Abstract
Intracardiac thrombus is a rare but treatable complication following DeVega tricuspid annuloplasty in the setting of orthotopic heart transplantation. Consistent imaging in the post-transplantation period is therefore essential for early identification and management of thromboembolic complications.
Key Words: cardiac magnetic resonance, echocardiography, heart transplantation, tricuspid valve
Graphical Abstract
Tricuspid regurgitation (TR) is the most common valvular complication in orthotopic heart transplantation (OHT) recipients and may occur in up to 84% of cases.1 The development of TR can severely affect clinical outcomes and lead to right ventricular dysfunction and increased mortality.2 Previous institutions, including our own (University of Chicago Medicine, Chicago, Illinois), have demonstrated decreased rates of TR with prophylactic DeVega tricuspid valve repair (TVR) at the time of OHT.1,3 However, thromboembolic complications after DeVega TVR are scarcely reported. Accordingly, we describe 5 cases of patients who developed intracardiac thrombi following OHT with DeVega TVR.
Learning Objectives
-
•
To recognize thrombus as a potential complication of DeVega TVR after OHT.
-
•
To highlight the importance of surveillance imaging at post-transplant follow-up visits.
Case 1
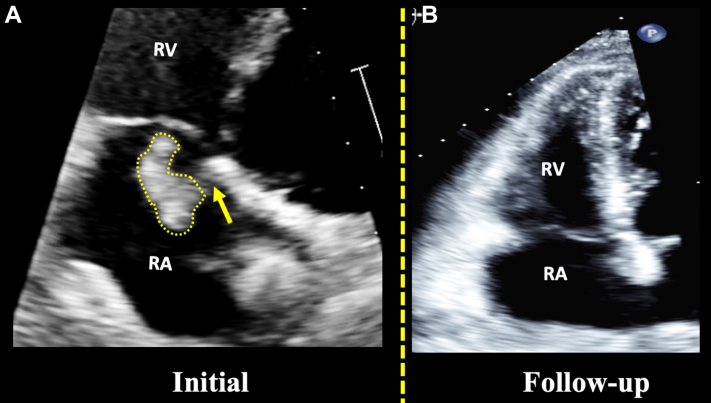
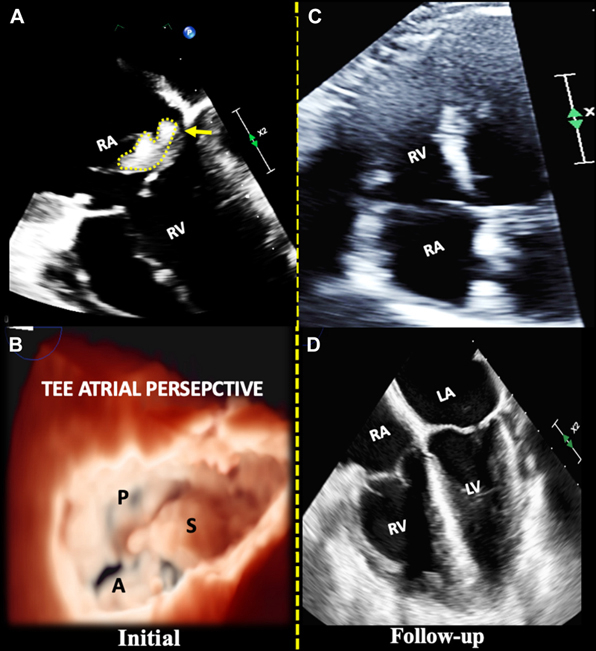
A 52-year-old man with a history of OHT with DeVega TVR for ischemic cardiomyopathy (ICM) was admitted to the hospital for evaluation of a 1.2 × 1.3 cm tricuspid valve (TV) mass seen on a routine transthoracic echocardiogram (TTE) 6 months post-OHT (Figure 1A). A transesophageal echocardiogram (TEE) confirmed the presence of the mobile mass attached to the base of the TV near the site of the DeVega repair (Figure 1B, Video 1). On admission, he was afebrile, and a full infectious disease work-up was completed, with negative blood culture results and a normal sedimentation rate. Given concern for thrombus, the patient was started on warfarin.
Figure 1.
Case 1 Echocardiograms
(Left) (A) 4-chamber transthoracic echocardiogram and (B) 3-dimensional transesophageal echocardiogram (TEE) in Case 1 demonstrating a right atrial thrombus (yellow outline) with an attachment site (arrow) near the DeVega tricuspid repair. (Right) (C) Apical 4-chamber transthoracic echocardiogram and (D) transesophageal echocardiogram depicting resolution of the thrombus following anticoagulation. Created with BioRender.com. A = anterior leaflet of tricuspid valve; LA = left atrium; LV = left ventricle; P = posterior leaflet of tricuspid valve; RA = right atrium; RV = right ventricle; S = septal leaflet of tricuspid valve.
Follow-Up
After 1 year without resolution on serial TTEs, the patient was admitted briefly to the cardiac surgery team in July 2023 for consideration for robotic removal of the mass. On that admission, repeat TTE demonstrated complete resolution of the mass (Figures 1C and 1D). The patient has remained on warfarin since May 2023 without recurrence.
Case 2
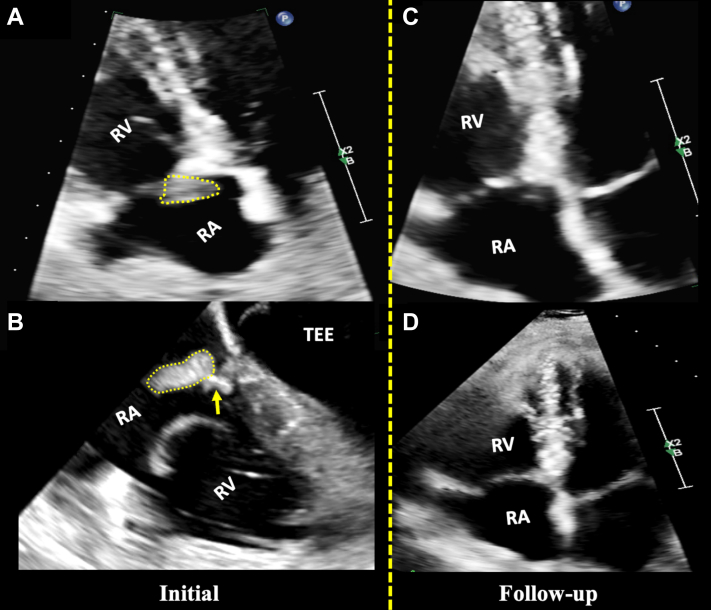
A 72-year-old man who underwent OHT with DeVega TVR for nonischemic cardiomyopathy (NICM) presented for routine TTE monitoring 3 months postoperatively. His post-OHT course remained uncomplicated, without signs of rejection. On imaging, a 2.0 × 1.0 cm mobile mass was incidentally identified near the DeVega surgical repair site (Figure 2A, Video 2). On cardiac magnetic resonance (CMR), the mass was hypoenhancing on both standard and long inversion time late gadolinium enhancement imaging, consistent with thrombus. The patient was consequently bridged to warfarin therapy before discharge.
Figure 2.
Case 2 Echocardiograms
Right ventricular focused apical 4-chamber view transthoracic echocardiogram in Case 2 demonstrating the thrombus (yellow outline) with an attachment site (arrow) near the DeVega repair site (A) at the time of diagnosis with (B) interval resolution following treatment with anticoagulation. Created with BioRender.com. Abbreviations as in Figure 1.
Follow-Up
The patient was continued on warfarin for 3 months for presumed intracardiac thrombus, with resolution of the mass noted on TTE. Although the mass was evident on 1 interim TTE, the patient’s most recent imaging again demonstrated mass resolution (Figure 2B).
Case 3
A 67-year-old man who had undergone heart transplantation with DeVega TVR for ICM presented for a 3-month follow-up visit in clinic. He remained asymptomatic, without signs of rejection. A screening TTE was obtained and demonstrated a large echodensity on the atrial aspect of the TV (Figure 3A). A broad infectious disease work-up was obtained, and results were ultimately negative. A TEE further delineated a 0.6 × 1.8 cm mobile mass attached to the DeVega repair site (Figure 3B). He was transitioned to apixaban (Eliquis) for presumed thrombus and an empiric 6-week course of ceftriaxone and vancomycin.
Figure 3.
Case 3 Echocardiograms
(Left) (A) Apical 4-chamber transthoracic echocardiogram and (B) transesophageal echocardiogram (TEE) in Case 3 demonstrating the mobile thrombus in the right atrium (RA) with an attachment site (arrow) near the DeVega repair site at the time of diagnosis (yellow outline). (Right) (C) Standard and (D) right ventricular focused apical 4-chamber transthoracic echocardiogram demonstrating interval resolution of the thrombus with anticoagulation. Created with BioRender.com. Abbreviations as in Figure 1.
Follow-Up
Intravenous antibiotics were discontinued after 2.5 weeks of treatment out of low concern for endocarditis. A TTE 2 months later demonstrated resolution of the mass with anticoagulation, thus favoring thrombus (Figures 3C and 3D). He has continued to take apixaban without recurrence on subsequent imaging.
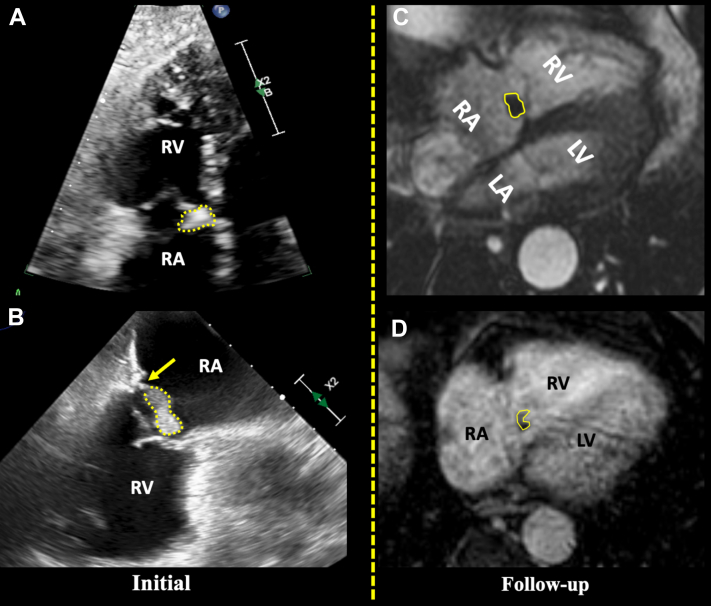
Case 4
A 52-year-old man who underwent OHT with DeVega TVR for NICM presented for routine follow-up 1 year and 9 months after surgery. His post-OHT course was uncomplicated to that point, without rejection. A TTE was obtained at this visit, and the findings elicited concern for a large mass abutting the TV (Figure 4A). A subsequent TEE confirmed a 2.1 × 0.9 cm mobile mass attached to the DeVega repair site (Figure 4B, Video 3).
Figure 4.
Case 4 Echocardiograms
(Left) (A) Apical 4-chamber transthoracic echocardiogram and (B) transesophageal echocardiogram in Case 4 demonstrating the mobile right atrial thrombus with an attachment site (arrow) near the DeVega repair at the time of diagnosis (yellow outline). (Right) Cardiac magnetic resonance following anticoagulation demonstrating interval improvement in the size of the thrombus on (C) 4-chamber cine steady-state free precession views. (D) The mass is hypointense on postcontrast dynamic enhanced-T1 high-resolution isotropic volume examination (e-THRIVE) imaging, consistent with thrombus. Created with BioRender.com. Abbreviations as in Figure 1.
Follow-up
Given the absence of infectious symptoms, thrombus was suspected, and the patient was started on rivaroxaban (Xarelto). A subsequent TTE and CMR obtained 6 months later showed a slight interval improvement in size to 1.7 × 0.9 cm (Figures 4C and 4D). Rivaroxaban was continued with no defined discontinuation date.
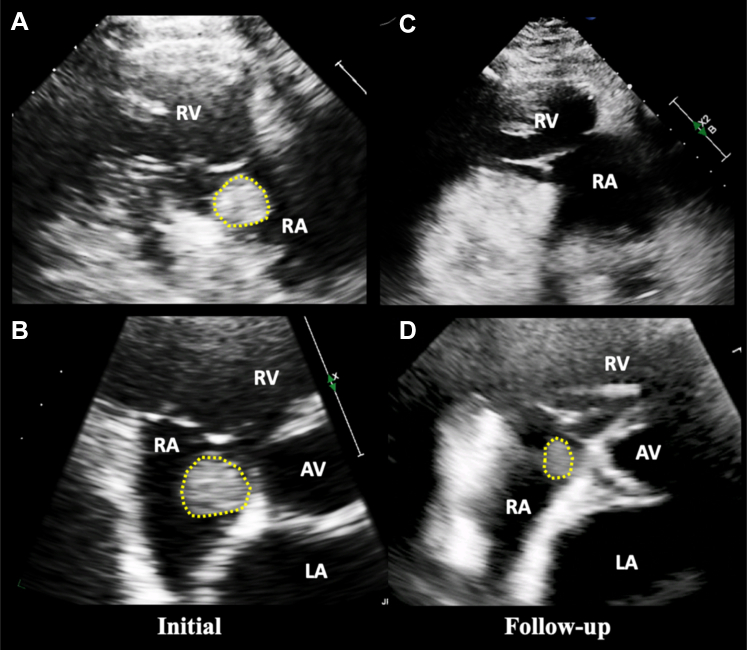
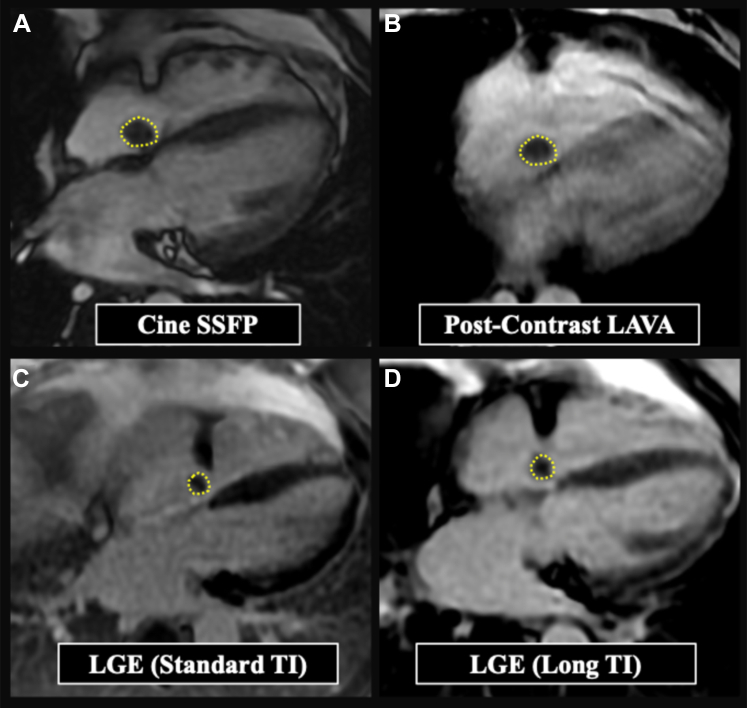
Case 5
A 42-year-old man with a history of multiple venous thromboemboli (who is receiving lifelong apixaban) and OHT with DeVega TVR presented for 6-month follow-up. His donor heart was functioning well, without rejection. His surveillance TTE showed a large, mobile echodensity (2.0 × 1.6 cm) that appeared to attach at the base of the TV (Figures 5A and 5B, Video 4). On CMR, the mass was hypoenhancing on both standard and long inversion time late gadolinium enhancement imaging, consistent with thrombus (Figure 6). The patient was started on warfarin.
Figure 5.
Case 5 Echocardiograms
(Left) (A) Right ventricular inflow and (B) parasternal short-axis transthoracic echocardiographic views in Case 5 that demonstrate a large, round, mobile thrombus in the right atrium near the site of the DeVega repair. (Right) Follow-up (C) right ventricular inflow and (D) parasternal short-axis transthoracic echocardiographic views demonstrating interval improvement in response to anticoagulation. Created with BioRender.com. Abbreviations as in Figure 1.
Figure 6.
Case 5 Cardiac Magnetic Resonance
Tissue characteristics of the mass in Case 5 are shown. The mass is (A) rounded in appearance on balanced steady-state free precession (bSSFP) cines and is hypoenhancing on (B) postcontrast liver acceleration volume acquisition (LAVA) and (C) standard and (D) long inversion time (TI) late gadolinium enhancement (LGE) imaging, consistent with thrombus. Created with BioRender.com.
Follow-up
Because of noncompliance with warfarin, the patient was transitioned to rivaroxaban. Although the thrombus was initially stable on serial echocardiograms, a TTE performed 2.5 years later showed interval improvement in the thrombus with anticoagulation to 1.3 × 0.9 (Figures 5C and 5D).
Discussion
We describe 5 cases of presumed thrombus occurring at the site of the DeVega repair following OHT. In totality, results of infectious disease work-up were negative. Antibiotics were safely deferred in all but 1 patient, thus making endocarditis highly unlikely. In all cases, follow-up imaging revealed interval improvement or resolution of the thrombus with anticoagulation. Importantly, none of the patients experienced major bleeding or thromboembolic complications.
To our knowledge, ours is the first case series to describe intracardiac thrombi as a complication of DeVega TVR following OHT. After careful review of all 143 OHT cases performed from 2021 to 2023 at our institution, we identified intracardiac thrombi in 5 (3.5%) cases, a finding suggesting that this complication is more prevalent than initially thought. In all but 1 case, the thrombi were identified within 3 to 6 months postoperatively. None of the patients experienced rejection or graft failure, thereby suggesting that thrombus formation is likely unrelated to graft status. In 2 of the 5 cases, subsequent endomyocardial biopsies were deferred in favor of noninvasive rejection testing because of the thrombus. None of the other patients experienced thromboembolic events during biopsy.
Overall, the mechanisms that may influence thrombus formation at the DeVega site in the post-OHT setting are unclear and may be multifactorial. Thromboembolism caused by DeVaga repair is extremely rare in patients who are not OHT recipients, with only a few cases reported.4,5 OHT does result in increased levels of prothrombotic and proinflammatory factors, with increased venous thromboembolic risk, a finding suggesting that increased inflammation and hypercoagulability may play roles.6, 7, 8 Of note, the DeVega repair technique leaves a tail at the base of the septal leaflet commissure, which is where thrombus was visualized in our patients.9 We hypothesize that the foreign material from the tail may also serve as a nidus for thrombus. In response to this case series, our surgeons plan to use a shorter tail in future DeVega repairs during OHT. None of the patients had tricuspid stenosis, thus suggesting that stasis is not a major contributor.
Given the favorable response to anticoagulation in all cases, our findings should not dissuade clinicians from using prophylactic DeVega repair. Rather, our series highlights the need for a routine surveillance TTE in the post-OHT setting, including a careful evaluation of the TVR.
Conclusions
Thromboembolic complications are rare but important complications of DeVega TVR following OHT. Routine surveillance of the TVR site by using echocardiography is essential to identify thrombus formation and guide management rapidly.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Case 1 Imaging
(Left) Midesophageal apical 4-chamber and (right) 3-dimensional transesophageal echocardiographic view from the right atrial perspective in Case 1 illustrating the mobile thrombus.
Case 2 Imaging
(Left) 2-dimensional 2 and (right) color Doppler right ventricular focused apical 4-chamber view in Case 2 demonstrating the mobile thrombus attached near the DeVega repair.
Case 4 Imaging
(Left) 2-dimensional lower esophageal and (right) 3-dimensional transesophageal echocardiography from the right atrial perspective in Case 4 that shows the thrombus at the site of the tricuspid valve repair.
Case 5 Imaging
(Left) Right ventricular inflow and (right) parasternal short-axis transthoracic echocardiographic views demonstrating a rounded, mobile thrombus in the right atrium.
References
- 1.Bacusca A.E., Tarus A., Burlacu A., Enache M., Tinica G. A meta-analysis on prophylactic donor heart tricuspid annuloplasty in orthotopic heart transplantation: high hopes from a small intervention. Healthcare (Basel) 2021;9(3):306. doi: 10.3390/healthcare9030306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson C.A., Shernan S.K., Leacche M., et al. Severity of intraoperative tricuspid regurgitation predicts poor late survival following cardiac transplantation. Ann Thorac Surg. 2004;78:1635–1642. doi: 10.1016/j.athoracsur.2004.05.028. [DOI] [PubMed] [Google Scholar]
- 3.Jeevanandam V., Russell H., Mather P., et al. A one-year comparison of prophylactic donor tricuspid annuloplasty in heart transplantation. Ann Thorac Surg. 2004;78:759–766. doi: 10.1016/j.athoracsur.2004.03.083. [DOI] [PubMed] [Google Scholar]
- 4.Efe S.C., Unkun T., Izci S., et al. Thrombus formation on the tricuspid valve after De Vega’s annuloplasty and repair of endocardial cushion defect. J Cardiovasc Thorac Res. 2014;6:203–204. doi: 10.15171/jcvtr.2014.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abbass M., Mariani S., Musa S., Erba N., Masini F., Lentini S. Case Report: right atrial organized thrombus three years after tricuspid annuloplasty. F1000Res. 2023;12:6. doi: 10.12688/f1000research.129157.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forrat R., Ferrera R., Boissonnat P., et al. High prevalence of thromoembolic complications in heart transplant recipients. Which preventive strategy. Transplantation. 1996;61:757–762. doi: 10.1097/00007890-199603150-00015. [DOI] [PubMed] [Google Scholar]
- 7.White M., Ross H., Haddad H., et al. Subclinical inflammation and prothrombotic state in heart transplant recipients: impact of cyclosporin microemulsion vs. tacrolimus. Transplantation. 2006;82:763–770. doi: 10.1097/01.tp.0000232286.22319.e0. [DOI] [PubMed] [Google Scholar]
- 8.Kubala L., Ciz M., Vondracek J., et al. Perioperative and postoperative course of cytokines and the metabolic activity of neutrophils in human cardiac operations and heart transplantation. J Thorac Cardiovasc Surg. 2002;124:1122–1129. doi: 10.1067/mtc.2002.125814. [DOI] [PubMed] [Google Scholar]
- 9.Belluschi I., Del Forno B., Lapenna E., et al. Surgical techniques for tricuspid valve disease. Front Cardiovasc Med. 2018;5:118. doi: 10.3389/fcvm.2018.00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Case 1 Imaging
(Left) Midesophageal apical 4-chamber and (right) 3-dimensional transesophageal echocardiographic view from the right atrial perspective in Case 1 illustrating the mobile thrombus.
Case 2 Imaging
(Left) 2-dimensional 2 and (right) color Doppler right ventricular focused apical 4-chamber view in Case 2 demonstrating the mobile thrombus attached near the DeVega repair.
Case 4 Imaging
(Left) 2-dimensional lower esophageal and (right) 3-dimensional transesophageal echocardiography from the right atrial perspective in Case 4 that shows the thrombus at the site of the tricuspid valve repair.
Case 5 Imaging
(Left) Right ventricular inflow and (right) parasternal short-axis transthoracic echocardiographic views demonstrating a rounded, mobile thrombus in the right atrium.