Abstract
Background:
The selection and allocation of surgeons with a greater potential for high surgical performance are essential aspects of improving the quality, safety, and effectiveness of surgical procedures. Objective of this trial was to determine the existence of basic skills and traits that would predict better performance in surgery, and those predictive factors that constitute a driving force in different stages of training.
Materials and methods:
The randomized crossover training trial took place from January 2021 to December 2021 and was conducted at an educational training center for minimally invasive surgery. A total of n=87 physicians (residents and experts) from surgical disciplines and n=239 fifth-year medical students were studied. The participants underwent extensive neuropsychological testing and surgical training, which was performed with conventional as well as robot-assisted laparoscopy by way of identical brief tasks conducted six times in a randomized crossover setting. Main Outcome was the latent factor structure of ‘psychomotor skills’, ‘personality’, and ‘motivation’ based on structural equation modeling.
Results:
The training performance of both students and physicians was significantly explained by the interaction of the three factors (explained variance: 8.2% for students, 23.8% for physicians). In students, motivation (explained variance 8.4%) and personality (explained variance 4.5%) revealed the highest contribution to surgical training performance (explained variance through psychomotor skills 1.1%). In physicians, psychomotor skills (explained variance 27.4%) made the greatest contribution to surgical training performance (explained variance through motivation 2.3%; explained variance through personality 10.5%).
Conclusion:
The study showed that surgical performance is sensitive to, and fragile in regard of nonsurgery-related general individual traits. This aligns with the notion that early selection of surgeons with prospects of high surgical performance is possible, and perhaps even necessary in order to keep up with future demands on the medical system.
Keywords: aptitude, laparoscopy, personality, psychomotor skills, robotic, surgical training
Introduction
Highlights
Motivation contributed significantly to high surgical performance in students.
Personality contributed significantly to high surgical performance in students.
Psychomotor skills contributed significantly to surgical performance in physicians.
Surgical performance is sensitive to nonsurgery-related general individual traits.
Selection of surgeons with prospects of high surgical performance seems possible.
A large majority of surgeons would describe their work as a passion1. The desire to become a surgeon frequently arises from, or is related to, personal attitudes, motivation, and previous experience in surgery. Some of those aspects may be specific individual traits independent of surgery as such, but could still predetermine surgical performance along with other basic neuropsychological skills. To date, we lack a comprehensive strategy that could be applied in the occupational setting to assess individual characteristics as predictors of a surgeon’s aptitude. Thus, we also lack a standardized means of identifying doctors suited to this profession, as has been done in other professions and fields. In the aircraft industry, for instance, evaluation tests for selecting candidates have been in use for several decades. These tests comprise basic neuropsychological factors including cognitive abilities (e.g. spatial and numerical abilities), motor-related competencies (e.g. psychomotor abilities and multitasking), and personality traits2. The selection of individuals based on specific patterns of these factors resulted in better performance for the majority of aircraft industry procedures and the achievement of an exceptionally high level of safety in the aircraft3,4. We lack such standardized evaluation strategies for surgeons. The in-hospital mortality rate after visceral surgery in Germany is nearly 2%5; some of the complications are probably surgeon-related6. These facts reveal the need for improvement in surgical performance, as the latter is essential to ensure the quality and safety of surgical procedures. The recruitment of personnel could well be the starting point of this endeavor.
Surgery is a complex synergy of medical rationale, technical approaches, and the surgeon performing the procedure. While the medical rationale, devices, and surgical techniques are checked regularly in regard of their efficacy, economy, and safety7–9, the surgeons’ aptitude has received scant attention10. The surgeon’s aptitude is formed by basic neuropsychological skills and individual traits, which interact with medical rationale, devices, and the ability to learn surgical techniques. The entire package can be reinforced and extended by training procedures to some extent. We have some preliminary evidence to show that surgical performance can, at least in part, be predicted by certain skills and traits11. Cognitive and visuospatial factors were shown to be the most important skills for surgical performance10. Personality traits were also found to influence preoperative indications12 and intraoperative decisions13. Interestingly, personality traits correlated with the performance of experienced surgeons and were also identified as predictive factors for success throughout the education of surgeons14.
Although these studies have provided initial evidence of surgical aptitude being a key component of surgical performance, the investigated features remained at the level of single, unselected variables. This has resulted in rather mixed patterns and findings. Given the fact that these variables strongly interact with each other, as different personality factors interact to constitute an individual’s general personality, research needs to proceed by taking such interaction and correlation into account. Applying this consideration in terms of viewing a variety of factors constituting surgical aptitude would culminate in the formulation of specific valid effects on surgical performance. This may then serve as the central aspect in the complex selection or allocation of surgeons. These phenomena have been discussed in previous studies10,15, and have been underlined by research in the field of psychological and cognitive (neuro)science, where the consideration of individual factors rather than their interplay resulted in rather small effect sizes16–18. However, the variables studied so far did not encompass aspects relevant to surgery. Apart from personality and neuropsychological skills, the quantity of effort and motivation were shown to be critical factors for achieving high performance in the occupational setting19–23.
These factors viewed together call for a more efficient assessment and analytical approach in regard of advanced machine learning methods, well selected skills and traits, and especially their interactions. Therefore, we designed an interdisciplinary study comprising a team of gynecologists and neuropsychologists to utilize knowledge from both fields, applying and combining advanced methodologies in clinical training. We defined a set of variables as inter-related factors, so-called latent constructs, within a structural equation modeling (SEM) framework24. These latent constructs cover three key factors of surgical aptitude, namely psychomotor skills, personality and motivation, and were derived from a modern training setting comprising students and physicians. To further account for potential contributions of each of the considered variables, we applied further machine learning algorithms to determine their respective level of importance for surgical training performance.
Based on this study design, we aimed to address the following questions: Do specific basic skills and traits create a predisposition for better performance in surgery, and which of these factors are the driving force within the constellation? Do prediction models differ in terms of their constitution, depending on surgical experience (students vs. physicians)? In other words, does the duration of practice make certain factors more important for the selection or allocation of persons to the surgeon’s profession?
Methods
Participants and recruitment
The investigation extended from 1 January 2021 to 31 December 2021 and was conducted at an educational training center for minimally invasive surgery. Postgraduates of general surgery, urology, and gynecology who attended minimally surgical training courses were invited to attend the study on a voluntary basis. The training courses7,8 have been certified by the German Society of Gynecological Endoscopy (AGE e.V.). Furthermore, medical students in their fifth year of training were invited to attend the study as part of their syllabus. The provision of training tools and aids was supported financially by the faculty through an innovative teaching fund. Informed consent was obtained from all participants. The study was approved by the responsible ethics committee.
Study protocol
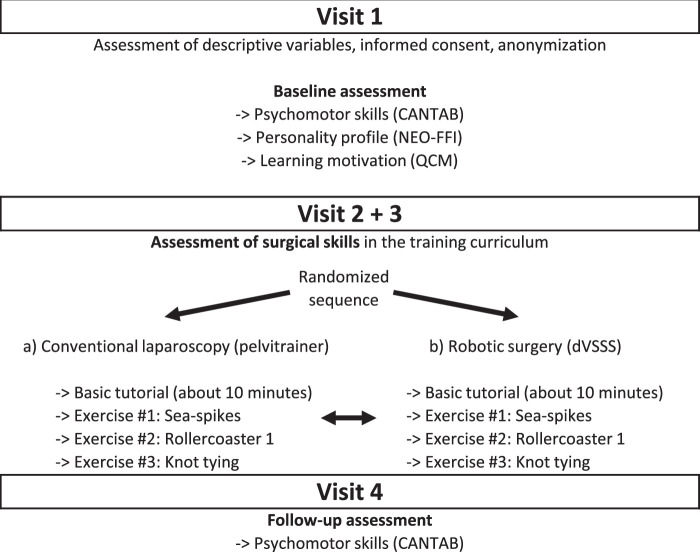
A randomized crossover surgical training trial was designed. The first visit included an assessment of the participant’s personality profile, psychomotor skills, and learning motivation by the use of the assessment tools described below. Other descriptive variables, such as demographic data, occupational experience, surgical experience, and intended specialization, were registered.
At the next two visits, identical surgical tasks were performed in randomized sequence, with the da Vinci Surgical Skills Simulator (dVSSS) (Intuitive Surgical, Inc.) and the conventional pelvitrainer (Karl Storz GmbH & Co. KG). A minimum interval of one day and a maximum interval 14 days was permitted between the two training sessions.
The study plan is shown in Figure 1. The training setting and the registered parameters are summarized in Figure 2.
Figure 1.
Study Protocol. CANTAB, Cambridge Neuropsychological Test Automated Battery; NEO-FFI, NEO Five Factor Inventory; QCM, questionnaire on current motivation.
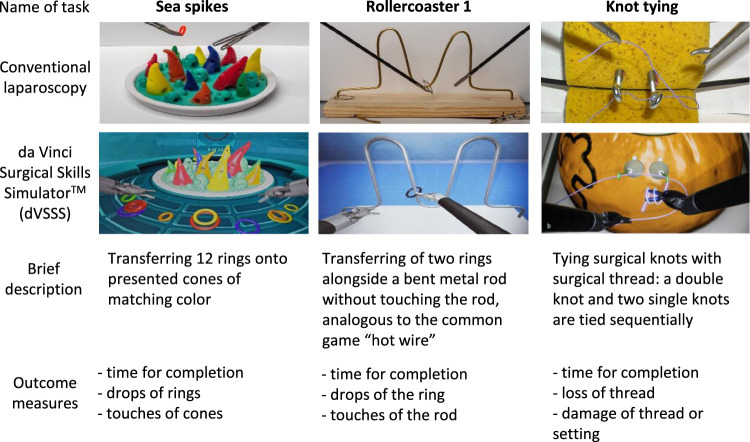
Figure 2.
Surgical tasks.
Assessment of psychomotor skills using the Cambridge neuropsychological test automated battery (CANTAB)
The CANTAB is a digital platform for the assessment of neuropsychological attributes. It is a sensitive and validated digital assessment battery, widely used, with over 2000 peer-reviewed publications and 100 000 citations25. Through reliable and randomized presentation of stimuli and measurements26, computer-based tasks of this nature make it possible to capture the behavior and neuropsychological performance of individuals with an accuracy of milliseconds.
Together with neuropsychologists, the surgeons identified a set of CANTAB tasks to investigate those psychomotor skills that seemed most relevant in the context of surgical aptitude. The tasks included the following: Motor-Screening Task (MOT), Paired Associates Learning (PAL), Rapid Visual Information Processing (RVP), Rapid Visual Information Processing (RVP), and Reaction Time Task (RTI). The tasks were carried out on identical tablets (Apple iPad 2017) under standardized conditions as recommended by Cambridge Cognition Limited.
Assessment of personality using the NEO five factor inventory (NEO-FFI)
The NEO-FFI is a self-reporting pen-and-pencil questionnaire assessing five personality traits27,28: Neuroticism (N), Extraversion (E), Openness to Experience (O), Agreeableness (A), and Conscientiousness (C). We used a validated German version29 with 60 items. For analyses, we used the sum scores of the five personality traits, respectively.
Assessment of motivation using the questionnaire on current motivation (QCM)
The motivation in learning situations was evaluated using QCM19. It contains 18 items to measure four motivational factors: anxiety, probability of success, interest, and challenge. For each item, participants have to rate their level of agreement/disagreement to the statement on a seven point Likert-scale (from 1 – ‘does not apply’ to 7 – ‘does apply’)19.
Surgical training course and assessment of surgical performance
Performance and training progress in surgical tasks were recorded. Laparoscopy as well as robot-assisted techniques were used to accomplish three different training tasks. The training setting can be seen in Figure 2. After a basic tutorial, each task was performed three times sequentially with conventional or robotic technique. Then the participants switched to the complementary technique and accomplished the tasks in the same manner. On the next visit, the order of the methods was reversed. For conventional laparoscopy, we used the classical pelvitrainer and 2D full HD camera of Karl Storz (Karl Storz GmbH & Co. KG). The camera with a 30-degree optic was fixed in a standard overview perspective in all tasks so there was no need for camera assistance. For robotic tasks, the dVSSS was used.
The dVSSS recorded all parameters autonomously; conventional laparoscopy performance was documented by two doctoral candidates (J.C. and C.K.) after each task. The process was continuously supervised by experienced research team members. Additionally, to count the touches in ‘Rollercoaster 1’ with the laparoscopy trainer, a device was developed that counted the touches automatically with registration of electric contact. The registered parameters are described in Figure 2.
Statistics
The data were analyzed using a combination of statistical software, including IBM SPSS Statistics 2730 and AMOS31, as well as the Python packages semopy for conducting SEM and shap for generating SHapley Additive exPlanations (SHAP) values based on machine learning techniques.
Latent prediction models based on structural equation modeling
SEM enables the investigator to examine relationships among different factors composed of several variables, constituting so-called latent constructs32. Latent constructs are characteristics estimated by single measured variables serving as indicators of the respective construct33. We used SEM to scrutinize the influence of the three latent constructs – motivation, psychomotor skills, and personality traits – on surgical performance in our training setting. Sex, age, and previous experience with the training set-up were included to avoid any bias. We applied the following model exclusion criteria in the SEM analyses: (a) failure to converge after 240 iterations, (b) a parsimonious goodness of fit (PGFI) of 0.10, (c) a squared multiple correlation exceeding 1, (d) a probability of close fit p0.05, which includes a root mean squared error of approximation (RMSEA) significantly differing from 0, and (e) reconstruction errors (values other than 1 along the correlation matrix diagonal). We then ranked the models from lowest to highest RMSEA, the highest to lowest goodness of fit (GFI), including more conservative adjusted GFI (AGFI) and PGFI estimates.
Importance level identification of single variables based on machine learning
We generated SHAP (Shapley Additive exPlainations) values using a machine learning approach in Python (SHAP library) to identify how each of the single variables, in contrast to latent constructs like in SEM, are related to the training performance in both students and physicians. For this value generation, first, we preprocessed the data by standardizing the continuous variables and one-hot encoding the categorical variables. We then trained a Random Forest Regressor model, selected for its effectiveness in handling regression tasks. Configured with 1000 decision trees, the model was trained using 70% of the provided data to learn the relationships between predictors and outcomes and the hyperparameters were tuned using cross-validation. After training, the model made predictions on a separate 30% of the data, serving as a test set to evaluate its performance. To quantify prediction accuracy, we computed the absolute errors between the predicted and actual values. The Mean Absolute Error (MAE) provided an overall measure of prediction error. Assessing accuracy, we utilized the Mean Absolute Percentage Error (MAPE) to assess the model’s performance in predicting the training performance of students and physicians. The model achieved an accuracy of 80.12% for students and 73.28% for physicians. Once the model was trained, we used the optimized model to generate SHAP values for each feature (variable) in the testing data via the SHAP package in Python. This allowed us to explain the contribution of each feature to the predicted outcome of the model. One of the key benefits of SHAP values is that they provide a way to decompose the prediction of a complex model into simple additive components. Combined approach of the Random Forest Regressor model with SHAP analysis allowed testing the importance of single variables in predicting training performance. For visualization of the SHAP values, we used summary plots and individual contribution plots to gain insight into the importance of each feature and to identify any nonlinear relationships or interactions that may have been missed by more traditional statistical techniques.
Results
Participants and demographic data
Overall, n=323 (203 female) persons participated in the trial. Of these, 237 were designated as students. These were individuals with undergraduate degrees, equivalent qualifications, or lower levels of education. The remaining 86 participants were classified as physicians and possessed a master’s degree, equivalent qualifications, or higher levels of education, and were in different stages of their medical career. The study population and their demographics are shown in Table 1.
Table 1.
Demographic data.
| Overall | Studentsa | Physiciansb | |
|---|---|---|---|
| Participants [n] | 323 | 237 | 86 |
| Female | 203 (62.8) | 146 (61.6%) | 57 (66.3%) |
| Male | 120 (37.2%) | 91 (38.4%) | 29 (33.7%) |
| Mean age [years (± SD)] | M=28.13, SD=5.39 | M=25.87, SD=3.05 | M=34.35, SD=5.55 |
| Training starts with [n] | |||
| Conventional laparoscopy | 131 (40.6%) | 99 (41.8%) | 32 (37.2%) |
| dVSSS | 192 (59.4%) | 138 (58.2%) | 54 (62.8%) |
Level of education: undergraduate degree, equivalent, or less).
Level of education: master’s degree, equivalent, or higher).
Surgical training performance
All of the attendees improved their surgical performance in the course of the training sessions. The learning curve is shown in Figure 3.
Figure 3.
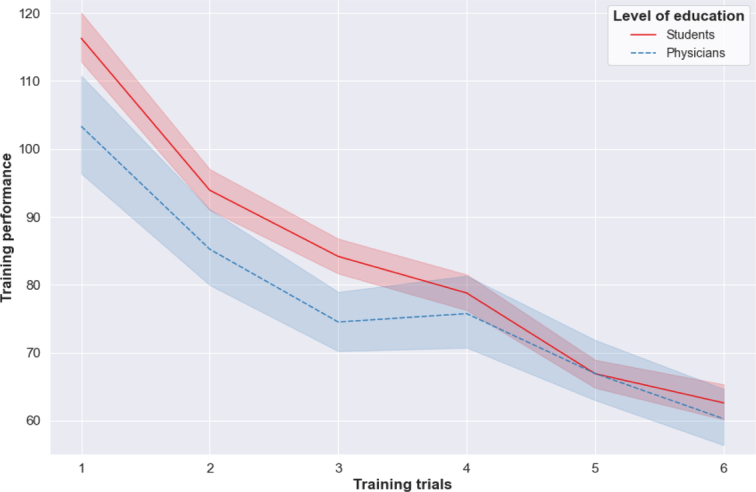
Learning curve.
Latent prediction models based on structural equation modeling
The model of surgical performance for students, based on three latent factors, that is, motivation, personality, and psychomotor skills, revealed a normed fit index (NFI) of 0.334 and a comparative fit index (CFI) of 0.365. The latent factors of motivation (explained variance, 8.4%; R2=0.109; R2 corrected=0.84), personality (explained variance, 4.5%; R2=0.074; R2 corrected = 0.045), and psychomotor skills (explained variance, 1.1%; R2=0.042; R2 corrected=0.011) are weighted differently, with motivation and personality contributing most to the students’ surgical training performance. There is strong evidence that the model fits the data well (adjusted R2=0.082). The model of the students’ cohort is shown in Figure 4.
Figure 4.
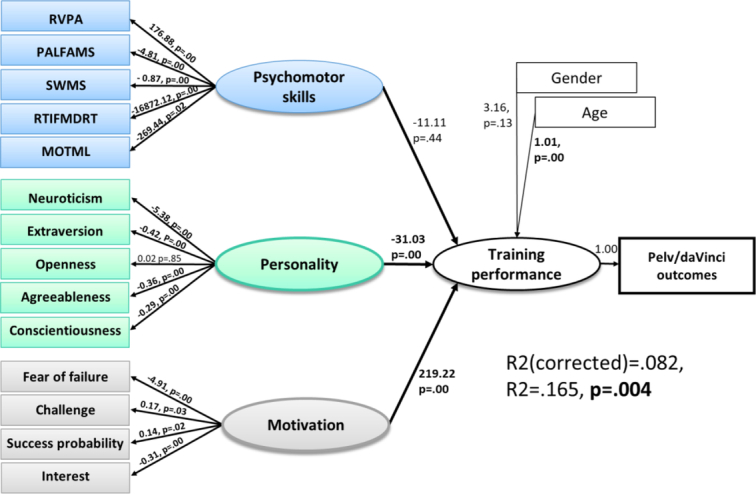
Structural equation model (SEM) in Students. Note: The training performance of students was tested for its prediction by the latent constructs psychomotor skills, personality, and motivation, and the covariates of sex and age, using an SEM approach. Psychomotor skills were modeled as being constituted by the variables visual information processing (RVPA), learning-based memory (PALFAMS), spatial working memory (SWMS), reaction time capabilities (RTIFMDRT), and motor response capabilities (MOTML). Personality was modeled as being constituted by neuroticism, extraversion, openness, agreeableness, and conscientiousness. Motivation was modeled as being constituted by fear of failure, challenge, probability of success, and interest [P<0.05].
The model of surgical performance of physicians based on three latent factors – motivation, personality, and psychomotor skills – revealed a normed fit index (NFI) of 0.404 and a comparative fit index (CFI) of 0.510. The latent factors of motivation (explained variance, 2.3%; R2=0.052; R2 corrected=0.023), personality (explained variance, 10.5%; R2=0.181; R2 corrected=0.105), and psychomotor skills (explained variance, 27.4%; R2=0.339; R2 corrected=0.274) are weighted differently, with psychomotor skills contributing the most to physicians’ surgical training performance. There is strong evidence that the model fits the data well: the adjusted R2=0.238 indicated a relatively high proportion of explained variance (Fig. 5).
Figure 5.
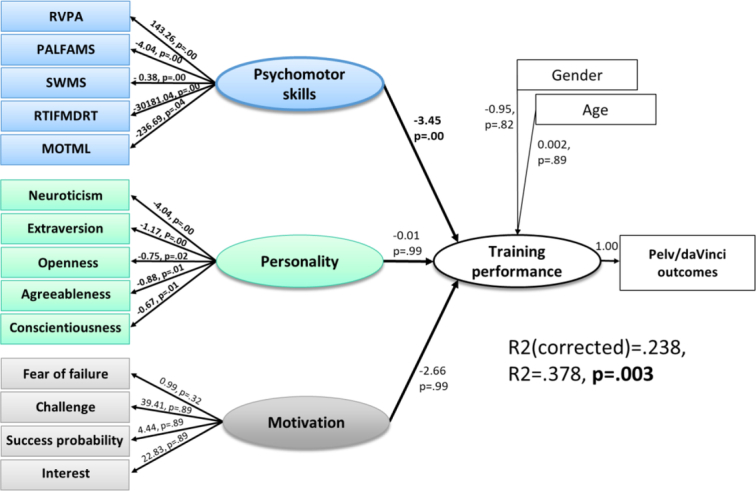
Structural Equation Model (SEM) in Physicians. Note: The training performance of physicians was tested for its prediction by the latent constructs psychomotor skills, personality, and motivation, and the covariates of gender and age, using an SEM approach. Psychomotor skills were modeled as being constituted by the variables visual information processing (RVPA), learning-based memory (PALFAMS), spatial working memory (SWMS), reaction time capabilities (RTIFMDRT), and motor response capabilities (MOTML). Personality was modeled as being constituted by neuroticism, extraversion, openness, agreeableness, and conscientiousness. Motivation was modeled as being constituted by fear of failure, challenge, probability of success, and interest [P<0.05].
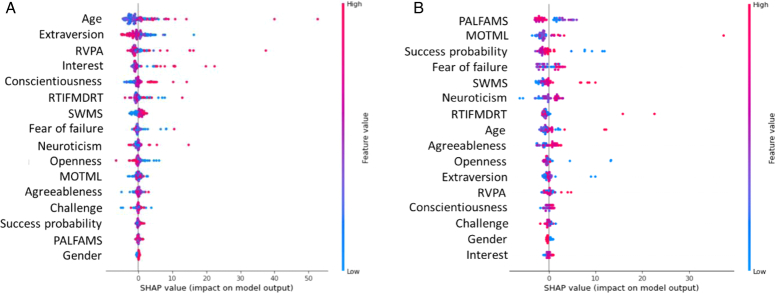
Importance levels of single variables based on machine learning
Machine learning was used to determine the individual contributions of the predictor variables for good surgical performance, indicated by SHAP values. The most important features for students were age and the personality trait of extraversion (Fig. 6a), while the foremost features for physicians (Fig. 6b) were the psychomotor skills of learning-based memory and motor response capabilities.
Figure 6.
Summary plot of the distribution of SHAP values for each variable across the entire dataset to identify the most important single variables for the prediction of training performance. (A) SHapley Additive exPlanations (SHAPs) in the student sample. (B) SHAPs in the physician sample. SHAP values constitute the contribution of each of the single variables related to psychomotor skills, personality, and motivation to the prediction of training performance. A positive SHAP value (in pink) indicates that the variable increases training performance, while a negative value indicates that the variable reduces training performance. The magnitude of the SHAP values reflects the strength of the respective variable’s influence on training performance, reflected also by the order of the variables, indicating their impact on prediction – a higher order signifies a greater contribution. [MOTML, motor-screening task - mean latency; PALFAMS, paired associates learning – first attempt memory].
Discussion
In this randomized, crossover training setting, structural equation modeling showed a significant contribution of psychomotor skills, motivation and personality to the surgical training performance of both students and physicians. Interestingly, while the significant driving forces in students were motivation and personality, the significant driving force in physicians was psychomotor skills. With regard to the order of importance of the variables, the most important variables for students were age and the personality trait of extraversion, while the most important variables for physicians were the psychomotor skills of learning-based memory and motor response capabilities. These outcomes show that the early stages of the surgical training process are sensitive to, and fragile in regard of nonsurgery-related general individual traits such as personality and motivation: While the level of psychomotor skills plays a minor role in students, personality traits and the level of motivation in surgical trainees are the driving forces for achieving good results in training tasks. This is confirmed by the proportion of explained variance, which differed markedly between students (8.2%) and physicians (23.8%). It also emphasizes the effectiveness of continuous training and the fact that, in this fragile period of study, many other factors might come into play. Those could be the well-known factors of medical rationale and technical approaches, but also additional individual characteristics. Future studies should be focused on the above mentioned aspects and also include longitudinal investigations to yield an exhaustive battery of tests for surgical aptitude in the respective structural setting.
In a meta-analysis by Kramp et al.34, only two psychomotor abilities were associated with performance in laparoscopy35,36. In a systematic review, M. El Boghdady and B. M. Ewalds-Kvist investigated the effect of ‘innate aptitude’ in the form of visuospatial, psychomotor, and manual manipulative skills on the performance of surgical tasks11. Medical students with low ‘innate aptitude’ were unable to achieve the skills needed for a competent career in surgery. Therefore, the authors concluded that training cannot compensate for deficiency in certain skills needed for laparoscopy11. However, the ‘soft skills’ personality and motivation have not been tested for potential relations and contributions. While our findings demonstrated the significant role of psychomotor skills in surgical training performance, this was the driving force only for experienced surgeons. For students, the key factors of successful training performance were personality and motivation. This suggests that surgical aptitude involves more than visuospatial, psychomotor, or manipulative skills, and that the constitution of this aptitude changes during the training process: it is strongly correlated with surgical experience.
Currently, we have a large variety of training curricula for laparoscopy in various specialties all over the world. While most of them have not yet been validated, a small number of comprehensive evidence-based curricula have been developed37. Training curricula contain technical skill components with different training methods including box trainers, virtual reality trainers, or animal models. Some of these also include cognitive components37,38. Our results highlight the importance of incorporating additional factors such as personality traits and motivation in future training curricula. This might include the assessment of motivation by the use of appropriate methods before training sessions or even efforts to increase motivation before training courses, such as the stimulation of curiosity39, prospects of reward, or setting individual goals for the attendees40. In addition, emphasizing the value of educational activity and letting the trainees select their own strategies might be useful41, especially if these enhance their motivation for the training per se.
While personality assessments in medical education have been suggested as a means of improving the core of the medical profession, namely the physician-patient relationship42, our data highlight the importance of personality facets for surgical training and performance. Thus, the advancement of a training curriculum may well include individual adjustment, such as intensifying the training in the nonclinical environment of a simulator or virtual reality training before proceeding to in vivo surgery, especially when personality factors like neuroticism are prominent. As in sports, where athletes need to show a greater likelihood for risk events and lower risk perception43, specific personality traits may help surgeons to achieve better performance during the first years of their training. It also could reduce the duration of training for some other surgeons. The evaluation of personality traits within training curricula seems to be useful for this purpose. Considering these coherences, early surgical training seems to increasingly important in the medical education system. The strong influences of nonsurgical related traits of the early training phases probably could so be reduced over time to eventually reach a setting where psychomotor skills get in the focus for achievement of high surgical performance. Also, a checkup of psychomotor skills levels within the course of medical school or training curricula could be considered, since these appear to be the central correlate for high surgical performance in trained surgeons. Finally, training of specific psychomotor skills outside the operation theater or surgical training simulators could be a possibility, especially when these are low in the beginning in some individuals.
With the presented study we could provide robust and representative data fulfilling the high requirements for advanced statistical analysis, especially in relation to cohort sizes of some of the preceding studies on this topic35,44. Scientific investigation and collection of further data, combined with the use of well-fitting methods such as SEM and machine learning to meet the requirements of well-conceived data analysis for complex coherences between heterogeneous factors appear vital, not least because there may be hitherto unknown factors that strongly influence surgical education. Therefore, future studies should be conducted on this topic. These could focus on first-year or second-year residents or even better be carried out in a longitudinal assessment with another evaluation after several years of surgical training. Investigations on the impact of training of specific psychomotor skills beyond surgical training environment also seem to be of high interest for optimization of training modalities. Since the differences in training of conventional or robotic laparoscopy still remain unclear, future studies should also target this issue.
Limitations
The SEM approach is a reasonable method for prediction modeling in complex coherences in the neurosciences and psychology. However, since the current data stem from a cross-sectional design, future studies should also be based on a longitudinal approach to assess trajectories over the surgeons’ complete process of learning and their development. A further limitation was that the test setting was very brief. Nevertheless, the explained variances in the calculated SEM were relatively high. Finally, there is inconsistent evidence of the possibility of skill transfer between conventional and robotic training methods45. Therefore, and to incorporate the wide spectrum of laparoscopic surgery that most modern surgeons are confronted with, performance measures from both methods were summarized. Further research will be needed to assess, in detail, the interrelationships of training and the application of surgical techniques.
Conclusion
The study showed that the early stages of surgical training are sensitive to, and fragile in regard of nonsurgery-related general individual traits such as personality and motivation. The investigation underlined the effectiveness of continuous training, and supports early implementation of surgical training in medical education. Future studies should elaborate on those aspects, including longitudinal investigations and the interrelationships between robotic and conventional techniques.
Ethical approval
The study was approved by the ethics committee of the University Clinic of Kiel (D 448/21).
Consent
The study was approved by the responsible ethics committee. Written informed consent was obtained from the volunteers for publication of this report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
The provision of training tools and aids was supported financially by the faculty through an innovative teaching fund. We acknowledge financial support by DFG within the funding programme Open Access-Publikationskosten.
Author contribution
Z.R., J.P., I.A., and F.N.: conceptualization; F.N., I.A., L.M., N.M., and L.A.: methodology; N.M., F.N., and I.A.: administration; F.N., S.S., and K.J.: software; V.G., J.A., L.M., L.A.: validation; S.S. and K.J.: formal analysis; J.-S.C., C.K., J.P., J.A., and V.G.: investigation; I.A. and F.N.: resources; J.-S.C. and C.K.: data curation; Z.R., J.P., K.J., and S.S.: writing – original draft; I.A., F.N., and N.M.: Writing – review and editing; K.J. and S.S.: visualization; I.A., F.N., N.M., and L.M.: supervision; I.A., N.M., and F.N.: project administration; Z.R. and I.A.: funding acquisition.
Conflicts of interest disclosure
The author declares no conflict of interest.
Research registration unique identifying number (UIN)
As the study did not fulfill the National Institutes of Health definition of Clinical Trials 3, no trial registration was performed.
Guarantor
I. Alkatout and F. Nees.
Data availability statement
The data are available on request.
Provenance and peer review
Not applicable.
Footnotes
Zino Ruchay, Julian Pape, Frauke Nees, and Ibrahim Alkatout contributed equally to this manuscript.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 9 May 2024
Contributor Information
Zino Ruchay, Email: zino.ruchay@uksh.de.
Julian Pape, Email: julianmaria.pape@uksh.de.
Julia-Sophie Cordt, Email: julia-s.cordt@gmx.de.
Carolina Kerres, Email: c.kerres@hotmail.com.
Sebastian Siehl, Email: siehl@med-psych.uni-kiel.de.
Karina Jansone, Email: karina.jansone@zi-mannheim.de.
Johannes Ackermann, Email: johannes.ackermann@uksh.de.
Veronika Guenther, Email: Veronika.Guenther@uksh.de.
Liselotte Mettler, Email: profmettler@gmx.de.
Leila Allahqoli, Email: lallahqoli@gmail.com.
Nicolai Maass, Email: nicolai.maass@uksh.de.
Frauke Nees, Email: nees@med-psych.uni-kiel.de.
Ibrahim Alkatout, Email: Ibrahim.Alkatout@uksh.de.
References
- 1. Singletary SE. A fire in our hearts: passion and the art of surgery. Ann Surg Oncol 2010;17:364–370. [DOI] [PubMed] [Google Scholar]
- 2. European flight academy. https://www.european-flight-academy.com/en/selection-process
- 3. Bailey M. Evolution of Aptitude Testing in the RAF, RTO MP-55 1999. https://apps.dtic.mil/sti/pdfs/ADP010369.pdf
- 4. Nance JJ. Why Hospitals Should Fly: The Ultimate Flight Plan to Patient Safety and Quality Care. Second River Healthcare Press; 2008:225. [Google Scholar]
- 5. Baum P, Diers J, Lichthardt S, et al. Mortality and complications following visceral surgery: a nationwide analysis based on the diagnostic categories used in German Hospital invoicing data. Dtsch Arztebl Int 2019;116:739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang D, Gu D, Rao C, et al. Outcome differences between surgeons performing first and subsequent coronary artery bypass grafting procedures in a day: a retrospective comparative cohort study. BMJ Qual Saf 2023;32:192–201. [DOI] [PubMed] [Google Scholar]
- 7. Ackermann J, Pahls J, Baumann J, et al. The pelvitrainer for training in laparoscopic surgery - a prospective, multicenter, interdisciplinary study: experimental research. Int J Surg 2022;101:106604. [DOI] [PubMed] [Google Scholar]
- 8. Alkatout I, Dhanawat J, Ackermann J, et al. Video feedback and video modeling in teaching laparoscopic surgery: a visionary concept from Kiel. J Clin Med 2021;10:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ackermann J, Baumann J, Pape J, et al. Factors influencing surgical performance and learning progress in minimally invasive surgery - results of an interdisciplinary muticenter study. Int J Surg 2023;109:2975–2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Louridas M, Szasz P, de Montbrun S, et al. Can we predict technical aptitude?: a systematic review. Ann Surg 2016;263:673–691. [DOI] [PubMed] [Google Scholar]
- 11. El Boghdady M, Ewalds-Kvist BM. The innate aptitude’s effect on the surgical task performance: a systematic review. Updates Surg 2021;73:2079–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Teunis T, Janssen SJ, Guitton TG, et al. Surgeon personality is associated with recommendation for operative treatment. Hand (N Y) 2015;10:779–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moug SJ, Henderson N, Tiernan J, et al. The colorectal surgeon’s personality may influence the rectal anastomotic decision. Colorectal Dis 2018;20:970–980. [DOI] [PubMed] [Google Scholar]
- 14. Hughes BD, Perone JA, Cummins CB, et al. Personality testing may identify applicants who will become successful in general surgery residency. J Surg Res 2019;233:240–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moorthy K, Munz Y, Sarker SK, et al. Objective assessment of technical skills in surgery. BMJ 2003;327:1032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ioannidis JP. Why most published research findings are false. PLoS Med 2005;2:e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Button KS, Ioannidis JP, Mokrysz C, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci 2013;14:365–376. [DOI] [PubMed] [Google Scholar]
- 18. Bellazzi R, Zupan B. Predictive data mining in clinical medicine: current issues and guidelines. Int J Med Inform 2008;77:81–97. [DOI] [PubMed] [Google Scholar]
- 19. Rheinberg F, Vollmeyer R, Burns B. QCM: A questionnaire to assess current motivation in learning situations. Diagnostica 2001;47:57–66. [Google Scholar]
- 20. Atkinson JW. Motivational determinants of intellective performance and cumulative achievement In: Atkinson JW, Raynor JO, editors. Motivation and achievement. Winston; 1974:389–410. [Google Scholar]
- 21. Bloom BS. Individuelle Unterschiede in der Schulleistung: ein überholtes Problem? In: Edelstein W, Hopf D, editors. Bedingungen des Bildungsprozesses. Klett; 1973:251–284. [Google Scholar]
- 22. Heller KA. Schuleignungsprognostik In: Heller KA, editor. Begabungsdiagnostik in der Schul- und Erziehungsberatung. Huber; 1991:213–235. [Google Scholar]
- 23. Helmke A, Weinert FE. Bedingungsfaktoren schulischer Leistungen In: Weinert FE, editor. Enzyklopädie der Psychologie Serie Pädagogische Psychologie, Bd 3: Psychologie des Unterrichts und der Schule. Hogrefe; 1997:71–176. [Google Scholar]
- 24. South SC, Jarnecke AM. Structural equation modeling of personality disorders and pathological personality traits. Personality Disorders: Theory, Research, and Treatment. 2017;8:113–29. [DOI] [PubMed] [Google Scholar]
- 25.https://www.cambridgecognition.com/what-we-do/gold-standard-cognitive-research/ Cambridge Cognition Limited ©. 2022.
- 26. Schatz P, Browndyke J. Applications of computer-based neuropsychological assessment. J Head Trauma Rehabil 2002;17:395–410. [DOI] [PubMed] [Google Scholar]
- 27. Costa P, McCrae R. Neo PI-R professional manual. Psychol Assessm Res 1992;396:223–256. [Google Scholar]
- 28. Paul Costa RRM, Jr. The NEO-PI/NEO-FFI manual supplement. Psychological Assessment Resources; 1989. [Google Scholar]
- 29. Borkenau P, Ostendorf F. NEO-Fünf-Faktoren-Inventar (NEO-FFI) nach Costa und McCrae (Handanweisung). Hogrefe; 1993. [Google Scholar]
- 30. IBM Corp . IBM SPSS Statistics for Windows. IBM CorpReleased; 2020. Version 27.0. [Google Scholar]
- 31. Arbuckle JL. IBM SPSS Amos (Version 260) [Computer Program]. IBM; 2019. SPSS2019. [Google Scholar]
- 32. Deng L, Yang M, Marcoulides KM. Structural equation modeling with many variables: a systematic review of issues and developments. Front Psychol 2018;9:580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Galbraith JI, Moustaki I, Bartholomew D, et al. The Analysis and Interpretation of Multivariate Data for Social Scientists 2002.
- 34. Kramp KH, van Det MJ, Hoff C, et al. The predictive value of aptitude assessment in laparoscopic surgery: a meta-analysis. Med Educ 2016;50:409–427. [DOI] [PubMed] [Google Scholar]
- 35. Stefanidis D, Korndorffer JR, Jr, Black FW, et al. Psychomotor testing predicts rate of skill acquisition for proficiency-based laparoscopic skills training. Surgery 2006;140:252–262. [DOI] [PubMed] [Google Scholar]
- 36. Nugent E. The evaluation of fundamental ability in acquiring minimally invasive surgical skill sets. Royal College of Surgeons in Ireland. Thesis. Acessed 29 June 2023. 10.25419/rcsi.10815617.v1 [DOI]
- 37. Palter VN. Comprehensive training curricula for minimally invasive surgery. J Grad Med Educ 2011;3:293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Stefanidis D, Heniford BT. The formula for a successful laparoscopic skills curriculum. Arch Surg 2009;144:77–82. [DOI] [PubMed] [Google Scholar]
- 39. Halamish V, Madmon I, Moed A. Motivation to learn. Exp Psychol 2019;66:319–330. [DOI] [PubMed] [Google Scholar]
- 40. Morris LS, Grehl MM, Rutter SB, et al. On what motivates us: a detailed review of intrinsic v. extrinsic motivation. Psychol Med 2022;52:1801–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pelaccia T, Viau R. Motivation in medical education. Med Teach 2017;39:136–140. [DOI] [PubMed] [Google Scholar]
- 42. Suciu N, Meliț LE, Mărginean CO. A holistic approach of personality traits in medical students: an integrative review. Int J Environ Res Public Health 2021;18:12822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Guo C, Xiao B, Zhang Z, et al. Relationships between risk events, personality traits, and risk perception of adolescent athletes in sports training. Int J Environ Res Public Health 2022;19:445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Buckley CE, Kavanagh DO, Nugent E, et al. The impact of aptitude on the learning curve for laparoscopic suturing. Am J Surg 2014;207:263–270. [DOI] [PubMed] [Google Scholar]
- 45. Chahal B, Aydin A, Amin MSA, et al. Transfer of open and laparoscopic skills to robotic surgery: a systematic review. J Robot Surg 2023;17:1207–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available on request.