Abstract
Background:
Previous research in sport populations has demonstrated that abnormal magnetic resonance imaging (MRI) findings may be present in individuals without symptoms or known pathology. Extending this understanding to ballet, particularly in relation to the foot and ankle, is important to guide medical advice given to dancers.
Purpose:
To assess foot and ankle MRI scans in asymptomatic ballet dancers focusing on bone marrow edema and the posterior ankle and to investigate whether these MRI findings would become symptomatic within 1 year.
Study Design:
Case series; Level of evidence, 4.
Methods:
In total, 31 healthy dancers (62 feet/ankles; 15 male and 16 female; age, 26.5 ± 4.3 years) who were dancing in full capacity were recruited from an elite professional ballet company. Orthogonal 3-plane short tau inversion recovery imaging of both feet and ankles was obtained using 3T MRI and the images were reviewed using a standardized evaluation form by 2 musculoskeletal radiologists. Injuries in the company were recorded and positive MRI findings were assessed for correlation with any injuries requiring medical attention during the subsequent 12 months.
Results:
A total of 51 (82%) of the 62 feet and ankles had ≥1 area of bone marrow edema. The most common locations of bone marrow edema were the talus (n = 41; 66%), followed by first metatarsal (n = 14; 23%). Os trigonum and Stieda process were seen in 5 (8%) and 8 (13%) ankles, respectively. Among them, 2 os trigona showed bone marrow edema. Fluid in the anterior and posterior talocrural joints and the subtalar joint was observed in 48%, 63%, and 63% of these joints, respectively. Fluid around foot and ankle tendons was observed, with the most prevalent being the flexor hallucis longus tendon (n = 13; 21%). Two dancers who had positive findings on their MRI subsequently developed symptoms during the next 12 months.
Conclusion:
Positive MRI findings are commonplace in the foot and ankle of asymptomatic professional ballet dancers. The majority do not result in the development of symptoms requiring medical attention within 12 months. Careful interpretation of MRI findings with the dancer's clinical picture is required before recommending activity modification or further intervention.
Keywords: dance, ballet, foot, ankle, imaging, magnetic resonance, posterior ankle impingement syndrome, bone marrow edema, sports medicine
Injuries to the lower limb constitute some of the highest injury burden in elite ballet dancers, with the majority occurring in either the foot or the ankle.12,22,24,28,34 The use of magnetic resonance imaging (MRI) is considered the gold standard imaging tool for the most common injuries such as posterior ankle impingement syndrome (PAIS), ligamentous injury, and bone stress reaction.1,14,29
It is known from research in sports populations that positive MRI findings can be found in individuals without symptoms or known pathology.6,10,16,20,26,35 Bone marrow edema in asymptomatic athletes has been reported in several sports such as ankles in runners, 16 knees in swimmers, 35 pubis in footballers, 6 and knees in basketball players. 20 Patellar tendinopathy, quadriceps tendinopathy, and cartilage findings were common in asymptomatic collegiate basketball players. 26 Peritendinous fluid was found in elite, asymptomatic rowers’ wrists. 10 These findings seen on MRI scans can be secondary to the repetitive high loads to which athletes are exposed during training, and they may not be pathological or related to an injury.6,10,16,20 Extending this understanding to ballet is important for medical practitioners to better understand MRI findings and subsequently provide accurate advice to dancers.
Studies have shown a high prevalence of bone marrow edema in the talus and cuneiform bones in ballet dancers, but these studies were limited in participant numbers, low-resolution imaging, and inclusion of dancers with pain.11,13,22 Furthermore, they have not examined the forefoot, which is also a common site of pathology in ballet dancers. 15 A previous MRI study of PAIS in 25 ballet dancers lacked a control group, making it difficult to exclude the possibility that the MRI features were related to training intensity. 27 Although a recent cross-sectional study found no association between symptoms and MRI findings for PAIS in ballet dancers, whether dancers with positive MRI findings subsequently developed PAIS was not investigated. 5 Therefore, further research is required to better understand the positive MRI findings in asymptomatic ballet dancers and their relationship to future symptoms.
The aims of this study were to (1) assess foot and ankle MRI findings in asymptomatic ballet dancers focusing on bone marrow edema and posterior ankle impingement and (2) investigate whether these MRI findings would become symptomatic within 1 year.
Methods
Participants
This prospective study recruited 31 healthy dancers (15 male and 16 female; age, 26.5 ± 4.3 years) who were dancing in full capacity at an elite professional ballet company with about 75% of its repertoire being classical. MRIs were taken during the rehearsal period at around the ninth month of an 11-month season, when dancers usually take 1.25 hour–long classes 6 days per week and join some rehearsals. Dancers were excluded from participating in this study if they had experienced an ankle sprain, PAIS, or any other foot or ankle pain requiring modification of dance activities for >1 week, previous foot or ankle surgery, and fracture or bone stress reaction to the foot or ankle in the past 6 months. Research ethics committee approval was given (reference No. 272602), and written informed consent was obtained from each participant before participation.
Magnetic Resonance Imaging
Orthogonal 3-plane MRIs were scanned for both feet and ankles using a Siemens 3-T scanner (Siemens, Healthcare) using imaging parameters as follows: sagittal short tau inversion recovery (STIR) (slice thickness [ST], 3 mm; repetition time [TR], 5550 ms; inversion time [TI], 140 ms; echo time [TE], 31 ms; matrix, 320 × 320); axial STIR (ST, 3 mm; TR, 5860 ms; TI, 140 ms; TE, 31 ms; matrix, 320 × 320); and coronal STIR (ST, 3.5 mm; TR, 5080 ms; TI, 140 ms; TE, 31 ms; matrix, 256 × 256). To ensure homogeneous marrow fat suppression, short T1-inversion imaging was acquired rather than spectral fat saturation. Spectral fat saturation in the foot and ankle can be subject to artifact making the identification of bone marrow edema inaccurate. Hence, STIR sequence was selected for this study. STIR sequence is the most sensitive sequence for bone marrow edema, joint effusion, and tendon sheath effusion detection in the foot and ankle. STIR wide field of view (FOV, 270 mm) whole foot and ankle imaging was performed to optimize study scan time, as whole marrow area can be assessed in 3 planes within allotted time per patient. Fine detail analysis of soft tissues was not required for this project. MRI scans were independently reviewed using a standardized evaluation form by 2 experienced fellowship-trained musculoskeletal radiologists (J.C.L. and A.W.M.M.) each with >20 years of experience, with findings being agreed through consensus. The following abnormalities were evaluated: bone marrow edema, PAIS-related findings such as os trigonum and Stieda process, joint effusion, and fluid around tendons.
The evaluation form included:
Bone marrow edema: presence or absence of bone marrow edema of anterior, middle, and posterior tibia; head, neck, body, and posterior process of the talus; anteromedial, anterolateral, and insertion of Achilles tendon; around the posterior subtalar joint and other areas of the calcaneus; tarsal bones; first to fifth metatarsals; first to fifth phalanges; and medial and lateral sesamoids. It was graded using the grading of Lazzarini: 0 (no edema), 1 (increased signal intensity involving <25% of the bone), 2 (increased signal intensity involving 25% to 50% of the bone), and 3 (increased signal intensity involving >50% of the bone). 19
Findings associated with PAIS: presence or absence of os trigonum and Stieda process and, if present, existence of high signal area. In addition, presence or absence of local synovitis involving the posterior tibiotalar and subtalar joints, thickening of posterior capsule, and existence of intermalleolar ligament were evaluated.
Joint effusion and effusion at retrocalcaneal bursa: presence or absence of effusion at anterior tibiotalar joint, posterior tibiotalar joint, posterior subtalar joint, and retrocalcaneal bursa.
Tendons: presence or absence of fluid around flexor hallucis longus (FHL), peroneal, and posterior tibialis tendons. It was graded using the grading by Schweitzer: 0 (no fluid) and 1, 2, and 3 (radius of the fluid collection <0.25, 0.25-1.0, and >1.0 times the diameter of the tendon, respectively). 32
Injury Record Analysis
All injuries were recorded by in-house chartered physical therapists with 13 years of experience on mean within 24 hours of their onset using a standardized injury assessment form (Version 6.5.11; Smartabase). Injury diagnosis was recorded using Version 10 of the Orchard Sports Injury Classification System as recommended in the International Olympic Committee consensus statement.3,8 Positive MRI findings were assessed for correlation with any medical attention injuries that had taken place in the subsequent 12 months. In the 12-month period, there were 5 weeks of rehearsals only, 38 weeks of rehearsals and performances, 3 weeks of tour, and 6 weeks of holiday.
Results
Foot and Ankle Abnormalities
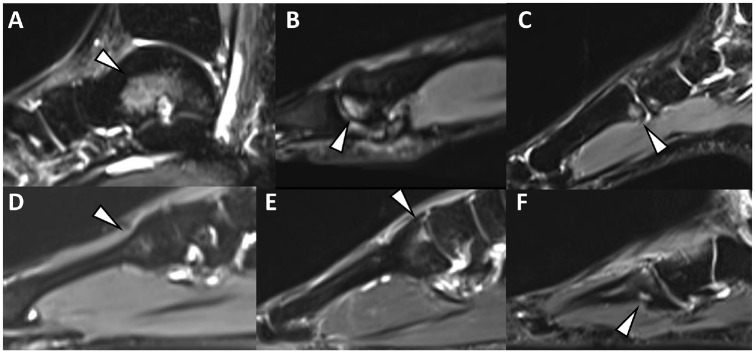
A total of 51 feet and ankles (82%) had ≥1 site with bone marrow edema. Table 1 shows the details of the locations and grades of the bone marrow edema, and Figure 1 shows the examples of the findings. The most common sites were the talus (n = 41; 66%), followed by first metatarsal (n = 14; 23%), distal tibia (n = 7; 11%), cuboid (n = 5; 8%), medial cuneiform (n = 5; 8%), medial sesamoid (n = 5; 8%), and second metatarsal (n = 4; 6%). While 74% of all the bone marrow oedema were grade 1, grades 2 (17%) and 3 (9%) were also observed (Figure 1A). The location of the bone marrow edema within the talus was as follows: head (n = 11), neck (n = 16), body (n = 32), and posterior process (n = 1), and that of the first metatarsal was as follows: head only (n = 8); base only (n = 3); head and shaft (n = 2); and head, shaft, and base (n = 1). Bone marrow edema within the second metatarsal was seen in the base (n = 2), shaft and base (n = 1), and head and base (n = 1). Two of the second metatarsal base bone marrow edemas were seen beside the joint, resembling degenerative changes (Figure 1E).
Table 1.
Locations and Grade of Bone Marrow Edema Lesions a
| Overall | Grade | ||||||
|---|---|---|---|---|---|---|---|
| n (%) | Female | Male | 1 | 2 | 3 | ||
| Distal tibia | |||||||
| Anterior | 2 (3.2) | 1 | 1 | 2 | 0 | 0 | |
| Middle | 3 (4.8) | 1 | 2 | 3 | 0 | 0 | |
| Posterior | 2 (3.2) | 0 | 2 | 2 | 0 | 0 | |
| Talus | |||||||
| Head | 11 (17.7) | 8 | 3 | 7 | 4 | 0 | |
| Neck | 16 (25.8) | 9 | 7 | 10 | 6 | 0 | |
| Body | 32 (51.6) | 18 | 14 | 20 | 7 | 5 | |
| Posterior process | 1 (1.6) | 0 | 1 | 1 | 0 | 0 | |
| Calcaneus | |||||||
| Place of PAIS | 1 (1.6) | 0 | 1 | 1 | 0 | 0 | |
| Insertion of Achilles tendon | 1 (1.6) | 0 | 1 | 0 | 0 | 1 | |
| Anterolateral | 1 (1.6) | 0 | 1 | 1 | 0 | 0 | |
| Cuboid | 5 (8.1) | 3 | 2 | 5 | 0 | 0 | |
| Navicular | 3 (4.8) | 0 | 3 | 3 | 0 | 0 | |
| Cuneiform | |||||||
| Lateral | 1 (1.6) | 0 | 1 | 0 | 0 | 1 | |
| Intermediate | 2 (3.2) | 1 | 1 | 2 | 0 | 0 | |
| Medial | 5 (8.1) | 3 | 2 | 5 | 0 | 0 | |
| Metatarsal | |||||||
| First | 14 (22.6) | 6 | 8 | 14 | 0 | 0 | |
| Second | 4 (6.5) | 2 | 2 | 3 | 1 | 0 | |
| Fourth | 1 (1.6) | 1 | 0 | 1 | 0 | 0 | |
| Fifth | 1 (1.6) | 0 | 1 | 1 | 0 | 0 | |
| Phalange | |||||||
| First | 3 (4.8) | 0 | 3 | 2 | 0 | 1 | |
| Fifth | 1 (1.6) | 0 | 1 | 1 | 0 | 0 | |
| Sesamoid | |||||||
| Medial | 5 (8.1) | 3 | 2 | 1 | 2 | 2 | |
Data are presented as n unless otherwise indicated. PAIS, posterior ankle impingement syndrome.
Figure 1.
Examples of bone marrow edema (arrowheads). (A) Talar body, (B) first metatarsal head, (C) first metatarsal base, (D, E) second metatarsal base, and (F) fourth metatarsal base.
Specific findings relating to PAIS demonstrated an os trigonum in 5 (8%) and Stieda process in 8 (13%) ankles, 1 and 2 of which were bilateral, respectively. Among them, 2 os trigona showed bone marrow edema, but no Stieda process had bone marrow edema (Figure 2). Additionally, the posterior intermalleolar ligament was seen in 31 ankles (50%). Posterior synovitis was seen in 11 ankles (18%) and posterior capsular thickening was observed in 6 ankles (10%). Other findings and details are shown in Table 2.
Figure 2.
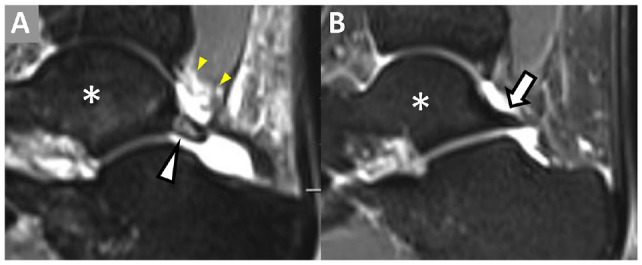
(A) Os trigonum with high signal intensity (white arrowhead) and synovitis (yellow arrowheads). (B) Stieda process (arrow). *, talus.
Table 2.
Findings Associated With PAIS a
| Overall | |||
|---|---|---|---|
| n (%) | Female, n | Male, n | |
| Anatomic variants at the posterior ankle | |||
| Os trigonum | 5 (8) | 3 | 2 |
| Stieda process | 8 (13) | 4 | 4 |
| Posterior intermalleolar ligament | 31 (50) | 12 | 19 |
| MRI features of PAIS | |||
| Bone marrow edema | |||
| Os trigonum | 2 (3) | 1 | 1 |
| Stieda process | 0 (0) | 0 | 0 |
| Synchondrosis high signal in os trigonum | 2 (3) | 1 | 1 |
| Posterior synovitis | 11 (18) | 4 | 7 |
| Posterior capsular thickening | 6 (10) | 3 | 3 |
MRI, magnetic resonance imaging; PAIS, posterior ankle impingement syndrome.
The presence of joint fluid and fluid around tendons is summarized in Table 3. Joint fluid was commonly observed in tibiotalar and subtalar joints (Figure 3A) and fluid around the tendons most observed around the FHL (n = 13; 21%) (Figure 3B).
Table 3.
MRI Findings of Joint and Tendon Fluid a
| Overall | |||||
|---|---|---|---|---|---|
| n (%) | Female, n | Male, n | Note | ||
| Joint fluid | |||||
| Anterior tibiotalar | 30 (48) | 16 | 14 | ||
| Posterior tibiotalar | 39 (63) | 20 | 19 | ||
| Posterior subtalar | 39 (63) | 22 | 17 | ||
| Retrocalcaneal bursa | 9 (15) | 6 | 3 | ||
| Fluid around tendon | |||||
| FHL | 13 (21) | 7 | 6 | Grade 1 (n = 3), grade 2 (n = 6), grade 3 (n = 4) | |
| Peroneal | 6 (10) | 4 | 2 | Grade 1 (n = 4), grade 2 (n = 2), grade 3 (n = 0) | |
| Posterior tibialis | 8 (13) | 5 | 3 | Grade 1 (n = 4), grade 2 (n = 3), grade 3 (n = 1) | |
FHL, flexor hallucis longus; MRI, magnetic resonance imaging.
Figure 3.
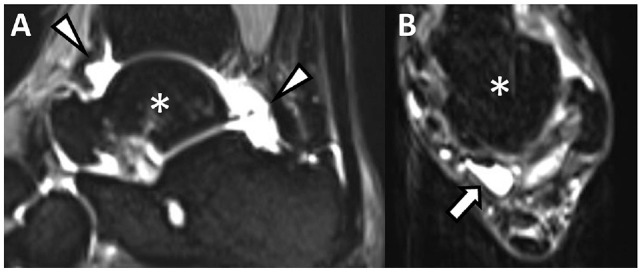
(A) Joint fluid around tibiotalar joint and subtalar joint (arrowheads). (B) Fluid around flexor hallucis longus tendon (arrow). *, talus.
Development of Foot and Ankle Pain Related to MRI Findings Within 1 Year
Fourteen foot and ankle medical attention injuries such as PAIS, anterior ankle impingement syndrome, Achilles tendinopathy, sprain of the first metatarsophalangeal joint, and foot muscle spasm were observed within the following 12 months; 2 of the injuries could be attributed to abnormalities on the MRI scan. One ankle with bone marrow edema at the distal anterior tibia and anterior ankle joint fluid went on to develop anterior ankle impingement syndrome (Figure 4A) and 1 ankle with Stieda process went on to develop FHL symptoms (Figure 4B).
Figure 4.
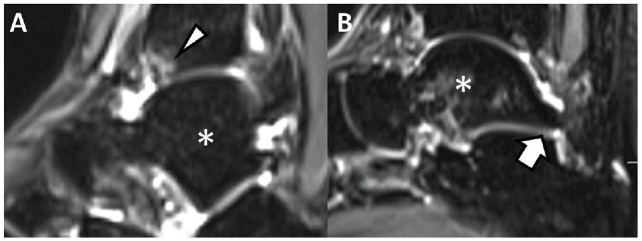
(A) Bone marrow edema at the distal anterior tibia (arrowhead). (B) Stieda process (arrow). *, talus.
Discussion
This study assessed foot and ankle MRI findings in 31 asymptomatic professional ballet dancers and investigated whether the MRI findings would become symptomatic within 1 year. The most important finding of the present study is that positive MRI findings in the foot and ankle of asymptomatic ballet dancers are highly prevalent but very few of these become symptomatic within 1 year. Of the asymptomatic professional ballet dancers’ foot and ankle MRIs, 82% had ≥1 site of bone marrow edema. Furthermore, joint fluid and fluid around key foot and ankle tendons is a common finding. These abnormalities may be due to physiological stress during dancing. Furthermore, these results suggest that abnormal findings should be expected on MRI investigations of the feet and ankles of elite ballet dancers. Only 2 positive findings went on to correlate with subsequent injuries, suggesting that dancers may not need to modify activity immediately when such MRI abnormalities are observed without any symptoms.
The most common finding was bone marrow edema. Pathologic cause of bone marrow edema on MRI includes fracture, stress response, infection, tumor, and avascular necrosis.18,23,36 More importantly, however, medical practitioners must assess whether bone marrow edema in this asymptomatic cohort would be an indicator of those who would go on to experience these pathologies, pain, or injury. High prevalence of bone marrow edema in asymptomatic athletes has been reported,6,16,20,35 and 1 study 17 showed most asymptomatic runners showed bone marrow edema lesions, more than half of them fluctuating during the season, and clinical complaints occurring during the season were not related to the bone marrow edema. Similar results were observed in the present study; only 1 site of bone marrow edema went on to become symptomatic within a 12-month period. The cause of these MRI changes remains unclear, but they may be related to biomechanical stress related to the dancing, which can lead to bone remodeling.17,19,33
The talus was the most common site for bone marrow edema. This is in keeping with a previous study where 9 of the 12 ankle MRIs of active professional dancers showed bone marrow edema of the talus. 11 However, previous studies included dancers with pain, and imaging studies among asymptomatic dancers are scarce. Furthermore, MRI studies of asymptomatic ballet dancers’ feet have not been investigated. The present study investigated foot MRI findings, as well as those of the ankle, and it was revealed that, after the talus, the bones mostly affected were at the medial side of the foot including first metatarsal, medial cuneiform, and medial sesamoid. Bone marrow edema in the asymptomatic foot and ankle has been also reported in professional, university, and amateur runners.17,19,37 Bone marrow edema was seen mostly in the calcaneus (19%-40%), talus (16%-31%), and navicular (3.3%-27.5%). The current study suggests that the frequency of bone marrow edema of the talus is greater in professional ballet dancers compared with runners, whereas the reverse is true for the calcaneus. Although most bone marrow edema did not become symptomatic within 1 year, distribution of the bone marrow edema may represent areas of higher biomechanical stress in ballet. Demi pointe and en pointe positions require weightbearing in maximal ankle and midfoot plantarflexion,30,31 and ballet-specific landing technique starts from the toe rather than the heel. 2 Ballet is also performed in varying degrees of hip external rotation or “turn out.” Dancing, jumping, and landing with external rotation of the hips will put greater strain on the medial structures of the foot and ankle. 7 Clinicians should be aware that these sites are likely to express varying levels of bone stress.
Stress fractures pose a significant burden to ballet dancers, and the base of the second metatarsal is a commonly affected site.15,22,25 Thus, it would be useful if we could understand whether the bone marrow edema at the base of the second metatarsal in asymptomatic ballet dancers would lead to symptomatic stress fractures. In our study, we observed a low prevalence of bone marrow edema at the base of the second metatarsal (4 feet; 6.5%). Two appeared to be degenerative in nature rather than stress reaction and those remaining were of low intensity. Given the low prevalence of bone marrow edema at the base of the second metatarsal in this asymptomatic cohort, clinicians should remain vigilant when symptomatic or asymptomatic dancers exhibit positive MRI findings in this area.
PAIS is one of the most common problems in ballet dancers.15,21 In a recent study, it was reported that there was no association between MRI findings and posterior ankle pain or a positive ankle plantarflexion pain provocation test. 5 The study raised questions regarding the significance of MRI features in the management of PAIS. However, it is important to note that the study had a limited number of participants and included individuals engaged in different activities, such as dancers and athletes. 5 In a retrospective review of 25 MRI examinations of the ankles conducted on 23 ballet dancers who sought orthopaedic consultation and were clinically diagnosed with PAIS, the authors aimed to determine the prevalence of MRI features in this specific population. 27 The most frequently observed imaging feature of PAIS was posterior synovitis (100%). Additionally, thickening of the posterior capsule (52%) and tenosynovitis of the FHL (68%) were common findings. Os trigonum was present in 28% of the cases, and among them, 86% exhibited bone marrow edema. Furthermore, bone marrow edema in the posterior talus was frequently observed (40%). 27 Although these imaging features can assist in the clinical management of individual patients, the study suggests caution when comparing these common MRI findings in the population, as these features might represent variations of normal for this particular group of patients due to the intensity of their training. 27 While the direct comparison between the current study and the literature is challenging due to differences in MRI evaluation, methods, and participant backgrounds, the presence of the aforementioned features was less prevalent in asymptomatic dancers in the present study compared with those diagnosed with PAIS in previous literature. 27 However, it is important to note that these features were still present, albeit to a lesser extent, in the asymptomatic population. This implies a potential correlation between these MRI findings and pathology or pain, emphasizing the need for cautious interpretation of the MRI features and comprehensive clinical assessment in the diagnosis and management of PAIS.
Joint fluid in talocrural and subtalar joints is often seen even in the asymptomatic general population, with joint fluid seen on the MRI in 87% to 96% of healthy volunteers.9,32 No statistical difference in the presence of joint fluid around the ankle was found between volunteers and patients with various ankle disorders such as occult fractures, osteochondritis dissecans, and Achilles tendon disorders. 32 Few studies have investigated the prevalence of joint fluid in ballet dancers, but 1 study reported posterior subtalar or talocrural joint effusion synovitis in 95% to 100% of active ballet dancers. 4 Although less common, the authors also noted joint fluid in the anterior talocrural joint, posterior talocrural joint, and subtalar joint as a common finding. This suggests that careful interpretation should be made when observing ankle joint fluid in the ankle of a ballet dancer.
Tendon pain is a common injury among ballet dancers. 15 Fluid around the tendons is more commonly reported with fluid in the tendon sheath of the FHL, posterior tibialis, and peroneus longus tendon observed in 17% to 31% of a healthy population and patients with various ankle symptoms. 32 Among ballet dancers, tenosynovitis was observed in 21.1% of the actively dancing dancers. 4 This is consistent with the findings of our study. Interestingly, the presence of grade 3 fluid did not progress to become symptomatic within 12 months. Therefore, a large volume of fluid found within a tendon sheath does not always correlate with symptoms.
Limitations
This study is not without limitations. First, because the primary purpose was to investigate the presence of bone marrow edema, only STIR sequences were taken, so ligaments and tendons were not assessed. Second, some participants may have not declared incidences of pain, as their dancing activities were not affected. However, we attempted to minimize this risk by excluding the dancers with foot or ankle pain requiring assessment from the medical team and any modification of dance activities that lasted for >1 week in the past 6 months. Third, there was no control group of nonathletes and nonathletes performing dance. Instead, the results were compared with literature on nonathletes and athletes.
Conclusion
There is a high prevalence of abnormal findings on MRIs of the foot and ankle in asymptomatic professional ballet dancers. The majority of these do not result in either medical attention or time-loss injury within 12 months. Common findings in active professional ballet dancers include bone marrow edema of the talus and first metatarsal head, tibiotalar and subtalar joint fluid, and fluid around the FHL tendon. Therefore, careful interpretation of MRI findings with the dancer's clinical picture is required before recommending activity modification or further intervention.
Acknowledgments
The authors thank all the dancers who participated in this study and the physical therapists and doctors who worked with the Royal Ballet and recorded the injury data used in this study. The authors also thank Mrs Carol Brigstocke and the Royal Opera House for funding this study.
Footnotes
Final revision submitted January 28, 2024; accepted February 13, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by Mrs Carol Brigstocke and the Royal Opera House. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from West Midlands—Coventry & Warwickshire Research Ethics Committee (ref No. 272602).
References
- 1. Albisetti W, Perugia D, De Bartolomeo O, Tagliabue L, Camerucci E, Calori GM. Stress fractures of the base of the metatarsal bones in young trainee ballet dancers. Int Orthop. 2010;34(1):51-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Azevedo AM, Oliveira R, Vaz JR, Cortes N. Oxford foot model kinematics in landings: a comparison between professional dancers and non-dancers. J Sci Med Sport. 2020;23(4):347-352. [DOI] [PubMed] [Google Scholar]
- 3. Bahr R, Clarsen B, Derman W, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br J Sports Med. 2020;54(7):372-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baillie P, Cook J, Ferrar K, Smith P, Lam J, Mayes S. Magnetic resonance imaging findings associated with posterior ankle impingement syndrome are prevalent in elite ballet dancers and athletes. Skeletal Radiol. 2021;50(12):2423-2431. [DOI] [PubMed] [Google Scholar]
- 5. Baillie P, Ferrar K, Cook J, Smith P, Lam J, Mayes S. Posterior ankle impingement syndrome clinical features are not associated with imaging findings in elite ballet dancers and athletes. Clin J Sport Med. 2022;32(6):600-607. [DOI] [PubMed] [Google Scholar]
- 6. Branci S, Thorborg K, Bech BH, Boesen M, Nielsen MB, Holmich P. MRI findings in soccer players with long-standing adductor-related groin pain and asymptomatic controls. Br J Sports Med. 2015;49(10):681-691. [DOI] [PubMed] [Google Scholar]
- 7. Carter SL, Bryant AR, Hopper LS. An analysis of the foot in turnout using a dance specific 3D multi-segment foot model. J Foot Ankle Res. 2019;12:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Clarsen B, Bahr R. Matching the choice of injury/illness definition to study setting, purpose and design: one size does not fit all! Br J Sports Med. 2014;48(7):510-512. [DOI] [PubMed] [Google Scholar]
- 9. De Grove V, Willekens I, Lenchik L, Shahabpour M, de Mey J, De Maeseneer M. Fluid distribution in ankle and midfoot joints: MR findings in asymptomatic volunteers. Surg Radiol Anat. 2018;40(5):481-487. [DOI] [PubMed] [Google Scholar]
- 10. Drew MK, Trease L, Caneiro JP, et al. Normative MRI, ultrasound and muscle functional MRI findings in the forearms of asymptomatic elite rowers. J Sci Med Sport. 2016;19(2):103-108. [DOI] [PubMed] [Google Scholar]
- 11. Elias I, Zoga AC, Raikin SM, et al. Bone stress injury of the ankle in professional ballet dancers seen on MRI. BMC Musculoskelet Disord. 2008;9:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Garrick JG, Requa RK. Ballet injuries: an analysis of epidemiology and financial outcome. Am J Sports Med. 1993;21(4):586-590. [DOI] [PubMed] [Google Scholar]
- 13. Gorelik N, Casagranda BU, Colucci PG, et al. Spotty bone marrow: a frequent MRI finding in the feet of ballet dancers. J Dance Med Sci. 2022;26(2):125-133. [DOI] [PubMed] [Google Scholar]
- 14. Hillier JC, Peace K, Hulme A, Healy JC. Pictorial review: MRI features of foot and ankle injuries in ballet dancers. Br J Radiol. 2004;77(918):532-537. [DOI] [PubMed] [Google Scholar]
- 15. Katakura M, Kedgley AE, Shaw JW, et al. Epidemiological characteristics of foot and ankle injuries in 2 professional ballet companies: a 3-season cohort study of 588 medical attention injuries and 255 time-loss injuries. Orthop J Sports Med. 2023;11(2):23259671221134131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kornaat PR, de Jonge MC, Maas M. Bone marrow edema-like signal in the athlete. Eur J Radiol. 2008;67(1):49-53. [DOI] [PubMed] [Google Scholar]
- 17. Kornaat PR, Van de Velde SK. Bone marrow edema lesions in the professional runner. Am J Sports Med. 2014;42(5):1242-1246. [DOI] [PubMed] [Google Scholar]
- 18. Kroon HM, Bloem JL, Holscher HC, van der Woude HJ, Reijnierse M, Taminiau AH. MR imaging of edema accompanying benign and malignant bone tumors. Skeletal Radiol. 1994;23(4):261-269. [DOI] [PubMed] [Google Scholar]
- 19. Lazzarini KM, Troiano RN, Smith RC. Can running cause the appearance of marrow edema on MR images of the foot and ankle? Radiology. 1997;202(2):540-542. [DOI] [PubMed] [Google Scholar]
- 20. Major NM, Helms CA. MR imaging of the knee: findings in asymptomatic collegiate basketball players. AJR Am J Roentgenol. 2002;179(3):641-644. [DOI] [PubMed] [Google Scholar]
- 21. Mattiussi AM, Shaw JW, Williams S, et al. Injury epidemiology in professional ballet: a five-season prospective study of 1596 medical attention injuries and 543 time-loss injuries. Br J Sports Med. 2021;55(15):843-850. [DOI] [PubMed] [Google Scholar]
- 22. Miskovsky S, Khambete P, Faraji N, et al. Prevalence of asymptomatic talar bone marrow edema in professional ballet dancers: preliminary data from a 2-year prospective study. Orthop J Sports Med. 2023;11(5):23259671231159910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Morrison WB, Schweitzer ME, Bock GW, et al. Diagnosis of osteomyelitis: utility of fat-suppressed contrast-enhanced MR imaging. Radiology. 1993;189(1):251-257. [DOI] [PubMed] [Google Scholar]
- 24. Nilsson C, Leanderson J, Wykman A, Strender LE. The injury panorama in a Swedish professional ballet company. Knee Surg Sports Traumatol Arthrosc. 2001;9(4):242-246. [DOI] [PubMed] [Google Scholar]
- 25. O’Malley MJ, Hamilton WG, Munyak J, DeFranco MJ. Stress fractures at the base of the second metatarsal in ballet dancers. Foot Ankle Int. 1996;17(2):89-94. [DOI] [PubMed] [Google Scholar]
- 26. Pappas GP, Vogelsong MA, Staroswiecki E, Gold GE, Safran MR. Magnetic resonance imaging of asymptomatic knees in collegiate basketball players: the effect of one season of play. Clin J Sport Med. 2016;26(6):483-489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Peace KA, Hillier JC, Hulme A, Healy JC. MRI features of posterior ankle impingement syndrome in ballet dancers: a review of 25 cases. Clin Radiol. 2004;59(11):1025-1033. [DOI] [PubMed] [Google Scholar]
- 28. Ramkumar PN, Farber J, Arnouk J, Varner KE, McCulloch PC. Injuries in a professional ballet dance company: a 10-year retrospective study. J Dance Med Sci. 2016;20(1):30-37. [DOI] [PubMed] [Google Scholar]
- 29. Roche AJ, Calder JD, Lloyd Williams R. Posterior ankle impingement in dancers and athletes. Foot Ankle Clin. 2013;18(2):301-318. [DOI] [PubMed] [Google Scholar]
- 30. Russell JA, Shave RM, Kruse DW, Koutedakis Y, Wyon MA. Ankle and foot contributions to extreme plantar- and dorsiflexion in female ballet dancers. Foot Ankle Int. 2011;32(2):183-188. [DOI] [PubMed] [Google Scholar]
- 31. Russell JA, Shave RM, Yoshioka H, Kruse DW, Koutedakis Y, Wyon MA. Magnetic resonance imaging of the ankle in female ballet dancers en pointe. Acta Radiol. 2010;51(6):655-661. [DOI] [PubMed] [Google Scholar]
- 32. Schweitzer ME, van Leersum M, Ehrlich SS, Wapner K. Fluid in normal and abnormal ankle joints: amount and distribution as seen on MR images. AJR Am J Roentgenol. 1994;162(1):111-114. [DOI] [PubMed] [Google Scholar]
- 33. Schweitzer ME, White LM. Does altered biomechanics cause marrow edema? Radiology. 1996;198(3):851-853. [DOI] [PubMed] [Google Scholar]
- 34. Smith PJ, Gerrie BJ, Varner KE, McCulloch PC, Lintner DM, Harris JD. Incidence and prevalence of musculoskeletal injury in ballet: a systematic review. Orthop J Sports Med. 2015;3(7):2325967115592621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Soder RB, Mizerkowski MD, Petkowicz R, Baldisserotto M. MRI of the knee in asymptomatic adolescent swimmers: a controlled study. Br J Sports Med. 2012;46(4):268-272. [DOI] [PubMed] [Google Scholar]
- 36. Vande Berg BE, Malghem JJ, Labaisse MA, Noel HM, Maldague BE. MR imaging of avascular necrosis and transient marrow edema of the femoral head. Radiographics. 1993;13(3):501-520. [DOI] [PubMed] [Google Scholar]
- 37. Yao W, Zhang Y, Zhang L, et al. MRI features of and factors related to ankle injuries in asymptomatic amateur marathon runners. Skeletal Radiol. 2021;50(1):87-95. [DOI] [PMC free article] [PubMed] [Google Scholar]