Abstract
Objective
We have known that cognitive difficulties are related to functional outcomes in schizophrenia for many years. However, we have only paid attention to potential treatments relatively recently, so implementation has been slow.
Methods
This is a narrative review describing the development of cognitive remediation treatments to improve cognitive skills and their effects on functioning. It also reviews the types of cognitive remediation with some evidence on their effects.
Results
Models of treatment have now been clarified and have led to a landmark paper by cognitive remediation experts around the world on the ingredients of cognitive remediation to produce the most benefit. This expert judgement on good clinical practice was justified by a large meta-analysis that supported the extra benefit of the four ingredients: an active therapist, massed practice of cognitive skills, the teaching of cognitive strategies and additional rehabilitation to transfer skills to real life.
Conclusion
Although there is evidence of efficacy and of the beneficial therapy ingredients there is little implementation of cognitive remediation, so the establishment of cognitive remediation into mental health services needs an implementation pathway.
Keywords: Schizophrenia, Psychotic disorder, Cognition, Rehabilitation
INTRODUCTION
A little history
Cognitive problems were part of the diagnosis of schizophrenia from when the name was first coined by both Bleuler [1] and Kraepelin (1893 [2]). We have known about cognitive difficulties in people with a diagnosis of schizophrenia for more than 50 years. McGhie and Chapman [3] reported on the attention and concentration difficulties that meant they had difficulty in keeping track of conversations. Much later these same issues are being reported by people in the early stages of psychosis not just at times when they are having an acute episode but in-between these episodes [4]. We also know that these cognitive difficulties appear early and do not seem to change very much over the lifetime and although domains of cognitive difficulties differ between individuals most individuals have poorer cognition than might be expected from the social conditions and family resources [5,6].
The recognition that cognitive problems did not change over time suggested that they were immutable, so no specific therapy was developed. But soon came the recognition that cognitive difficulties were related to real life outcomes and could predict functioning even when there were adequate recovery programs in place [7]. For instance, Bell and Bryson [8] at Yale have a good rehabilitation program to help people with a diagnosis of schizophrenia find jobs and they reported that cognitive problems predict the outcomes from these programs, similarly, Mueser and colleagues [9] demonstrated that the acquisition of skills following social skills training is affected by cognitive impairments, especially memory problems. Finally, it has become more obvious that cognitive difficulties are related to the level independence gained and this affects the costs to services. In a study of local services where cognitive difficulties had been measured, Patel and colleagues [10] discovered that cognition was the largest predictor of costs.
All these associations moved cognitive impairment up the agenda and specifically the potential of a therapy to improve cognition and therefore improve functional outcome. However, all was not plain sailing. Several articles had appeared in an issue of Schizophrenia Bulletin with titles such as “Cognitive rehabilitation for schizophrenia: Is it possible? Is it necessary?” [11] and “Cognitive Remediation in schizophrenia: Proceed … with caution!” [12] suggesting that the clinical academic community were not hopeful about the outcome of this endeavour. Part of this scepticism was a result of cognitive impairments being considered vulnerability factors for a diagnosis of schizophrenia and so were part of the disorder. There is a lot of evidence, both historical and current, showing that cognitive difficulties are noticeable years before the onset of psychosis [13], so some clinicians and academics thought that it was going to be difficult to change the trajectory of cognition or the cognitive decline often seen in those who develop psychosis. Since the development of cognitive remediation—a therapy aimed at improving cognition with the assumption that this will aid functional outcome—there have also been false claims made for cognitive remediation therapy which continues to fuel the earlier scepticism of its worth.
METHODS
The review considers trials and meta-analyses as well as expert opinion to produce a narrative concentrating on the development of cognitive remediation, the breadth of the therapy, its effectiveness and the models of action of the effects. The review also covers what is needed to implement therapy.
RESULTS
Cognitive remediation therapies
For a therapy to be considered as cognitive remediation it must be an intervention targeting cognitive deficit using scientific principles of learning with the ultimate goal of improving functional outcomes. Its effectiveness is enhanced when provided in a context (formal or informal) that provides support and opportunity for extending everyday functioning from the Cognitive Remediation Experts Workshop in 2012. Wykes and Reeder [14] suggested a list of ingredients that might be helpful. These include: 1) extensive practice–as we know that individuals with a diagnosis of schizophrenia often have poor memories so making sure that practice is more extensive means that learning in one session is more likely to transfer over to the next session. 2) Errorless learning–reducing the number of errors keeps reinforcement high and learning accurate so is likely to increase engagement in therapy. 3) Verbal monitoring–by repeating the instructions for the task at first overtly then covertly, it avoids forgetting the instructions and increases attention to the task. 4) Scaffolding means making tasks manageable but still a challenge so that cognitive skills are stretched. 5) Teaching Strategies explicitly so that they are not only developed but can be used in other tasks.
One meta-analysis has shown that it makes no difference whether a strategic or non-strategic approach is employed to get a cognitive benefit, but only a strategic approach provides a benefit for functioning [15]. This study also demonstrated that adding a rehabilitation program alongside cognitive remediation with a strategic approach, doubles the functioning benefit. Subsequently McGurk and colleagues [16] discovered that adding cognitive remediation to supported employment also helped to prevent failure in those who had already failed a course of supported employment and so provided evidence that rehabilitation without cognitive remediation might waste both time and resources. Bowie and colleagues [17] investigated what was the added benefit to functioning of adding cognitive remediation to two other interventions. They demonstrated that cognitive remediation alone improves cognition but had only a small effect on employment and community skills. Providing skills training alone had little effect on any outcome, but when it was added to the other skills training, there was an improvement in cognition, employment, and community skills. There are, data in people with first episode psychosis showing that adding cognitive remediation to cognitive behavior therapy (CBTp) reduced the number of sessions of CBTp needed to achieve the same symptom reduction, and cognitive change was associated with this symptom reduction [18]. There is also evidence that adding exercise to cognitive remediation also boosts functioning [19]. So, cognitive remediation alone, if it includes teaching strategies, improves functioning and that adding it to many other very different interventions boosts the benefits of those interventions and therefore saves costs.
Trials of Cognitive Remediation (CR) therapies have been carried out across the globe and there are many meta-analyses that show that cognitive remediation has an effect on cognition, functioning and occasionally on symptoms after the end of therapy and some that also show a durable benefit [15,20,21]. Recently there have also been studies showing effects on negative symptoms including further meta-analyses [22] and arguments for including cognitive remediation for negative symptoms into guidance [23]. But there have also been negative studies, tests of cognitive remediation that did not reveal any benefit. For instance, Dickinson et al. [24], and Gomar et al. [25] both found that their cognitive remediation programs produced no benefits. These are important studies as they may tell us something about how to provide cognitive remediation that does produce a benefit. Both studies included older participants, much older than other studies, and the Gomar study had very little support from a therapist. Both also provided two forms of cognitive remediation that had little evidence of potential benefit. What these studies tell us is that we need to develop CR treatments that are tested across the age range as older people may require more sessions and more support from a therapist.
In general, the benefits of CR have not changed over the ten years of meta-analyses, but their results have taken a considerable time to be favorably considered by guidance panels. In 2023 there were at least eight countries with cognitive remediation in their guidance, but they often differed from each other. The German and European Psychiatric Association guidance described the evidence of benefits as very high and recommended it should be offered to those who had some cognitive difficulties. In comparison the American Psychiatric Association and the UK National Institute of Health and Care Excellence both rated the evidence as low and so made CR only a suggestion rather than a recommendation.
Personalisation of therapy
Although we know that CR produces benefits, we do not yet know who benefits the most and when services must decide where to place their resources. One study by Bell et al. [26] from Yale followed up people who had received supported employment, where half had also received cognitive remediation, to investigate whether the boost in employment was still noticeable after two years. They found that the effects had disappeared when considering the whole group, although those with the poorest outcomes still showed a benefit over the longer term.
Type of CR
CBTp is known by its acronym even though some programs may concentrate more on behavior than cognition or vice versa. In contrast CR has many forms and all have been given a different name. So, it is not surprising that this adds to confusion about which to use. We know at least that strategies are important for functioning benefits [15], but apart from that it is unclear what sorts of tasks should be included. For instance, whether the CR needs to be generic (addressing all potential cognitive domains) or specific (only addressing the domains that are the most compromised). Bossert et al. [27], and Franck et al. [28] tested these two types and neither study found a benefit for specific CRs over the generic ones. It is possible that this is due to higher level, more complex, areas of cognitive functioning require lower levels such as attention, short term memory etc. Generic versions might strengthen cognitive domains that were less impaired that allowed a boost to overall cognition. Generic forms also allow the potential for providing positive reinforcement for tasks that require skills that are not so impaired. This would then provide a boost to self-esteem and self-efficacy that will benefit all cognitive tasks. Similarly, Scoriels et al. [29] set out to discover whether auditory or visual training would work better and found that visual training was more efficient at remediating cognitive deficits and symptoms. Importantly their participants were people who were clinically stable and had a diagnosis of schizophrenia, and it may be that this effect is only relevant for that group rather than early psychosis participants who may have a more volatile symptom pattern.
Most programs currently used are provided via a computer, and we do not know how sophisticated they need to be. One Mind PsyberGuide [30] is a free rating service for online and app-based therapies. I used it to assess an old, relatively early phase online therapy (CogPack) against a much more sophisticated one (BrainHQ). The ratings were obviously different for the sophistication of the games, but the evidence of benefits was not much different, with CogPack edging a little ahead.
We also do not yet know what the optimal number of sessions is. Many people quote 20 which is the number of sessions my research team consider as a minimal dose. However, there is little evidence that this number is suitable for all. For instance, 120 sessions can provide no benefit and 20 sessions can provide one [31,32]. So, there is no identified number of sessions for benefit and an optimal dose is likely to be related to personal characteristics and the type of program employed.
Refinement of cognitive remediation
The cognitive remediation experts who drew up the CR definition also looked at the good practice that might achieve benefit and developed a White paper on the characteristics of a CR that would provide improvements [33]. The four characteristics they thought produced benefit are: 1) facilitation by an active therapist, 2) cognitive exercise, 3) procedures to develop problem-solving strategies, and 4) procedures to facilitate transfer to real world functioning.
Using this set of characteristics Vita et al. [34] rated the CR trials on three characteristics as one, cognitive exercises, is included all the cognitive remediation programs. They then carried out a meta-analysis to understand if these characteristics individually or together were important. Over all the trials there was a cognitive and functioning improvement, but his team also found that all three characteristics predicted improved benefit, and when all the characteristics were present, the difference in benefit was statistically significant.
An active therapist is needed
Although an active therapist provides increased benefits, we also need to understand why it might be beneficial. There are several reasons why this might be the case including: 1) improved therapeutic alliance that then affects engagement [35], 2) improved strategy use [36], 3) the therapist is highly valued by the service user [37,38], 4) therapist value affects perceived treatment usefulness [39], and may not only predict engagement in CR but also engagement in other treatments [40].
The effects found in the Vita meta-analysis have also been found by other meta-analyses for cognitive outcomes [20].
The model of remediation–does it just involve boosting cognition?
The current definition of the effects of remediation is that therapy boosts cognition that then leads to functional improvements, but there are few studies that test this model. For instance, Wykes and colleagues [41] in a work quality study investigated whether the cognitive flexibility, memory, or planning improvements lead to work quality benefits. Only planning improvements were related and only accounted for 15% of the variance leaving 85% of the variance unaccounted for. Similarly, Peña and colleagues [42] found only partial mediation of processing speed improvement on functional outcome. A better understanding of the mechanisms of the effects of cognitive remediation on functioning would allow us to adapt the therapy to produce the most durable benefits. Wykes and Spaulding [43] developed a model that has since been expanded (Figure 1). The current model includes most variables known to affect functional outcome–the goal of cognitive remediation. The model provides different pathways that are not mutually exclusive, and individuals could take one or more pathways to achieve benefits. Many benefits in the model are likely to have independent effects, e.g., self-efficacy can have an impact on many other functional outcomes other than the one measured and may be a facilitator of long-term durability. But this means that cognition is not necessarily the driver of all effects and there are potentially other drivers of change that need to be considered within the therapy itself.
Figure 1.
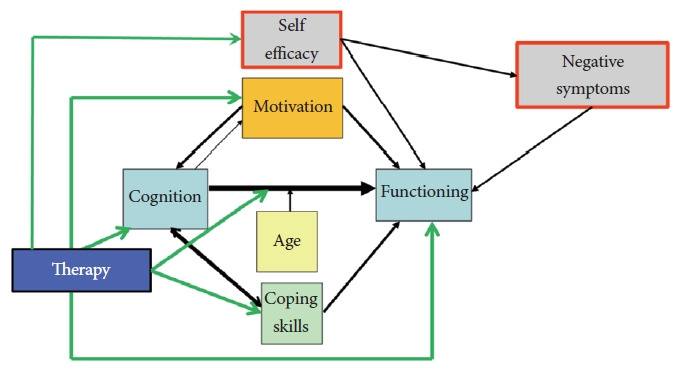
A potential Model of the Mechanism of cognitive remediation therapies. Adapted from Wykes et al. Schizophr Bull 2011;37 (Suppl 2):S80-S90[43], under the terms of the Creative Commons License (CC BY NC).
Metacognition–potential missing link
Metacognition is divided into two strands, metacognitive knowledge, and metacognitive regulation. Metacognitive knowledge consists of understanding your strengths and weaknesses, how different mood states affect cognition and the strategies that are available to the individual. Metacognitive regulation is about when to use problem solving strategies especially for specific types of tasks. This requires self-reflection. We know that using metacognition in education benefits learning [44,45]. It can reduce the time for learning by about 8 months and has durable effects. We also know that when you consider metacognition as a predictor of functioning often the association with cognition disappears or becomes very small. For instance, in a two-year follow-up study of people in early psychosis services Wright et al. [46] discovered that metacognition had an odds ratio of 1.9 on the prediction of being in work or not, with poorer metacognition predicting fewer people in work. Other evidence also supports the potential for metacognition involvement. Best and colleagues [47] compared executive functioning training versus Perceptual processing training. Both were equally good at post treatment, but when assessed at follow-up the executive training improved cognition, functional competence, and community functioning far more than perceptual training. Executive functioning training incorporates self-reflection and the regulation of approaches to problems, in other words trains metacognition. The recognition of the importance of metacognition was first proposed as a pedagogical tool by Wykes and Reeder [14] and was subsequently built into the therapy known as CIRCuiTSTM [48,49] and this program has also been shown to improve metacognition [50]. Importantly this therapy builds both metacognitive knowledge and metacognitive regulation by encouraging self-reflection on tasks and strategies that may be helpful to learning. The software program is also recovery oriented with personal recovery goals designed at the start so that learning on tasks and exercises mimic real world situations which can improve the implementation of learnt skills to the real world.
Implementing cognitive remediation
We investigated the implementation of cognitive remediation into UK National Health Service (NHS) early intervention services in a program of activities to address key barriers, the lack of some evidence as well as understanding the service user perspective and cost-effectiveness. The key issues investigated were: 1) the barriers and facilitators perceived by staff that would need to be optimised for successful implementation. 2) As active therapists are essential for the best effects we need online therapist training for faster roll-out. 3) Satisfaction with the therapy and preferences of staff and patients as if the service users do not like therapy, then the uptake in services is likely to be poor. 4) We need to understand how much therapist time is required for a successful outcome, where the outcome is one used in services. 5) We need evidence that this therapy is cost-effective.
Staff Barriers and facilitators
The main barriers were time and resources as well as understanding whether there is a clinical need. A facilitator was understanding the clinical efficacy of cognitive remediation [51].
Training for therapists
We developed an online program with mixed media and short quizzes as well as an identifiable module structure. The development of the training model was aided by naïve and expert therapists as well as experts in education. We tested whether it was acceptable with naïve therapists and made changes based on their feedback and then evaluated it with more than a 100 people to understand whether we could teach the competences that would allow the therapists to begin their CR provision. We found that most therapists passed the test on the first occasion and that those who dropped out did so early, and usually because of a lack of time for training during their working day [52].
Satisfaction and drop-out
Vita et al. [53] investigated drop-out in cognitive remediation trials as a proxy for acceptability and found that it was only 17% in the cognitive training arms.
How much therapist time is essential
Wykes et al. [54] tested three levels of therapist support: 1) independent where a service user had access to a therapist, but the program was completed at home, 2) group treatment with up to four individuals with one therapist, and 3) face-to-face therapy with one therapist and one service user.
All these active arms were compared to standard care that in UK NHS early intervention services was a high level of support including employment specialists. The main outcome was personal recovery goals as measured by the Goal Attainment Scale, chosen to reflect the care outcomes measured in services. The results demonstrated that both group and face-to-face therapy were successful in improving outcomes [54].
Cost-effectiveness
People with cognitive difficulties are more costly to treat and care for, but we also know that once they have received cognitive remediation the costs of their care decrease [55,56]. But a further question is whether this treatment is cost effective. This is usually assessed through estimations of the costs of improving the measure of Quality Adjusted Life Years (QALY) by one point. Wykes et al. [54] showed that cognitive remediation provided in a group or face-to-face was cost-effective and the overall cost of a QALY was less than £5,000. This figure is below the UK National Institute for Health and Clinical Excellence guidelines to accept a treatment into the UK NHS.
CONCLUSION
Cognitive remediation is effective especially if it includes key drivers such as a therapist and additional rehabilitation. The mechanism of action is still vague although metacognition could be another key characteristic to boost benefits. Although there should continue to be investigations of the potential ingredients of cognitive remediation, given its proven benefits it should be widely available, particularly as it aids personal recovery goals and overall functioning, and individuals are satisfied with the outcomes. Cost benefits are also clear. Implementation of novel treatments requires therapist training as it is an essential ingredient and the resources such as time and access to technology. The technology issues are likely to be overcome relatively quickly with availability increasing soon. Our team at CIRCuiTSTM has now reduced the online training sessions to fit into the time available for professional continuing development to increase the pool of skilled therapists. By advertising the efficacy and clinical need to health care teams will we decrease barriers and increase the likelihood of staff being aware of the likely benefits to their patients. Reducing costs is also important to service providers who need to spread scarce resources. Importantly a recent survey in Australia showed that people with a diagnosis of schizophrenia want this therapy although most had not received it [4]. It is now up to clinical academics to partner with patients to move this therapy into standard care so more can receive its obvious benefits.
Acknowledgments
TW acknowledges her NIHR Senior Investigator award and the support of the NIHR Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the author and not necessarily those of the NIHR or the Department of Health and Social Care.
Footnotes
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Conflicts of Interest
The author has no potential conflicts of interest to disclose.
Funding Statement
None
REFERENCES
- 1.Bleuler E. Dementia praecox or the group of schizophrenias. New York: International Universities Press; 1950. [Google Scholar]
- 2.Falkai P, Rossner MJ, Schulze TG, Hasan A, Brzózka MM, Malchow B, et al. Kraepelin revisited: schizophrenia from degeneration to failed regeneration. Mol Psychiatry. 2015;20:671–676. doi: 10.1038/mp.2015.35. [DOI] [PubMed] [Google Scholar]
- 3.McGhie A, Chapman J. Disorders of attention and perception in early schizophrenia. Br J Med Psychol. 1961;34:103–116. doi: 10.1111/j.2044-8341.1961.tb00936.x. [DOI] [PubMed] [Google Scholar]
- 4.Bryce S, Cheng N, Dalton A, Ojinnaka A, Stainton A, Zbukvic I, et al. Cognitive health treatment priorities and preferences among young people with mental illness: The your mind, your choice survey. Early Interv Psychiatry. 2024;18:94–101. doi: 10.1111/eip.13436. [DOI] [PubMed] [Google Scholar]
- 5.McCleery A, Ventura J, Kern RS, Subotnik KL, Gretchen-Doorly D, Green MF, et al. Cognitive functioning in first-episode schizophrenia: MATRICS consensus cognitive battery (MCCB) profile of impairment. Schizophr Res. 2014;157:33–39. doi: 10.1016/j.schres.2014.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Rheenen TE, Lewandowski KE, Tan EJ, Ospina LH, Ongur D, Neill E, et al. Characterizing cognitive heterogeneity on the schizophrenia-bipolar disorder spectrum. Psychol Med. 2017;47:1848–1864. doi: 10.1017/S0033291717000307. [DOI] [PubMed] [Google Scholar]
- 7.Wykes T, Dunn G. Cognitive deficit and the prediction of rehabilitation success in a chronic psychiatric group. Psychol Med. 1992;22:389–398. doi: 10.1017/s0033291700030336. [DOI] [PubMed] [Google Scholar]
- 8.Bell MD, Bryson G. Work rehabilitation in schizophrenia: does cognitive impairment limit improvement? Schizophr Bull. 2001;27:269–279. doi: 10.1093/oxfordjournals.schbul.a006873. [DOI] [PubMed] [Google Scholar]
- 9.Mueser KT, Bellack AS, Douglas MS, Wade JH. Prediction of social skill acquisition in schizophrenic and major affective disorder patients from memory and symptomatology. Psychiatry Res. 1991;37:281–296. doi: 10.1016/0165-1781(91)90064-v. [DOI] [PubMed] [Google Scholar]
- 10.Patel A, Everitt B, Knapp M, Reeder C, Grant D, Ecker C, et al. Schizophrenia patients with cognitive deficits: factors associated with costs. Schizophr Bull. 2006;32:776–785. doi: 10.1093/schbul/sbl013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bellack AS, Mueser KT. Psychosocial treatment for schizophrenia. Schizophr Bull. 1993;19:317–336. doi: 10.1093/schbul/19.2.317. [DOI] [PubMed] [Google Scholar]
- 12.Hogarty GE, Flesher S. Cognitive remediation in schizophrenia: proceed... with caution! Schizophr Bull. 1992;18:51–57. doi: 10.1093/schbul/18.1.51. [DOI] [PubMed] [Google Scholar]
- 13.Seidman LJ, Cherkerzian S, Goldstein JM, Agnew-Blais J, Tsuang MT, Buka SL. Neuropsychological performance and family history in children at age 7 who develop adult schizophrenia or bipolar psychosis in the New England family studies. Psychol Med. 2013;43:119–131. doi: 10.1017/S0033291712000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wykes T, Reeder C. Cognitive remediation therapy for schizophrenia: theory and practice. 1st New York: Taylor & Francis; 2005. [Google Scholar]
- 15.Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168:472–485. doi: 10.1176/appi.ajp.2010.10060855. [DOI] [PubMed] [Google Scholar]
- 16.McGurk SR, Mueser KT, Xie H, Welsh J, Kaiser S, Drake RE, et al. Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial. Am J Psychiatry. 2015;172:852–861. doi: 10.1176/appi.ajp.2015.14030374. [DOI] [PubMed] [Google Scholar]
- 17.Bowie CR, McGurk SR, Mausbach B, Patterson TL, Harvey PD. Combined cognitive remediation and functional skills training for schizophrenia: effects on cognition, functional competence, and real-world behavior. Am J Psychiatry. 2012;169:710–718. doi: 10.1176/appi.ajp.2012.11091337. [DOI] [PubMed] [Google Scholar]
- 18.Drake RJ, Day CJ, Picucci R, Warburton J, Larkin W, Husain N, et al. A naturalistic, randomized, controlled trial combining cognitive remediation with cognitive-behavioural therapy after first-episode non-affective psychosis. Psychol Med. 2014;44:1889–1899. doi: 10.1017/S0033291713002559. [DOI] [PubMed] [Google Scholar]
- 19.Nuechterlein KH, Ventura J, McEwen SC, Gretchen-Doorly D, Vinogradov S, Subotnik KL. Enhancing cognitive training through aerobic exercise after a first schizophrenia episode: theoretical conception and pilot study. Schizophr Bull. 2016;42(Suppl 1):S44–S52. doi: 10.1093/schbul/sbw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kambeitz-Ilankovic L, Betz LT, Dominke C, Haas SS, Subramaniam K, Fisher M, et al. Multi-outcome meta-analysis (MOMA) of cognitive remediation in schizophrenia: revisiting the relevance of human coaching and elucidating interplay between multiple outcomes. Neurosci Biobehav Rev. 2019;107:828–845. doi: 10.1016/j.neubiorev.2019.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lejeune JA, Northrop A, Kurtz MM. A meta-analysis of cognitive remediation for schizophrenia: efficacy and the role of participant and treatment factors. Schizophr Bull. 2021;47:997–1006. doi: 10.1093/schbul/sbab022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cella M, Preti A, Edwards C, Dow T, Wykes T. Cognitive remediation for negative symptoms of schizophrenia: a network meta-analysis. Clin Psychol Rev. 2017;52:43–51. doi: 10.1016/j.cpr.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 23.Penadés R, Wykes T. Use of cognitive remediation to treat negative symptoms in schizophrenia: is it time yet? Br J Psychiatry. 2023;223:319–320. doi: 10.1192/bjp.2023.50. [DOI] [PubMed] [Google Scholar]
- 24.Dickinson D, Tenhula W, Morris S, Brown C, Peer J, Spencer K, et al. A randomized, controlled trial of computer-assisted cognitive remediation for schizophrenia. Am J Psychiatry. 2010;167:170–180. doi: 10.1176/appi.ajp.2009.09020264. [DOI] [PubMed] [Google Scholar]
- 25.Gomar JJ, Valls E, Radua J, Mareca C, Tristany J, del Olmo F, et al. A multisite, randomized controlled clinical trial of computerized cognitive remediation therapy for schizophrenia. Schizophr Bull. 2015;41:1387–1396. doi: 10.1093/schbul/sbv059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bell MD, Choi KH, Dyer C, Wexler BE. Benefits of cognitive remediation and supported employment for schizophrenia patients with poor community functioning. Psychiatr Serv. 2014;65:469–475. doi: 10.1176/appi.ps.201200505. [DOI] [PubMed] [Google Scholar]
- 27.Bossert M, Westermann C, Schilling TM, Weisbrod M, Roesch-Ely D, Aschenbrenner S. Computer-assisted cognitive remediation in schizophrenia: efficacy of an individualized vs. generic exercise plan. Front Psychiatry. 2020;11:555052. doi: 10.3389/fpsyt.2020.555052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Franck N, Duboc C, Sundby C, Amado I, Wykes T, Demily C, et al. Specific vs general cognitive remediation for executive functioning in schizophrenia: a multicenter randomized trial. Schizophr Res. 2013;147:68–74. doi: 10.1016/j.schres.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 29.Scoriels L, Genaro LT, Mororó LGC, Keffer S, Guimarães ALDV, Ribeiro PVS, et al. Auditory versus visual neuroscience-informed cognitive training in schizophrenia: effects on cognition, symptoms and quality of life. Schizophr Res. 2020;222:319–326. doi: 10.1016/j.schres.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Apps and digital health resources reviewed by experts. Available at: https://onemindpsyberguide.org. Accessed February 6, 2020.
- 31.Siu AMH, Ng RSH, Poon MYC, Chong CSY, Siu CMW, Lau SPK. Evaluation of a computer-assisted cognitive remediation program for young people with psychosis: a pilot study. Schizophr Res Cogn. 2020;23:100188. doi: 10.1016/j.scog.2020.100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mahncke HW, Kim SJ, Rose A, Stasio C, Buckley P, Caroff S, et al. Evaluation of a plasticity-based cognitive training program in schizophrenia: results from the eCaesar trial. Schizophr Res. 2019;208:182–189. doi: 10.1016/j.schres.2019.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bowie CR, Bell MD, Fiszdon JM, Johannesen JK, Lindenmayer JP, McGurk SR, et al. Cognitive remediation for schizophrenia: an expert working group white paper on core techniques. Schizophr Res. 2020;215:49–53. doi: 10.1016/j.schres.2019.10.047. [DOI] [PubMed] [Google Scholar]
- 34.Vita A, Barlati S, Ceraso A, Nibbio G, Ariu C, Deste G, et al. Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2021;78:848–858. doi: 10.1001/jamapsychiatry.2021.0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huddy V, Reeder C, Kontis D, Wykes T, Stahl D. The effect of working alliance on adherence and outcome in cognitive remediation therapy. J Nerv Ment Dis. 2012;200:614–619. doi: 10.1097/NMD.0b013e31825bfc31. [DOI] [PubMed] [Google Scholar]
- 36.Cella M, Wykes T. The nuts and bolts of cognitive remediation: exploring how different training components relate to cognitive and functional gains. Schizophr Res. 2019;203:12–16. doi: 10.1016/j.schres.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 37.Rose D, Wykes T, Farrier D, Doran AM, Sporle T, Bogner D. What do clients think of cognitive remediation therapy?: a consumer-led investigation of satisfaction and side effects. Am J Psychiatr Rehabil. 2008;11:181–204. [Google Scholar]
- 38.Contreras NA, Lee S, Tan EJ, Castle DJ, Rossell SL. How is cognitive remediation training perceived by people with schizophrenia? A qualitative study examining personal experiences. J Ment Health. 2016;25:260–266. doi: 10.3109/09638237.2016.1167856. [DOI] [PubMed] [Google Scholar]
- 39.Bryce SD, Rossell SL, Lee SJ, Lawrence RJ, Tan EJ, Carruthers SP, et al. Neurocognitive and self-efficacy benefits of cognitive remediation in schizophrenia: a randomized controlled trial. J Int Neuropsychol Soc. 2018;24:549–562. doi: 10.1017/S1355617717001369. [DOI] [PubMed] [Google Scholar]
- 40.Thomas M, Rusten K. Trial implementation of CIRCuiTS cognitive remediation therapy for people with schizophrenia in Orange, New South Wales. Aust J Rural Health. 2019;27:463–468. doi: 10.1111/ajr.12578. [DOI] [PubMed] [Google Scholar]
- 41.Wykes T, Reeder C, Huddy V, Taylor R, Wood H, Ghirasim N, et al. Developing models of how cognitive improvements change functioning: mediation, moderation and moderated mediation. Schizophr Res. 2012;138:88–93. doi: 10.1016/j.schres.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peña J, Ibarretxe-Bilbao N, Sánchez P, Uriarte JJ, Elizagarate E, Gutierrez M, et al. Mechanisms of functional improvement through cognitive rehabilitation in schizophrenia. J Psychiatr Res. 2018;101:21–27. doi: 10.1016/j.jpsychires.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 43.Wykes T, Spaulding WD. Thinking about the future cognitive remediation therapy—what works and could we do better? Schizophr Bull. 2011;37(Suppl 2):S80–S90. doi: 10.1093/schbul/sbr064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haller EP, Child DA, Walberg HJ. Can comprehension be taught?: a quantitative synthesis of “metacognitive” studies. Educ Res. 1988;17:5–8. [Google Scholar]
- 45.De Boer H, Donker AS, Kostons DD, Van der Werf GP. Long-term effects of metacognitive strategy instruction on student academic performance: a meta-analysis. Educ Res Rev. 2018;24:98–115. [Google Scholar]
- 46.Wright AC, Davies G, Fowler D, Greenwood K. Three-year follow-up study exploring metacognition and function in individuals with first episode psychosis. Front Psychiatry. 2019;10:182. doi: 10.3389/fpsyt.2019.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Best MW, Milanovic M, Iftene F, Bowie CR. A randomized controlled trial of executive functioning training compared with perceptual training for schizophrenia spectrum disorders: effects on neurophysiology, neurocognition, and functioning. Am J Psychiatry. 2019;176:297–306. doi: 10.1176/appi.ajp.2018.18070849. [DOI] [PubMed] [Google Scholar]
- 48.Reeder C, Pile V, Crawford P, Cella M, Rose D, Wykes T, et al. The feasibility and acceptability to service users of CIRCuiTS, a computerized cognitive remediation therapy programme for schizophrenia. Behav Cogn Psychother. 2016;44:288–305. doi: 10.1017/S1352465815000168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reeder C, Huddy V, Cella M, Taylor R, Greenwood K, Landau S, et al. A new generation computerised metacognitive cognitive remediation programme for schizophrenia (CIRCuiTS): a randomised controlled trial. Psychol Med. 2017;47:2720–2730. doi: 10.1017/S0033291717001234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cella M, Edwards C, Swan S, Elliot K, Reeder C, Wykes T. Exploring the effects of cognitive remediation on metacognition in people with schizophrenia. J Exp Psychopathol. 2019;10:2043808719826846. [Google Scholar]
- 51.Lammas F, Phillips A, Dopson S, Joyce E, Csipke E, Wykes T. The organisational climate of NHS early intervention services (EIS) for psychosis: a qualitative analysis. BMC Health Serv Res. 2022;22:509. doi: 10.1186/s12913-022-07790-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Taylor R, Crowther A, Tinch-Taylor R, Lewin CDC, Cali C, Reeder C, et al. Evaluation of a new online cognitive remediation therapy (CIRCuiTSTM) training for mental health professionals. Psychol Psychother. 2024;97:234–247. doi: 10.1111/papt.12510. [DOI] [PubMed] [Google Scholar]
- 53.Vita A, Barlati S, Ceraso A, Deste G, Nibbio G, Wykes T. Acceptability of cognitive remediation for schizophrenia: a systematic review and meta-analysis of randomized controlled trials. Psychol Med. 2023;53:3661–3671. doi: 10.1017/S0033291722000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wykes T, Stringer D, Boadu J, Tinch-Taylor R, Csipke E, Cella M, et al. Cognitive remediation works but how should we provide it? An adaptive randomized controlled trial of delivery methods using a patient nominated recovery outcome in first-episode participants. Schizophr Bull. 2023;49:614–625. doi: 10.1093/schbul/sbac214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reeder C, Harris V, Pickles A, Patel A, Cella M, Wykes T. Does change in cognitive function predict change in costs of care for people with a schizophrenia diagnosis following cognitive remediation therapy? Schizophr Bull. 2014;40:1472–1481. doi: 10.1093/schbul/sbu046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Garrido G, Penadés R, Barrios M, Aragay N, Ramos I, Vallès V, et al. Computer-assisted cognitive remediation therapy in schizophrenia: durability of the effects and cost-utility analysis. Psychiatry Res. 2017;254:198–204. doi: 10.1016/j.psychres.2017.04.065. [DOI] [PubMed] [Google Scholar]


