Abstract
Early brain development depends on adequate transport of thyroid hormones (THs) from the maternal circulation to the fetus. To reach the fetal brain, THs have to cross several physiological barriers, including the placenta, blood–brain-barrier and blood–cerebrospinal fluid-barrier. Transport across these barriers is facilitated by thyroid hormone transmembrane transporters (THTMTs). Some endocrine disrupting chemicals (EDCs) can interfere with the transport of THs by THTMTs. To screen chemicals for their capacity to disrupt THTMT facilitated TH transport, in vitro screening assays are required. In this study, we developed assays for two THTMTs, organic anion transporter polypeptide 1C1 (OATP1C1) and organic anion transporter 4 (OAT4), both known to play a role in the transport of THs across barriers. We used overexpressing cell models for both OATP1C1 and OAT4, which showed an increased uptake of radiolabeled T4 compared to control cell lines. Using these models, we screened various reference and environmental chemicals for their ability to inhibit T4 uptake by OATP1C1 and OAT4. Tetrabromobisphenol A (TBBPA) was identified as an OATP1C1 inhibitor, more potent than any of the reference chemicals tested. Additionally perfluorooctanesulfonic acid (PFOS), perfluoroctanic acid (PFOA), pentachlorophenol and quercetin were identified as OATP1C1 inhibitors in a similar range of potency to the reference chemicals tested. Bromosulfophthalein, TBBPA, PFOA and PFOS were identified as potent OAT4 inhibitors. These results demonstrate that EDCs commonly found in our environment can disrupt TH transport by THTMTs, and contribute to the identification of molecular mechanisms underlying TH system disruption chemicals.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00204-024-03787-2.
Keywords: Endocrine disrupting chemicals, Thyroid hormones, In vitro bioassays, Organic anion transporter polypeptide 1C1, Organic anion transporter 4
Introduction
Early neurodevelopmental processes are heavily dependent on adequate amount of thyroid hormones (THs) in the fetal brain. Severe hypothyroidism and hyperthyroidism during fetal brain development cause irreversible structural alterations to the fetal brain which lead to cognitive defects, motor function loss and behavioral problems. TH concentrations in the brain are kept within a small optimal range, as even modest changes in TH homeostasis can lead to loss of IQ (Korevaar et al. 2018). Most of the TH in the brain is derived from circulating thyroxine (T4), which gets locally converted by deiodinase enzymes into biologically active triiodothyronine (T3). The fetal thyroid gland does not produce a sufficient amount of TH during the initial stages of gestation, therefore the fetus is dependent on a maternal supply of TH (Chan and Kilby 2000). To reach the fetal brain, THs need to cross several physiological barriers: the placenta, blood–brain-barrier (BBB) and the blood–cerebrospinal fluid barrier (BCSFB). Transport across these barriers, as well as cellular influx and efflux, is mediated through TH transmembrane transporters (THTMTs). Several THTMTs from different protein families have been identified to date. Monocarboxylate 8 (MCT8) is the best studied THTMT and mutations of MCT8 are linked with a severe neurodevelopment disorder called the Allan–Herndon–Dudley syndrome (AHDS) (Schwartz et al. 2005). Other THTMTs than MCT8 are also considered to play a major role in TH transport, however the full range of important THTMTs is not yet known.
Organic anion transporter polypeptide 1C1 (OATP1C1) is another THTMT that plays an important role in the transport of T4 across the BBB and BCSFB. OATP1C1 has been characterized as a bidirectional high affinity T4 transporter independent of sodium and adenosine triphosphate (Pizzagalli et al. 2002). OATP1C1 is abundantly present in astrocytes, microglia cells, pyramidal and interneurons in the motor cortex and the apical and basolateral surface of the choroid plexus epithelial cells in humans (Roberts et al. 2008; Wang et al. 2023). OATP1C1 is also highly expressed in rodent cortical microvessels, but not in humans or macaques (Roberts et al. 2008; Wang et al. 2023). The importance of OATP1C1 as a THTMT is further elucidated in animal models. In zebrafish, knockout of OATP1C1 results in structural alteration of radial glial cells, shorter axon neurons, enlarged thyroid gland and changes in behavioral locomotor activity (Admati et al. 2020). In rodent models, knock out of OATP1C1 leads to decreased TH in the brain, without abnormal circulating THs, and hypothyroidism of the central nervous system, but lacks neurological abnormalities and behavioral problems typically observed in human hypothyroid patients (Mayerl et al. 2012). However, rodents lacking both OATP1C1 and MCT8 do exhibit severe neurodevelopmental adverse effects comparable to effects seen in human MCT8-deficiency patients. Interestingly, MCT8 knockout rodent models alone do not display these neurological effects, suggesting that OATP1C1 provides an alternative route of TH transport in this case. To date, only a single case study of OATP1C1 deficiency has been reported in humans, detailing a mutation in the gene encoding OATP1C1 that led to brain hypothyroidism due to reduced T4 transport capabilities of OATP1C1 (Strømme et al. 2018). This patient exhibited symptoms comparable to hypothyroidism, such as cognitive degeneration, loss of motor functions and intolerance to cold. However, serum TH concentrations, for both T3 and T4, were within a normal range. Overall, these data indicate that OATP1C1 is a major contributor to TH homeostasis in the brain by facilitating T4 transport across the BBB and BCSFB.
In the placenta, a substantial amount of T4 transport still cannot be attributed to known THTMTs, including MCT8 (Loubière et al. 2012). A good candidate for this unidentified T4 placental THTMT is organic anion transporter 4 (OAT4). OAT4 is highly expressed in the basal membrane of the syncytiotrophoblasts in the placenta (Cha et al. 2000) and is a known important transporter in the placenta, where it can transport sulfated steroid hormone precursors, perfluorocarboxylates and other organic anions (Cha et al. 2000; Kummu et al. 2015; Tomi et al. 2015). Recently, OAT4 has been identified as a novel efficient T4 transporter (Chen et al. 2023). As such there is increasing evidence that OAT4 is an important THTMT in the placenta.
Exposure to endocrine disrupting chemicals (EDCs) can potentially interfere with the transport of TH across the physiological barriers and cause altered TH concentrations in the fetal brain. Therefore, assays that can detect chemical interferences on TH transport are of vital importance. Particularly, there is a need for rapid in vitro screening assays that can identify potential EDCs acting upon THTMT mediated transport. Recently such screening in vitro assay has been described for MCT8 (Jayarama-Naidu et al. 2015; Wagenaars et al. 2023), but no assays exist for other THTMTs, such as OATP1C1 and OAT4. In this study we developed in vitro assays that can identify potential EDCs that interfere with OATP1C1 and OAT4 mediated TH transmembrane transport, by generating THTMT overexpressing cell models and exposing them to radioactive labelled T4. These assays were subsequently used in inhibition studies to screen a set of environmental contaminants.
Materials and methods
Materials
Indocyanine green (ICG) was purchased from Cayman Chemical (Uden, The Netherlands). perfluorooctanoic acid (PFOA) was obtained from Acros Organics (Landsmeer, the Netherlands). Diclofenac (DIC), bisphenol-F (BPF), perfluorooctanesulfonic acid (PFOS) and imidacloprid (IMI) were obtained from Fluka (Geel, Belgium). Bromosulfophthalein (BSP) was purchased from Alfa Aesar (Kandel, Germany). Bisphenol-S (BPS) and bisphenol-Z (BPZ) were obtained from TRC Canada (Toronto, Canada). Sulforhodamine 101 (SR101), lesinurad (LESI), quercetin (QCT), bisphenol-AF (BPAF), triclosan (TCS), 4-hydroxycinnamic acid (4HCA) were all obtained from Merck Life Science. All other chemicals were obtained from Sigma Aldrich (Zwijndrecht, the Netherlands). l-Tryptophan was dissolved in uptake buffer and BCH in 1 M NH4OH, while all other chemicals were dissolved in dimethylsulfoxide (DMSO). 125I-T4 was purchased from Perkin Elmer (Groningen, the Netherlands). Plastics used during the experiments were purchased from Starstedt (Etten-Leur, The Netherlands).
Generation of OAT4 construct
To generate Madin-Darby canine kidney (MDCK-1) cells that stably express OAT4, the gene insert of OAT4 from the pCMV6-OAT4-myc-DDK vector (Chen et al. 2023) was amplified using specific primers (forward: 5′-CACCATGGCGTTCTCGAAGCTCTT-3′; reverse: 5′-GAGCGAGGTACTTTCCACAGTGA-3′) and then subcloned into the pENTR™/D-TOPO® Vector using the pENTR™/D-TOPO™ Cloning Kit (Thermo Fisher). Subsequently OAT4 in pENTR™/D-TOPO® Vector was shuffled into the pLenti6/V5-DEST vector (Thermo Fisher) using Gateway™ LR Clonase™ II Enzyme mix (Thermo Fisher) according to the manufacture’s protocol.
Generation of stable MDCK-1 cells over-expressing OAT4 and OATP1C1
To generate an OAT4 lentivirus, 293FT cells were transfected with 3 µg pLenti6/V5-DEST-OAT4 or empty pLenti6/V5-DEST vector, the packaging vectors (3 µg pLP1and 3 µg pLP2) and 3 µg envelope vector pVSV-G at 70% confluency using X-tremeGENE 9 Transfection Reagent (Roche). The cell culture medium was refreshed 24 h after transfection and viral supernatants were collected at 48 h and 72 h post transfection and filtered through a 0.45 µM PES filter (GE Healthcare). To generate an OAT4 stable cell line, MDCK-1 cells were plated in 12-well plates with full growth medium and transduced with fresh viral supernatants in the absence of antibiotics in medium. After 2 days, MDCK-1 cells transduced with OAT4 (MDCK-OAT4) or empty vector (MDCK-DEST) were selected in full growth medium supplemented with 2 µg/mL blasticidin and further maintained under blasticidin selection. Chinese hamster ovary (CHO-K1) cells overexpressing OATP1C1 (CHO-K1 OATP1C1) were generated as previously described by Pizzagalli et al. (2002) and kindly provided by the University Hospital of Zürich (Dr Michele Visentin).
Cell culture and seeding
MDCK-OAT4 and MDCK-DEST cells were cultured in DMEM:F12 (l-glutamine, 15 mM HEPES) (Gibco) supplemented with (100 µg/mL penicillin + 100 µg/mL streptomycin), 10% fetal calf serum (Gibco) and 2 µg/mL blasticidin (Sigma). CHO-K1 OATP1C1 or WT cells were cultured in F12 nutrient mix (Gibco) supplemented with (100 µg/mL penicillin + 100 µg/mL streptomycin), 10% fetal calf serum (Gibco) and 100 µg/µL G418 (Sigma). All cell cultures were incubated at 37 °C with 5% CO2 saturation until 80% confluency. MDCK-OAT4 and MDCK-DEST cells were seeded in 96 wells plate at a density of 4 × 105 cells in 100 µL medium per well and incubated for 24 h before the start of the MDCK-OAT4 TH uptake assay. CHO-K1 OATP1C1 and WT cells were seeded in 96 wells plate at a density of 3 × 105 cells in 100 µL medium per well 72 h before the CHO-K1 OATP1C1 TH uptake assay. Medium from CHO-K1 OATP1C1 or WT assay plates was changed to serum-free F12 medium containing 5 mM sodium-butyrate 24 h before start of the CHO-K1 OATP1C1 TH uptake assay to increase transfected expression of SV-40 promotor plasmids.
THTMT TH uptake assay with 125I-T4 tracer
To start the THTMT assay with 125I-T4 tracer, medium was removed from assay plates and cells were washed with 200 µL phosphate buffered saline (PBS). Each well received 80 µL of uptake buffer (125 mM NaCl, 10 mM HEPES, 5 mM KCl, 1.3 mM CaCl2, 1.2 mM MgCl2, pH adjusted to 7.4 and freshly added 5.6 mM d-glucose). Subsequently 10 µL of a tenfold stock of test compound in uptake buffer (solvent concentration 1% v/v) was added to each well. The assay was started with the addition of 10 µL of T4 tracer solution, with a final concentration of 10 nM cold T4 and approximately 10.000 counts per minute (cpm) 125I-T4, solved in uptake buffer. Cells were exposed at 37 °C for 20 min (MDCK-OAT4) or 30 min (CHO-K1 OATP1C1), unless stated differently. After exposure, cells were immediately washed with ice-cold PBS supplemented with 0.1% bovine serum albumin (BSA). Subsequently, cells were lysed in 50 µL of 0.1 M NaOH under continuous shaking at room temperature. After 20 min, cell lysates were manually transferred into separate 5 mL polypropylene tubes. One tube was also prepared with 10 µL of the T4 tracer solution. Radioactivity was measured in a Wizard2 gamma counter (Perkin Elmer).
For the CHO-K1 OATP1C1 TH uptake assay total of 29 chemicals (Table 1) were selected for the EDC screening based on available literature data. Two negative control compounds (IBU, BCH) and five positive control chemicals (DIC, PRB, ICG, SR101, BSP, LESI) were included. The same chemicals were selected for the MDCK-OAT4 TH uptake assay, with the exception of BPF, VRP and TCS. Two positive control chemicals (PRB, LESI) were included, while no available literature have yet described negative control chemicals for OAT4 mediated TH uptake. The THTMT TH uptake assay was then performed as described earlier. A range finding study was performed at either 10 or 100 µM, depending on solubility of the chemical. A chemical that significantly inhibited T4 uptake by < 80% of the control was considered as a positive hit, i.e. inhibitors (One Way ANOVA). A concentration of 100 µM ICG was used as a reference chemical for OATP1C1 and 100 µM LESI for OAT4. At least three independent experiments were performed for each chemical. Each individual experiment contained three technical replicates of each control and concentration tested.
Table 1.
Test compounds and their inclusion criteria
| CAS | Compound | Abbreviation | Inclusion criteria | Reference | Supplier |
|---|---|---|---|---|---|
| 15687-27-1 | Ibuprofen | IBU | Negative control (OATP1C1) | Westholm et al. (2009) | Sigma-Aldrich |
| 20448-79-7 | 2-Amino-bicycloheptane-2-carboxylic acid | BCH | Negative control (OATP1C1) | Tohyama et al. (2004) | Sigma-Aldrich |
| 15307-79-6 | Diclofenac | DIC | OATP1C1 inhibitor | Westholm et al. (2009) | Fluka |
| 57-66-9 | Probenecid | PRB | OATP1C1/OAT4 inhibitor | Tohyama et al. (2004); Chen et al. (2023) | Sigma-Aldrich |
| 3599-32-4 | Indocyanine green | ICG | OATP1C1 inhibitor | Westholm et al. (2009) | Cayman Chemical |
| 60311-02-6 | Sulforhodamine 101 | SR101 | OATP1C1 inhibitor | Bakos et al. (2020) | Merck Life Science |
| 71-67-0 | Bromosulfophthalein | BSP | OATP1C1 substrate | Sugiyama et al. (2003) | Alfa Aesar |
| 878672-00-5 | Lesinurad | LESI | OAT4 inhibitor | Chen et al. (2023) | Merck Life Science |
| 51-52-5 | Propylthiouracil | PTU | TPO inhibitor | Friedman et al. (2016) | Sigma-Aldrich |
| 117-39-5 | Quercetin | QCT | TPO inhibitor | Friedman et al. (2016) | Merck Life Science |
| 1763-23-1 | Perfluorooctanesulfonic acid | PFOS | NIS inhibitor/TTR binding | Buckalew et al. (2020); Weiss et al. (2015) | Fluka |
| 73-22-3 | l-Tryptophan | TRP | LAT1/2 inhibitor | Chen et al. (2022a, b) | Sigma-Aldrich |
| 13292-46-1 | Rifampicin | RIF | OATP inhibitor | Chen et al. (2022a, b) | Sigma-Aldrich |
| 152-11-4 | Verapamil | VRP | OATP inhibitor | Chen et al. (2022a, b) | Sigma-Aldrich |
| 335-67-1 | Perfluorooctanoic acid | PFOA | TTR binding | Weiss et al. (2009) | Sigma-Aldrich |
| 87-86-5 | Pentachlorophenol | PCP | TTR binding | Hamers et al. (2006) | Sigma-Aldrich |
| 79-94-7 | Tetrabromobisphenol-A | TBBPA | TTR binding | Hamers et al. (2006) | Sigma-Aldrich |
| 115-09-3 | Methyl mercury | MeHg | MCT8 inhibitor | Wagenaars et al. (2023) | Sigma-Aldrich |
| 33889-69-9 | Silychristin | SY | MCT8-inhibitor | Johannes et al. (2016) | Merck Life Science |
| 80-05-7 | Bisphenol-A | BPA | MCT8-inhibitor | Wagenaars et al. (2023) | Sigma-Aldrich |
| 843-55-0 | Bisphenol-Z | BPZ | MCT8-inhibitor | Wagenaars et al. (2023) | TRC Canada |
| 1478-61-1 | Bisphenol-AF | BPAF | MCT8-inhibitor | Wagenaars et al. (2023) | Merck Life Science |
| 80-09-1 | Bisphenol-S | BPS | BPA-like | TRC Canada | |
| 620-92-8 | Bisphenol-F | BPF | BPA-like | Fluka | |
| 3380-34-5 | Triclosan | TCS | decreased brain T4 in pups | Gilbert et al. (2021) | Merck Life Science |
| 138261-41-3 | Imidacloprid | IMI | decreased plasma T4 in rats | Ibrahim et al. (2015) | Fluka |
| 4999-79-5 | β-Estradiol-3-sulfate | β-E3S | OAT4 substrate | Skwara et al. (2017) | Sigma-Aldrich |
| 69-93-2 | Uric acid | UA | OAT4 substrate | Skwara et al. (2017) | Sigma-Aldrich |
| 7400-08-0 | 4-Hydroxycinnamic acid | 4HCA | OAT4 substrate | Wong et al. (2011) | Merck Life Science |
Cell viability assay
Cell viability was assessed through the quantitation of ATP present in cells using the commercially available CellTiter-Glo® luminescent cell viability assay and performed according to the manufacturer’s instruction (Promega, Leiden, the Netherlands). Briefly, cells were seeded as described earlier in opaque-walled clear-bottom 96 well plates. On the day of the experiment, each well was washed with 200 µL phosphate buffered saline (PBS) and exposed to 80 µL of uptake buffer, 10 µL of a tenfold stock of test compound solved in uptake buffer or control and 10 µL of T4 (final concentration 10 nM). 0.1% DMSO was used as a solvent control, while 10% DMSO was used as a positive control. After exposure for the indicated times similar to THTMT TH uptake assay, cells were immediately washed with ice-cold PBS + 0.1%BSA and exposed to 100 µL of the CellTiter-Glo® Reagent. Plates were then shaken on an orbital shaker for 2 min and left to incubate at room temperature for 10 min. Luminescence was measured on a BioTek Cytation 5 microplate reader. A similar range finding study was performed as for the THTMT TH uptake assay, where chemicals that showed a decrease in cell viability < 90% of the control were subsequently tested in eight concentrations to obtain a full concentration response curve. Each individual experiment was repeated at least twice and contained three technical replicates of each control and concentration tested.
Data analysis
Raw values were normalized to the total amount of radioactivity in the T4 tracer solution. These values were expressed as a percentage of total radioactivity added (or uptake percentage) and used for all further data analysis. Statistically significant differences between the T4 uptake of transfected and wild type cells, in the presence or absence of inhibitor, were determined by two-way ANOVA (α = 5%, two-sided). Concentration–response analysis for the T4 uptake in both cell models was performed using a best-fit-approach as previously described (Scholze et al. 2001; Wagenaars et al. 2023). In brief, uptake values were normalized to the median response of the vehicle and positive controls for each plate. A control renormalization step was performed on a plate-to-plate basis as previously described (Krebs et al. 2018; Wagenaars et al. 2023). Chemical-specific potencies were derived from the regression analysis on the control-normalized effect responses and expressed as benchmark concentration (BMC), with the benchmark response level (BMR) determined as 80% of the vehicle control (i.e. 20% inhibition). Statistical analysis were performed using GraphPad Prism version 8 for Windows (GraphPad Software, San Diego, California USA) and SAS 9.3 (SAS Institute, Cary NC).
Results
TH uptake in CHO-K1 OATP1C1 and MDCK-OAT4
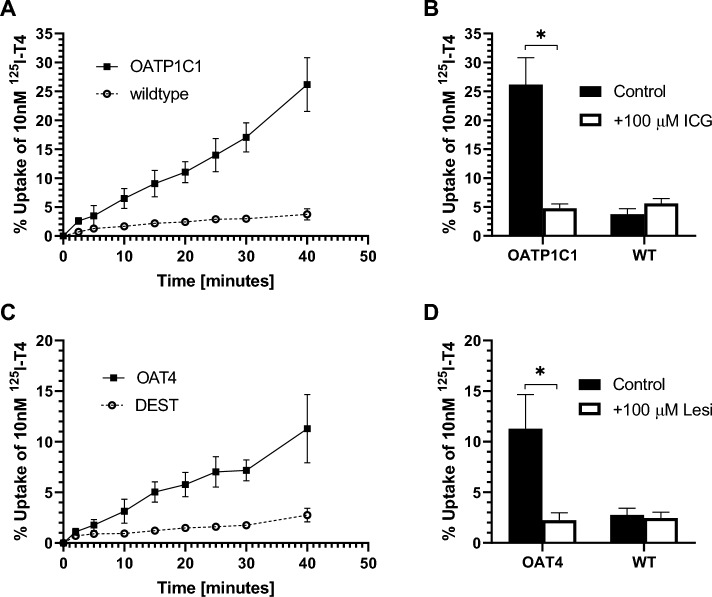
To characterize the in vitro kinetics, the TH uptake in CHO-K1 OATP1C1 and MDCK-OAT4 was measured at different incubation times. In CHO-K1 OATP1C1 cells, T4 uptake increased over time up to ~ 25% T4 added at t = 40 min (Fig. 1A), compared to < 4% in CHO-K1 WT cells. The ~ sixfold increase in T4 uptake in CHO-K1 OATP1C1 cells compared to CHO-K1 wildtype cells at t = 40 min decreased back to control when co-exposed to a known inhibitor of OATP1C1, i.e. 100 µM ICG (Fig. 1B). To keep in the linear T4 uptake range, all further experiments were performed with 30 min incubation times, where T4 uptake in CHO-K1 OATP1C1 (~ 17%) was 5.5-fold higher than CHO-K1 wildtype cells (~ 3%). T4 uptake in MDCK-OAT4 cells increased up until t = 25 min, plateaued at t = 30 min at ~ 7% T4 uptake (Fig. 1C). T4 uptake in MDCK-DEST cells increased up until t = 40 min at ~ 4% T4 uptake. At t = 40 min, MDCK-OAT4 cells had a fivefold higher T4 uptake compared to MDCK-DEST cells. Similar as for the CHO-K1 OATP1C1 cells, T4 uptake by the MDCK-OAT4 cells decreased back to control concentrations when cells were co-exposed to a known OAT4 inhibitor, i.e. 100 µM LESI (Fig. 1D). For all experiments hereafter an incubation time of 20 min was used, where T4 uptake in MDCK-OAT4 (~ 5.7%) was ~ fourfold higher compared to MDKC-DEST cells (~ 1.4%).
Fig. 1.
Kinetics of the CHO-K1 OATP1C1 and MDCK-OAT4 T4 uptake assay. A The uptake of 125I-T4 in time, expressed as a percentage of total T4, in CHO-K1 OATP1C1 or CHO-K1 wildtype cells. B Comparison between the percentage of 125I-T4 uptake in CHO-K1 OATP1C1 and CHO-K1 WT cells after 40 min incubation, in the absence and presence of 100 µM ICG. C Uptake of 125I-T4 uptake in time expressed as a percentage of total T4 in MDCK-OAT4 and MDCK-DEST cells over time. D Comparison of the percentage of 125I-T4 uptake in MDCK-OAT4 and MDCK-DEST cells after 40 min incubation, with and without 100 µM LESI. Data is shown as the mean ± SD, N = 3. Comparisons with a p values below 0.05 are indicated by a star
EDC screening with THTMT TH uptake assays
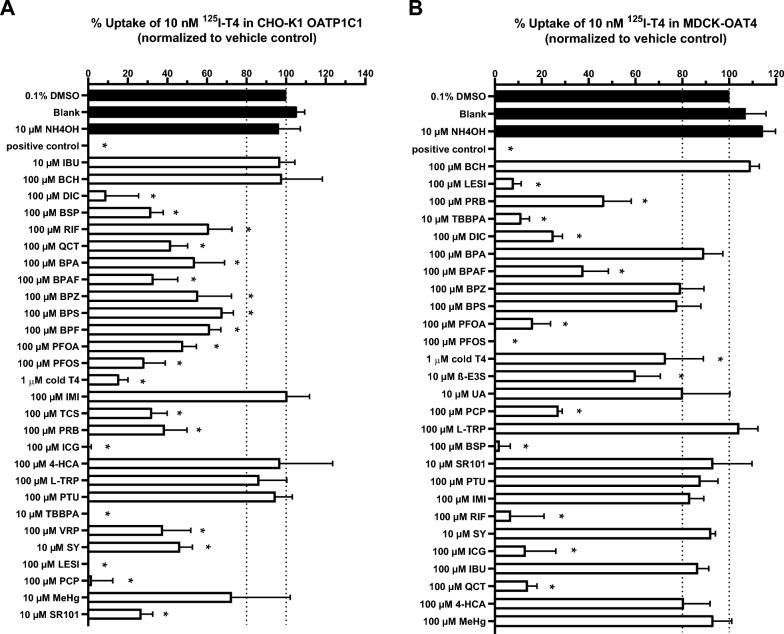
To screen for chemicals that inhibit the THTMTs, all selected chemicals were initially tested at a single high concentration of 100 or 10 µM, depending on their solubility (Fig. 2). There was no difference between T4 uptake exposed to solvent controls 0.1% DMSO or 10 µM NH4OH and the uptake buffer (blank). In the CHO-K1 OATP1C1 TH uptake assay, both negative control compounds, IBU and BCH, did not decrease T4 uptake (Fig. 2A). Neither IMI, 4HCA, L-TRP, PTU nor MeHg decreased OATP1C1 mediated T4 uptake significantly below 80%, while all other compounds did. Highest inhibition was found for TBBPA followed by (in decreasing order of potency) ICG, LESI, PCP, PFOS, BSP, TCS, PRB, BPAF, DIC, QCT, SR101, PFOA, BPA, BPZ, VRP, SY, RIF, BPF and BPS. Addition of an excess of unlabeled 1 µM T4 also quenched the uptake of 125I-T4 in CHO-K1 OATP1C1 cells, indicating a saturable uptake (Fig. 2A). In the MDCK-OAT4 TH uptake assay, no decrease in T4 uptake below 80% was observed for BCH, BPA, BPZ, BPS, UA, L-TRP, SR101, PTU, IMI, SY, IBU, 4HCA and MeHg (Fig. 2B), while all other chemicals did. Highest inhibition was found for PFOS, followed by (in decreasing order of potency) BSP, LESI, RIF, TBBPA, ICG, QCT, PFOA, DIC, PCP, BPAF, PRB, TCS, VRP, β-E3S and BPF.
Fig. 2.
Percentage of 125I-T4 uptake compared to the vehicle control 0.1% DMSO in A CHO-K1 OATP1C1 and B MDCK-OAT4 cells in the presence of selected chemicals. CHO-K1 OATP1C1 and MDCK-OAT4 cells were exposed to 10 nM T4 and 10–100 µM of selected chemicals for 30 min and 20 min respectively. Chemicals that decreased T4 uptake below 80% (i.e. 20% inhibition) after exposure were considered positive hits. 0.1% DMSO was used as vehicle control, 100 µM ICG was used as a positive control for OATP1C1 and 100 µM LESI for OAT4 (in black). Results are shown as mean ± SD, N = 3. Comparisons with a p values below 0.05 are indicated by a star
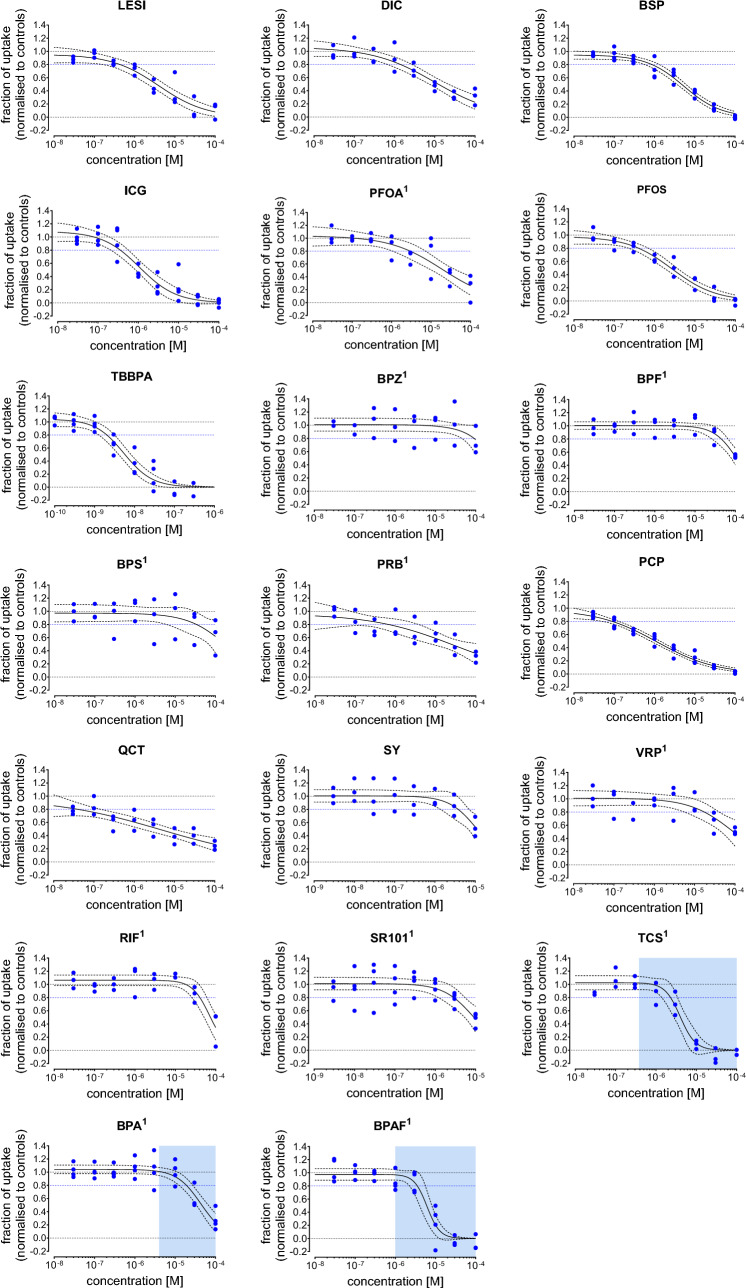
The 20 inhibitors from the CHO-K1 OATP1C1 range finding study were subsequently measured in eight concentrations to obtain full concentration–response curves (Fig. 3). TCS, BPA and BPAF all displayed sigmoidal concentration response patterns, but these responses were confounded by cytotoxic effects (Supplementary Figure S1). Cytotoxic effects were not observed for any other chemicals at the highest concentration tested (data not shown). LESI, PFOS, ICG, TBBPA, BSP and PCP displayed full sigmoidal concentration response patterns. Additionally, DIC and PFOA seem to display a sigmoidal concentration response pattern, but a full concentration response curve could not be established with these chemicals. BPZ, BPS, BPF, SY, VRP and RIF only inhibited T4 uptake at concentrations near the maximum concentration tested in the THTMT TH uptake assay and a full concentration response pattern could not be established. The concentrations response patterns for QCT and PRB appear to be more linear than sigmoidal, but no full concentration response pattern could be established. For each chemical, the BMC20 (i.e. 20% reduction in T4 uptake) was derived, which is provided together with the number of independent experiments, the lowest concentration with cytotoxic effect (IC10) and the best fit regression model in Table 2. TBBPA was the most potent OATP1C1 inhibitor (BMC20 = 0.0020 µM), followed by (in decreasing order of potency) QCT, PCP, ICG, PFOS, LESI, PRB, BSP, DIC, SR101, PFOA, SY, VRP, BPS, RIF and BPF. The concentration–response data observed for BPZ was considered as not sufficient for the derivation of a reliable BMC20 estimation. For three compounds (TCS, BPAF, and BPA) the BMC20s were in the range of cytotoxic concentrations, suggesting that the decrease in T4 uptake is not due to OATP1C1 inhibition, but rather due to reduced cell functioning.
Fig. 3.
Concentration–response curves for test chemicals that showed inhibition towards OATP1C1 mediated uptake of T4 (10 nM) in the CHO-K1 OATP1C1 TH uptake assay. The fraction of 125I-T4 uptake is normalized to the positive control, 100 µM ICG, (lower limit = 0.0) and to the DMSO control (upper limit = 1.0). Blue dots indicate the plate medians from three independent experiments, all control and chemical concentrations were tested in triplicates per plate. The black line indicates the best-fit concentrations response curve, the dotted line the corresponding 95% confidence interval. The blue dotted line indicates the BMC20, the concentration that inhibits the 125I-T4 uptake by 20%. The concentration range at which cytotoxicity was observed is indicated with a blue box. Compounds for which a control renormalization step was performed are marked with an1 (color figure online)
Table 2.
Inhibition of T4 uptake and cytotoxicity of individual compounds in the CHO-K1 OATP1C1 TH uptake assay
|
Substance (by order of BMC20) |
Concentration response function | T4 uptake inhibition | Cytotoxicity | |||||
|---|---|---|---|---|---|---|---|---|
| Nstudy | RM | BMC20 (M), [CI] | IC10 (M) | |||||
| Tetrabromobisphenol A | 4 | Logit | − 23.30 | − 2.82 | 0* | 1.042 | 2.03E−09 [1.28E−09; 3.22E−09] | > 3.00E−07 |
| Quercetin | 3 | Logit | − 3.90 | − 0.73 | 0* | 0.974 | 3.94E−08 [4.41E−09; 3.51E−07] | > 1.00E−04 |
| Pentachlorophenol | 4 | Logit | − 8.05 | − 1.35 | 0* | 0.977 | 8.81E−08 [5.80E−08; 1.34E−07] | > 1.85E−05 |
| Indocyanine green | 4 | Logit | − 13.10 | − 2.19 | 0* | 1.084 | 3.60E−07 [2.17E−07; 5.97E−07] | > 1.00E−04 |
| Perfluorooctanesulfonic acid | 3 | Logit | − 10.23 | − 1.84 | 0* | 0.976 | 4.03E−07 [2.32E−07; 7.00E−07] | > 1.00E−04 |
| Lesinurad | 3 | Logit | − 9.22 | − 1.71 | 0* | 0.954 | 4.34E−07 [1.97E−07; 9.56E−07] | > 1.00E−04 |
| Probenecid | 3 | Logit | − 4.42 | − 0.97 | 0* | 0.962 | 6.66E−07 [1.24E−07; 3.57E−06] | > 1.00E−04 |
| Bromosulfophthalein | 4 | Logit | − 11.37 | − 2.16 | 0* | 0.946 | 8.72E−07 [5.70E−07; 1.33E−06] | > 1.00E−04 |
| Diclofenac | 3 | Logit | − 6.56 | − 1.31 | 0* | 1.062 | 1.40E−06 [6.84E−07; 2.87E−06] | > 1.00E−04 |
| Triclosan | 3 | Logit | − 28.80 | − 5.33 | 0* | 1.025 | 2.30E−06 [1.38E−06; 3.83E−06] | 3.78E−07 |
| Sulforhodamine 101 | 4 | Logit | − 13.60 | − 2.69 | 0* | 1.011 | 2.86E−06 [1.29E−06; 6.34E−06] | > 1.00E−05 |
| Perfluorooctanoic acid | 3 | Logit | − 7.08 | − 1.50 | 0* | 1.036 | 2.94E−06 [1.04E−06; 8.36E−06] | > 1.00E−04 |
| Bisphenol AF | 4 | Logit | − 32.69 | − 6.27 | 0* | 0.975 | 3.52E−06 [2.03E−06; 6.11E−06] | 9.09E−07 |
| Silychristin | 3 | Logit | − 14.50 | − 2.92 | 0* | 1.005 | 3.78E−06 [1.54E−06; 9.27E−06] | > 1.00E−05 |
| Verapamil | 3 | Logit | − 7.60 | − 1.88 | 0* | 1.010 | 1.74E−05 [6.34E−06; 4.79E−05] | > 1.00E−04 |
| Bisphenol A | 4 | Logit | − 14.60 | − 3.35 | 0* | 1.042 | 1.90E−05 [1.28E−05; 2.83E−05] | 4.34E−06 |
| Bisphenol S | 3 | Logit | − 7.72 | − 2.07 | 0* | 0.972 | 3.38E−05 [7.87E−06; 1.45E−04] | > 1.00E−04 |
| Rifampicin | 3 | Logit | − 19.48 | − 4.69 | 0* | 1.063 | 4.06E−05 [2.58E−05; 6.38E−05] | > 1.00E−04 |
| Bisphenol F | 3 | Logit | − 14.10 | − 3.56 | 0* | 1.004 | 4.49E−05 [2.80E−05; 7.20E−05] | > 1.00E−04 |
| Bisphenol Z | 4 | Linear | – | − 2293 | – | 1.009 | n.d. [n.d.; n.d.] | > 1.00E−04 |
BMC20: concentration that inhibits the T3 uptake by 20%; IC10: concentration that inhibits cell viability by 10% in the CellTiter-Glo® luminescent cell viability assay. Values in brackets denote the upper and lower limits of the approximate 95% confidence interval (CI); the column “RM” indicates the mathematical regression function as defined at Scholze et al. (2001): estimated model parameters, given for concentrations expressed in M (rounded values), with * highlighting parameters that were not estimated but constrained to a fixed value. Nstudy = number of independent experiments
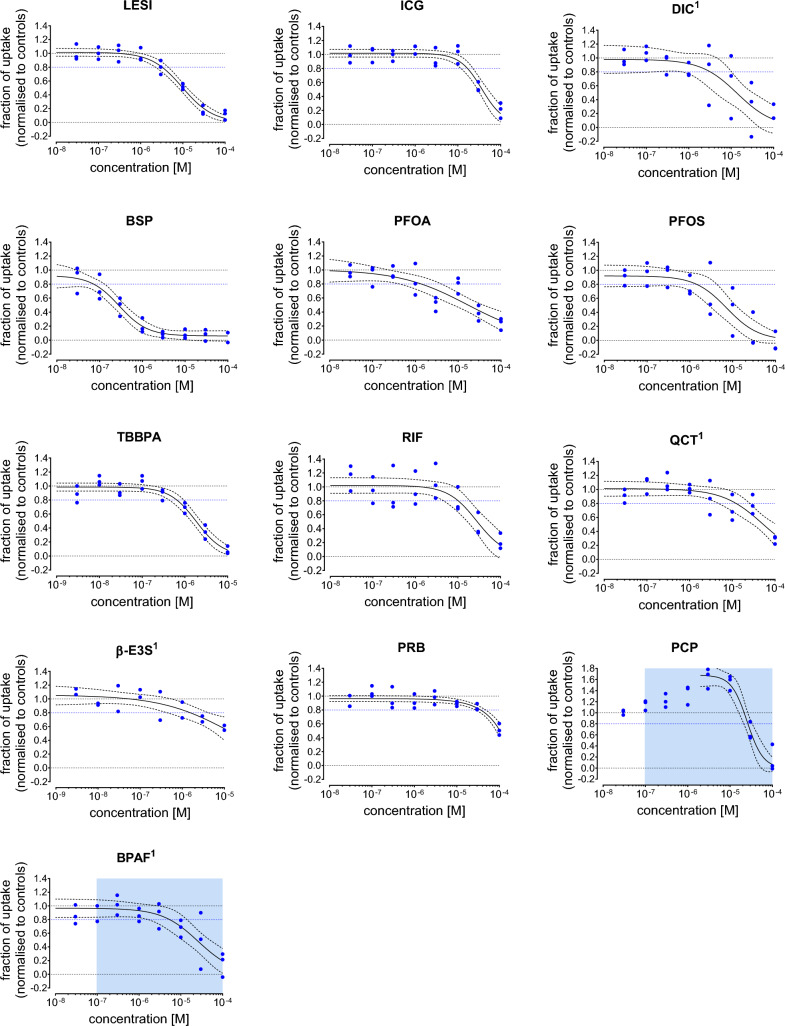
Thirteen inhibitors from the MDCK-OAT4 TH uptake range finding screening were also measured in eight concentrations to obtain full concentration response curves (Fig. 4). With the exception of PCP and BPAF (Supplementary Figure S2), none of the other chemicals were cytotoxic at the highest concentrations tested (data now shown). The BMC20, the number of independent experiments, the lowest concentration with cytotoxic effect and the best fit regression model used are summarized in Table 3. LESI, ICG, DIC, BSP, PFOS and TBBPA all displayed sigmoidal concentration response patterns. For PFOA, RIF, QCT and β-E3S a full concentration response pattern could not be established. BSP was the most potent OAT4 inhibitor (BMC20 = 0.072 µM), followed by TBBPA, PFOA, PFOS, β-E3S, DIC, LESI, RIF, QCT, ICG and PRB. The BMC20 values for BPAF and PCP were estimated at concentrations at which cytotoxic effects occurred, suggesting that the observed decrease in T4 uptake is due to reduced cell functioning, and not due to OAT4 inhibition specifically.
Fig. 4.
Concentration–response curves for test chemicals that showed OAT4 mediated uptake of T4 (10 nM) inhibition in the MDCK-OAT4 TH uptake assay. The fraction of 125I-T4 uptake is normalized to the positive control, 100 µM LESI (lower limit = 0.0) and to the DMSO control (upper limit = 1.0). Blue dots indicate the plate medians from three independent experiments, all control and chemical concentrations were tested in triplicates per plate. The black line indicates the best-fit concentrations response curve, the dotted line the corresponding 95% confidence interval. The blue dotted line indicates the BMC20, the concentration that inhibits the 125I-T4 uptake by 20%. The concentration range at which cytotoxicity was observed is indicated with a blue box. Compounds for which a control renormalization step was performed are marked with an1 (color figure online)
Table 3.
Inhibition of uptake and cytotoxicity of individual compounds in the MDCK-OAT4 TH uptake assay
|
Substance (by order of BMC20) |
Concentration response function | T4 uptake inhibition | Cytotoxicity | |||||
|---|---|---|---|---|---|---|---|---|
| Nstudy | RM | BMC20 (M), [CI] | IC10 (M) | |||||
| Bromosulfophthalein | 3 | Logit | − 19.76 | − 3.02 | 0.059 | 0.922 | 7.25E−08 [3.85E−08; 1.36E−07] | > 1.00E−04 |
| Tetrabromobisphenol A | 3 | Logit | − 18.37 | − 3.21 | 0 | 0.986 | 6.49E−07 [4.32E−07; 9.74E−07] | > 1.00E−05 |
| Perfluorooctanoic acid | 3 | Logit | − 5.98 | − 1.25 | 0 | 1.006 | 1.38E−06 [4.27E−07; 4.44E−06] | > 1.00E−04 |
| Perfluorooctanesulfonic acid | 3 | Logit | − 13.81 | − 2.69 | 0 | 0.920 | 1.44E−06 [4.08E−07; 5.05E−06] | > 1.00E−04 |
| ß-Estrone-3-sulfate | 2 | Logit | − 5.89 | − 1.21 | 0 | 1.056 | 1.55E−06 [5.32E−07; 4.51E−06] | > 1.00E−05 |
| Diclofenac | 3 | Logit | − 11.41 | − 2.35 | 0 | 0.980 | 3.22E−06 [6.39E−07; 1.62E−05] | > 1.00E−04 |
| Lesinurad | 3 | Logit | − 13.72 | − 2.74 | 0 | 1.016 | 3.23E−06 [2.26E−06; 4.61E−06] | > 1.00E−04 |
| Bisphenol AF | 3 | Logit | − 10.62 | − 2.32 | 0 | 0.966 | 5.39E−06 [1.65E−06; 1.76E−05] | 9.69E−08 |
| Rifampicin | 3 | Logit | − 13.49 | − 2.96 | 0 | 1.021 | 1.02E−05 [4.85E−06; 2.14E−05] | > 1.00E−04 |
| Quercetin | 3 | Logit | − 9.12 | − 2.13 | 0 | 1.010 | 1.23E−05 [4.77E−06; 3.16E−05] | > 1.00E−04 |
| Indocyanine green | 3 | Logit | − 17.36 | − 3.91 | 0 | 1.017 | 1.68E−05 [1.20E−05; 2.33E−05] | > 1.00E−05 |
| Pentachlorophenol | 3 | Logit | − 24.58 | − 5.35 | 0 | 1.678 | 2.65E−05 [2.17E−05; 3.23E−05] | 1.14E−06 |
| Probenecid | 3 | Linear | – | − 4474 | 0 | 0.963 | 3.65E−05 [2.69E−05; 4.61E−05] | > 1.00E−04 |
BMC20: concentration that inhibits the T3 uptake by 20%; IC10: concentration that inhibits cell viability by 10% in the CellTiter-Glo® luminescent cell viability assay. Values in brackets denote the upper and lower limits of the approximate 95% confidence interval (CI); the column “RM” indicates the mathematical regression function as defined at Scholze et al. (2001): estimated model parameters, given for concentrations expressed in M (rounded values), with * highlighting parameters that were not estimated but set to a fixed value. Nstudy = number of independent experiments
Discussion
In this study we developed in vitro TH uptake assays to screen for potential EDCs acting upon OATP1C1 and OAT4 facilitated transmembrane transport of TH. We validated both TH uptake assays by using negative controls and known inhibitors as positive control. Moreover we showed the inhibitory effects of a number of environmental contaminants. As expected, in both OATP1C1 and OAT4 overexpressing cell lines the uptake of 125I-T4 was higher than in the control cell lines. Several studies have tested the effect of chemicals on T4 transmembrane transport by rat, murine or human OATP1C1 in HEK293 transfected cells lines. Westholm et al. (2009) showed that several nonsteroidal anti-inflammatory drugs (NSAIDS), such as DIC, as well as ICG can inhibit T4 (1 nM) transmembrane transport by oatp1c1 with an IC50 of 4 µM and 0.1 µM, respectively. Tohyama et al. (2004) demonstrated that PRB is a weak inhibitor of oatp1c1 T4 facilitated transmembrane transport (Ki value = 293 µM). Bakos et al. (2020) found that the fluorescent dye SR101 was a substrate of OATP1C1 that could compete with T4 uptake. In our TH uptake assay, these compounds also interfered with OATP1C1-facilitated T4 uptake at similar potencies. Moreover, BCH and IBU were previously shown not to interact with OATP1C1, which was confirmed in our in vitro TH uptake assay. For OAT4, only PRB and LESI have been reported as OAT4 inhibitors interfering with T4 transmembrane transport (Chen et al. 2023). Both compounds also inhibited T4 uptake by OAT4 in our TH uptake assay. The high agreement between previously published data and our screening results confirms that our in vitro TH uptake assays can reliable detect chemicals known to be inhibitors of OATP1C1 or OAT4.
In addition to already known inhibitors of OATP1C1 and OAT4, we also tested various environmentally relevant industrial chemicals and pharmaceuticals. We demonstrated that TBBPA is a potent OATP1C1 inhibitor, while other bisphenols only exerted weak to no inhibition. TBBPA is considered as a widely discussed chemical with regards to TH-dependent endocrine disruption and neurotoxic effects: in rats, TBBPA is known to decrease serum (free) T4, while it simultaneously causes thinning of the brain cortex, but it exerts no effect on serum T3 or TSH (Cope et al. 2015). Several other studies have shown a similar effect of TBBPA on circulating T4 in both rat and mice (Sinkó et al. 2022; Van der Ven et al. 2008). Moreover, auditory deficits have been reported after TBBPA exposure in both rats and mice (Lilienthal et al. 2008; Park et al. 2016). A recent study has found that TBBPA exposure causes decreased TH concentrations and thyroid histological changes, but has no overt effect on brain development and neurological behavior in mice (Song et al. 2024). The risk of TBBPA in humans is still heavily debated, some studies suggests that, due its rapid metabolism and excretion in humans, TBBPA should not be considered a neurotoxicant for humans (Kacew and Hayes 2020). However, there are still concerns about the neurotoxic effect of TBBPA in embryos and continuously exposed humans (Dong et al. 2021; Feiteiro et al. 2021; Zhou et al. 2020). Limited data are available on the effect of TBBPA on TH concentrations and neurological effects in humans. A cross-sectional study in Belgium found no significant effect of TBBPA exposure on circulating TH concentrations or any neurobehavioral characteristics (Kiciński et al. 2012). TBBPA is a known potent transthyretin (TTR) binder, competing with T4 for binding to TTR (Hamers et al. 2006). Our data indicate a strong correlation between the potencies of chemicals displaying inhibited OATP1C1-mediated T4 transport and TTR binding. PCP is similarly a potent TTR binder (Hamers et al. 2006), which in our TH uptake assay significantly reduced T4 uptake by OATP1C1. In rat animal models, exposure to PCP significantly reduced the transport of T4 into the brain and CSF (Van Raaij et al. 1994), in ram lambs exposure to PCP was associated with a lower serum T4 concentration (Beard et al. 1999). In a Dutch cohort, PCP in umbilical cord blood has been associated with reduced serum TH concentrations as well as reduced neuropsychological functioning, including cognitive, motor function and behavioral performance, in 5–6 year old children (Roze et al. 2009). Similarly in a Canadian cohort, high serum and umbilical cord concentrations of PCP were associated with lower free T4 concentrations in newborns (Sandau et al. 2002). In our study, other known TTR inhibitors, such as PFOS and PFOA also reduced the uptake of T4 in both the OATP1C1 and OAT4 overexpressing cell lines. PFOS and PFOA are known substrates of OAT4 and are transported through OAT4 in placenta perfusion models (Kummu et al. 2015). Moreover, PFOS and PFOA can cross the BCSFB and accumulate in the CSF (Hu et al. 2023; Wang et al. 2018). In addition to PFOS and PFOA, many other perfluorinated chemicals are transported by OAT4, including PFDA, PFNA, PFHpA and PFHxS (Louisse et al. 2023).
The miniaturization of the THTMT TH uptake assays in 96 wells format allows for quick screening of multiple chemicals. Recently similar studies were published on MCT8 inhibition using a non-radioactive method (Johannes et al. 2016; Wagenaars et al. 2023). This method is based on the Sandell-Kolthoff methodology, which uses a colorimetric redox reaction of cerium and arsenate (i.e. the Sandell-Kolthoff reaction (Sandell and Kolthoff 1937)) to indirectly quantify uptake of THs by measuring the iodide in cells (Jayarama-Naidu et al. 2015; Renko et al. 2012). For HTS purposes, a non-radioactive method would be more preferable. However the non-radioactive method was not feasible with the current CHO-K1 OATP1C1 and MDCK-OAT4 TH uptake assay, most probably due to the sensitivity limitations of the non-radioactive method. Although the radioactive TH uptake assays is more sensitive, it also requires expensive radioactive isotopes that can only be used in a specialized lab and produces radioactive waste. Nonetheless, both methods are be suitable for the screening of possible THTMT inhibitors.
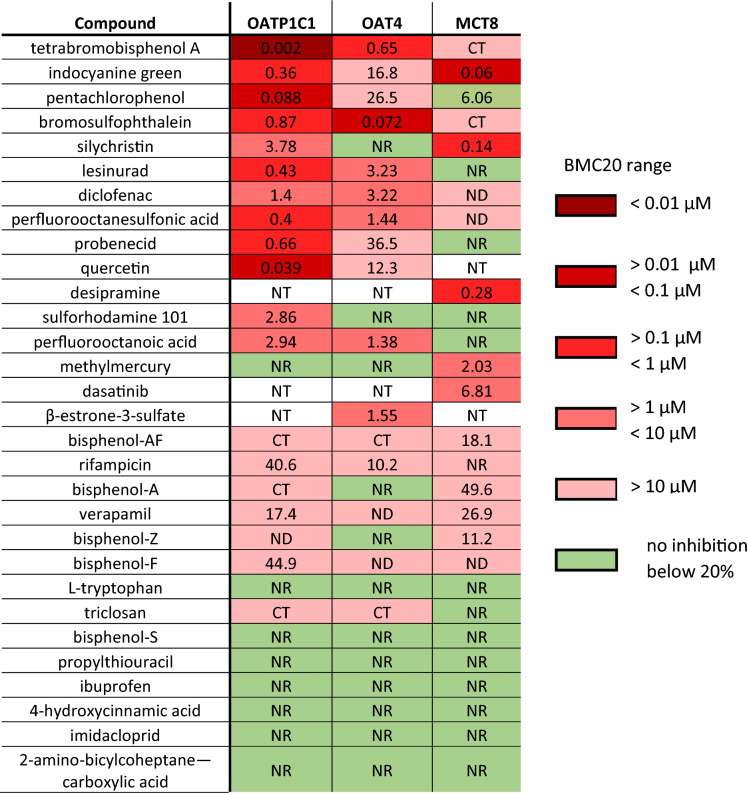
A summary overview of the potencies of all tested chemicals in each THTMT TH uptake assay, as well as data from our previous study on MCT8 inhibition (Wagenaars et al. 2023) is presented in Fig. 5. A large overlap in inhibitory effect on TH uptake exists between the tested chemicals on each THTMT, although the potencies of each inhibitor can differ greatly between THTMTs. For example, TBBPA, PCP and QCT have very high inhibitory potencies in the CHO-K1 OATP1C1 TH uptake assay but > tenfold lower values in the MDCK-OAT4 and MDCK-MCT8 TH uptake assay. Similarly, SY and ICG appear to be very potent in the MDCK-MCT8 TH uptake assay, but with a much lower potency in the CHO-K1 OATP1C1 and MDCK-OAT4 TH uptake assay. BSP is a very potent OAT4 inhibitor, with a lower potency in the CHO-K1 OATP1C1 and MDCK-MCT8 TH uptake assay. These data show that THTMT TH uptake assays are suitable to identify THTMT specific inhibitors and might be vital in future studies to elucidate the contribution of THTMTs on the total TH uptake. Moreover, a more extensive screening of chemicals in a battery of THTMT overexpressing cell lines assays can help to identify chemicals which inhibit multiple THTMTs and are more likely to cause adversity in vivo. A battery of in vitro THTMTs TH uptake assays should therefore include the most important THTMTs identified so far as well as any newly identified important THTMTs.
Fig. 5.
Overview of the potency of THTMT inhibitors on different THTMT TH uptake assays. Data for the MCT8 column was taken from Wagenaars et al. (2023). The calculated BMC20 value is given for each THTMT TH uptake assay, as well as a color graded range of BMC20 as shown in the figure legend. Compounds for which no inhibition below 20% was observed are marked in red. ND = no BMC20 value was determined, NR = no significant response observed, NT = not tested, CT = cytotoxic at BMC20 (color figure online)
For many of the chemicals tested positively in our THTMT TH uptake assays, TH system disrupting effects have been reported in animal toxicity studies or in human epidemiological studies. These studies usually only report TH changes in blood serum concentrations. THTMT inhibition, however, may not always be reflected by changes in serum TH concentrations, as shown by OATP1C1 knock out models and the OATP1C1 deficient patient (Mayerl et al. 2012; Strømme et al. 2018). Therefore, unless structural neurological and neurobehavioral effects are described, as in the case for PFOS, PFOA, PCP and TBBPA (Roze et al. 2009), the interpretation of our data in relation to in vivo effects becomes more complicated. The lack of in vivo animal studies reporting TH concentrations in brain most likely stems from the analytical difficulties of measuring TH in a complex matrix such as brain homogenates. However, recent efforts have improved TH analytics of rodent and mouse brain (De Angelis et al. 2022; Ford et al. 2023). As such TH measurements of brain content will become more prominent in the future and can give more insights into the effect of THTMT inhibitors on brain TH content in vivo. Only few studies have reported on the effect of EDCs on the transport of TH into the cerebrospinal fluid (CSF), even though the CSF has been acknowledged as an important reservoir for TH (Dratman et al. 1991; Richardson et al. 2015). TH concentrations in CSF and TH CSF:serum ratios can be indicative of neurological adverse effects, even when serum TH concentrations are within normal ranges (Funkquist et al. 2020). Thus, incorporating CSF sampling in in vivo animal studies on EDCs would provide important data with regards to the effect of THTMT inhibitors, especially for THTMTs present in the BCSFB.
In conclusion, we developed two in vitro assays for the detection of EDCs acting upon OATP1C1 and OAT4 facilitated transmembrane transport of T4. Both THTMT TH uptake assays corresponded well with previously available literature. Furthermore, we identified several chemicals that inhibited OATP1C1 facilitated T4 transmembrane transport, including TBBPA, PCP, PFOS and PFOA. Additionally, we identified BSP, TBBPA, PFOS and PFOA as a potent inhibitor of OAT4 mediated transport. These THTMT TH uptake assays can be used to rapidly screen for potential EDCs interfering with TH transport across physiological barriers, which can provide more information on the molecular mechanisms of TH system disrupting chemicals. Moreover, data from these THTMT TH uptake assays can be used to prioritize EDCs for further toxicological studies.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank Dr. Michele Visentin from the University Hospital of Zürich for providing the CHO-K1 OATP1C1 cell lines, and prof. MD. Robin Peeters from the Erasmus University Medical Center for constructive discussions and advice in producing this manuscript.
Abbreviations
- 4HCA
4-Hydroxycinnamic acid
- AHDS
Allan–Herndon–Dudley syndrome
- BBB
Blood–brain-barrier
- BCH
2-Amino-bicycloheptane-2-carboxylic acid
- BCSFB
Blood–cerebral-spinal-fluid barrier
- β-E3S
β-Estradiol-3-sulfate
- BMC
Benchmark concentration
- BMR
Benchmark response level
- BPA
Bisphenol-A
- BPAF
Bisphenol-AF
- BPF
Bisphenol-F
- BPS
Bisphenol-S
- BPZ
Bisphenol-Z
- BSP
Bromosulfopthalein
- BSA
Bovine serum albumin
- CHO-K1
Chinese hamster ovary
- cpm
Counts per minute
- DIC
Diclofenac
- DIO
Deiodinase
- DMI
Desipramine
- DMSO
Dimethylsulfoxide
- EDCs
Endocrine disrupting chemicals
- HTS
High-throughput screening
- IBU
Ibuprofen
- IC
Inhibitory concentration
- ICG
Indocyanine green
- IMI
Imidacloprid
- LESI
Lesinurad
- MCT8
Monocarboxylate transporter 8
- MDCK
Madin Darby canine kidney
- MeHg
Methyl mercury
- NaOH
Sodium hydroxide
- NSAIDS
Nonsteroidal anti-inflammatory drugs
- OATP1C1
Organic anion transporter polypeptide 1C1 (human)
- Oatp1c1
Organic anion transporter polypeptide 1C1 (rodent)
- OAT4
Organic anion transporter 4
- PBS
Phosphate-buffered saline
- PCP
Pentachlorophenol
- PFOA
Perfluorooctanoic acid
- PFOS
Perfluorooctane sulfonic acid
- PRB
Probenecid
- PTU
Propylthiouracil
- QCT
Quercetin
- RIF
Rifampicin
- rT3
Reverse T3
- SR101
Sulforhodamine 101
- SY
Silychristin
- T3
3,5,3′-Tri-iodothyronine
- T4
Thyroxine
- TBBPA
Tetrabromobisphenol-A
- TBBPS
Tetrabromobisphenol-S
- TCS
Triclosan
- TH
Thyroid hormone
- THS
Thyroid hormone system
- THTMT
Thyroid hormone transmembrane transporter
- TRP
l-Tryptophan
- TTR
Transthyretin
- UA
Uric acid
- VRP
Verapamil
- WT
Wildtype
Author contributions
The manuscript was written through contributions of all authors. All authors have given approval to the final version of the manuscript.
Funding
This work was funded by the EU Horizon 2020 project ATHENA (Assays for the identification of Thyroid Hormone axis-disrupting chemicals: Elaborating Novel Assessment strategies, under grant number 825161.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Admati I, Wasserman-Bartov T, Tovin A, Rozenblat R, Blitz E, Zada D, Lerer-Goldshtein T, Appelbaum L (2020) Neural alterations and hyperactivity of the hypothalamic–pituitary–thyroid axis in oatp1c1 deficiency. Thyroid 30:161–174. 10.1089/thy.2019.0320 10.1089/thy.2019.0320 [DOI] [PubMed] [Google Scholar]
- Bakos É, Német O, Patik I, Kucsma N, Várady G, Szakács G, Özvegy-Laczka C (2020) A novel fluorescence-based functional assay for human OATP1A2 and OATP1C1 identifies interaction between third-generation P-gp inhibitors and OATP1A2. FEBS J 287(12):2468–2485. 10.1111/febs.15156 10.1111/febs.15156 [DOI] [PubMed] [Google Scholar]
- Beard AP, Bartlewski PM, Chandolia RK, Honaramooz A, Rawlings NC (1999) Reproductive and endocrine function in rams exposed to the organochlorine pesticides lindane and pentachlorophenol from conception. Reproduction 115(2):303–314. 10.1530/jrf.0.1150303 10.1530/jrf.0.1150303 [DOI] [PubMed] [Google Scholar]
- Buckalew AR, Wang J, Murr AS, Deisenroth C, Stewart WM, Stoker TE, Laws SC (2020) Evaluation of potential sodium-iodide symporter (NIS) inhibitors using a secondary Fischer rat thyroid follicular cell (FRTL-5) radioactive iodide uptake (RAIU) assay. Arch Toxicol 94(3):873–885. 10.1007/s00204-020-02664-y 10.1007/s00204-020-02664-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cha SH, Sekine T, Kusuhara H, Yu E, Kim JY, Kim K, Sugiyama Y, Kanai Y, Endou H (2000) Molecular cloning and characterization of multispecific organic anion transporter 4 expressed in the placenta*. J Biol Chem 275:4507–4512. 10.1074/jbc.275.6.4507 10.1074/jbc.275.6.4507 [DOI] [PubMed] [Google Scholar]
- Chan S, Kilby MD (2000) Thyroid hormone and central nervous system development. J Endocrinol 165:1–8. 10.1677/joe.0.1650001 10.1677/joe.0.1650001 [DOI] [PubMed] [Google Scholar]
- Chen Z, Meima ME, Peeters RP, Visser WE (2022a) Thyroid hormone transporters in pregnancy and fetal development. Int J Mol Sci 23(23):15113. 10.3390/ijms232315113 10.3390/ijms232315113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, van der Sman ASE, Groeneweg S, de Rooij LJ, Visser WE, Peeters RP, Meima ME (2022b) Thyroid hormone transporters in a human placental cell model. Thyroid. 10.1089/thy.2021.0503 10.1089/thy.2021.0503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Peeters RP, Flach W, de Rooij LJ, Yildiz S, Teumer A, Nauck M, Sterenborg RBTM, Rutten JHW, Medici M, Edward Visser W, Meima ME (2023) Novel (sulfated) thyroid hormone transporters in the solute carrier 22 family. Eur Thyr J. 10.1530/ETJ-23-0023 10.1530/ETJ-23-0023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cope RB, Kacew S, Dourson M (2015) A reproductive, developmental and neurobehavioral study following oral exposure of tetrabromobisphenol A on Sprague-Dawley rats. Toxicology 329:49–59. 10.1016/j.tox.2014.12.013 10.1016/j.tox.2014.12.013 [DOI] [PubMed] [Google Scholar]
- De Angelis M, Maity-Kumar G, Schriever SC, Kozlova EV, Müller TD, Pfluger PT, Curras-Collazo MC, Schramm KW (2022) Development and validation of an LC-MS/MS methodology for the quantification of thyroid hormones in dko MCT8/OATP1C1 mouse brain. J Pharma Biomed Anal 221:115038. 10.1016/j.jpba.2022.115038 10.1016/j.jpba.2022.115038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong M, Li Y, Zhu M, Qin Z (2021) Tetrabromobisphenol A: a neurotoxicant or not? Environ Sci Pollut Res 28:54466–54476. 10.1007/s11356-021-15166-w/Published 10.1007/s11356-021-15166-w/Published [DOI] [PubMed] [Google Scholar]
- Dratman MB, Crutchfield FL, Schoenhoff MB (1991) Transport of iodothyronines from bloodstream to brain: contributions by blood:brain and choroid plexus:cerebrospinal fluid barriers. Brain Res 554:229–236. 10.1016/0006-8993(91)90194-z 10.1016/0006-8993(91)90194-z [DOI] [PubMed] [Google Scholar]
- Feiteiro J, Mariana M, Cairrão E (2021) Health toxicity effects of brominated flame retardants: from environmental to human exposure. In Environ Pollut 285:117475. 10.1016/j.envpol.2021.117475 10.1016/j.envpol.2021.117475 [DOI] [PubMed] [Google Scholar]
- Ford J, Riutta C, Kosian PA, O’Shaughessy K, Gilbert M (2023) Reducing uncertainties in quantitative adverse outcome pathways by analysis of thyroid hormone in the neonatal rat brain. Toxicol Sci 193(2):192–203. 10.1093/toxsci/kfad040 10.1093/toxsci/kfad040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman KP, Watt ED, Hornung MW, Hedge JM, Judson RS, Crofton KM, Houck KA, Simmons SO (2016) Tiered high-throughput screening approach to identify thyroperoxidase inhibitors within the toxcast phase I and II chemical libraries. Toxicol Sci 151(1):160–180. 10.1093/toxsci/kfw034 10.1093/toxsci/kfw034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funkquist A, Bengtsson A, Johansson PM, Svensson J, Bjellerup P, Blennow K, Wandt B, Sjöberg S (2020) Low CSF/serum ratio of free T4 is associated with decreased quality of life in mild hypothyroidism—a pilot study: CSF/s-T4 associated with QoL in hypothyroidism. J Clin Transl Endocrinol. 10.1016/j.jcte.2020.100218 10.1016/j.jcte.2020.100218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert ME, O’Shaughnessy KL, Thomas SE, Riutta C, Wood CR, Smith A, Oshiro WO, Ford RL, Hotchkiss MG, Hassan I, Ford JL (2021) Thyroid disruptors: extrathyroidal sites of chemical action and neurodevelopmental outcome-an examination using triclosan and perfluorohexane sulfonate. Toxicol Sci 183(1):195–213. 10.1093/toxsci/kfab080 10.1093/toxsci/kfab080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamers T, Kamstra JH, Sonneveld E, Murk AJ, Kester MHA, Andersson PL, Legler J, Brouwer A (2006) In vitro profiling of the endocrine-disrupting potency of brominated flame retardants. Toxicol Sci 92(1):157–173. 10.1093/toxsci/kfj187 10.1093/toxsci/kfj187 [DOI] [PubMed] [Google Scholar]
- Hu W, Zhang MY, Liu LY, Zhang ZF, Guo Y (2023) Perfluoroalkyl and polyfluoroalkyl substances (PFASs) crossing the blood-cerebrospinal fluid barrier: their occurrence in human cerebrospinal fluid. J Hazard Mater. 10.1016/j.jhazmat.2022.130003 10.1016/j.jhazmat.2022.130003 [DOI] [PubMed] [Google Scholar]
- Ibrahim KA, El-Desouky MA, Abou-Yousef HM, Gabrowny KH, El-Sayed ASM (2015) Imidacloprid and/or esfenvalerate induce apoptosis and disrupt thyroid hormones in neonatal rats. Glob J Biotechnol Biochem 10:106–112. 10.5829/idosi.gjbb.2015.10.03.1121 10.5829/idosi.gjbb.2015.10.03.1121 [DOI] [Google Scholar]
- Jayarama-Naidu R, Johannes J, Meyer F, Wirth EK, Schomburg L, Köhrle J, Renko K (2015) A nonradioactive uptake assay for rapid analysis of thyroid hormone transporter function. Endocrinology 156(7):2739–2745. 10.1210/en.2015-1016 10.1210/en.2015-1016 [DOI] [PubMed] [Google Scholar]
- Johannes J, Jayarama-Naidu R, Meyer F, Wirth EK, Schweizer U, Schomburg L, Köhrle J, Renko K (2016) Silychristin, a flavonolignan derived from the milk thistle, is a potent inhibitor of the thyroid hormone transporter MCT8. Endocrinology 157(4):1694–1701. 10.1210/en.2015-1933 10.1210/en.2015-1933 [DOI] [PubMed] [Google Scholar]
- Kacew S, Hayes AW (2020) Absence of neurotoxicity and lack of neurobehavioral consequences due to exposure to tetrabromobisphenol A (TBBPA) exposure in humans, animals and zebrafish. Arch Toxicol 94(1):59–66. 10.1007/s00204-019-02627-y 10.1007/s00204-019-02627-y [DOI] [PubMed] [Google Scholar]
- Kiciński M, Viaene MK, Den Hond E, Schoeters G, Covaci A, Dirtu AC, Nelen V, Bruckers L, Croes K, Sioen I, Baeyens W, Van Larebeke N, Nawrot TS (2012) Neurobehavioral function and low-level exposure to brominated flame retardants in adolescents: a cross-sectional study. Environ Health: Glob Access Sci Source. 10.1186/1476-069X-11-86 10.1186/1476-069X-11-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korevaar TIM, Tiemeier H, Peeters RP (2018) Clinical associations of maternal thyroid function with foetal brain development: epidemiological interpretation and overview of available evidence. Clin Endocrinol 89(2):129–138. 10.1111/cen.13724 10.1111/cen.13724 [DOI] [PubMed] [Google Scholar]
- Krebs A, Nyffeler J, Rahnenführer J, Leist M (2018) Normalization of data for viability and relative cell function curves. ALTEX. 10.14573/altex.1803231 10.14573/altex.1803231 [DOI] [PubMed] [Google Scholar]
- Kummu M, Sieppi E, Koponen J, Laatio L, Vähäkangas K, Kiviranta H, Rautio A, Myllynen P (2015) Organic anion transporter 4 (OAT 4) modifies placental transfer of perfluorinated alkyl acids PFOS and PFOA in human placental ex vivo perfusion system. Placenta 36(10):1185–1191. 10.1016/j.placenta.2015.07.119 10.1016/j.placenta.2015.07.119 [DOI] [PubMed] [Google Scholar]
- Lilienthal H, Verwer CM, van der Ven LTM, Piersma AH, Vos JG (2008) Exposure to tetrabromobisphenol A (TBBPA) in Wistar rats: neurobehavioral effects in offspring from a one-generation reproduction study. Toxicology 246(1):45–54. 10.1016/j.tox.2008.01.007 10.1016/j.tox.2008.01.007 [DOI] [PubMed] [Google Scholar]
- Loubière LS, Vasilopoulou E, Glazier JD, Taylor PM, Franklyn JA, Kilby MD, Chan SY (2012) Expression and function of thyroid hormone transporters in the microvillous plasma membrane of human term placental syncytiotrophoblast. Endocrinology 153(12):6126–6135. 10.1210/en.2012-1753 10.1210/en.2012-1753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louisse J, Dellafiora L, van den Heuvel JJMW, Rijkers D, Leenders L, Dorne JLCM, Punt A, Russel FGM, Koenderink JB (2023) Perfluoroalkyl substances (PFASs) are substrates of the renal human organic anion transporter 4 (OAT4). Arch Toxicol 97(3):685–696. 10.1007/s00204-022-03428-6 10.1007/s00204-022-03428-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayerl S, Visser TJ, Darras VM, Horn S, Heuer H (2012) Impact of Oatp1c1 deficiency on thyroid hormone metabolism and action in the mouse brain. Endocrinology 153(3):1528–1537. 10.1210/en.2011-1633 10.1210/en.2011-1633 [DOI] [PubMed] [Google Scholar]
- Park C, Kim SJ, Lee WK, Moon SK, Kwak SA, Choe SK, Park R (2016) Tetrabromobisphenol-A induces apoptotic death of auditory cells and hearing loss. Biochem Biophys Res Commun 478(4):1667–1673. 10.1016/j.bbrc.2016.09.001 10.1016/j.bbrc.2016.09.001 [DOI] [PubMed] [Google Scholar]
- Pizzagalli F, Hagenbuch B, Stieger B, Klenk U, Folkers G, Meier PJ (2002) Identification of a novel human organic anion transporting polypeptide as a high affinity thyroxine transporter. Mol Endocrinol 16(10):2283–2296. 10.1210/me.2001-0309 10.1210/me.2001-0309 [DOI] [PubMed] [Google Scholar]
- Renko K, Hoefig CS, Hiller F, Schomburg L, Köhrle J (2012) Identification of iopanoic acid as substrate of type 1 deiodinase by a novel nonradioactive iodide-release assay. Endocrinology 153(5):2506–2513. 10.1210/en.2011-1863 10.1210/en.2011-1863 [DOI] [PubMed] [Google Scholar]
- Richardson SJ, Wijayagunaratne RC, D’Souza DG, Darras VM, Van Herck SLJ (2015) Transport of thyroid hormones via the choroid plexus into the brain: The roles of transthyretin and thyroid hormone transmembrane transporters. Front Neurosci. 10.3389/fnins.2015.00066 10.3389/fnins.2015.00066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LM, Woodford K, Zhou M, Black DS, Haggerty JE, Tate EH, Grindstaff KK, Mengesha W, Raman C, Zerangue N (2008) Expression of the thyroid hormone transporters monocarboxylate transporter-8 (SLC16A2) and organic ion transporter-14 (SLCO1C1) at the blood-brain barrier. Endocrinology 149(12):6251–6261. 10.1210/en.2008-0378 10.1210/en.2008-0378 [DOI] [PubMed] [Google Scholar]
- Roze E, Meijer L, Bakker A, Van Braeckel KNJA, Sauer PJJ, Bos AF (2009) Prenatal exposure to organohalogens, including brominated flame retardants, influences motor, cognitive, and behavioral performance at school age. Environ Health Perspect 117(12):1953–1958. 10.1289/ehp.0901015 10.1289/ehp.0901015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandau CD, Ayotte P, Dewailly É, Duffe J, Norstrom RJ (2002) Pentachlorophenol and hydroxylated polychlorinated biphenyl metabolites in umbilical cord plasma of neonates from coastal populations in Québec. Environ Health Perspect 110:611–616. 10.1289/ehp.00108611 10.1289/ehp.00108611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandell EB, Kolthoff IM (1937) Micro determination of iodine by a catalytic method. Mikrochim Acta 1(1):9–25. 10.1007/BF01476194 10.1007/BF01476194 [DOI] [Google Scholar]
- Scholze M, Boedeker W, Faust M, Backhaus T, Altenburger R, Horst Grimme L (2001) A general best-fit method for concentration-response curves and the estimation of low-effect concentrations. Environ Toxicol Chem 20(2):448–457 [PubMed] [Google Scholar]
- Schwartz CE, May MM, Carpenter NJ, Rogers RC, Martin J, Bialer MG, Ward J, Sanabria J, Marsa S, Lewis JA, Echeverri R, Lubs HA, Voeller K, Simensen RJ, Stevenson RE (2005) Allan-Herndon-Dudley syndrome and the monocarboxylate transporter 8 (MCT8) gene. Am J Hum Genet 77:41–53 10.1086/431313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinkó R, Rada K, Kollár A, Mohácsik P, Tenk M, Fekete C, Gereben B (2022) Tetrabromobisphenol A and Diclazuril evoke tissue-specific changes of thyroid hormone signaling in male thyroid hormone action indicator mice. Int J Mol Sci. 10.3390/ijms232314782 10.3390/ijms232314782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skwara P, Schömig E, Gründemann D (2017) A novel mode of operation of SLC22A11: membrane insertion of estrone sulfate versus translocation of uric acid and glutamate. Biochem Pharmacol 128:74–82. 10.1016/j.bcp.2016.12.020 10.1016/j.bcp.2016.12.020 [DOI] [PubMed] [Google Scholar]
- Song S, Li Y, Lv L, Dong M, Qin Z (2024) Tetrabromobisphenol A exerts thyroid disrupting effects but has little overt impact on postnatal brain development and neurobehaviors in mice. J Environ Sci 142:1–10. 10.1016/j.jes.2023.10.028 10.1016/j.jes.2023.10.028 [DOI] [PubMed] [Google Scholar]
- Strømme P, Groeneweg S, Lima De Souza EC, Zevenbergen C, Torgersbråten A, Holmgren A, Gurcan E, Meima ME, Peeters RP, Visser WE, Høneren Johansson L, Babovic A, Zetterberg H, Heuer H, Frengen E, Misceo D, Visser TJ (2018) Mutated thyroid hormone transporter OATP1C1 associates with severe brain hypometabolism and juvenile neurodegeneration. Thyroid 28(11):1406–1415. 10.1089/thy.2018.0595 10.1089/thy.2018.0595 [DOI] [PubMed] [Google Scholar]
- Sugiyama D, Kusuhara H, Taniguchi H, Ishikawa S, Nozaki Y, Aburatani H, Sugiyama Y (2003) Functional characterization of rat brain-specific organic anion transporter (Oatp14) at the blood-brain barrier. J Biol Chem 278(44):43489–43495. 10.1074/jbc.M306933200 10.1074/jbc.M306933200 [DOI] [PubMed] [Google Scholar]
- Tohyama K, Kusuhara H, Sugiyama Y (2004) Involvement of multispecific organic anion transporter, Oatp14 (Slc21a14), in the transport of thyroxine across the blood-brain barrier. Endocrinology 145(9):4384–4391. 10.1210/en.2004-0058 10.1210/en.2004-0058 [DOI] [PubMed] [Google Scholar]
- Tomi M, Eguchi H, Ozaki M, Tawara T, Nishimura S, Higuchi K, Maruyama T, Nishimura T, Nakashima E (2015) Role of OAT4 in uptake of estriol precursor 16α-hydroxydehydroepiandrosterone sulfate into human placental syncytiotrophoblasts from fetus. Endocrinology 156(7):2704–2712. 10.1210/en.2015-1130 10.1210/en.2015-1130 [DOI] [PubMed] [Google Scholar]
- Van der Ven LTM, Van de Kuil T, Verhoef A, Verwer CM, Lilienthal H, Leonards PEG, Schauer UMD, Cantón RF, Litens S, De Jong FH, Visser TJ, Dekant W, Stern N, Håkansson H, Slob W, Van den Berg M, Vos JG, Piersma AH (2008) Endocrine effects of tetrabromobisphenol-A (TBBPA) in Wistar rats as tested in a one-generation reproduction study and a subacute toxicity study. Toxicology 245(1–2):76–89. 10.1016/j.tox.2007.12.009 10.1016/j.tox.2007.12.009 [DOI] [PubMed] [Google Scholar]
- Van Raaij JA, Van den Berg KJ, Engel R, Bragt PC, Notten WR (1994) Reduction fluid and of thyroxine uptake into cerebrospinal rat brain by hexachlorobenzene and pentachlorophenol. Toxicology 94:197–208. 10.1016/0300-483X(91)90168-Z 10.1016/0300-483X(91)90168-Z [DOI] [PubMed] [Google Scholar]
- Wagenaars F, Cenijn P, Scholze M, Frädrich C, Renko K, Köhrle J, Hamers T (2023) Screening for endocrine disrupting chemicals inhibiting monocarboxylate 8 (MCT8) transporter facilitated thyroid hormone transport using a modified nonradioactive assay. Toxicol In Vitro. 10.1016/j.tiv.2023.105770 10.1016/j.tiv.2023.105770 [DOI] [PubMed] [Google Scholar]
- Wang J, Pan Y, Cui Q, Yao B, Wang J, Dai J (2018) Penetration of PFASs across the blood cerebrospinal fluid barrier and its determinants in humans. Environ Sci Technol 52(22):13553–13561. 10.1021/acs.est.8b04550 10.1021/acs.est.8b04550 [DOI] [PubMed] [Google Scholar]
- Wang Y, Wang T, Montero-Pedrazuela A, Guadaño-Ferraz A, Rausell E (2023) Thyroid hormone transporters MCT8 and OATP1C1 are expressed in pyramidal neurons and interneurons in the adult motor cortex of human and macaque brain. Int Mol Sci. 10.3390/ijms24043207 10.3390/ijms24043207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss JM, Andersson PL, Lamoree MH, Leonards PEG, van Leeuwen SPJ, Hamers T (2009) Competitive binding of poly- and perfluorinated compounds to the thyroid hormone transport protein transthyretin. Toxicol Sci 109(2):206–216. 10.1093/toxsci/kfp055 10.1093/toxsci/kfp055 [DOI] [PubMed] [Google Scholar]
- Weiss JM, Andersson PL, Zhang J, Simon E, Leonards PEG, Hamers T, Lamoree MH (2015) Tracing thyroid hormone-disrupting compounds: database compilation and structure-activity evaluation for an effect-directed analysis of sediment. Anal Bioanal Chem 407(19):5625–5634. 10.1007/s00216-015-8736-9 10.1007/s00216-015-8736-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westholm DE, Stenehjem DD, Rumbley JN, Drewes LR, Anderson GW (2009) Competitive inhibition of organic anion transporting polypeptide 1c1-mediated thyroxine transport by the fenamate class of nonsteroidal antiinflammatory drugs. Endocrinology 150(2):1025–1032. 10.1210/en.2008-0188 10.1210/en.2008-0188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong CC, Barron D, Orfila C, Dionisi F, Krajcsi P, Williamson G (2011) Interaction of hydroxycinnamic acids and their conjugates with organic anion transporters and ATP-binding cassette transporters. Mol Nutr Food Res 55(7):979–988. 10.1002/mnfr.201000652 10.1002/mnfr.201000652 [DOI] [PubMed] [Google Scholar]
- Zhou H, Yin N, Faiola F (2020) Tetrabromobisphenol A (TBBPA): a controversial environmental pollutant. J Environ Sci 97:54–66. 10.1016/j.jes.2020.04.039 10.1016/j.jes.2020.04.039 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.