Abstract
Background:
The use of cuffed endotracheal tubes (ETTs) has become the standard of care in pediatric practice. The rationale for the use of a cuffed ETT is to minimize pressure around the cricoid while providing an effective airway seal. However, safe care requires that the cuff lie distal to the cricoid ring following endotracheal intubation. The current study demonstrates the capability of computed tomography (CT) imaging in identifying the position of the cuff of the ETT in intubated patients.
Methods:
The study included patients ranging in age from 1 month to 10 years who underwent neck and chest CT imaging that required general anesthesia and endotracheal intubation. The location of the ETT and of the cuff within the airway was determined from axial CT images at three levels (proximal, middle, and distal). Anatomical orientations were tabulated, and percent chances of each orientation were determined for the ETT and the cuff.
Results:
The study cohort included 42 patients ranging in age from 1 to 114 months. An ETT with a polyvinylchloride cuff was used in 24 patients, and an ETT with a polyurethane cuff was used in 18 patients. The ETT was located near the posterior wall of the trachea in approximately 24–38% of patients, being most likely to be centrally located at the proximal end and at its mid-portion. The middle part of the cuff was most likely to be positioned in the mid-portion of the trachea but tended to skew anteriorly at both the proximal and distal ends.
Conclusion:
This is the first study using CT imaging to identify the uniformity of cuff inflation within the trachea in children. With commonly used cuffed ETTs, cuff inflation and the final position of ETT cuff within the tracheal lumen were not uniform. Future investigations are needed to determine the reasons for this asymmetry and its clinical implications.
Keywords: Computed tomography imaging, cricoid ring, endotracheal intubation, endotracheal tube cuff, pediatric airway, trachea
Introduction
The debate regarding the use of cuffed versus uncuffed endotracheal tubes (ETTs) in infants and children has generally been settled in favor of the use of cuffed ETTs. This has resulted in a change in clinical practice in both the operating rooms and the pediatric intensive care unit. This change in practice has been driven by clinical studies demonstrating clinical advantages with the use of cuffed ETTs including enhanced efficacy in sealing the airway during positive pressure ventilation, assurance of a stable and predictable tidal volume, prevention of aspiration, a decreased need for ETT exchange, and a decreased incidence of a sore throat.[1,2,3,4,5]
The ETT as well as the cuff which is placed within the airway can pose a risk for airway injury in children.[6,7,8] While the etiology of airway complications from endotracheal intubation is multi-factorial, malpositioning of the cuff and high intra-cuff pressures are two factors which may be responsible.[9,10,11] The ideal configuration of the cuff of the ETT should guarantee equal expansion of the cuff on all sides of the ETT. Although this has generally been assumed to be the case, there are no studies evaluating the orientation of the cuff of the ETT and its inflation within the airway in children. The aim of this study is to define the orientation of the cuff of the ETT within the airway in infants and children using computed tomography (CT) imaging.
Methods
After obtaining IRB approval, this retrospective observational study was performed at Sidra Medicine (Doha, Qatar) date of approval July 17, 2023. As a retrospective study, the need for individual informed consent was not deemed necessary. The study included patients ranging in age from 1 month to 10 years who underwent neck and chest CT imaging that required general anesthesia and endotracheal intubation from January 2018 until January 2020. Exclusion criteria included patients with a history of airway pathology, previous tracheostomy, the presence of a mediastinal mass, diaphragmatic hernia, extra-pulmonary and intra-thoracic masses, pre-term infants, and patients with genetic/chromosomal syndromes. The data were identified and retrieved from the picture archive and communicating systems (PACS) of the Department of Radiology. As a retrospective study, the study protocol did not control the process of endotracheal intubation including the type of ETT used, medications used for the induction and maintenance of anesthesia including neuromuscular blocking agents, or the technique of laryngoscopy. Standard clinical methods including the presence of exhaled end-tidal carbon dioxide and equal bilateral breath sounds were used to confirm the position of the ETT. Demographic data were recorded, as well as the type and the size of the ETT used.
The CT scans were performed with the head and neck in the neutral position as deemed necessary by the imaging protocols. All imaging acquisitions were made using two identical CT scanners with identical imaging protocols and configurations (SOMATOM Definition Flash, Siemens Healthineers AG, Erlangen, Germany). Acquired data were transferred to the standalone workstation (syngo.via, Siemens Healthineers AG, Erlangen, Germany, Software version VB30A_HF06) for evaluation. Sinogram Affirmed Iterative Reconstruction (SAFIRE) at Level 3 was used on all images. Images were reconstructed using the soft kernel (I30), with the abdomen window on default settings. Two pediatric anesthesiologists evaluated the CT scans in consensus with each other. The location of the ETT and of the cuff within the airway were determined from axial CT images at three levels (proximal, middle, and distal aspects of the cuff) [Figures 1 and 2]. Anatomical orientations were tabulated and percent chances of each orientation were determined for the ETT and the cuff.
Figure 1.
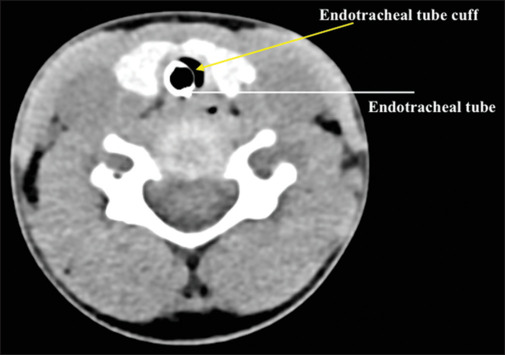
Axial CT image of a patient showing the location of the cuff of the ETT within the airway. The ETT cuff is skewed anteriorly with the ETT displaced posteriorly
Figure 2.

Axial CT image of a patient showing the location of the distal end of the ETT within the airway. The ETT is positioned in the middle of the airway
Statistical analysis
Demographic data as well as the characteristics and the size of the ETT were summarized as mean ± standard deviation (SD) or counts with percentages. Data analysis was performed in Stata/SE 16.1, and a two-tailed P < 0.05 was considered statistically significant.
Results
The study cohort included 42 patients ranging in age from 1 to 114 months and in weight from 2.94 to 61.8 kilograms [Table 1]. A standard ETT with a polyvinylchloride cuff was used in 24 patients, and a Microcuff® ETT with a polyurethane cuff was used in 18 patients. The sizes and types of ETTs used are listed in Table 2. The positions of the ETT and the cuff are shown in Figure 3 (proximal, middle, and distal). The ETT was located near the posterior wall of the trachea in approximately 24–38% of patients, being most likely to be centrally located at the proximal end and at its mid-portion. The middle part of the cuff was most likely to be positioned in the mid-portion of the trachea but tended to skew anteriorly at both the proximal and distal ends. The mid-section of both the ETT and the cuff had the highest chance (57–60%) of having a central orientation in the trachea, while the distal end had the lowest chance of being centered (26–29%).
Table 1.
Demographic data of the study cohort
| Study parameters | Results | |
|---|---|---|
| Number of patients | 42 | |
| Age (months) | 41.6±7.1 | |
| Gender (male/female) | 25/17 | |
| Height (centimeters) | 86.7±5.0 | |
| Weight (kilograms) | 14.7±1.9 |
Table 2.
ETT characteristics of the study cohort (n=42)
| ETT information | Number | |
|---|---|---|
| Type of ETT* (standard/Microcuff®) | 24/18 | |
| ETT size (mm ID) | ||
| 3.0 | 4 | |
| 3.5 | 9 | |
| 4.0 | 6 | |
| 4.5 | 12 | |
| 5.0 | 3 | |
| 5.5 | 4 | |
| 6.0 | 3 | |
| 6.5 | 1 |
*Standard ETT with a polyvinylchloride cuff or Microcuff® with a polyurethane cuff
Figure 3.

Positions of the ETT and the cuff within the airway in the study cohort of 42 patients
Discussion
We have previously demonstrated the feasibility of using CT imaging to identify the position of an ETT cuff within the airway in infants and children.[12] Our previous study was the first to demonstrate the use of CT imaging to evaluate the position of the cuff in relationship to the cricoid ring using sagittal images. For the first time, the current study uses axial images to evaluate the symmetry of cuff inflation and the position of the ETT and its cuff within the airway. In general, we noted that cuff inflation was not uniform and that in the many patients, there was skewing of the cuff and the ETT away from the center of the trachea. Although it may have been assumed that cuff inflation would be uniform, the current study demonstrates the non-uniformity of cuff inflation and the potential for the cuff and ETT to be positioned away from the center of the trachea. Non-uniform inflation occurred with both polyurethane and polyvinylchloride cuffs.
Despite the reported clinical advantages of using a cuffed ETT, excessive pressure within the cuff related to its over-inflation or other factors may lead to the potential for damage to the tracheal mucosa.[8] Concerns regarding the cuff pressure relate to not only the instantaneous intra-cuff pressure but also the duration of endotracheal intubation. In general, the intra-cuff pressure should be maintained at ≤20–30 cmH2O.[13] Various assumptions are made when arriving at the recommendation to limit intra-cuff pressures to this level. In the normal state, it has been estimated that the capillary perfusion pressure of the tracheal mucosa in man is 22 mmHg with a pressure at the arterial end of approximately 30 mmHg. In an animal model, progressive obstruction of venous outflow results in an increase of the pressure at the arterial end so that pressures in excess of 50 mmHg are needed to cause tracheal mucosal injury.[14] In an endoscopic study evaluating tracheal blood flow in man, obstruction to mucosal blood flow occurred at a lateral pressure above 22 mmHg (30 cmH2O).[15] When assessed using scanning electron microscopy in an animal model, no difference in damage to the tracheal mucosa was noted when comparing cuff inflation to seal the airway to a peak inflating pressure of 20 cmH2O, which resulted in a median intra-cuff pressure of 14 cmH2O, versus inflation of the cuff to an intra-cuff pressure of 20 cmH2O.[11] In a retrospective clinical study of 2953 pediatric patients over a 4-year period, the incidence of the stridor was less than 1% when a slight leak around the ETT was noted with the application of 25 cmH2O of continuous positive pressure to the airway.[16] These studies have been used to develop the current recommendations to limit the intra-cuff pressure to less than 20–30 cmH2O. However, despite following these recommendations, damage to the tracheal mucosa with airway sequelae may occur, thereby supporting the clinical impression that other factors play a role, including co-morbid conditions including those which affect cardiovascular function and perfusion pressure, genetic factors, pre-existing airway abnormalities, and the duration of endotracheal intubation and the intra-cuff pressure. The current study poses another possibility that may impact tracheal mucosa, malposition of the ETT within the airway, and the potential for non-uniform cuff inflation with variations in the cuff–mucosa interface.
We had generally assumed that cuff inflation was symmetrical; however, the current study demonstrates that this is not the case. Several factors (both internal and external to the cuff) may impact the uniformity of cuff inflation, including the type of cuff (polyurethane or polyvinyl chloride), shape of the cuff (cylindrical or tapered), thickness of the cuff material and its uniformity, and the inflation method including the technique used to cuff sealing of the airway. The thickness of a polyurethane cuff is estimated to be approximately 7–10 μm compared to 50 μm for a polyvinylchloride cuff.[17] Commonly used ETTs have a natural curvature or the Magill curve, which serves to facilitate placement into the trachea without a style. This curve may result in an asymmetric direction and subsequent placement of the ETT within the airway. This could be corrected by making the distal 1/3rd of the ETT straight and confining the Magill curve to the upper half of the ETT. Additionally, it is also possible that external factors such as the anatomy or shape of the airway or patient positioning may impact the inflation of the cuff.
Previous studies have demonstrated differences between in vitro and in vivo characteristics of cuff inflation with the potential for redundancy of the cuff material with the formation of recesses and longitudinal channels on the surface when inflated within the trachea.[18] This redundancy was such that it resulted in ineffective sealing of the airway as demonstrated by the passage of dye around the cuff of the ETT. The cuff material may not expand uniformly throughout the inflation process, thereby creating areas of contact and non-contact between the cuff and the tracheal wall. This may result in varying pressures at the point of contact.[19,20]
In general, an intra-cuff pressure of 20–30 cmH2O is recommended so that adequate ventilation can be provided during the application of positive pressure and the aspiration of secretions from above the cuff can be prevented.[21] In clinical practice, several techniques may be used to ensure a cuff pressure within these ranges, including slowly inflating the cuff to seal the airway while auscultating and holding CPAP at 20–30 cmH2O, palpation of the pilot balloon, monitoring of inhaled and exhaled tidal volumes or flow volume loops, and use of a manometer.[8,13,22,23,24,25] Variations in pressure and rate of inflation during filling of the cuff may theoretically result in asymmetric cuff inflation, especially when differences exist in the tensile strength of the cuff, which may result in areas that inflate more rapidly as the intra-cuff pressure increases.
Limitations of the current study included its retrospective nature and a somewhat limited cohort size. Our cohort size was restricted by the number of available patients with CT imaging with an ETT in place. The study cohort was also affected by the need to include only those CT images with optimal image quality as we had to ensure visibility of the cuff of the ETT within the trachea, resulting in a further decrease in sample size. This impacted our ability to draw conclusions regarding differences in outcome based on patient demographics (age, weight, height) as well as the type of ETT used and the cuff (polyvinylchloride versus polyurethane). The retrospective study also eliminated the potential for standardization of the anesthetic technique for ETT placement, so there was variation in the methodology used by the individual practitioners including the choice of ETT, medications and technique of endotracheal intubation, the technique used to confirm the correct location of the ETT within the trachea, and most importantly the technique of cuff inflation.
In conclusion, the current study demonstrates the feasibility of using CT imaging to identify the uniformity of cuff inflation within the trachea as well as the position of the ETT. Although the ideal location of the ETT cuff inside the airway has not clearly been identified, as the cricoid and subglottic regions are relatively non-distensible when compared to the lower aspects of the airway, it is generally recommended that the cuff be placed below the cricoid. With commonly used cuffed ETTs, the current study suggests that cuff inflation and the final position of the cuff and the tip of the ETT within the tracheal lumen are not uniform. Future investigations are needed to determine the reasons for this asymmetry and its clinical implications. More importantly, if this asymmetry in inflation is responsible for airway trauma, mechanisms to avoid it need to be determined.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Khine HH, Corddry DH, Kettrick RG, Martin TM, McCloskey JJ, Rose JB, et al. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology. 1997;86:627–31. doi: 10.1097/00000542-199703000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Motoyama EK. The shape of the pediatric larynx: Cylindrical or funnel shaped? Anesth Analg. 2009;108:1379–81. doi: 10.1213/ane.0b013e31819ed494. [DOI] [PubMed] [Google Scholar]
- 3.Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC. Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children. Br J Anaesth. 2009;103:867–73. doi: 10.1093/bja/aep290. [DOI] [PubMed] [Google Scholar]
- 4.de Wit M, Peelen LM, van Wolfswinkel L, de Graaff JC. The incidence of postoperative respiratory complications: A retrospective analysis of cuffed vs uncuffed tracheal tubes in children 0-7 years of age. Paediatr Anaesth. 2018;210:17–28. doi: 10.1111/pan.13340. [DOI] [PubMed] [Google Scholar]
- 5.de Orange FA, Andrade RG, Lemos A, Borges PS, Figueiroa J, Kovatsis PG. Cuffed versus uncuffed endotracheal tubes for general anaesthesia in children aged eight years and under. Cochrane Database Syst Rev. 2017;11:CD011954. doi: 10.1002/14651858.CD011954.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhardwaj N. Pediatric cuffed endotracheal tubes. J Anaesth Clin Pharm. 2013;29:13–8. doi: 10.4103/0970-9185.105786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.James I. Cuffed tubes in children. Paediatr Anaesth. 2001;11:259–63. doi: 10.1046/j.1460-9592.2001.00675.x. [DOI] [PubMed] [Google Scholar]
- 8.Tobias JD. Pediatric airway anatomy may not be what we thought: Implications for clinical practice and the use of cuffed endotracheal tubes. Paediatr Anaesth. 2015;25:9–19. doi: 10.1111/pan.12528. [DOI] [PubMed] [Google Scholar]
- 9.Minnigerode B, Richter HG. Pathophysiology of subglottic tracheal stenosis in childhood. Prog Pediatr Surg. 1987;21:1–7. doi: 10.1007/978-3-642-71665-2_1. [DOI] [PubMed] [Google Scholar]
- 10.Liu H, Chen JC, Holinger LD, Gonzales-Crussi F. Histopathologic fundamentals of acquired laryngeal stenosis. Pathol Lab Med. 1995;15:655–77. doi: 10.3109/15513819509027004. [DOI] [PubMed] [Google Scholar]
- 11.Kutter APN, Bittermann AG, Bettschart-Wolfensberger R, Spielmann N, Hartnack S, Ziegler U, et al. Do lower cuff pressures reduce damage to the tracheal mucosa? A scanning electron microscopy study in neonatal pigs. Paediatr Anaesth. 2013;23:117–21. doi: 10.1111/pan.12066. [DOI] [PubMed] [Google Scholar]
- 12.Wani TM, John J, Bahun V, AlGhamdi F, Tumin D, Tobias JD. Endotracheal tube cuff position in relation to the cricoid in children: A retrospective computed tomography-based analysis. Saudi J Anaesth. 2021;15:403–8. doi: 10.4103/sja.sja_396_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tobias JD, Schwartz L, Rice J, Jatana K, Kang DR. Cuffed endotracheal tubes in infants and children: Should we routinely measure the cuff pressure? Int J Pediatr Otothrinolaryng. 2012;76:61–3. doi: 10.1016/j.ijporl.2011.09.033. [DOI] [PubMed] [Google Scholar]
- 14.Nordin U. The trachea and cuff induced tracheal injury. An experimental study on causative factors and prevention. Acta Otolaryngol. 1976;345(suppl):1–71. [PubMed] [Google Scholar]
- 15.Seegobin RD, Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: Endoscopic study of effects of four large cuff volumes. Br Med J. 1984;288:965–8. doi: 10.1136/bmj.288.6422.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Black AE, Hatch DJ, Nauth-Misir N. Complications of nasotracheal intubation in neonates, infants and children: A review of 4 years’ experience in a children’s hospital. Br J Anaesth. 1990;65:461–7. doi: 10.1093/bja/65.4.461. [DOI] [PubMed] [Google Scholar]
- 17.Dullenkopf A, Schmitz A, Frei M, Gerber AC, Weiss M. Air leakage around endotracheal tube cuffs. Eur J Anaesth. 2004;21:448–53. doi: 10.1017/s0265021504006064. [DOI] [PubMed] [Google Scholar]
- 18.Negro MS, Barreto G, Antonelli RQ, Baldasso TA, Meirelles LR, Moreira MM, et al. Effectiveness of the endotracheal tube cuff on the trachea: Physical and mechanical aspects. Rev Bras Cir Cardiovasc. 2014;29:552–8. doi: 10.5935/1678-9741.20140096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maguire S, Haury F, Jew K. An in vitro comparison of tracheostomy tube cuffs. Med Devices (Auckl) 2015;8:185–92. doi: 10.2147/MDER.S76960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Bassi G, Ranzani OT, Marti JD, Giunta V, Luque N, Isetta V, et al. An in vitro study to assess determinant features associated with fluid sealing in the design of endotracheal tube cuffs and exerted tracheal pressures. Crit Care Med. 2013;41:518–26. doi: 10.1097/CCM.0b013e31826a4804. [DOI] [PubMed] [Google Scholar]
- 21.Sole ML, Su X, Talbert S, Penoyer DA, Kalita S, Jimenez E, et al. Evaluation of an intervention to maintain endotracheal tube cuff pressure within therapeutic range. Am J Crit Care. 2011;20:109–17. doi: 10.4037/ajcc2011661. quiz 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moon KM, Donaworth S, Hagele MS, Kim SS, Willer BL, Tobias JD. Endotracheal tube cuff pressures in the operating room of a pediatric hospital: A quality improvement initiative. Pediatr Qual Saf. 2022;7:e619. doi: 10.1097/pq9.0000000000000619. doi: 10.1097/pq9.0000000000000619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bryant J, Werner J, Moss E, Tobias JD. Can the intracuff pressure be estimated by palpation of the pilot balloon? ICU Director. 2013;4:170–2. [Google Scholar]
- 24.Borhazowal R, Harde M, Bhadade R, Dave S, Aswar SG. Comparison between two endotracheal tube cuff inflation methods; Just-seal Vs. stethoscope-guided. J Clin Diagn Res. 2017;11:UC01–3. doi: 10.7860/JCDR/2017/26301.10017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Almarakbi WA, Kaki AM. Tracheal tube cuff inflation guided by pressure volume loop closure associated with lower postoperative cuff-related complications: Prospective, randomized clinical trial. Saudi J Anaesth. 2014;8:328–34. doi: 10.4103/1658-354X.136422. [DOI] [PMC free article] [PubMed] [Google Scholar]


