Abstract
BACKGROUND
Neurenteric cysts are rare congenital lesions from heterotopic endodermal tissue, often presenting with radiculopathy or myelopathy in young adults. Gross-total resection is curative; however, the surgical approach remains widely debated for cervicothoracic cases. While the posterior approach is common, the anterior approach has had success in adults. The authors present the first pediatric case of anterior corpectomy with gross-total resection of a cervicothoracic neurenteric cyst alongside an extensive literature review.
OBSERVATIONS
A 10-year-old male, who had undergone a previous cyst resection via a posterior approach at an outside institution, presented with back pain, paraplegia, and urinary incontinence. Magnetic resonance imaging of the spine revealed a ventral hyperintense cyst at C7–T1 consistent with a neurenteric cyst. An anterior approach involving C7 and T1 corpectomies was performed, including intradural exploration leading to complete cyst resection. This was followed by the placement of an expandable cage and anterior and posterior fixation with arthrodesis for stabilization. The patient’s symptoms completely resolved after surgery, and there has been no recurrence.
LESSONS
The anterior approach is a viable option for cervicothoracic neurenteric cyst resection in the pediatric population and can aid in gross-total resection by providing better lesion visualization. More studies are needed on long-term outcomes of the anterior approach in pediatric populations.
Keywords: neurenteric cyst, teratomatous cyst, congenital spinal lesion, case report
ABBREVIATIONS: CSF = cerebrospinal fluid, CT = computed tomography, MRI = magnetic resonance imaging, PRIMSA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Neurenteric cysts are rare spinal cord lesions stemming from heterotopic endodermal tissue and comprise about 0.7%–1.3% of all spinal cord tumors.1 Most patients with symptomatic neurenteric cysts are diagnosed in their 20s or 30s, but pediatric cases have also been reported.2–6 Symptoms include pain, myelopathy, and radiculopathy, and these symptoms have been shown to wax and wane as cyst leakage and shifts in osmotic pressure change cyst volume.7, 8 Resection is the first-line treatment for neurenteric cysts, with gross-total resection associated with the lowest rates of recurrence.9 However, despite knowing the curative nature of gross-total resection, there is little consensus on the surgical approach, with 3 approaches, posterior, anterior, and lateral, described in the literature.10 Currently, the posterior approach is the most commonly described, and there is little information surrounding the complications and outcomes of both the lateral and anterior approaches. Here, we present a pediatric case of a neurenteric cyst at the cervicothoracic junction treated with an anterior surgical approach alongside an extensive literature review.
Illustrative Case
A 10-year-old male with no significant past medical history presented to a hospital outside the United States with progressive symptoms of back pain, paraplegia, and urinary incontinence. The symptoms worsened over a 3- to 6-month period. Computed tomography (CT) and subsequently magnetic resonance imaging (MRI) were performed, revealing a large extramedullary lesion ventral to the spinal cord at the cervicothoracic junction. The differential diagnosis included an arachnoid cyst and a neurenteric cyst. The patient was seen by a neurosurgeon, who treated the patient with C6, C7, and T1 laminectomy and cyst aspiration through a midline dorsal approach. The child developed additional weakness immediately after surgery; however, he improved to near-normal strength and sensation after 6 weeks of rehabilitation. Ultimately, pathology from the cyst aspiration confirmed an arachnoid cyst diagnosis.
The child immigrated to the United States, and he presented 1 year later to our hospital with a 6-week history of progressive symptoms: worsening back pain, difficulty ambulating, and urinary incontinence. He reported back pain at the level of the shoulder blades that occurred approximately 3–4 times a day for 30 minutes to an hour. The symptoms initially improved with massage and spinal flexion; however, over the 3 weeks prior to presentation, the pain worsened, and he developed gait instability and priapism, which prompted emergency room evaluation.
During our initial evaluation, he had full proximal upper-extremity strength, slight grip weakness, and 4+/5 weakness in both legs. His gait was unsteady, and he had myelopathy with 3 beats of clonus bilaterally and 3+ reflexes at the patella and ankle.
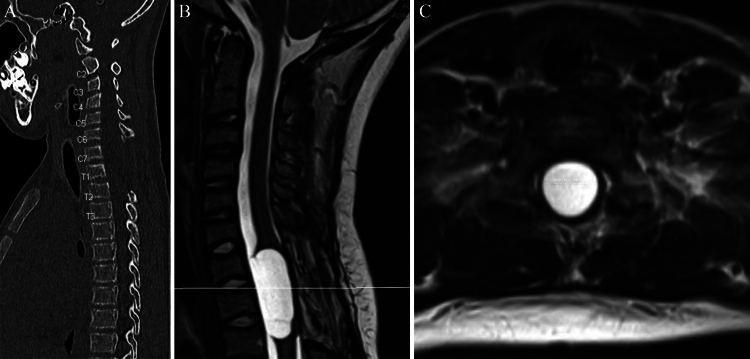
He underwent urgent MRI, which demonstrated a T1-hypointense, T2-hyperintense cystic lesion appearing to originate ventral to the spinal cord at the cervicothoracic junction. It was 1 cm in diameter and 3 cm in length (Fig. 1). A thin lip of spinal cord was stretched anterior to the most superior and inferior segments. Our differential diagnosis based on MRI included neurenteric cyst, neuroglial cyst, arachnoid cyst, or epidermoid cyst.
FIG. 1.
Preoperative noncontrast CT (A) of the cervical spine with prior C7–T1 laminectomies. The top of the sternum is approximately at the same level as the C7–T1 ventral cyst. Sagittal (B) and axial (C) preoperative MRI with a partially intramedullary cystic lesion in the ventral spinal cord at the level of C7–T1.
Due to the patient’s progressive gait dysfunction and myelopathy, surgical treatment was offered. A posterior approach would have required a 3-cm midline myelotomy to access the ventral mass, putting the patient at high risk for postoperative deficit. The sternum was low enough that an anterior approach was feasible. Furthermore, an anterior approach would provide direct access to the entirety of the cyst without having to traverse the spinal cord. Thus, we decided to perform C7 and T1 corpectomies to access the ventral dura, followed by cyst resection and anterior reconstruction. Posterior instrumented fusion was also performed because the prior surgery included extensive facetectomies at C6–7 and C7–T1, which would likely increase the risk of pseudoarthrosis with anterior fixation/arthrodesis alone.
Salient Points of the Operative Procedure
The patient was taken for a standard anterior approach for cervical corpectomy, and C7 and T1 corpectomies were performed. We saved bone for later arthrodesis. After the corpectomy was performed, it was straightforward to perform a midline durotomy, and the cyst and cyst wall were easily resected from this approach. We used 4-0 Nurolon sutures for a watertight dural closure, augmented by Tisseel. An expandable cage was placed and expanded to an adequate height, and bone graft was packed into the cage for arthrodesis. An anterior buttress plate was placed for anterior fixation. Following wound closure, the patient was placed prone for a standard posterior approach instrumented fusion between C6 and T2.
We used neuromonitoring throughout the case, and after cyst resection, the motor evoked potentials began improving and continued improving throughout the remainder of the case.
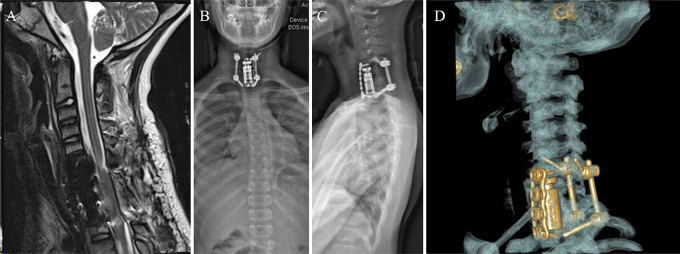
The patient tolerated the procedure well and experienced immediate resolution of pain after surgery. He was monitored in the neurointensive care unit for 1 day before being transferred to the ward for 6 days without any complications. He had no postoperative movement restrictions, and the day after surgery, he was walking with unsteadiness only to tandem gait. Otherwise, his physical examination remained unchanged from the preoperative examination. He was discharged with a cervical collar, which was weaned 3 months after surgery. Postoperative MRI showed resolution of the spinal cord deformation and cyst (Fig. 2A).
FIG. 2.
Postoperative noncontrast T2-weighted MRI (A) of the cervicothoracic spine shows no residual cyst. The previously seen spinal cord deformation has resolved. Postoperative anteroposterior (B) and lateral (C) scoliosis radiographs and ghost protocol CT (D) showing placement of the expandable corpectomy cage in place of the C7 and T1 vertebral bodies, anterior plate, and lateral mass screws at C6 with pedicle screws at T2, with overall good alignment.
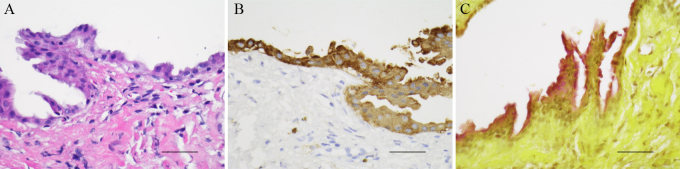
Pathology was consistent with a neurenteric cyst (Fig. 3). Histologically, there were small fragments of collagenous tissue with an epithelial lining composed of cuboidal to columnar cells with patchy cilia and rare goblet cells (Fig. 3A). The epithelial cells stained positive for pancytokeratin (Fig. 3B) and EMA and were negative for GFAP and S100. Goblet cells were highlighted with mucicarmine stain (Fig. 3C). No glial tissue was identified.
FIG. 3.
A: The cyst wall is composed of dense connective tissue and is lined by cuboidal to columnar cells with rare goblet cells (hematoxylin and eosin). B: Epithelial lining is immunoreactive for pancytokeratin. C: Goblet cells are highlighted with mucicarmine stain. Bars = 0.05 mm.
At the 13-month follow-up, the patient had solid arthrodesis on CT and no recurrence of the cyst on MRI. He had no back pain or weakness, and his examination was much improved with the resolution of myelopathy, clonus, and hyperreflexia, as well as full strength and normal gait and station. He had no additional episodes of priapism.
Literature Review
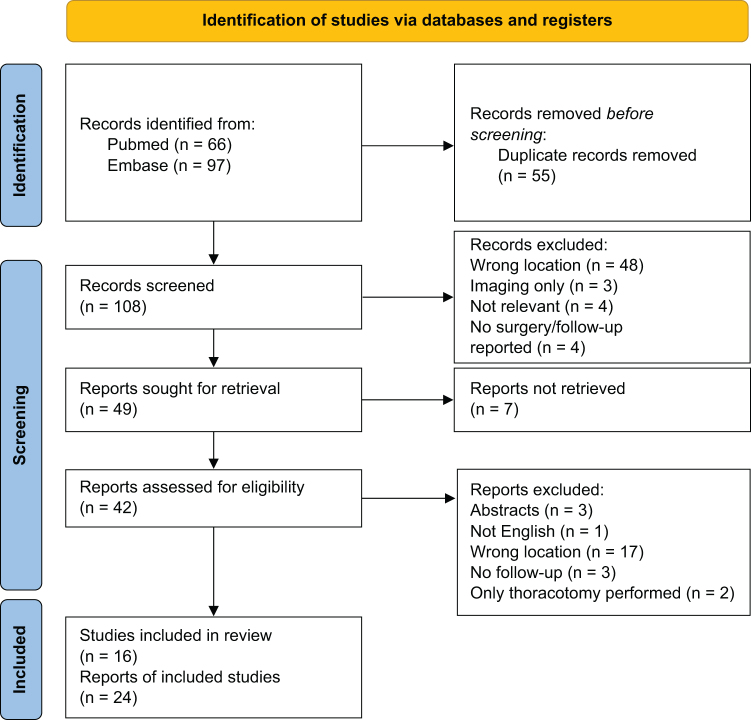
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 methodology (Fig. 4) was used to identify relevant cases. Abstracts describing neurenteric cysts in areas other than the cervicothoracic junction were excluded.11 Abstracts focusing only on imaging and those without postoperative follow-up were also excluded. We performed a full-text review for the remaining abstracts, and an additional 26 were excluded based on incorrect cyst location, lack of follow-up, lack of neurosurgical intervention, and lack of a full English-language paper, yielding 16 studies for this review. From these 16 papers, we report 25 cases of neurenteric cysts, including our own, at the cervicothoracic junction. Information regarding patient age, sex, symptoms, cyst level, MRI findings, surgical approach, complications, outcomes, recurrence, and follow-up deficits were collected (Table 1).
FIG. 4.
PRISMA flow diagram. From Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
TABLE 1.
Reported cases of neurenteric cysts at the cervicothoracic junction in children and adults
| Authors & Year | Age (yrs) | Sex | Symptoms | Spinal Level | Imaging | Surgical Approach | Outcome | Reccurrence | Surgical Complication | Follow-Up Deficit |
|---|---|---|---|---|---|---|---|---|---|---|
| Salehani et al., 202122 | 45 | M | Progressive, rt LE weakness & inability to walk | C6–7 | Ventral, T2-hyperintense, nonenhancing, intradural, extramedullary lesion | Ant C6–7 corpectomies w/ ant plating & fixation from C5 to T1 | Total resection, improvement of weakness 1 mo later | No recurrence 1 mo postop | None | None |
| Unnithan, 202230 | 48 | Not reported | Hand & LE weakness, spastic gait, decreased sensation below T6, brisk ankle & knee reflexes | C7–T1 | Ventral, T1-hypointense, T2-hyperintense, nonenhancing, intradural, extramedullary cystic lesion | C7–T1 laminectomy | Total resection, improved myelopathy 2 wks later | No | Pseudo-meningocele | Mild neck pain w/ lat movement 5 yrs later |
| Chen et al., 202026 | 0.25 | F | Torticollis, rt claw hand, impaired movement of rt forearm, impaired rt thumb adduction & index finger flexion, ankylosis of rt elbow | C4–T6 | Enlarged dumbbell cystic lesion in paravertebral region w/ intradural extramedullary extension via rt C4–5 foramen to intrathoracic cavity | C3–T1 laminectomy & thoracotomy | Total resection, improvement of denervation on EMG 4 mos later | No recurrence 4 yrs postop | None | None |
| Singh et al., 201719 | 1.5 | Not reported | Imbalance w/ repeated falls, truncal ataxia, LE hypertonia (lt>rt) | C7–T1 | Ventral, T2-hyperintense, cystic lesion | Far lat approach | Total resection, symptomatic improvement 3 mos later | No recurrence 6 mos postop | None | None |
| Can et al., 201525 | 29 | M | Klippel-Feil syndrome, progressive paresthesia, UE weakness (lt>rt), LE hyperreflexia & muscle spasms, sensory deficits in lt hand, weakness in lt biceps | C4–7 | Congenital fusion C5–T1 & a ventral, T2-hyperintense, nonenhancing, intradural, extramedullary cystic lesion | C4–T1 laminectomy | Total resection, symptomatic improvement 7 mos postop | T1, contrast- enhancing focus at C6 7 mos later | None | None |
| Ito et al., 201120 | 14 | F | 2 mos of progressive neck & shoulder pain, vesicoureteral disturbances, hyperreflexia of lt biceps & patellar tendon | C6–7 | Ant, intradural, slightly enhancing cystic lesion | Ant C6 corpectomy w/ removal of inferior margin of C5 & superior margin of C7 & ant spinal fusion | STR, immediate pain improvement | No recurrence 18 mos postop | None | None |
| Cai et al., 200824 | 10 | M | LE weakness for 1 mo, back pain for 15 days, sphincter incontinence for 4 days, LE hypotonia, & weak plantar reflex | C6–T2 | Ventral, intradural, extramedullary oval cyst hyperintense to CSF | C5–T2 laminectomy | Incomplete resection, neurologically normal 13 mos postop | No reccurrence 13 mos postop | Not reported | None |
| Garg et al., 20087 | 8 | M | Myelopathy | C7–T2 | Ventral, intradural extramedullary | Dorsal approach | Partial resection, symptomatic improvement | Recurred 3 times over 23 yrs | Not reported | Not reported |
| Garg et al., 20087 | 35 | M | Myelopathy | C7–T1 | Ventral, intradural extramedullary | Dorsal approach | Partial resection, symptomatic improvement | No recurrence 15 yrs postop | Not reported | Not reported |
| Garg et al., 20087 | 4 | M | Myelopathy | C5–T1 | Ventral, intradural extramedullary | Dorsal approach | Total resection, symptomatic improvement | No recurrence 2 yrs postop | Not reported | Not reported |
| Garg et al., 20087 | 28 | M | Myelopathy | C5–T1 | Ventral, intradural extramedullary | Dorsal approach | Total resection, no change | No recurrence 2 mos postop | Not reported | Not reported |
| Garg et al., 20087 | 4 | M | Sudden-onset myelopathy | C6–T1 | Ventral, intradural extramedullary | Dorsal approach resulting in total resection | Total resection, no change | 1 recurrence 13 mos postop | Not reported | Not reported |
| Garg et al., 20087 | 30 | M | Myelopathy | C6–T1 | Ventral, intradural extramedullary spina bifida at C7 | Dorsal approach resulting in total resection | Total resection, symptomatic improvement | No recurrence 3 yrs postop | Not reported | Not reported |
| Sasani et al., 200716 | 41 | F | Neck pain for 9 mos, moderate constriction of head movement in flexion & extension | C7 |
Ant, T1-hyperintense, T2-hypointense, intradural, extramedullary cystic lesion | Ant discectomy & corpectomy of C7 | Total resection, immediate pain resolution | No recurrence 18 mos postop | None | None |
| Sasani et al., 200716 | 39 | F | 1 yr of neck pain | C7–T1 | Ant, T1-hyperintense, T2-hypointense, intradural, extramedullary cystic lesion | Ant discectomy & partial corpectomy of C7–T1 w/ placement of ant cervical plates | Total resection | No recurrence 18 mos postop | None | None |
| Awasthy et al., 200523 | 12 | F | Hemiparesis | C6–T2 | Ant, intradural, extramedullary cystic lesion | Pst laminectomy | Total resection | No | None | None |
| de Oliveira et al., 20054 | 4 | M | Acute tetraparesis | C5–T3 | Ant, T1-hypointense, T2-hyperintense, nonenhancing, intradural, extramedullary cystic lesion | Pst laminectomy | Total resection, neurological function intact | No recurrence 2.5 yrs postop | None | None |
| de Oliveira et al., 20054 | 2 | F | History of diastematomyelia, acute paraparesis | C7–T1 | Ant, T1-hypointense, T2-hyperintense, nonenhancing, intradural, extramedullary cystic lesion | Pst laminectomy | Total resection, symptomatic improvement | No recurrence 8 yrs postop | None | Persistent LE weakness |
| Shenoy & Raja, 20046 | 3 | M | Intermittent fever for 2 mos, neck pain for 10 days, LE weakness, difficulty passing urine for 5 days, LE hypertonia & hyperreflexia | C7–T1 | Ant, T1-hypointense, T2-hyperintense, extramedullary cystic lesion w/ segmental syringomyelia below lesion | Pst C6–T3 laminectomy w/ total resection | Total resection | No recurrence 3 yrs postop | None | No neurological improvement |
| Laidlaw, 200321 | 36 | F | Sensory change in all limbs, mild neck & interscapular pain, urinary frequency & urgency, down-going lt plantar reflex | C6–7 | Ventral, T1 hypointense, T2 hyperintense, w/ small enhancing region, intradural | Median C6 & C7 corpectomies w/ titanium plate in C5 & T1 bodies | Total resection, complete resolution of symptoms | No | CSF collection postop day 4, resolved in 2 mos | None |
| Kim et al., 199927 | 5 | F | Sudden, rapid quadriparesis | C4–T2 | Ventral, T1 hypointense, T2 hyperintense, intradural, extramedullary | Pst laminectomy | STR, complete resolution of symptoms | No recurrence 19 mos postop | Not reported | None |
| Kim et al., 199927 | 38 | M | Lt UE weakness & pain for 23 yrs, rt UE weakness & pain for 8 mos | C4–7 | Ventral, T1 hypointense, T2 hyperintense, intradural, extramedullary | Pst laminectomy | STR, improved weakness | No recurrence 9 mos later | Not reported | Persisting pain |
| Prasad et al., 199629 | 6 | M | Cervicothoracic kyphoscoliosis, spastic paraparesis, mild weakness of hand grip | Upper cervical–T3 | Ventral cystic lesion & pst spina bifida w/ hypoplastic T1 & T2 | C4–7 laminectomy | Total resection, spasticity relief | No | None | None |
| Matsushima et al., 198528 | 8 | F | Intermittent episodes of quadriparesis since age 4 yrs, spastic paresis, hyperesthesia below C7, bilat absent triceps reflex, restricted neck motion | C5–T1 | Ant, intradural, extramedullary | C4–T1 laminectomy | STR, complete resolution of symptoms | No recurrence 3 yrs postop | None | None |
ant = anterior; EMG = electromyography; LE = lower extremity; pst = posterior; STR = subtotal resection; UE = upper extremity.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
Neurenteric cysts are uncommon congenital abnormalities of the spinal axis resulting from the incomplete separation of the endoderm and notochord during the 3rd week of embryogenesis.10 As a result, they are lined with heterotopic endodermal tissue, the cells of which secrete large amounts of the proteinaceous fluid found within the cyst.12 Since their initial description in 1928, neurenteric cysts have undergone numerous name changes, including teratomatous cysts and intestinomas, and have been reported in both the adult and pediatric population.4, 10 In pediatric populations, approximately 60% of neurenteric cyst cases are reported in males.10 Reported symptoms in children include those seen in adults, such as back pain, radiculopathy, and myelopathy, in addition to unique signs including aseptic and pyogenic meningitis, chronic pyrexia, incontinence, and paraplegia.4, 6, 7, 9, 13
Neurenteric cysts are commonly found with lesions ventral to the spinal cord.2, 9 Approximately 90% are intradural/extramedullary, with the remaining 10% being intradural/intramedullary or extradural.14 The first-line treatment is gross-total resection to avoid cyst recurrence.9 Although anterior, posterior, and lateral surgical approaches have been reported, the posterior approach is most commonly described.15
The posterior approach involves a laminectomy for cyst exposure, with risks including spinal cord, dura, and nerve root injury, as well as hematoma, all relating to the degree of exposure.10, 16 Despite these potential risks, few surgical complications have been reported;4 however, this does not mean that the approach is without technical challenges, as the spine can obstruct the cyst view, making resection of the cyst and any associated adhesions difficult. Although this approach is the most commonly reported, there is ongoing debate concerning whether it is the best method.10
The anterior approach, in contrast, involves corpectomy. While it provides better visualization to ventral cysts, aiding in gross-total resection,9 it comes with its own surgical challenges, sometimes requiring instrumented fusion after corpectomy. Risks include neurovascular compromise, cerebrospinal fluid (CSF) leakage, and hematoma.16
The final approach, the lateral approach, is the least reported, but isolated case reports praise it for wide exposure and good visualization of the cyst-cord interface, particularly in high cervical cysts,17, 18 although 1 case reported the approach at the cervicothoracic junction.19 Risks include CSF leakage, nerve injury, vertebral artery injury, and bleeding from the prevertebral venous plexus.17, 19
In this case report, we present a pediatric patient with an anterior cervicothoracic partially intramedullary cyst in the C7–T1 region that was completely resected using an anterior surgical strategy, resulting in C7 and T1 corpectomies and combined C6–T2 anterior and posterior fusions. Given the cyst’s location, we determined that an anterior corpectomy would offer the highest probability of achieving complete resection and avoiding recurrence while minimizing the risk of trauma to the spinal cord.
An anterior approach to the resection of neurenteric cysts has been previously reported in the literature.16, 20–22 However, this is the first report of an anterior corpectomy and fixation in a pediatric patient that resulted in the complete resection of a neurenteric cyst.
In order to better characterize overall outcomes and complications of the anterior approach compared to the posterior, we reviewed all reported cases of neurenteric cysts at the cervicothoracic junction. We report 4 cases of anterior corpectomy with age ranges from 14 to 45 years. Three patients had total resection, while 1, a 14-year-old patient, underwent subtotal resection. No surgical complications were reported. All patients experienced symptomatic improvement, and none experienced recurrence during follow-up. No postoperative neurological deficits were reported.
Eighteen patients underwent posterior laminectomy, of whom 12 were pediatric. Ages ranged from 3 months to 48 years. Six cases resulted in subtotal resection. Overall, 3 patients who underwent posterior laminectomy, 2 of whom were pediatric, experienced recurrence. Two patients had surgical complications (pseudomeningocele and fluid collection), and 2 experienced the persistence of neurological deficits after surgery. One patient had no symptomatic improvement after resection.
One patient underwent the lateral approach with no symptomatic improvement and no recurrence.
Lessons
Overall, the anterior approach is a feasible option for cyst resection at the cervicothoracic junction, as our own case and review of the literature show positive symptomatic improvement and no recurrence. This lack of recurrence may be attributable to higher rates of total resection due to improved tumor visibility. We recommend the anterior approach on a case-by-case basis according to imaging findings and the perceived level of cyst exposure given other approaches. Although we report success with this approach in the pediatric population, it remains significantly underreported, necessitating more data to better understand long-term outcomes.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Flores, Bauer. Acquisition of data: Tantry, McGinnis, Bauer. Analysis and interpretation of data: Flores, McGinnis, Bauer. Drafting the article: Ricciardelli, Tantry, Flores, McGinnis. Critically revising the article: Ricciardelli, Flores, McGinnis, Bauer. Reviewed submitted version of manuscript: Ricciardelli, Flores, McGinnis, Bauer. Approved the final version of the manuscript on behalf of all authors: Ricciardelli. Study supervision: Flores, Bauer.
Correspondence
Ashley Ricciardelli: Baylor College of Medicine, Houston, TX. ashley.ricciardelli@bcm.edu.
References
- 1.Fortuna A, Mercuri S. Intradural spinal cysts. Acta Neurochir (Wien). 1983;68(3-4):289-314. [DOI] [PubMed] [Google Scholar]
- 2.Agnoli AL, Laun A, Schönmayr R. Enterogenous intraspinal cysts. J Neurosurg. 1984;61(5):834-840. [DOI] [PubMed] [Google Scholar]
- 3.Arai Y, Yamauchi Y, Tsuji T, Fukasaku S, Yokota R, Kudo T. Spinal neurenteric cyst. Report of two cases and review of forty-one cases reported in Japan. Spine. 1992;17(11):1421-1424. [PubMed] [Google Scholar]
- 4.de Oliveira RS, Cinalli G, Roujeau T, Sainte-Rose C, Pierre-Kahn A, Zerah M. Neurenteric cysts in children: 16 consecutive cases and review of the literature. J Neurosurg. 2005;103(6suppl):512-523. [DOI] [PubMed] [Google Scholar]
- 5.Rao MB, Rout D, Misra BK, Radhakrishnan VV. Craniospinal and spinal enterogenous cysts—report of three cases. Clin Neurol Neurosurg. 1996;98(1):32-36. [DOI] [PubMed] [Google Scholar]
- 6.Shenoy SN, Raja A. Spinal neurenteric cyst: report of 4 cases and review of the literature. Pediatr Neurosurg. 2004;40(6):284-292. [DOI] [PubMed] [Google Scholar]
- 7.Garg N, Sampath S, Yasha TC, Chandramouli BA, Devi BI, Kovoor JME. Is total excision of spinal neurenteric cysts possible? Br J Neurosurg. 2008;22(2):241-251. [DOI] [PubMed] [Google Scholar]
- 8.Vinters HV, Gilbert JJ. Neurenteric cysts of the spinal cord mimicking multiple sclerosis. Can J Neurol Sci. 1981;8(2):159-161. [DOI] [PubMed] [Google Scholar]
- 9.Menezes AH, Ryken TC. Craniocervical intradural neurenteric cysts. Pediatr Neurosurg. 1995;22(2):88-95. [DOI] [PubMed] [Google Scholar]
- 10.Savage JJ, Casey JN, McNeill IT, Sherman JH. Neurenteric cysts of the spine. J Craniovertebr Junction Spine. 2010;1(1):58-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paolini S, Ciappetta P, Domenicucci M, Guiducci A. Intramedullary neurenteric cyst with a false mural nodule: case report. Neurosurgery. 2003;52(1):243-246. [DOI] [PubMed] [Google Scholar]
- 13.Rizk T, Lahoud GA, Maarrawi J, et al. Acute paraplegia revealing an intraspinal neurenteric cyst in a child. Childs Nerv Syst. 2001;17(12):754-757. [DOI] [PubMed] [Google Scholar]
- 14.Lippman CR, Arginteanu M, Purohit D, Naidich TP, Camins MB. Intramedullary neurenteric cysts of the spine. Case report and review of the literature. J Neurosurg. 2001;94(2suppl):305-309. [DOI] [PubMed] [Google Scholar]
- 15.Shukla M, Behari S, Guruprasad B, et al. Spinal neurenteric cysts: associated developmental anomalies and rationale of surgical approaches. Acta Neurochir (Wien). 2015;157(9):1601-1610. [DOI] [PubMed] [Google Scholar]
- 16.Sasani M, Ozer AF, Oktenoglu BT, Peker K, Bozkus MH, Sarioglu AC. Excision of an asymptomatic cervical intradural neurenteric cyst through the anterior approach: a study of two cases and a review of the literature. Spine J. 2007;7(6):720-727. [DOI] [PubMed] [Google Scholar]
- 17.Abhishek A, Anushree A, Patir R, Sehgal AD. Extreme lateral approach in a case of acute-onset quadriplegia due to high cervical neurenteric cyst. Pediatr Neurosurg. 2007;43(2):134-136. [DOI] [PubMed] [Google Scholar]
- 18.Song JK, Burkey BB, Konrad PE. Lateral approach to a neurenteric cyst of the cervical spine: case presentation and review of surgical technique. Spine. 2003;28(4):E81-E85. [DOI] [PubMed] [Google Scholar]
- 19.Singh H, Patir R, Vaishya S, Gupta A, Miglani R. Application of a far-lateral approach to the subaxial spine: application, technical difficulties, and results. World Neurosurg. 2017;100:167-172. [DOI] [PubMed] [Google Scholar]
- 20.Ito K, Aoyama T, Kiuchi T, et al. Ventral intradural endodermal cyst in the cervical spine treated with anterior corpectomy—case report. Neurol Med Chir (Tokyo). 2011;51(12):863-866. [DOI] [PubMed] [Google Scholar]
- 21.Laidlaw JD. Iso-intense neuroenteric cyst in the lower cervical spine treated with ventral resection and anterior fusion utilising sternal notch exposure: case report, technical note and literature review. J Clin Neurosci. 2003;10(5):606-612. [DOI] [PubMed] [Google Scholar]
- 22.Salehani A, Howell S, Harmon D. Management of a cervical spine neurenteric cyst via an anterior surgical approach: illustrative case. J Neurosurg Case Lessons. 2021;1(5):CASE20119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Awasthy N, Gupta H, Sharma K. Neuroenteric cyst: a rare cause of childhood hemiparesis. J Pediatr Neurol. 2005;3:179-181. [Google Scholar]
- 24.Cai C, Hu X, Shen C, Yang W, Zhang Q. Intraspinal neurenteric cysts in children. Can J Neurol Sci J Can Sci Neurol. 2008;35(5):609-615. [DOI] [PubMed] [Google Scholar]
- 25.Can A, Dos Santos Rubio EJ, Jasperse B, Verdijk RM, Harhangi BS. Spinal neurenteric cyst in association with Klippel-Feil syndrome: case report and literature review. World Neurosurg. 2015;84(2):592.e9-592.e14. [DOI] [PubMed] [Google Scholar]
- 26.Chen CY, Tsai HL, Yang TF, Liang ML. Congenital dumbbell neurenteric cyst mimics neonatal brachial plexus injury. Pediatr Neonatol. 2020;61(5):563-564. [DOI] [PubMed] [Google Scholar]
- 27.Kim CY, Wang KC, Choe G, et al. Neurenteric cyst: its various presentations. Childs Nerv Syst. 1999;15(6-7):333-341. [DOI] [PubMed] [Google Scholar]
- 28.Matsushima T, Fukui M, Egami H. Epithelial cells in a so-called intraspinal neurenteric cyst: a light and electron microscopic study. Surg Neurol. 1985;24(6):656-660. [DOI] [PubMed] [Google Scholar]
- 29.Prasad VS, Reddy DR, Murty JM. Cervico-thoracic neurenteric cyst: clinicoradiological correlation with embryogenesis. Childs Nerv Syst. 1996;12(1):48-51. [DOI] [PubMed] [Google Scholar]
- 30.Unnithan AKA. A case of neurenteric cyst of spine mimicking an arachnoid cyst. Spinal Cord Ser Cases. 2022;8(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]