Abstract
Background
Rett syndrome (RTT) is a severe X-linked neurodevelopmental disorder associated with multiple neurologic impairments. Previous studies have shown challenges to the quality of life of individuals with RTT and their caregivers. However, instruments applied to quantify disease burden have not adequately captured the impact of these impairments on affected individuals and their families. Consequently, an international collaboration of stakeholders aimed at evaluating Burden of Illness (BOI) in RTT was organized.
Methods
Based on literature reviews and qualitative interviews with parents of children and adults with RTT, a caregiver questionnaire was constructed to evaluate 22 problems (inclusive of core characteristics, functional impairments, and comorbidities) often experienced with RTT, rated mainly with a 5-level Likert scale. The questionnaire was administered anonymously online to an international sample of 756 caregivers (predominantly parents) of girls and women with RTT. Descriptive statistics were used to identify problems of high frequency and impact on affected individuals and caregivers. Chi-square tests characterized the relationship between problem severity and impact responses, while nonparametric ANOVAs of raw and z-score adjusted scores identified agreement between severity and impact on individual and caregiver. Secondary inferential tests were used to determine the roles of age, clinical type, and country of residence on BOI in RTT.
Results
There was variability in reported frequency of problems, with the most prevalent, severe and impactful being those related to the core features of RTT (i.e., communication and fine and gross motor impairments). Chi-square analyses demonstrated interdependence between severity and impact responses, while ANOVAs showed that many problems had disproportionately greater impact than severity, either on affected individuals (e.g., hand stereotypies) or their caregivers (e.g., sleep difficulties, seizures, pain, and behavioral abnormalities). With certain exceptions (e.g., breath-holding, seizures), age, clinical type, or country of residence did not influence these BOI profiles.
Conclusions
Our data demonstrate that core features and related impairments are particularly impactful in RTT. However, problems with mild severity can also have disproportionate impact on affected individuals and, particularly, on their caregivers. Future analyses will examine the role of factors such as treatment outcomes, healthcare services, and healthcare provider’s perspectives, in these BOI profiles.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13023-024-03313-8.
Keywords: Rett syndrome, Quality of life, Intellectual disability, Caregiver, Parent-proxy report
Background
Rett Syndrome (RTT; OMIM 312750) is a rare X-linked neurodevelopmental disorder that occurs predominantly in girls and women with an incidence of approximately 1 in 10,000 female births worldwide [1, 2]. Most individuals with RTT (> 96%) carry a pathogenic variant in the methyl-CpG-binding protein 2 (MECP2) gene, which encodes the transcriptional regulator MeCP2 [3, 4]. The disorder is characterized by progression of neurologic impairment throughout development into adulthood [5, 6]. Most individuals with RTT appear to develop normally until around 6–18 months of age, after which they experience a period of regression characterized by loss of spoken language and fine motor skills. This regression, in conjunction with impairment in ambulation and development of hand stereotypic movements, constitute the core diagnostic features of the disorder [5]. Recovery of language and fine motor skills is limited as is the further development of gross motor skills [5, 6]. In addition to these impairments, other neurologic and systemic manifestations frequently develop [7]; these include seizures [8], sleep problems [9], breathing abnormalities [10], aberrant behaviors [11], musculoskeletal abnormalities (e.g., scoliosis) [12, 13], and gastrointestinal dysfunction [14]. Although the clinical manifestations of RTT reach relative stability after childhood, further decline in multiple functions may become evident at older ages. Adulthood is a period characterized by limited motor (e.g., emergence of Parkinsonian features) and communication abilities, as well as for the development of internalizing behavioral abnormalities (e.g., depression-like symptoms) [11, 15–17].
Thanks to advances in medical and allied health care, including better recognition of factors affecting morbidity and mortality, many individuals with RTT survive into their 50 s [18–20]. However, ongoing functional deficits and comorbidities experienced may pose significant physical, psychological, social and financial burden on affected individuals and their caregivers. Several studies examining the impact of RTT identified challenges to quality of life of affected individuals [21–23], their siblings [24, 25], and their caregivers [25–31]. These investigations have identified multiple factors affecting outcomes and quality of life in RTT. For affected individuals, these include ability to communicate and ambulate, feeding skills, age of onset of hand stereotypies, severity of seizures, sleep problems and behavioral abnormalities [21–23, 32–36]. The impact on the caregiver’s physical and mental well-being is dependent on, among others, the severity of the child’s physical and behavioral impairments, in particular feeding difficulties; caregiver age and demands; financial challenges; and challenges to family functioning [25–28, 31]. Findings on maternal mental health suggest an increased risk of anxiety but they are not conclusive about depression [25–27]. Of interest is the observation that caregiver mental health is more affected than physical quality of life, and that this profile does not change over a 5-year period [28]. A small study on siblings of girls and women with RTT showed relatively good psychological adjustment, in comparison with population norms [24], while another larger investigation, contrasting the impact with that on siblings of children with Down syndrome, found both benefits and disadvantages for the RTT group [24, 25].
Despite this increasing literature, many questions remain about the burden of RTT on affected individuals and their families. Previous studies have applied standardized instruments (e.g., Child Health Questionnaire 50) which are not validated for evaluating a population like RTT, with severe communication, motor impairments and other unique clinical features (e.g., “Rett episodes”). Moreover, many surveys have been implemented with relatively small caregiver samples that may not have captured the population-level variability of the disorder and familial experience. Recently, domains of quality of life important for children [37] and adults with RTT have been explored [38]. Accordingly, new instruments and analytical strategies are being developed to investigate the impact of RTT on individuals [37, 39] and their caregivers [40].
One of these initiatives, reported in the present study, was to implement a comprehensive, large-scale, international study to investigate RTT specific issues. To accomplish these goals, RTT stakeholders representing affected families, clinicians, researchers, and drug developers, in the USA, Europe, and Australia, joined efforts in a “Burden of Illness” project. Here, we report initial results from the caregiver survey on BOI in females with RTT to identify (1) problems (core features, functional impairments, comorbidities) of greater frequency and impact, (2) relationships between severity of a problem, as assessed by caregivers, and its impact on individuals and caregivers, (3) agreement between impact on affected individual and impact on caregiver, and (4) roles of age, clinical type, and country of residence on BOI in RTT.
Methods
Data sources
Caregivers of female and male individuals with RTT, both children and adults, from the USA, United Kingdom, Italy, Germany, and Australia were invited to participate by their countries’ advocacy groups. In Australia, most participants were recruited from the Australian Rett Syndrome Database [41]. For this study, caregivers were defined as those who reported being 18 years or older and spending at least 10 h per week caring for an individual with RTT. No clinical type (diagnosis of classic or atypical RTT) was required for participation. Because of their different prevalence and clinical features, here we report only on girls and women with caregiver-reported RTT. A separate analysis will investigate the survey data of caregivers of male individuals. As shown in Table 1 most caregivers (96%) were parents of affected individuals. A small proportion (4%) of surveys were completed by grandparents, siblings, and paid caregivers. A total of 756 caregivers provided verified surveys of female individuals with RTT. Survey verification was performed by reviewing responses and open text entries to validate that the data provided was complete and legitimate. Surveys that were identified as being completed in an erroneous manner (i.e., user acceptance testing responses, duplicate entries, nonsensical open text fields with clearly invalid responses) were removed from the analyses (N = 326). Profiles of affected individuals and their caregivers participating in the present study are shown in Table 1.
Table 1.
Demographic and clinical features of affected individuals and caregivers
| Age (years) | Diagnosis age (years) | Full dataset | Diagnosis | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Classic Rett syndrome | Atypical Rett syndrome | Don’t know | ||||||||||
| Mean | (SD) | Mean | (SD) | N | (%) | N | (%) | N | (%) | N | (%) | |
| Total | 16.72 | 10.67 | 4.30 | 4.65 | 756 | 100 | 519 | 69 | 143 | 19 | 94 | 12 |
| Age | Mean | (SD) | Mean | (SD) | N | (%) | N | (%)** | N | (%)** | N | (%)** |
| Child (< 12 years) | 6.82 | 2.87 | 2.75 | 1.36 | 303 | 40.1 | 214 | 70.6 | 48 | 15.8 | 41 | 13.5 |
| Adolescent (12–18 years) | 15.10 | 1.72 | 3.53 | 2.77 | 152 | 20.1 | 104 | 68.4 | 33 | 21.7 | 15 | 9.9 |
| Adult (> 19 years) | 27.50 | 7.71 | 6.24 | 6.50 | 301 | 39.8 | 201 | 66.8 | 62 | 20.6 | 38 | 12.6 |
| Mutation | ||||||||||||
| MECP2 Mutation | 15.83 | 10.34 | 4.11 | 4.53 | 673 | 89.0 | 486 | 72.2 | 113 | 16.8 | 74 | 11.0 |
| No MECP2 Mutation Identified | 23.62 | 10.01 | 6.03 | 5.01 | 31 | 4.1 | 6 | 19.4 | 21 | 67.7 | 4 | 12.9 |
| Don’t know | 24.10 | 11.03 | 5.75 | 5.59 | 52 | 6.9 | 27 | 51.9 | 9 | 17.3 | 16 | 30.8 |
| Region | ||||||||||||
| United States | 16.70 | 11.13 | 4.01 | 4.14 | 415 | 54.9 | 282 | 68.0 | 86 | 20.7 | 47 | 11.3 |
| Europe* | 16.24 | 10.51 | 4.58 | 5.25 | 259 | 34.3 | 193 | 74.5 | 42 | 16.2 | 24 | 9.3 |
| Australia | 18.36 | 8.49 | 4.86 | 5.07 | 82 | 10.8 | 44 | 53.7 | 15 | 18.3 | 23 | 28.0 |
| Caregiver | ||||||||||||
| Parent | 16.75 | 10.57 | 4.31 | 4.57 | 728 | 96.3 | 502 | 69.0 | 140 | 19.2 | 86 | 11.8 |
| Grandparent | 9.81 | 9.93 | 2.32 | 0.98 | 14 | 1.9 | 7 | 50.0 | 3 | 21.4 | 4 | 28.6 |
| Sibling | 36.08 | 15.27 | 15.72 | 16.60 | 3 | 0.4 | 1 | 33.3 | 0 | 0.0 | 2 | 66.7 |
| Paid caregiver | 17.95 | 10.59 | 3.24 | 3.85 | 11 | 1.5 | 9 | 81.8 | 0 | 0.0 | 2 | 18.2 |
*Europe includes United Kingdom (N = 103), Germany (N = 100), and Italy (N = 56)
**Percent of respective analysis group when caregiver selected the diagnosis of “Classic”, “Atypical”, or “Don’t know”
Approval to conduct the study was obtained from ethics committees in each country and either written or electronic informed consent was obtained for all participants. Surveys were completed anonymously, no identifying information was collected, and data were maintained confidential in accordance with the ethics protocol.
Procedure
The caregiver BOI survey was developed following literature review, input from an advisory board of experts (both clinicians and caregivers), and concept elicitation (qualitative) interviews with 15 parents of children and adults with RTT. Survey development included caregiver cognitive debriefing for evaluating the relevance and comprehension of the sections and questions. The questionnaire included 138 questions covering 22 characteristic problems (core clinical features, functional impairments, comorbidities), spanning 15 domains (Table 2). Additional sections on quality of life, healthcare resource utilization, and general impact on caregivers (health and relationships, work productivity, financial impact), comprising an additional 38 questions were not analyzed in the present study because of its focus on the impact of specific problems in RTT. Responses to these questions will be included in subsequent analyses and published in a separate paper. Ratings of problem severity were based on caregivers’ experiences during the previous 4 weeks. Problem impact was assessed by the caregiver; including both impact on the affected individual’s ability to participate in daily activities (Impact on individual) and impact on the caregiver (e.g., physical or emotional well-being). Example sections of the caregiver survey are presented in Supplementary Material.
Table 2.
Profile of responses to severity, impact on individual, and impact on caregiver questions
| Domain | Problem (order of survey presentation) | % Reporting the problem | Question | % of Responses at 2 highest levels in those reporting problem | Raw scores | Z-scores | ||
|---|---|---|---|---|---|---|---|---|
| Median | Mean (SD) | Median | Mean (SD) | |||||
| Breathing | Breath-Holding | 56.6 | Severity | 28.7 | 3 | 2.74 (1.2) | − 0.36 | − 0.51 (0.69) |
| Impact-individual | 18.0 | 2 | 2.34 (1.21) | − 1.15 | − 0.9 (0.92) | |||
| Impact-caregiver | 27.3 | 3 | 2.67 (1.22) | − 0.39 | − 0.64 (0.93) | |||
| Hyperventilatione | 35.4 | Severity | 26.5 | 3 | 2.76 (1.08) | − 0.36 | − 0.5 (0.62) | |
| Impact-individual | 23.9 | 2 | 2.54 (1.18) | − 1.15 | − 0.74 (0.9) | |||
| Impact-caregiver | 27.2 | 3 | 2.71 (1.15) | − 0.39 | − 0.61 (0.87) | |||
| Air swallowing | 41.5 | Severity | 34.1 | 3 | 2.99 (1.17) | − 0.36 | − 0.36 (0.67) | |
| Impact-individual | 20.7 | 2 | 2.52 (1.19) | − 1.15 | − 0.76 (0.9) | |||
| Impact-caregiver | 28.7 | 3 | 2.71 (1.27) | − 0.39 | − 0.61 (0.96) | |||
| Hand use | Functional hand usec, f | 95.9 | Severity | 76.0 | 5 | 5.1 (0.92) | 0.79 | 0.84 (0.53) |
| Impact-individual | 90.1 | 5 | 4.59 (0.78) | 1.13 | 0.82 (0.59) | |||
| Impact-caregiver | 72.7 | 4 | 4.03 (1.12) | 0.37 | 0.39 (0.85) | |||
| Involuntary movements | Hand stereotypies | 97.8 | Severity | 69.7 | 4 | 3.84 (1.1) | 0.21 | 0.12 (0.63) |
| Impact-individual | 74.3 | 5 | 4.11 (1.12) | 1.13 | 0.45 (0.85) | |||
| Impact-caregiver | 57.4 | 4 | 3.62 (1.26) | 0.37 | 0.08 (0.96) | |||
| Gastrointestinal | Constipationd | 79.0 | Severity | 41.0 | 3 | 3.26 (1.08) | − 0.36 | − 0.21 (0.62) |
| Impact-individual | 26.8 | 3 | 2.79 (1.21) | − 0.39 | − 0.55 (0.92) | |||
| Impact-caregiver | 44.6 | 3 | 3.29 (1.23) | − 0.39 | − 0.17 (0.94) | |||
| Gastroesophageal reflux | 37.6 | Severity | 27.1 | 3 | 2.84 (1.08) | − 0.36 | − 0.45 (0.62) | |
| Impact-individual | 23.6 | 2 | 2.67 (1.16) | − 1.15 | − 0.65 (0.88) | |||
| Impact-caregiver | 34.2 | 3 | 2.99 (1.22) | − 0.39 | − 0.4 (0.93) | |||
| Feeding | Oral feedingf | 68.4 | Severity | 29.6 | 4 | 4.14 (1.01) | 0.21 | 0.29 (0.58) |
| Impact-individual | 35.6 | 3 | 2.92 (1.25) | − 0.39 | − 0.45 (0.95) | |||
| Impact-caregiver | 54.4 | 4 | 3.51 (1.23) | 0.37 | 0 (0.94) | |||
| Scoliosis | Scoliosisd | 59.3 | Severity | 24.6 | 3 | 2.67 (1.22) | − 0.36 | − 0.55 (0.7) |
| Impact-individual | 27.9 | 3 | 2.67 (1.32) | − 0.39 | − 0.64 (1) | |||
| Impact-caregiver | 37.5 | 3 | 2.96 (1.33) | − 0.39 | − 0.42 (1.02) | |||
| Communication | Understandinga, e, f | 48.8 | Severity | 48.5 | 4 | 4.14 (0.99) | 0.21 | 0.29 (0.56) |
| Impact-individual | 79.1 | 5 | 4.22 (0.97) | 1.13 | 0.53 (0.74) | |||
| Impact-caregiver | 74.8 | 4 | 4.12 (1.08) | 0.37 | 0.46 (0.82) | |||
| Nonverbal self-expressione, f | 62.8 | Severity | 25.7 | 4 | 3.97 (0.85) | 0.21 | 0.2 (0.49) | |
| Impact-individual | 81.7 | 5 | 4.32 (0.93) | 1.13 | 0.61 (0.71) | |||
| Impact-caregiver | 76.4 | 5 | 4.18 (1.09) | 1.13 | 0.5 (0.83) | |||
| Verbal self-expressionf | 92.7 | Severity | 80.7 | 6 | 5.28 (0.9) | 1.36 | 0.95 (0.51) | |
| Impact-individual | 88.2 | 5 | 4.5 (0.88) | 1.13 | 0.75 (0.67) | |||
| Impact-caregiver | 80.9 | 5 | 4.32 (1.05) | 1.13 | 0.61 (0.8) | |||
| Mobility | Standing unsupportede, f | 75.7 | Severity | 77.6 | 6 | 5.34 (1.04) | 1.36 | 0.98 (0.59) |
| Impact-individual | 90.0 | 5 | 4.59 (0.77) | 1.13 | 0.82 (0.59) | |||
| Impact-caregiver | 87.1 | 5 | 4.49 (0.91) | 1.13 | 0.74 (0.69) | |||
| Walking with assistanceb, f | 69.7 | Severity | 60.2 | 5 | 4.86 (1.15) | 0.79 | 0.71 (0.66) | |
| Impact-individual | 91.8 | 5 | 4.64 (0.73) | 1.13 | 0.86 (0.55) | |||
| Impact-caregiver | 88.2 | 5 | 4.54 (0.86) | 1.13 | 0.78 (0.65) | |||
| Walking independentlye, f | 82.4 | Severity | 78.0 | 6 | 5.37 (1.01) | 1.36 | 1 (0.58) | |
| Impact-individual | 88.3 | 5 | 4.53 (0.82) | 1.13 | 0.77 (0.62) | |||
| Impact-caregiver | 86.0 | 5 | 4.46 (0.93) | 1.13 | 0.72 (0.71) | |||
| Sleep | Sleep difficultiesc | 71.8 | Severity | 37.6 | 3 | 3.13 (1.03) | − 0.36 | − 0.28 (0.59) |
| Impact-individual | 37.0 | 3 | 3.18 (1.12) | − 0.39 | − 0.25 (0.85) | |||
| Impact-caregiver | 63.0 | 4 | 3.85 (1.12) | 0.37 | 0.25 (0.85) | |||
| Epilepsy | Seizures | 36.8 | Severity | 30.2 | 2 | 2.67 (1.44) | − 0.93 | − 0.55 (0.82) |
| Impact-individual | 49.3 | 3 | 3.45 (1.27) | − 0.39 | − 0.05 (0.96) | |||
| Impact-caregiver | 65.1 | 4 | 3.85 (1.16) | 0.37 | 0.26 (0.89) | |||
| Rett episodes | Rett episodes | 79.2 | Severity | 25.2 | 3 | 2.68 (1.14) | − 0.36 | − 0.54 (0.65) |
| Impact-individual | 29.0 | 3 | 2.81 (1.22) | − 0.39 | − 0.54 (0.93) | |||
| Impact-caregiver | 37.6 | 3 | 3.08 (1.26) | − 0.39 | − 0.33 (0.96) | |||
| Dystonia | Dystoniac, d | 53.0 | Severity | 22.2 | 3 | 2.79 (1.07) | − 0.36 | − 0.48 (0.61) |
| Impact-individual | 32.9 | 3 | 3.02 (1.15) | − 0.39 | − 0.38 (0.88) | |||
| Impact-caregiver | 39.4 | 3 | 3.20 (1.2) | − 0.39 | − 0.24 (0.91) | |||
| Pain | Painc | 73.0 | Severity | 20.1 | 2.5 | 2.57 (1.1) | − 0.65 | − 0.61 (0.63) |
| Impact-individual | 31.3 | 3 | 2.93 (1.2) | − 0.39 | − 0.45 (0.92) | |||
| Impact-caregiver | 57.6 | 4 | 3.62 (1.22) | 0.37 | 0.08 (0.93) | |||
| Behaviors | Behavioral abnormalitiesc | 79.9 | Severity | 34.3 | 3 | 3.06 (1.07) | − 0.36 | − 0.33 (0.61) |
| Impact-individual | 39.9 | 3 | 3.23 (1.1) | − 0.39 | − 0.22 (0.84) | |||
| Impact-caregiver | 63.9 | 4 | 3.86 (1.12) | 0.37 | 0.26 (0.85) | |||
| Self-care | Self-caree, f | 98.5 | Severity | 98.0 | 6 | 5.91 (0.38) | 1.36 | 1.31 (0.22) |
| Impact-individual | 80.7 | 5 | 4.3 (1.17) | 1.13 | 0.6 (0.89) | |||
| Impact-caregiver | 87.1 | 5 | 4.5 (0.97) | 1.13 | 0.74 (0.74) | |||
Core features and related impairments in bold
aChi-square severity versus impact individual and severity versus impact caregiver not significant
bFriedman’s ANOVA not significant
cDunn Bonferroni’s post hoc severity versus impact-individual not significant
dDunn Bonferroni’s post hoc severity versus impact-caregiver not significant
eDunn Bonferroni’s post hoc impact-individual versus impact-caregiver not significant
Surveys were completed via web interface. Analyses were performed on surveys from caregivers with a valid and unique entry (IP address), who met the definition of caregiver, and reported that the affected individual was female. If there were duplicate entries for a single caregiver, the most complete surveys were included and the least complete were discarded. For the present study, we excluded a few surveys (n = 14) from caregivers who reported that the affected individual had either a FOXG1 or a CDKL5 variant, since pathogenic variants of these genes are now considered distinctive disorders [42, 43].
Questions on impact on individual, impact on caregiver and half of those assessing severity, were scored using a 5-level Likert scale, ranging from very mild/low to very severe/high. For severity items evaluating episodic manifestations (i.e., pain, seizures, “Rett episodes”) a ‘None in the past 4 weeks’ option was added below the very mild/low option. Severity items evaluating functional impairments were scored using 6 levels, ranging from excellent to unable. The survey was translated from English into German, Italian, and Spanish following the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) task force guidance and were administered online.
Data analysis
The primary analyses included data on demographics and sample characteristics and the questions on severity, impact on individual, or impact on caregiver for the entire sample. The full dataset of 756 surveys was divided into groups for secondary analyses based on age, clinical type, and country or region of residence: children (individuals younger than 12 years), adolescents (individuals between 12 and 18 years), and adults (individuals older than 18 years); clinical type (diagnosis of classic or atypical RTT); residential country/region: Australia, Europe (European countries were grouped), and the United States. Because most caregivers reported a “known” MECP2 pathogenic variant (~ 89%), this parameter was not included in the analyses.
We calculated raw scores from the caregivers’ categorical responses to all questions, assigning 0 to “none”, 1 through 5 to “very mild/low” through “very severe/high”, and 6 to “unable”. To control for heterogeneity between questions with 5 or more severity levels, we standardized responses across the entire set of 22 problems by calculating z-scores. As the analyses required a comparison of severity and impact on the individual and caregiver, for each problem we only analyzed surveys where the caregiver confirmed that the individual was affected by the problem and responded to the severity, impact on individual, and impact on caregiver questions. We excluded surveys where the caregiver confirmed that the individual was affected by the problem but one or more of these questions were not responded to (n = 0–11, depending on the problem).
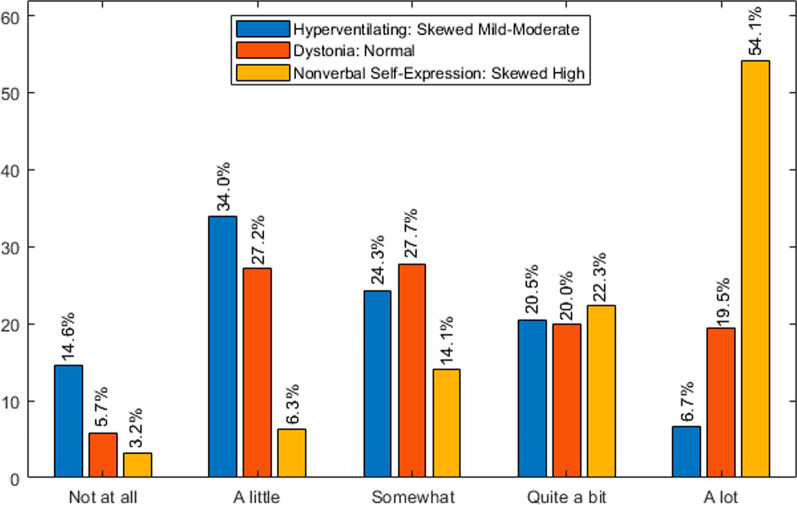
Descriptive analyses depicted in Table 2 include overall frequency of problems (percentage of caregivers reporting the problem), distribution of categorical responses (i.e., percentage of two highest-level responses in those reporting the problem), and median, mean, and standard deviation of raw scores and z-scores for each severity and impact question. In addition, we profiled descriptive data as frequency histograms (Fig. 1). Since severity and impact questions for each of the 22 problems were answered by the same caregiver, we examined interdependence of responses by the chi-square test. Considering that most of chi-square tests were significant, indicating that most responses for a given problem were statistically dependent on each other, we further investigated the nature of their relationship by comparing z-scores on severity, impact on individual, and impact on caregiver for each problem. Given the lack of normal distribution and the relatedness of scores, we conducted ANOVAs using the nonparametric Friedman’s test. This was followed by Dunn-Bonferroni post hoc tests correcting for within-problem multiple comparisons. Since each problem was deemed to be an independent subject of investigation, no multiple comparison corrections across the dataset (i.e., between problems) were conducted. ANOVAs were performed on the full dataset (primary analyses) and on the groups mentioned above (secondary analyses) and illustrated in Tables 2 and 3 for the entire cohort and Tables 4 and 5 for the group analyses. ANOVA summary tables (Tables 3, 4, 5) depict significant mean differences between severity and/or impact scores for each problem. For these summaries, non-significant post hoc differences were considered as approximately equal means. Analyses and histograms were performed using Matlab 9.7.0 (R2019b; The Mathworks Inc., Natick, Massachusetts) and the IBM SPSS Statistics version 29.0.1.0 (171) software (https://www.ibm.com/products/spss-statistics).
Fig. 1.
Patterns of distribution of responses in caregiver survey: three examples of impact caregiver frequency histograms
Table 3.
Primary analyses full dataset: relationships between severity, impact on individual, and impact on caregiver
| Severity > impact | Severity = impact | Impact > severity | Total | |
|---|---|---|---|---|
| Impact individual > impact caregiver | Verbal self-expression^ | Functional hand use^ | Hand stereotypies | 3 |
| 1 | 1 | 1 | ||
| Impact individual = impact caregiver | Hyperventilation | 6 | ||
| Standing unsupported^ | ||||
| Walking independently^ | Walking with assistance^ | Nonverbal self-expression^ | ||
| Self-care^ | ||||
| 4 | 1 | 1 | ||
| Impact caregiver > impact individual | Gastroesophageal reflux | 12 | ||
| Sleep difficulties | ||||
| Breath-holding | Constipation | Seizures | ||
| air swallowing | Scoliosis | Rett episodes | ||
| oral feeding^ | Dystonia | |||
| Pain | ||||
| Behavioral abnormalities | ||||
| 3 | 2 | 7 | ||
| Total | 8 | 4 | 9 | 21 |
Core features and related impairments in bold
Relationship between the severity and impact could not be determined for “Understanding”
^Impairment in function
Table 4.
Secondary analyses age: relationships between severity, impact on individual and impact on caregiver
| Severity > impact | Severity = impact | Impact > severity | Total | |
|---|---|---|---|---|
| A. Child (< 12 years) | ||||
| Impact individual > impact caregiver | Functional hand use^ | Hand stereotypies | 2 | |
| 0 | 1 | 1 | ||
| Impact individual = impact caregiver | Hyperventilation | 9 | ||
| Air swallowing | ||||
| Verbal self-expression^ | Understanding^ | |||
| Standing unsupported^ | Walking with assistance^ | Nonverbal self-expression^ | ||
| Walking independently^ | ||||
| Self-care^ | ||||
| 6 | 1 | 2 | ||
| Impact caregiver > impact individual | Scoliosis | 11 | ||
| Breath-holding | Sleep difficulties | |||
| Constipation | Seizures | |||
| Gastroesophageal reflux | Rett episodes | |||
| Oral feeding^ | Dystonia | |||
| Pain | ||||
| Behavioral abnormalities | ||||
| 0 | 4 | 7 | ||
| Total | 6 | 6 | 10 | 22 |
| B. Adolescent (12–18 years) | ||||
| Impact individual > impact caregiver | Functional hand use^ | Hand stereotypies | 2 | |
| 0 | 1 | 1 | ||
| Impact individual = impact caregiver | Breath-holding | 14 | ||
| Hyperventilation | Gastroesophageal reflux | |||
| Air swallowing | Understanding^ | Nonverbal self-expression^ | ||
| Verbal self-expression^ | Walking with assistance^ | Seizures | ||
| Standing unsupported^ | Rett episodes | |||
| Walking independently^ | Dystonia | |||
| Self-care^ | ||||
| 7 | 5 | 2 | ||
| Impact caregiver > impact individual | Scoliosis | 6 | ||
| Constipation | Sleep difficulties | |||
| Oral feeding^ | Pain | |||
| Behavioral abnormalities | ||||
| 0 | 2 | 4 | ||
| Total | 7 | 8 | 7 | 22 |
| C. Adult (> 18 years) | ||||
| Impact individual > impact caregiver | Functional hand use^ | Hand stereotypies | 4 | |
| Verbal self-expression^ | Nonverbal self-expression^ | |||
| 2 | 0 | 2 | ||
| Impact individual = impact caregiver | Hyperventilation | 8 | ||
| Air swallowing | ||||
| Scoliosis | ||||
| Standing unsupported^ | Dystonia | Seizures | ||
| Walking independently^ | ||||
| Self-care^ | ||||
| 6 | 1 | 1 | ||
| Impact caregiver > impact individual | Breath-holding | Constipation | Sleep difficulties | 8 |
| Oral feeding^ | Gastroesophageal reflux | Pain | ||
| Rett episodes | Behavioral abnormalities | |||
| 2 | 3 | 3 | ||
| Total | 10 | 4 | 6 | 20 |
Core features and related impairments in bold
Relationship between severity and impact could not be determined for “Understanding” and “Walking with Assistance”
^Impairment in function
Table 5.
Secondary analyses residential region: relationships between severity, impact on individual, and impact on caregiver
| Severity > impact | Severity = impact | Impact > severity | Total | |
|---|---|---|---|---|
| A. United States of America | ||||
| Impact individual > impact caregiver | Functional hand use^ | 1 | ||
| 0 | 1 | 0 | ||
| Impact individual = impact caregiver | Hyperventilation | 8 | ||
| Verbal self-expression^ | Walking with assistance^ | |||
| Standing unsupported^ | Dystonia | Nonverbal self-expression^ | ||
| Walking independently^ | ||||
| Self-care^ | ||||
| 5 | 2 | 1 | ||
| Impact caregiver > impact individual | Hand stereotypies | Sleep difficulties | 12 | |
| Breath-holding | Constipation | Seizures | ||
| Air swallowing | Gastroesophageal reflux | Rett episodes | ||
| Oral feeding^ | Pain | |||
| Scoliosis | Behavioral abnormalities | |||
| 2 | 5 | 5 | ||
| Total | 7 | 8 | 6 | 21 |
| B. Europe | ||||
| Impact individual > impact caregiver | Functional hand use^ | Hand stereotypies | 2 | |
| 0 | 1 | 1 | ||
| Impact individual = impact caregiver | Air swallowing | 10 | ||
| Gastroesophageal reflux | ||||
| Verbal self-expression^ | Hyperventilation | |||
| Standing unsupported^ | Walking with assistance^ | Nonverbal self-expression^ | ||
| Walking independently^ | Dystonia | |||
| Self-care^ | ||||
| 6 | 3 | 1 | ||
| Impact caregiver > impact individual | Breath-holding | Sleep difficulties | 8 | |
| Constipation | Rett episodes | |||
| Oral feeding^ | Pain | |||
| Scoliosis | Behavioral abnormalities | |||
| 0 | 4 | 4 | ||
| Total | 6 | 8 | 6 | 20 |
| C. Australia | ||||
| Impact individual > impact caregiver | Functional hand use^ | Hand stereotypies | 2 | |
| 0 | 1 | 1 | ||
| Impact individual = impact caregiver | Hyperventilation | 8 | ||
| Breath-holding | Scoliosis | |||
| Air swallowing | Nonverbal self-expression^ | |||
| Self-care^ | Rett episodes | |||
| Dystonia | ||||
| 3 | 5 | 0 | ||
| Impact caregiver > impact individual | Sleep difficulties | 4 | ||
| Constipation | Pain | |||
| Behavioral abnormalities | ||||
| 0 | 1 | 3 | ||
| Total | 3 | 7 | 4 | 14 |
(A) Relationship between the severity and impact could not be determined for “Understanding”. (B) Relationship between the severity and impact could not be determined for “Understanding” and “Seizures”. (C) Relationship between the severity and impact could not be determined for “ Gastroesophageal Reflux”, “Oral Feeding”, “Understanding”, “Verbal Self-Expression”, “Standing Unsupported”, “Walking with Assistance”, “Walking Independently”, and “Seizures”
Core features and impairments in bold
^Impairment in function
Results
Characteristics of the RTT subject sample
The majority of caregivers reported on individuals with classic RTT (~ 69%) with a MECP2 variant (89%). The age range of affected individuals was wide (1.0–61.0 years), with mean and median values of 16.7 and 15.3 years, respectively. Approximately, 40% were children, 20% were adolescents, and 40% were adults. The mean and median age of diagnosis were 4.3. and 2.8 years, respectively (classic RTT mean 3.8 years, median 2.5 years; atypical RTT mean 5.7 years, median 3.9 years), in line with published reports [44, 45]. Approximately 69% of caregivers reported a clinical presentation of classic RTT, ~ 19% reported atypical RTT, and ~ 12% reported ‘don’t know’. Caregiver responses indicated that ~ 55% resided in the U.S.A., ~ 34% in Europe, and ~ 11% in Australia. The country groups only differed in frequency of classic RTT presentation, which was lower for caregivers residing in Australia (~ 54%) as compared to those residing in Europe (75%) or the U.S.A. (68%). For details, see Table 1.
Frequency of problems
Table 2 depicts the frequency of problems (percentage of caregivers reporting the problem), distribution of categorical responses (i.e., percentage of two highest-level responses in those reporting the problem), and raw and z-score means, medians and SDs for the full dataset. There was a wide range of frequency of problems, from ~ 35% for hyperventilation to 99% for impairments in self-care activities of daily living. Core features or impairments were present in 70–98% of affected individuals, while other problems were more variable. For instance, seizures were reported by 37% of caregivers, dystonia by 53%, and constipation by 79%. Rett episodes (i.e., non-epileptic vacant spells/absences and dystonic crises/episodes) and behavioral abnormalities, which are not included in many surveys of the disorder, were also frequent, both approximately 79%.
Magnitude of clinical severity and impact
As shown in Table 2 for the primary analyses, frequency and scores on severity and impact were greater for problems representing core features of the disorder and related impairments. Specifically, mean severity and impact z-scores were positive for functional hand use, hand stereotypies, verbal self-expression, standing unsupported, walking with assistance, walking independently, and self-care. Additionally, severity of oral feeding had a positive mean z-score but the corresponding impact scores did not. Of these problems, severity was greater than impact for verbal self-expression, standing unsupported, walking independently, oral feeding, and self-care. For the remaining problems with positive mean severity and impact z-scores, impact on individual was greatest. Positive mean z-scores were also found in impact on caregiver for sleep difficulties, seizures, pain, and behavioral abnormalities.
Discrepancy between severity and impact
Chi-square analyses demonstrated that, with the exception of understanding, severity and impact responses were statistically inter-dependent (Table 2). Subsequently, Friedman’s ANOVAs showed significant differences between severity and impact scores for all problems but walking with assistance (Table 2). ANOVA post hoc tests showed that there were nine problems that had a significant and disproportionally higher impact than severity while severity and impact scores were comparable for four problems and severity was greater than impact for eight (Table 3). Seven out of nine problems with greater impact than severity affected more caregivers than individuals with RTT; most of them are typically manifested with variable frequency over time. These “episodic” problems include sleep difficulties, seizures, Rett episodes, pain, and behavioral abnormalities. Among particularly impactful problems, only hand stereotypies affected individuals with RTT more than caregivers (Table 3). Figure 1 illustrates different patterns of impact on caregiver.
Effect of age, clinical type, and country of residence
Secondary analyses showed that score profiles and relationships between severity and impact identified for the entire sample were in general replicated in the age, clinical type, and region group analyses (Tables 4, 5). This was particularly true for problems with greater impact than severity. However, there were exceptions, mainly influenced by subject’s age. Breath-holding, oral feeding, and scoliosis were relatively more impactful than severe in younger individuals, while gastroesophageal reflux, dystonia, and Rett episodes that were less impactful than severe in older individuals. Interestingly, seizures were less impactful for caregivers of adolescents and adults and nonverbal self-expression was more impactful on individuals than caregivers in adults (versus similar impact in children and adolescents) (Table 4). While seizures were particularly impactful in the USA group, their level of impact could not be determined in the European and Australian groups (Table 5). Other significant severity-impact differences were not replicated for some variables in adolescents, individuals with atypical RTT, or in the Australian group, most likely because of the smaller size of these groups.
Discussion
Rett syndrome (RTT) is a severe neurodevelopmental disorder characterized by a wide and variable range of neurologic impairments and comorbidities, the severity of which can accumulate over time. This study presents an initial overview of BOI in girls and women with RTT. Through an international collaboration of multiple stakeholders, which developed and implemented a caregiver survey targeting 22 RTT-characteristic problems across a large international sample, we were able to identify the most impactful problems, their differential effect on affected individuals and caregivers, and their relationship with clinical severity as estimated by caregivers. We found that among the most frequent, severe and impactful problems were those related to the core features of RTT and related impairments, namely hand function, hand stereotypies, communication and motor impairments, and self-care. We also demonstrated that many problems, particularly those that are episodic in nature (e.g., sleep difficulties, seizures, pain, and behavioral abnormalities), have disproportionately greater impact than severity, affecting caregivers more than individuals with RTT. In the main, these profiles of BOI were not influenced by the affected individuals’ age, clinical type, or country of residence.
Previous studies on quality of life of individuals with RTT and their caregivers have identified multiple factors affecting outcomes. Ability to ambulate, feeding skills, severity of seizures, sleep problems and behavioral abnormalities have impact on quality of life of individuals with RTT [21–23]. Greater severity of child’s impairments, caregiver age and demands, and family function and financial challenges also play a role in caregivers’ physical and mental well-being [25–29, 31]. While these data are extremely valuable, to our knowledge, no study has examined the differential impacts of features characteristic to RTT on affected individuals and their caregivers or the relationship between problem severity and quality of life. Furthermore, the considerable phenotypical variability of RTT [5, 46, 47] makes analysis of large subject samples, as the one employed in this study, imperative in order to obtain representative and reproducible findings.
Problems related to the core diagnostic features of RTT [5], involving communication, fine motor, and gross motor function, as well as self-care, were among the most frequent, severe and impactful manifestations. Our analyses demonstrated an expected interdependence between severity and impact scores, due to the fact that all scoring was conducted by caregivers who were assessing the affected children and themselves. Nonetheless, there was significantly greater impact than severity on both core features (i.e., hand stereotypies, nonverbal self-expression) and common symptoms of mild to moderate severity (e.g., gastroesophageal reflux, sleep difficulties, behavioral abnormalities). This was a novel finding that emphasizes that clinical severity, as estimated by caregivers, may underestimate BOI. Verbal self-expression and self-care seemed to be less impactful than severe, although their overall level of impact and severity were high. Other distinctive RTT manifestations that were particularly impactful on caregivers included seizures, Rett episodes, and pain. As with sleep difficulties and behavioral abnormalities, they were characterized by relatively lower frequency or severity than other problems but also by an episodic nature. Despite this, in evaluations covering only the previous month, caregivers reported they were markedly affected by the occurrence of these problems. Whether their unpredictability contributes to their marked impact is unknown; however, these results agree with informal clinic observations. Our findings also highlight the importance of relatively recently investigated problems in RTT, such as sleep and non-autistic behavioral difficulties [9, 11, 48–51]. They are also in line with studies of individuals with other neurodevelopmental disorders which show that sleep difficulties in children can exacerbate parents’ existing strain and fatigue, adversely affecting their mental health and parenting [30, 52, 53]. The BOI profiles reported here are also in agreement with a recent investigation on top caregiver concerns in RTT, which reported communication, seizures, walking/balance issues, lack of hand use, and constipation as top concerns for caregivers of individuals with classic RTT [54].
Comparisons of impact on individuals and caregivers demonstrated that the latter appear to be more affected by many of the RTT-characteristic problems evaluated in this project. Caregiver’s role in providing daily care, sometimes representing all essential needs of daily living, can be affected by seemingly milder impairments that add emotional, and physical burden and limit time availability for other activities [21, 30, 40]. Our findings are in correspondence to previous studies on morbidity and mortality [19, 20] and quality of life of affected individuals and caregivers [21–23, 25–28, 31, 40] but insights into the wide range of problems and the relative independence of impact from clinical severity for some problems is novel. Indeed, even RTT-characteristic problems that are mild in severity can place a disproportionate burden on affected individuals and, particularly, on their caregivers. Interestingly, the profiles of severity and impact reported for the total subject sample were to large extent replicated in analyses of age, clinical type, and country of residence groups. For instance, the greater impact of seizures on caregivers of younger than older individuals and those residing in the USA may reflect different levels of tolerance for this unpredictable type of symptom.
Despite the large subject sample and multiple countries of origin, our data had limitations. Approximately one third of the submitted entries were determined to be invalid at the initial data quality control phase. This problem is inherent to conducting anonymous online surveys. Among them, assessment of problem severity by caregivers did not follow specific guidelines, there was limited verification of caregivers’ understanding of the survey or of the accuracy of responses about clinical type or genetic variants, and there were structural inconsistencies in the survey (e.g., item severity assessed through 5–7 options). Although analyses included age, clinical type, and country of residence groups, some subgroups were relatively small in size (i.e., adolescents, individuals with atypical RTT, Australian sample), which could prevent the replication of some findings. We acknowledge that we did not have data on specific MECP2 pathogenic variants, which are known to influence clinical severity but whose effects on impact are not yet known. Additionally, this international survey included caregivers from a range of communities with disparate degrees of exposure to families with children impacted by other serious disorders. Thus, their perception of severity will undoubtably be relative to their specific experience. Therefore, the present report should be considered as an initial overview analysis of BOI in RTT. We expect that follow-up studies will address some of the abovementioned issues by expanding the current analyses. For instance, investigating the role of treatments and their outcomes, healthcare resource utilization, and other factors on RTT burden. Additional collected data on impact on caregiver (health, relationships, financial impact) would further delineate groups particularly impacted by the clinical manifestations of RTT.
Conclusions
This large-scale study of BOI in RTT demonstrated that the most impactful problems were those related to the core features of the disorder and that even mildly severe clinical manifestations can disproportionately impact affected individuals and their caregivers. Future analyses should explore the influence of other factors such as clinical evolution, treatment outcomes, and access to healthcare services. Similar analyses from the healthcare provider perspective should also expand our understanding of BOI in RTT.
Supplementary Information
Acknowledgements
We thank the families and clinicians who participated in this project. This project would have not been possible without the efforts from Rett syndrome advocacy groups in the USA, UK, Italy, Germany, and Australia. We are grateful to Steve Kaminsky (International Rett Syndrome Foundation), who was instrumental in the development of the study; the initial sponsor, Newron Pharmaceuticals; and to the Parexel team, who assisted with the implementation of the surveys.
Abbreviations
- RTT
Rett syndrome
- MECP2
Methyl-CpG-binding protein 2
- BOI
Burden of illness
Author contributions
WEK, AKP, JLN, PN, GDS, TEB, GST, LMGC, OM: design or conceptualization of study. JD, HL, CB, CUM: data collection. WEK, AKP, JLN, JD, HL, GDS, LMGC, LMO, KVB: drafting or revising manuscript for intellectual content, analysis, or interpretation. All authors: drafting or revising manuscript for intellectual content. Statistical analyses were conducted by WEK, HMO, LMO, and VV-F. All authors read and approved the final manuscript.
Funding
Support for data collection was provided by Newron Pharmaceuticals and for data management and analysis by Anavex Life Sciences Corp. JD is supported by a Fellowship from the Stan Perron Charitable Foundation. MO is supported by the NIMH Intramural Research Program (ZIAMH002955). The views expressed in this article do not necessarily represent the views of the National Institutes of Health, the Department of Health and Human Services, or the United States Government.
Availability of data and materials
Data are available through Anavex Life Sciences Corp. and the International Rett Syndrome Foundation.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the ISPOR Code of Ethics 2017, Good Epidemiology Practices and with the ethical principles laid down in the Declaration of Helsinki. Compliance with these regulatory standards and guidance provided assurance that the rights, safety and wellbeing of subjects participating in this study are protected. Approval to conduct the study was obtained from ethics committees to comply with local laws and regulations in the United States, Europe and Australia; written or electronic informed consent was obtained for all participants.
Consent for publication
Not applicable.
Competing interests
WEK is currently the Chief Scientific Officer of Anavex Life Sciences Corp. He received funding from the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC), and he has been a consultant for Anavex, AveXis, Acadia, EryDel, Neuren Pharmaceuticals, Newron, GW Pharmaceuticals, Marinus, Biohaven, Zynerba, Ovid Therapeutics, and Stalicla. He has done clinical trials with Neuren. AKP received funding from the NIH and is a consultant for Anavex, Taysha Gene Therapies, Neurogene, and Acadia. He is a member of the DSMB for Taysha Gene Therapies and has done clinical trials with Anavex, Acadia, GW Pharmaceuticals, and the Rett Syndrome Research Trust (RSRT). JLN received funding from the NIH, International Rett Syndrome Foundation (IRSF) and RSRT. He is a consultant for Acadia, Analysis Group, AveXis, GW Pharmaceuticals, Hoffmann-La Roche, Myrtelle, Neurogene, Newron, Signant Health, Taysha Gene Therapies, and for the preparation of CME activities for PeerView Institute MedEdicus and Medscape; he serves on the scientific advisory board of Alcyone Lifesciences and is a scientific cofounder of LizarBio Therapeutics; and he was also a member of a data safety monitoring board for clinical trials conducted by Ovid Therapeutics. He has done clinical trials with Acadia and Newron. JD has consulted for Marinus, Newron, Orion, Taysha, Neurogene, Acadia and AveXis. She has done clinical trials with Newron and Anavex. HL has consulted for Acadia, Avexis, Anavex, GW Pharmaceuticals, Newron, Neurogene, Marinus, and Ovid Therapeutics. She has received funding from the NIH, International Foundation for CDKL5 Research and the Loulou Foundation. HMO, KVB, ERH, and CUM are Anavex employees. VV-F is a consultant for Anavex. The rest of the authors, PN, GDS, TEB, GST, LMGC, OM, and CB, declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Laurvick CL, de Klerk N, Bower C, Christodoulou J, Ravine D, Ellaway C, et al. Rett syndrome in Australia: a review of the epidemiology. J Pediatr. 2006;148(3):347–52. 10.1016/j.jpeds.2005.10.037 [DOI] [PubMed] [Google Scholar]
- 2.Fehr S, Bebbington A, Nassar N, Downs J, Ronen GM, Klerk DE, N, et al. Trends in the diagnosis of Rett syndrome in Australia. Pediatr Res. 2011;70(3):313–9. 10.1203/PDR.0b013e3182242461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nat Genet. 1999;23(2):185–8. 10.1038/13810 [DOI] [PubMed] [Google Scholar]
- 4.Gold WA, Krishnarajy R, Ellaway C, Christodoulou J. Rett syndrome: a genetic update and clinical review focusing on comorbidities. ACS Chem Neurosci. 2018;9(2):167–76. 10.1021/acschemneuro.7b00346 [DOI] [PubMed] [Google Scholar]
- 5.Neul JL, Kaufmann WE, Glaze DG, Christodoulou J, Clarke AJ, Bahi-Buisson N, et al. Rett syndrome: revised diagnostic criteria and nomenclature. Ann Neurol. 2010;68(6):944–50. 10.1002/ana.22124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fu C, Armstrong D, Marsh E, Lieberman D, Motil K, Witt R, et al. Multisystem comorbidities in classic Rett syndrome: a scoping review. BMJ Paediatr Open. 2020;4(1):e000731. 10.1136/bmjpo-2020-000731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu C, Armstrong D, Marsh E, Lieberman D, Motil K, Witt R, et al. Consensus guidelines on managing Rett syndrome across the lifespan. BMJ Paediatr Open. 2020;4(1):e000717. 10.1136/bmjpo-2020-000717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tarquinio DC, Hou W, Berg A, Kaufmann WE, Lane JB, Skinner SA, et al. Longitudinal course of epilepsy in Rett syndrome and related disorders. Brain. 2017;140(2):306–18. 10.1093/brain/aww302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Veatch OJ, Malow BA, Lee HS, Knight A, Barrish JO, Neul JL, et al. Evaluating sleep disturbances in children with rare genetic neurodevelopmental syndromes. Pediatr Neurol. 2021;123:30–7. 10.1016/j.pediatrneurol.2021.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tarquinio DC, Hou W, Neul JL, Berkmen GK, Drummond J, Aronoff E, et al. The course of awake breathing disturbances across the lifespan in Rett syndrome. Brain Dev. 2018;40(7):515–29. 10.1016/j.braindev.2018.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buchanan CB, Stallworth JL, Scott AE, Glaze DG, Lane JB, Skinner SA, et al. Behavioral profiles in Rett syndrome: data from the natural history study. Brain Dev. 2019;41(2):123–34. 10.1016/j.braindev.2018.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Percy AK, Lee HS, Neul JL, Lane JB, Skinner SA, Geerts SP, et al. Profiling scoliosis in Rett syndrome. Pediatr Res. 2010;67(4):435–9. 10.1203/PDR.0b013e3181d0187f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Killian JT, Lane JB, Lee HS, Skinner SA, Kaufmann WE, Glaze DG, et al. Scoliosis in Rett syndrome: progression, comorbidities, and predictors. Pediatr Neurol. 2017;70:20–5. 10.1016/j.pediatrneurol.2017.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Motil KJ, Caeg E, Barrish JO, Geerts S, Lane JB, Percy AK, et al. Gastrointestinal and nutritional problems occur frequently throughout life in girls and women with Rett syndrome. J Pediatr Gastroenterol Nutr. 2012;55(3):292–8. 10.1097/MPG.0b013e31824b6159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schönewolf-Greulich B, Stahlhut M, Larsen JL, Syhler B, Bisgaard AM. Functional abilities in aging women with Rett syndrome—the Danish cohort. Disabil Rehabil. 2017;39(9):911–8. 10.3109/09638288.2016.1170896 [DOI] [PubMed] [Google Scholar]
- 16.Peron A, Canevini MP, Ghelma F, Arancio R, Savini MN, Vignoli A. Phenotypes in adult patients with Rett syndrome: results of a 13-year experience and insights into healthcare transition. J Med Genet. 2022;59(1):39–45. 10.1136/jmedgenet-2020-107333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bisgaard AM, Wong K, Hojfeldt AK, Larsen JL, Schonewolf-Greulich B, Ronde G, et al. Decline in gross motor skills in adult Rett syndrome; results from a Danish longitudinal study. Am J Med Genet A. 2021;185(12):3683–93. 10.1002/ajmg.a.62429 [DOI] [PubMed] [Google Scholar]
- 18.Kirby RS, Lane JB, Childers J, Skinner SA, Annese F, Barrish JO, et al. Longevity in Rett syndrome: analysis of the North American Database. J Pediatr. 2010;156(1):135-8.e1. 10.1016/j.jpeds.2009.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson A, Wong K, Jacoby P, Downs J, Leonard H. Twenty years of surveillance in Rett syndrome: What does this tell us? Orphanet J Rare Dis. 2014;9:87. 10.1186/1750-1172-9-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tarquinio DC, Hou W, Neul JL, Kaufmann WE, Glaze DG, Motil KJ, et al. The changing face of survival in Rett syndrome and MECP2-related disorders. Pediatr Neurol. 2015;53(5):402–11. 10.1016/j.pediatrneurol.2015.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lane JB, Lee HS, Smith LW, Cheng P, Percy AK, Glaze DG, et al. Clinical severity and quality of life in children and adolescents with Rett syndrome. Neurology. 2011;77(20):1812–8. 10.1212/WNL.0b013e3182377dd2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parisi L, Di Filippo T, Roccella M. The Quality of Life in Girls with Rett Syndrome. Ment Illn. 2016;8(1):6302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mendoza J, Downs J, Wong K, Leonard H. Determinants of quality of life in Rett syndrome: new findings on associations with genotype. J Med Genet. 2021;58(9):637–44. 10.1136/jmedgenet-2020-107120 [DOI] [PubMed] [Google Scholar]
- 24.Mulroy S, Robertson L, Aiberti K, Leonard H, Bower C. The impact of having a sibling with an intellectual disability: parental perspectives in two disorders. J Intellect Disabil Res. 2008;52(Pt 3):216–29. 10.1111/j.1365-2788.2007.01005.x [DOI] [PubMed] [Google Scholar]
- 25.Cianfaglione R, Hastings RP, Felce D, Clarke A, Kerr MP. Psychological well-being of mothers and siblings in families of girls and women with Rett syndrome. J Autism Dev Disord. 2015;45(9):2939–46. 10.1007/s10803-015-2457-y [DOI] [PubMed] [Google Scholar]
- 26.Laurvick CL, Msall ME, Silburn S, Bower C, de Klerk N, Leonard H. Physical and mental health of mothers caring for a child with Rett syndrome. Pediatrics. 2006;118(4):e1152–64. 10.1542/peds.2006-0439 [DOI] [PubMed] [Google Scholar]
- 27.Sarajlija A, Djurić M, Tepavcević DK. Health-related quality of life and depression in Rett syndrome caregivers. Vojnosanit Pregl. 2013;70(9):842–7. 10.2298/VSP1309842S [DOI] [PubMed] [Google Scholar]
- 28.Killian JT, Lane JB, Lee HS, Pelham JH, Skinner SA, Kaufmann WE, et al. Caretaker quality of life in Rett syndrome: disorder features and psychological predictors. Pediatr Neurol. 2016;58:67–74. 10.1016/j.pediatrneurol.2015.12.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mori Y, Downs J, Wong K, Heyworth J, Leonard H. Comparing parental well-being and its determinants across three different genetic disorders causing intellectual disability. J Autism Dev Disord. 2018;48(5):1651–65. 10.1007/s10803-017-3420-x [DOI] [PubMed] [Google Scholar]
- 30.Mori Y, Downs J, Wong K, Leonard H. Longitudinal effects of caregiving on parental well-being: the example of Rett syndrome, a severe neurological disorder. Eur Child Adolesc Psychiatry. 2019;28(4):505–20. 10.1007/s00787-018-1214-0 [DOI] [PubMed] [Google Scholar]
- 31.Palacios-Ceña D, Famoso-Pérez P, Salom-Moreno J, Carrasco-Garrido P, Pérez-Corrales J, Paras-Bravo P, et al. “Living an obstacle course”: a qualitative study examining the experiences of caregivers of children with Rett syndrome. Int J Environ Res Public Health. 2018;16(1):41. 10.3390/ijerph16010041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mackay J, Downs J, Wong K, Heyworth J, Epstein A, Leonard H. Autonomic breathing abnormalities in Rett syndrome: caregiver perspectives in an international database study. J Neurodev Disord. 2017;9:15. 10.1186/s11689-017-9196-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boban S, Leonard H, Wong K, Wilson A, Downs J. Sleep disturbances in Rett syndrome: Impact and management including use of sleep hygiene practices. Am J Med Genet A. 2018;176(7):1569–77. 10.1002/ajmg.a.38829 [DOI] [PubMed] [Google Scholar]
- 34.Reddihough D, Leonard H, Jacoby P, Kim R, Epstein A, Murphy N, et al. Comorbidities and quality of life in children with intellectual disability. Child Care Health Dev. 2021;47(5):654–66. 10.1111/cch.12873 [DOI] [PubMed] [Google Scholar]
- 35.Williams K, Jacoby P, Whitehouse A, Kim R, Epstein A, Murphy N, et al. Functioning, participation, and quality of life in children with intellectual disability: an observational study. Dev Med Child Neurol. 2021;63(1):89–96. 10.1111/dmcn.14657 [DOI] [PubMed] [Google Scholar]
- 36.Leonard H, Whitehouse A, Jacoby P, Benke T, Demarest S, Saldaris J, et al. Quality of life beyond diagnosis in intellectual disability—latent profiling. Res Dev Disabil. 2022;129:104322. 10.1016/j.ridd.2022.104322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Epstein A, Leonard H, Davis E, Williams K, Reddihough D, Murphy N, et al. Conceptualizing a quality of life framework for girls with Rett syndrome using qualitative methods. Am J Med Genet A. 2016;170(3):645–53. 10.1002/ajmg.a.37500 [DOI] [PubMed] [Google Scholar]
- 38.Strugnell A, Leonard H, Epstein A, Downs J. Using directed-content analysis to identify a framework for understanding quality of life in adults with Rett syndrome. Disabil Rehabil. 2020;42(26):3800–7. 10.1080/09638288.2019.1610801 [DOI] [PubMed] [Google Scholar]
- 39.Downs J, Jacoby P, Leonard H, Epstein A, Murphy N, Davis E, et al. Psychometric properties of the Quality of Life Inventory-Disability (QI-Disability) measure. Qual Life Res. 2019;28(3):783–94. 10.1007/s11136-018-2057-3 [DOI] [PubMed] [Google Scholar]
- 40.Lane JB, Salter AR, Jones NE, Cutter G, Horrigan J, Skinner SA, et al. Assessment of caregiver inventory for Rett syndrome. J Autism Dev Disord. 2017;47(4):1102–12. 10.1007/s10803-017-3034-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wong K, Downs J, Ellaway C, Baikie G, Ravikumara M, Jacoby P, et al. Impact of gastrostomy placement on nutritional status, physical health, and parental well-being of females with Rett syndrome: a longitudinal study of an Australian population. J Pediatr. 2018;200:188–95. 10.1016/j.jpeds.2018.04.050 [DOI] [PubMed] [Google Scholar]
- 42.Ma M, Adams HR, Seltzer LE, Dobyns WB, Paciorkowski AR. Phenotype differentiation of FOXG1 and MECP2 disorders: a new method for characterization of developmental encephalopathies. J Pediatr. 2016;178:233-40.e10. 10.1016/j.jpeds.2016.08.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fehr S, Wilson M, Downs J, Williams S, Murgia A, Sartori S, et al. The CDKL5 disorder is an independent clinical entity associated with early-onset encephalopathy. Eur J Hum Genet. 2013;21(3):266–73. 10.1038/ejhg.2012.156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fehr S, Downs J, Bebbington A, Leonard H. Atypical presentations and specific genotypes are associated with a delay in diagnosis in females with Rett syndrome. Am J Med Genet A. 2010;152A(10):2535–42. 10.1002/ajmg.a.33640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tarquinio DC, Hou W, Neul JL, Lane JB, Barnes KV, O’Leary HM, et al. Age of diagnosis in Rett syndrome: patterns of recognition among diagnosticians and risk factors for late diagnosis. Pediatr Neurol. 2015;52(6):585–91. 10.1016/j.pediatrneurol.2015.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bebbington A, Anderson A, Ravine D, Fyfe S, Pineda M, de Klerk N, et al. Investigating genotype-phenotype relationships in Rett syndrome using an international data set. Neurology. 2008;70(11):868–75. 10.1212/01.wnl.0000304752.50773.ec [DOI] [PubMed] [Google Scholar]
- 47.Cuddapah VA, Pillai RB, Shekar KV, Lane JB, Motil KJ, Skinner SA, et al. Methyl-CpG-binding protein 2 (MECP2) mutation type is associated with disease severity in Rett syndrome. J Med Genet. 2014;51(3):152–8. 10.1136/jmedgenet-2013-102113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boban S, Wong K, Epstein A, Anderson B, Murphy N, Downs J, et al. Determinants of sleep disturbances in Rett syndrome: novel findings in relation to genotype. Am J Med Genet A. 2016;170(9):2292–300. 10.1002/ajmg.a.37784 [DOI] [PubMed] [Google Scholar]
- 49.Gilbertson M, Richardson C, Eastwood P, Wilson A, Jacoby P, Leonard H, et al. Determinants of sleep problems in children with intellectual disability. J Sleep Res. 2021;30(5):e13361. 10.1111/jsr.13361 [DOI] [PubMed] [Google Scholar]
- 50.Buchanan CB, Stallworth JL, Joy AE, Dixon RE, Scott AE, Beisang AA, et al. Anxiety-like behavior and anxiolytic treatment in the Rett syndrome natural history study. J Neurodev Disord. 2022;14(1):31. 10.1186/s11689-022-09432-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kay C, Leonard H, Smith J, Wong K, Downs J. Genotype and sleep independently predict mental health in Rett syndrome: an observational study. J Med Genet. 2023;60(10):951–9. 10.1136/jmg-2022-108905 [DOI] [PubMed] [Google Scholar]
- 52.Gallop K, Lloyd AJ, Olt J, Marshall J. Impact of developmental and epileptic encephalopathies on caregivers: a literature review. Epilepsy Behav. 2021;124:108324. 10.1016/j.yebeh.2021.108324 [DOI] [PubMed] [Google Scholar]
- 53.Budimirovic DB, Protic DD, Delahunty CM, Andrews HF, Choo TH, Xu Q, et al. Sleep problems in fragile X syndrome: cross-sectional analysis of a large clinic-based cohort. Am J Med Genet A. 2022;188(4):1029–39. 10.1002/ajmg.a.62601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Neul JL, Benke TA, Marsh ED, Suter B, Silveira L, Fu C, et al. Top caregiver concerns in Rett syndrome and related disorders: data from the US natural history study. J Neurodev Disord. 2023;15(1):33. 10.1186/s11689-023-09502-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available through Anavex Life Sciences Corp. and the International Rett Syndrome Foundation.