Abstract
Background
The goal of conventional endodontic therapy is to clean the root canal system thoroughly, restore tooth function, and prevent re-infection. Success depends on understanding root canal morphology, resolving apical periodontitis, and using proper techniques. Studies highlight variations in root canal anatomy, with cone-beam computed tomography (CBCT) being crucial for accurate diagnosis despite its high cost and limited availability.
Material/Methods
This retrospective study reviewed CBCT images of 1820 (907 male, 913 female) patients aged 18 to 78 years. Analysis included 2081 mandibular first molars for variations in root and canal morphology and right- and left-side symmetry. Inter-orifice distance was measured, along with distance from the cementoenamel junction (CEJ) to the level of canal bifurcation.
Results
In this study, 96.01% of teeth had 2 roots and 3.89% had 3 roots. The percentages of canal configuration were 77.70% for 3 canals, 21.58% for 4 canals, 0.67% for 2 canals, and 0.05% for 1 canal. The inter-orifice distance was 2.07 mm for 2 canals in 1 root and 2.86 mm for 2 canals in separate distal roots. Distance from the CEJ to canal bifurcation varied significantly between 2 canals within 1 distal root (3.35 mm), 2 canals in separate distal roots (1.60 mm), as well as between distal (3.35 mm) and mesial roots (1.10 mm).
Conclusions
In mandibular first molars, only 3.89% have additional distolingual roots. Sex and ethnicity showed no influence on number of roots and canals. Distal canals showed a deeper bifurcation and greater inter-orifice distance than did mesial canals.
Keywords: Anatomy, Dental Pulp Cavity, Root Canal Therapy
Introduction
The objective of conventional endodontic therapy is to achieve thorough debridement of the root canal system, restore the tooth’s function, and prevent re-infection [1]. Accurate knowledge of the intricate root canal morphology, which can vary considerably across different demographic groups, is essential for endodontic success [2–4].
Endodontic treatment outcome is influenced by multiple factors, particularly those related to the resolution and prevention of the recurrence of apical periodontitis [5]. These factors include the initial microbial load, peri-radicular damage, state of the pulp prior to treatment, presence of a preoperative periapical radiolucency, technique and quality of the root canal filling, presence of missed canals [6], and quality of the coronal restoration placed following root canal treatment [7].
Missed canals in teeth that have undergone root canal treatment can result from inadequate access cavity preparation or insufficient understanding of dental morphology and canal architecture. These unaddressed canals can harbor microbial colonies, leading to the persistence of apical periodontitis [8]. To avoid such outcomes, thorough and formative knowledge of dental anatomy and the intricacies of the root canal system is imperative. Furthermore, meticulous analysis and interpretation of radiographic images, taking into account various horizontal angles, are critical throughout the stages of root canal therapy [9].
The first molar in the mandibular arch, which often requires root canal treatment, typically has 2 roots, mesial and distal, along with 3 root canals: 2 mesial and 1 distal [10]. Notably, dental anatomy variations have been observed, including the occurrence of an additional third root in the mandibular first molar, identified as the radix entomolaris [11]. This extra root is predominantly positioned distolingually and exhibits a global prevalence ranging from 1.35% to 33.33%, with significant variations across different ethnic groups [12–14]. Conversely, when an extra root is located mesiobuccally, it is classified as radix paramolaris [11].
The mesial root of mandibular first molars typically contains 2 canals, which can terminate in 1 or 2 apical foramina [15]. The distal root usually has 1 large canal; however, in approximately 30% of cases, 2 canals are present [16]. Studies have reported varying prevalence of 4 canals in mandibular first molars, as follows: 19.5% in Malaysia [17], 21% in Italy [18], 24% in Brazil [19], 31.57% in Iran [20], 45% in China [21], 50% in Korea [22], and 59% in Sudan [23].
Recent studies utilizing cone-beam computed tomography (CBCT) have provided insights into the root and canal morphology of permanent mandibular first molars in various regions of Saudi Arabia. Mashyakhy et al conducted a study in southern region of Saudi Arabia, evaluating 174 CBCT images. The findings revealed that 97.1% of mandibular first molars were 2-rooted, and 2.9% were 3-rooted. The most prevalent canal configuration was 3 canals (73%), followed by 4 canals (25.3%) and 2 canals (1.7%). No significant associations were found between the number of roots, canals, and patient sex. Symmetry between the right and left sides was observed in the number of roots of all teeth and in 56.4% of teeth in the number of canals [24]. Another study investigated the prevalence of radix entomolaris in the middle region of Saudi using a sample of 400 CBCT images. The prevalence of mandibular molars with 3 roots was 12.5%, and with 4 roots, it was 0.5%. Men exhibited a higher prevalence of 3 roots (60%) than women (40%) [14]. In a recent systematic review of root canal morphology of permanent mandibular teeth in different regions of Saudi Arabia, most teeth had 2 roots (98.9%), while only 0.2% had 3 roots. Three canals were prevalent in 58.7% of cases, while 4 canals were present in 40.6% of cases, and only 0.7% of the teeth had 2 canals [25].
In recent decades, various methods have been used to investigate the complex anatomy of root and canal system. These methods include the replication of pulpal space anatomy using vulcanite casts, as performed in Hess’s early studies [26], transverse tooth sectioning [27], canal staining and clearing techniques [10], modified canal staining [3], conventional radiographic imaging [28], and computed tomography (CT) scans [29–31].
While conventional radiography is routinely used to assess complex root canal anatomy, its main limitation is the bidimensional representation of images, which can lead to the oversight of additional root canals or anatomical variations [32]. Modified canal staining provides a 3-dimensional view of the pulp chamber without compromising the tooth’s structural integrity, yet it cannot be applied in vivo [3]. Sectioning, particularly with abrasive sandpaper discs, risks altering the internal canal configuration and compromising the structural integrity of the tooth [27].
The introduction of CBCT in the 1990s has led to significant advancements in endodontic diagnostics [30]. Nevertheless, the high cost of CBCT has limited its widespread use in routine endodontic diagnostics and treatment. CBCT is acknowledged as the most accurate imaging modality for identifying root canal anatomy. In an in vitro study by Tira et al, CBCT was compared with 2 digital radiographic technologies, the charged coupled device and photostimulable phosphor plate, and showed that conventional digital radiography missed at least 1 root canal in 40% of cases, which could compromise the success of endodontic procedures [33]. Similar findings were reported by Subbarao et al, who demonstrated the superiority of CBCT, alongside modified canal staining and clearing techniques, over digital radiography in accurately identifying root canal structures [34].
To the best of our knowledge, no morphological study has looked into the prevalence of third root and fourth root canals in the permanent mandibular first molars in the sub-population of Jeddah, Saudi Arabia. Furthermore, certain aspects of the root and canal morphology of permanent mandibular first molars in Saudi Arabia revealed by CBCT have not been previously reported in the literature. These include measurements of the inter-orifice distance and the distance from the cementoenamel junction (CEJ) to the level of canal bifurcation. Therefore, in this study, we aimed to evaluate variations in root and canal morphology of 2081 left and right mandibular first molars in 1820 Saudi patients, using CBCT.
Material and Methods
Sample Selection
The protocol of this retrospective cohort study was approved by the Institutional Ethics Committee at King Abdulaziz University, Jeddah, Saudi Arabia (approval number: 104-10-20). A total of 6203 CBCT scans were obtained between January 2014 and April 2021, as part of the patient diagnosis, treatment planning, and implant placement decision making. They were filtered according to the region to be scanned. A total of 3256 CBCT scans were acquired targeting the mandibular jaw. In which, 2040 were female patients’ scans and 1210 were male patients’ scans. Sample size was calculated using the following parameters: alpha=0.0500, power=0.8000, delta=−0.0270 (difference), p1=0.0570, and p2=0.0300. The estimated sample size was N=1790. The exclusion criteria were set as the following: images showing artifacts that interfered with the observation of the tooth of concern, making the evaluation of those teeth challenging. The following artifacts were identified during interpretation of the images: motion artifact, teeth restored with metal crowns, dental implants in adjacent teeth, and if the entire tooth was not showing. Any teeth with root resorption, canal calcification, or incomplete apex formation were excluded from the study. Inclusion criteria were as follows: patients 18 years and older, with fully matured apices.
CBCT Scanning and Analysis
Images of 1820 randomly selected CBCTs were captured using the i-CAT Classic CBCT device (Imaging International Sciences, Hatfield, PA, USA). In total, there were 907 scans from male patients and 913 scans from female patients. All CBCT exposures were performed with the minimum exposure necessary for adequate image quality by experienced licensed technicians. CBCT images were evaluated by 1 observer on a 24-inch HP monitor (EliteDisplay E243, CA, USA) with a resolution of 1920×1080 pixels, in a reporting room without windows. The scans were checked and analyzed using OnDemand3D software (Cybermed Inc, Daejeon, South Korea). Reevaluation was done for 30 images with an interval period of 2 months to measure the intra-rater agreement.
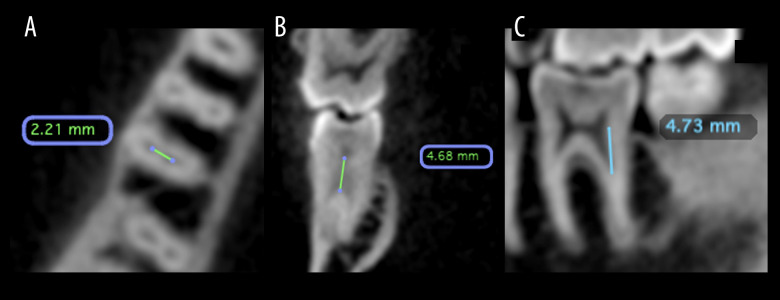
The number of roots and number of canals were analyzed using the axial view. The examiner placed the origin of the horizontal and the vertical axis on the center of the crown from the axial view, then the examiner scrolled downward until the root apex. The axial view was also used to measure the inter-orifice distance (length of a line between center points of 2 orifices) between the 2 mesial canals and between the 2 distal canals, if present (Figure 1A). The examiner placed the origin of the horizontal and the vertical axis on the center of the crown of the tooth to adjust the views. The selected section for the evaluation was the cross-sectional view for this posterior tooth. The evaluation was done by adjusting the vertical (bucco-lingual) reference line in the axial plane through the center of the root, then aligning the vertical reference line in mesio-distal and bucco-lingual through the center of the root along its longitudinal axis. After that, the examiner scrolled downward through the axial view until the beginning of the separation. At that level, a line was drawn using a ruler to measure the distance between the orifices of the 2 distal canals. From there on, the examiner moved to corrected-sagittal and cross-sectional views to measure the distance from the CEJ until the level where the canal divided into 2 separate canals. A ruler was used to measure the distance from the CEJ to the bisecting level (Figure 1B, 1C). The examiner could magnify images and change viewing settings, such as density, contrast, and sharpness, to enhance visibility and identification of the examined structures. This procedure was done for mesial and distal roots.
Figure 1. CBCT images of permanent mandibular first molar.
This figure shows different views of the CBCT image of lower permanent mandibular first molar. (A) Shows an axial cross section of CBCT image of the tooth. This view is used to measure inter-orifice distance (IOD) between the 2 mesial canals and between the 2 distal canals if present; (B, C) show coronal and sagittal cross sections (respectively) of CBCT images of the tooth. These images are used to measure the distance from the cementoenamel junction (CEJ) to canal division in the corrected-sagittal view.
Personal information, such as sex and ethnic background, were documented. The prevalence of 3-rooted permanent mandibular first molars and the prevalence of missed or extracted, root canal-filled, and the presence of missed root canal in root canal-filled mandibular first molars were also recorded and analyzed. Sex ratio, ethnicity, and symmetrical analysis between right and left side on the same individual were also collected.
Statistical Analysis
All data were analyzed with the Stata software, version 16 (StataCorp, College Station, TX, USA) and the IBM Statistical Package for Social Sciences Statistics version 28 (IBM Corp, Armonk, NY, USA). Descriptive statistics were used to describe the categorical and quantitative variables. For categorical variables, frequencies and column percentages were calculated. Frequencies and column percentages of the permanent mandibular first molars’ characteristics (number of roots and number of canals) by sex and by nationality (ethnicity) were compared using the Pearson chi-square test. However, when the Pearson chi-square test was not applicable, the Fisher exact test was used, and its P value was reported. The same test was used to compare missed/unfilled canals in root canal-filled permanent mandibular first molars between the 2 canals in 1 root and the 2 canals in 2 distal roots.
We tested the hypothesis using a 2-sample Wilcoxon rank-sum test (Mann-Whitney). The test was used to assess the statistical difference between inter-orifice distance measured in 1 root with 2 canals and in 2 separate roots with 2 canals. Also, the test was used to assess the statistical difference between inter-orifice distance measured in 1 root with 2 canals in the distal and mesial roots. Moreover, the same test was used to assess the statistical difference between distance from CEJ to canal separation in 1 root with 2 canals and in 2 separate roots with 2 canals measured from the sagittal and coronal views. The level of agreement between the right and left sides (symmetry) was assessed using kappa statistics (value). The kappa value represents the proportion of agreement between the 2 sides beyond the agreement occurring due to chance. The P value of P<0.001 suggests that the kappa value is statistically significant from zero. A kappa value between 0.61 and 0.80 means good, and between 0.81 and 1.00 means very good.
Results
The weighted kappa for the intra-rater agreement revealed an almost perfect agreement between the 2 measurements (first and second) for the distance from CEJ to canal division and for sagittal view (Cohen kappa=0.840) and coronal view (Cohen kappa=0.870), and substantial agreement for inter-orifice distance (Cohen kappa=0.642).
In this study, we assessed 1820 participants, evaluating a total of 3640 mandibular first molars. The patient age range was 18 to 78 years, with a mean age of 30.1 years. The condition of these molars was classified as sound, missing, or root-filled, comprising 41.51%, 42.69%, and 15.66% of the sample, respectively, with a cumulative count of 2081 mandibular first molars.
Number of Roots and Canals
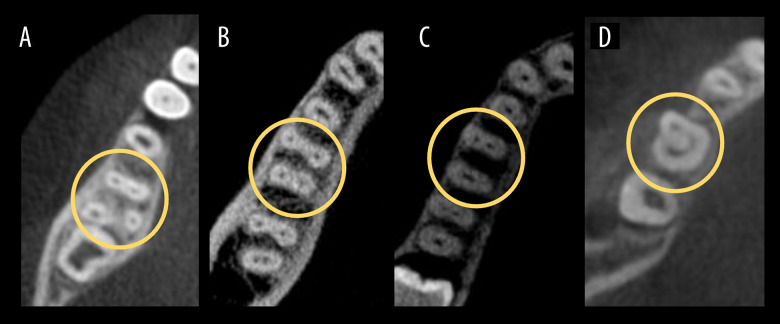
Regarding the number of roots, 1998 (96.01%) had 2 roots, 81 (3.89%) had 3 roots, and only 2 (0.10%) exhibited a single root. Concerning canal number, most molars had 3 canals, totaling 1617 (77.70%), followed by 449 (21.58%) with 4 canals, 14 (0.67%) with 2 canals, and only 1 (0.05%) with 1 canal. Among the teeth with 4 canals, 368 of 449 (81.96%) featured the additional canal within the same distal root, while 81 cases (18.04%) presented an extra canal located in an additional distolingual root, known as the radix entomolaris, as shown in Figure 2.
Figure 2. Anatomical variations found in permanent mandibular first molars.
This figure shows coronal cross-sectional views illustrating different anatomical variants found in permanent mandibular first molars. (A) Shows 3 roots with 4 canals; (B) shows 2 roots with 4 canals; (C) shows 2 roots with 3 canals; and (D) shows 1 root with 2 canals.
Comparison by Sex
The analysis indicated that 53.05% (n=1104) of patients were men and 43.87% (n=977) were women. There was no statistically significant difference between sex in the number of roots and number of canals (Table 1).
Table 1.
Comparisons of permanent mandibular first molars characteristics by sex.
| Characteristic n (%) | Male (n=1104) | Female (n=977) | χ2 value | P value* |
|---|---|---|---|---|
| Number of roots | ||||
| 1 | 1 (0.09) | 1 (0.10) | 1.37 | 0.886 |
| 2 | 1060 (96.01) | 938 (96.01) | ||
| 3 | 43 (3.89) | 38 (3.89) | ||
| Number of canals | ||||
| 1 | 1 (0.09) | 0 (0.00) | 5.38 | 0.110 |
| 2 | 4 (0.36) | 10 (1.02) | ||
| 3 | 870 (78.80) | 747 (76.46) | ||
| 4 | 229 (20.74) | 220 (22.52) |
χ2 – Chi-square test.
Fisher exact test and its P value are used because Pearson chi-square is not applicable.
Comparison by Ethnic Group
Of the total patients (n=3640) evaluated, most patients were Saudi, accounting for 2694 (74.01%) of the sample, followed by 682 (18.74%) individuals from the Middle East and North Africa region, 114 (3.13%) African, 106 (2.91%) Asian, 14 (0.38%) European, and, finally, 2 (0.05%) North American. There was no statistically significant difference in the number of roots and number of canals between Saudi and non-Saudi patients (Table 2).
Table 2.
Comparisons of permanent mandibular first molars characteristics by ethnic group.
| Characteristic n (%) | Saudi (n=1554) | Non-Saudi (n=527) | χ2 value | P value* |
|---|---|---|---|---|
| Number of roots | ||||
| 1 | 2 (0.13) | 0 (0.00) | 0.84 | 0.886 |
| 2 | 1490 (95.88) | 508 (96.39) | ||
| 3 | 62 (3.99) | 19 (3.61) | ||
| Number of canals | ||||
| 1 | 1 (0.06) | 0 (0.00) | 3.798 | 0.247 |
| 2 | 8 (0.51) | 6 (1.14) | ||
| 3 | 1218 (78.38) | 399 (75.71) | ||
| 4 | 327 (21.04) | 122 (23.15) |
χ2 – Chi-square test.
Fisher exact test and its P value are used because Pearson chi-square is not applicable.
Inter-Orifice Distance
The distolingual canal was separated from the distobuccal canal by 2.07 mm when both canals were located in the same distal root or 2.86 mm when canals occurred in 2 separate distal roots.
However, the mesio-lingual canal and the mesio-buccal canal were separated by 1.85 mm, and both canals were located in the same mesial root.
The median distance of distolingual-distobuccal was much greater than that of mesio-lingual–mesio-buccal (P<0.05). There was a significant difference in the inter-orifice distance of 2 canals in 1 root between the distal and mesial roots (Table 3). Also, there was a significant difference in the inter-orifice distance of 2 canals in 1 distal root (2.07 mm) and in 2 canals in 2 separate distal roots (2.86 mm). Results for statistical comparisons for inter-orifice distance measured in 1 distal root with 2 canals and in 2 separate distal roots with 2 canals are presented in Table 4.
Table 3.
Statistical comparisons for inter-orifice distance measured in 1 root with 2 canals between the distal and mesial roots.
| Group | n | Median [IQR] (mm) | Z value* | P value |
|---|---|---|---|---|
| Distal root | 244 | 2.07 [0.65] | 7.60 | <0.001# |
| Mesial root | 810 | 1.8 [0.57] |
Two-sample Wilcoxon rank-sum (Mann-Whitney) test;
Statistical significance (P<0.05).
Table 4.
Statistical comparisons for inter-orifice distance measured in 1 distal root with 2 canals and in 2 separate distal roots with 2 canals.
| Root | Subgroup | n | Median [IQR] (mm) | Z value* | P value |
|---|---|---|---|---|---|
| Distal | Two canals in 1 root | 244 | 2.07 [0.65] | −7.38 | <0.001# |
| Two canals in 2 roots | 59 | 2.86 [0.97] |
Two-sample Wilcoxon rank-sum (Mann-Whitney) test;
Statistical significance (P<0.05).
Distance from CEJ to Canal Separation
Regarding the distance measured from CEJ to the level of canal separation, a statistically significant difference was found in the distal root between 2 canals in 1 distal root and 2 canals in 2 separate distal roots from the sagittal and coronal views. Also, when comparing mesial and distal roots, our results showed that there was a significant difference in the distance from CEJ to canal separation in 1 root with 2 canals between the distal and mesial root measured from the sagittal and coronal views. Results for statistical comparisons are presented in Tables 5 and 6.
Table 5.
Statistical comparisons for distance from cementoenamel junction to canal separation measured in 1 distal root with 2 canals and in 2 separate distal roots with 2 canals.
| View | Subgroup | n | Median [IQR] (mm) | Z value* | P value |
|---|---|---|---|---|---|
| Sagittal | Two canals in 1 root | 244 | 3.73 [1.53] | 8.89 | <0.001# |
| Two canals in 2 roots | 59 | 2.10 [1.05] | |||
| Coronal | Two canals in 1 root | 244 | 3.35 [1.41] | 9.47 | <0.001# |
| Two canals in 2 roots | 59 | 1.60 [1.06] |
Two-sample Wilcoxon rank-sum (Mann-Whitney) test;
Statistical significance (P<0.05).
Table 6.
Statistical comparisons for distance from cementoenamel junction to canal separation measured in 1 root with 2 canals between distal and mesial roots with 2 canals.
| View | Subgroup | n | Median [IQR] (mm) | Z value* | P value |
|---|---|---|---|---|---|
| Sagittal | Distal root | 244 | 3.73 [1.53] | 20.04 | <0.001# |
| Mesial root | 810 | 1.59 [1.09] | |||
| Coronal | Distal root | 244 | 3.35 [1.41] | 21.00 | <0.001# |
| Mesial root | 810 | 1.10 [1.17] |
Two-sample Wilcoxon rank-sum (Mann-Whitney) test;
Statistical significance (P<0.05).
Correlation Between Right and Left Sides
Root Symmetry
Of the 1820 patients examined, only 832 had both right and left permanent mandibular first molars present. The results showed a 64% symmetry in the number of roots between the right and left sides (P<0.001), with the most common symmetrical presentation being 2 roots, observed in 785 patients.
Canal Symmetry
Additionally, there was 80% symmetry in the number of canals between the right and left sides (P<0.001), with the predominant symmetrical arrangement being 3 canals in 623 patients, followed by 4 canals in 148 patients.
Missed/Unfilled Canal in Root Canal-Filled Permanent Mandibular First Molars
Within the cohort examined in this study, of the 570 root-filled permanent mandibular first molars, 97 (17%) exhibited a missed canal. The incidence of missed canals occurred in the following order: distolingual in 34 cases (35.05%), mesiolingual in 21 cases (21.65%), distobuccal in 20 cases (20.62%), mesiobuccal in 17 cases (17.53%), and, lastly, the distal canal in 5 cases (5.15%). These findings are presented in Table 7.
Table 7.
Frequencies and percentages for missed/unfilled canal in root canal filled mandibular first molars.
| Missed canals n (%) | Total (N=97) |
|---|---|
| Distal | 5 (5.15) |
| Disto-buccal | 20 (20.62) |
| Disto-lingual | 34 (35.05) |
| Mesio-lingual | 21 (21.65) |
| Mesio-buccal | 17 (17.53) |
Furthermore, a statistically significant difference was observed in the frequency of missed distolingual canals when they shared the same root with the distobuccal canal, as opposed to when they were in a separate distolingual root (P<0.05).
Discussion
In this retrospective study, we aimed to evaluate the prevalence of third roots and second distal canals in the permanent mandibular first molars among a subpopulation from Jeddah, Saudi Arabia, using CBCT. We also aimed to measure the inter-orifice distances between mesiobuccal-mesiolingual and distobuccal-distolingual canal orifices at the pulpal floor level, as well as the distances from the CEJ to the canal bifurcation points in mesial and distal roots, for better design and location of the access cavity. Accurate identification of the root canal orifices is critical in designing endodontic access and optimizing the efficiency and efficacy of endodontic procedures while reducing the risk of procedural errors and complications, therefore ensuring better treatment outcomes.
In the present study of mandibular first molars, 96.01% of patients had 2 roots, while 3.89% had 3 roots. The predominant canal configuration included 3 canals (77.70%), followed by 4 (21.58%), 2 (0.67%), and 1 canal (0.05%), with no notable discrepancies in root and canal distribution by sex or ethnic background. The interorifice distance measured 2.07 mm for 2 canals within a single root and 2.86 mm for 2 canals located in separate distal roots. Significant variations in inter-orifice distance were observed between distal (2.07 mm) and mesial roots (1.80 mm). The distance from the CEJ to canal bifurcation differed notably between 2 canals within 1 distal root (3.35 mm) and 2 canals in separate distal roots (1.60 mm), as well as between distal (3.35 mm) and mesial roots (1.10 mm). Overall, 17% of root-filled mandibular first molars had missed canals, with the distolingual canal being the most overlooked (35.05%).
Thorough preoperative assessment, including diagnostic imaging techniques such as radiographs or CBCT scans plays a pivotal role in precise identification of root canal anatomy. CBCT offers superior capabilities over conventional radiographic methods, such as charged coupled devices and photostimulable phosphor plates, in identifying root canal morphology, as noted by Matherne et al [33] and confirmed by Blattner et al and Zheng et al for detecting second mesio-buccal canals in maxillary first molars [29,35]. It has been reported that examination with digital radiography resulted in missing 1 root canal space in 40% of the cases, when compared with CBCT examinations [33]. In a study conducted by Sharifishoshtari et al, the diagnostic precision of CBCT was evaluated by comparing it with a sectioning technique for assessing root canal morphology in mandibular first molars. The findings demonstrated that CBCT achieved diagnostic accuracies of 80% on the mesial surface, 99% on the distal surface, and 96% overall. These results suggest that CBCT is a reliable technique for accurately evaluating the intricate root canal morphology of mandibular first molars, particularly when other modalities are less effective [36]. The resolution of CBCT images is as meticulous as that obtained through root canal staining and clearing techniques in discovering root anatomy [34]. Patel et al stated that the 3-dimensional CBCT imaging technique allows for superior visualization of the number of root canals and their directions [37]. Additionally, CBCT facilitates accurate visualization of the root canal system in multiple planes, avoiding the superimposition of anatomical structures, as reported by Cotton et al and Neelakantan et al [34,38], and offers high-resolution images with minimized radiation exposure and brief scanning times [34].
Findings from this study enrich the existing data pool regarding the root anatomy and canal morphology of the permanent mandibular first molar in the Saudi population, boasting a larger sample size than previous studies, thereby enhancing the reliability of morphological information [14,24,39–41]. Most of the sample population in the present study exhibited 2-rooted mandibular first molars, in line with findings in Saudi and Brazilian populations, as reported by Mashyakhy et al and Silva et al, respectively, and with the systematic review done by de Pablo et al [42,43].
The prevalence of mandibular first molars with 3 roots was 3.9%, consistent with findings from studies by Mashyakhy et al in the Saudi population (2.9%) and Alhadainy et al in the Yemeni population (3.2%) [24,44]. Higher prevalences were reported by Alenezi et al in the Saudi population (12.5%) and de Pablo et al in the Brazilian population (13%) [14,43]. Studies focusing on East Asian populations have consistently reported higher percentages of mandibular first molars with 3 roots. In a study by Kim et al on Korean individuals of Mongolian descent, extra distal roots were found in 25.82% of examined molars [22]. These findings substantiate that East Asian populations exhibit a greater prevalence of mandibular first molars with 3 roots than do other ethnic groups. Although 4-rooted mandibular first molars were reported by Alenezi et al in the Saudi population at 0.5% [14], it was not seen in our present research. C-shaped canal configurations were rare, seen only in 2 of 2081 patients (0.1%). This result aligns with the findings of Alfawaz et al in the Saudi population, who reported a prevalence of 0.2% [45]. However, C-shaped canal configurations were not found by Mashyakhy et al [24].
The universal assessment of root canal prevalence indicated that 61.3%, 35.7%, and 1% of the evaluated teeth contained 3 canals, 4 canals, and 5 canals, respectively [43]. In the present study, 77.7% of cases showed 3 root canals, while 4 canals were identified in 21.6% of cases. These results align with findings reported by Al-Qarni et al and Mashyakhy et al in studies involving Saudi populations, but are notably lower than the incidence of 4 canals reported in a Korean population, which was documented at 50.36% [22,24,46].
In this research, the presence of mandibular first molars with 2 root canals was documented at 0.67%, confirming the results published by Caputo et al in a Brazilian population [19], but was lower than those presented in an Italian population (9.4%) and Pakistani (7.8%) population, as reported by Plotino et al and Marwat et al, respectively [18,47]. In the present study, regarding the mandibular first molar with 4 root canals, 81.96% had 2 distal canals in the distal root, while 18.04% had 2 distal canals in 2 separate roots. Kim et al reported the same findings in a Korean population [48].
We also assessed anatomical symmetry between the right and left sides and found a significant degree of symmetry in the number of roots and canals. The most common symmetrical configuration was 2 roots and 3 canals, which is comparable to findings in other populations [14,24,49–54].
In the present study, the inter-orifice distance between the distolingual and distobuccal canals in separate distal roots was measured at 2.86 mm, aligning with the findings of Tu et al of 2.7 mm [12] but contrasting with the findings of Duman et al, with a reported mean of 1.63 mm and standard deviation of 0.66 mm [54]. These discrepancies could be attributed to variations in sample sizes or differences in radiographic interpretation and CBCT imaging parameters. For the mesial root, the inter-orifice distance between the mesio-lingual and mesio-buccal canals was determined to be 1.8 mm, which differed from the 2.35 mm reported by Gu et al, using micro-CT scans [55]. The disparity in measurements suggests that the access cavity design for mandibular first molars should extend further distally than mesially, rather than a conventional trapezoidal shape, to account for the asymmetrical distribution of canal orifices. This finding challenges the conventional symmetry law proposed by Kranser and Rankow [56], indicating that canal orifices in mandibular first molars are not equidistant from a mesiodistal line drawn through the pulp chamber floor’s center but are biased toward the mesial aspect, potentially complicating access for less experienced clinicians [57].
The CEJ served as the reference landmark for determining the point at which the canal bifurcates into 2 separate pathways. According to our study, the mesial root bifurcated at distances of 1.59 mm and 1.1 mm from the CEJ in sagittal and coronal views, respectively. Conversely, the bifurcation in the distal root occurred at 3.73 mm in the sagittal view and 3.35 mm in the coronal view, indicating that the division of the mesial canals occurrs near the pulp floor level [58], whereas the distal canals branch deeper within the root structure, making their identification and access more challenging.
The prevalence of missed canals in our study was found to be 17%, which is consistent with the findings of Iqbal et al [59]. This contrasts with the higher incidence of 42% reported by Hoen and Pink et al in teeth subjected to non-surgical retreatment. Comparatively, Karabucak et al and Mashyakhy et al reported a slightly elevated overall incidence of missed canals, documented at 23% and 25%, respectively [60,61]. In our study, the distolingual canal was the predominantly missed canal, at 35.05%, followed by mesio-lingual, at 21.65%. These findings are comparable to those reported by Karabucak et al and in contrast to those of Mashyakhy et al, in which the mesiobuccal and distobuccal were the most commonly untreated canals.
Our results highlight the frequent occurrence of a fourth canal in mandibular first molars, which underscores the necessity of anticipating and locating all 4 present canals during molar endodontic therapy. Endodontists should expect a second canal in the distal root of mandibular molars. Additionally, the likelihood of extra roots beyond the typical anatomy should be anticipated and diligently treated to avoid the unfavorable outcome of missed canals when left untreated.
These results emphasize the complexity of this tooth’s anatomy. Clinicians should pay special attention to the configuration and root canal system before starting any root canal treatment procedures. The precise location of each canal is critical; the mesiobuccal canal orifice is located beneath the mesiobuccal cusp, while the mesiolingual canal orifice is situated lingual to the central groove. The orifice of the second distal canal is placed distolingually from the major canal or canals of the distal root. Generally, these orifices are positioned in the mesial two-thirds of the crown [9]. Our reported findings and measurements suggest shifting the endodontic molar access in a distolingual direction to include the distolingual canal and confine the access to the mesial half of the tooth. Magnification, illumination, and appropriate armamentarium, along with knowledge of the root and canal anatomy, are essential tools for the practitioner to treat the entire root canal system [62].
The primary limitation of this research is its retrospective cohort design, which led to the unavailability of certain data due to incomplete records [63]. The research sample was also restricted to a single center, potentially affecting the generalizability of the results. Furthermore, the medium field of view of the CBCT used presents drawbacks, such as a larger irradiated area and diminished spatial resolution [64]. The American Association of Endodontists and the American Academy of Oral and Maxillofacial Radiology have jointly recommended the application of a small field of view for the detection of additional canals or in cases of complex anatomical structures [65]. Addressing these methodological constraints is recommended for future investigations.
Conclusions
Within the limitations of this study, CBCT imaging emerges as a reliable tool for accurately identifying root canal anatomy and configurations, owing to its precise, non-invasive, and replicable imaging capability. Among this Saudi populations’ mandibular first molars, a minority (3.89%) exhibited an additional distolingual root. Sex and ethnic background did not correlate with variations in root or canal numbers. Distal canals presented with a deeper bifurcation (3.73 mm) and a larger interorifice distance (2.07 mm) than did mesial canals. Most patients displayed bilateral symmetry in root (64%) and canal (80%) counts. Notably, the distolingual canal was frequently overlooked, remaining untreated in 35% of root-filled mandibular first molars.
Acknowledgments
The authors acknowledge with thanks DSR for technical and financial support.
Footnotes
Conflict of interest: None declared
Declaration of Figures’ Authenticity: All figures sumbitted have been created by the authors, who confirm that the images are oroginal with no duplication and have not been previously published in whole or in part.
Financial support: This project was funded by the Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah, under grant no. G-584-165-1441
References
- 1.Grecca FS, Garcia RB, Bramante CM, et al. A quantitative analysis of rotary, ultrasonic and manual techniques to treat proximally flattened root canals. J Appl Oral Sci. 2007;15(2):89–93. doi: 10.1590/S1678-77572007000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tratman EK. Three rooted lower molars in man and their racial distribution. Br Dent J. 1938;64:264–74. [Google Scholar]
- 3.Weng XL, Yu SB, Zhao SL, et al. Root canal morphology of permanent maxillary teeth in the Han nationality in Chinese Guanzhong area: A new modified root canal staining technique. J Endod. 2009;35(5):651–56. doi: 10.1016/j.joen.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Neelakantan P, Subbarao C, Ahuja R, et al. Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. J Endod. 2010;36(10):1622–27. doi: 10.1016/j.joen.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Ng YL, Mann V, Gulabivala K. Outcome of secondary root canal treatment: A systematic review of the literature. Int Endod J. 2008;41(12):1026–46. doi: 10.1111/j.1365-2591.2008.01484.x. [DOI] [PubMed] [Google Scholar]
- 6.Nair PN. On the causes of persistent apical periodontitis: A review. Int Endod J. 2006;39(4):249–81. doi: 10.1111/j.1365-2591.2006.01099.x. [DOI] [PubMed] [Google Scholar]
- 7.Chandra A. Discuss the factors that affect the outcome of endodontic treatment. Aust Endod J. 2009;35(2):98–107. doi: 10.1111/j.1747-4477.2009.00199.x. [DOI] [PubMed] [Google Scholar]
- 8.Wolcott J, Ishley D, Kennedy W, et al. A 5 yr clinical investigation of second mesiobuccal canals in endodontically treated and retreated maxillary molars. J Endod. 2005;31(4):262–64. doi: 10.1097/01.don.0000140581.38492.8b. [DOI] [PubMed] [Google Scholar]
- 9.Versiani MA, Martins J, Ordinola-Zapata R. Anatomical complexities affecting root canal preparation: a narrative review. Aust Dent J. 2023;68(Suppl 1):S5–S23. doi: 10.1111/adj.12992. [DOI] [PubMed] [Google Scholar]
- 10.Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58(5):589–99. doi: 10.1016/0030-4220(84)90085-9. [DOI] [PubMed] [Google Scholar]
- 11.Bolk L. Bemerkungen über Wurzelvariationen am menschlichen unteren Molaren. Zeitschrift für Morphologie und Anthropologie. 1915;17(3):605–10. [in German] [Google Scholar]
- 12.Tu MG, Huang HL, Hsue SS, et al. Detection of permanent three-rooted mandibular first molars by cone-beam computed tomography imaging in Taiwanese individuals. J Endod. 2009;35(4):503–7. doi: 10.1016/j.joen.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 13.Schäfer E, Breuer D, Janzen S. The prevalence of three-rooted mandibular permanent first molars in a German population. J Endod. 2009;35(2):202–5. doi: 10.1016/j.joen.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Alenezi K, Alharbi B, Kolarkodi SH. Prevalence of three rooted mandibular permanent first molars in Qassim population in Saudi Arabia. International Journal of Medicine in Developing Countries. 2020;4(11):1797–800. [Google Scholar]
- 15.Bakland LK, Baumgartner JC, Ingle JI. Ingle’s endodontics 6. Hamilton, Ontario: BC Decker; 2008. [Google Scholar]
- 16.Walton RE, Torabinejad M. Endodontics: principles and practice. 2009 [Google Scholar]
- 17.Pan JYY, Parolia A, Chuah SR, et al. Root canal morphology of permanent teeth in a Malaysian subpopulation using cone-beam computed tomography. BMC Oral Health. 2019;19(1):14. doi: 10.1186/s12903-019-0710-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plotino G, Tocci L, Grande NM, et al. Symmetry of root and root canal morphology of maxillary and mandibular molars in a white population: A cone-beam computed tomography study in vivo. J Endod. 2013;39(12):1545–48. doi: 10.1016/j.joen.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 19.Caputo BV, Noro Filho GA, de Andrade Salgado DM, et al. Evaluation of the root canal morphology of molars by using cone-beam computed tomography in a Brazilian population: Part I. J Endod. 2016;42(11):1604–7. doi: 10.1016/j.joen.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 20.Shahi S, Yavari HR, Rahimi S, Torkamani R. Root canal morphology of human mandibular first permanent molars in an Iranian population. J Dent Res Dent Clin Dent Prospects. 2008;2(1):20–23. doi: 10.5681/joddd.2008.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker RT. Root form and canal anatomy of mandibular first molars in a southern Chinese population. Endod Dent Traumatol. 1988;4(1):19–22. doi: 10.1111/j.1600-9657.1988.tb00287.x. [DOI] [PubMed] [Google Scholar]
- 22.Kim SY, Kim BS, Woo J, Kim Y. Morphology of mandibular first molars analyzed by cone-beam computed tomography in a Korean population: Variations in the number of roots and canals. J Endod. 2013;39(12):1516–21. doi: 10.1016/j.joen.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 23.Ahmed HA, Abu-bakr NH, Yahia NA, Ibrahim YE. Root and canal morphology of permanent mandibular molars in a Sudanese population. Int Endod J. 2007;40(10):766–71. doi: 10.1111/j.1365-2591.2007.1283.x. [Erratum in: Int Endod J. 2007; 40(12):1008] [DOI] [PubMed] [Google Scholar]
- 24.Mashyakhy M, Chourasia HR, Halboub E, et al. Anatomical variations and bilateral symmetry of roots and root canal system of mandibular first permanent molars in Saudi Arabian population utilizing cone-beam computed tomography. Saudi Dent J. 2019;31(4):481–86. doi: 10.1016/j.sdentj.2019.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mashyakhy M, AlTuwaijri N, Alessa R, et al. Anatomical evaluation of root and root canal morphology of permanent mandibular dentition among the Saudi Arabian population: A systematic review. Biomed Res Int. 2022;2022:2400314. doi: 10.1155/2022/2400314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hess W, Zürcher E, Dolamore WH. The anatomy of the root-canals of the teeth of the permanent dentition. New York: William Wood; 1925. [Google Scholar]
- 27.Weine FS, Healey HJ, Gerstein H, Evanson L. Canal configuration in the mesiobuccal root of the maxillary first molar and its endodontic significance. Oral Surg Oral Med Oral Pathol. 1969;28(3):419–25. doi: 10.1016/0030-4220(69)90237-0. [DOI] [PubMed] [Google Scholar]
- 28.Pineda F, Kuttler Y. Mesiodistal and buccolingual roentgenographic investigation of 7,275 root canals. Oral Surg Oral Med Oral Pathol. 1972;33(1):101–10. doi: 10.1016/0030-4220(72)90214-9. [DOI] [PubMed] [Google Scholar]
- 29.Zheng QH, Wang Y, Zhou XD, et al. A cone-beam computed tomography study of maxillary first permanent molar root and canal morphology in a Chinese population. J Endod. 2010;36(9):1480–84. doi: 10.1016/j.joen.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 30.Tachibana H, Matsumoto K. Applicability of X-ray computerized tomography in endodontics. Endod Dent Traumatol. 1990;6(1):16–20. doi: 10.1111/j.1600-9657.1990.tb00381.x. [DOI] [PubMed] [Google Scholar]
- 31.Cohenca N, Shemesh H. Clinical applications of cone beam computed tomography in endodontics: A comprehensive review. Quintessence Int. 2015;46(8):657–68. doi: 10.3290/j.qi.a34396. [DOI] [PubMed] [Google Scholar]
- 32.Zhang R, Wang H, Tian YY, et al. Use of cone-beam computed tomography to evaluate root and canal morphology of mandibular molars in Chinese individuals. Int Endod J. 2011;44(11):990–99. doi: 10.1111/j.1365-2591.2011.01904.x. [DOI] [PubMed] [Google Scholar]
- 33.Matherne RP, Angelopoulos C, Kulild JC, Tira D. Use of cone-beam computed tomography to identify root canal systems in vitro. J Endod. 2008;34(1):87–89. doi: 10.1016/j.joen.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 34.Neelakantan P, Subbarao C, Subbarao CV. Comparative evaluation of modified canal staining and clearing technique, cone-beam computed tomography, peripheral quantitative computed tomography, spiral computed tomography, and plain and contrast medium-enhanced digital radiography in studying root canal morphology. J Endod. 2010;36(9):1547–51. doi: 10.1016/j.joen.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 35.Blattner TC, George N, Lee CC, et al. Efficacy of cone-beam computed tomography as a modality to accurately identify the presence of second mesiobuccal canals in maxillary first and second molars: A pilot study. J Endod. 2010;36(5):867–70. doi: 10.1016/j.joen.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 36.Yazdizadeh M, Alavinezhad P, Sadrishahrezaei A, Sharifishoshtari S. Root canal morphology of mandibular first molars: Comparison of the diagnostic accuracy of cone-beam computed tomography and the sectioning technique. Dent Res J (Isfahan) 2023;20:103. [PMC free article] [PubMed] [Google Scholar]
- 37.Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007;40(10):818–30. doi: 10.1111/j.1365-2591.2007.01299.x. [DOI] [PubMed] [Google Scholar]
- 38.Cotton TP, Geisler TM, Holden DT, et al. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007;33(9):1121–32. doi: 10.1016/j.joen.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 39.Alswilem R, Abouonq A, Iqbal A, et al. Three-dimensional cone-beam computed tomography assessment of additional canals of permanent first molars: A pinocchio for successful root canal treatment. J Int Soc Prev Community Dent. 2018;8(3):259–63. doi: 10.4103/jispcd.JISPCD_3_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Riyahi AM, Alssum K, Hadadi H, et al. Prevalence of three-rooted mandibular permanent first and second molars in the Saudi population. Saudi Dent J. 2019;31(4):492–95. doi: 10.1016/j.sdentj.2019.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-Alawi H, Al-Nazhan S, Al-Maflehi N, et al. The prevalence of radix molaris in the mandibular first molars of a Saudi subpopulation based on cone-beam computed tomography. Restor Dent Endod. 2019;45(1):e1. doi: 10.5395/rde.2020.45.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Silva EJ, Nejaim Y, Silva AV, et al. Evaluation of root canal configuration of mandibular molars in a Brazilian population by using cone-beam computed tomography: An in vivo study. J Endod. 2013;39(7):849–52. doi: 10.1016/j.joen.2013.04.030. [DOI] [PubMed] [Google Scholar]
- 43.de Pablo OV, Estevez R, Péix Sánchez M, et al. Root anatomy and canal configuration of the permanent mandibular first molar: A systematic review. J Endod. 2010;36(12):1919–31. doi: 10.1016/j.joen.2010.08.055. [DOI] [PubMed] [Google Scholar]
- 44.Senan EM, Madfa AA, Alhadainy HA. Root and canal configuration of mandibular first molars in a Yemeni population: A cone-beam computed tomography. Eur Endod J. 2020;5(1):10–17. doi: 10.14744/eej.2020.99609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alfawaz H, Alqedairi A, Alkhayyal AK, et al. Prevalence of C-shaped canal system in mandibular first and second molars in a Saudi population assessed via cone beam computed tomography: A retrospective study. Clin Oral Investig. 2019;23(1):107–12. doi: 10.1007/s00784-018-2415-0. [DOI] [PubMed] [Google Scholar]
- 46.Al Qarni MA. Variations in root canal morphology of mandibular first molar in Assir population. Pakistan Oral & Dental Journal. 2016;36(2):293. [Google Scholar]
- 47.Marwat T, Nausheen N, Nasir U. Determination of number and configuration of canals in permanent lower first molar by cone beam computed tomography. Khyber Medical University Journal. 2019;11(1):32–36. [Google Scholar]
- 48.Kim Y, Roh BD, Shin Y, et al. Morphological characteristics and classification of mandibular first molars having 2 distal roots or canals: 3-dimensional biometric analysis using cone-beam computed tomography in a Korean population. J Endod. 2018;44(1):46–50. doi: 10.1016/j.joen.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 49.Al-Nazhan S. The prevelance of two canals in MB root of endodonticallyl treated maxillary first molars among Saudi Arabian sub. Saudi Dent J. 2005;17:24–28. [Google Scholar]
- 50.Rahimi S, Mokhtari H, Ranjkesh B, et al. Prevalence of extra roots in permanent mandibular first molars in Iranian population: A CBCT Analysis. Iran Endod J. 2017;12(1):70–73. doi: 10.22037/iej.2017.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Y, Zheng QH, Zhou XD, et al. Evaluation of the root and canal morphology of mandibular first permanent molars in a western Chinese population by cone-beam computed tomography. J Endod. 2010;36(11):1786–89. doi: 10.1016/j.joen.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 52.Pan JYY, Parolia A, Chuah SR, et al. Root canal morphology of permanent teeth in a Malaysian subpopulation using cone-beam computed tomography. BMC Oral Health. 2019;19(1):14. doi: 10.1186/s12903-019-0710-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Song JS, Choi HJ, Jung IY, et al. The prevalence and morphologic classification of distolingual roots in the mandibular molars in a Korean population. J Endod. 2010;36(4):653–57. doi: 10.1016/j.joen.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 54.Duman SB, Duman S, Bayrakdar IS, et al. Evaluation of radix entomolaris in mandibular first and second molars using cone-beam computed tomography and review of the literature. Oral Radiol. 2020;36(4):320–26. doi: 10.1007/s11282-019-00406-0. [Erratum in: Oral Radiol. 2022;38(3):443] [DOI] [PubMed] [Google Scholar]
- 55.Gu Y, Lu Q, Wang H, et al. Root canal morphology of permanent three-rooted mandibular first molars – part I: Pulp floor and root canal system. J Endod. 2010;36(6):990–94. doi: 10.1016/j.joen.2010.02.030. [DOI] [PubMed] [Google Scholar]
- 56.Krasner P, Rankow HJ. Anatomy of the pulp-chamber floor. J Endod. 2004;30(1):5–16. doi: 10.1097/00004770-200401000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Wilcox LR, Walton RE, Case WB. Molar access: Shape and outline according to orifice locations. J Endod. 1989;15(7):315–18. doi: 10.1016/S0099-2399(89)80054-8. [DOI] [PubMed] [Google Scholar]
- 58.Cimilli H, Mumcu G, Cimilli T, et al. The correlation between root canal patterns and interorificial distance in mandibular first molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(2):e16–21. doi: 10.1016/j.tripleo.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 59.Iqbal A. The factors responsible for endodontic treatment failure in the permanent dentitions of the patients reported to the College of Dentistry, the University of Aljouf, Kingdom of Saudi Arabia. J Clin Diagn Res. 2016;10(5):ZC146–48. doi: 10.7860/JCDR/2016/14272.7884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Karabucak B, Bunes A, Chehoud C, et al. Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: A cone-beam computed tomography study. J Endod. 2016;42(4):538–41. doi: 10.1016/j.joen.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 61.Mashyakhy M, Hadi FA, Alhazmi HA, et al. Prevalence of missed canals and their association with apical periodontitis in posterior endodontically treated teeth: A CBCT study. Int J Dent. 2021;2021:9962429. doi: 10.1155/2021/9962429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chourasia HR, Meshram GK, Warhadpande M, Dakshindas D. Root canal morphology of mandibular first permanent molars in an Indian population. Int J Dent. 2012;2012:745152. doi: 10.1155/2012/745152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Talari K, Goyal M. Retrospective studies – utility and caveats. J R Coll Physicians Edinb. 2020;50(4):398–402. doi: 10.4997/JRCPE.2020.409. [DOI] [PubMed] [Google Scholar]
- 64.Venskutonis T, Plotino G, Juodzbalys G, Mickevičienė L. The importance of cone-beam computed tomography in the management of endodontic problems: A review of the literature. J Endod. 2014;40(12):1895–901. doi: 10.1016/j.joen.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 65.American Association of Endodontists; American Acadamey of Oral and Maxillofacial Radiography. AAE and AAOMR joint position statement. Use of cone-beam-computed tomography in endodontics. Pa Dent J (Harrisb) 2011;78(1):37–39. [PubMed] [Google Scholar]