Abstract
Restricted mouth opening is a challenging airway in pediatric patients with temperomandibular joint (TMJ) ankylosis. The fiber-optic bronchoscopic nasotracheal intubation technique continues to be the gold standard for difficult airway, among the techniques available such as submandibular intubation, retrograde intubation, and tracheostomy. However, awake fiber-optic bronchoscopy (FOB) is difficult to achieve in pediatric patients. Prior planning of the anesthetic method and effective collaboration with the surgeon are crucial for excellent outcomes in such challenging airway cases. We present a successful awake fiber-optic bronchoscopy with high-flow nasal oxygen (HFNO), airway blocks, and deep sedation in the case of bilateral TMJ ankylosis of a pediatric age group with reduced mouth opening. We conclude that awake intubation using HFNO and airway blocks helps to achieve oxygenation and ease of intubation in difficult airway management.
Keywords: Airway, HFNO, limited mouth opening, pediatric difficult airway, sedation, TMJ ankylosis
Introduction
Temperomandibular joint (TMJ) ankylosis is a condition that limits mouth opening and impairs the ability of the jaw to move normally and if worsened may lead to jaw stiffness in a growing child due to mandibular development. Managing the anesthetic concerns of children with restricted mouth opening is a challenging task. Technically, it includes both managing pediatric patients and dealing with difficult airway situations. Fiber-optic bronchoscopy (FOB) has a well-established role in patients with restricted airways, but it is highly challenging in pediatric patients because of reduced lung reserve and their lack of willingness to cooperate.
Case Report
A 14-year-old male weighing 43 kg presented with complaints of difficulty in mouth opening for 3 years and deformity of face for the past 5 years. The boy had an infection of the left ear at the age of 8 years for which he did not seek any medical attention. Repeated bilateral ear infection was noted after 1 year. He gradually developed an inability to open his mouth, increasing in severity to a present state of less than one finger, which resulted in the patient’s reduced food intake.
Airway assessment: ‘Bird facies’ with severely retrognathic mandible and micrognathia and bilateral condylar movement not palpable. Oral examination showed restricted mouth opening with an inter-incisor gap of 3 mm with buck teeth [Figure 1]. The orthopantomogram showed a lack of structural organization and the restriction of bilateral TMJ space. Computed tomography (CT) skull shows fusion of bilateral mandibular condyle with glenoid fossa. A diagnosis of bilateral bony TMJ ankylosis was confirmed. The patient’s vitals were appropriate for his age. Cardio-respiratory examination was normal. All other biochemical investigations were within normal limits. After a thorough pre-operative assessment, a challenging airway was predicted and awake fiber-optic intubation (AFOI) was planned. After adequate counseling, written informed assent from the child and consent were taken from the guardian. The otorhinolaryngology team was informed, and as a backup plan, a tracheostomy set was kept prepared.
Figure 1.
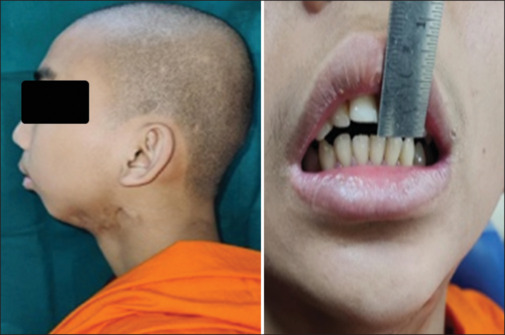
Profile of the patient showing bird facies with retrognathic mandible and buck teeth
Preparation
After confirming nil per oral status, intravenous glycopyrrolate 4 mcg/kg was given to reduce the secretions. The airway was prepared with 2 ml lignocaine with adrenaline 2% nebulization, 20 minutes before the procedure. All resuscitation tools and the difficult airway cart were kept on board. The tracheostomy equipment was set up in case of emergency.
After shifting the patient inside the operation theatre, standard ASA (American Society of Anesthesiologists) monitors were connected. The patient was started on high-flow nasal oxygen (HFNO) support at 50 L O2. After a loading dose of 1 mcg/kg/hr dexmedetomidine for 10 minutes, maintenance of 0.5 mcg/kg/hr infusion was administered intravenously for conscious sedation. With anatomical landmark guidance, bilateral superior laryngeal nerve (SLN) and recurrent laryngeal nerve block (RLN) were administered with 2% lignocaine 1 ml on each side for the SLN block and 4 ml 4% lignocaine for the RLN block. The total dose of lignocaine administered was within the toxic limits of the local anesthetic. AFOI was performed through the left nostril. Following the visualization of vocal cords, a 100 mg bolus of propofol was given and the trachea was intubated successfully with a well-lubricated size 6.0 flexometallic tube. The patient was maintained on oxygen, air (FiO2 0.40), and sevoflurane, and atracurium was given for skeletal muscle relaxation. Volume-controlled ventilation was used to maintain EtCO2 at optimal levels. Intra-operatively, the patient remained stable. Al Kayat Bramley incision was made, and bilateral excision of the ankylotic mass with temporalis muscle inter-position gap arthroplasty and right cricoidectomy with advancement genioplasty were performed, which increased mouth opening to 42 mm post-operatively [Figure 2].
Figure 2.

Postoperative improvement in mouth opening
Because of prolonged surgery and suspected airway edema, the patient was electively ventilated and observed in intensive care. He was extubated once fully awake and intact airway reflexes were resumed. The post-operative period was uneventful.
Discussion
TMJ ankylosis, a unique disease, is characterized by reduced mouth opening. Blind nasal, submandibular intubation, retrograde intubation, fiber-optic-aided nasal intubation, and tracheostomy are available methods.[1] Each method has a few potential risks. Blind nasal intubation typically needs multiple attempts, which may result in hemorrhage, laryngeal edema, and airway loss. Retrograde intubation is a challenging procedure that is rarely performed on a child with limited mouth opening. Since tracheostomy is an invasive procedure with associated morbidity, it is often reserved for emergencies. If nasotracheal fiber-optic intubation is intended, it is important to take precautions to prevent epistaxis. When a patient is conscious, they can protect themselves from aspirating blood, but when they are unconscious, they lose this protective mechanism.[2]
A pediatric airway can be managed with ease if there is good planning and readiness to tackle any complications that arise.[3] A “cannot intubate and cannot ventilate” scenario is a possibility if the condition worsens.[4] The gold standard for securing such a challenging airway is an awake fiber-optic intubation.[5]
However, awake fiber-optic intubation is not often successful in pediatric patients. In the pediatric population, patient cooperation is crucial. This can be initiated with adequate pre-operative counseling and airway preparation. But in children, this is usually not attainable. Hence, adequate sedation or general anesthesia may be required. There is a tendency for airway collapse with the onset of general anesthesia and muscular relaxation, and there is no opportunity for jaw thrust and chin lift in a patient with TMJ ankylosis. So, fiber-optic intubation under sedation with spontaneous respiration is most likely the safest method of securing the airway.[6]
So, in our case, xylometazoline nasal drops were given to avoid bleeding, which can obscure vision. Dexmedetomidine was used for sedation. It is a selective alpha-2 adrenoceptor agonist that benefits patients undergoing AFOI who have a difficult or unstable airway by sedating them and anxiolyzing them, with no effect on respiration.[7]
To prevent laryngospasm during intubation attempts, SLN block, recurrent laryngeal nerve block provides adequate airway anesthesia, lesser patient discomfort, and faster intubation to aid in AFOI.[8,9] In spontaneously breathing patients undergoing AFOI, HFNO improves oxygenation, which can extend the time interval until critical desaturation through the delivery of apneic oxygenation.[10]
Conclusion
We conclude that HFNO-supported, topical anesthetized, fiber-optic bronchoscopy with sedation not only helps by providing adequate time for its use and oxygenation but also helps in securing a difficult airway.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sharma A, Dwivedi D, Sharma RM. Temporomandibular joint ankylosis: “A pediatric difficult airway management”. Anesth Essays Res. 2018;12:282–4. doi: 10.4103/aer.AER_122_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kang JM, Lee KW, Kim DO, Yi JW. Airway management of an ankylosing spondylitis patient with severe temporomandibular joint ankylosis and impossible mouth opening. Korean J Anesthesiol. 2013;64:84–6. doi: 10.4097/kjae.2013.64.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akshara P, Govindan DK. Complete temporomandibular joint ankylosis with nil mouth opening: An anaesthetic challenge. J Basic Clin Appl Health Sci. 2022;5:49–51. [Google Scholar]
- 4.Kawasaki T, Sata T, Kawasaki C, Ogata M, Shigematsu A. Airway management of a child with temporomandibular joint ankylosis following otitis media. Anaesthesia. 2002;57:294–5. doi: 10.1111/j.1365-2044.2002.2520_19.x. [DOI] [PubMed] [Google Scholar]
- 5.Malik S, Dubey M, Batra V, Naithani B. Nasal fiberoptic intubation: A saviour during handling a pediatric difficult airway. Indian J Oral Sci. 2012;3:180. [Google Scholar]
- 6.Kundra P, Vasudevan A, Ravishankar M. Video-assisted fiberoptic intubation for temporomandibular ankylosis. Paediatr Anaesth. 2006;16:458–61. doi: 10.1111/j.1460-9592.2005.01730.x. [DOI] [PubMed] [Google Scholar]
- 7.Gupta K, Jain M, Gupta PK, Rastogi B, Saxena SK, Manngo A. Dexmedetomidine premedication for fiberoptic intubation in patients of temporomandibular joint ankylosis: A randomized clinical trial. Saudi J Anaesth. 2012;6:219–23. doi: 10.4103/1658-354X.101211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh J, Shakya S, Shrestha B, Subedi B, Singh PB. Awake fiberoptic intubation in cervical spine injury: A comparison between atomized local anesthesia versus airway nerve blocks. Kathmandu Univ Med J (KUMJ) 2018;16:323–7. [PubMed] [Google Scholar]
- 9.Gupta B, Kohli S, Farooque K, Jalwal G, Gupta D, Sinha S, et al. Topical airway anesthesia for awake fiberoptic intubation: Comparison between airway nerve blocks and nebulized lignocaine by ultrasonic nebulizer. Saudi J Anaesth. 2014;8(Suppl 1):S15–9. doi: 10.4103/1658-354X.144056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Badiger S, John M, Fearnley RA, Ahmad I. Optimizing oxygenation and intubation conditions during awake fibre-optic intubation using a high-flow nasal oxygen-delivery system. Br J Anaesth. 2015;115:629–32. doi: 10.1093/bja/aev262. [DOI] [PubMed] [Google Scholar]


