrated such that avoiding biopsy in the setting of a sub-threshold test reduces biopsies by about one third, resulting in delayed detection or non-detection of 5% to 10% of clinically significant prostate cancers.13 A meta-analysis of studies included in the evidence base for this guideline showed that use of secondary biomarkers would reduce the number of biopsies by 35% (95% CI: 26% to 44%; p<0.0001), and 9% (95% CI: 6% to 11%; p<0.0001) of clinically significant prostate cancers would not be detected (see Guideline for complete list of included studies). Given their significant impact on biopsy reduction and their projected minimal impact on life expectancy, such tests may be of value among patients with modestly elevated PSA tests, especially in patients with a prior negative biopsy, in whom PSA alone is not recommended as the sole trigger for re-biopsy. This statement applies to both initial and repeat biopsy situations.
Table 2:
Available Biomarker Assays
| Test | Biomarker Component | Clinical Variable | Biopsy Population |
|---|---|---|---|
| Serum | |||
| 4Kscore | PSA, fPSA, iPSA, hK2 | Age, prior biopsy status, DRE (optional) | Initial biopsy Repeat biopsy |
| IsoPSA* | All PSA isoforms | None | Not specified |
| Proclarix | THBS1, CTSD, PSA, fPSA | Age, prostate volume (optional) | Mixed |
| PHI | p2PSA, fPSA, PSA | None | Initial biopsy Repeat biopsy |
| STHLM-3 | 232 genetic polymorphisms (SNPs), PSA, fPSA, iPSA, hK2, MSMB, MIC1 | Age, family history, previous biopsy, DRE (optional) | Mixed |
| Post-DRE Urine | |||
| PCA3 | PCA3 | Some studies add age, PSA, prostate volume | Initial biopsy Repeat biopsy |
| MPS | PCA3, TMPRSS2:ERG, PSA | None | Initial biopsy Repeat biopsy |
| SelectMDx | HOXC6, DLX1 mRNA | Age, PSA, prostate volume, DRE | Initial biopsy |
| TMPRSS2:ERG | TMPRSS2:ERG | None | Initial biopsy |
| Urine | |||
| ExoDx Prostate Intelliscore | PCA3, ERG, SPDEF mRNA | None | Initial biopsy Repeat biopsy |
| MiR Sentinel | Small non-coding RNAs | None | Mixed |
| Tissue | |||
| Confirm MDx | Hypermethylation of GSTP1, APC, RASSF1 | None | Repeat biopsy |
(Abbreviations: DRE, digital rectal exam; fPSA, free PSA; iPSA, intact PSA; mRNA, messenger ribonucleic acid; PSA, prostate-specific antigen; SNP, single-nucleotide polymorphism.)
IsoPSA was not included in the initial literature search; however, it was identified on a secondary targeted search and included here for completeness.
Note: Please see Supplementary References for references to these assays
18. For patients with a PSA > 50 ng/mL and no clinical concerns for infection or other cause for increased PSA (e.g., recent prostate instrumentation), clinicians may omit a prostate biopsy in cases where biopsy poses significant risk or where the need for prostate cancer treatment is urgent (e.g., impending spinal cord compression). (Expert Opinion)
For patients with a PSA > 50 ng/mL and no evidence of inflammation, infection, recent instrumentation or catheterization, the likelihood of high-grade prostate cancer has been estimated to be as high as 98.5%.14 Therefore, in situations where biopsy may be risky (e.g., anticoagulation, significant comorbidity, frailty) or delay urgent treatment (e.g., spinal cord compromise from metastases), immediate biopsy can be delayed or omitted. The extremely high risk for prostate cancer should be shared with the patient, and SDM should be used to decide whether to omit an immediate prostate biopsy. This recommendation does not exclude the potential to proceed with biopsy or other prostate cancer evaluation, if deemed clinically appropriate. In addition, it does not obviate the need for biopsy later (e.g., required for treatment, insurance, genetic testing). Imaging to establish extent of disease or confirm metastasis may be helpful if an immediate biopsy is not performed.
Repeat Biopsy
19. Clinicians should communicate with patients following biopsy to review biopsy results, reassess risk of undetected or future development of GG2+ disease, and mutually decide whether to discontinue screening, continue screening, or perform adjunctive testing for early reassessment of risk. (Clinical Principle)
20. Clinicians should not discontinue prostate cancer screening based solely on a negative prostate biopsy. (Strong Recommendation; Evidence Level: Grade C)
21. After a negative biopsy, clinicians should not solely use a PSA threshold to decide whether to repeat the biopsy. (Strong Recommendation; Evidence Level: Grade B)
22. If the clinician and patient decide to continue screening after a negative biopsy, clinicians should re-evaluate the patient within the normal screening interval (two to four years) or sooner, depending on risk of clinically significant prostate cancer and life expectancy. (Clinical Principle)
23. At the time of re-evaluation after negative biopsy, clinicians should use a risk assessment tool that incorporates the protective effect of prior negative biopsy. (Strong Recommendation; Evidence Level: Grade B)
Following a prostate biopsy, clinicians should share biopsy results with patients and make recommendations for further follow-up. Routine management after a negative biopsy would be resumption of screening. The timing of the next evaluation should mirror the standard screening interval, such that a patient should be re-evaluated within two to four years or sooner, typically with a PSA.
Previous biopsy reduces the risk of identifying GG2+ disease on subsequent biopsy and should be considered in decisions about further management. However, the protective effect of a negative biopsy subsides over time since prior biopsy. Patients with a prior negative biopsy remain at risk for undetected or subsequent development of GG2+ disease. The systematic review performed for this guideline showed that 5% to 25% of patients who undergo a subsequent biopsy in the short term are diagnosed with GG2+ disease. (See Guideline for complete list of included studies) Additionally, over a 20-year time horizon, the risk of prostate cancer mortality ranges from 1.4% to 5.2%.15, 16 Therefore, a negative biopsy alone should not be used to justify discontinuation of prostate cancer screening.
PSA level alone should not be used to decide whether to repeat the prostate biopsy in patients with a previous negative biopsy.17 While PSA does factor into risk calculation, it should not be used exclusively to justify repeat biopsy, especially if the original biopsy was prompted by an elevated PSA, because this can result in repeated unnecessary biopsies. If concern remains elevated for GG2+ based on PSA density, previous MRI findings, or other factors, the clinician and patient may consider adjunctive testing (blood, urine, or tissue tests), or MRI (if not previously performed) to further risk stratify the patient and guide further management.
The likelihood of identifying GG2+ disease on subsequent biopsy has been associated with several factors, including age, Black ancestry, total PSA, percent free PSA, PSA density, abnormal DRE findings, presence of germline mutations, pathology findings on prior biopsy (e.g., atypical intraductal proliferation (AIP)), results of available adjunctive testing, number of cores taken at initial biopsy, MRI findings, planned method of subsequent biopsy (e.g., number of cores, saturation, template mapping), and family history.
Given the multiple factors involved in computing the risk of GG2+ disease, the Panel recommends use of a risk calculator that incorporates standard factors, with or without additional factors.
24. After a negative initial biopsy in patients with low probability for harboring GG2+ prostate cancer, clinicians should not reflexively perform biomarker testing. (Clinical Principle)
The goal of early detection is to identify patients at high risk for harboring GG2+ prostate cancer. While biomarkers may improve the capacity to identify patients at risk for high-grade disease, these tests provide the probability of disease or high-grade disease. In patients with a negative biopsy, and low probability for GG2+ disease, it is unlikely that additional biomarker tests will be informative.
25. After a negative biopsy, clinicians may use blood-, urine-, or tissue-based biomarkers selectively for further risk stratification if results are likely to influence the decision regarding repeat biopsy or otherwise substantively change the patient’s management. (Conditional Recommendation; Evidence Level: Grade C)
Blood-, urine-, or tissue-based biomarkers may provide additional information for risk stratification in patients with a prior negative biopsy and ongoing suspicion for GG2+ prostate cancer. Several biomarkers (see Table 2) have been developed and reported, with varying performance characteristics. These tests present percentage risk of biopsy-detectable disease (and/or GG2+), and it is up to the clinician and patient to decide on the threshold for proceeding with a biopsy, with consideration given to the performance metrics of the test. Moreover, how to integrate the use of these tests with mpMRI in prostate cancer early detection paradigms is yet to be studied comprehensively. It is imperative that clinicians are familiar with biomarkers, understand what information or data each test provides, and consider whether additional information will impact management decisions before ordering a test.
26. In patients with focal (one core) HGPIN on biopsy, clinicians should not perform immediate repeat biopsy. (Moderate Recommendation; Evidence Level: Grade C)
The risk of cancer detection following a diagnosis of HGPIN has evolved. Early reports that utilized less than 12-core systematic sampling often found a high risk of undetected prostate cancer.18, 19 However, contemporary studies indicate a 20% to 30% risk of any cancer detected (not just high-grade) in subsequent biopsies,20–22 which is the same risk following an initial benign biopsy. As such, immediate repeat biopsy is not recommended for patients with a diagnosis of focal HGPIN.23 Nonetheless, routine follow up is warranted.
27. In patients with multifocal HGPIN, clinicians may proceed with additional risk evaluation, guided by PSA/DRE and mpMRI findings. (Expert Opinion)
Few studies on the risk of prostate cancer following an initial diagnosis of HGPIN have focused on multifocal HGPIN (e.g., HGPIN in ≥ 2 cores). More recent data with repeat biopsy done with mpMRI guidance demonstrate that in approximately 25% of patients with previous multifocal HGPIN, serum PSA and/or DRE normalize after the biopsy.24 Thus, a recommendation to repeat a prostate biopsy after HGPIN should be based on PSA and DRE evolution, and mpMRI findings. Due to a lack of data, repeat prostate biopsy should not be recommended solely because of a previous diagnosis of HGPIN, even if multifocal.
28. In patients with ASAP, clinicians should perform additional testing. (Expert Opinion)
29. In patients with AIP, clinicians should perform additional testing. (Expert Opinion)
In routine pathology reports, ASAP is synonymous with a small focus (or foci) of atypical glands suspicious, but not definitive, for a diagnosis of carcinoma.25 An ASAP finding alone on needle biopsy is associated with a 30% to 50% risk of prostate cancer detection on repeat biopsy,19, 20, 22, 23, 26–28 with approximately 10% to 20% of these being GG2+.19, 26–28 Given these risks, additional testing should be considered following an ASAP diagnosis, which may include repeat systematic needle biopsy with consideration of mpMRI +/− targeted biopsy, PSA, as well as urine, or serum biomarkers.
AIP describes lesions with greater architectural complexity and/or cytologic atypia than would be expected in HGPIN but lacking definitive criteria for the diagnosis of intraductal carcinoma (IDC-P).29, 30 Although there are no prospective studies or those with extended follow up, available data suggest a close association of AIP with unsampled IDC-P.29, 30 Given these associations, a diagnosis of AIP as either the sole finding or together with only GG1 cancer, warrants additional testing, which may include early repeat systematic needle biopsy or MRI +/− targeted biopsy. The timing of additional testing should be based on reassessment of risk and SDM.
30. In patients undergoing repeat biopsy with no prior prostate MRI, clinicians should obtain a prostate MRI prior to biopsy. (Strong Recommendation; Evidence Level: Grade C)
In patients with a prior negative systematic biopsy, MRI will show a suspicious target in 36% to 90% of patients, and a biopsy directed to the target will be positive in 37% to 66% of patients,31–33 with GG2+ cancer in 21% to 60% of patients.31–33 Given the substantial rates of suspicious target identification and positive predictive value (PPV) for GG2+ disease in the repeat biopsy setting, an mpMRI is recommended if there was no prior MRI.
31. In patients with indications for a repeat biopsy who do not have a suspicious lesion on MRI, clinicians may proceed with a systematic biopsy. (Conditional Recommendation; Evidence Level: Grade B)
Repeat biopsy should be used judiciously after an initial negative biopsy as repeat biopsy detects fewer and less lethal cancers. Medicare data show 38% of patients with an initial negative biopsy of the prostate undergo a repeat biopsy within 5 years, and the percentage of positive biopsies falls from 34% for the first biopsy to 25% for the second.34 Nevertheless, many patients have indications for repeat biopsy. Factors that may identify patients likely to have clinically significant prostate cancer after a negative biopsy and a negative MRI include a PSA density > 0.15 ng/mL,35 a PHI density value > 0.44,36 or a PSA velocity of 0.27 ng/mL/year or greater.37 MRI can be an important factor in the decision to perform a repeat biopsy, although a meta-analysis of 29 eligible studies with 8,503 participants38 suggested mpMRI misses 13% of all cancers.
32. In patients undergoing repeat biopsy and who have a suspicious lesion on MRI, clinicians should perform targeted biopsies of the suspicious lesion and may also perform a systematic template biopsy. (Moderate Recommendation [targeted biopsies]/ Conditional Recommendation [systematic template biopsy]; Evidence Level: Grade C)
In the repeat biopsy setting with targeted and systematic biopsy, the frequency of cancer found in systematic biopsy samples range from 5% to 10% across multiple studies.10, 39, 40 While these results suggest a combined biopsy with systematic and targeted cores optimizes cancer yield, such an approach entails obtaining a larger number of cores, which may increase patient discomfort and other biopsy-associated complications,41, 42 and the apparent incremental yield of off-target biopsy samples may be influenced by the sampling error associated with software image registration at targeted biopsy.43
Biopsy Technique
33. Clinicians may use software registration of MRI and ultrasound images during fusion biopsy, when available. (Expert Opinion)
Targeted prostate biopsy of a visible lesion on mpMRI can be performed using software-based registration of mpMRI images and real-time ultrasound or cognitive registration. Other than in one randomized control trial (RCT)44 where software-based registration demonstrated better cancer detection rate (CDR) compared with cognitive registration (33.3% versus 19.0%; p=0.016), both approaches have been shown to have similar CDR in multiple studies (see Guideline for full references), inclusive of an RCT showing no difference in CDR of software-based versus cognitive fusion or in-bore MRI targeted biopsy.45 Nonetheless, use of software registration facilitates the fusion of multiple MRI and ultrasound images in two to three planes, allowing for the creation of a composite image that provides a more comprehensive view of the target lesion. Clinicians who adopt the cognitive fusion technique exclusively should undergo advanced training in MRI interpretation to optimize cancer detection.
34. Clinicians should obtain at least two needle biopsy cores per target in patients with suspicious prostate lesion(s) on MRI. (Moderate Recommendation; Evidence Level: Grade C)
The optimal number of biopsy cores per MRI target may differ based on multiple factors including patient characteristics (e.g., age, PSA, biopsy naïve versus prior biopsy), target characteristics (e.g., size, location, PI-RADS classification), and biopsy approach/technique (e.g., software fusion versus cognitive fusion, transrectal versus transperineal).46 In general, higher number of biopsy cores per target improves the CDR, at the potential expense of increased complication rate and time.47 However, the incremental value in cancer detection is diminished after obtaining more than three cores per target.47
35. Clinicians may use either a transrectal or transperineal biopsy route when performing a biopsy. (Conditional Recommendation; Evidence Level: Grade C)
In patients with a suspicion for GG2+ prostate cancer who are undergoing biopsy, the CDRs associated with transrectal versus transperineal biopsy route are not significantly different.48 There is some suggestion that transperineal biopsy may detect anterior and apical cancers at a higher rate; however, prospective, randomized data are lacking and existing data are contradictory.49 Recent meta-analyses and retrospective reviews of single center data suggest a lower risk of infection with the transperineal approach; however, prospective, randomized data are lacking to make a definitive conclusion.49 Use of transperineal biopsies may have some value in patients who have experienced infectious complications with a prior biopsy, are at higher risk for biopsy-related infection, or have anterior lesions that may not be as easily accessible transrectally. Trials in this space are ongoing. On the other hand, use of transrectal approach may be appropriate in certain situations (e.g., patient preference/comfort, patient cannot be placed into the lithotomy position, clinician training/experience or lack of appropriate equipment for the transperineal approach). Moreover, use of adjunctive measures (e.g., rectal swab cultures, augmented antibiotic approaches) to reduce sepsis for a transrectal biopsy approach have also been shown to reduce sepsis.50
Future Directions
While we have seen increasing data to support greater specificity in prostate cancer detection, there remain many areas where future data may help guide future practices. There are a plethora of biomarkers to assess the likelihood of high-grade prostate cancer; however, little evidence exists on comparative effectiveness, how they complement each other, or how stepwise algorithms perform. Further, MRI imaging of the prostate, while commonly utilized, has not been shown to impact meaningful long-term outcomes such as cancer-specific mortality. Finally, use of transperineal versus transrectal biopsy varies widely and questions regarding diagnostic capabilities, risks of infection, and the value of antibiotic prophylaxis remain unanswered.
Supplementary Material
Abbreviations
- 95% CI
95% confidence interval
- APC
Adenomatous polyposis coli gene
- AS
Active surveillance
- ASAP
Atypical small acinar proliferation
- AUA
American Urological Association
- CDR
Cancer detection rate
- CTSD
Cathepsin D
- DLX1
Distal-Less Homeobox 1 gene
- DRE
Digital rectal exam
- ERSPC
European randomized study of screening for prostate cancer
- fPSA
Free prostate-specific antigen
- GG
Grade group
- GRADE
Grading of Recommendations Assessment, Development, and Evaluation
- GSTP1
Glutathione S-transferase P1–1
- HGPIN
High-grade prostatic intraepithelial neoplasia
- hk2
Human kallikrein 2
- HOXC6
Homeobox C6-gene
- IDC-P
Intraductal carcinoma of prostate
- iPSA
Intact PSA
- MIC1
Macrophage inhibitory factor 1
- mpMRI
Multi-parametric magnetic resonance imaging
- MPS
MyProstateScore
- MRI
Magnetic resonance imaging
- mRNA
Messenger ribonucleic acid
- MSMB
Microseminoprotein-beta
- NND
Number needed to diagnose
- NNS
Number needed to screen
- p2PSA
[−2]pro-prostate-specific antigen
- PBCG
Prostate biopsy collaborative group
- PCA3
Prostate cancer antigen 3 gene
- PCPT
Prostate cancer prevention trial
- PHI
Prostate health index
- PI-RADS
Prostate Imaging Reporting & Data System
- PLCO
Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial
- PPV
Positive predictive value
- PSA
Prostate-specific antigen
- RASSF1
Ras Association Domain Family Member 1
- RCT
Randomized control trial
- RR
Relative risk
- SDM
Shared decision-making
- SNPs
Single-nucleotide polymorphisms
- SPDEF
SAM pointed domain containing ETS transcriptional factor
- SSA
Social Security Administration
- STHLM-3
Stockholm
- SUO
Society of Urologic Oncology
- THBS1
Thrombospondin-1
- TMPRSS2:ERG
Transmembrane serine protease 2-ETS-related gene
Contributor Information
John T. Wei, University of Michigan.
Daniel Barocas, Vanderbilt University.
Sigrid Carlsson, Memorial Sloan Kettering Cancer Center.
Fergus Coakley, Oregon Health & Science University.
Scott Eggener, University of Chicago.
Ruth Etzioni, Fred Hutchinson Cancer Center.
Samson W. Fine, Memorial Sloan Kettering Cancer Center.
Misop Han, Johns Hopkins University.
Sennett K. Kim, American Urological Association
Erin Kirkby, American Urological Association.
Badrinath R. Konety, Allina Health.
Martin Miner, Brown University.
Kelvin Moses, Vanderbilt University.
Merel G. Nissenberg, National Alliance of State Prostate Cancer Coalitions.
Peter A. Pinto, National Institutes of Health.
Simpa S. Salami, University of Michigan.
Lesley Souter, Nomadic E.B.M Methodology.
Ian M. Thompson, CHRISTUS Health.
Daniel W. Lin, University of Washington.
References
- 1.Wei JT, Feng Z, Partin AW et al. : Can urinary pca3 supplement psa in the early detection of prostate cancer? Journal of Clinical Oncology 2014; 32: 4066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eastham JA, Boorjian SA and Kirkby E: Clinically localized prostate cancer: Aua/astro guideline. J Urol 2022; 208: 505. [DOI] [PubMed] [Google Scholar]
- 3.Kasivisvanathan V, Rannikko AS, Borghi M et al. : Mri-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 2018; 378: 1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drost FH, Osses DF, Nieboer D et al. : Prostate mri, with or without mri-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database of Systematic Reviews 2019; 4: CD012663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cata E, Andras I, Ferro M et al. : Systematic sampling during mri-us fusion prostate biopsy can overcome errors of targeting-prospective single center experience after 300 cases in first biopsy setting. Translational Andrology & Urology 2020; 9: 2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng Y, Qi F, Liang L et al. : Use of prostate systematic and targeted biopsy on the basis of bi-parametric magnetic resonance imaging in biopsy-naive patients. Journal of Investigative Surgery 2020: 1. [DOI] [PubMed] [Google Scholar]
- 7.Coker MA, Glaser ZA, Gordetsky JB et al. : Targets missed: Predictors of mri-targeted biopsy failing to accurately localize prostate cancer found on systematic biopsy. Prostate Cancer Prostatic Dis 2018; 21: 549. [DOI] [PubMed] [Google Scholar]
- 8.Brisbane WG, Priester AM, Ballon J et al. : Targeted prostate biopsy: Umbra, penumbra, and value of perilesional sampling. Eur Urol 2022; 82: 303. [DOI] [PubMed] [Google Scholar]
- 9.Kim YJ, Huh JS and Park KK: Effectiveness of bi-parametric mr/us fusion biopsy for detecting clinically significant prostate cancer in prostate biopsy naive men. Yonsei Medical Journal 2019; 60: 346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahdoot M, Wilbur AR, Reese SE et al. : Mri-targeted, systematic, and combined biopsy for prostate cancer diagnosis. New England Journal of Medicine 2020; 382: 917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hugosson J, Månsson M, Wallström J et al. : Prostate cancer screening with psa and mri followed by targeted biopsy only. N Engl J Med 2022; 387: 2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sathianathen NJ, Omer A, Harriss E et al. : Negative predictive value of multiparametric magnetic resonance imaging in the detection of clinically significant prostate cancer in the prostate imaging reporting and data system era: A systematic review and meta-analysis. European Urology 2020; 78: 402. [DOI] [PubMed] [Google Scholar]
- 13.Eyrich NW, Morgan TM and Tosoian JJ: Biomarkers for detection of clinically significant prostate cancer: Contemporary clinical data and future directions. Transl Androl Urol 2021; 10: 3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gerstenbluth RE, Seftel AD, Hampel N et al. : The accuracy of the increased prostate specific antigen level (greater than or equal to 20 ng./ml.) in predicting prostate cancer: Is biopsy always required? Journal of Urology 2002; 168: 1990. [DOI] [PubMed] [Google Scholar]
- 15.Palmstedt E, Mansson M, Franlund M et al. : Long-term outcomes for men in a prostate screening trial with an initial benign prostate biopsy: A population-based cohort. Eur Urol Oncol 2019; 2: 716. [DOI] [PubMed] [Google Scholar]
- 16.Klemann N, Roder MA, Helgstrand JT et al. : Risk of prostate cancer diagnosis and mortality in men with a benign initial transrectal ultrasound-guided biopsy set: A population-based study. Lancet Oncol 2017; 18: 221. [DOI] [PubMed] [Google Scholar]
- 17.Ankerst DP, Straubinger J, Selig K et al. : A contemporary prostate biopsy risk calculator based on multiple heterogeneous cohorts. Eur Urol 2018; 74: 197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herawi M, Kahane H, Cavallo C et al. : Risk of prostate cancer on first re-biopsy within 1 year following a diagnosis of high grade prostatic intraepithelial neoplasia is related to the number of cores sampled. J Urol 2006; 175: 121. [DOI] [PubMed] [Google Scholar]
- 19.Tosoian JJ, Alam R, Ball MW et al. : Managing high-grade prostatic intraepithelial neoplasia (hgpin) and atypical glands on prostate biopsy. Nat Rev Urol 2018; 15: 55. [DOI] [PubMed] [Google Scholar]
- 20.Kim TS, Ko KJ, Shin SJ et al. : Multiple cores of high grade prostatic intraepithelial neoplasia and any core of atypia on first biopsy are significant predictor for cancer detection at a repeat biopsy. Korean Journal of Urology 2015; 56: 796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel P, Nayak JG, Biljetina Z et al. : Prostate cancer after initial high-grade prostatic intraepithelial neoplasia and benign prostate biopsy. Canadian Journal of Urology 2015; 22: 8056. [PubMed] [Google Scholar]
- 22.Wiener S, Haddock P, Cusano J et al. : Incidence of clinically significant prostate cancer after a diagnosis of atypical small acinar proliferation, high-grade prostatic intraepithelial neoplasia, or benign tissue. Urology 2017; 110: 161. [DOI] [PubMed] [Google Scholar]
- 23.Oderda M, Rosazza M, Agnello M et al. : Natural history of widespread high grade prostatic intraepithelial neoplasia and atypical small acinar proliferation: Should we rebiopsy them all? Scandinavian Journal of Urology 2021; 55: 129. [DOI] [PubMed] [Google Scholar]
- 24.Morote J, Schwartzmann I, Celma A et al. : The current recommendation for the management of isolated high-grade prostatic intraepithelial neoplasia. BJU International 2021; 10: 10. [DOI] [PubMed] [Google Scholar]
- 25.Schlesinger C, Bostwick DG and Iczkowski KA: High-grade prostatic intraepithelial neoplasia and atypical small acinar proliferation: Predictive value for cancer in current practice. Am J Surg Pathol 2005; 29: 1201. [DOI] [PubMed] [Google Scholar]
- 26.Leone A, Gershman B, Rotker K et al. : Atypical small acinar proliferation (asap): Is a repeat biopsy necessary asap? A multi-institutional review. Prostate Cancer & Prostatic Diseases 2016; 19: 68. [DOI] [PubMed] [Google Scholar]
- 27.Warlick C, Feia K, Tomasini J et al. : Rate of gleason 7 or higher prostate cancer on repeat biopsy after a diagnosis of atypical small acinar proliferation. Prostate Cancer & Prostatic Diseases 2015; 18: 255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dorin RP, Wiener S, Harris CD et al. : Prostate atypia: Does repeat biopsy detect clinically significant prostate cancer? Prostate 2015; 75: 673. [DOI] [PubMed] [Google Scholar]
- 29.Shah RB, Yoon J, Liu G et al. : Atypical intraductal proliferation and intraductal carcinoma of the prostate on core needle biopsy: A comparative clinicopathological and molecular study with a proposal to expand the morphological spectrum of intraductal carcinoma. Histopathology 2017; 71: 693. [DOI] [PubMed] [Google Scholar]
- 30.Shah RB, Nguyen JK, Przybycin CG et al. : Atypical intraductal proliferation detected in prostate needle biopsy is a marker of unsampled intraductal carcinoma and other adverse pathological features: A prospective clinicopathological study of 62 cases with emphasis on pathological outcomes. Histopathology 2019; 75(3): 346. [DOI] [PubMed] [Google Scholar]
- 31.Arsov C, Rabenalt R, Blondin D et al. : Prospective randomized trial comparing magnetic resonance imaging (mri)-guided in-bore biopsy to mri-ultrasound fusion and transrectal ultrasound-guided prostate biopsy in patients with prior negative biopsies. European Urology 2015; 68: 713. [DOI] [PubMed] [Google Scholar]
- 32.Sonn GA, Chang E, Natarajan S et al. : Value of targeted prostate biopsy using magnetic resonance-ultrasound fusion in men with prior negative biopsy and elevated prostate-specific antigen. European Urology 2014; 65: 809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meermeier NP, Foster BR, Liu JJ et al. : Impact of direct mri-guided biopsy of the prostate on clinical management. AJR American Journal of Roentgenology 2019; 213: 371. [DOI] [PubMed] [Google Scholar]
- 34.Welch HG, Fisher ES, Gottlieb DJ et al. : Detection of prostate cancer via biopsy in the medicare-seer population during the psa era. Journal of the National Cancer Institute 2007; 99: 1395. [DOI] [PubMed] [Google Scholar]
- 35.Distler FA, Radtke JP, Bonekamp D et al. : The value of psa density in combination with pi-rads for the accuracy of prostate cancer prediction. J Urol 2017; 198: 575. [DOI] [PubMed] [Google Scholar]
- 36.Druskin SC, Tosoian JJ, Young A et al. : Combining prostate health index density, magnetic resonance imaging and prior negative biopsy status to improve the detection of clinically significant prostate cancer. BJU International 2018; 121: 619. [DOI] [PubMed] [Google Scholar]
- 37.Kamal O, Comerford J, Foster BR et al. : Intermediate-term oncological outcomes after a negative endorectal coil multiparametric mri of the prostate in patients without biopsy proven prostate cancer. Clinical Imaging 2022; [DOI] [PubMed] [Google Scholar]
- 38.Zhen L, Liu X, Yegang C et al. : Accuracy of multiparametric magnetic resonance imaging for diagnosing prostate cancer: A systematic review and meta-analysis. BMC Cancer 2019; 19: 1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patel N, Cricco-Lizza E, Kasabwala K et al. : The role of systematic and targeted biopsies in light of overlap on magnetic resonance imaging ultrasound fusion biopsy. European Urology Oncology 2018; 1: 263. [DOI] [PubMed] [Google Scholar]
- 40.Salami SS, Ben-Levi E, Yaskiv O et al. : In patients with a previous negative prostate biopsy and a suspicious lesion on magnetic resonance imaging, is a 12-core biopsy still necessary in addition to a targeted biopsy? BJU International 2015; 115: 562. [DOI] [PubMed] [Google Scholar]
- 41.Loeb S, Carter HB, Berndt SI et al. : Is repeat prostate biopsy associated with a greater risk of hospitalization? Data from seer-medicare. Journal of Urology 2013; 189: 867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fujita K, Landis P, McNeil BK et al. : Serial prostate biopsies are associated with an increased risk of erectile dysfunction in men with prostate cancer on active surveillance. J Urol 2009; 182: 2664. [DOI] [PubMed] [Google Scholar]
- 43.Hale GR, Czarniecki M, Cheng A et al. : Comparison of elastic and rigid registration during magnetic resonance imaging/ultrasound fusion-guided prostate biopsy: A multi-operator phantom study. J Urol 2018; 200: 1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Izadpanahi MH, Elahian A, Gholipour F et al. : Diagnostic yield of fusion magnetic resonance-guided prostate biopsy versus cognitive-guided biopsy in biopsy-naive patients: A head-to-head randomized controlled trial. Prostate Cancer & Prostatic Diseases 2021; 27: 27. [DOI] [PubMed] [Google Scholar]
- 45.Wegelin O, Exterkate L, van der Leest M et al. : The future trial: A multicenter randomised controlled trial on target biopsy techniques based on magnetic resonance imaging in the diagnosis of prostate cancer in patients with prior negative biopsies. European Urology 2019; 75: 582. [DOI] [PubMed] [Google Scholar]
- 46.Sonmez G, Demirtas T, Tombul ST et al. : What is the ideal number of biopsy cores per lesion in targeted prostate biopsy? Prostate International 2020; 8: 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Subramanian N, Recchimuzzi DZ, Xi Y et al. : Impact of the number of cores on the prostate cancer detection rate in men undergoing in-bore magnetic resonance imaging-guided targeted biopsies. J Comput Assist Tomogr 2021; 45: 203. [DOI] [PubMed] [Google Scholar]
- 48.Ristau BT, Allaway M, Cendo D et al. : Free-hand transperineal prostate biopsy provides acceptable cancer detection and minimizes risk of infection: Evolving experience with a 10-sector template. Urol Oncol 2018; 36: 528.e15. [DOI] [PubMed] [Google Scholar]
- 49.Meyer AR, Mamawala M, Winoker JS et al. : Transperineal prostate biopsy improves the detection of clinically significant prostate cancer among men on active surveillance. J Urol 2021; 205: 1069. [DOI] [PubMed] [Google Scholar]
- 50.Womble PR, Linsell SM, Gao Y et al. : A statewide intervention to reduce hospitalizations after prostate biopsy. J Urol 2015; 194: 403. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


