Abstract
Background
Approximately 15% of women in low-and middle-income countries experience common perinatal mental disorders. Yet, many women, even if diagnosed with mental health conditions, are untreated due to poor quality care, limited accessibility, limited knowledge, and stigma. This paper describes how mental health-related stigma influences pregnant women’s decisions not to disclose their conditions and to seek treatment in Vietnam, all of which exacerbate inequitable access to maternal mental healthcare.
Methods
A mixed-method realist study was conducted, comprising 22 in-depth interviews, four focus group discussions (total participants n = 44), and a self-administered questionnaire completed by 639 pregnant women. A parallel convergent model for mixed methods analysis was employed. Data were analyzed using the realist logic of analysis, an iterative process aimed at refining identified theories. Survey data underwent analysis using SPSS 22 and descriptive analysis. Qualitative data were analyzed using configurations of context, mechanisms, and outcomes to elucidate causal links and provide explanations for complexity.
Results
Nearly half of pregnant women (43.5%) would try to hide their mental health issues and 38.3% avoid having help from a mental health professional, highlighting the substantial extent of stigma affecting health-seeking and accessing care. Four key areas highlight the role of stigma in maternal mental health: fear and stigmatizing language contribute to the concealment of mental illness, rendering it unnoticed; unconsciousness, normalization, and low literacy of maternal mental health; shame, household structure and gender roles during pregnancy; and the interplay of regulations, referral pathways, and access to mental health support services further compounds the challenges.
Conclusion
Addressing mental health-related stigma could influence the decision of disclosure and health-seeking behaviors, which could in turn improve responsiveness of the local health system to the needs of pregnant women with mental health needs, by offering prompt attention, a wide range of choices, and improved communication. Potential interventions to decrease stigma and improve access to mental healthcare for pregnant women in Vietnam should target structural and organizational levels and may include improvements in screening and referrals for perinatal mental care screening, thus preventing complications.
Keywords: Stigma, Maternal health, Realist evaluation, Disclosure, Health system responsiveness, Perinatal mental disorders, Vietnam
Background
Approximately 15% of women in low-and middle-income countries experience common perinatal mental disorders (CPMDs) antenatally and 20% postnatally [1]. CPMDs include depression, anxiety, and psychosis during pregnancy or in the first year of postpartum [2]. Risk factors include a history of illness, significant life stressors, poor marital relationships, and poor social support [3, 4]. These CPMDs can significantly impact the mother including various aspects of mother’s lives (obstetrics outcomes such as preterm birth and low birth weight, preterm delivery and economic outcomes [5, 6] and have long-lasting consequences on the child’s brain development and birth weight, impairing growth and increasing infection susceptibility [6–9]. Yet, many women, even if diagnosed with mental health conditions, are untreated due to poor quality care, limited accessibility, limited knowledge, and stigma [10].
Stigma, a key neglected and under-researched barrier to accessibility of care, refers to problems of knowledge (ignorance), attitudes (prejudice) and behaviour (discrimination) [11]. Stigma related to mental health is universal, extending across cultures [10]. This includes stigma by association, which is the attribution of stereotypes and discrimination against family members or mental health workers. Stigma threatens well-being and health through adverse impacts on mental healthcare seeking, utilization, and health outcomes [12]. Stigma operates across micro and meso contexts of health services delivery in some illnesses such as mental conditions and infectious diseases, thus affecting the ability of a health system to be responsive – “…being cognisant and respond appropriately to the universally legitimate expectations of individuals” ([13] p.3) – constraining interactions between policymakers, managers, and services providers [14]. Different manifestations of stigma prevent individuals from seeking help and formal health care [15–20]. However, the specific impacts of stigma can vary across illnesses and cultural contexts [18, 21] and its intersections with ethnicity, gender, disability and class [18, 19].
The Government of Vietnam approved the National Strategy on People’s Care and Protection (2001, 2011 to 2020 and the vision towards 2030) with a commitment to ensuring access to essential health services to promote good physical and mental health. Vietnam also endorsed the WHO Mental Health Action Plan 2013–2020 and, in 2015, ratified the United Nations Convention on the Rights of Persons with Disabilities, committing to the fundamental human rights of citizens with disabilities, including those with mental conditions [22]. Although the government has attempted to establish community-based mental healthcare since 1998, mental healthcare in Vietnam still has a narrow focus on severe conditions (e.g. schizophrenia), with no integration of mental health at the primary care level and limited funding [16]. Arguably, this further contributes towards the structural stigmatisation of individuals with mental health illnesses.
The prevalence of CPMDs in Vietnam ranges from 16.9% to 39.9% [8, 23–25]. Most of the existing research has concentrated on the causes of CPMDs, such as intimate partner violence, emotional abuse, and both physical and sexual violence. These studies have noted an increase in symptoms of CPMDs among women during and after pregnancy [24, 26–28]. Despite this, there has been a noticeable gap in the literature regarding the effects of mental health-related stigma on the likelihood of pregnant women to seek out healthcare services. Furthermore, the voices, and perspectives of these pregnant women and healthcare stakeholders concerning the healthcare system remain largely unexplored. In this paper, we bridge this knowledge gap by exploring both the impact of stigma on pregnant women's engagement with the healthcare system and the perceptions of the system held by these women and healthcare providers.
This paper contributes to the current literature on mental health-related stigma through reporting results from a mixed-methods realist study [29] examining how pregnant women with mental health conditions interact with the Vietnamese health system. Additionally, it increases understanding of the crucial contextual factors that enable or constrain those interactions, while providing a theoretically-based explanation of aspects of the system that impacted women’s help-seeking behavior across individual, organisational, and societal levels. Moreover, this paper responds to the call for evidence on health systems barriers to achieve health equity on underserved populations such as young women from low-and-middle income countries [30]. It is anticipated that this study will hold significant interest and relevance for policymakers, practitioners, and academics dedicated to advancing knowledge about and combating stigma associated with perinatal mental health at primary healthcare facilities. Ultimately, this will enhance health systems responsiveness to maternal mental health needs in Vietnam and other similar low-and middle-income countries.
Methods
This paper reports phase one Vietnam findings of a collaborative three-phase realist evaluation of health system responsiveness to the maternal mental health needs in Vietnam and Ghana [30]. Phase one focused on understanding the local context of maternal mental healthcare provision and utilisation. In Phase two and three an intervention to improve system responsiveness was co-produced with the local stakeholders in Vietnam and Ghana and evaluated.
Realist evaluation is a theory-driven methodological approach that focuses on understanding what works, how it works, under what conditions, and for whom it works. It does so by analysing causal pathways through the context-mechanism-outcome configurations (CMOs). Context encompasses the conditions surrounding programs, including political and economic conditions, cultural norms, and beliefs. Mechanisms involve the reasoning process through which individuals interpret and respond to programs or interventions within their specific context, as well as their interaction with available resources. Outcomes are the patterns of intended and unintended consequences resulting from mechanisms triggered in varying contexts [31–33]. Realist evaluations work with program theories (hypotheses about how programs are supposed to work) at their centre, typically including phases of theory gleaning, development, testing, refining and consolidation [30].
In our study, iterative rounds of literature reviews were conducted from June 2020 to November 2022 to identify and examine empirical studies on health systems responsiveness and the policies on maternal and mental health in Vietnam. The survey and qualitative data collection took place from April to October 2022, and it aimed to refine the initial hypotheses (program theories) inferred from the reviews. The researchers engaged in regular discussions throughout the process, and a stakeholder workshop was organized in November 2022 to review the initial findings.
Study setting
Bac Giang province was purposively selected to facilitate the inclusion of urban and rural communities. Situated in Northeast Vietnam in the Red River Delta region, it has approximately two million inhabitants across ten districts and 209 communes. The province’s industrial zones are rapidly developing, attracting migrants from neighboring provinces [34]. Two districts were purposely selected to represent urban and rural settings (population of each district is about 240,000 inhabitants, the urban district is 300 km square while the rural district is 600 km square), within each district, three communes were randomly selected to ensure participant heterogeneity for the development our program theory and intervention design.
Data collection
Data was collected using quantitative and qualitative methods. For quantitative part, we recruited all pregnant women who were above 12 weeks gestation, were living within the study area from June–September. Lists of pregnant women in each commune were provided by local commune health centers. A self-administrated questionnaire comprising basic demographic information and four items assessing attitudes towards mental health illness was administered to 639 pregnant women from six random communes of two selected districts (commune is a local sub-district tier of Vietnamese health system) in Bac Giang province. Women self-administer the paper-based questionnaireat their homes, under the supervision of the researchers. The aim to understand their views on maternal mental health and the resulting health-seeking behaviors. The items were adopted from the Mental Health Literacy Scale of O’Connor et al. [35], translated and culturally adapted in Vietnam [36]. Items are rated on a 5-point Likert scale, ranging from “very likely” to “very unlikely”.
The qualitative data collection included face-to-face in-depth interviews (IDIs n = 22) and focus group discussions (FGDs n = 4, each groups consisting of 5–6 persons and total participants of focus group discussion participants n = 22), with a total of 44 participants (Table 1). These were conducted with purposefully identified key health systems actors (policymakers, managers, providers, service users, and collaborators from community groups), using the realist interviewing technique [31–33].
Table 1.
Qualitative data collection
| Participants | Method | |
|---|---|---|
| Interviews | Focus Groups | |
| National level | 4 | |
| Policymakers on mental health services and maternal and child health care services at the Ministry of Health | 3 | |
| Mental health care provider | 1 | |
| Provincial level | 8 | |
| Health managers at the Centres for Disease Control and Prevention | 2 | |
| Health managers in the provincial obstetric gynaecology (OBGYN) public hospital, a private hospital, and a psychiatric hospital | 3 | |
| Health providers in the provincial public hospital, a private hospital, and a psychiatric hospital | 3 | |
| District and commune level | ||
| Health managers in district hospitals | 2 | |
| Health providers in district hospitals | 2 | |
| Health providers in commune health centers (2 groups, each group n = 5) | - | 10 (2 × 5) |
| Representative of Women Union, Youth Union, village health workers (Collaborators) (2 groups, each group n = 6) | - | 12 (2 × 6) |
| Pregnant women | 6 | |
| Total | 22 IDI | 4 FGDs [22 participants] |
| Overall number of participants | 44 | |
The qualitative data were collected using semi-structured topic guides designed to explore the initial program theories identified in the realist literature reviews conducted in parallel [30]. The topic guides were tailored to individual respondents and allowed for in-depth exploration of issues. The semi structured combines a pre-determined set of open questions (questions that prompt discussion) with the opportunity for the interviewer to explore particular themes or responses further. For instance, from healthcare providers, we sought insights on the structural and organizational levels of maternal mental healthcare provision and its management at health facilities. With pregnant women and community health workers, we focused on understanding their views on mental health issues, their experiences, and the healthcare seeking by pregnant women. Interviews and focus groups were conducted in Vietnamese, audio recorded, and lasted approximately 60 to 90 min. To ensure privacy and confidentiality, they were all held in a reserved place and were conducted by four experienced female researchers.
Data analysis
A parallel convergent model for mixed-methods analysis was used, with quantitative and qualitative data being collected simultaneously and analysed autonomously before being triangulated during the interpretation phase guided by our initial program theory (see Table 2).
Table 2.
Initial program theory guiding data collection
| IF in the communities and health facilities, there is low priority, low Mental Health (MH) literacy of Maternal Mental Health (MMH), strong stigma towards MH (reflected in shame, lack of support for MMH, hiding the MMH symptoms/cases), THEN there will be likely low demand to clinical care, delay to seeking/receiving care and adherence to clinical care, lack of support to MMH care. IF there is a lack of trust in clinical MMH services, lack of privacy and confidentiality services, beliefs on alternative care, IF there are barriers to access MMH (such as poverty, ethnicity, disadvantaged areas), lack of health insurance coverage for mental health services at Primary Health Care (PHC) level, THEN there will be likely low demand to clinical care, delay to seeking care, receiving care and adherence to clinical care, lack of support to MMH care. IF there are high risk groups to MMH (such as those suffering from miscarriage, in high-risk pregnancy, victim of violence), there will be likely high demand to clinical care, THEN the health workers will be likely to pay timely attention to these groups (thus addressing issues of communication, screening, counselling and referrals). |
Data were analyzed using the realist logic of analysis, an iterative process aimed at refining identified theories. Survey data underwent descriptive analysis with the support of SPSS 22. Descriptive analysis was used to describe the frequency distribution of pregnant women's perceptions of mental illness and stigma variable. The IDIs and FGDs were transcribed, and transcripts were initially coded for themes related to the program theory, with the support of NVIVO 11 and Mindjet Manager software [37]. To generate the initial codes, the research team commenced with themes according to Cook and colleagues (2014) framework on a multilevel approach to stigma and public health [38] and program theory guiding data collection. Qualitative data were further analyzed using realist context-mechanism-outcome configurations to elucidate causal links and provide explanations for complexity.
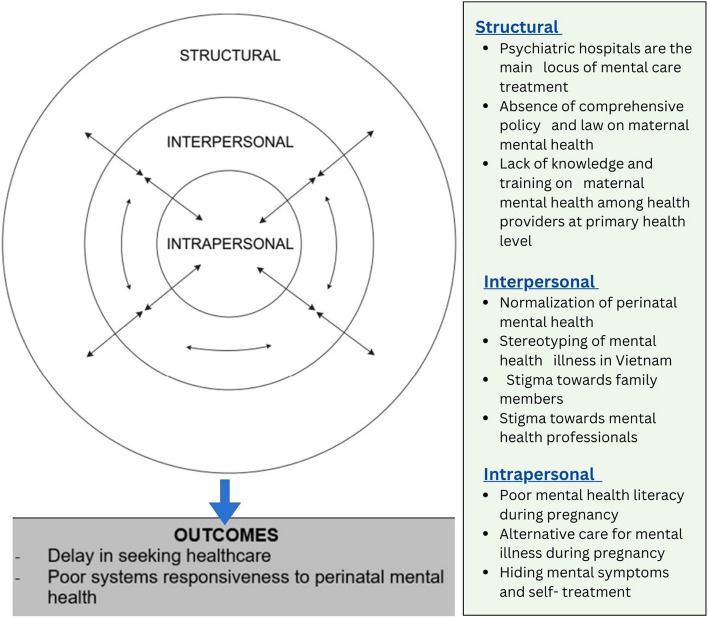
The revised program theory presented in this paper draws on Cook’s et al.’s stigma theory to elucidate how stigma influences interactions of pregnant women with mental health conditions with health services in Vietnam [38]. Cook et al. (2014) proposed that mental health-related stigma in healthcare operates across three interrelated levels: intrapersonal, interpersonal, and structural [38]. Intrapersonal stigma refers to the person’s values mindset, literacy level and resultant behaviors [38]. Interpersonal stigma extends to include prejudices against people facing stigma, their families, and professionals providing relevant services. Structural stigma encompasses health system-related factors contributing to stigma, including insufficient priority given to mental healthcare by policymakers and providers, limited staff expertise, inadequate care practices, and over-reliance on institutionalised care [18, 19, 38]. These three levels of stigma are interrelated and collectively influence stigma consequences, such as delays in health-seeking, self-treatment, pursuing of alternative care and, consequently, decreased health system responsiveness to perinatal mental health.
Results
Characteristics of participants involved in the quantitative study
Six hundred thirty-nine pregnant women were enrolled in the study. Participant characteristics by health facility are shown in Table 1. The largest age group was 25–29 (28.3%). The majority were of Kinh ethnicity (89.7%) and had no religion (90.9%). The majority of participants were factory workers (64.6%). More than half were in the second trimester (52.3%), about one-third in the third trimester (34.2%), and 13.5% in the first trimester. About 80% of women have an average income of 2–6 million VND (about 90 to 250 USD). Over a third had one child (35.4%), 28.8% were experiencing their first pregnancy, and few had more than three children.
Findings
Four key areas highlight the influence of stigma in maternal mental health: fear and stigmatizing language contribute to the concealment of mental illness, rendering it unnoticed; unconsciousness, normalisation and low literacy of maternal mental health; shame, household structure and gender roles during pregnancy; and the interplay of regulations, referral pathways, and access to mental health support services further compounds the challenges.
Understanding invisibility: Fear and stigmatizing language
Stigmatizing terminology in the Vietnamese constructs of mental health and illness differ from Western cultures conceptually and semantically. Conceptualization of psychiatric illness in traditional Vietnamese medicine is related to the blurring of psychic and physical health concepts in the term ‘tam than’ [39]. Mental illness, or ‘benh tam than’, is referred to as “madness” in Vietnamese, including severe psychiatric disorders such as schizophrenia. Benh tam than carries stereotyped connotations of wildness, unpredictability, and danger, often leading to avoidance and operating as a taboo word [40, 41]. There is a belief that ‘’madness’’ is a consequence of one’s improper behavior in a previous life, for which the person is now being punished [42]. This could explain why 28.8% of the pregnant women we surveyed considered people with mental illnesses to be dangerous (Tables 3 and 4). This was corroborated by a manager from a provincial centre for disease control who explained:
“Tâm thần” [mental health] means “điên” [madness]. This means a very severe condition; people have to go to a psychiatric hospital for treatment, so people are terrified. Folks called it “thần kinh” [madness]. This has been stigmatized and carries a bad reputation (CDC Manager).
Table 3.
Characteristics of pregnant women
| Characteristics | |
|---|---|
| Total | 639 (100%) |
| Age group | |
| 16–19 | 30 (4.7%) |
| 20–24 | 161 (25.2%) |
| 25–29 | 181 (28.3%) |
| 30–34 | 160 (25.0%) |
| 35- 43 | 107 (16.7%) |
| Marital status | |
| Unmarried/others | 27 (4.2%) |
| Married | 612 (95.8%) |
| Education | |
| Illiteracy /Primary | 19 (2.3%) |
| Secondary | 158 (24.7%) |
| High School | 336 (52.6%) |
| College + | 126 (19.8%) |
| Ethnicity | |
| Kinh | 573 (89.7%) |
| Others | 66 (10.3%) |
| Religion | |
| No | 581 (90.9%) |
| Yes | 58 (9.1%) |
| Occupation | |
| Farmer | 48 (7.5%) |
| Factory worker | 413 (64.6%) |
| Public officer | 42 (6.6%) |
| Freelancer | 111 (17.4%) |
| Others | 25 (3.9%) |
| Economic income | |
| < 2 VND mil/month | 87 (13.6%) |
| 2–4 VND mil/month | 374 (58.5%) |
| 4–6 VND mil/month | 131 (20.5%) |
| > 6 VND mil/month | 47 (7.4%) |
| Gestational age | |
| 1st trimester | 86 (13.5%) |
| 2nd trimester | 334 (52.3%) |
| 3rd trimester | 219 (34.2%) |
Table 4.
Survey of pregnant women's perceptions of mental illness and stigma
| Item | Mental health-related stigma | Number (N = 639] | Percent |
|---|---|---|---|
| 1 |
People with a mental illness are dangerous |
184 | 28.8 |
| 2 | It is best to avoid people with a mental illness so that you don't develop this problem | 244 | 38.2 |
| Hiding information on mental health-related illness | |||
| 1 | If I had a mental illness, I would not tell anyone | 278 | 43.5 |
| 2 | If I had a mental illness, I would not seek help from a mental health professional | 245 | 38.3 |
This stereotype has a long history and has profoundly impacted contemporary cultural beliefs on mental health illness [43]. To avoid the fear associated with mental health stigma, many people prefer to use other words “tinh than/mind” or “tam ly/ psychology” instead of “tam than/mental health”. This includes healthcare staff who are aware of the impact that these words may have on their clients, especially when the initial common mental health symptoms are normalized since they are not severe such as anxiety and stress, as explained by one of the district health providers we interviewed:
If that was the case, anxiety, stress, I think using the word “tam than” would be a little difficult. Using the words “tinh thần” or “tam ly” would be much better (District 2, Health Provider).
These connotations impact people’s interactions with mental health institutions as people also preferred to access the general hospital instead of the psychiatric hospital or the department named ‘psychology’ instead of ‘psychiatry’. Additionally, stigma by association expands not only to families but also to healthcare staff. Psychiatrists were referred to as bac si tam than, which means “doctors who treat madness”, which implies a dismissive attitude towards those entrusted to their care [44]. These perceptions shaped peoples’ attitudes toward mental health professionals. Psychiatrists often felt that they were looked down upon by other health staff and community members, leading them to conceal their employment at psychiatric hospitals:
Mental health is very stigmatized. The community does not only stigmatize people with mental health conditions but also health staff at provincial psychiatric hospitals. We state that we are doctors and nurses, but we will not confess that we work in psychiatric hospitals. Psychiatry does not receive respect from the community. Very few people want to learn this specialty. Our salary is very low, and because we meet psychiatric patients, people think we also will have psychiatric problems [laughed] (Provincial Mental Hospital Manager).
This central manager also corroborated plans to change the name of the psychiatric hospital to mental health hospital to avoid misunderstanding and stigma towards mental health.
In summary, using stigmatizing language contributed to public stigma—stereotypes, attitudes, and discrimination towards the stigmatized group [45]—and the concealment and invisibility of mental health conditions.
Unconsciousness, normalisation and low literacy of maternal mental health
Alongside language barriers, religious and societal beliefs, such as Confucianism and Buddhism, influence Vietnamese perceptions of mental health, due to their holistic view of the mind–body relationship. In this perception, psychological disturbance was often associated with physical disruptions, differing from the typology of independent mental disorders found in Western psychiatry [46]. Mental health-related conditions during pregnancy such as anxiety and stress were considered natural phenomena [39] by both healthcare staff and women participants. These mild symptoms could be overcome after pregnancy and thus were often overlooked contributing to women’s delayed help-seeking. This view is illustrated by this quote from one of the health managers we interviewed:
Anxiety and stress during pregnancy are mainly due to hormonal changes and other vulnerabilities such as family conflict, financial difficulties, etc. Therefore, we mostly focus on physical condition and skip other conditions (Central Manager).
The tendency to normalize mental health problems as being temporary (linked to the hormone cycle during pregnancy) is a possible explanation for the underutilization of mental health services. Nevertheless, in our study, women who experienced perinatal mental health conditions described common symptoms including anxiety, low mood, and behavioral changes such as irritability, sleep, and eating disorders [46–48]. Most women experienced these symptoms during pregnancy only and did not relate them to a mental health condition. This unperceived health need was also noted by one of the village health workers reflecting on her own experience of pregnancy and her mental health:
When I was pregnant, I didn't understand why I was so hot-tempered. No matter what anyone said to me, no matter how small it was, I felt furious. Meanwhile, even though my family was very comforting, I still couldn’t help but feel anxious, restless, and very uncomfortable. At that time, I got angry very easily. Before getting pregnant, I never got angry about those things. But when I was pregnant, my mentality changed. I felt distressed every time, so even a small incident could make me uncomfortable and angry. Fortunately, I have my husband, who is always caring and close to me. So, it wasn’t so bad (District 2, Village Health Worker).
When experiencing these symptoms, pregnant women would seek help from various sources, including information from the internet, support from friends, family members, traditional healers, spiritual ceremonies, or other health services, but not formal healthcare institutions, highlighting a potentially stigmatising experiences of seeking healthcare from health facilities. This pattern of behavior was confirmed by our survey findings, where over one-third of pregnant women (38.3%) stated they would not seek health professionals help, if they had a mental illness (Table 4).
Even if diagnosed with a mental health condition, pregnant women avoided mental health medication during pregnancy due to the belief that this could affect fetus growth, especially if they were identified as high-risk pregnancies. They preferred instead to take vitamins and practice yoga. This was explained by one of our participants who had a mental health condition and carried twins:
During pregnancy, I do not want to have medication. I only take vitamins. There is yoga exercise which is good for breathing. I do not take sleeping tablets. I do not want to affect the fetus (District 2 Hospital, Woman with mental health condition).
If pregnant women were able to recognize these mental health symptoms, our quantitative results (Table 4) showed that 43.5% of our sample of pregnant women will not tell anyone. Concealing one's illness is a behavior associated with stigma and serves as a mechanism with numerous unintended consequences, as the risk of the stigma being exposed persists [49]. The fear of being discovered acts as a source of psychological distress for all those actively concealing their stigmatized condition or profession [50], as women endure the anxiety of potentially being discovered and mental health workers being ‘discredited’ [51]. Thus, stigma can also infiltrate the provision of health services, potentially undermining health systems responsiveness, as one hospital manager reflected:
I think most general health providers... are reluctant to work with mental health because of the stigma (Central Hospital Manager, Provider)
Nevertheless, social distancing and other preventive measures for COVID-19 posed a risk of exacerbating psychological disorders in Vietnam. Women faced a double and unequal burden of work and family duties [52], which increased their social isolation and exposing gender inequality issues. Mental illness received more attention after COVID19 when the media highlighted more deaths related to postnatal depression. This awareness was confirmed by a manager in a provincial mental hospital:
After COVID-19, the post-covid condition with death cases related to depression are complicated, especially among pregnant women. They worry too much; they come more to hospitals to ask about their condition. In the past, few people were thinking about mental illness (Provincial Mental Hospital Manager).
Shame, household structure and gender roles during pregnancy
The tradition of relocation closer to or with in-laws after marriage, coupled with the belief that children belong to their father’s lineage, could potentially risk gender-based emotional and physical interpersonal violence [26]. In addition, there is a strong cultural preference for male children, which could affect women who were known to carry female fetuses [53]. Consequently, family relationships were identified both as potential risk factors for CPMDs and as essential sources of support [23]. The data from our study suggested that relationships with parents-in-law could be particularly stressful during pregnancy in some families, and pregnant women did not always find the support they needed. One of the pregnant women we interviewed explained how these family conflicts impacted her friend’s mental health during pregnancy:
My sister-in-law was very stressed because her mother-in-law did not sympathize with her. She lost her appetite and only wanted snack food, which costs some money. She could not buy food because she feared her mother-in-law scolding her. She lost weight and was very stressed (District 2 Hospital Woman).
Family dynamics could thus suppress women’s emotions and created social isolation and discrimination. This may influence health-seeking behaviors from family members or health services, especially considering the additional pressure of being disloyal by bringing shame (associated stigma) to their family and community [26]. This is significant because our interviews revealed that families, including husbands and parents, are crucial sources of support for pregnant women with CPMDs and many of them do, as explained by one of our participants:
My parents also encourage me; my parents-in-law also support me. My husband also takes care of me, changes the nutrition, so I felt easier, not so stressed (Pregnant woman with mental health condition).
In our survey data, 38.2% of women responded that it is best to avoid people with mental illness because they may develop this condition. In Vietnam, beliefs regarding the causes of mental disorders hover between the natural and the supernatural. They vary according to an individual’s level of education and socioeconomic class. Spiritual beliefs related to ancestors, reincarnation, and karma provide cultural explanations where deities and ancestors could influence a person’s fate [54]. This highlights the reasoning for considering a person with mental illness as punishment for their previous sins or the sins of their entire family, or insanity could be considered possession by angry ancestral spirits [44] and could therefore condemn the honor of the whole family along with the individual [43]. Our qualitative data also suggested that families of pregnant women with mental illness often were blamed. This pattern was observed by one the hospital providers interviewed:
The families-in-law often blamed pregnant women as they did something wrong so this [mental illness] could happen to them. This creates more pressures on pregnant women (Provincial Obstetrics and Gynecology Hospital Provider).
Pregnant women’s family members not only serve as caregivers for individuals with mental health conditions but are also likely to encounter stigma by association, occasionally experiencing self-stigma [17].
The interplay of low prioritisation, referral pathways and access to health care
The lack of a dedicated mental health law has been a continued problem in Vietnam, resulting in insufficient protection of the fundamental human rights of people with mental illnesses [43]. Moreover, there have been few advocacy groups for mental health patients in Vietnam, and little opportunity for their representation in policy-making structures [55]. The lack of advocacy and prioritisation for establishing a national mental health policy was confirmed by participants as a significant barrier to long-term solutions to mental health.
I must say that I am not satisfied with the mental health program, especially the leadership of the national psychiatric hospital. They are not fully devoted to mental health programs and have no advocacy for mental health on the health policy agenda (Central Manager).
In our study, the needs of women with CPMDs went largely unrecognized, and virtually no services address these conditions [56]. Most pregnant women with mental health conditions were referred to the provincial hospital instead of direct referrals to a provincial psychiatric hospital. Almost no pregnant women were referred to provincial psychiatric hospital from the Obstetrics and Gynecology network, except in cases with prior history of schizophrenia or severe depression. This was corroborated by mental hospital managers, as illustrated below:
Only severe patients with existing mental illness will be referred to psychiatric hospitals. This is because those patients did not cooperate well during antenatal check-ups in the Obstetrics hospital. Those are with very severe depression, epilepsy, so they came. (Provincial Mental Hospital Manager)
The referral pathway reflected fragmented service provision and a lack of collaboration between maternal and mental health providers [57], contributing to a lack of choice of mental healthcare services at the PHC level and only a few women receiving care at psychiatric hospitals.
Additionally, there is also shortage of mental health staff with high workload and low salaries coupled with lack of knowledge about maternal mental health in continuous medical education programs. Furthermore, psychiatrists worked in hospitals in big cities such as Hanoi and Ho Chi Minh, rather than in rural health services [58]. This was reflected in the significant gap between psychiatrists in provinces and was evident in the fieldwork, where, in some provinces, the only psychiatrist available was retiring.
So firstly, the number of specialist doctors [psychiatrist] is declining; they are very few. I have visited several provinces and evaluated non-communicable diseases and mental health programs. Some provinces had only one psychiatric doctor, and some are retiring, so, no more any psychiatrist in the province (Central Manager).
The scarcity of psychiatrists constrained mental healthcare accessibility, with only half of the provinces hosting provincial psychiatric hospitals, and half had only psychiatric wards in provincial hospitals in Vietnam [59]. In addition, the Vietnamese healthcare system has a distinct vertical division between maternal healthcare and mental health care. While maternal healthcare has a comprehensive four-tier vertical system, mental health care is primarily developed only at the provincial and central levels. Consequently, the primary healthcare level lacks healthcare workers specialized in mental health within the system [60]. Ultimately, this structural stigma towards mental health profession and professionals is likely to further contribute to a lack of recognition of maternal mental healthcare as a policy priority at the PHC level.
Discussion
This study has shown that, in Vietnam, stigma operates at three levels, influencing the interactions between pregnant women and healthcare services. Consequently, it impacts the responsiveness of health systems to maternal mental health needs, as well as women’s decision-making regarding disclosure of perinatal mental health problems and help-seeking behavior. The program theory we examined focused on increasing understanding of how contextual interconnected issues relate to individuals (perinatal women), relationships between individuals and others, and barriers in their environment (micro-meso-macro contexts). Using Cook’s [38] taxonomy of interpersonal, intrapersonal and structural stigma to guide data analysis led to the development of a revised theory (see Table 5) that increased our nuanced understanding of the context in which women experience mental health conditions, and the mechanisms operating in health systems interactions. This revised program theory will support our study co-produced intervention to increase overall health systems responsiveness for maternal mental health in Vietnam.
Table 5.
Refined program theory after data collection and analysis
| In a socio-cultural context based on gender norms during pregnancy where often the fetus takes priority over women’s needs from families and women’s themselves, and in a society where maternal mental health is normalised as not seen as pathological; and where there is low literacy of maternal mental health, women are often unconscious of the relevance of their own symptoms. Since mental illness language also operates as a taboo, the fear of discrimination and family shame influence self-referral, family referrals and maternal services referral pathways and overall access to health care for pregnant women. Because of the fear of disclosure, women often self-care using alternative therapies instead of seeking support from health services and engaging with healthcare institutions, which in turn offer insufficient coverage for maternal mental health. Health care providers’ focus when engaging with women’s in high-risk groups for MMH (miscarriage, high risk pregnancy, victim of violence, etc.) appears to be primarily on the fetus and women’s physical health outcomes with little attention to their emotional and psychological needs. |
Cook’s conceptual framework enabled in-depth understanding of this complex area (Fig. 1). At the interpersonal level, the local cultural context shapes stigma and discrimination in mental health [6, 21]. This context often leads to the normalization of CPMDs, perpetuates stereotypes of mental illness as dangerous, and fosters biases towards mental health patients among communities, some family members, and even mental health professionals. These finding echoes other studies from similar Asian contexts, such as China, Hongkong, and Singapore, where severe mental illnesses are often perceived as dangerous and aggressive, and the stigma experienced by family members is pervasive [61]. In our study, gender appeared to discriminate further for mental health conditions, a finding consistent with other research indicating that gender intersects with mental health-related stigma and influences its severity [19].
Fig. 1.
Interpersonal, Intrapersonal, and Structural Stigma in pregnant women’s mental health
At the intrapersonal level, in rural Vietnam, stigma manifested with common cultural beliefs that mental diseases should not be healed medically but rather with traditional and religious practices [46, 62, 63]. The psychiatric hospitals and psychiatrists were seen as not helpful or even worsening the situation [46, 62]. Our literature review identified that in certain rural areas, the use of fortune tellers for spiritual healing is quite common due to low cost and reduced stigma [44]. If their condition does not improve, women may access health facilities later. However, our findings did not encounter this phenomenon. Instead, women with mental health conditions, especially those with high-risk pregnancies, reported a reluctance to engage with prescribed medication, prioritizing the health of their fetus over their mental health needs.
In our study, more than one-third of pregnant women with symptoms of mental health conditions were reluctant to seek care from health professionals. Self-stigma contributed to fear of acknowledging mental health conditions, possibly leading to shame, avoidance of sharing information, and delays in seeking healthcare, with only the severely ill coming to psychiatric hospitals. In China, similar results were reported, where stigma on mental health also led to avoidance of seeking mental healthcare and medication during pregnancy [64]. This similarity could be due to similar Confucian culture and political and administrative management systems. In addition to cultural issues, socio-economic contexts of poverty and access to healthcare are also associated with outcomes of mental illness and determine the environment in which stigma is enacted and experienced [21].
While women in our study were able to identify common mental symptoms such as worry, anxiety, and stress, they did not associate these with mental health. The limited knowledge of mental health among Vietnamese people in Vietnam and among Vietnamese immigrants in US is reported [46, 48]. Attitudes and beliefs surrounding mental health in Vietnam are shaped by a combination of limited knowledge and a blend of traditional and modern perspectives [46]. There exists a particular negative attitude towards mental illnesses associated with socially disruptive and dangerous behavior [46, 65]. The population’s awareness of mental disorders is somewhat limited in Vietnam compared to Western countries, possibly leading to a higher risk of stigma in Vietnam [59].
At the interpersonal stigma, stigma towards mental health professionals is particularly challenging in Vietnam. Mental health professionals were devalued and perceived as incompetent, unskilful, and unhelpful. The social standing of psychiatrists is relatively low compared to other medical specialties, contributing to very few students choosing to study psychiatry [62, 63]. Our qualitative and quantitative data confirmed this observation: maternal health workers within obstetrics and gynecology networks did not refer pregnant women with mental health conditions to psychiatric hospitals, and psychiatrists were reluctant to disclose that they worked in psychiatric hospitals.
This stigma and low social position have been linked to shortages and low retention of mental health professionals [59], contributing to a lack of choices in maternal mental healthcare at the PHC level, which underlines the lack of support for mental health in Vietnam [62]. These negative attitudes towards mental health professionals are similar elsewhere in Asia [64, 66]. Therefore, the intervention in the community in the future in Vietnam may face challenges. Whilst this change takes time, similar programs have been successful in India [67] and Malawi [68] and Vietnam can learn from these examples.
Stigma is rooted in cultural values and stereotypes, and this was reflected in studies examining Vietnamese American and other Asian American backgrounds [48, 69]. Despite residing in the United States, they remain dismissive of mental health concerns. They prioritized “saving face”, and keeping problems inside rather than discussing them openly, leading women to seek coping mechanisms independently. This highlights the potential to enhance engagement in mental health services by providing cultural sensitivity training for healthcare professionals.
Structural stigma contributed to the lack of integrated perinatal mental healthcare [70] and training and knowledge on mental health among maternal health providers at the PHC level. This finding is confirmed by another study from Vietnam, where almost none of the CPMDs were detected at the PHC level, and no referrals were sent [23]. Most care was given by counseling on rest or nutrition without attention and communication on mental health conditions during antenatal checkups [71]. Healthcare providers often overlook mental health concerns, resulting in a failure to initiate communication about mental health issues. This contributes to a lack of mental healthcare, potentially increasing delays in accessing and receiving the necessary mental healthcare services.
The recent three-year “National Plan for Prevention and Control of non-communicable diseases and mental disorders for 2022–2025” establishes that 100% of medical staff that implement the prevention and control of mental disorders at all levels should receive training in the prevention, supervision, detection, management, diagnosis, and treatment of common mental disorders. All pregnant women should receive screening, counseling, and prevention for mental health disorders. However, the plan was promulgated without financial commitments from the government and did not provide sufficient guidance for provincial health departments to develop local mental health plans. This may echo the low priority of mental healthcare at the policy level in Vietnam [58]. In 2020, the National Health Target Program on Mental Health was stopped due to a change in government policy, and no funding mechanisms were given for mental health programs at the local levels.
Our study demonstrates that maternal mental health stigma operates at three levels: interpersonal, intrapersonal, and structural. Stigma is rooted in cultural values and stereotypes and gender intersects with stigma and affects pregnant women’s access and choice to mental healthcare because of the fear and shame embedded in the micro-meso-macro contexts in which they live. Maternal mental health in Vietnam has commonly been studied focusing on interpersonal violence [26, 28, 72] or child health [8]. To our knowledge this is the first study that incorporates the voices of pregnant women with mental health conditions and healthcare staff in Vietnam. Stigma associated with some illnesses (e.g., infectious diseases, mental disorders) have direct negative effects in people’s interactions with health systems across the world. Our results help advance the understanding of mental health stigma and its manifestations, shaping the health system's responsiveness to maternal mental health [73].
We found that barriers to prevention, screening, diagnosis, and treatment of mental health conditions are enabled by the dangerous mix of unconsciousness and reluctance to label mental health due to fear of stigmatisation by women themselves but also healthcare services. This manifests into oscillating unperceived unmet need (when women do not perceive they need health care) and subjective chosen unmet need (women choosing not to demand healthcare) [74]. This has implications for women-centred, equity-oriented interventions and the measurement of unmet needs in health policy and systems studies.
Women’s antenatal visits should allow time for communication, ascertain patients’ concerns, and discuss mental health issues. The trust and continuity of mental health services from primary to tertiary care with a horizontal referral at each level should be linked to the concept of ‘choice’ of service, as reported in Germany [75] and Iran [76]. Our findings also reaffirm that health systems responsiveness entails a socially constructed set of interactions between people and their health system, shaped by their initial expectations rooted within respective cultural contexts [14]. Therefore, strategies to improve health systems responsiveness should address both the ‘people’ and the ‘systems’ sides of such interactions [30]. Broadly, such strategies contribute towards improving health equity and justice among vulnerable populations such as women in low- and- middle income countries.
Limitations of the study
This study provides valuable insights into the barriers affecting women’s decision to disclose and access treatment for perinatal common mental health needs in the context of a low- and middle-income country. Yet, the study has some limitations. Firstly, the use of selection of one province may have constrained broader generalizability. Secondly, the representation of various stakeholders at different levels may not have fully captured the diversity of perspectives and experiences across groups. Nonetheless, we are confident that these limitations did not undermine the validity of our findings.
Conclusion and recommendations
Mental health is a complex issue, and improving access to maternal mental healthcare requires multiple efforts to address stigma across interpersonal, structural, and intrapersonal levels. Stigma is a significant deterrent to mental healthcare seeking. Its reduction will help improve the health system's responsiveness by providing services closer to the people, offering prompt attention, and better communication. Addressing stigma can enhance awareness of mental health services, help reduce delays in care-seeking and transform services to be truly responsive to maternal mental health needs.
Therefore, it is essential to have psychoeducational programs in communities to enhance awareness of common mental disorders and reduce the negative attitudes towards mental healthcare systems and mental health professionals. Improvements in perinatal mental care, including early screening mental health problems and intervention, could help prevent complications. Long-term interventions targeted at structural and organizational levels and directed to health professionals and the community to decrease the stigma on mental health in Vietnam are needed. One could advocate for national policy, shifting from hospital care to community-based mental healthcare and anti-stigma training [77]. Future studies should explore the specific and unique needs of pregnant women in these communities.
Acknowledgements
We thank all participants who participated in this research. The authors acknowledge the valuable inputs and comments provided by Dr Anna Cronin de Chavez and the reviewers of the paper.
Abbreviations
- CPMDs
Common perinatal mental disorders
- ESRC
Economic and Social research council
- FGDs
Focus group discussion
- MRC
Medical research council
- PHC
Primary health care
- WHO
World Health Organization
Authors’ contributions
LMT, LTV, NTQC and DTHT conducted data collection. LTV performed the statistical analysis. LTV, BTTH and DTHT coordinated data collection. BTTH, SM, TM and AM conceptualized and supervised the study. LMT, BTTH and DTTD conceptualized the first draft manuscript and conducted qualitative data analysis. LMT for data visualization. LMT, TM, AM and SM revised the manuscript and LMT finalized the manuscript. TM, AM, KL, SM and LMT provided substantial review and editing for content. All authors reviewed and approved the final manuscript.
Funding
The research reported in this paper received funding from the Joint Health Systems Research Initiative comprising Medical Research Council (MRC), Foreign, Commonwealth & Development Office (FCDO) and Wellcome Trust (grant ref: MR/T023481/2). The views are of the authors only and do not necessarily represent those of the funders.
Availability of data and materials
Data is provided within the manuscript. Further supplementary information files can be shared if required.
Declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Boards of the Hanoi University of Public Health (Ref. 33/2022-YTCC-HD3), London School of Hygiene and Tropical Medicine (Ref 22981), and the University of Leeds (Ref. MREC 19–051). The research was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all study participants before fieldwork, and their anonymity and confidentiality were preserved during data analysis and in reporting findings.
Consent for publication
Not applicable. Participant details are anonymized.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fisher J, de Cabral Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139g–49g. 10.2471/BLT.11.091850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Hara MW, Wisner KL. Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):3–12. 10.1016/j.bpobgyn.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anuk D, Özkan M, Kizir A, Özkan S. The characteristics and risk factors for common psychiatric disorders in patients with cancer seeking help for mental health. BMC Psychiatry. 2019;19(1):269. 10.1186/s12888-019-2251-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Addisu A, Kumsa H, Adane S, Diress G, Tesfaye A, Arage MW, et al. Common Mental Disorder and Associated Factors among Women Attending Antenatal Care Follow-Up in North Wollo Public Health Facilities, Amhara Region, Northeast Ethiopia: A Cross-Sectional Study. Depress Res Treat. 2024;2024:8828975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Misgana T, Gebremichael B, Weldesenbet AB, Tesfaye D, Tamiru D, Tariku M, et al. Association between antenatal common mental disorders symptoms, and adverse obstetric and perinatal outcomes: A community-based prospective cohort study in Eastern Ethiopia. J Affect Disord. 2024;355:31–9. 10.1016/j.jad.2024.03.153 [DOI] [PubMed] [Google Scholar]
- 6.Pokharel A, Philip S, Khound M, El Hayek S, de Filippis R, Ransing R, et al. Mental illness stigma among perinatal women in low- and middle-income countries: early career psychiatrists’ perspective. Front Psychiatry. 2023;14:1283715. 10.3389/fpsyt.2023.1283715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jane RW Fisher, Meena Cabral de Mello, Takashi Izutsu, Tuan Tran. The Ha Noi expert statement: recognition of maternal mental health in resource-constrained settings is essential for achieving the Millennium Development Goals. Int J Ment Health Addict. 2011;5(2). 10.1186/1752-4458-5-2. [DOI] [PMC free article] [PubMed]
- 8.Nguyen PH, Saha KK, Ali D, Menon P, Manohar S, Mai LT, et al. Maternal mental health is associated with child undernutrition and illness in Bangladesh. Public Health Nutr. 2014;17(6):1318–27. 10.1017/S1368980013001043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hue MT, Van Nguyet NH, Nha PP, Vu NT, Duc PM, Van Trang NT, et al. Factors associated with antenatal depression among pregnant women in Vietnam: A multisite cross-sectional survey. Health Psychol Open. 2020;7(1):2055102920914076. 10.1177/2055102920914076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. World mental health report. Geneva: Transforming mental health for all; 2022. [Google Scholar]
- 11.Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: ignorance, prejudice or discrimination? Br J Psychiatry. 2007;190:192–3. 10.1192/bjp.bp.106.025791 [DOI] [PubMed] [Google Scholar]
- 12.Henderson C, Noblett J, Parke H, Clement S, Caffrey A, Gale-Grant O, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014;1(6):467–82. 10.1016/S2215-0366(14)00023-6 [DOI] [PubMed] [Google Scholar]
- 13.de Silva A. A framework for measuring responsiveness. GPE discussion paper series no 32. World Health Organization: Geneva; 2000. p. 3. [Google Scholar]
- 14.Mirzoev T, Kane S. What is health systems responsiveness? Review of existing knowledge and proposed conceptual framework. BMJ Glob Health. 2017;2(4):e000486. 10.1136/bmjgh-2017-000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen T, Tran T, Tran H, Tran T, Fisher J. The burden of clinically significant symptoms of common and severe mental disorders among adults in Vietnam: a population-based cross-sectional survey. BMC Public Health. 2019;19(1):1173. 10.1186/s12889-019-7513-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen T, Tran T, Ha T, Fisher J. Challenges in integrating mental health into primary care in Vietnam. 2019. p. 1–21. [Google Scholar]
- 17.Lauber C, Rössler W. Stigma towards people with mental illness in developing countries in Asia. Int Rev Psychiatry. 2007;19(2):157–78. 10.1080/09540260701278903 [DOI] [PubMed] [Google Scholar]
- 18.Thornicroft G, Sunkel C, Aliev AA, Baker S, Brohan E, El Chammay R, Davies K, Demissie M, Duncan J, Fekadu W, Gronholm PC. The Lancet Commission on ending stigma and discrimination in mental health. Lancet. 2022;400(10361):1438–80. [DOI] [PubMed]
- 19.Stangl AL, Earnshaw VA, Logie CH, van Brakel W, Leikness CS, Barré I, et al. The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31. 10.1186/s12916-019-1271-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ottewell N. Stigma against mental illness: Perspectives of mental health service users. Ment Health Prev. 2016;4(3):115–23. 10.1016/j.mhp.2016.10.001 [DOI] [Google Scholar]
- 21.Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L, Thornicroft G. Stigma and discrimination related to mental illness in low- and middle-income countries. Epidemiol Psychiatr Sci. 2015;24(5):382–94. 10.1017/S2045796015000359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim W. Diversity among Southeast Asian ethnic groups. J Ethn Cult Divers Soc Work. 2006;15(3–4):83–100. 10.1300/J051v15n03_04 [DOI] [Google Scholar]
- 23.Abrams D, Nguyen LT, Murphy J, Lee YA, Tran NK, Wiljer D. Perceptions and experiences of perinatal mental disorders in rural, predominantly ethnic minority communities in northern Vietnam. Int J Ment Health Syst. 2016;10:10. 10.1186/s13033-016-0043-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Ngo T, Gammeltoft T, Nguyen HTT, Meyrowitsch DW, Rasch V. Antenatal depressive symptoms and adverse birth outcomes in Hanoi. Vietnam PLoS One. 2018;13(11):e0206650. 10.1371/journal.pone.0206650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisher JR, Tran H, Tran T. Relative socioeconomic advantage and mood during advanced pregnancy in women in Vietnam. Int J Ment Health Syst. 2007;1(1):3. 10.1186/1752-4458-1-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nhị TT, Hạnh NTT, Gammeltoft TM. Emotional violence and maternal mental health: a qualitative study among women in northern Vietnam. BMC Womens Health. 2018;18(1):58. 10.1186/s12905-018-0553-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoang TN, Van TN, Gammeltoft T, Dan WM, Nguyen Thi Thuy H, Rasch V. Association between intimate partner violence during pregnancy and adverse pregnancy outcomes in Vietnam: a prospective cohort study. PLoS One. 2016;11(9):e0162844. 10.1371/journal.pone.0162844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vung ND, Ostergren PO, Krantz G. Intimate partner violence against women, health effects and health care seeking in rural Vietnam. Eur J Public Health. 2009;19(2):178–82. 10.1093/eurpub/ckn136 [DOI] [PubMed] [Google Scholar]
- 29.Pawson R, Bellamy JL. Realist synthesis: an explanatory focus for systematic review. In: Popay J, ed. Moving beyond effectiveness in evidence synthesis: methodological issues in the synthesis of diverse sources of evidence. London, UK: National Institute 559 for Health and Clinical Excellence; 2006. p. 83–94.
- 30.Mirzoev T, de ChavezCronin A, Manzano A, Agyepong IA, Ashinyo ME, Danso-Appiah A, et al. Protocol for a realist synthesis of health systems responsiveness in low-income and middle-income countries. BMJ Open. 2021;11(6):e046992. 10.1136/bmjopen-2020-046992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pawson R, Tilley N, Tilley N. Realistic evaluation. London, Thousand Oaks, Calif; Sage Publication: 1997.
- 32.Manzano A. The craft of interviewing in realist evaluation. Evaluation. 2016;22(3):342–60. 10.1177/1356389016638615 [DOI] [Google Scholar]
- 33.Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci. 2015;10(1):1–7. 10.1186/s13012-015-0237-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vietnam General Statistic Office. Completed results of the 2019 population and housing census. 2020. [Google Scholar]
- 35.O’Connor M, Casey L. The Mental Health Literacy Scale (MHLS): A new scale-based measure of mental health literacy. Psychiatry Res. 2015;229(1–2):511–6. 10.1016/j.psychres.2015.05.064 [DOI] [PubMed] [Google Scholar]
- 36.Dang HM, Weiss B, Trung L, Ho H. Mental health literacy and intervention program adaptation in the internationalization of school psychology for Vietnam. Psychol Sch. 2018;55(8):941–54. 10.1002/pits.22156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 38.Cook JE, Purdie-Vaughns V, Meyer IH, Busch JTA. Intervening within and across levels: A multilevel approach to stigma and public health. Soc Sci Med. 2014;103:101–9. 10.1016/j.socscimed.2013.09.023 [DOI] [PubMed] [Google Scholar]
- 39.Phan T, Silove D. An overview of indigenous descriptions of mental phenomena and the range of traditional healing practices amongst the Vietnamese. Transcult Psychiatry. 1999;36(1):79–94. 10.1177/136346159903600105 [DOI] [Google Scholar]
- 40.Martensen LK, Hahn E, Duc CT, Schomerus G, Böge K, Dettling M, et al. Impact and differences of illness course perception on the desire for social distance towards people with symptoms of depression or schizophrenia in Hanoi. Vietnam Asian Journal of Psychiatry. 2020;50:101973. 10.1016/j.ajp.2020.101973 [DOI] [PubMed] [Google Scholar]
- 41.Gaines R. Culture & Schizophrenia: How the Manifestation of Schizophrenia Symptoms in Hue Reflects Vietnamese Culture. Independent Study Project (ISP) Collection. 2014. p. 1826. https://digitalcollections.sit.edu/isp_collection/1826.
- 42.Do M, McCleary J, Nguyen D, Winfrey K. 2047 Mental illness public stigma, culture, and acculturation among Vietnamese Americans. Journal of Clinical and Translational Science. 2018;2(S1):17–9. 10.1017/cts.2018.93 [DOI] [Google Scholar]
- 43.Minas H, Edington C, La N, Kakuma R. Mental health in Vietnam. 2017. p. 145–61. [Google Scholar]
- 44.Nguyen A. Cultural and social attitudes towards mental illness in Ho Chi Minh City, Vietnam. Stanford Univ Res J. 2003;2:27–31.
- 45.Ta TM, Zieger A, Schomerus G, Cao TD, Dettling M, Do XT, et al. Influence of urbanity on perception of mental illness stigma: a population based study in urban and rural Hanoi. Vietnam Int J Soc Psychiatry. 2016;62(8):685–95. 10.1177/0020764016670430 [DOI] [PubMed] [Google Scholar]
- 46.van der Ham L, Wright P, Van TV, Doan VD, Broerse JE. Perceptions of mental health and help-seeking behavior in an urban community in Vietnam: an explorative study. Community Ment Health J. 2011;47(5):574–82. 10.1007/s10597-011-9393-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Watson H, Harrop D, Walton E, Young A, Soltani H. A systematic review of ethnic minority women’s experiences of perinatal mental health conditions and services in Europe. PLoS ONE. 2019;14(1):e0210587. 10.1371/journal.pone.0210587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Do M, Pham NN, Wallick S, Nastasi BK. Perceptions of mental illness and related stigma among Vietnamese populations: findings from a mixed method study. J Immigr Minor Health. 2014;16(6):1294–8. 10.1007/s10903-014-0018-7 [DOI] [PubMed] [Google Scholar]
- 49.Goffman I. Stigma: Notes on the management of spoiled identity: Englewood Cliffs. NJ: Prentice-Hall; 1963. [Google Scholar]
- 50.Pachankis JE. The psychological implications of concealing a stigma: a cognitive-affective-behavioral model. Psychol Bull. 2007;133(2):328–45. 10.1037/0033-2909.133.2.328 [DOI] [PubMed] [Google Scholar]
- 51.Bos AER, Pryor JB, Reeder GD, Stutterheim SE. Stigma: Advances in theory and research. Basic Appl Soc Psych. 2013;35(1):1–9. 10.1080/01973533.2012.746147 [DOI] [Google Scholar]
- 52.Le XTT, Dang AK, Toweh J, Nguyen QN, Le HT, Do TTT, et al. Evaluating the psychological impacts related to COVID-19 of Vietnamese people under the first nationwide partial lockdown in Vietnam. Front Psychiatry. 2020;11:824. 10.3389/fpsyt.2020.00824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Do HP, Tran BX, Nguyen CT, Vo TV, Baker PRA, Dunne MP. Inter-partner violence during pregnancy, maternal mental health and birth outcomes in Vietnam: A systematic review. Child Youth Serv Rev. 2019;96:255–65. 10.1016/j.childyouth.2018.11.039 [DOI] [Google Scholar]
- 54.Ha VS, Whittaker A. “Pray to all four directions”: a qualitative study of syncretic care seeking by Vietnamese families for their children with autism spectrum disorder. Disabil Rehabil. 2023;45(4):684–95. 10.1080/09638288.2022.2040613 [DOI] [PubMed] [Google Scholar]
- 55.Lee K, Zappelli R, Goldner EM, Vu NC, Corbett KK, Murphy J. The Political Economy of Mental Health in Vietnam: Key Lessons for Countries in Transition. Asia Pac Policy Stud. 2015;2(2):266–79.
- 56.Fisher J, Tran T, La BT, Kriitmaa K, Rosenthal D, Tran T. Common perinatal mental disorders in northern Viet Nam: community prevalence and health care use. Bull World Health Organ. 2010;88(10):737–45. 10.2471/BLT.09.067066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Murphy J, Corbett KK, Linh DT, Oanh PT, Nguyen VC. Barriers and facilitators to the integration of depression services in primary care in Vietnam: a mixed methods study. BMC Health Serv Res. 2018;18(1):641. 10.1186/s12913-018-3416-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ministry of Health, Health Partnership Group. Joint annual health review. Strengthening prevention and control of non-communicable disease. Hanoi: Medical Publishing House; 2014. p. 2015. [Google Scholar]
- 59.Vuong DA, Van Ginneken E, Morris J, Ha ST, Busse R. Mental health in Vietnam: Burden of disease and availability of services. Asian J Psychiatr. 2011;4(1):65–70. 10.1016/j.ajp.2011.01.005 [DOI] [PubMed] [Google Scholar]
- 60.Nguyen T, Tran T, Tran H, Tran TD, Fisher J. Challenges in integrating mental health into primary care in Vietnam. InInnovations in global mental health. Cham: Springer International Publishing; 2021. p. 1249–1269.
- 61.Zhang Z, Sun K, Jatchavala C, Koh J, Chia Y, Bose J, et al. Overview of stigma against psychiatric illnesses and advancements of anti-stigma activities in six Asian societies. Int J Environ Res Public Health. 2020;17(1):280. 10.3390/ijerph17010280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ta TMT, Böge K, Cao TD, Schomerus G, Nguyen TD, Dettling M, et al. Public attitudes towards psychiatrists in the metropolitan area of Hanoi. Asian J Psychiatr. 2018;32:44–9. 10.1016/j.ajp.2017.11.031 [DOI] [PubMed] [Google Scholar]
- 63.Overseas Development Institute, UNICEF. Mental health and psychosocial wellbeing among children and young people in selected provinces and cities in Viet Nam. Hanoi, Vietnam; 2018. https://www.unicef.org/vietnam/media/976/file/Study%20on%20mental%20health%20and%20psychosocial%20wellbeing%20of%20Children%20and%20Young%20people%20in%20V.
- 64.Zhou C, Xu Y. Time to break mental illness-related stigma and discrimination in China. Asian J Psychiatr. 2021;66:102881. 10.1016/j.ajp.2021.102881 [DOI] [PubMed] [Google Scholar]
- 65.Tesfaye Y, Agenagnew L, Anand S, Tucho GT, Birhanu Z, Ahmed G, et al. Knowledge of the community regarding mental health problems: a cross-sectional study. BMC Psychol. 2021;9(1):106. 10.1186/s40359-021-00607-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Njaka S, Ogbodo BA, Okpua NC, Uwa AN. A systematic review on prevalence and perceived impacts of associative stigma on mental health professionals. Int J Nurs Sci. 2023;18:100533. [Google Scholar]
- 67.Chinnayya HP, Chandrashekar CR, Moily S, Puttamma, Raghuram A, Subramanya KR, et al. Training primary care health workers in mental health care: evaluation of attitudes towards mental illness before and after training. Int J Soc Psychiatry. 1990;36(4):300–7. 10.1177/002076409003600408 [DOI] [PubMed] [Google Scholar]
- 68.Kokota D, Lund C, Ahrens J, Breuer E, Gilfillan S. Evaluation of mhGAP training for primary healthcare workers in Mulanje, Malawi: a quasi-experimental and time series study. Int J Ment Health Syst. 2020;14(1):3. 10.1186/s13033-020-0337-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Augsberger A, Yeung A, Dougher M, Hahm HC. Factors influencing the underutilization of mental health services among Asian American women with a history of depression and suicide. BMC Health Serv Res. 2015;15:542. 10.1186/s12913-015-1191-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Trang DTH, Ha BTT, Vui LT, Chi NTQ, Thi LM, Duong DTT, Hung DT, Cronin de Chavez A, Manzano A, Lakin K, Kane S, Mirzoev T. Understanding the barriers to integrating maternal and mental health at primary health care in Vietnam. Health Policy Plan. 2024;39(6):541–51. 10.1093/heapol/czae027. [DOI] [PMC free article] [PubMed]
- 71.Abrahams Z, Schneider M, Honikman S, Olckers P, Boisits S, Seward N, et al. Health systems strengthening interventions for perinatal common mental disorders and experiences of domestic violence in Cape Town, South Africa: protocol for a pilot implementation study. Pilot Feasibility Stud. 2022;8(1):100. 10.1186/s40814-022-01053-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fisher J, Tran T, Duc Tran T, Dwyer T, Nguyen T, Casey GJ, et al. Prevalence and risk factors for symptoms of common mental disorders in early and late pregnancy in Vietnamese women: a prospective population-based study. J Affect Disord. 2013;146(2):213–9. 10.1016/j.jad.2012.09.007 [DOI] [PubMed] [Google Scholar]
- 73.World Health Organization. World Health Report 2000. Health Systems: Improving Performance. Geneva; 2000. [Google Scholar]
- 74.Allin S, Grignon M, Le Grand J. Subjective unmet need and utilization of health care services in Canada: what are the equity implications? Soc Sci Med. 2010;70(3):465–72. 10.1016/j.socscimed.2009.10.027 [DOI] [PubMed] [Google Scholar]
- 75.Bramesfeld A, Klippel U, Seidel G, Schwartz FW, Dierks ML. How do patients expect the mental health service system to act? Testing the WHO responsiveness concept for its appropriateness in mental health care. Soc Sci Med. 2007;65(5):880–9. 10.1016/j.socscimed.2007.03.056 [DOI] [PubMed] [Google Scholar]
- 76.Forouzan AS, Ghazinour M, Dejman M, Rafeiey H, San SM. Testing the WHO responsiveness concept in the Iranian mental healthcare system: a qualitative study of service users. BMC Health Serv Res. 2011;11:325. 10.1186/1472-6963-11-325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.McNab SE, Dryer SL, Fitzgerald L, Gomez P, Bhatti AM, Kenyi E, et al. The silent burden: a landscape analysis of common perinatal mental disorders in low- and middle-income countries. BMC Pregnancy Childbirth. 2022;22(1):342. 10.1186/s12884-022-04589-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is provided within the manuscript. Further supplementary information files can be shared if required.