Abstract
Cervical radiculopathy might affect finger movement and dexterity. Postoperative features and clinical outcomes comparing C8 radiculopathies with other radiculopathies are unknown. This prospective multicenter study analyzed 359 patients undergoing single-level surgery for pure cervical radiculopathy (C5, 48; C6, 132; C7, 149; C8, 30). Background data and pre- and 1-year postoperative neck disability index (NDI) and numerical rating scale (NRS) scores were collected. The C5–7 and C8 radiculopathy groups were compared after propensity score matching, with clinical significance determined by minimal clinically important differences (MCID). Postoperative arm numbness was significantly higher than upper back or neck numbness, and arm pain was reduced the most (3.4 points) after surgery among the C5–8 radiculopathy groups. The C8 radiculopathy group had worse postoperative NDI scores (p = 0.026), upper back pain (p = 0.042), change in arm pain NRS scores (p = 0.021), and upper back numbness (p = 0.028) than the C5–7 group. NDI achieved MCID in both groups, but neck and arm pain NRS did not achieve MCID in the C8 group. In conclusion, although arm numbness persisted, arm pain was relieved after surgery for cervical radiculopathy. Patients with C8 radiculopathy exhibited worse NDI and change in NRS arm pain score than those with C5–7 radiculopathy.
Keywords: Cervical spine, Nerve root, Radiculopathy, Patient-reported outcome measures, Propensity score
Subject terms: Neurological disorders, Diseases of the nervous system, Spine regulation and structure
Introduction
Cervical radiculopathy is a condition that presents bilateral or unilateral paresthesia of the nerve root distribution. Affected patients are most frequently 45–54 years of age, and symptomatic cases of cervical radiculopathy occur based on the frequency of nerve root involvement in C7, C6, C5, and C8, wherein C6 and C7 roots account for most cases1. Approximately 75–90% of patients improve within 4–8 weeks with conservative treatment; however, surgical treatment may be needed for patients who do not improve2–4.
The symptoms of C5, C6, C7, and C8 nerve root radiculopathies differ, and the areas of muscle weakness and sensory deficits in the upper extremities vary according to the responsible nerve root5,6. Notably, C8 radiculopathy can significantly affect finger and hand movement and dexterity; therefore, postoperative outcomes and prognoses are important considerations for this nerve root level. Drop finger can occur with C8 radiculopathy, and such cases have been reported to have poor clinical outcomes7. Few studies have focused on postoperative outcomes specific to C8 radiculopathy8–10, and information comparing C8 radiculopathies with other cervical radiculopathies is lacking.
This study aimed to elucidate and confirm the features of cervical radiculopathies using patient-reported outcome measures (PROM) scores and compare the clinical outcomes between surgeries for C5–7 and C8 radiculopathies. Through this comparison, we aimed to provide information on clinical outcomes to further understand cervical radiculopathy.
Methods
We hypothesized that C8 radiculopathy would have poorer outcomes than C5–7 radiculopathies because a previous study reported poor postoperative recovery for C8 radiculopathy in clinical practice7. This study was approved by the University of Tokyo Hospital ethics committee (approval no. 10335), and all experiments were performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study.
Study design and patient samples
Retrospective data were obtained from the surveillance records of 359 patients who had undergone cervical spine surgery for radiculopathy. These patients had undergone procedures between 2017 and 2022 at one of the 11 hospitals participating in this prospective multicenter study. Patients with missing data in the current survey research items were excluded. The inclusion criterion was degenerative cervical radiculopathy without myelopathy or myeloradiculopathy. All patients had the diagnosis of “single-level cervical radiculopathy” on their preoperative surveillance record. This record also included demographic data, as detailed later in this section. Patients who underwent surgeries at a single intervertebral level were investigated because, even in cases of diagnosed single-level radiculopathy, overlapping symptoms from adjacent levels could not be definitively ruled out in cases of multiple intervertebral level surgery. Among the aforementioned patients, those with complete demographic data and patient-oriented questionnaires preoperatively and 1 year postoperatively were included. Patients with diagnoses of spinal tumors, rheumatoid arthritis, congenital abnormalities, infection, or trauma were excluded. The level of radiculopathy was classified as C5, C6, C7, or C8. The demographic data and clinical outcomes among patients undergoing surgery for C5, C6, C7, and C8 radiculopathies were investigated and compared. Subsequently, the surgical outcomes of patients with C8 radiculopathy were compared with those with C5, C6, and C7 radiculopathies (collectively).
Data collection
Demographic data, including age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status classification, presence of diabetes mellitus (DM), etiology (disc hernia or not), surgical procedure, and surgical level, were collected. Radiculopathy diagnosis, surgical indication, surgical procedure, and surgical level for the responsible nerve root were determined by the surgeons at each institution. Surgical procedures were classified as anterior decompression and fusion, posterior decompression, and posterior decompression and fusion.
Clinical outcomes
The PROM score questionnaires were collected preoperatively and included the Neck Disability Index (NDI) and numerical rating scale (NRS) for pain and numbness in the neck (A), upper back (B), and arms (C) (Fig. 1). At the 1-year postoperative follow-up, patients were encouraged to complete the same questionnaires. Additionally, improvement at each level and in the overall NDI rate (number of patients with radiculopathy exhibiting improvement [preoperative NDI score − postoperative NDI score > 0]/number of patients with radiculopathy), the NDI improvement rate ([preoperative NDI score − postoperative NDI score]/ [preoperative NDI score] ´ 100), and changes in the NRS scores (preoperative NRS score − postoperative NRS score) were analyzed. We also examined whether improvement of NDI, NRS neck pain, and NRS arm pain reached a MCID postoperatively. Using previously published results by Parker et al., we defined the MCID thresholds to be 17.3% for NDI, 2.6 points for NRS neck, and 4.1 points for NRS arm pain11.
Figure 1.
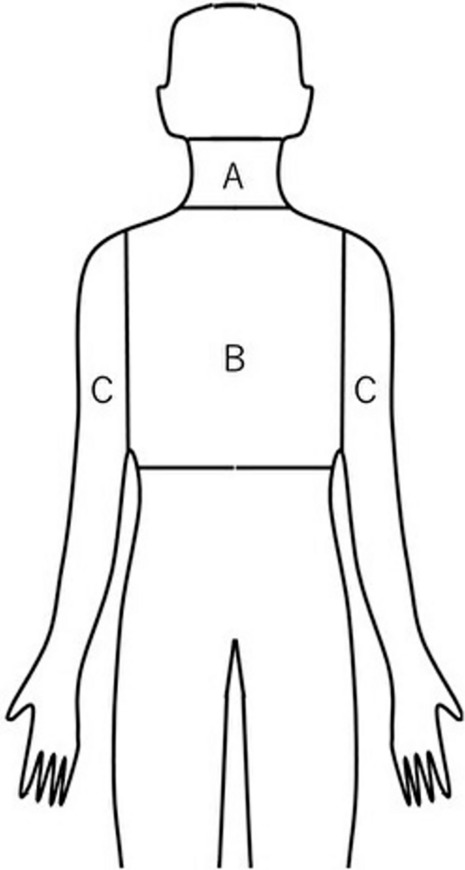
Areas of potential pain and numbness as indicated by the numerical rating scale.
Statistical analyses
Background data and PROM scores were compared using one-way analysis of variance (ANOVA) for categorical and continuous variables among those with C5, C6, C7, and C8 radiculopathies. Based on the ANOVA results, Tukey's multiple comparison test was performed for a detailed investigation of the statistical differences between the subgroups. Background data and PROM scores between patients with C5–7 and C8 radiculopathies were also analyzed using an unpaired t-test or Mann–Whitney U test for continuous variables and the chi-square test for categorical variables, as appropriate. To adjust for preoperative background factors between patients with C5–7 and C8 radiculopathies, propensity score matching was performed using logistic regression models. Demographic data including age, sex, BMI, ASA classification, DM, etiology (disc hernia or not), surgical procedure (posterior decompression, anterior decompression and fusion, and posterior decompression and fusion), and preoperative NDI scores were used for one-to-one propensity score matching between the two groups. The caliper of propensity matching was set at 0.20. R statistical software, version 2.8.1 (The R Foundation for Statistical Computing, Vienna, Austria), was used for statistical analyses. A p-value of < 0.05 was considered statistically significant.
Ethics approval
The study was approved by the University of Tokyo Hospital ethics committee, and all experiments were performed in accordance with the relevant guidelines and regulations.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Results
Among 359 patients who completely answered the PROM questions and underwent single-level intervertebral surgery for cervical radiculopathy, nerve root level involvement included 48 cases at C5, 132 at C6, 149 at C7, and 30 at C8.
The percentages of patients with improved NDI scores (preoperative NDI minus postoperative NDI > 0) at 1 year after surgery for cervical radiculopathy were as follows: C5, 85.4% (41/48); C6, 82.6% (109/132); C7, 90.6% (135/149); and C8, 73.3% (22/30). The overall improvement rate was 85.5% (307/359). The preoperative patient demographic data for age, ASA classification, etiology, and procedure involving the different nerve root levels were significantly different (Table 1).
Table 1.
Preoperative demographic data and overall NDI improvement rate.
| Total (mean [SD]) | C5 (mean [SD]) | C6 (mean [SD]) | C7 (mean [SD]) | C8 (mean [SD]) | p-value | |
|---|---|---|---|---|---|---|
| n | 359 | 48 | 132 | 149 | 30 | |
| Overall NDI improvement rate (%) | 85.5 | 85.4 | 82.6 | 90.6 | 73.3 | |
| Age (years) | 54.7 [10.9] | 60.9 [12.0] | 52.6 [10.9] | 53.4 [9.6] | 59.8 [10.2] | < 0.001 |
| Sex (male, %) | 75.2 | 75.0 | 75.8 | 79.9 | 73.3 | 0.767 |
| BMI (kg/m2) | 23.8 [3.4] | 23.5 [3.2] | 24.0 [3.7] | 23.7 [3.2] | 23.9 [3.5] | 0.873 |
| ASA grade (grade 1:2:3:4, %) | 40:56:3:0 | 29:64:6:0 | 39:60:2:0 | 38:58:5:0 | 80:20:0:0 | < 0.001 |
| Diabetes mellitus (%) | 9.7 | 8.3 | 8.3 | 11.4 | 10.0 | 0.830 |
| Etiology (disc hernia, %) | 31.8 | 33.3 | 40.2 | 27.5 | 13.3 | 0.016 |
| Surgical procedure (PD:ADF:PDF, %) | 72:25:2 | 52:46:2 | 72:27:1 | 79:18:3 | 87:10:3 | 0.002 |
ASA: American Society of Anesthesiologists Classification; ADF: anterior decompression and fusion; BMI: body mass index; NDI: neck disability index; PD: posterior decompression; PDF: posterior decompression and fusion; SD: standard deviation.
Bold values indicate p < 0.05.
The mean improvement rate in the overall NDI score was 49.2%. A comparison of the NRS score between pre- and postoperative data indicated an overall 2.5–3.4-point decrease in neck, upper back, and arm pain and a 0.8–3.4-point decrease in neck, upper back, and arm numbness. Arm pain was reduced the most after surgery among the C5–8 radiculopathy groups. These improvements (changes in NRS) were greater in the arms than in the upper back and neck; however, the postoperative residual NRS arm scores were also higher.
The four radiculopathy groups (namely: C5, C6, C7, and C8) revealed no significant differences in preoperative NDI scores; however, postoperative NDI scores (p = 0.013) and NDI improvement rates (p = 0.026) were significantly different among the four groups (Table 2).
Table 2.
Comparison of preoperative and postoperative data among surgeries for C5, 6, 7, and C8 radiculopathies.
| Total (mean [SD]) | C5 (mean [SD]) | C6 (mean [SD]) | C7 (mean [SD]) | C8 (mean [SD]) | p-value | |
|---|---|---|---|---|---|---|
| Preoperative PROM (NDI and NRS scores) | ||||||
| NDI scores | 17.1 [8.1] | 16.1[9.0] | 17.6 [7.6] | 17.4 [8.4] | 15.5 [8.2] | 0.447 |
| Neck pain | 4.4 [2.9] | 3.6 [2.7] | 4.8 [2.9] | 4.6 [2.9] | 3.0 [3.3] | 0.004 |
| Upper back pain | 3.4 [3.3] | 1.3 [2.4] | 3.3 [3.3] | 4.0 [3.4] | 3.9 [3.4] | < 0.001 |
| Arm pain | 5.4 [3.1] | 3.8[3.2] | 5.7 [2.8] | 5.9 [3.1] | 4.9 [2.9] | < 0.001 |
| Neck numbness | 1.6 [2.6] | 1.0 [1.9] | 1.7 [2.7] | 1.7 [2.8] | 1.0 [1.9] | 0.184 |
| Upper back numbness | 1.3 [2.5] | 0.4 [1.4] | 1.3 [2.5] | 1.7 [2.8] | 0.9 [1.7] | 0.008 |
| Arm numbness | 5.6 [2.9] | 3.9 [3.0] | 5.9 [2.7] | 6.0 [2.9] | 5.4 [3.0] | < 0.001 |
| Postoperative PROM (NDI and NRS scores) | ||||||
| NDI scores | 8.2 [7.7] | 8.0 [7.1] | 9.5 [8.4] | 6.8 [7.0] | 10.0 [7.7] | 0.013 |
| NDI improvement rate (%) | 49.2 [47.0] | 51.2 [39.4] | 43.9 [46.2] | 56.5 [50.0] | 32.5 [41.1] | 0.026 |
| Neck pain | 1.9 [2.4] | 1.9 [2.3] | 2.1 [2.5] | 1.7 [2.3] | 1.7 [2.3] | 0.521 |
| Changes in NRS | ||||||
| Neck pain | 2.5 [3.0] | 1.7 [2.4] | 2.7 [3.1] | 2.9 [3.0] | 1.3 [2.6] | 0.009 |
| Upper back pain | 1.3 [2.1] | 0.6 [1.4] | 1.6 [2.3] | 1.2 [1.9] | 1.6 [2.3] | 0.038 |
| Changes in NRS | ||||||
| Upper back pain | 2.1 [3.4] | 0.8 [2.0] | 1.8[3.3] | 2.8 [3.4] | 2.3 [4.4] | 0.002 |
| Arm pain | 2.0 [2.5] | 1.7 [2.1] | 2.6 [2.8] | 1.5 [2.1] | 2.8 [3.0] | 0.001 |
| Changes in NRS | ||||||
| Arm pain | 3.4 [3.6] | 2.1 [3.2] | 3.1 [3.5] | 4.4 [3.7] | 2.0 [3.4] | < 0.001 |
| Neck numbness | 0.8 [1.9] | 0.7 [2.1] | 1.0 [2.1] | 0.6 [1.5] | 1.0 [2.1] | 0.352 |
| Changes in NRS | ||||||
| Neck numbness | 0.8 [2.6] | 0.3 [2.2] | 0.8 [2.6] | 1.2 [2.9] | 0.0 [1.2] | 0.070 |
| Upper back numbness | 0.5[1.3] | 0.2 [0.7] | 0.6 [1.6] | 0.4 [1.9] | 0.4 [0.8] | 0.249 |
| Changes in NRS | ||||||
| Upper back numbness | 0.8 [2.4] | 0.2 [1.6] | 0.7 [2.4] | 1.3 [2.7] | 0.5 [1.9] | 0.021 |
| Arm numbness | 2.3 [2.7] | 1.5 [2.4] | 2.8 [2.9] | 1.9 [2.5] | 3.1 [2.8] | 0.003 |
| Changes in NRS | ||||||
| Arm numbness | 3.4 [3.4] | 2.4 [3.1] | 3.1 [3.5] | 4.1 [3.2] | 2.3 [3.4] | 0.001 |
NDI: neck disability index; NRS: numerical rating scale; PRO: patient-reported outcome; SD: standard deviation.
Bold values indicate p < 0.05.
One-way ANOVA for the NRS scores for the three groups of patients with postoperative neck, upper back, and arm numbness and for the three groups of patients with postoperative neck, upper back, and arm pain exhibited significant differences among the three numbness and three pain groups (F [2,1074] = 10.43, p < 0.001; F[2,1074] = 81.66, p < 0.001, respectively). Tukey’s multiple comparison test confirmed the absence of significant differences between the neck and upper back numbness groups and between the arm and neck pain groups (p > 0.05). However, significant differences were observed between the arm and upper back numbness groups (p < 0.001), between the arm and neck numbness groups (p < 0.001), between the upper back and neck pain groups (p = 0.002), and between the upper back and arm pain groups (p < 0.001) (Table 3).
Table 3.
Comparison of postoperative NRS scores among neck, upper back, and arm symptoms in C5–8 radiculopathy.
| Comparison | Mean difference | 95% confidence interval | p-value |
|---|---|---|---|
| Postoperative numbness | |||
| Neck vs. upper back | 0.29 | − 0.06, 0.65 | 0.133 |
| Arm vs. upper back | 1.81 | 1.45, 2.17 | < 0.001 |
| Arm vs. neck | 1.52 | 1.16, 1.88 | < 0.001 |
| Postoperative pain | |||
| Neck vs. upper back | 0.59 | 0.18, 1.00 | 0.002 |
| Arm vs. upper back | 0.76 | 0.35, 1.17 | < 0.001 |
| Arm vs. neck | 0.17 | − 0.24, 0.58 | 0.595 |
NRS: numerical rating scale.
Bold values indicate p < 0.05. Tukey’s multiple comparison test results.
The C8 radiculopathy group had the worst postoperative NDI score (Table 2). Additionally, this group was significantly different from the C5–7 radiculopathy group in terms of age, ASA grade, etiology, and NDI improvement rate. However, no significant differences in preoperative or 1-year postoperative NDI scores without propensity score matching were noted (Table 4).
Table 4.
Comparison of demographic data and clinical outcomes between patients with C5-7 and C8 radiculopathies.
| C5-7 radiculopathy (mean [SD]) | C8 radiculopathy (mean [SD]) | p-value | |
|---|---|---|---|
| N | 329 | 30 | |
| Age (years) | 54.2 [10.8] | 59.8 [10.2] | 0.006 |
| Sex (male, %) | 77.5 | 73.3 | 0.650 |
| BMI (kg/m2) | 23.8 [3.4] | 23.9 [3.5] | 0.892 |
| ASA grade (grade 1:2:3:4) | 37:59:4:0 | 80:20:0:0 | < 0.001 |
| Diabetes mellitus (%) | 9.7 | 10.0 | 1.000 |
| Surgical procedure (PD:ADF:PDF, %) | 72:26:2 | 87:10:3 | 0.078 |
| Etiology (disc hernia, %) | 33.4 | 13.3 | 0.024 |
| NDI scores | |||
| Preoperative | 17.3 [8.1] | 15.5 [8.2] | 0.242 |
| Postoperative | 8.0 [7.7] | 10.0 [7.7] | 0.180 |
| Improvement rate at the individual level (%) | 50.7 [47.3] | 32.5 [41.1] | 0.043 |
| NRS neck pain | |||
| Preoperative | 4.5 [2.9] | 3.0 [3.3] | 0.006 |
| Postoperative | 1.9 [2.4] | 1.7 [2.3] | 0.695 |
| Changes | 2.6 [3.0] | 1.3 [2.6] | 0.015 |
| NRS upper back pain | |||
| Preoperative | 3.3 [3.3] | 3.9 [3.4] | 0.346 |
| Postoperative | 1.3 [2.1] | 1.6 [2.3] | 0.420 |
| Changes | 2.1 [3.3] | 2.3 [4.4] | 0.669 |
| NRS arm pain | |||
| Preoperative | 5.5 [3.1] | 4.9 [2.9] | 0.281 |
| Postoperative | 2.0 [2.5] | 2.8 [3.0] | 0.071 |
| Changes | 3.5 [3.6] | 2.0 [3.4] | 0.030 |
| NRS neck numbness | |||
| Preoperative | 1.6 [2.7] | 1.0 [1.9] | 0.253 |
| Postoperative | 0.7 [1.9] | 1.0 [2.1] | 0.460 |
| Changes | 0.9 [2.4] | 0.5 [1.9] | 0.432 |
| NRS upper back numbness | |||
| Preoperative | 1.3 [2.5] | 0.9 [1.7] | 0.324 |
| Postoperative | 0.5 [1.3] | 0.4 [0.8] | 0.654 |
| Changes | 0.9 [2.4] | 0.5 [1.9] | 0.432 |
| NRS arm numbness | |||
| Preoperative | 5.7 [2.9] | 5.4 [3.0] | 0.612 |
| Postoperative | 2.2 [2.7] | 3.1 [2.8] | 0.082 |
| Changes | 3.5 [3.4] | 2.3 [3.4] | 0.066 |
ASA: American Society of Anesthesiologists; ADF: anterior decompression and fusion; BMI: body mass index; NDI: neck disability index; NRS: numerical rating scale; PD: posterior decompression; PDF: posterior decompression and fusion; SD: standard deviation.
Bold values indicate p < 0.05.
Upon matching patient backgrounds with age, sex, BMI, ASA physical status classification, presence of DM, etiology (disc hernia or not), surgical procedure, and preoperative NDI scores, we found significant differences in postoperative NDI scores (p = 0.026), postoperative upper back pain and numbness (p = 0.042; p = 0.028, respectively), and changes in the NRS scores of arm pain (p = 0.021) between patients with C5–7 and C8 radiculopathies (Table 5). Regarding minimal clinically important difference (MCID), the improvement rate of the NDI score, changes in NRS neck pain, and changes in NRS arm pain for the C5–7 radiculopathy group were 57.1%, 2.8, and 4.1, respectively. The improvement rate of the NDI score, changes in NRS neck pain, and changes in NRS arm pain for the C8 radiculopathy group were 29.1%, 1.3, and 1.7, respectively (Table 5).
Table 5.
Comparison of demographic data and clinical outcomes of matched patients using propensity score-matched (age, sex, BMI, ASA grade, diabetes mellitus, surgical procedure, etiology, and preoperative NDI) analysis.
| C5–7 radiculopathy (mean [SD]) | C8 radiculopathy (mean [SD]) | p-value | |
|---|---|---|---|
| n | 22 | 22 | |
| Age (years) | 57.7 [11.2] | 57.7 [10.7] | 1.000 |
| Sex (male, %) | 77.3 | 68.2 | 0.736 |
| BMI (kg/m2) | 24.6 [3.6] | 23.3 [3.6] | 0.226 |
| ASA grade (grade 1:2:3:4) | 64:36:0:0 | 73:27:0:0 | 0.747 |
| Diabetes mellitus (%) | 18.2 | 4.5 | 0.345 |
| Surgical procedure (PD:ADF:PDF, %) | 91:9:0 | 86:9:5 | 1.000 |
| Etiology (disc hernia, %) | 22.7 | 18.2 | 1.000 |
| Preoperative NDI scores | 15.4 [5.5] | 16.0 [8.7] | 0.772 |
| Postoperative NDI and NRS scores | |||
| NDI scores | |||
| Postoperative | 5.6 [ 6.0] | 10.6 [ 8.5] | 0.026 |
| Improvement rate at the individual level (%) | 57.1 [49.6] | 29.1 [42.2] | 0.050 |
| NRS neck pain | |||
| Postoperative | 1.0 [1.8] | 1.5 [2.9] | 0.382 |
| Changes | 2.8 [2.6] | 1.3 [2.7] | 0.067 |
| NRS upper back pain | |||
| Postoperative | 0.4 [0.9] | 1.3 [1.9] | 0.042 |
| Changes | 3.1 [3.5] | 2.6 [4.0] | 0.636 |
| NRS arm pain | |||
| Postoperative | 1.3 [2.1] | 2.9 [3.0] | 0.053 |
| Changes | 4.1 [3.1] | 1.7 [3.6] | 0.021 |
| NRS neck numbness | |||
| Postoperative | 0.1 [0.2] | 0.7 [1.8] | 0.081 |
| Changes | 0.8 [1.8] | 0.2 [1.3] | 0.218 |
| NRS upper back numbness | |||
| Postoperative | 0.1 [0.2] | 0.5 [0.9] | 0.028 |
| Changes | 0.5 [1.4] | 0.4 [2.1] | 0.802 |
| NRS arm numbness | |||
| Postoperative | 1.9 [2.2] | 2.8 [2.6] | 0.200 |
| Changes | 3.9 [3.4] | 2.2 [3.7] | 0.120 |
ASA: American Society of Anesthesiologists; ADF: anterior decompression and fusion; BMI: body mass index; NDI: neck disability index; NRS: numerical rating scale; PD: posterior decompression; PDF: posterior decompression and fusion; SD: standard deviation.
Bold values indicate p < 0.05.
Discussion
At 1 year postoperatively, 85.5% of patients with cervical radiculopathy had improved NDI; of these, 90.6%—the highest proportion of patients—had undergone surgery for C7 radiculopathy and 73.3%—the lowest proportion of patients—for C8 radiculopathy.
The NRS scores of all patients with cervical radiculopathy indicated that arm numbness was more likely to persist than upper back and neck numbness (p < 0.001; p < 0.001, respectively). Furthermore, upper back pain was less likely to persist than neck pain (p = 0.002) or arm pain (p < 0.001).
Comparison after propensity matching analysis also revealed that the C8 radiculopathy group was significantly inferior to the C5–7 radiculopathy group in terms of postoperative NDI scores (p = 0.026). In the C5–7 radiculopathy group, MCID was achieved postoperatively in all PROM parameters (NDI, NRS neck pain, and NRS arm pain). However, in the C8 radiculopathy group, although improvement of NDI achieved the MCID, improvement of NRS neck and arm pain did not achieve the MCID.
Our study compared the surgical outcomes for C8 radiculopathy with those for other cervical radiculopathy levels after single-level intervertebral surgeries. We limited the study to cervical radiculopathy by nerve root levels because few studies have focused on comparing surgical outcomes among nerve root levels. Therefore, the present study is novel. Our literature screening did not reveal any other studies that compared the surgical outcomes for C8 radiculopathy with those for other nerve root levels. A few case series limited to anterior surgery reported surgical outcomes for C8 radiculopathy as generally good8–10. Regarding surgical frequency in posterior foraminotomy, the percentage of C8 radiculopathy per nerve root level is reported to be low (8%)12. Similarly, randomized controlled trials comparing surgical procedures for single-level radiculopathy involving different nerve root levels have not focused on the C7/T1 intervertebral level. The incidence of C8 radiculopathy might have been so negligible that it was not reported in these studies13.
The postoperative outcomes in past reports are varied, including satisfactory outcomes ranging from 75–94% for radiculopathy14–17. Several reports on finger drop, which is thought to be caused by C8 (or C7) radiculopathy, reported postoperative muscle strength improvements of 53–74%7,18,19.
One possible reason for the subpar clinical outcome of C8 nerve root radiculopathy is the long distance from the site of nerve root damage to the hand, which is the output site of neurotransmission. Regarding motor impairment, cervical spondylotic amyotrophy (CSA), a condition that describes overlapping cervical nerve root disease and nerve compression sites, is also characterized by muscle atrophy and weakness, generally without sensory deficits. Previous reports suggest a worse prognosis for distal than for proximal CSA20–22. These results may be due to the long distance between the nerve compression site and the atrophied muscle21. C8 nerve root disease, which similarly presents in the distal part of the upper extremity, may not respond as well to surgery as other nerve root-level diseases.
Regarding sensory impairment, radiculopathy-induced symptoms in this study indicated that the improvement rate of NRS numbness in the distal anatomical areas (i.e., arm) was worse than that in the proximal areas (neck, upper back). This suggests that the distal upper limb remains symptomatic after radiculopathy surgery and that nerve recovery may be less than satisfactory in cases involving the nerve root periphery where the output of nerve transmission is distant from the foramen, since sensory deficits depend on the nerve fiber length and symptoms often appear at the distal end of the longest nerve. The related mechanism is thought to involve nutrient scarcity in peripheral axons, i.e., those that are far away from the cell body, where nutritive substances are synthesized. Therefore, a “dying-back degeneration” starts distally and moves proximally23.
Another consideration for these results is the surgical difficulty level because of anatomical differences. (Fig. 2) For example, the higher nerve roots, such as the C5 nerve root, run at a more ventral angle, whereas the lower nerve roots, such as C8, are laterally oriented; therefore, lateral decompression is required in posterior approach surgeries24. Additionally, the ribs overhang T1 laterally at the cervicothoracic junction; therefore, surgeons must be aware of this anatomical peculiarity at this level compared to that of other levels. For anterior surgeries, surgeons must reach deeper into the affected areas to decompress the C7/T1 intervertebral level while simultaneously being aware of the location of the sternum7. The penetrated nuclei in herniated discs at the C7/T1 level may be more lateral than those in the paramedian area25. Therefore, care must be taken to avoid inadequate lateral decompression, especially in the case of C8 radiculopathy.
Figure 2.
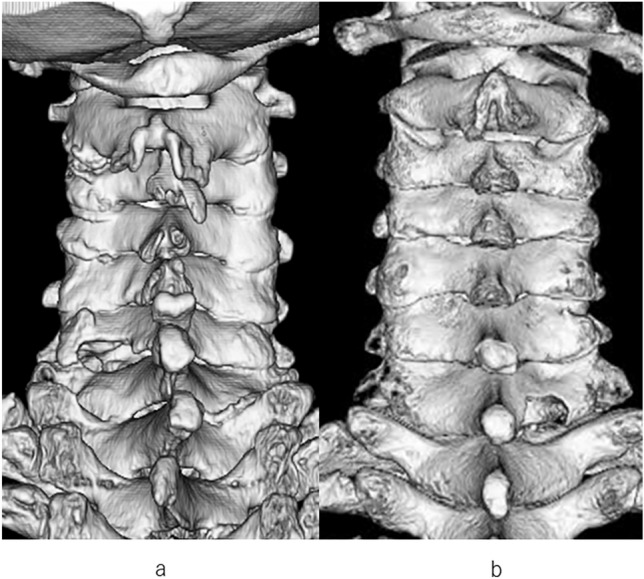
(a) Postoperative three-dimensional computed tomography (3DCT) of left C7 radiculopathy (the C5–7 radiculopathy group). (b) Postoperative 3DCT of right C8 radiculopathy.
Our study demonstrated that C8 radiculopathy did not differ from C5–7 radiculopathies in terms of postoperative residual arm numbness. However, compared to C5–7 radiculopathies, C8 radiculopathy resulted in residual postoperative upper back pain and less improvement in arm pain (Table 5). The surgical difficulty level might have led to this difference in clinical outcomes.
Our study had several limitations. First, the diagnosis of radiculopathy without myelopathy and myeloradiculopathy, surgical technique, timing of surgery, and diagnosis at the nerve root level were surgeon-dependent, with no uniformity in the treatment criteria, which might have affected surgical outcomes. Second, the postoperative follow-up period was relatively short, and long-term results may differ from those of the present study. Third, our data were from a surveillance-based prospective multicenter study, resulting in a decreased survey collection rate owing to missing data, which might have led to a selection bias. In addition, because we analyzed questionnaire results, practical and objective assessment tools for muscle strength and sensory impairment were not included in our analysis. Fourth, the degree of paralysis, the duration of symptoms prior to surgery, and imaging evaluation, which may affect surgical outcomes, were not included in the surveillance. For paralysis, questions on motor function were included in the NDI questionnaire, which was used for matching. Regarding the duration of symptoms, we chose not to include it in the propensity matching owing to the challenges in managing recurrent symptoms once they have improved and differentiating them when they co-exist with other peripheral neuropathies.
In conclusion, the results of this study will provide surgeons with key information to assist in surgical decision-making and discussions with patients regarding the benefits and drawbacks of cervical radiculopathy surgeries and outcomes. For example, patient knowledge would be enhanced by knowing that the surgery is likely to ease pain in the arm and upper back region, but arm numbness may persist, and that surgery for C8 radiculopathy may be less likely to improve symptoms than surgery for other cervical radiculopathies.
Acknowledgements
We would like to thank Editage [http://www.editage.com] for editing and reviewing this manuscript for English language.
Author contributions
MO, NK, NT, AH, TO, YT, RO, MF, HI, SK, YM, YT, ST and YO contributed to the study conception and design. Material preparation, data collection and analysis were performed by MO and YO. The first draft of the manuscript was written by MO and NK, NT, AH, TO, YT, RO, MF, HI, SK, YM, YT, ST and YO commented on previous versions of the manuscript. MO, NK, NT, AH, TO, YT, RO, MF, HI, SK, YM, YT, ST and YO read and approved the final manuscript.
Data availability
The raw measurement data collected during the current study is available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Radhakrishnan, K., Litchy, W. J., O’Fallon, W. M. & Kurland, L. T. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain117, 325–335 (1994). 10.1093/brain/117.2.325 [DOI] [PubMed] [Google Scholar]
- 2.Alentado, V. J., Lubelski, D., Steinmetz, M. P., Benzel, E. C. & Mroz, T. E. Optimal duration of conservative management prior to surgery for cervical and lumbar radiculopathy: A literature review. Glob. Spine J.4, 279–286 (2014). 10.1055/s-0034-1387807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woods, B. I. & Hilibrand, A. S. Cervical radiculopathy: Epidemiology, etiology, diagnosis, and treatment. J. Spinal Disord. Tech.28, E251–E259 (2015). 10.1097/BSD.0000000000000284 [DOI] [PubMed] [Google Scholar]
- 4.Rhee, J. M., Yoon, T. & Riew, K. D. Cervical radiculopathy. J. Am. Acad. Orthop. Surg.15, 486–494 (2007). 10.5435/00124635-200708000-00005 [DOI] [PubMed] [Google Scholar]
- 5.Slipman, C. W., Plastaras, C. T., Palmitier, R. A., Huston, C. W. & Sterenfeld, E. B. Symptom provocation of fluoroscopically guided cervical nerve root stimulation. Are dynatomal maps identical to dermatomal maps?. Spine23, 2235–2242 (1998). 10.1097/00007632-199810150-00019 [DOI] [PubMed] [Google Scholar]
- 6.Yoss, R. E., Corbin, K. B., MacCarty, C. S. & Love, J. G. Significance of symptoms and signs in localization of involved root in cervical disk protrusion. Neurology7, 673–683 (1957). 10.1212/WNL.7.10.673 [DOI] [PubMed] [Google Scholar]
- 7.Furukawa, M., Kamata, M., Kuramoto, T., Takeuchi, Y. & Kawabata, S. Surgical results of microscopic cervical foraminotomy for cervical radiculopathy presenting drop finger and proposal of classification based on drop finger patterns. Spine Surg. Relat. Res.4, 23–30 (2020). 10.22603/ssrr.2019-0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takeuchi, M. et al. Transvertebral anterior key hole foraminotomy without fusion for the cervicothoracic junction. Acta Neurochir.154, 1797–1802 (2012). 10.1007/s00701-012-1484-0 [DOI] [PubMed] [Google Scholar]
- 9.Post, N. H., Cooper, P. R., Frempong-Boadu, A. K. & Costa, M. E. Unique features of herniated discs at the cervicothoracic junction: Clinical presentation, imaging, operative management, and outcome after anterior decompressive operation in 10 patients. Neurosurgery58, 497–501 (2006) (discussion 497–501; discussion 497). 10.1227/01.NEU.0000197118.86658.A6 [DOI] [PubMed] [Google Scholar]
- 10.Lee, J. G., Kim, H. S., Ju, C. I. & Kim, S. W. Clinical features of herniated disc at cervicothoracic junction level treated by anterior approach. Korean J. Spine13, 53–56 (2016). 10.14245/kjs.2016.13.2.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parker, S. L., Godil, S. S., Shau, D. N., Mendenhall, S. K. & McGirt, M. J. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: Clinical article. J. Neurosurg. Spine18, 154–160 (2013). 10.3171/2012.10.SPINE12312 [DOI] [PubMed] [Google Scholar]
- 12.Adamson, T. E. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy: Results of a new technique in 100 cases. J. Neurosurg.95(Supplement), 51–57 (2001). [DOI] [PubMed] [Google Scholar]
- 13.Broekema, A. E. H. et al. Noninferiority of posterior cervical foraminotomy vs anterior cervical discectomy with fusion for procedural success and reduction in arm pain among patients with cervical radiculopathy at 1 year: The FACET Randomized Clinical Trial. JAMA Neurol.80, 40–48 (2023). 10.1001/jamaneurol.2022.4208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sampath, P., Bendebba, M., Davis, J. D. & Ducker, T. Outcome in patients with cervical radiculopathy. Prospective, multicenter study with independent clinical review. Spine24, 591–597 (1999). 10.1097/00007632-199903150-00021 [DOI] [PubMed] [Google Scholar]
- 15.Engquist, M. et al. Surgery versus nonsurgical treatment of cervical radiculopathy: A prospective, randomized study comparing surgery plus physiotherapy with physiotherapy alone with a 2-year follow-up. Spine38, 1715–1722 (2013). 10.1097/BRS.0b013e31829ff095 [DOI] [PubMed] [Google Scholar]
- 16.Scholz, T. et al. Anterior cervical decompression and fusion or posterior foraminotomy for cervical radiculopathy: Results of a single-center series. J. Neurol. Surg. A Cent. Eur. Neurosurg.79, 211–217 (2018). 10.1055/s-0037-1607225 [DOI] [PubMed] [Google Scholar]
- 17.Korinth, M. C., Krüger, A., Oertel, M. F. & Gilsbach, J. M. Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease: Results in 292 patients with monoradiculopathy. Spine31, 1207–1214 (2006) (discussion 1215). 10.1097/01.brs.0000217604.02663.59 [DOI] [PubMed] [Google Scholar]
- 18.Makino, T. et al. Detailed features and prognostic factors of twenty-three patients with drop finger caused by cervical radiculopathy: A retrospective multicentre study. Int. Orthop.45, 2909–2916 (2021). 10.1007/s00264-021-05197-w [DOI] [PubMed] [Google Scholar]
- 19.Koda, M. et al. Drop finger caused by 8th cervical nerve root impairment: A clinical case series. Eur. Spine J.26, 1096–1100 (2017). 10.1007/s00586-016-4836-2 [DOI] [PubMed] [Google Scholar]
- 20.Jiang, S. D., Jiang, L. S. & Dai, L. Y. Cervical spondylotic amyotrophy. Eur. Spine J.20, 351–357 (2011). 10.1007/s00586-010-1544-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang, J. et al. Predisposing factors for poor outcome of surgery for cervical spondylotic amyotrophy: A multivariate analysis. Sci. Rep.6, 39512 (2016). 10.1038/srep39512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fujiwara, Y. et al. Surgical outcome of posterior decompression for cervical spondylosis with unilateral upper extremity amyotrophy. Spine31, E728–E732 (2006). 10.1097/01.brs.0000240207.00747.82 [DOI] [PubMed] [Google Scholar]
- 23.Prior, R., Van Helleputte, L., Benoy, V. & Van Den Bosch, L. Defective axonal transport: A common pathological mechanism in inherited and acquired peripheral neuropathies. Neurobiol. Dis.105, 300–320 (2017). 10.1016/j.nbd.2017.02.009 [DOI] [PubMed] [Google Scholar]
- 24.Tanaka, N., Fujimoto, Y., An, H. S., Ikuta, Y. & Yasuda, M. The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine25, 286–291 (2000). 10.1097/00007632-200002010-00005 [DOI] [PubMed] [Google Scholar]
- 25.Yamazaki, S., Kokubun, S., Ishii, Y. & Tanaka, Y. Courses of cervical disc herniation causing myelopathy or radiculopathy: An analysis based on computed tomographic discograms. Spine28, 1171–1175 (2003). 10.1097/01.BRS.0000067262.69584.0A [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw measurement data collected during the current study is available from the corresponding author on reasonable request.


