Abstract
Objective
To investigate if individual and contextual socioeconomic factors are associated with contraceptive use in Brazilian women from 18 to 49 years old, stratified by parity.
Methods
Cross-sectional, population-based study that analyzed data from 16,879 women from 18 to 49 years old, respondents of the 2013 National Health Survey. Individual factors such as reproductive history, access to health services, and sociodemographic characteristics were considered; and as contextual factors, Human Development Index (HDI), Sociodemographic Index (SDI) Primary Health Care Coverage (PHC coverage) and Average Monthly Income were included. Multilevel logistic regression models were estimated, stratified by parity, with women being level 1 and States and Federal District of level 2 units.
Results
Nulliparous women had lower prevalence of contraceptive use (77.9 %) when compared with primiparous and multiparous (88.7 %), as well as greater variability in the chance of using contraception (ICC = 2.1 vs. ICC = 1.1, respectively). Women who lived in States with higher levels of HDI, average monthly income and SDI were more likely to use contraception. The greater PHC coverage was positively associated with the use of contraceptives for primiparous/multiparous women and negatively for the nulliparous. Furthermore, higher education increased the chances of using contraception, both for nulliparous and primiparous/multiparous women.
Conclusions
The high contraceptive coverage in Brazil hides important inequities in access, highlighting contextual characteristics associated with the use of contraceptives, in addition to individual factors. The lower prevalence and chance of using contraceptives for nulliparous women with greater social vulnerability reveal inequity and priority in public policies.
Implications for practice
The need to improve access to contraception is highlighted, considering both the individual and contextual vulnerabilities of women, which implies ensuring timely and qualified access to contraceptive methods, especially for young and nulliparous women who are more socially vulnerable.
Keywords: Contraception, Family planning, Parity, Health inequalities, Multilevel analysis, Sexual and reproductive health
Highlights
-
•
The high prevalence of contraceptive use in the country hides important inequities in its access.
-
•
Women living in States with better socioeconomic conditions are more likely to use contraception.
-
•
Nulliparous women with greater social vulnerability have lower prevalence and less chance of using contraceptives.
-
•
The greater PHC coverage was positively associated with the use of contraceptives for parous women and negatively for the nulliparous.
-
•
Public policies must consider individual and contextual characteristics to reduce inequities in access to contraception.
1. Introduction
Contraceptive use has increased significantly worldwide due to greater availability of modern methods and less desire to have children [1]. Despite this increase, there are many inequalities among and within countries in access to contraception, such as disparities regarding socioeconomic status, urban/rural area of residence, geographic region [2,3], schooling level [1,2], empowerment of women [[1], [2], [3]], and parity [3].
In Brazil, contraceptive use increased significantly between 1986 and 2013 [[4], [5], [6]], with coverage above 80 % since 2006 [5,6]. However, access to contraception is also marked by socioeconomic inequalities, being the younger, less educated, with lower economic class, living in the North and Northeast regions, of black and mixed-race, the ones who present the lowest prevalence of contraceptive use [6,7].
Studies have shown that the chance of using contraceptives is also influenced by characteristics of the environment in which women live [[8], [9], [10], [11], [12], [13], [14]]. This relationship occurs mainly in countries with greater social inequalities and lower prevalence of contraceptive use, as in some African countries [[10], [11], [12], [13], [14]]. For instance, in Ethiopia, 24 % of the variability in contraceptive use was explained by characteristics of the context [12], while in Nigeria this proportion was 38.5 % [10]. Thus, environmental factors, such as greater health services coverage, proximity, lower poverty [11,13,14] and higher literacy rates [10,13,14] were also associated with a greater chance of using contraception in these settings.
In European populations studies the existence of a socioeconomic gradient in access to contraceptives have also been shown [8,9]. To our knowledge one study has evaluated whether individual and contextual factors were associated with the use of oral hormonal contraceptives among adolescents in Brazil [15]. And there was a greater chance of adolescents using the pill during their last sexual intercourse in contexts (Brazilian state capitals and the Federal District) with low maternal mortality rates and high antenatal coverage [15]. Thus, further investigation is needed on whether this inequality also represents a problem in access to contraception among women of reproductive age, which might be the reality of other countries with contexts similar to Brazil. Moreover, this investigation might advance when conducted regardless of the contraceptive type and including all women.
Several socioeconomic and health access indicators vary between States and Federal District in Brazil, which justifies the investigation of contextual aspects regarding access to contraception. Indeed, other studies have already shown the existence of marked socioeconomic and demographic inequalities affecting women's health [[4], [5], [6]], but they have not evaluated the influence of contextual variables in these outcomes.
Moreover, there is evidence of discrimination in the provision of these services based on age, marital status and parity, in which nulliparous, younger and single women [3,[16], [17], [18], [19]], are the most excluded of such services, while those with children have greater opportunities due to the universality of care provided to the pregnancy and puerperal period and child health [[16], [17], [18], [19]]. Analyzing the factors associated with the use of contraceptives in these two groups of women separately would allow assessing whether these differences are also a reality in Brazil, which could also be based on the different reasons and needs these women might have when pursuing contraception.
Thus, this study aimed to investigate if individual and contextual socioeconomic factors are associated with contraceptive use in Brazilian women aged 18–49 years, stratified by parity.
2. Methods
This is a cross-sectional epidemiological study that used data from the first edition of National Health Survey (PNS), 2013. The survey is representative of the Brazilian population and has a complex sampling plan by conglomerates in three stages of selection: census sectors, households and residents aged 18 years or more. At each stage, the selection of participants is made by simple random sampling [20]. Other publications with greater details of the sampling plan and methodological aspects have already been published [20].
The PNS was approved by the National Research Ethics Committee (CONEP no. 328.159/2013 and CAAE no. 10853812.7.0000.0008) and followed the ethical precepts of Resolution 466/12, of the National Health Council in Brazil. The data are available in the public domain, and it is not possible to identify the subjects through data manipulation.
The studied population consisted of women aged 18–49 years who responded to the “Module R – Women's Health”. Of the 60,202 individuals interviewed, 34,282 were women, of which 22,621 were at reproductive age. Pregnant women and women who did not know if they were pregnant (n = 930), hysterectomized women (n = 659), the ones who did not menstruate (n = 998) and who had not had sexual intercourse in the previous 12 months (n = 3,155) were excluded, totaling an n of 16,879 women eligible for the study. Of these women, 4,201 were nulliparous and 12,678 were primiparous or multiparous.
The outcome variable was based on the questions: R.34 “Do you currently use any method to avoid pregnancy?”; R.35 “What is the reason for not avoiding pregnancy?”; and R.36 “What method to avoid pregnancy you currently use?”. Contraceptive use was categorized by yes and no answers. Women who answered that they did not use methods because they had undergone tubal ligation or vasectomy by their partners were included in the “yes” category. Women who answered yes to question R.34, but not to all the methods mentioned, were also included in the “no” category (n = 108).
In order to assess the individual and contextual factors associated with contraceptive use, we considered the theoretical-conceptual model of the social determinants of health [21]. Thus, individual-level explanatory variables included: characteristics of reproductive history (age of first pregnancy and number of children); access to health services (participation in a reproductive planning group; registration at the basic health unit and having a health care plan). As for sociodemographic characteristics, place of residence; region; age group; education; color; marital status and paid work were considered. The contextual factors were: sociodemographic index (SDI), 2013 [22]; human development index (HDI), 2010 [23]; average monthly income [24]; and PHC coverage in 2013 [25].
The SDI is a measure of the sociodemographic development of a place, estimated from the average per capita income, average years of schooling and fertility rate, expressed on a scale from 0 to 1 [22]. The index closer to 1 indicates a better socioeconomic development and was extracted from the Global Burden of Disease (GBD) platform [22]. The HDI is a measure of long-term progress in three basic dimensions of human development: income, education and health, and is ranked low (0.550–0.699), medium (0.700–0.799) and high (≥0.800). It was obtained from the platform of the United Nations Development Program (UNDP) [23]. The nominal average monthly income of people aged 15 and over is one of the indicators of sustainable development and is estimated with data from the National Household Sample Survey (PNAD) [24]. In this study, the average monthly income was estimated for the years 2012, 2013 and 2014. PHC coverage corresponds to the estimated coverage of the population served by the Family Health Strategy teams, and by equivalent Primary Care teams regarding the population estimate. Data were extracted from the website e-gestor of the Primary Care, and the average monthly coverage of each Brazilian Federative Unit in 2013 was considered [25].
These contextual data from States and Federal District were added to the PNS database. Then, the variables were categorized into quartiles in which worst scenarios were defined as reference categories.
Firstly, to estimate the prevalence of contraceptive use, we considered in the numerator the women who reported using contraception and in the denominator all the women included in the study. Then, we estimated the prevalence of contraceptive use by States and Federal District and individual variables with their respective 95% confidence intervals (95% CI). For these estimates, aspects of the complex sampling design were considered: stratum, cluster and weight of individuals to obtain population estimates.
To analyze the individual and contextual factors associated with the use of contraceptives, we estimated multilevel logistic regression, considering women as level 1 and the States and Federal District as level 2 units. Then, the null model was performed to verify the existence of variability of the intercept between the States and Federal District. Caterpillar plots were also used to assess variance residuals and identify differences in terms of the chance of using contraceptives between the States and Federal District. Thus, after validating the assumptions of the multilevel model, a bivariate analysis of the individual and contextual characteristics associated with contraceptive use was conducted. Next, the individual variables with a p-value <0.20 were inserted into the respective multivariate models in level 1, according to theoretical-conceptual model, with the variables of the most proximal level (reproductive history) being inserted first; followed by intermediate level variables (access to health services); and finally, the variables of the most distal level (sociodemographic characteristics). Subsequently, contextual variables were included. Since these variables were highly correlated, a multilevel model was estimated for each contextual variable.
Finally, we presented the fixed and random effects, respectively, as point estimate of the parameter (Odds Ratio, OR), 95% CI, and level 2 variance. The intraclass correlation coefficient (ICC) was quantified to examine the proportion of total variance attributed to the level 2 [26]. The percentage of variance reduction was estimated between the null model and each subsequent model to assess the proportion of variance explained by the variables included in the model [26]. The Akaike information criterion (AIC) and the Bayesian information criterion (BIC) were used to compare the models and evaluate the fit, and the best model was considered the one with the lowest AIC and BIC [26]. The maximum likelihood test was also performed. In addition, a sensitivity analysis was carried out comparing the AIC and BIC of the models considering only the individual variables and the models that include the context variables. The multilevel models showed a better fit (lower AIC and BIC) than the individual models.
All analyzes were stratified by parity, as previous studies have shown differences in access to contraception between these two groups [[16], [17], [18], [19]]. All individual and contextual variables were considered in the modeling for both groups of women, except for number of children, which does not apply to nulliparous women. For women who have already given birth, this variable considered women who had only stillbirths in the first category (stillbirth/one child). Data were analyzed using the Statistical Software for Professional (Stata), version 14, and maps with the prevalence of contraceptive use were created using QGis software.
3. Results
Among Brazilian women of reproductive age, 24.9% were nulliparous and 75.1% primiparous or multiparous. Nulliparous women had lower participation in reproductive planning groups (2.5% vs. 4.7%), lower proportion of PHC enrollment (47.6% vs. 58.3%), higher proportion of access to health insurance (37.9% vs. 27.7%), were aged 18 to 24 (44.1% vs.13.1 %), with a high level of schooling (35.3% vs. 16.9%), of white color (53.1% vs. 43.8%), had paid work (76.4% vs. 63.4%) and lived without a partner (55.7% vs. 18.3%) when compared to the primiparous/multiparous group.
The prevalence of contraceptive use was 85.0%, higher for women who had already given birth (87.9 %) when compared with those who never had (77.7%) (p < 0.0001) (Table 1). Nulliparous women who lived in rural areas (64.0%; p = 0.0007) and Northeast region (65.9%; p < 0.0001); over 35 years old (p < 0.0001); less educated (66.2%; p < 0.0001); black (70.8%; p = 0.0089); without paid work (72.7%; p = 0.0286); and with a partner (70.6%; p < 0.0001) had a lower prevalence of contraceptive use (Table 2). Among primiparous/multiparous women, it was observed that women who lived without a partner (83.9%; p < 0.0001) and who lived in the North (83.1%; p < 0.0001) had a lower prevalence of contraceptive use (Table 2).
Table 1.
Characteristics of Brazilian women at reproductive age, PNS-2013.
| Individual characteristics | Nulliparous (%) | Primiparous/Multiparous (%) |
|---|---|---|
| Age at 1st pregnancy | ||
| Never got pregnant | 93.7 (92.5; 94.8) | 0 |
| <20 years | 1.9 (1.3; 2.8) | 48.3 (46.7; 50.0) |
| >20 years | 4.3 (3.5; 5.3) | 51.7 (50.0; 53.3) |
| Number of children | ||
| Stillborn/one child | NA | 35.5 (34.0; 37.0) |
| Two children | NA | 34.7 (33.2; 36.2) |
| Three or more | NA | 29.8 (28.4; 31.3) |
| Reproductive Planning Group | ||
| No | 97.5 (96.6; 98.2) | 95.3 (94.5; 96.0) |
| Yes | 2.5 (1.8; 3.4) | 4.7 (4.0; 5.5) |
| PHC registration | ||
| No | 52.4 (49.5; 55.3) | 41.7 (40.0; 43.5) |
| Yes | 47.6 (44.7; 50.5) | 58.3 (56.5; 60.0) |
| Health care plan | ||
| No | 62.1 (59.4; 64.7) | 72.3 (70.7; 73.8) |
| Yes | 37.9 (35.3; 40.6) | 27.7 (26.2; 29.3) |
| Place of living | ||
| Rural | 7.5 (6.2; 9.0) | 14.9 (14.0; 15.8) |
| Urban | 92.5 (90.9; 93.8) | 85.1 (84.2; 86.0) |
| Region | ||
| North | 7.4 (6.4; 8.4) | 8.8 (8.2; 9.4) |
| Northeast | 22.2 (20.1; 24.5) | 29.5 (28.2; 30.8) |
| Southeast | 45.6 (42.8; 48.4) | 40.1 (38.6; 41.7) |
| South | 16.8 (15.0; 18.9) | 14.0 (12.9; 15.1) |
| Midwest | 8.0 (7.1; 8.9) | 7.6 (7.1; 8.1) |
| Age group | ||
| 18–24 years | 44.1(41.3; 46.9) | 13.1 (11.9; 14.3) |
| 25–29 years | 20.4 (18.5; 22.5) | 14.8 (13.9; 15.8) |
| 30–34 years | 15.9 (14.1; 17.9) | 21.6 (20.4; 22.9) |
| 35–39 years | 9.0 (7.7; 10.5) | 20.1 (18.9; 21.4) |
| 40–44 years | 6.4 (5.3; 7.7) | 17.9 (16.8; 19.1) |
| 45–49 years | 4.2 (3.4; 5.2) | 12.5 (11.4; 13.6) |
| Schooling | ||
| 0–8 years of schooling | 16.7 (14.8; 18.8) | 42.1 (40.6; 43.6) |
| 9–11 years of schooling | 47.9 (45.2; 50.7) | 41.0 (39.5; 42.6) |
| 12 or more years of schooling | 35.3 (32.7; 38.1) | 16.9 (15.6; 18.2) |
| Skin color | ||
| Black | 7.9 (6.5; 9.5) | 8.8 (7.9; 9.7) |
| White/Asian | 53.1 (50.3; 55.9) | 43.8 (42.3; 45.3) |
| Mixed race | 38.8 (36.1; 41.6) | 46.9 (45.4; 48.4) |
| Indigenous | 0.2 (0.1; 0.4) | 0.6 (0.4; 0.8) |
| Work status | ||
| Not working | 23.6 (21.4; 26.1) | 36.5 (35.1; 38.0) |
| Paid job | 76.4 (73.9; 78.6) | 63.4 (62.0; 64.9) |
| Living with partner | ||
| No | 55.7 (53.0; 58.4) | 18.3 (17.2; 19.4) |
| Yes | 44.3 (41.6; 46.9) | 81.7 (80.6; 82.8) |
Table 2.
Prevalence of contraceptive use stratified by parity in Brazilian women aged 18–49 years, according to reproductive history, access to health services and sociodemographic characteristics, PNS 2013.
| Prevalence of contraceptive use |
||||||
|---|---|---|---|---|---|---|
| Variables | All women (n = 16,879) |
Nulliparous (n = 4201) |
Parous women (n = 12,678) |
|||
| %a (CI95 %)b | pc | %a (CI95 %)b | pc | %a (CI95 %)b | pc | |
| Age at 1st pregnancy | <0.0001 | <0.0001 | <0.0001 | |||
| Never got pregnant | 78.7 (76.1; 81.1) | 78.7 (76.1; 81.1) | NA | |||
| <20 years | 87.7 (86.2; 89.0) | 87.6 (78.8; 93.1) | 87.7 (86.2; 89.0) | |||
| >20 years | 87.0 (85.6; 88.3) | 51.5 (40.6; 62.3) | 88.2 (86.8; 89.4) | |||
| Number of children | <0.0001 | <0.0001 | ||||
| Stillborn/one child | 84.1 (82.1; 85.8) | NA | 84.1 (82.1; 85.8) | |||
| Two children | 91.1 (89.6; 92.3) | NA | 91.1 (89.6; 92.3) | |||
| Three or more | 88.9 (87.0; 90.5) | NA | 88.9 (87.0; 90.5) | |||
| Reproductive Planning Group | 0.0209 | 0.8769 | 0.0259 | |||
| No | 84.8 (83.7; 85.8) | 77.7 (75.0; 80.1) | 87.7 (86.7; 88.7) | |||
| Yes | 90.2 (85.8; 93.4) | 78.8 (62.0; 89.4) | 92.7 (88.4; 95.4) | |||
| PHCregistration | 0.1304 | 0.5809 | 0.1374 | |||
| No | 84.2 (82.6; 85.6) | 78.4 (75.0; 81.4) | 87.1 (85.4; 88.5) | |||
| Yes | 85.7 (84.3; 87.0) | 77.0 (73.0; 80.5) | 88.6 (87.3; 89.7) | |||
| Health care plan | 0.1449 | 0.0352 | 0.2357 | |||
| No | 84.6 (83.3; 85.7) | 75.8 (72.3; 79.0) | 87.6 (86.4; 88.7) | |||
| Yes | 86.0 (84.3; 87.6) | 80.9 (77.2; 84.1) | 88.9 (87.0; 90.5) | |||
| Place of living | 0.0301 | 0.0007 | 0.0814 | |||
| Rural | 82.5 (79.8; 84.9) | 64.0 (54.1; 72.2) | 86.2 (84.1; 88.2) | |||
| Urban | 85.4 (84.3; 86.4) | 78.8 (76.1; 81.3) | 88.2 (87.1; 89.3) | |||
| Region | <0.0001 | <0.0001 | <0.0001 | |||
| North | 81.0 (78.4; 83.4) | 74.7 (69.2; 79.6) | 83.1 (80.2; 85.6) | |||
| Northeast | 82.4 (80.2; 84.4) | 65.9 (59.2; 72.0) | 87.4 (85.7; 88.9) | |||
| Southeast | 86.0 (84.2; 87.6) | 81.9 (77.8; 85.3) | 87.8 (85.9; 89.5) | |||
| Midwest | 87.1 (85.3; 88.7) | 80.8 (76.6; 84.3) | 89.8 (87.8; 91.4) | |||
| South | 88.4 (86.3; 90.1) | 81.8 (77.2; 85.7) | 91.5 (89.1; 93.4) | |||
| Age group | 0.5598 | <0.0001 | 0.1472 | |||
| 18–24 years | 84.0 (81.3; 86.4) | 81.8 (77.5; 85.5) | 86.9 (83.6; 89.6) | |||
| 25–29 years | 84.5 (82.2; 86.5) | 81.7 (77.6; 85.1) | 86.0 (83.2; 88.5) | |||
| 30–34 years | 85.5 (83.3; 87.4) | 78.6 (73.0; 83.3) | 87.5 (85.0; 89.6) | |||
| 35–39 years | 84.7 (82.5; 86.8) | 63.9 (55.3; 71.6) | 88.5 (86.4; 90.3) | |||
| 40–44 years | 86.9 (84.6; 88.9) | 62.4 (52.7; 71.3) | 90.4 (88.4; 92.2) | |||
| 45–49 years | 84.9 (81.9; 87.4) | 64.5 (53.2; 74.4) | 87.6 (84.8; 89.9) | |||
| Schooling | 0.13 | <0.0001 | 0.0264 | |||
| 0–8 years of schooling | 83.7 (82.0; 85.2) | 66.2 (59.3; 72.4) | 86.4 (84.9; 87.9) | |||
| 9–11 years of schooling | 85.7 (84.1; 87.1) | 78.9 (75.2; 82.1) | 88.8 (87.2; 90.2) | |||
| 12 or more years of schooling | 85.9 (83.7; 87.8) | 81.6 (77.6; 85.0) | 89.5 (87.2; 91.5) | |||
| Skin color | 0.1078 | 0.0089 | 0.4604 | |||
| Black | 82.6 (78.0; 86.4) | 70.8 (59.0; 80.4) | 86.9 (83.1; 89.9) | |||
| White/Asian | 86.2 (84.8; 87.5) | 81.4 (78.4; 84.0) | 88.5 (86.8; 89.9) | |||
| Mixed race | 84.2 (82.7; 85.6) | 74.0 (69.5; 78.1) | 87.6 (86.3; 88.8) | |||
| Indigenous | 88.1 (76.9; 94.3) | 81.3 (55.2; 93.9) | 89.1 (76.0; 95.5) | |||
| Work status | 0.1675 | 0.0286 | 0.1217 | |||
| Not working | 84.0 (82.1; 85.7) | 72.7 (66.7; 78.0) | 86.9 (85.1; 88.5) | |||
| Paid job | 85.5 (84.3; 86.7) | 79.3 (76.4; 81.8) | 88.5 (87.3; 89.7) | |||
| Living with partner | 0.0788 | <0.0001 | <0.0001 | |||
| No | 83.6 (81.5; 85.5) | 83.3 (80.1; 86.1) | <0.0001 | 83.9 (81.1; 86.4) | <0.0001 | |
| Yes | 85.6 (84.4; 86.7) | 70.6 (66.6; 74.3) | 88.8 (87.9; 89.8) | |||
| Total | 85.0 (84.0; 86.0) | 77.7 (75.1; 80.1) | 87.9 (86.9; 88.9) | |||
NOTE: a (%) – prevalence; b (CI95%) – confidence interval of 95%; c (p) – value for, Pearson's chi-square test.
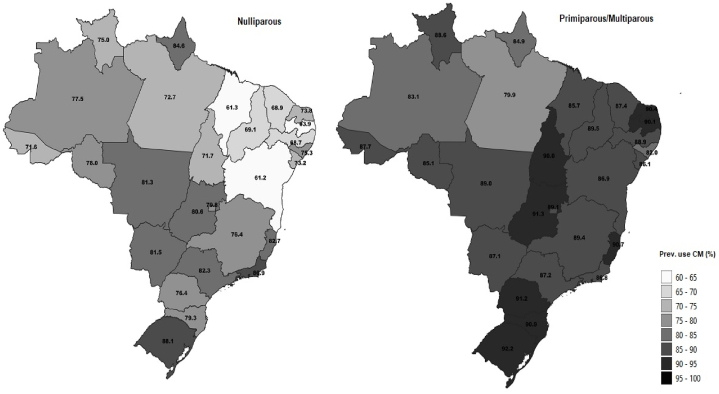
Fig. 1 shows the prevalence of contraceptive use by Brazilian States and Federal District. Among nulliparous women, prevalence ranged from 61.2% in Bahia to 88.1% in Rio Grande do Sul. There was a lower prevalence of contraceptive use (<70%) in the states of the Northeast region (Bahia, Maranhão, Paraíba, Pernambuco, Ceará and Piauí) (Fig. 1/Table 3). Among primiparous/multiparous women, the prevalence of contraceptive use varied from 79.9% in Pará to 92.2% in Rio Grande do Sul. Of the 27 clusters evaluated, 23 had a prevalence of contraceptive use of more than 85% (Fig. 1/Table 3).
Fig. 1.
Prevalence of contraceptive use in Brazilian States and Federal District stratified by parity, PNS-Brazil, 2013.
Table 3.
Socioeconomic indicators and prevalence of contraceptive method use in Brazilian States and Federal District.
| Use of contraceptive methods |
Socioeconomic indicators |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ranking | States | Nulliparous (%) | Ranking | States | Primiparous/Multiparous women (%) | Ranking | States | HDI 2010 | Ranking | States | SDI 2013 | Ranking | States | Average monthly income - 2012, 2013, 2014 (Brazilian reais) | Ranking | States | PHC coverage 2013 |
| 1 | BA | 61.16 | 1 | PA | 79.92 | 1 | AL | 0.631 | 1 | MA | 0.5809 | 1 | AL | R$ 928,00 | 1 | PA | 53.23 |
| 2 | MA | 61.34 | 2 | AL | 81.99 | 2 | MA | 0.639 | 2 | PI | 0.5846 | 2 | CE | R$ 973,00 | 2 | SP | 54.4 |
| 3 | PB | 63.92 | 3 | AM | 83.14 | 3 | PA | 0.646 | 3 | AL | 0.5917 | 3 | MA | R$ 985,67 | 3 | DF | 57.44 |
| 4 | PE | 68.71 | 4 | AP | 84.92 | 4 | PI | 0.646 | 4 | PB | 0.6098 | 4 | PI | R$ 995,33 | 4 | RJ | 57.54 |
| 5 | CE | 68.89 | 5 | RO | 85.06 | 5 | PB | 0.658 | 5 | PA | 0.6119 | 5 | PE | R$ 1.063,67 | 5 | AM | 63.11 |
| 6 | PI | 69.11 | 6 | MA | 85.68 | 6 | BA | 0.66 | 6 | CE | 0.6186 | 6 | PA | R$ 1.069,67 | 6 | RS | 63.45 |
| 7 | AC | 71.56 | 7 | SE | 86.06 | 7 | AC | 0.663 | 7 | BA | 0.6198 | 7 | PB | R$ 1.071,00 | 7 | RO | 67.88 |
| 8 | TO | 71.68 | 8 | RJ | 86.81 | 8 | SE | 0.665 | 8 | AC | 0.6205 | 8 | BA | R$ 1.097,00 | 8 | ES | 69.14 |
| 9 | PA | 72.71 | 9 | BA | 86.91 | 9 | PE | 0.673 | 9 | PE | 0.6234 | 9 | SE | R$ 1.120,00 | 9 | MT | 69.17 |
| 10 | SE | 73.19 | 10 | MS | 87.13 | 10 | AM | 0.674 | 10 | RN | 0.6388 | 10 | RN | R$ 1.146,67 | 10 | MS | 69.84 |
| 11 | RN | 73.85 | 11 | SP | 87.17 | 11 | CE | 0.682 | 11 | SE | 0.6415 | 11 | TO | R$ 1.273,33 | 11 | RR | 69.86 |
| 12 | RR | 74.99 | 12 | CE | 87.36 | 12 | RN | 0.684 | 12 | TO | 0.6491 | 12 | AC | R$ 1.280,67 | 12 | BA | 70.04 |
| 13 | AL | 75.35 | 13 | AC | 87.66 | 13 | RO | 0.69 | 13 | RO | 0.6528 | 13 | AM | R$ 1.303,00 | 13 | GO | 71.6 |
| 14 | PR | 76.38 | 14 | RR | 88.57 | 14 | TO | 0.699 | 14 | RR | 0.6662 | 14 | RO | R$ 1.372,67 | 14 | PR | 73.32 |
| 15 | MG | 76.44 | 15 | PE | 88.91 | 15 | RR | 0.707 | 15 | AM | 0.6663 | 15 | RR | R$ 1.419,00 | 15 | PE | 74.64 |
| 16 | AM | 77.45 | 16 | MT | 89.0 | 16 | AP | 0.708 | 16 | MS | 0.6694 | 16 | AP | R$ 1.481,33 | 16 | CE | 77.75 |
| 17 | RO | 78.05 | 17 | DF | 89.07 | 17 | MT | 0.725 | 17 | AP | 0.6703 | 17 | MG | R$ 1.492,67 | 17 | AP | 79.03 |
| 18 | SC | 79.33 | 18 | MG | 89.37 | 18 | MS | 0.729 | 18 | GO | 0.676 | 18 | GO | R$ 1.552,33 | 18 | AL | 80.58 |
| 19 | DF | 79.85 | 19 | PI | 89.54 | 19 | MG | 0.731 | 19 | MT | 0.6803 | 19 | ES | R$ 1.572,00 | 19 | MA | 81.58 |
| 20 | GO | 80.59 | 20 | TO | 90.04 | 20 | GO | 0.735 | 20 | MG | 0.6855 | 20 | MT | R$ 1.697,33 | 20 | MG | 82.42 |
| 21 | MT | 81.3 | 21 | PB | 90.11 | 21 | ES | 0.74 | 21 | ES | 0.7048 | 21 | MS | R$ 1.721,33 | 21 | AC | 82.54 |
| 22 | MS | 81.49 | 22 | RN | 90.37 | 22 | RS | 0.746 | 22 | PR | 0.7057 | 22 | RS | R$ 1.729,00 | 22 | SC | 85.75 |
| 23 | SP | 82.3 | 23 | ES | 90.66 | 23 | PR | 0.749 | 23 | RS | 0.7171 | 23 | PR | R$ 1.744,67 | 23 | RN | 87.72 |
| 24 | ES | 82.71 | 24 | SC | 90.88 | 24 | RJ | 0.761 | 24 | SC | 0.7224 | 24 | SC | R$ 1.814,00 | 24 | SE | 88.11 |
| 25 | AP | 84.58 | 25 | PR | 91.24 | 25 | SC | 0.774 | 25 | RJ | 0.7356 | 25 | RJ | R$ 1.883,33 | 25 | TO | 90.59 |
| 26 | RJ | 86.89 | 26 | GO | 91.35 | 26 | SP | 0.783 | 26 | SP | 0.745 | 26 | SP | R$ 1.966,00 | 26 | PB | 96.65 |
| 27 | RS | 88.07 | 27 | RS | 92.2 | 27 | DF | 0.824 | 27 | DF | 0.8179 | 27 | DF | R$ 3.112,00 | 27 | PI | 98.62 |
As for the contextual characteristics, the indicators (HDI, SDI, monthly average income) with higher levels of development were found in the States of the South (Paraná, Santa Catarina and Rio Grande do Sul) and Southeast (São Paulo and Rio de Janeiro) regions, plus the Federal District, while the lowest levels were found in the ones of the Northeast (Alagoas, Maranhão, Piauí and Paraíba). On the other hand, States with the highest PHC coverage are located in the Northeast (Piauí, Tocantins, Paraíba and Sergipe), while the lowest coverage is observed in the Southeast (São Paulo, Rio de Janeiro) and the Federal District, with the exception of Pará, which has the lowest coverage and is located in the North (Table 3).
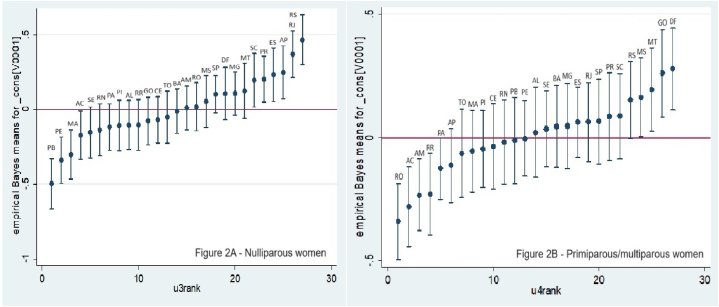
Fig. 2 shows the random effects estimates, and nulliparous women had less chance of using contraceptives in the States of Paraíba, Pernambuco (Northeast), Maranhão and Acre (North). The highest chances of using contraceptives were in Santa Catarina, Paraná, Espírito Santo, Amapá, Rio de Janeiro and Rio Grande do Sul (Fig. 2A). The null model shows that 2.1% of the variability in the chance of using contraceptives among nulliparous women is attributable to the States (ICC:0.021; p < 0.001) (Table 4). Among primiparous/multiparous women, the lower chance of using contraceptives were observed in Rondônia, Acre, Amazonas and Roraima (North), while Rio Grande do Sul, Mato Grosso do Sul, Mato Grosso, Goiás and the Federal District (South and Midwest) presented higher chances of using contraceptive methods (Fig. 2B). In this group, the variability in the chance of contraceptive use attributed to States was 1.1% (ICC: 0.0108; p < 0.0001) (Table 4). Both null models showed a statistically significant result (p < 0.0001) in the likelihood ratio test, indicating model fit improvement with the inclusion of contextual random effects (Table 4).
Fig. 2.
Graphs of variance residuals, chance of using contraceptives stratified by parity, according to States and Federal District, Brazil, PNS 2013.
Table 4.
Variability of the chance of using contraception between Brazilian states and the Federal District, according to the parity of women of reproductive age (null model/empty model), PNS 2013.
| Model null | Nulliparous | Primiparous/multiparous women |
|---|---|---|
| n | 4,201 | 12,678 |
| Coefficient | 1.23 (1.10–1.35) | 1.99 (1.90–2.08) |
| Variance | 0.703 (0.298–1.656) | 0.0359 (0.015–0.083) |
| ICCa | 2.09 (0.90–4.79) | 1.08 (0.47–2.47) |
| LR testb | 19.9 (p < 0.0001) | 20.84 (p < 0.0001) |
| AICc/BICd | 4434.7/4453.7 | 9408.3/9423.2 |
NOTE: a (ICC) – Intraclass correlation coefficient; b (LR test) – The maximum likelihood test; c (AIC) – Akaike information criterion; d (BIC) – Bayesian information criterion.
Moreover, living in urban areas and having more schooling were positively associated with contraceptive use, while being older and living with a partner were associated with lower contraceptive use among the nulliparous (Table 5). As for the contextual variables, the higher HDI, SDI and average monthly income (3rd and 4th quartile), the greater the chance of using contraceptives. On the contrary, higher PHC coverage (4th quartile) was associated with lower contraceptive use in this group. The SDI showed the greatest reduction in variance (82.8 %) and lowest AIC/BIC, showing that women living in States with better socioeconomic indicators are more likely to use contraceptives (Table 5).
Table 5.
Individual and contextual factors associated with contraceptive use in nulliparous Brazilian women at reproductive age, PNS-Brazil, 2013.
| Variables | Model IDH 2010 |
Model SDI 2013 |
Model Average monthly income |
Model PHC coverage |
|---|---|---|---|---|
| ORa (CI95 %)b | ORa (CI95 %)b | ORa (CI95 %)b | ORa (CI95 %)b | |
| FIXED EFFECTS | ||||
| Place of living | ||||
| Rural | Ref. | Ref. | Ref. | Ref. |
| Urban | 1.36 (1.07; 1.71) | 1.36 (1.07; 1.72) | 1.36 (1.08; 1.73) | 1.39 (1.09; 1.76) |
| Age group | ||||
| 18–24 years | Ref. | Ref. | Ref. | Ref. |
| 25–29 years | 0.80 (0.65; 0.99) | 0.80 (0.65; 0.99) | 0.80 (0.65; 0.99) | 0.80 (0.65; 0.99) |
| 30–34 years | 0.77 (0.61; 0.97) | 0.76 (0.61; 0.96) | 0.77 (0.61; 0.97) | 0.77 (0.61; 0.97) |
| 35–39 years | 0.45 (0.35; 0.58) | 0.45 (0.35; 0.57) | 0.45 (0.35; 0.58) | 0.45 (0.35; 0.57) |
| 40–44 years | 0.44 (0.34; 0.58) | 0.44 (0.34; 0.57) | 0.44 (0.34; 0.58) | 0.44 (0.34; 0.58) |
| 45–49 years | 0.44 (0.32; 0.62) | 0.44 (0.32; 0.62) | 0.45 (0.32; 0.63) | 0.46 (0.33; 0.64) |
| Schooling | ||||
| 0–8 years of schooling | Ref. | Ref. | Ref. | Ref. |
| 9–11 years of schooling | 1.33 (1.08; 1.62) | 1.32 (1.08; 1.61) | 1.33 (1.08; 1.62) | 1.34 (1.10; 1.64) |
| 12 to more years of schooling | 1.43 (1.15; 1.78) | 1.42 (1.15; 1.77) | 1.43 (1.15; 1.77) | 1.48 (1.19; 1.84) |
| Living with partner | ||||
| No | Ref. | Ref. | Ref. | Ref. |
| Yes | 0.60 (0.52; 0.71) | 0.60 (0.52; 0.71) | 0.60 (0.51; 0.70) | 0.61 (0.52; 0.71) |
| Contextual variables | HDI 2010 | SDI 2013 | Monthly average income | PHC coverage |
| 1st quartile | Ref. | Ref. | Ref. | Ref. |
| 2nd quartile | 1.17 (0.91; 1.50) | 1.11 (0.88; 1.41) | 1.24 (0.97; 1.58) | 1.02 (0.74; 1.41) |
| 3rd quartile | 1.66 (1.29; 2.13) | 1.57 (1.22; 2.02) | 1.70 (1.34; 2.16) | 0.81 (0.58; 1.12) |
| 4rh quartile | 1.68 (1.27; 2.22) | 1.79 (1.39; 2.31) | 1.72 (1.31; 2.25) | 0.71 (0.51; 0.99) |
| RANDOM EFFECTS | ||||
| Variance (CI95 %) | 0.18 (0.03; 0.95) | 0.13 (0.01; 0.95) | 0.15 (0.02; 0.96) | 0.44 (0.15; 1.26) |
| Variance reduction | 0.54 (74.3 %) | 0.57 (81.4 %) | 0.55 (78.6 %) | 0.26 (37.1 %) |
| ICCc(CI95 %) | 0.54 (0.10; 2.80) | 0.41 (0.05; 2.81) | 0.46 (0.07; 2.84) | 1.32 (0.47; 3.68) |
| AICd/BICe | 4264.7/4353.5 | 4261.1/4349.9 | 4263.3/4352.1 | 4275.6/4364.4 |
NOTE: a (OR) – Odds Ratio; b (CI95 %) – Confidence interval = 95 %; c (ICC) – Intraclass correlation coefficient; d (AIC) – Akaike information criterion; e (BIC) – Bayesian information criterion.
Women who have already given birth, with two or more children, participated in reproductive planning groups, with a higher educational level, living with a partner and with paid work status had a higher chance of using contraceptives in the primiparous/multiparous group (Table 6). On the other hand, those over 40, presented a decreased chance of using contraception. As for contextual variables, higher HDI, higher average monthly income (3rd quartile) and greater PHC coverage (2nd and 4th quartile) were positively associated with contraceptive use. The HDI (44.4 %) and the average monthly income (41.7 %) showed a greater reduction in variance and the SDI did not show a statistically significant association with the use of contraceptives (p = 0.055) (Table 6).
Table 6.
Individual and contextual factors associated with contraceptive use in primiparous and multiparous Brazilian women at reproductive age, PNS-Brazil, 2013.
| Variables | Model IDH 2010 |
Model SDI 2013 |
Model Monthly average income |
Model PHC coverage |
|---|---|---|---|---|
| ORa (CI95 %)b | ORa (CI95 %)b | ORa (CI95 %)b | ORa (CI95 %)b | |
| FIXED EFFECTS | ||||
| Number of children | ||||
| Stillborn/One child | Ref. | Ref. | Ref. | Ref. |
| Two children | 1.88 (1.64; 2.16) | 1.88 (1.65; 2.16) | 1.88 (1.64; 2.16) | 1.87 (1.64; 2.15) |
| Three or more | 1.84 (1.59; 2.12) | 1.83 (1.58; 2.12) | 1.84 (1.59; 2.13) | 1.81 (1.57; 2.10) |
| Reproductive Planning Group | ||||
| No | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.50 (1.11; 2.02) | 1.49 (1.11; 2.01) | 1.49 (1.11; 2.01) | 1.50 (1.11; 2.02) |
| Age group | ||||
| 18–24 years | Ref. | Ref. | Ref. | Ref. |
| 25–29 years | 0.95 (0.78; 1.16) | 0.95 (0.78; 1.16) | 0.95 (0.78; 1.16) | 0.95 (0.78; 1.16) |
| 30–34 years | 0.98 (0.80; 1.19) | 0.97 (0.80; 1.19) | 0.98 (0.80; 1.19) | 0.98 (0.81; 1.20) |
| 35–39 years | 0.91 (0.74; 1.12) | 0.91 (0.74; 1.12) | 0.91 (0.74; 1.12) | 0.92 (0.75; 1.13) |
| 40–44 years | 0.88 (0.71; 1.09) | 0.88 (0.71; 1.09) | 0.88 (0.71; 1.09) | 0.89 (0.72; 1.11) |
| 45–49 years | 0.72 (0.57; 0.90) | 0.72 (0.57; 0.90) | 0.72 (0.57; 0.90) | 0.73 (0.58; 0.92) |
| Schooling | ||||
| 0–8 years | Ref. | Ref. | Ref. | Ref. |
| 9–11 years | 1.33 (1.17; 1.50) | 1.32 (1.17; 1.50) | 1.33 (1.17; 1.50) | 1.33 (1.17; 1.51) |
| 12 to more years | 1.28 (1.09; 1.51) | 1.27 (1.08; 1.50) | 1.28 (1.08; 1.51) | 1.28 (1.09; 1.51) |
| Living with partner | ||||
| No | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.15 (1.02; 1.31) | 1.15 (1.02; 1.31) | 1.15 (1.02; 1.31) | 1.15 (1.02; 1.31) |
| Work status | ||||
| No | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.13 (1.01; 1.28) | 1.14 (1.01; 1.28) | 1.13 (1.01; 1.31) | 1.15 (1.02; 1.29) |
| Contextual variable | HDI 2010 | SDI 2013 | Monthly average income | PHC coverage |
| 1° quartile | Ref. | Ref. | Ref. | Ref. |
| 2° quartile | 0.97 (0.79; 1.18) | 0.97 (0.78; 1.20) | 0.98 (0.80; 1.19) | 1.30 (1.02; 1.67) |
| 3° quartile | 1.41 (1.14; 1.75) | 1.27 (0.99; 1.62) | 1.42 (1.15; 1.75) | 1.18 (0.93; 1.51) |
| 4° quartile | 1.11 (0.87; 1.41) | 1.21 (0.94; 1.56) | 1.11 (0.87; 1.42) | 1.39 (1.07; 1.79) |
| RANDOM EFFECTS | ||||
| Variance | 0.20 (0.07; 0.60) | 0.30 (0.12; 0.74) | 0.21 (0.07; 0.60) | 0.29 (0.11; 0.73) |
| Variance reduction | 0.16 (44.4 %) | 0.06 (16.7 %) | 0.16 (41.7 %) | 0.07 (19.4 %) |
| ICCc(CI95 %) | 0.62 (0.22; 1.79) | 0.90 (0.36; 2.20) | 0.62 (0.21; 1.80) | 0.87 (0.34; 2.18) |
| AICd/BICe | 9287.9/9414.5 | 9293.3/9419.9 | 9287.9/9414.5 | 9292.9/9419.6 |
NOTE: a (OR) – Odds Ratio; b (Ci95 %) – Confidence interval = 95 %; c (ICC) – intraclass correlation coefficient; d (AIC) – Akaike information criterion; e (BIC) – Bayesian information criterion.
4. Discussion
Our results showed that individual and contextual characteristics were associated with the use of contraceptives by Brazilian women at reproductive age. Women residing in States with higher levels of socioeconomic indicators, such as HDI, SDI and average monthly income, were more likely to use contraceptives. For nulliparous women, these indicators better explained the variability of contraceptive use between States, as they presented a higher percentage of variance reduction (greater than 75%), in addition to greater strengths of association and socioeconomic gradient. The contextual variable PHC coverage was negatively associated with contraceptive use by nulliparous women, which corroborates the hypothesis that these women, especially those with greater social vulnerability, face greater challenges in accessing contraception in the country.
These findings corroborate results in contexts of high-income countries that, even in a better socioeconomic context, there were also differences in the chance of using contraception [8,9]. For instance, in Spain, the highest percentage of women with higher education and the highest enrollment rate of children aged 0–2 in schools were positively associated with the use of modern contraception [9]. The highest percentage of family poverty was negatively associated with contraceptive use [8,9].
Similar results have also been observed in low and middle-income countries, mainly in the ones of African continent, such as Nigeria [10,14], Ethiopia [12,13] and Mali [11], which are characterized by lower contraceptive prevalence and a higher level of social inequalities. In Nigeria and Ethiopia, the study population was restricted to married women and showed that women living in clusters with higher income and higher education were more likely to use modern contraceptives [10,[12], [13], [14]]. In Mali, the study population included young women aged 15 to 24 and the lower the wealth quintile and literacy rate of the clusters, the lower the chance of using contraceptives [11].
Another study that included 14 Latin American and Caribbean countries, excluding Brazil, assessed the individual and contextual factors associated with the demand for contraception, an indicator that refers to women of reproductive age and sexually active who use contraceptives, which ranged from 43.4% in Bolivia to 89.5% in Cuba [27]. Moreover, 11.8% of the variability in demand for contraception met was attributed to context, with women living in countries with high gender inequality being 70% less likely to have their demand for contraception met [27]. Although comparison must take into consideration the differences in the outcome this study corroborates our results in considering the contextual factors in access to contraception in countries with similar characteristics, such as high coverage of contraceptive use and exacerbated social inequalities.
The worst levels of socioeconomic indicators registered (lowest SDI, HDI and average monthly income) and the lowest prevalence of contraceptive use were found in States in the North and Northeast regions. Such results confirm that strong socioeconomic and demographic inequalities in the country may affect access to contraception. Additionally, a previous evaluation of aspects related to access to oral and injectable contraceptives in the country showed that most women obtained these contraceptive methods in pharmacies, with their own resources [7], reinforcing the impact of socioeconomic inequalities and contextual determinants, such as income on access to contraception in the country.
Brazil has experienced considerable economic growth and improvements in socioeconomic indicators over the last 20–30 years, but it remains as one of the most unequal countries in the world [28] and the lowest level of these indicators is observed in the States from North and Northeast regions [29]. Furthermore, Brazilian society is characterized by social stratification and disparities in infrastructure and availability of public services between individuals, neighborhoods, States and regions [4,[30], [31], [32]]. Consequently, inequalities in health, with regard to various health outcomes has been reported in relation to individual socioeconomic position [33,34] geographic region [35,36] and socioeconomic indicators, such as income inequality, measured by the Gini index [37]. Therefore, our findings corroborate the constant need for interventions to reduce such health inequalities in the country.
In addition, we found that greater PHC coverage was positively associated with a higher chance of using contraception in the group of women who had already given birth, contrary to what was found in the group of nulliparous women. A possible explanation for this difference would be the greater opportunities of access to contraception for those who have already given birth, as they are included in health services due to antenatal care, after birth and child health [17]. Such programs are known to have expanded with the increase of PHC coverage and have contributed to advances in maternal and child health, including access to contraception [4,32]. Previous study showed that municipalities with greater PHC coverage had greater availability of contraceptives, suggesting that such availability is directly associated with coverage [38]. These authors have shown this indicator to be an important determinant of contraceptive use, corroborating our findings. However, they also showed that the North region had the worst levels of availability, remaining below 80% for all inputs, except condoms [38]. This result supports our findings, which showed a lower prevalence of contraceptive use by women in the States in this region.
Other studies have shown that the greater the parity and the number of children, the more likely women are to want to space or limit the number of children and, consequently, the greater the use of contraceptives [39,40]. This could be explained by the higher motivation of these women to use contraception, considering they may have already reached the desired family size, as well as greater access to reproductive planning services, since care for these women is already well structured in these services [16,17]. Moreover, this is one of the priorities PHC areas in Brazil. Therefore, parity may have shown itself once again as a marker of access to health services, explaining the greater access found in the primiparous/multiparous women, as already reported in other countries [[14], [15], [16]].
A multilevel analysis on the use of the pill among adolescents in Brazil showed no association with PHC coverage [15], which may reflect lower access of the younger and single population to reproductive planning services. Another factor that may explain the more vulnerable condition of nulliparous women is the bias of health professionals, who tend to not consider the need for contraception of these women regardless of age [19]. Moreover, younger women may face other access barriers, such as the costs associated with the use of contraceptives, distance from health services, lack of knowledge about contraception, fear of side effects and opposition from partners, as previously described [16,17]. We also observed that almost half of the women who gave birth had their first pregnancy before the age of 20, reinforcing the lower access of young and nulliparous women to contraception opportunely. This highlights the need to improve the policies of reproductive planning for this population.
As for individual factors, schooling and age group were associated with the use of contraceptives. Thus, it is emphasized that the relationship between higher education and fertility has a lasting impact on women's lives, as it serves as a resource of knowledge, empowerment, an instrument for socioeconomic mobility and a modifier of attitudes that influence the reproductive desires and behavior, including the consistent use of contraceptives [41]. This corroborates our findings, which showed that higher education increases the chances of using contraceptives on both groups.
As for age, the lower chance of using contraceptives in older age groups can be explained by these women's perception of a lower risk of pregnancies, despite all the women in this study having reported an active sexual life in the last 12 months. Moreover, delays in fertility or perceived deficiencies as a result of previous contraceptive use can lead to dissatisfaction and lower use of methods, regardless of current desire to have children [42]. This can expose women to the risk of an unintended and hazardous pregnancy. Additionally, living with a partner was associated with lower chance of using contraception for nulliparous women and higher chance for parous women, which can be explained by the desire to have children.
For primiparous/multiparous women, other individual factors were associated with a greater chance of using contraceptives: having two or more children, participation in reproductive planning groups, and paid work, once again corroborating our hypothesis that these women have more opportunities to access reproductive health services. For nulliparous women living in urban areas the chance of using contraceptives is augmented, which can be explained by the more facilitated access to health services in urban contexts. Furthermore, the individual and contextual factors are associated with the outcome differently. While having a partner decreased the chance of using contraception among nulliparous it increased the chance of parous women. Also, the participation of reproductive planning educational group was associated with greater chance of using contraception among primiparous/multiparous but not for nulliparous. These corroborates the differences in access to contraception when considering the parity of women.
Finally, the need for interventions to reduce observed inequalities in access to contraception in the country is emphasized, which may include strategies both to reduce observed regional socioeconomic inequalities, as well as policies that promote the use of contraceptives regardless of women's parity, especially for the group of nulliparous women with greater social vulnerability. The following strategies are suggested: investments in educational programs, such as in schools, to raise awareness among teenagers on the importance of using contraception and planning reproductive life; improvement in access to health services, particularly in relation to the strengthening and adequate financing of the Unified Health System and qualification of PHC professionals in the provision of contraception; and monitoring and evaluation of indicators of access to contraception in the country to support public policies to promote universal and equitable access to contraception.
5. Limitations
Contextual factors at the level of Brazilian States and Federal District can hide residual differences when referring to the contexts of small municipalities or metropolitan regions within each State. Thus, associations found having contextual variables as exposures should be interpreted with caution, since the plausibility of the associations may not be similar even when referring to geographically smaller contexts. Other limitations can be mentioned, such as the lack of data on women's desire to become pregnant, a determining factor in the use of contraceptives; and the use of cross-sectional data, which implies that causality cannot be inferred, although the factors associated to contraceptive use in the final model do not suggest the possibility of reverse causation.
Nevertheless, the availability of data on access to contraception in the first edition of the PNS used in this study is an advance, since the latest national data on contraception are from the National Survey of Demography and Health, carried out in 2006. Although the most current version of the 2019 PNS is available, changes in some questions from the survey questionnaire, including the exclusion of them, hinders the reproducibility of variables used in the present study. In addition, the contextual indicators investigated in the present study (HDI, SDI and Average monthly income) are not updated for the 2019 period, which would also imply the difficulty of replicating this study using the same parameters. Added to these analytical limits are the changes in the country's political and economic scenario between the two surveys. From 2006 to 2013, several public policies were implemented in the area of Sexual and Reproductive Health, such as the National Policy on Sexual and Reproductive Rights (2005) and the National Policy on Family Planning (2007), which expanded access to contraception in the country [43]. It was also a period characterized by rapid economic changes, with inflation controlled in 1994, and strong economic growth between 2004 and 2011, which favored the reduction of socioeconomic inequalities in the country [4,32,44]. As of 2014, there was a sudden interruption of this entire process of political and programmatic advancement in the area of Sexual and Reproductive Health, with budget cuts [45] and the extinction of public policies, such as the National Plan of Policies for Women [[44], [45], [46]], as well as setbacks in abortion legislation [43,44], and worsening of the country's economic scenario, with increased unemployment and poverty [43,44].
These results could be a point of reference for the continuous monitoring of access to contraception in the country and elucidate crucial role of contraception access and use surveillance for other settings with similar issues. Thus, our analysis contributes for understanding differences in contraceptive use among women even with data that are not so current. The prevalence of use may have varied over time, but it is unlikely that the mechanisms determining its use are different today. In any case, if these mechanisms have really changed in the last few years, the updated data is incomplete which hinders the reproducibility of the present study.
Despite these limits, the use of multilevel analysis as an adequate technique to simultaneously assess individual and contextual factors associated with the use of contraceptives, makes it possible to identify inequities in access to contraception in the country. Such injustices can be made invisible in the face of high coverage of contraceptive use, as demonstrated in other low and middle-income countries [3]. Another strength is the analysis which have shown differences in the use of contraception in each stratum of parity in terms of the magnitude of use, including the contextual factors associated with the outcome. This might have better explained the greater variability in the use of contraceptives for the nulliparous group.
Another aspect that should be valued in this investigation refers to the inclusion of all women of reproductive age, not just the married ones, most of whom are primiparous/multiparous, as in many studies. Those women account for less than half of women at reproductive age in Brazil and worldwide they represent 15.7% of all users of modern contraceptives. Thus, an increase in demand for contraception is expected among single women worldwide [47].
6. Conclusion
The results of the present study highlight the need to expand access to contraception, considering, in addition to individual vulnerabilities, the context in which women live, affecting their choices and reproductive outcomes. This implies guaranteeing sexual and reproductive rights and, consequently, timely and qualified access to contraceptive methods, regardless of women's age, marital status and parity. It is also important to regularly monitor contraceptive indicators in order to support reproductive planning policies in the country, as well as to address persistent geographical and socioeconomic inequalities, since they may have worsened after the covid-19 pandemic and the austerity measures implemented in recent years.
Ethical approval
The PNS was approved by the National Research Ethics Committee (Conep number. 328.159/2013 and CAAE number 10853812.7.0000.0008) and followed the ethical precepts of Resolution 466/12, of the National Health Council. The data are available in the public domain, and it is not possible to identify the subjects through data manipulation.
Funding
This research has not received any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Fernanda Gontijo Araújo: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. Gustavo Velasquez-Melendez: Formal analysis, Methodology, Supervision, Validation, Writing – review & editing. Mariana Santos Felisbino-Mendes: Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Resources, Software, Supervision, Validation, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We acknowledge the Graduate Program in Nursing of Universidade Federal de Minas Gerais for support in translating this study using resources from PROAP/CAPES (Coordination for the Improvement of Higher Education Personnel).
Footnotes
** This article is part of the PhD dissertation of Fernanda Gontijo Araújo, Graduate Program in Nursing, Department of Maternal and Child Nursing and Public Health, School of Nursing at the Universidade Federal de Minas Gerais.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e34833.
Contributor Information
Fernanda Gontijo Araújo, Email: fernandagontijo2005@hotmail.com.
Gustavo Velasquez-Melendez, Email: jguveme@gmail.com.
Mariana Santos Felisbino-Mendes, Email: marianafelisbino@yahoo.com.br, marianafelisbino@gmail.com.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Sully E.A., Biddlecom J.E., Darroch J.E., Riley T., Ashford L.S., Lince-Deroche N., et al. Guttmacher Institute; New York: 2020. Adding it up: Investing in Sexual and Reproductive Health 2019. [DOI] [Google Scholar]
- 2.Ewerling F., Victora C.G., Raj A., Coll C.V.N., Hellwig F., Barros A.J.D. Demand for family planning satisfied with modern methods among sexually active women in low- and middle-income countries: who is lagging behind? Reprod. Health. 2018 Mar 6;15(1):42. doi: 10.1186/s12978-018-0483-x. PMID: 29510682; PMCID: PMC5840731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sully E.A., Biddlecom A., Darroch J.E. Not all inequalities are equal: differences in coverage across the continuum of reproductive health services. BMJ Glob. Health. 2019;4 doi: 10.1136/bmjgh-2019-001695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.França G.V., Restrepo-Méndez M.C., Maia M.F., Victora C.G., Barros A.J. Coverage and equity in reproductive and maternal health interventions in Brazil: impressive progress following the implementation of the Unified Health System. Int. J. Equity Health. 2016;15(1):149. doi: 10.1186/s12939-016-0445-2. PMID: 27852276; PMCID: PMC5112713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cavenaghi S.A., Diniz J.E. The everlasting outmoded contraceptive method mix in Brazil and its legacy. Braz. J. Popul. Stud. 2019;36 doi: 10.20947/S0103-3098a0103. [DOI] [Google Scholar]
- 6.Trindade R.E., Siqueira B.B., Paula T.F., Felisbino-Mendes M.S. Uso de contracepção e desigualdades do planejamento reprodutivo das mulheres brasileiras. Cien Saude Colet. 2021;26(2):3493–3504. doi: 10.1590/1413-81232021269.2.24332019. [DOI] [PubMed] [Google Scholar]
- 7.Farias M.R., Leite S.N., Tavares N.U.L., Oliveira M.A., Arrais P.S.D., Bertoldi A.D., et al. Use of and access to oral and injectable contraceptives in Brazil. Rev. Saude Publica. 2016;50(2) doi: 10.1590/S1518-8787.2016050006176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bentley R., Kavanagh A., Smith A. Area disadvantage, socioeconomic position and women's contraception use: a multilevel study in the UK. BMJ Sex Reprod Health. 2009;35:221–226. doi: 10.1783/147118909789587277. [DOI] [PubMed] [Google Scholar]
- 9.Muñoz D.R., Pérez G., Gotsens M., Rodriguez-Sanz M. Regional inequalities in the use of contraception in Spain: a multilevel approach. Health Place. 2012;18(2):408–414. doi: 10.1016/j.healthplace.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Ejembi C.L., Tukur D., Alhaji A.A. Contextual factors influencing modern contraceptive use in Nigeria. DHS Working Papers. 2015;120 doi: 10.13140/RG.2.1.1719.5923. [DOI] [Google Scholar]
- 11.Ahinkorah B.O., Seidu A., Appiah F., Budu E., Adu C., Aderoju Y.B.G., et al. Individual and community-level factors associated with modern contraceptive use among adolescent girls and young women in Mali: a mixed effects multilevel analysis of the 2018 Mali demographic and health survey. Contracept Reprod Med. 2020;5(27) doi: 10.1186/s40834-020-00132-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tegegne T.K., Chojenta C., Forder P.M., Getachew T., Smith R., Loxton D. Spatial variations and associated factors of modern contraceptive use in Ethiopia: a spatial and multilevel analysis. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-037532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Terefe B., Getnet M., Akalu Y., Belsti Y., Diress M., Gela Y.Y., Getahun A.B., Bitew D.A., Belay D.G. Geospatial variations and determinants of contraceptive utilization among married reproductive age women in Ethiopia: spatial and multilevel analysis of Ethiopian Demographic and Health Survey, 2019. Front. Glob. Womens Health. 2023;4 doi: 10.3389/fgwh.2023.1151031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bolarinwa O.A., Ajayi K.V., Okeke S.R., Hailegebreal S., Odimegwu C. Spatial distribution and multilevel analysis of factors associated with long-acting reversible contraceptive use among sexually active women of reproductive age in Nigeria. Arch Public Health. 2023; Jun 2;81(1):99. doi: 10.1186/s13690-023-01110-6. PMID: 37269016; PMCID: PMC10236581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borges A.L.V., Duarte L.S., Lay A.A.R., Fujimori E. Individual and context correlates of the oral pill and condom use among Brazilian female adolescents. BMC Wom. Health. 2021;21(307) doi: 10.1186/s12905-021-01447-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He Y., Zhang N., Wang J., He N., Du Y., Ding J.X., et al. Evaluation of two intervention models on contraceptive attitudes and behaviors among nulliparous women in Shanghai, China: a clustered randomized controlled trial. Reprod. Health. 2017;14(1):73. doi: 10.1186/s12978-017-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Behrman J.A., Wright K.Q., Grant M.J., Soler-Hampejsek E. Trends in modern contraceptive use among young adult women in sub-Saharan Africa 1990 to 2014. Stud. Fam. Plann. 2018;49(4):319–344. doi: 10.1111/sifp.12075. [DOI] [PubMed] [Google Scholar]
- 18.Singh P., Singh K.K., Singh A., Pandey A. The levels and trends of contraceptive use before first birth in India (2015-16): a cross-sectional analysis. BMC Publ. Health. 2020;20(1):771. doi: 10.1186/s12889-020-08917-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dieci M., Wagner Z., Friedman W., Burgess S., Vandermark J., McCoy S.I., et al. Measuring family planning provider bias: a discrete choice experiment among Burkinabé, Pakistani, and Tanzanian providers. Stud. Fam. Plann. 2021;52(3):299–320. doi: 10.1111/sifp.12170. [DOI] [PubMed] [Google Scholar]
- 20.Szwarcwald C.L., Malta D.C., Pereira C.A., Vieira M.L.F.P., Conde W.L., Souza Junior P.R.B., et al. Pesquisa Nacional de Saúde no Brasil: concepção e metodologia de aplicação. Cien Saude Colet. 2014;19(2):333–342. doi: 10.1590/1413-81232014192.14072012. [DOI] [PubMed] [Google Scholar]
- 21.Buss P.M. Pellegrini Filho A. A saúde e seus determinantes sociais. Physis: Revista de Saúde Coletiva. 2007;17:77–93. doi: 10.1590/S0103-73312007000100006. [DOI] [Google Scholar]
- 22.Global Burden of Disease Collaborative Network . Institute for Health Metrics and Evaluation (IHME); Seattle, United States of America: 2016. Global Burden of Disease Study 2015 (GBD 2015) Socio-Demographic Index (SDI) 1980–2015.http://ghdx.healthdata.org/record/global-burden-disease-study-2015-gbd-2015-socio-demographic-index-sdi-1980%E2%80%932015 [cited 2022 Apr 25] Available from: [Google Scholar]
- 23.Programa das Nações Unidas para o Desenvolvimento Humano (PNUD) Atlas de Desenvolvimento no Brasil. 2013 http://www.atlasbrasil.org.br/ranking [Internet] [cited 2022 Apr 25] Available from: [Google Scholar]
- 24.Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Amostra por Domicílios [Internet]. [cited 2022 Apr 25] Available from: <https://sidra.ibge.gov.br/tabela/5794#notas-tabela>.
- 25.Brasil. E-gestor Atenção Básica. Informação e Gestão da Atenção Básica. [Internet] [cited 2022 Apr 25] Available from: https://egestorab.saude.gov.br/paginas/acessoPublico/relatorios/relHistoricoCoberturaAB.xhtml.
- 26.Merlo J., Chaix B., Ohlsson H., Beckman A., Johnell K., Hierpe P., et al. Brief conceitual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J. Epidemiol. Community Health. 2006;60(4):290–297. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moreira L.R., Blumenberg C., Caicedo Velasquez B.E., Ewerling F., Balandrán A., Vidaletti L.P., Varela A.R., Hellwig F., Ponce de Leon R.G., Barros A.J.D., Silveira M.F., Wehrmeister F.C. The role of gender inequality and health expenditure on the coverage of demand for family planning satisfied by modern contraceptives: a multilevel analysis of cross-sectional studies in 14 LAC countries. Lancet Reg Health Am. 2023 Feb 8;19 doi: 10.1016/j.lana.2023.100435. PMID: 36950033; PMCID: PMC10025422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsounta E., Osueke A.I. International Monetary Fund; Washington: 2014. What Is behind Latin America's Declining Income Inequality? IMF Working Paper 14/124.https://www.imf.org/en/Publications/WP/Issues/2016/12/31/What-is-Behind-Latin-Americas-Declining-Income-Inequality-41748 [Internet] [cited 2024 May 30]. Available from: [Google Scholar]
- 29.Boing A.F., Boing A.C., Wagner K.J.P., Subramanian S.V. Narrowing geographic inequality in life expectancy in Brazil: a multilevel analysis between 1991 and 2010. Publ. Health. 2020 Mar;180:102–108. doi: 10.1016/j.puhe.2019.11.015. Epub 2019 Dec 24. PMID: 31881463. [DOI] [PubMed] [Google Scholar]
- 30.Paim J., Travassos C., Almeida C., Bahia L., Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011; May 21;377(9779):1778–1797. doi: 10.1016/S0140-6736(11)60054-8. Epub 2011 May 9. PMID: 21561655. [DOI] [PubMed] [Google Scholar]
- 31.Victora C.G., Aquino E.M., do Carmo Leal M., Monteiro C.A., Barros F.C., Szwarcwald C.L. Maternal and child health in Brazil: progress and challenges. Lancet. 2011 May 28;377(9780):1863–1876. doi: 10.1016/S0140-6736(11)60138-4. Epub 2011 May 9. PMID: 21561656. [DOI] [PubMed] [Google Scholar]
- 32.Castro M.C., Massuda A., Almeida G., Menezes-Filho N.A., Andrade M.V., de Souza Noronha K.V.M., Rocha R., Macinko J., Hone T., Tasca R., Giovanella L., Malik A.M., Werneck H., Fachini L.A., Atun R. Brazil's unified health system: the first 30 years and prospects for the future. Lancet. 2019 Jul 27;394(10195):345–356. doi: 10.1016/S0140-6736(19)31243-7. Epub 2019 Jul 11. PMID: 31303318. [DOI] [PubMed] [Google Scholar]
- 33.Lima-Costa M.F., De Oliveira C., Macinko J., Marmot M. Socioeconomic inequalities in health in older adults in Brazil and England. Am J Public Health. 2012 Aug;102(8):1535–1541. doi: 10.2105/AJPH.2012.300765. Epub 2012 Jun 14. PMID: 22698020; PMCID: PMC3464850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Malta D.C., Bernal R.T., de Souza M.F., Szwarcwald C.L., Lima M.G., Barros M.B. Social inequalities in the prevalence of self-reported chronic non-communicable diseases in Brazil: national health survey 2013. Int. J. Equity Health. 2016 Nov 17;15(1):153. doi: 10.1186/s12939-016-0427-4. PMID: 27852264; PMCID: PMC5112650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Szwarcwald C.L., Souza Júnior PR., Marques A.P., Almeida W.D., Montilla D.E. Inequalities in healthy life expectancy by Brazilian geographic regions: findings from the National Health Survey, 2013. Int. J. Equity Health. 2016 Nov 17;15(1):141. doi: 10.1186/s12939-016-0432-7. PMID: 27852270; PMCID: PMC5112675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oliveira A.P.C., Gabriel M., Poz M.R.D., Dussault G. Challenges for ensuring availability and accessibility toin health care services under Brazil's Unified Health System (SUS) Cien Saude Colet. 2017 Apr;22(4):1165–1180. doi: 10.1590/1413-81232017224.31382016. Portuguese, English. doi: 10.1590/1413-81232017224.31382016. Erratum in: Cien Saude Colet. 2017 Jul;22(7):2397-2424. PMID: 28444043. [DOI] [PubMed] [Google Scholar]
- 37.Vincens N., Emmelin M., Stafström M. The interplay of contextual layers: a multilevel analysis of income distribution, neighborhood infrastructure, socioeconomic position and self-rated health in Brazil. Health Place. 2018 Jul;52:155–162. doi: 10.1016/j.healthplace.2018.05.012. Epub 2018 Jun 9. PMID: 29894906. [DOI] [PubMed] [Google Scholar]
- 38.Ruivo A.C.O., Facchini L.A., Tomasi E., Wachs L.S., Fassa A.C.G. Disponibilidade de insumos para o planejamento reprodutivo nos três ciclos do Programa de Melhoria do Acesso e da Qualidade da Atenção Básica: 2012, 2014 e 2018. Cad. Saúde Pública. 2021;37(6) doi: 10.1590/0102-311X00123220. [DOI] [PubMed] [Google Scholar]
- 39.Almalik M., Mosleh S., Almasarweh I. Are users of modern and traditional contraceptive methods in Jordan different? East. Mediterr. Health J. 2018;24(4):377–384. doi: 10.26719/2018.24.4.377. [DOI] [PubMed] [Google Scholar]
- 40.Kebede A., Abaya S.G., Merdassa E., Bekuma T.T. Factors affecting demand for modern contraceptives among currently married reproductive age women in rural Kebeles of Nunu Kumba district, Oromia, Ethiopia. Contracept Reprod Med. 2019;4(21) doi: 10.1186/s40834-019-0103-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rios Neto E., Miranda-Ribeiro A., Miranda-Ribeiro P. Fertility differentials by education in Brazil: from the conclusion of fertility to the onset of postponement transition. Popul. Dev. Rev. 2018;44(3):489–517. http://www.jstor.org/stable/26622852 [Google Scholar]
- 42.Kaplan B., Nahum R., Yairi Y., Hirsch M., Pardo J., Yogev Y., et al. Use of various contraceptive methods and time of conception in a community-based population. Eur. J. Obstet. Gynecol. Reprod. Biol. X. 2005;123:72–76. doi: 10.1016/j.ejogrb.2005.06.033. [DOI] [PubMed] [Google Scholar]
- 43.Alves J.E.D., Cavenaghi S. Progressos e retrocessos na conquista da equidade de gênero no Brasil. Rev. Usp. 2019;122:11–26. doi: 10.11606/issn.2316-9036.v0i122p11-26. [DOI] [Google Scholar]
- 44.Ventura D. After testing times, Brazil is back. BMJ. 2023;380:48. doi: 10.1136/bmj.p48. PMID: 36634925. [DOI] [PubMed] [Google Scholar]
- 45.Rossi P., Dweck E. Impacts of new fiscal regime on health and education. Cad Saúde Pública [online]. 457. 2016;32 doi: 10.1590/0102-311X00194316. [DOI] [PubMed] [Google Scholar]
- 46.Gonçalves R., Abreu S. Do plano nacional de políticas para as mulheres ao "machistério" de Temer. Rev. 519 Polit. Públicas. 2019;22(2):753–771. doi: 10.18764/2178-2865.v22n2p753-771. [DOI] [Google Scholar]
- 47.Kantorová V., Wheldon M.C., Uefing P., Dasgupta A.N.Z. Estimating progress towards meeting women's contraceptive needs in 185 countries: a bayesian hierarchical modelling study. PLoS Med. 2020;17(2) doi: 10.1371/journal.pmed.1003026. https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003026 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.