Abstract
Background
Tandem spinal stenosis (TSS) is a condition characterized by the narrowing of the spinal canal in multiple segments of the spine. Predominantly observed in the cervical and lumbar regions, TSS also manifests in the conjunction of the cervical and thoracic spine. The simultaneous occurrence of cervical and thoracic spinal stenosis engenders intricate symptoms, potentially leading to missed and delayed diagnosis. Furthermore, the presence of tandem cervical and thoracic stenosis (TCTS) introduces a notable impact on the decision-making calculus of surgeons when contemplating either one-staged or two-staged surgery. Currently, there is no agreed-upon strategy for surgical intervention of TCTS in the literature.
Methods
Medical databases in English (Pubmed, Web of Science, Embase, the Cochrane Database of Systematic Reviews) and Chinese (CNKI, Wanfang Data, VIP CMJD) were searched using Medical Subject Heading queries for the terms “tandem cervical and thoracic stenosis”, “cervical stenosis AND thoracic stenosis”, “tandem spinal stenosis” and “concomitant spinal stenosis” from January 1980 to March 2023. We included studies involving adult individuals with TCTS. Articles exclusively focused on disorders within a single spine region or devoid of any mention of spinal disorders were excluded.
Results
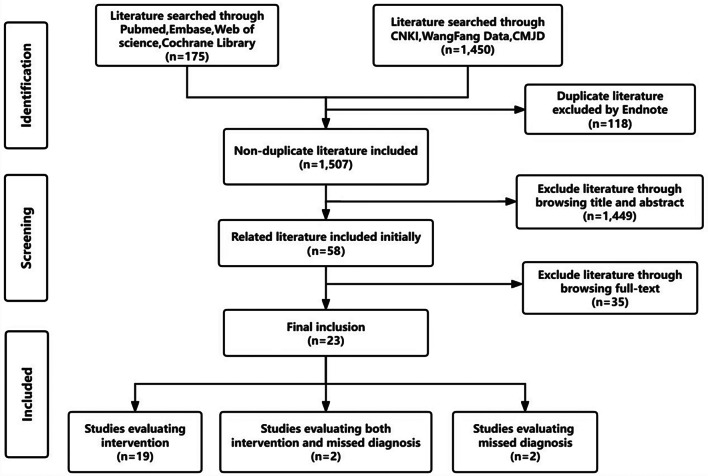
Initially, a total of 1625 literatures underwent consideration for inclusion in the study. Following the elimination of the duplicates through the utilization of EndNote, and a meticulous screening process involving scrutiny of abstracts and full-texts, 23 clinical studies met the predefined inclusion criteria. Of these, 2 studies solely focused on missed diagnosis, 19 studies exclusively discussed surgical strategy for TCTS, and 2 articles evaluated both surgical strategy and missed diagnosis.
Conclusion
Our study revealed a missed diagnosis rate of 7.2% in TCTS, with the thoracic stenosis emerging as the predominant area susceptible to oversight. Therefore, the meticulous identification of TCTS assumes paramount significance as the inaugural step in its effective management. While both one-staged and two-staged surgeries have exhibited efficacy in addressing TCTS, the selection of the optimal surgical plan should be contingent upon the individualized circumstances of the patients.
Keywords: Tandem cervical and thoracic stenosis, Tandem spinal stenosis, Missed diagnosis, Surgical strategy
Introduction
Tandem spinal stenosis (TSS) represents a pathological condition characterized by the synchronous narrowing of both the cervical and lumbar spines. Originally delineated by Teng and Papatheodorou [1] and subsequently defined by Dagi, it manifests as a clinical triad marked by intermittent lower limb claudication, gait disorders, and both lower and upper motor neuron signs [2]. Tandem cervical and thoracic stenosis (TCTS) is another important type of TSS, which refers to the stenosis of cervical and thoracic spine. The incidence of TCTS ranges from 2.9 to 44.4%, lower than the overall incidence of TSS [3]. Although the etiology of TCTS remains unclear, current studies posit that it may be associated with heterotopic ossification and ligament expansion triggered by degenerative spinal disease.
The missed diagnosis of TCTS may result in an extended preoperative duration and an unfavorable prognosis, given the inverse correlation between the underlying course and the prognosis of TCTS [4]. However, diagnosing TCTS poses a considerable challenge for clinicians, as the symptoms do not simply represent a symptomatic combination of cervical and thoracic stenosis. Determining whether the symptoms in the lower extremities stem from a cervical or thoracic lesion becomes a complex task, compounded by the fact that cervical spinal stenosis can partially mask the symptoms of thoracic spinal stenosis [5]. Furthermore, conventional imaging examinations such as magnetic resonance imaging (MRI) may not encompass the entire spine, potentially contributing to the missed identification of TCTS.
When deciding on surgical intervention for TCTS, surgeons encounter the dilemma of determining whether to prioritize the cervical or thoracic spine during the operative procedure. Historically, addressing cervical stenosis first was a prevalent approach among researchers. However, contemporary perspectives from numerous experienced authors present a spectrum of viewpoints, including single-region decompression, staged decompression, or simultaneous decompression. Despite the wealth of research, a conspicuous absence of consensus persists in the existing literature regarding the optimal surgical intervention for TCTS.
The principal objectives of this systematic review encompass the critical evaluation of surgical intervention strategies for TCTS and the exploration of methodologies aimed at averting missed diagnoses.
Materials and methods
Study selection
This systematic review adhered to the recommended guidelines and protocols established by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. A comprehensive search of English medical databases (Pubmed, Web of science, Embase, the Cochrane Database of Systematic Reviews) and Chinese medical databases [China National Knowledge Infrastructure(CNKI), Wanfang Data, VIP Chinese Medical Journal Database(CMJD)] were conducted from January 1980 to March 2023 using Medical Subject Heading queries for the terms “tandem cervical and thoracic stenosis”, “cervical stenosis AND thoracic stenosis”, “tandem spinal stenosis”, and “concomitant spinal stenosis”.
CNKI, a comprehensive Chinese digital library, encompasses an extensive array of academic resources across diverse medical disciplines, providing access to research articles, conference proceedings, and theses. Wanfang Data, a prominent Chinese information service provider, offers databases in various fields, including medicine and healthcare, featuring academic journals, conference proceedings, dissertations, and research projects.Additionally, the VIP CMJD, part of the VIP Information system, spans multiple disciplines, incorporating medical journals, conference papers, and clinical guidelines.These Chinese medical databases enable users to access pertinent medical literature through these platforms, utilizing Chinese keywords and advanced search options.Therefore, concerning the search methodology for Chinese medical databases, we will begin by translating English keywords into Chinese, followed by executing queries within the databases.
The inclusion criteria involved adult patients and clinical investigations focusing on TCTS. Exclusions were made for articles addressing diseases or those that only concerned a single spinal region. Abstracts, conference reports, review papers and case reports were intentionally omitted. To refine the selection of articles, two independent authors scrutinized all findings based on titles and abstracts. In recognition of the potential for inadvertent omissions, a comprehensive examination of the references in each included study was conducted. The scientific integrity of each included study underwent assessment through the utilization of the Grading of Recommendations Assessment, Development, and Evaluation(GRADE) system [6].
Data collection and analysis
Data extraction from relevant studies focused on two key categories: those investigating the missed diagnosis of TCTS and those evaluating surgical intervention in patients with TCTS. The data collected from these studies encompassed various aspects, including study design, study period, study population, sample size, order of intervention, and outcome measures. Quantitative descriptive statistics were applied to patients from all included studies whenever practical.
Results
PRISMA search results
This systematic review commenced with an initial pool of 1625 pieces of literature. Through the utilization of EndNote, duplicate entries were meticulously eliminated. Subsequently, two reviewers engaged in a comprehensive review process involving the scrutiny of titles, abstracts, and full texts, resulting in the identification of 23 studies that met the predetermined inclusion requirements. Among these clinical studies, a distribution emerged: 2 studies were exclusively dedicated to the exploration of missed diagnoses, 19 studies delved into surgical strategies for TCTS, and 2 articles undertook a dual evaluation, concurrently addressing both surgical strategy and missed diagnosis (Fig. 1).
Fig. 1.
Literature search flow chart. CNKI, China National Knowledge Infrastructure; CMJD, Chinese Medical Journal Database
Surgical intervention in TCTS
The encompassing evaluation of surgical interventions for patients with TCTS involved twenty-one studies, as outlined in Table 1 [4, 7–26]. Among the 681 patients included in this study, 392(57.5%) presented with TCTS. One-staged surgical procedures were implemented on 246 patients with TCTS, with 50 patients undergoing cervical decompression(CD), 37 receiving thoracic decompression(TD) in the first stage, and 159 experiencing one-staged combined decompression. Staged surgery was performed in 85 patients, with 44 receiving CD as the initial procedure, 7 receiving TD as the first step, and 34 cases where the specific surgical plan was not explicitly detailed. The studies frequently employed prognostic methods such as the Japanese Orthopedic Association (JOA) score, Nuirick score, Hirabayashi’s system score and patient satisfaction score. Postoperative complications were notably documented, with dural tear, cerebrospinal fluid leakage, and neurological deterioration emerging as the most common complications following surgical interventions.
Table 1.
Characteristics of studies evaluating intervention in patients with tandem cervical and thoracic stenosis
| Study period | Study | Design | Level of evidence | Included population | Total study (N) |
C + T stenosis (N) |
Main pattern of spinal stenosis | Order of intervention (N) |
Main complication | Outcome measure |
|---|---|---|---|---|---|---|---|---|---|---|
|
Wang et al. |
2010–2018 |
Retrospective Cohort |
IV |
C + T Stenosis |
34 | 34 |
C: OPLL/CSM T:OLF/OPLL/disc-herniation/DISH |
CD only (8) TD only (15) CTD(one-stage or two-stage)(11) |
Dural tears/ Thoracic de-teriorating compression /Hypoalbuminemia/Ne-urological deterioration |
JOA/ Recovery grade/Op-erative time/Blood loss/ Hospital stay/Inpatient ex-penditure/Complications |
|
Hu et al. |
2005–2012 | Retrospective Case Series | IV |
C + T Stenosis |
16 | 16 |
C: OPLL T: OPLL |
One-stage CTD(16) |
Neurological deteriorat-ion/CSF leakage/New radiculopathy |
JOA / Hirabayashi’s system |
|
Hu et al. |
2005–2013 | Retrospective Case Series | IV |
C + T Stenosis |
30 | 30 |
C: OPLL T: OPLL |
One-stage CTD (17) CD→TD(13) |
Immediate neurologic deterioration/Dural tears /Urinary deterioration |
JOA |
|
Chen et al. |
2005–2008 | Retrospective Case Series | IV |
C + T tand- em ossific-ation |
15 | 15 |
C: OPLL T: OPLL/OLF |
One-stage CTD(15) |
CSF leakage/C5palsy/ Neurodeterioration/ Hematoma |
JOA/Nurick classification/ Patient satisfaction |
|
Zhao et al. |
2010–2015 | Retrospective cohort study | IV |
Multilevel C +Upper T stenosis |
22 | 22 | Not defined |
One-stage CTD(12) Two-stage(10) |
Not defined |
JOA/Improvement rate/ Ex-tent of neurological funct- ion/Cost of hospitalization/ |
| Park et al . | 2003–2008 | Retrospective Cohort | IV | C OPLL | 68 | 23 |
C: OPLL T: OLF/OPLL |
CD→TD(6) | Not defined | Thoracic myelopathy |
| Shiokawa et al. | 1988–1999 | Retrospective Case Series | IV | T OLF | 31 | 12 |
C:Disc-herniation /OPLL T: OLF |
TD only (8) TD→CD(2) TD→LD(2) |
Wound infection | Nurick grade |
| Nishiura et al. | 1981–1996 | Retrospective Case Series | IV | T OLF | 37 | 8 |
C: OPLL T: OLF |
CD→TD(8) | No found |
Neurologic status/ Complications |
|
Chang et al. |
1987–1997 | Retrospective Case Series | IV | T CSM | 28 | 3 |
C: OPLL T: OLF/OPLL/Facet hypertrophy |
One-stage(1) TD→CD(2) |
Quadriparesis |
Nurick grede/ Neurologic status |
|
Uehara et al. |
2000–2012 | Retrospective Case Series | IV |
Surgery for TM |
50 | 11 |
C:Compressive myelopathy T: OPLL/OYL/ disc-herniation |
One-stage CTD(11) |
Dural tear/ Transient paraplegia /Motor paralysis/ Wound infection |
JOA / Blood loss Surgical times/ Complications |
|
Jannelli et al. |
2015–2018 | Retrospective Case Series | IV | TSS | 8 | 2 | Not defined | CD→TD(2) | Not defined | JOA/ODI questionnaire |
| Bhandutia et al. | 2006–2016 | Retrospective Cohort | IV | TSS | 33 | 2 | Not defined | CD→TD(2) | Not defined | Neurologic status |
| Kawaguchi et al. | 1986–2003 | Retrospective Case Series | IV | Ossified LSS | 20 | 5 |
C: OPLL T: OPLL /OLF |
LD only(2) LD→TD(2) CD →TD(1) |
Dural tear |
JOA /complications/ Operative time/ Blood loss |
|
Liao et al . |
2005–2010 | Retrospective Case Series | IV | C + T Tandem Ossification | 14 | 14 |
C: OPLL T: OPLL /OLF |
One-stage CTD(14) |
Hematoma /C5palsy/ Neurologic deterioration |
JOA/Nurick system/ Satisfaction rating |
|
Sun et al. |
1991–2003 | Retrospective Case Series | IV | Surgery for T OLF and CSM | 40 | 40 |
C:OPLL/Degenera-tive SS T:OLF/OLF + OPLL/ Disc-herniation |
One-stage CTD (18) TD only(9) Two-stage (13) |
CSF leakage/ Complete paraplegia |
Epstein |
|
Chen et al. |
1980–1997 | Retrospective Case Series | IV | T OLF | 72 | 27 |
C: OPLL /CSM T: OLF/OPLL/Disc-herniation |
One-stage (17) CD →TD(10) |
Symptom worsen/ Dural tear |
Epstein |
|
Li et al . |
1991–2005 | Retrospective Case Series | IV | T OPLL | 55 | 23 |
C:Developmental stenosis/OPLL T: OPLL /OPLL |
One-stage CTD(13) |
Symptom worsen |
Cervical spondylosis spi- nal cord function |
|
Ma et al. |
2004–2008 | Retrospective Case Series | IV | Surgery for C + T + L degenerat-ive disease | 79 | 79 |
C: Disc-herniation/ /OPLL / OLF T: Disc-herniation /OLF |
CD only(41) TD only (5) one-stage CTD(9) Two-stage(3) |
Wound liquefaction/ Infection/Hematoma/Enteroplegia/Urinary retention、infection /CSF leakage |
JOA |
|
Sun et al. |
2009–2012 | Retrospective Case Series | IV | C + T + L SS | 7 | 4 | Not defined |
One stage CTD(4) |
Hypostatic pneumo- nia/CSF leakage |
JOA-C/JOA-B/ODI/Oper- ative time/Blood loss/Hos- pital stay/Complication/ Patient satisfication |
|
Chen et al. |
1994–2003 | Retrospective Case Series | IV |
CSM+ T SS |
4 | 4 |
C: Developmental stenosis/Disc-herniation T: OLF / Articular Hyperosteogeny |
LD only(2) LD→TD(2) CD →TD(1) |
Not defined | Neurologic status |
|
Yao et al. |
2010–2015 | Retrospective Cohort | IV | Multilevel C stenosis + upper T stenosis | 18 | 18 |
C: OPLL T: OLF/OPLL |
One-stage CTD(10) Two-stage(8) |
C5 palsy/Fat liquef- action/Postoperative symptoms not relieved or worsened |
JOA/Improve rate/ T Cobb/C ROM |
| Total | 681 | 392 |
C cervical, T thoracic, L lumbar, OPLL ossification of posterior longitudinal ligament, OLF ossification of ligamentum flavum, DISH diffuse idiopathic skeletal hyperostosis, JOA Japanese Orthopaedic Association, CD cervical decompression, TD thoracic decompression, CTD cervical and thoracic decompression, LD lumbar decompression, CSF cerebrospinal fluid, CSM cervical spondylotic myelopathy, TM thoracic myelopathy, SS spinal stenosis
Missed diagnosis for TCTS
Missed diagnosis of TCTS was assessed in four clinical studies (Table 2). In a case-control study [27]involving 35 patients with cervical spondylotic myelopathy(CSM) complicated by thoracic ossification of ligamentum flavum(OLF), 6 patients with thoracic OLF were initially missed diagnosed. Following cervical decompression, symptoms in the upper extremity significantly improved, while lower extremity problems persisted or worsened over time. Subsequent utilization of thoracic MRI confirmed the diagnosis of TCTS. The rate of missed diagnosis was 17.1%. In a retrospective study, 318 individuals with cervical ossification of posterior longitudinal ligament (OPLL)were included [28]. 14 patients with thoracic OLF were misdiagnosed as cervical OPLL on admission. Thoracic OLF was unintentionally discovered after further testing in 7 patients before the original operation, while 5 cases remained an incorrect diagnosis. Following cervical decompression, persistent upper motor nerve dysfunction in both lower extremities prompted the eventual detection of the thoracic OLF. In another 2 cases, thoracic OLF was not correctly identified before the subsequent surgery. The percentage of missed diagnosis was 4.4%. Sun et al. [19]. conducted a retrospective review of 40 patients underwent surgery for thoracic OLF coupled with CSM. The study found that thoracic OLF was initially overlooked in 7 patients who were initially diagnosed with CSM. The symptoms in the lower extremities did not improve and actually worsened after cervical decompression. Ultimately, thoracic OLF was identified after additional testing, resulting in a missed diagnosis rate of 17.5%. In the evaluation of 8 symptomatic TCTS patients, Jannelli overlooked 2 instances of thoracic myelopathy, with a missed diagnosis rate of 25% [11]. Combining the data from these four studies, the overall missed diagnosis rate for the 401 patients was 7.2%, ranging from 4.4 to 25%, with all missed segments occurring in the thoracic spine.
Table 2.
Characteristics of studies evaluating miss diagnosis of tandem cervical and thoracic stenosis
| Study | Study period | Study design |
Level of evidence | Study population |
Total study N | Miss diagnosis N | Stenosis pattern of miss diagnosis | Outcome of study |
|---|---|---|---|---|---|---|---|---|
|
Sun el at. |
1994-2001 | Case control | III | CSM+T OLF | 35 | 6 | T OLF | 75% of those who meet the upper limb function score composition ratio > 36% and bladder function score ≤ 2 points are thoracic OLF combined with CSM |
|
Zhou el at. |
1987-1993 | Retrospective Case Series | IV | C OPLL | 318 | 14a | T OLF | There is a high possibility of cervical OPLL combined with thoracic OLF when it shows continuous cervical OPLL, mixed cervical OPLL and DISH disease involving multiple segments. |
|
Sun el at. |
1991-2003 | Retrospective Case Series | IV | T OLF +CSM | 40 | 7 | T OLF | When cervical MRI finds OLF in the upper thoracic spine, MRI examination of the entire thoracic spine should be performed to determine whether OLF occurs in the thoracolumbar and middle and lower thoracic spine. |
| Jannelli el at. | 2015-2018 | Retrospective Case Series | IV | TSS | 8 | 2 | Dorsal myelopathy | Electrophysiological techniques can be considered an objective and cost-effective tool in the assessment of TSS and can improve surgical decision-making. |
| Total | 401 | 29 |
CSM cervical spondylotic myelopathy, OLF ossification of ligamentum flavum, OPLL ossification of posterior longitudinal ligament, DISH diffuse idiopathic skeletal hyperostosis TSS tandem spinal stenosis
Discussion
The etiology of TCTS remains unclear. According to our included researches, degenerative factors such as ligament ossification and disc herniation stand as the primary causes of TCTS, with OPLL being the most common cause of cervical spinal canal stenosis and OLF and OPLL being the most frequent causes of thoracic spinal stenosis. Furthermore, TCTS has been be associated with congenital tandem cervical and thoracic spinal canal stenosis [29, 30]. Clinical studies have indicated metabolic variables may potentially contribute to the development of spinal canal stenosis. Adolescents with mucopolysaccharide type IV and hypoparathyroidism syndrome have been reported to develop multi-segmental tandem stenosis, as demonstrated by Mut et al. [31]and Lindert et al. [32]. Therefore, it is imperative for clinicians to to exercise meticulous discernment and differentiate between various causes when diagnosing TCTS.
Missed diagnosis for TCTS
The overall incidence of missed diagnosis of TCTS was found to be 7.2%, with a range from 4.4 to 25%, based on the studies included in the analysis. Importantly, all missed segments were identified in the thoracic spine. Thoracic spinal stenosis is relatively uncommon due to its steadier biomechanical characteristics when compared to cervical or lumbar spine [33]. Patients with TCTS may experience successive or concurrent indications induced by cervical or thoracic spinal stenosis [34], leading to a complex interplay of symptoms and signs. Notably, cervical myelopathy and thoracic spinal cord compression share similarities in the presentation of symptoms primarily because both conditions involve upper motor neuron dysfunction [10, 19, 20, 22]. Consequently, cervical myelopathy can obscure the symptoms of thoracic spinal cord compression, rendering it challenging to diagnose without proper evaluation. In addition, multi-level involvement is the characteristic feature of thoracic OLF [23], with the lower thoracic spine and thoracolumbar joint serving as predisposing sites [35–37]. Neglecting the lesions in the middle and lower thoracic spine is a risk if only the cervical spine is evaluated. Furthermore, It’s worth noting that the preoperative duration of thoracic stenosis was identified as the primary factor affecting surgical effectiveness. If the diagnosis is overlooked, the prognosis for the surgery may suffer considerably.
The accurate diagnosis of TCTS necessitates a comprehensive approach encompassing a thorough medical history, physical examination and imaging evaluation. Several studies have proposed that specific imaging features of the cervical spine, combined with characteristic symptoms or signs, can be instrumental in preventing missed diagnoses of TCTS. For instance, Sun et al. [27]. conducted a clinical study in which they performed MRI examinations of the whole-thoracic spine in patients exhibiting more severe lower limb dysfunction than upper limb dysfunction, or those with relatively intact upper limb function but signs of upper motor neuron injury with attenuated deep reflexes in both lower limbs. This meticulous approach helped in avoiding missed diagnoses of TCTS. Furthermore, they observed that 75% of individuals meeting both the composition ratio of upper limb function score > 36% and scores of urocystic function ≤ 2 points were cases with TCTS. Among 35 patients included, 20 had cervical OPLL (15 with a continuous type) and 8 had diffuse idiopathic skeletal hyperostosis (DISH), emphasizing the importance of considering thoracic OLF in these cases. Another study by Zhou et al. [28] recommended patients with cervical OPLL and DISH undergo a thoracic examination to ensure that thoracic OLF was not neglected. Park et al. [38]. conducted a retrospective study and found C7-T1 anterior epidural stenosis at the disc level as a predictor of thoracic stenosis. In addition, it should be noted that lower extremity symptoms are frequently exacerbated after cervical decompression if TCTS is originally misdiagnosed, necessitating further examination of the thoracic spine to prevent a ecurrence of missed diagnosis [19].
Operative management for TCTS
Operative intervention has been demonstrated to be an effective treatment option for TCTS, with conservative therapy potentially prolonging the course and risking disease aggravation. Nevertheless, an ongoing controversy persists regarding the choice between one-staged combined operation and staged operation as potential surgical interventions for TCTS.
One-staged combined operation
The advantages of one-staged combined operation consist of single hospitalization and anesthesia, which reduces hospital stays and lowers expenditures. However, it’s important to note that the increased intraoperative blood loss and prolonged operation length may elevate the probability of postoperative complications. Hu et al. [9]. investigated patients with tandem stenosis of cervical and upper-middle thoracic spine who underwent one-staged operation and found that it could provide a favorable prognosis of neurological function. However, it was observed that postoperative complications were more likely to occur in this group. In another study of Hu et al. [10]. , they concluded that patients with adjacent stenotic lesions could benefit from one-staged decompression; However, one-staged group experienced a higher incidence of dural tears compared to the two-staged group. Chen et al. [8]. conducted one-staged combined operation on patients with TCTS and observed that perioperative complications and progression of tandem ossification were associated with reduced patient satisfaction scores. Consequently, detailed communication with patients before surgery is deemed necessary. In a comparative study by Zhao et al. [14]. involving patients with tandem upper thoracic spinal stenosis and multi-segmental cervical spinal stenosis who underwent either one-staged or staged surgery, it was suggested that one-staged surgery resulted in greater short- and long-term improvement of neurological function compared to the staged operation, along with reduced hospitalization costs. Liao et al. [24] discovered that one-staged decompression could result in a satisfactory recovery of neurological function, but perioperative complications and ossification progression dramatically reduced patient satisfaction. In the treatment of thoracic OLF with CSM, Sun et al. [19]. compared one-staged and two-staged operation and showed that two-staged operation had a lower acceptable and outstanding rate than the one-staged operation did. Patients with simultaneous upper thoracic OLF and CSM are advised to receive one-staged decompression therapy. In the analysis of patients with TCTS, Chen et al. [20]. put forward one-staged surgery should be taken into consideration if the OLF was in the upper thoracic spine. Li et al. [23]. performed one-staged decompression on patients with upper thoracic OPLL complicated with cervical OPLL. They believed that one-staged decompression can streamline the produce and lead to extraordinary therapeutic results. Yao et al. [39]. conducted a study comparing the clinical effectiveness of one-staged and staged posterior decompression in the treatment of upper thoracic spinal stenosis coupled with multi-segmental cervical spine stenosis, suggesting that both one-staged and staged posterior decompression can produce positive clinical results, but one-staged operation has greater therapeutic efficacy than staged operation. In conclusion, one-staged combined operation emerges as an appropriate treatment option for patients with adjacent segmental stenosis, particularly for those with upper thoracic spinal stenosis concomitant with cervical spinal stenosis. Nevertheless, when confronted with a patient grappling with pronounced neurological afflictions in both the upper and lower extremities, devoid of manifest surgical contraindications, contemplation of one-staged operative intervention becomes tenable. It is imperative, however, to underscore that one-staged operation is associated with prolonged operative durations and heightened intraoperative perils. Moreover, it bears a heightened propensity for postoperative complications and the potential emergence of novel stenotic conditions at alternative levels, thereby attenuating patient satisfaction. Hence, a meticulous assessment of the holistic health status of each patient, coupled with comprehensive communication, is imperative prior to embarking on any surgical intervention. Ensuring sufficient postoperative management of complications further assumes paramount importance in the pursuit of optimal outcomes.
Two-staged operation
Two-staged operations exhibit the potential to diminish the incidence of complications by virtue of their reduced invasiveness. However, in certain cases, postoperative symptoms may not be relieved or even aggravated, necessitating additional hospitalization and contributing to a rise in medical expenditures. Sun et al. [19]. observed that patients manifesting severe symptoms in the lower extremities and mild symptoms in the upper extremities were advised to undergo thoracic spinal decompression as the initial step. However, the interval between staged operations did not become excessively protracted. In the study conducted by Chen et al. [20]. , focusing on patients with cervical OPLL or CSM complicated by thoracic OLF, the conclusion was drawn that in cases of concurrent severe cervical and thoracic compression, cervical decompression should take precedence. However, if the symptoms in the lower extremities were more severe than in the upper extremity, thoracic decompression should be done initially. Ma et al. [25]. in their investigation into cervical, thoracic, and lumbar degenerative diseases, posited that surgical intervention should be directed to the region exhibiting the most severe clinical symptoms and conspicuous spinal cord compression. They emphasized the inadvisability of relying solely on imaging findings to guide treatment decisions. For patients in compromised health or presenting with comorbidities such as diabetes, the suggestion is to conduct surgery initially in the proximal segment, with subsequent surgery in the distal segment three to six months later. Additionally, staged surgery is warranted when more than three adjacent segments of lesions are present. In summary, staged surgery confers significant advantages in minimizing undue trauma, particularly benefiting frail patients who may not withstand prolonged surgical procedures. When determining the sequence of decompression, it is paramount to prioritize the region displaying the most severe symptoms. For example, if the lower extremities exhibit more severe symptoms than the upper extremities, initiating with thoracic decompression is recommended. However, in cases where patients experience severe symptoms in both the upper and lower limbs, cervical decompression should take precedence. Nonetheless, it is crucial to monitor patients’ neurological function recovery constantly after the operation. If symptoms fail to ameliorate or worsen post-surgery, further decompression is advised for any residual stenosed segments.
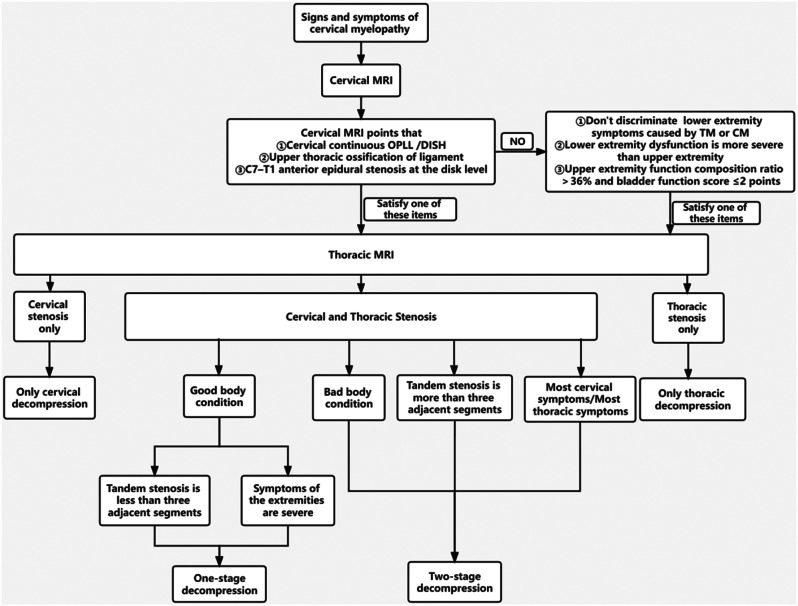
Diagnosis and surgery algorithm
Cervical spondylosis manifests with increasing prevalence in our contemporary society, and it possesses the proclivity to adeptly obfuscate the symptoms and signs associated with thoracic spinal canal stenosis. This may precipitate the erroneous categorization of individuals afflicted with thoracic canal stenosis as exclusively possessing cervical disorders. The clinical fraternity frequently disregards other facets of the spine, particularly the thoracic spine, subsequent to the identification of a cervical lesion through MRI. In light of these considerations, we conducted a systematic evaluation of the existing literature, formulating an algorithm for the diagnostic and surgical treatment of TCTS according to its symptoms and imaging characteristics (Fig. 2).
Fig. 2.
Flow-chart of diagnosis and treatment algorithm. OPLL, ossification of posterior longitudinal ligament; DISH, diffuse idiopathic skeletal hyperostosis; TM, thoracic myelopathy; CM, cervical myelopathy; MRI, Magnetic Resonance Imaging; The upper extremity score and bladder function score were derived from the Japanese Orthopedic Association(JOA) Spinal Cord Function Score. The upper extremity score is the sum of the upper extremity motor and sensory function scores.Upper extremity function composition ration = the upper extremity score/total JOA Spinal Cord Function score
Conclusion
In actuality, the incidence of TCTS is not as low as expected, primarily owing to the potential for missed diagnosis. A meticulous scrutiny of physical examinations and imaging becomes imperative when assessing individuals afflicted with myelopathy. Following diagnosis, conservative treatment seldom works while surgery frequently does. There are pros and cons to either one-staged or two-staged surgery, but both demonstrate comparable long-term outcomes. The optimal treatment plan should be selected based on the patients’ individual circumstances.
Acknowledgements
Yanze Lin is the first author, and Guoran Xu is the co-first author.
Abbreviations
- TSS
Tandem spinal stenosis
- TCTS
Tandem cervical and thoracic stenosis
- MRI
Magnetic resonance imaging
- CSM
Cervical spondylotic myelopathy
- OPLL
Ossification of posterior longitudinal ligament
- OLF
Ossification of ligamentum flavum
- JOA
Japanese orthopedic association
- DISH
Diffuse idiopathic skeletal hyperostosis
- CD
Cervical decompression
- TD
Thoracic decompression
- ACDF
Anterior cervical discectomy and fusion
- ACCF
Anterior cervical corpectomy and fusion
- CD
Circumferential decompression
Author contributions
YL and FF designed the study. YL, GX and YS performed database searches. GX, YS and JZ reviewed the studies. YL, GX and JZ worked on all images and tables. The text was written by YL and was reviewed by GX and FF. All the authors contributed to this article and approved the submitted version.
Funding
This research was supported in part by Zhejiang traditional Chinese medicine Science and Technology Program under grant number 2023ZL256,and the Medical Health Science and Technology Project of Zhejiang Provincial Health Commission (Grant No. 2024KY664) funds were received in support of this work.
Data availability
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yanze Lin and Guoran Xu contributed equally to this work.
References
- 1.Teng P, Papatheodorou C. Combined cervical and lumbar spondylosis. Arch Neurol. 1964;10:298–307. 10.1001/archneur.1964.00460150068007 [DOI] [PubMed] [Google Scholar]
- 2.Dagi TF, Tarkington MA, Leech JJ. Tandem lumbar and cervical spinal stenosis. Natural history, prognostic indices, and results after surgical decompression. J Neurosurg. 1987;66(6):842–9. 10.3171/jns.1987.66.6.0842 [DOI] [PubMed] [Google Scholar]
- 3.Dowlati E, Mualem W, Black J, Nunez J, Girish A, Fayed I, et al. Should asymptomatic cervical stenosis be treated in the setting of progressive thoracic myelopathy? A systematic review of the literature. Eur Spine J. 2022;31(2):275–87. 10.1007/s00586-021-07046-1 [DOI] [PubMed] [Google Scholar]
- 4.Chang UK, Choe WJ, Chung CK, Kim HJ. Surgical treatment for thoracic spinal stenosis. Spinal Cord. 2001;39(7):362–9. 10.1038/sj.sc.3101174 [DOI] [PubMed] [Google Scholar]
- 5.Ko SB, Lee SW, Shim JH. Paraplegia due to missed thoracic meningioma after Laminotomy for lumbar spinal stenosis: report of two cases. Asian Spine J. 2011;5(4):253–7. 10.4184/asj.2011.5.4.253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ (Clinical Res ed). 2004;328(7454):1490. 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhandutia A, Brown L, Nash A, Bussey IAN, Shasti M, Koh E, et al. Delayed diagnosis of Tandem spinal stenosis: a Retrospective Institutional Review. Int J Spine Surg. 2019;13(3):283–8. 10.14444/6038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, Chen DY, Wang XW, Lu XH, Yang HS, Miao JH. Single-stage combined decompression for patients with tandem ossification in the cervical and thoracic spine. Arch Orthop Trauma Surg. 2012;132(9):1219–26. 10.1007/s00402-012-1540-5 [DOI] [PubMed] [Google Scholar]
- 9.Hu P, Yu M, Liu X, Liu Z, Jiang L, Chen Z. One-staged combined decompression for the patients with cervico-thoracic tandem spinal stenosis. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European section of the cervical. Spine Res Soc. 2017;26(2):374–81. [DOI] [PubMed] [Google Scholar]
- 10.Hu PP, Yu M, Liu XG, Liu ZJ, Jiang L. Surgeries for patients with Tandem spinal stenosis in cervical and thoracic spine: combined or staged surgeries? World Neurosurg. 2017;107:115–23. 10.1016/j.wneu.2017.07.129 [DOI] [PubMed] [Google Scholar]
- 11.Jannelli G, Baticam NS, Tizi K, Truffert A, Lascano AM, Tessitore E. Symptomatic tandem spinal stenosis: a clinical, diagnostic, and surgical challenge. Neurosurg Rev. 2020;43(5):1289–95. 10.1007/s10143-019-01154-9 [DOI] [PubMed] [Google Scholar]
- 12.Uehara M, Tsutsumimoto T, Yui M, Ohta H, Ohba H, Misawa H. Single-stage surgery for compressive thoracic myelopathy associated with compressive cervical myelopathy and/or lumbar spinal canal stenosis. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European section of the cervical. Spine Res Soc. 2016;25(6):1904–11. [DOI] [PubMed] [Google Scholar]
- 13.Wang C, Wang QZ, Gao JH, Zhang L, Zhang L, Chen BH. Clinical comparison of selective versus nonselective decompression for symptomatic Tandem stenosis of the cervical and thoracic spine: a retrospective cohort study. Orthop Surg. 2021;13(2):537–45. 10.1111/os.12889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao BL, Ji C, Jiang JJ, Yin RF. Clinical effectiveness of treatment of combined upper thoracic spinal stenosis and multilevel cervical spinal stenosis with different posterior decompression surgeries. Int J Surg (London England). 2018;55:220–3. 10.1016/j.ijsu.2018.02.060 [DOI] [PubMed] [Google Scholar]
- 15.Kawaguchi Y, Oya T, Abe Y, Kanamori M, Ishihara H, Yasuda T, et al. Spinal stenosis due to ossified lumbar lesions. J Neurosurg Spine. 2005;3(4):262–70. 10.3171/spi.2005.3.4.0262 [DOI] [PubMed] [Google Scholar]
- 16.Park JY, Chin DK, Kim KS, Cho YE. Thoracic ligament ossification in patients with cervical ossification of the posterior longitudinal ligaments. Spine. 2008;33(13):E407–10. 10.1097/BRS.0b013e318175c276 [DOI] [PubMed] [Google Scholar]
- 17.Shiokawa K, Hanakita J, Suwa H, Saiki M, Oda M, Kajiwara M. Clinical analysis and prognostic study of ossified ligamentum flavum of the thoracic spine. J Neurosurg. 2001;94(2 Suppl):221–6. [DOI] [PubMed] [Google Scholar]
- 18.Nishiura I, Isozumi T, Nishihara K, Handa H, Koyama T. Surgical approach to ossification of the thoracic yellow ligament. Surg Neurol. 1999;51(4):368–72. 10.1016/S0090-3019(98)00051-2 [DOI] [PubMed] [Google Scholar]
- 19.Sun Co C, Zq LIU, Xg LIU, Zj, Qi Q, Guo Zq, et al. Selection of the surgical methods for the thoracic ossification of ligamentum flavum combined with cervical spondylotic myelopathy. Chin J Orthop. 2010;30:1087–90. [Google Scholar]
- 20.Chen Zq D, Gt LIU, Xg. The choice of treatment for ossification of Ligamentum Flavum of the thoracic spine. J Orthop. 1999;19:197–200. [Google Scholar]
- 21.Yao YZ, Yin RF, Huang J, Liu DL, Zang H. Different posterior decompression for patients with spinal canal stenosis in the upper thoracic and cervical spine. Natl Med J. 2016;96:1997–2001. [DOI] [PubMed] [Google Scholar]
- 22.Chen Zh T, Yz YC. Diagnosis and treatment of cervical and spondylotic myelopathy accompanied by thoracic spinal canal stenosis. Chin J Clin Neurosurg. 2003;8:34–5. [Google Scholar]
- 23.Ws LI, Zq C, Zen Y. Clinic characteristics and surgicalstrategy ofossification of the posterior longitudinal ligament of thoracic spine. Chin J Orthop. 2007;27:15–8. [Google Scholar]
- 24.LIao Xy C, Du, Chen Y, Wang X, Ll Y, Xw LIU, et al. One-stage combined decompression for tandem ossification in cervical and thoracic spine. J Spine Surg. 2015;13:65–70. [DOI] [PubMed] [Google Scholar]
- 25.MA X, Wang J. ClinicaI features and surgical treatment of the coexistence of cervical,thoracic and lumber degenerative disease. Chin J Orthop. 2010;30:1101–4. [Google Scholar]
- 26.Hy S, Xp L, Xh L, Js S, Ys W, Qq H, et al. Clinical curative effect analysis of one-staged spinal cord decompression for multilevel spinal stenosis in cervical, thoracic and lumbar. J Spinal Surg. 2015;13:289–93. [Google Scholar]
- 27.Cg S. Clinical diagnosis of myelopathy resulted from thoracic ossification of the ligament flavum associated with cervical spondyosis. J Spinal Surg. 2007;5:18–21. [Google Scholar]
- 28.Zhou F, Dang G. The diagnosis of MyeIopathy resulted from ossification of the Posterior Longitudinal Ligament of the Cervical Spine Associated with Ossfication of the Ligamentum Flavam of the thoracic spine. J Orthop. 1995;15:575–7. [Google Scholar]
- 29.Bajwa NS, Toy JO, Ahn NU. Is congenital bony stenosis of the cervical spine associated with congenital bony stenosis of the thoracic spine? An anatomic study of 1072 human cadaveric specimens. J Spin Disord Tech. 2013;26(1):E1–5. 10.1097/BSD.0b013e3182694320 [DOI] [PubMed] [Google Scholar]
- 30.Rahmanian A, Minagar S, Rakei SM, Taghipoor M, Mehrabani G, Razmkon A. A survey of Tandem spinal stenosis in Shiraz,Southern Iran. Neurosurg Q: Neurosurg Q; 2015. [Google Scholar]
- 31.Mut M, Cila A, Varli K, Akalan N. Multilevel myelopathy in Maroteaux-Lamy syndrome and review of the literature. Clin Neurol Neurosurg. 2005;107(3):230–5. 10.1016/j.clineuro.2004.05.003 [DOI] [PubMed] [Google Scholar]
- 32.Lindert EJv, Bartels RHMA, Noordam K. Spinal stenosis with paraparesis in Albright Hereditary Osteodystrophy. Pediatr Neurosurg. 2008;44:337–40. 10.1159/000138373 [DOI] [PubMed] [Google Scholar]
- 33.Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. Handb Clin Neurol. 2014;119:541–9. 10.1016/B978-0-7020-4086-3.00035-7 [DOI] [PubMed] [Google Scholar]
- 34.He Yc J, Jz L. Ym. Treatment and research progress of thoracic spinal stenosis. Chinese Journal of Bone and Joint.: Chinese Journal of Bone and Joint.; 2014.
- 35.Kuh SU, Kim YS, Cho YE, Jin BH, Kim KS, Yoon YS, et al. Contributing factors affecting the prognosis surgical outcome for thoracic OLF. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European section of the cervical. Spine Res Soc. 2006;15(4):485–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ben Hamouda K, Jemel H, Haouet S, Khaldi M. Thoracic myelopathy caused by ossification of the ligamentum flavum: a report of 18 cases. J Neurosurg. 2003;99(2 Suppl):157–61. [DOI] [PubMed] [Google Scholar]
- 37.Omojola MF, Cardoso ER, Fox AJ, Drake CG, Durward QJ. Thoracic myelopathy secondary to ossified ligamentum flavum. J Neurosurg. 1982;56(3):448–50. 10.3171/jns.1982.56.3.0448 [DOI] [PubMed] [Google Scholar]
- 38.Park MS, Moon SH, Kim TH, Oh JK, Lyu HD, Lee JH, et al. Asymptomatic stenosis in the cervical and thoracic spines of patients with symptomatic lumbar stenosis. Global Spine J. 2015;5(5):366–71. 10.1055/s-0035-1549031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yao YZ, Yin RF, Huang J, Liu DL, Zang H. Different posterior decompression for patients with spinal canal stenosis in the upper thoracic and cervical spine. Zhonghua Yi Xue Za Zhi. 2016;96(25):1997–2001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.