Abstract
The Russian invasion of Ukraine in February 2022 caused major disruptions of societal functions, including health care. Patients receiving medications for opioid use disorder (MOUD) depend on receiving daily treatment and face a risk of withdrawal in case of medication supply disruption. MOUD are banned in Russia, making treatment continuation impossible in temporarily occupied areas. In this paper, we review the situation with MOUD delivery in Ukraine during the first year of the Russia-Ukraine war. Legislative changes and mobilization of efforts in the time of crisis ensured treatment continuation for thousands of patients. In areas controlled by Ukraine, most patients were receiving take-home doses for up to 30 days, some experienced temporary dosing reductions. Programs in temporarily occupied regions were shut down likely leading to abrupt withdrawal among many patients. At least 10% of patients have been internally displaced. One year into the war, the number of MOUD patients in governmental clinics of Ukraine increased by 17%, and the data suggest that the coverage of private clinics has also increased. But the risks for program stability remain high as the current medication supply relies on one manufacturing facility. Using lessons learned from the crisis, we provide recommendations for future response to minimize the risks of major adverse outcomes among patients treated for opioid use disorder.
Keywords: opioid use disorder, methadone, medications for opioid use disorder, displacement, war, Ukraine
Introduction
On February 24, 2022, Russia launched a full-scale invasion of Ukraine causing major disruptions to all areas of societal life, including health care delivery (Altice, Bromberg, Dvoriak, et al., 2022; Altice, Bromberg, Klepikov, et al., 2022; Vasylyev et al., 2022). It is estimated that about a third of Ukraine’s population have been displaced (Office of the United Nations High Commissioner for Human Rights, May 5, 2022). The war created unique challenges for patients with opioid use disorder and providers of methadone and buprenorphine (medications for opioid use disorder, MOUD).
MOUD patients depend on receiving daily treatment with controlled substances, therefore disruption of supply chains and displacement put patients at risk of withdrawal and other negative health consequences. MOUD have been available in Ukraine since 2004 and are banned in Russia. The Ukrainian MOUD program has been growing steadily to become one of the largest in Eastern Europe and Central Asia in terms of the coverage (estimated to be 7.1% in 2021) and the largest in terms of the number of patients (UNAIDS, 2023a, 2023b). The National Strategy approved in 2019 (Cabinet of Ministers of Ukraine, 2019) sets an ambitious target – to enroll 40% of people with opioid use disorder in the program by 2030. As of February 1, 2022, 17,210 patients were receiving treatment across 205 governmental MOUD sites in Ukraine, and at least 3,000 patients were receiving MOUD in private clinics. About 40% of patients in governmental clinics (N=6,945) lived in regions that were initially targeted by the invasion (Public Health Center of the Ministry of Health of Ukraine, 2014–2023).
In this paper, we describe the key steps taken by the government of Ukraine to sustain the national MOUD program and the changes in MOUD program implementation during the first year of the war as patients and providers were adapting to the new realities. In Ukraine, MOUD is provided by governmental and private clinics (Dmitrieva et al., 2022). Governmental clinics provide treatment free of charge but require that patients meet certain criteria, including official registration at the clinic. Private clinics have fewer requirements for patient entry and provide fee-for-service MOUD prescriptions, which can be filled in select pharmacies with out-of-pocket payments. From a regulatory perspective, MOUD patients in private clinics receive “prolonged detoxification” rather than maintenance treatment to avoid tight regulations related to MOUD maintenance treatment. Because private clinics are not required to report to the Ministry of Health, information on their patients is limited. For this reason, our review is primarily focused on governmental MOUD program. However, realizing the importance of providing a complete picture, we also analyzed limited data available from private clinics.
To guide our analysis, we relied on the World Health Organization Health System Performance Assessment framework (Papanicolas et al., 2022), which builds upon pre-existing health system frameworks and provides a new overarching guidance for evaluation of health system functions and outcomes. The framework outlines the four key functions of a health care system which are aimed at preserving and improving health: governance (policy, stakeholder involvement, strategic information), resource generation (health workforce, infrastructure, and pharmaceuticals), financing, and service delivery. Under this framework, we focused our analysis on specific building blocks that were most affected by the war and critical in sustaining MOUD program, including policy changes, medication supply, workforce, and service delivery, whereas other areas (like financing) that were less affected by the war are only mentioned briefly. Our analysis is therefore structured around the following interrelated building blocks: policy; medication supply, and stakeholder involvement; workforce; and service delivery. We conclude our analysis with lessons learned from this unprecedented crisis, and implications for future response.
Data sources
Governmental surveillance and reporting
The Public Health Center of the Ministry of Health of Ukraine (PHC), as the main governmental entity responsible for MOUD program implementation, collects monthly reports from all governmental MOUD sites in Ukraine including information on patient enrollment and treatment termination, dosing, as well as prevalence of co-morbid conditions (Public Health Center of the Ministry of Health of Ukraine, 2014–2023). We used data from these reports along with the emergency reporting implemented by the PHC after February 24, 2022 to collect additional information from MOUD sites pertaining to the crisis. Some of these data were analyzed by the PHC and made available through their website (Public Health Center of the Ministry of Health of Ukraine, 2022a, 2022b). Governmental surveillance and reporting data used in this review includes information on the dynamics of the number of patients and operating sites, changes in MOUD dosing and delivery mode, and the number and regional distribution of internally displaced patients. While governmental statistics may have suffered from delays related to the war, reporting from clinics that sustained operations was largely unaffected since it is linked to medication stock monitoring. Besides governmental clinics, our analysis uses limited information from private clinics reported to the PHC (Public Health Center of the Ministry of Health of Ukraine, 2014–2023, 2022b).
MOUD patient survey
Between June and July, 2022, a survey was conducted among a random sample of N=700 MOUD patients from 8 regions of Ukraine: Ivano-Frankivsk, Kryvyi Rih (Dnipropetrovsk region), Lviv, Mykolaiv, Odesa, Poltava, Rivne, and Vinnytsia. (See supplementary material). The questionnaire included questions on treatment experiences, substance use, risk behavior, mental health, and other issues pertaining to opioid use disorder and treatment. Some questions in the survey (i.e., frequency of illicit substance use in the last 30 days) were asked twice to assess two time periods – 30 days before February 24, 2022 and 30 days prior to the survey. While this allowed the assessment of war-related changes, responses that refer to the period before February 2022 may be affected by recall bias.
MOUD provider survey
An anonymous online survey conducted between July and August of 2022 was completed by 143 MOUD providers from 108 sites located in 24 regions. (See Supplementary material). The survey included questions on changes in clinic operations since February 24, 2022, challenges, and technical assistance needs. The survey link was disseminated via email lists, short messages to mobile phones, and chat platforms. All physicians involved in MOUD provision at governmental clinics before and during the war were encouraged to participate during regular webinars conducted by the PHC.
Both surveys were commissioned by the PHC and implemented by the Ukrainian Institute on Public Health Policy. The IRB at the Ukrainian Institute on Public Health Policy approved the studies.
Findings
Policy, medication supply, and stakeholder involvement: Efforts mobilization
The early weeks of the war were chaotic. Besides safety concerns, MOUD patients and providers faced many logistical challenges related to service delivery. Participants of the provider survey named the risk of medication supply interruption (26.6%), increased workload (20.3%), emotional stress (8.4%), and patient and staff migration (7.7%) as the main challenges related to MOUD provision during war.
The main storage facility of MOUD is located in Vyshhorod, a suburb north-west of Kyiv, that was among the targets of an initial assault by Russian forces, making warehouse access unsafe. Furthermore, during the early days of the conflict, regular transportation companies refused to make MOUD deliveries to battleground regions. Uncertainty about the timing of the next shipment along with an unpredictable patient influx sometimes required unique solutions for the highest risk regions and relied on a close collaboration between the clinics, the PHC, and other stakeholders (Altice, Bromberg, Dvoriak, et al., 2022). Responding to the request from the PHC, in March 2022 NGO “Alliance for Public Health” stepped in and organized MOUD deliveries to high-risk cities surrounded by the Russian forces, sometimes resorting to concealing methadone in a large batch of other medications to pass through checkpoints.
As an emergency response in the first weeks of the war, the Ministry of Health of Ukraine issued a series of regulations aimed to facilitate patient transitions between MOUD sites and ensure sufficient medication supply. The most important policy changes were: Order #409 (enacted on March 4, 2022) which allowed dispensing or prescribing up to a 30-day take-home medication supply to patients (limited to 10 days prior to the war); Order #425 (enacted on March 7, 2022) which allowed MOUD clinics to maintain larger stocks of medications (up to 3 months of the estimated need), and Order #665 (enacted on April 20, 2022) which changed the rules of MOUD distribution across regions to be based on requests from clinics or regional health departments rather than centralized allocation (Public Health Center of the Ministry of Health of Ukraine, 2022b). In addition to the policy changes, during the early months of the war, the PHC conducted weekly monitoring of MOUD stockpiles at nearly every site to ensure that the limited supply of medications went where it was needed most, and in some cases coordinating re-distribution from one region to another. These steps were critical to provide patients with enough medications to relocate and enroll in treatment at the new location without interruption (Order #409) and provided MOUD sites with increased capacity to enroll an unpredictable influx of new patients (Orders #425 and 665). Around May, after the Russian retreat from the north, access to the main MOUD storage facilities was cleared and the situation with MOUD shipments in Ukraine stabilized. Variability in demand due to internal migration has since been managed by allowing the sites to maintain larger stockpiles of MOUD (Order #425).
Before the war, MOUD procurement in Ukraine was financed from the state budget. Realities of the war led to substantial budget cuts in many areas of governmental spending, including MOUD, requiring the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM) to step in and provide funding to ensure MOUD program continuation. GFATM and other international organizations offered to supply MOUD as humanitarian aid. But the process of customs clearance of controlled substances in Ukraine is highly regulated and requires unnecessary formal approvals from multiple state agencies, which led to substantial delays in shipments. Early in the war, the only two methadone and buprenorphine plants in Ukraine located in Kharkiv and Odesa shut down their operations as both regions were targeted by intense shelling, and Kharkiv has been under high risk of occupation. Around May, the Odesa plant resumed its work and is currently the main source of MOUD manufacturing in Ukraine. So far, manufacturing capacities of this plant have been sufficient to satisfy the demand, but risks remain high. The plant is located in one of the major cities in the south that has been a target of frequent missile strikes by Russian forces.
Service delivery and workforce: Internal migration
Despite efforts to prevent treatment interruptions, the number of MOUD patients dropped by about 5% or 836 patients during February of 2022 (Figure 1). According to the PHC, by the end of May 2022, 16 sites located in temporarily occupied regions or in regions neighboring the frontline were forced to close (Public Health Center of the Ministry of Health of Ukraine, 2022a). Before the war, these sites served 1,410 patients (8.2% of the total number of patients). The number of these patients who managed to flee their homes and continue treatment elsewhere is unknown, but as of August 1, 2022 at least 1,803 MOUD patients from all over the country (about 10% of the total pre-war number) have been internally displaced and started treatment at a new location (Public Health Center of the Ministry of Health of Ukraine, 2022b). During the same period (March – July 2022), the total number of MOUD patients who were reported as discharged due to relocation with or without referral to another site was 2,034. While 1,803 displaced patients who started treatment elsewhere is not strictly a subset of 2,034, the overlap is likely substantial and suggests that most of the patients who were internally displaced managed to re-enroll in treatment during March – July 2022 when Russian forces made most significant advances. Some patients who transitioned from private to governmental clinics experienced challenges related to the lack of medical documentation, in which case they were inducted as new patients according to the current protocols, and those who were previously receiving higher MOUD doses may have experienced withdrawal symptoms (Bromberg et al., 2022; Ivanchuk, 2023).
Figure 1:
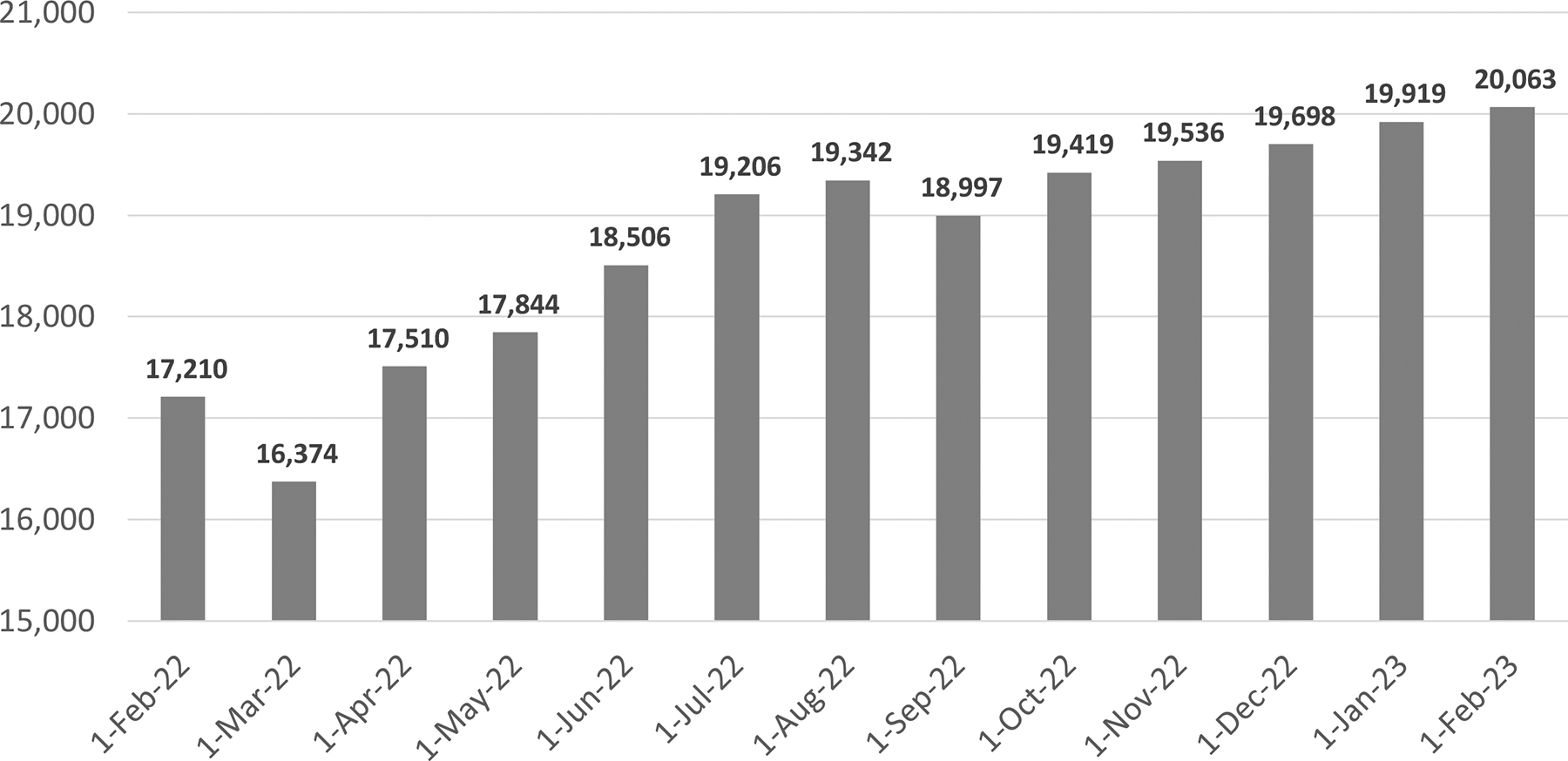
Number of MOUD patients in governmental clinics of Ukraine: January 2022 – January 2023.
Distribution of internally displaced patients across regions was highly unequal with several regions accepting a major proportion of these patients. Figure 2 shows regional distributions of internally displaced MOUD patients by origin and destination along with the outline of Ukrainian territory occupied by Russian forces as of September 2, 2022, before a major counter-offensive resulted in liberation of some of these areas (Soar Earth, 2022). Medical providers in regions that received the majority of displaced patients experienced a substantial workload increase. Between February 24 and June 1, 2022, the number of patients in Lviv increased by 55%, while the number of medical providers remained unchanged. At the same time, on average across the county, the number of MOUD providers did not change substantially since the beginning of the war. By June 1, 2022, the total number of doctors providing MOUD reduced by 4% (from 258 to 247) and the number of nurses reduced by 2% (from 326 to 319) primarily due to site closures in occupied regions. By the end of May 2022, average workload (measured as the number of patients per doctor) increased by 15% due to an overall increase of the number of patients (Figure 1).
Figure 2: Regional distribution of internally displaced MOUD patients as of September 1, 2022.
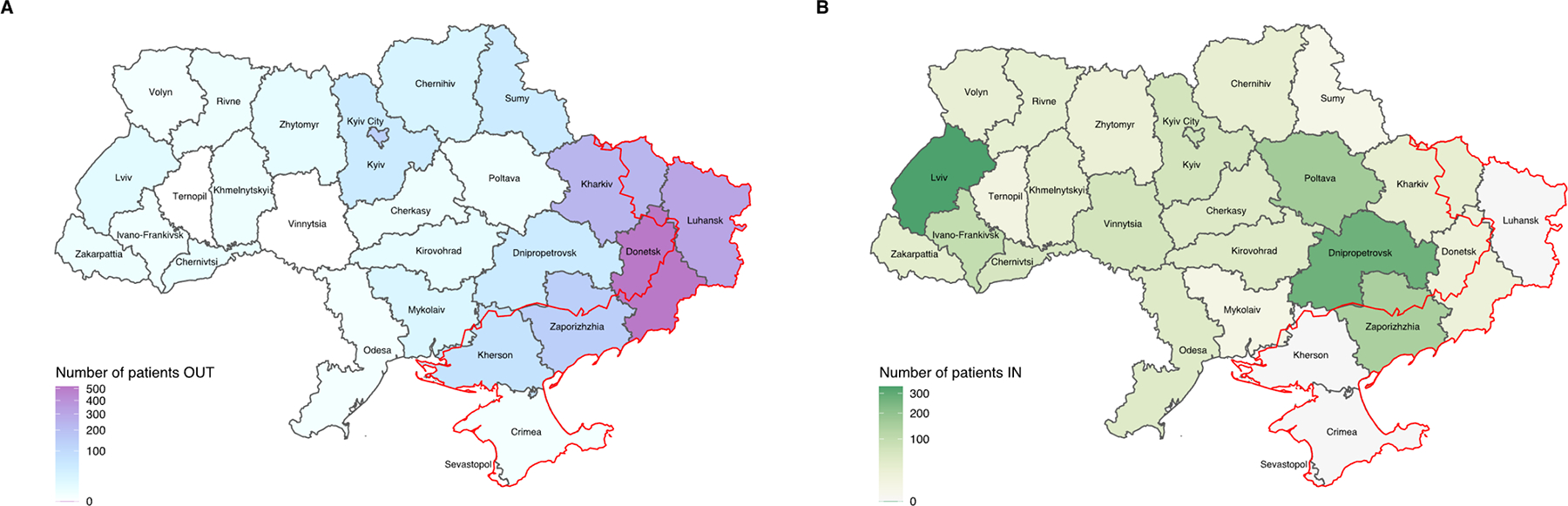
Plot A shows the number of MOUD patients who migrated out of each region. Plot B shows regional distribution of MOUD enrollment among internally displaced patients in governmental clinics (i.e. the number of displaced MOUD patients who re-enrolled in treatment in each of the regions). In both plots, the red line shows the part of Ukraine that was occupied by Russian forces as of September 2, 2022. Outline of the occupied territory is approximate (source: Soar Earth https://soar.earth/maps/13152).
Service delivery: MOUD coverage
Reduction in the number of MOUD patients during the first weeks of invasion was temporary. Figure 1 shows that only 5 weeks after the war started, the number of patients in governmental clinics returned to the pre-war level and has been steadily increasing since April (Public Health Center of the Ministry of Health of Ukraine, 2014–2023). As of February 1, 2023, 20,063 people were receiving MOUD in governmental clinics – a substantial increase of 16.6% (2,853 patients) compared to the pre-war coverage. While the absolute increase is the highest recorded since MOUD program started in 2004, the rate of increase is generally consistent with that observed in previous years (Supplementary Table S1). For example, in 2020, the number of MOUD patients increased by 20% due to COVID-19 pandemic related expansion of take-home dosing (Meteliuk et al., 2021). There may be several reasons for the observed increase. First, possible disruption of illicit drug markets and rising prices of street drugs may have pushed some people with opioid use disorder to seek a safety net in the form of MOUD treatment (Altice, Bromberg, Klepikov, et al., 2022; Public Health Center of the Ministry of Health of Ukraine, 2022a). Second, efforts to support internally displaced patients resulted in a relatively small treatment dropout while operating sites rapidly increased their capacity to enroll new or transitioning patients. The latter was facilitated by the flexible MOUD distribution and supply system along with the increase in take-home dosing coverage and duration that allowed serving higher number of patients without increasing staff requirements. Finally, there is evidence of substantial transition from private to governmental MOUD clinics. As of September 1, 2022, 1,234 of 18,997 (6.5%) patients were previously receiving MOUD in private clinics, raising a concern that the patient increase in governmental clinics may have been offset by the decrease in private clinics (Bromberg et al., 2022; Ivasiy et al., 2022; Public Health Center of the Ministry of Health of Ukraine, 2022a). While there were reports early in the war of private clinics being shut down or operating at reduced capacity due to medication supply disruptions (Ivanchuk, 2023; Public Health Center of the Ministry of Health of Ukraine, 2022a), it is unclear how many clinics and hence patients were affected by these disruptions. Based on the limited information private clinics report to the PHC, the number of patients they serve has likely increased since the war started (Supplement, Section 2). For example, analysis of data from 8 consistently reporting private clinics shows a 2.4-fold increase in the number of patients between February 1, 2022 – February 1, 2023 (Supplemental Table S4), although these data are insufficient to make assumptions about duration of treatment or retention of these patients.
Analysis of the provider survey corroborates state reporting: 63.6% of the survey respondents said that the number of patients at their site increased since the war started and 25.9% reported no major changes in the number of patients. Regional distribution of responses follows the pattern shown in Figure 2: respondents from Luhansk, Donetsk, and Kharkiv reported site closures and reduction of the number of patients, while most other regions reported increases. Several regions - most notably Kherson and Mykolaiv – reported both decreases and increases reflecting opposing dynamics across different sites in the same region (Supplemental Table S8).
Service delivery: Expansion of take-home dosing
Risks and logistical challenges of making daily trips to clinics along with relaxed policies related to take-home medications led to a further reduction of supervised medication intake – a shift that started during COVID-19 pandemic (Meteliuk et al., 2021). In the patient survey, almost 95% of respondents said that they received either take-home or prescription-based medications. Official reporting shows that during the first month of the war, nearly all Ukrainian regions transferred most of their patients (sometimes, up to a 100%) to take-home dosing (Supplementary Figure S1) – a trend confirmed by the provider survey, in which 67.8% of respondents said that since the beginning of the war they shifted most of their patients to take-home medications with no major differences by region (Supplementary Table S9). According to the official reporting, as of April 1, 2022, only 5.6% of patients across the country were on daily supervised treatment compared to 15.1% as of February 1, 2022 (Public Health Center of the Ministry of Health of Ukraine, 2014–2023). However, in mid-summer of 2022, the proportion of patients receiving daily supervised dosing increased to 8.8% - a trend that continued through January 2023 when this proportion reached 9.4% - still below the pre-war level of 15.1%. It is unclear whether doctors shifted some patients back to daily clinic visits, or the increase observed since April reflects the fact that new patients are formally required to receive supervised dosing until they stabilize.
One of the goals of the Order #409, which allowed providing patients with up to 30-day MOUD supply, was to prevent treatment interruptions and related negative outcomes among displaced patients. Individual-level data to assess the extent of MOUD interruption among displaced patients is unavailable but the high number of re-enrollments compared to relocation-related discharges suggests that displaced patients likely benefited from this policy. Unlike a nearly universal increase in the proportion of patients receiving take-home dosing, adoption of increased duration of take-home dosing was highly variable across regions. In the patient survey, none of the patients in Rivne, Ivano-Frankivsk and Lviv – regions in the west far from the frontline – reported getting more than 10 days of take-home medications. At the same time, between 79–97% of patients from the regions located close to the frontline – Poltava, Kryvyi Rih, Mykolaiv, and Odesa – reported receiving 11–30-day take-home MOUD (Supplemental Table S10). The highest proportion (96.6%) was reported in Kryvyi Rih located in Dnipropetrovsk region, which accepted a large influx of displaced patients (Figure 2). During regular calls between the PHC and MOUD providers, concerns have been raised that some patients were trying to obtain take-home medications at multiple sites around the same time, which may explain reluctance of some providers to increase take-home dosing duration unless it was necessary.
Service delivery: Reduction of MOUD doses
Under the medication supply uncertainty and faced with an influx of patients, many clinics decided to conserve medications by reducing MOUD doses to current patients. In the patient survey, 20.9% of participants reported that their MOUD dose was reduced since the war started with highly variable proportions across regions ranging from 0% in Mykolaiv to 79.3% in Poltava (Supplementary Table S11). This variability reflects different decisions made by regional MOUD providers with respect to the strategy to address potential medication shortages (Ivasiy et al., 2022). While some clinics prioritized current patients by restricting new enrollments, others chose to reduce doses to current patients to accommodate new and migrating patients.
Regional analysis of the provider survey shows similar findings on dose reductions, although proportions cannot be directly compared to those reported by patients (Supplementary Table S12). Overall, 24.5% of providers said that MOUD doses at their site had to be reduced to avoid potential treatment interruption, with the highest proportions reported in Kyiv (75.0%), Kharkiv (66.7%), and Poltava (54.5%). Interestingly, in Lviv – a region that enrolled most internally displaced patients (Figure 2) – a relatively small proportion of patients (14.5%) and providers (14.3%) reported dose reductions, which may be related to the adoption of an alternative medication conservation approach. Anecdotal reports suggest that in Lviv doctors encouraged patients to purchase medications from pharmacies during the period of high uncertainty (Ivasiy et al., 2022).
Figure 3 shows methadone dose changes between January 2022 – January 2023 among inducted stable patients across all governmental MOUD sites in Ukraine. The proportion of patients receiving less than 60 mg/day (considered to be a low therapeutic dose) increased from 9.8% in January to 14.1% in April, when it was the highest, but returned to the pre-war level by August and has been slowly going down since then. While the proportion of patients receiving a recommended therapeutic dose between 80–120 mg/day increased from 43.3% in January 2022 to 49.1% in January 2023, a uniform dose reduction led to substantially fewer patients receiving over 120 mg/day. The respective proportion decreased from 26.5% in January 2022 to 15.7% in May but has been slowly increasing since then up to 18.6% in January 2023. Trends in buprenorphine doses were similar.
Figure 3: Methadone doses in Ukraine: January 2022 – January 2023.
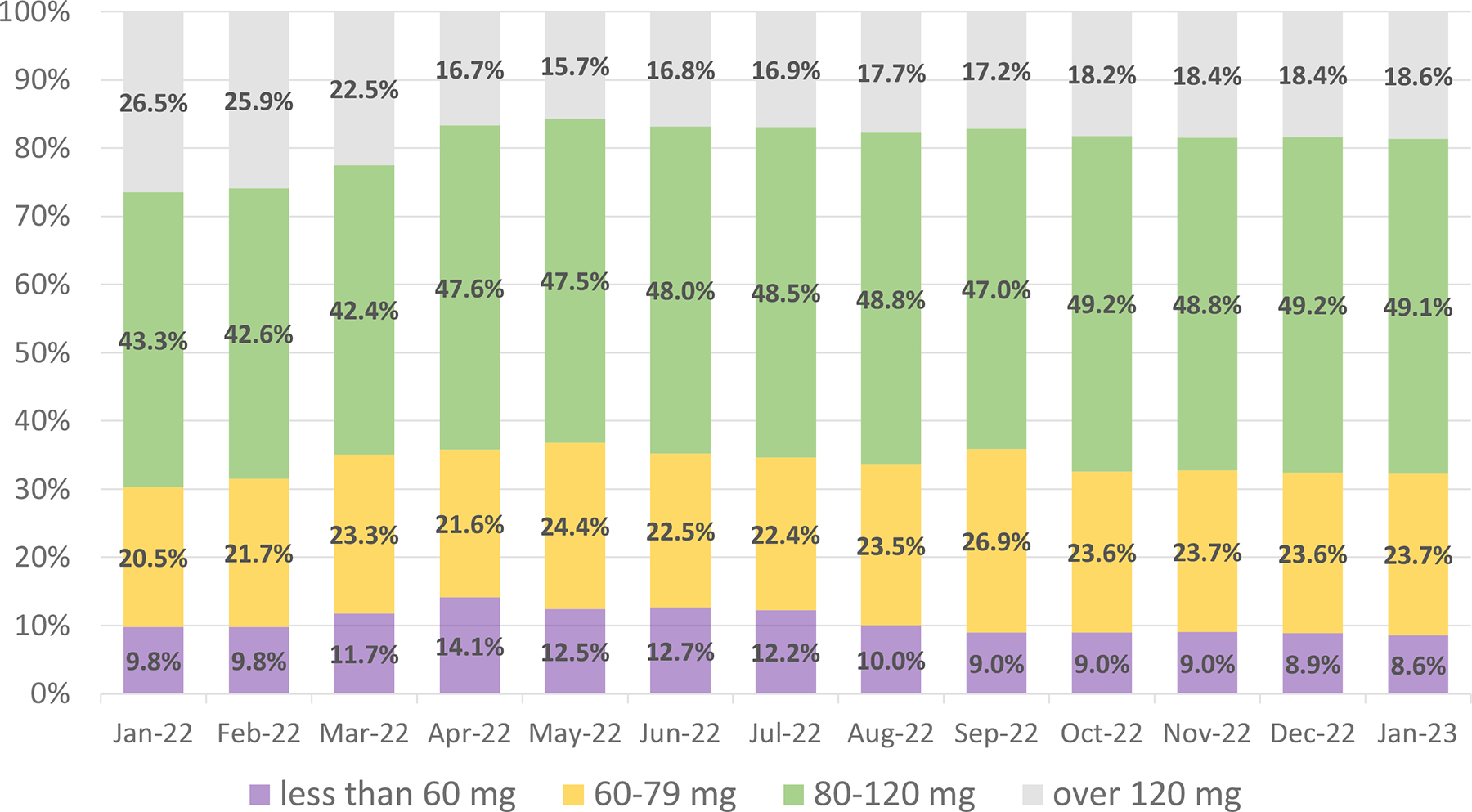
Proportion of inducted and stable MOUD patients in governmental clinics receiving methadone dose within a given range.
Reduction in MOUD dose may precipitate withdrawal symptoms and puts patients at risk of increased illicit drug consumption. In the patient survey, 22.1% of respondents said that in the last 30 days they had taken a higher medication dose than prescribed, primarily due to withdrawal symptoms (54.8%) and anxiety (47.7%); and 38.7% said that they would prefer receiving a higher medication dose. Responses differed substantially across regions (Supplementary Table S11). In Poltava, where almost 80% of patients reported dose reductions, and where 61.2% of patients expressed the desire to receive a higher dose, only 2.6% of patients said that they had taken a higher dose than prescribed. A similar proportion – 3.1% - was reported in Kryvyi Rih, but patients in Kryvyi Rih were receiving higher MOUD doses on average, did not experience major dose reductions, and very few of them (6.8%) expressed the desire to increase the dose. Interestingly, patients in Poltava and Kryvyi Rih reported the lowest prevalence of illicit drug use in the last 30 days (Supplementary Table S13), suggesting that access to illicit drugs may play a role in patients’ decisions to occasionally self-administer a higher MOUD dose. In places where access to illicit opioids may be limited – such as Poltava – patients could adopt MOUD conservation approach despite dose reduction and receiving longer-term take-home MOUD (Supplementary Tables S10 and S11). Overall, however, patients reported no differences in illicit drug consumption between the last 30 days and the 30 days before the war, suggesting that reduction in MOUD doses did not trigger substantial increases in illicit drug use, possibly due to limited access to illicit drugs (Table 1 and Supplementary Table S13).
Table 1:
Illicit drug use among MOUD patients in the last 30 days before the survey compared to 30 days before the start of the war (N=700).
| Substance | Used in the last 30 days before the survey: n (%) | Used in the 30 days before the war: n (%) | p-value* |
|---|---|---|---|
| Cannabis | 203 (29.0) | 217 (31.0) | 0.104 |
| Illicit opioids | 119 (17.0) | 143 (20.4) | 0.006 |
| Stimulants | 68 (9.7) | 69 (9.9) | 0.869 |
| Tranquilizers, antihistamines, and hypnotics | 230 (32.9) | 216 (30.9) | 0.066 |
p-value for McNemar’s test
While patients in many regions of Ukraine faced at least temporary medication dose reductions, discharges unrelated to displacement did not increase substantially. Pre-war, the average monthly proportion of patients who dropped out of treatment for reasons other than relocation was 1.4% and increased to 1.8% during the year after the war (Supplementary Table S2) (Public Health Center of the Ministry of Health of Ukraine, 2014–2023). In the patient survey, only 5% of participants reported missing an MOUD dose in the last 30 days, and none of them did so due to a lack of medication on site. At the same time, 10.5% of MOUD patients on ART reported an interruption of their HIV treatment since the war started – an important finding that requires further investigation.
Service delivery: Situation in temporarily occupied and active conflict regions
After the Russian troop withdrawal from northern regions in April 2022, five regions of Ukraine – Donetsk, Kharkiv, Kherson, Luhansk, and Zaporizhzhia - remained fully or partially occupied (Figure 2). A full account of what has been happening in occupied areas is impossible to obtain until these regions are liberated. It is clear, however, that patients who stayed in these regions are in critical situation. After the annexation of Crimea in 2014, MOUD programs there were quickly terminated leading to many deaths among patients who did not relocate (Carroll, 2019). Cases of MOUD patients and activists Andrii Yarovyi and Natalia Zelenina, who were illegally detained in occupied areas of Donetsk and Luhansk regions before the war, and released during prisoner swaps, offer examples of atrocious human rights violations (Hromadske News, 2022; International Charitable Foundation “Alliance for Public Health”, 2019, 2020; Ukrainian Parliament Commissioner for Human Rights, 2022). Patients who did not move out of occupied territories are likely facing the same risks.
Being fully under control of Ukraine before the war, Kherson region provided MOUD to 669 patients as of March 1, 2022. Despite occupation early in the war, 7 out of 8 sites in the region continued working, dispensing the remaining stores of the medications. In June, representatives of Russian-appointed administration confiscated the remaining stockpile of MOUD from the largest site in the city of Kherson. MOUD sites in Kherson region continued sending data updates to the PHC through August 1, when they reported that 442 patients were in treatment. The discharge of all remaining patients in Kherson led to a drop in the number of patients nationwide observed as of September 1 (Figure 1). The last operating MOUD site in Kherson region located in a small town Oleshky was shut down in October. Russian forces withdrew from the city of Kherson in November; however, a major part of the region continues to be under their control. According to the MOUD site staff from Kherson city, many patients managed to relocate to the neighboring sites during the occupation. In December 2022, after the site received the first post-occupation shipment of MOUD, most patients returned to the city.
MOUD programs in Luhansk region were completely terminated in May 2022, soon after invasion. The region has been partially occupied by Russian-supported separatists since 2014. Despite being a large densely populated region with a high prevalence of opioid use disorder (Berleva & Sazonova, 2017), as of February 1, 2022 only 366 patients were receiving MOUD across 3 sites in government-controlled areas of Luhansk region. The only two sites in Sieverodonetsk and Svatovo that continued operation after the invasion were forced to close in early May due intensive fighting and advancement of the Russian forces.
Despite the risks, most MOUD sites located in areas neighboring the frontline have continued serving their patients. Like Luhansk, Donetsk region has been partially occupied since 2014. Before the war, there were 863 MOUD patients in the region receiving treatment across 9 sites. After the tragic events in Mariupol (Office of the United Nations High Commissioner for Human Rights, June 16, 2022), two sites located in the city were destroyed. One site located in Bakhmut closed in June as the city became a target of daily shelling. As of February 1, 2023, 329 patients continued receiving treatment at three sites that remained open.
Several MOUD sites in Kharkiv, Chernihiv, Mykolaiv, and Zaporizhzhia regions closed due to intensive fighting, destruction of facilities, or occupation. At the same time, most sites in government-controlled areas remained open and operational since the beginning of the war with a small reduction in the number of patients (Public Health Center of the Ministry of Health of Ukraine, 2014–2023). A temporary disruption of MOUD delivery at municipal clinics located in the city of Kharkiv was managed via partnership with private clinics (Bromberg et al., 2022; Bromberg et al., 2023; Ivanchuk, 2023). The occupied parts of Kharkiv region have been liberated during the counter-offensive of Ukrainian forces in September 2022. PHC is currently working with local health authorities to reopen the previously closed sites in the area, but the progress is slow due to destruction of facilities.
Discussion: Lessons learned and implications for future response
It is impossible to be fully prepared for what war brings. While MOUD delivery in Ukraine has suffered from the military conflict, the extent of disruption in the areas controlled by Ukraine has been contained by the unprecedented efforts of multiple stakeholders at all levels. International aid, particularly from the GFATM, dedication of medical providers, and collaboration between the government and NGOs avoided major MOUD delivery hiatus to hundreds of patients. Russia’s attacks on Ukraine did not start in 2022 with the full-scale invasion. Annexation of Crimea in 2014 and a hybrid war in Donetsk and Luhansk regions were hard lessons that taught Ukraine to mobilize and act quickly when the need arises. Despite legal obstacles, the government demonstrated flexibility and partnered with civil society and the private sector to minimize MOUD interruptions where possible. During the first weeks of the war, the Ministry of Health enacted important legislative changes with the goal to minimize treatment interruptions and improve program resiliency under uncertainty. Experience of the first year of the war showed that these efforts, while they could be further optimized, were largely effective. Many of the successes can be attributed to the dedication of doctors and other service providers, who continued providing life-saving treatment despite the risks, even in occupied areas. Somewhat surprisingly, during the first year of the war, the number of MOUD patients in governmental clinics of Ukraine increased by about 17% despite forced treatment termination among patients who remained in occupied regions. Changes in the illicit drugs supply, patient transitions from private clinics, and increased capacity of existing sites to accept new patients are likely the main drivers of the observed increase. Changes in the coverage of private clinics is difficult to assess, but limited data suggest that the total number of patients served by these clinics likely increased as well.
The first response efforts during the early days of the war naturally focused on ensuring treatment continuation among existing patients and were extremely important. At the same time, as Ukraine’s experience showed, it is vital to prepare for a substantial influx of new and migrating patients that may vary across regions. Capacity to accept new patients depends on the medication supply and clinic staffing. The former can be managed through a flexible distribution system that minimizes delays between medication ordering and shipments, as was done in Ukraine. Orders #425 and #665 allowing larger MOUD stockpiles at the sites and flexible MOUD distribution remain active as of March 2023. The latter can be achieved by either increasing staffing capacity or optimizing medication delivery to patients. MOUD are controlled substances that typically require daily intake supervision in Ukraine and elsewhere. The COVID-19 pandemic catalyzed the shift to take-home MOUD (Meteliuk et al., 2021), which was further expanded due to the war and demonstrated feasibility in serving more patients within existing staffing resources. The Order #409, which allowed a 30-day take-home medication supply and proved to be effective in sustaining the MOUD program during the major wave of internal migration, was, however, terminated in November 2022 upon the official request by the Ministry of Justice. At that time, major patient migration was no longer happening, and concerns about increased medication diversion in the absence of a centralized patient registry, suboptimal treatment effectiveness under less frequent clinical care, and potential for increased risk of overdose began prevailing. Several studies conducted in the US to investigate potential risks following pandemic related MOUD take-home dosing expansion did not find increases in the risk of overdose or death and are reassuring (Krawczyk et al., 2023). Studies evaluating outcomes of expanded take-home dosing and piloting interventions to improve take-home MOUD adherence in Ukraine are underway and will provide evidence for a possible reenactment of the 30-day take-home dispensing.
During the first year of the war in Ukraine, many patients transitioned from private to governmental clinics, sometimes without proper medical documentation (Ivanchuk, 2023). In those instances, governmental clinics implemented a standard treatment induction protocol that was sometimes criticized for putting patients at risk of withdrawal (Bromberg et al., 2022), although critics did not include recommendations regarding the alternative course of action (Ivanchuk, 2023). Implementation of the national MOUD patient registry – a process which is currently underway – would address many of these challenges. Once fully operational, it will provide the means for more efficient patient monitoring to reduce diversion and expedite patient transfers between clinics, which has been problematic during the period of most active patient migration. It will also provide real-time information on the number of patients and MOUD needs across regions. Further strengthening communication, reporting, and partnerships between the PHC and private clinics is instrumental in establishing a safety net for patients in the time of crisis and ensure fair medication distribution in case there is a shortage (Altice, Bromberg, Klepikov, et al., 2022). Given the limited information about patients from private clinics, it is important that future research efforts address this gap.
A risk of intensified invasion remains high in many areas of Ukraine, therefore maintaining the state of emergency preparedness is warranted. Maintaining strategic stocks of MOUD at local levels is critical to reduce the risk of interruptions or doses reduction while keeping current supply chains operational. A single operating local manufacturer of MOUD in Ukraine prioritized governmental orders putting patients in private clinics at risk of treatment disruption, especially in the situation of increased MOUD demand across both governmental and private clinics (Public Health Center of the Ministry of Health of Ukraine, 2022a). Reliance on one manufacturing facility within the country to ensure uninterrupted access to treatment for over 20,000 patients, including those in private clinics, is a high-risk scenario. While national MOUD supply has so far been sufficient, it is important to diversify the sources of MOUD procurement in the country. A key step in this direction is de-regulation of import of controlled substances to allow faster transportation of international humanitarian aid across the border.
Despite all efforts, many MOUD sites in Ukraine, including those that accepted a major influx of internally displaced patients, had to implement medication dose reduction for existing patients to extend the medication supply and avoid interruptions. While this measure likely affected patient well-being and increased the frequency of withdrawal symptoms, patients did not report significant increases in illicit drug consumption compared to the pre-war period. In a time of crisis, a moderate temporary MOUD dose reduction may be an acceptable measure to manage equity while minimizing treatment drop-out.
The number of MOUD patients who remain in the areas controlled by Russia is unknown. Sadly, little can be done to help them beyond the efforts to organize safe evacuation corridors. Occupation of eastern and southern Ukraine during March and April 2022 was swift and evacuation efforts were jeopardized by Russian attacks on civilians and humanitarians. This creates a moral dilemma with respect to MOUD delivery to the regions at immediate risk of assault or occupation. Termination of MOUD supply puts patients at risk of interruption, while continuing MOUD delivery discourages patients from evacuation ordered by the government. Although there is no easy solution in situations like this, providing patients with the maximum possible medication supply, information, and assistance in relocation to another treatment site is likely an optimal decision given the risks they face in case of occupation.
Early in the war, internal patient migration was high and largely unmanaged. Patients who left their homes had to navigate the process of re-engaging in MOUD care on their own, causing stress, anxiety, and uncertainty. Although PHC established a chat bot to provide patients with information, these efforts could be strengthened by providing the most vulnerable with assistance to find housing and means of support while they were forced to flee their homes. The role of civil society in responding to the crisis cannot be overstated. Since the beginning of the war, Ukrainian NGOs have made enormous efforts to continue providing services to people who inject drugs, people living with HIV, and other vulnerable populations. Partnering with NGOs, such as the Association of MOUD patients of Ukraine and others, to organize a support network for displaced patients has been an important step to improve continuity of care.
Supplementary Material
Acknowledgements
We thank all health care workers and public health professionals in Ukraine for their remarkable resilience and commitment to serving people in this extremely challenging context, often risking their lives. We also thank international organizations and the global health community for their unwavering support of Ukraine, which is invaluable in overcoming the crisis. We thank Valeria Akbirova, Myroslava Filippovych, Natalia Saichuk, Natalia Tytarenko, Olena Makarenko, Anastasiya Forostyana for their crucial role in implementation of the surveys.
Research reported in this paper was supported by the grants “Strengthening HIV Treatment, Laboratory Services, Medication Assisted Therapy, and Program Monitoring in Ukraine under the President’s Emergency Plan for AIDS Relief (PEPFAR)” (NU2GGH002375) and “Gain Momentum In Reducing TB/ HIV Burden In Ukraine” from the Global Fund to Fight AIDS, Tuberculosis, and Malaria (GFATM). KD was supported by the Fogarty International Center of the National Institutes of Health (NIH) (grant D43TW010562 to the Research Foundation of the State University of New York). The funders of the studies had no role in design, data collection, data analysis, data interpretation, or writing of the report. The content is solely the responsibility of the authors and does not necessarily represent the official views of PEPFAR, GFATM and NIH.
Footnotes
Declarations of interests
The authors declare no competing interests.
References
- Altice FL, Bromberg DJ, Dvoriak S, Meteliuk A, Pykalo I, Islam Z, Azbel L, & Madden LM (2022). Extending a lifeline to people with HIV and opioid use disorder during the war in Ukraine. Lancet Public Health, 7(5), e482–e484. 10.1016/S2468-2667(22)00083-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Bromberg DJ, Klepikov A, Barzilay EJ, Islam Z, Dvoriak S, Farnum SO, & Madden LM (2022). Collaborative learning and response to opioid misuse and HIV prevention in Ukraine during war. Lancet Psychiatry, 9(11), 852–854. 10.1016/S2215-0366(22)00318-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berleva H, & Sazonova Y (2017). Analytical report “Estimation of the size of populations most-at-risk for HIV infection in Ukraine”. ICF “Alliance for Public Health”. Retrieved Feb 27, 2023 from http://aph.org.ua/wp-content/uploads/2016/12/o4sn16.pdf [Google Scholar]
- Bromberg DJ, Madden LM, Meteliuk A, Ivasiy R, de Leon SJG, Klyucharyov K, & Altice FL (2022). Medications for opioid use disorder during war in Ukraine: Innovations in public and private clinic cooperation. Lancet Reg Health Eur, 20, 100490. 10.1016/j.lanepe.2022.100490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bromberg DJ, Madden LM, Meteliuk A, Ivasiy R, Galvez de Leon SJ, Klyucharyov K, & Altice FL (2023). “Medications for opioid use disorder during the war in Ukraine: a more comprehensive view on the government response-Authors’ reply”. Lancet Reg Health Eur, 26, 100583. 10.1016/j.lanepe.2023.100583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabinet of Ministers of Ukraine. (2019). The National Strategy on response to HIV/AIDS, tuberculosis and viral hepatitis until 2030. Retrieved Aug 14, 2020 from https://zakon.rada.gov.ua/laws/show/1415-2019-%D1%80#Text
- Carroll JJ (2019). Sovereign Rules and Rearrangements: Banning Methadone in Occupied Crimea. Med Anthropol, 38(6), 508–522. 10.1080/01459740.2018.1532422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dmitrieva A, Stepanov V, & Mazhnaya A (2022). Managing Opioid Agonist Therapy in the Post-Soviet Limbo. Contemporary Drug Problems, 49(2), 148–169. 10.1177/00914509211063587 [DOI] [Google Scholar]
- Hromadske News. (2022). “Would be better if you killed someone”: 5 years in the “DNR” captivity. Retrieved Feb 27, 2023 from https://hromadske.ua/en/posts/would-be-better-if-you-killed-someone-5-years-in-the-dnr-captivity
- International Charitable Foundation “Alliance for Public Health”. (2019). Information about illegally convicted Andrii Yarovyi. Retrieved Feb 27, 2023 from https://aph.org.ua/en/news/information-about-illegally-convicted-andrii-yarovyi/
- International Charitable Foundation “Alliance for Public Health”. (2020). Andrii Yarovyi is back home after being captured ! Retrieved Feb 27, 2023 from https://aph.org.ua/en/news/andrii-yarovyi-is-back-home-after-being-captured/
- Ivanchuk I (2023). Medications for opioid use disorder during the war in Ukraine: a more comprehensive view on the government response. Lancet Reg Health Eur, 26, 100582. 10.1016/j.lanepe.2022.100582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivasiy R, Galvez de Leon SJ, Meteliuk A, Fomenko T, Pykalo I, Bromberg DJ, Madden LM, Farnum SO, Islam Z, & Altice FL (2022). Responding to health policy recommendations on managing opioid use disorder during Russia’s invasion of Ukraine: Divergent responses from the frontline to the west. Front Public Health, 10, 1044677. 10.3389/fpubh.2022.1044677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawczyk N, Rivera BD, Levin E, & Dooling BCE (2023). Synthesising evidence of the effects of COVID-19 regulatory changes on methadone treatment for opioid use disorder: implications for policy. Lancet Public Health, 8(3), e238–e246. 10.1016/S2468-2667(23)00023-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meteliuk A, Galvez de Leon SJ, Madden LM, Pykalo I, Fomenko T, Filippovych M, Farnum SO, Dvoryak S, Islam ZM, & Altice FL (2021). Rapid transitional response to the COVID-19 pandemic by opioid agonist treatment programs in Ukraine. J Subst Abuse Treat, 121, 108164. 10.1016/j.jsat.2020.108164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the United Nations High Commissioner for Human Rights. (June 16, 2022). High Commissioner updates the Human Rights Council on Mariupol, Ukraine. Retrieved Nov 23, 2022 from https://www.ohchr.org/en/statements/2022/06/high-commissioner-updates-human-rights-council-mariupol-ukraine
- Office of the United Nations High Commissioner for Human Rights. (May 5, 2022). Ukraine: Millions of displaced traumatised and urgently need help, say experts. Retrieved Nov 23, 2022 from https://www.ohchr.org/en/press-releases/2022/05/ukraine-millions-displaced-traumatised-and-urgently-need-help-say-experts
- Papanicolas I, Rajan D, Karanikolos M, Soucat A, & Figueras J (2022). Health system performance assessment: A framework for policy analysis. Geneva: World Health Organization. [PubMed] [Google Scholar]
- Public Health Center of the Ministry of Health of Ukraine. (2014–2023). Official statistics on the opioid substitution treatment program in Ukraine. Retrieved Feb 27, 2023 from https://phc.org.ua/kontrol-zakhvoryuvan/zalezhnist-vid-psikhoaktivnikh-rechovin/zamisna-pidtrimuvalna-terapiya-zpt/statistika-zpt
- Public Health Center of the Ministry of Health of Ukraine. (2022a). National Response of HIV, TB, VH and SMT Programs to Full-scale Russian Invasion. Retrieved Feb 27, 2023 from https://www.phc.org.ua/sites/default/files/users/user92/Report_eng_final_compressed_1.pdf
- Public Health Center of the Ministry of Health of Ukraine. (2022b). Situational reports on access to opioid substitution treatment in Ukraine (in Ukrainian). Retrieved Feb 27, 2023 from https://phc.org.ua/kontrol-zakhvoryuvan/zalezhnist-vid-psikhoaktivnikh-rechovin/zamisna-pidtrimuvalna-terapiya-zpt/situaciyni-zviti-pid-chas-voennogo-stanu
- Soar Earth. (2022). Map of the approximate situation in Ukraine as of September 2, 2022. Retrieved Nov 15, 2022 from https://soar.earth/maps/13152
- Ukrainian Parliament Commissioner for Human Rights. (2022). Natalia Zelenina, a citizen of Ukraine, has been illegally detained in the ORDO for the fifth year in a row. Retrieved Feb 27, 2023 from https://ombudsman.gov.ua/en/news_details/upovnovazhenij-gromadyanka-ukrayini-nataliya-zelenina-pyatij-rik-pospil-perebuvaye-u-nezakonnomu-uvyaznenni-v-ordo
- UNAIDS. (2023a). Eastern Europe and Central Asia Country Profiles. Retrieved May 5, 2023 from https://www.unaids.org/en/regionscountries/easterneuropeandcentralasia
- UNAIDS. (2023b). Key Populations Atlas. Retrieved May 5, 2023 from https://kpatlas.unaids.org/dashboard
- Vasylyev M, Skrzat-Klapaczynska A, Bernardino JI, Sandulescu O, Gilles C, Libois A, Curran A, Spinner CD, Rowley D, Bickel M, Aichelburg MC, Nozza S, Wensing A, Barber TJ, Waters L, Jordans C, Bramer W, Lakatos B, Tovba L, … European, A. C. S. Y. I. (2022). Unified European support framework to sustain the HIV cascade of care for people living with HIV including in displaced populations of war-struck Ukraine. Lancet HIV, 9(6), e438–e448. 10.1016/S2352-3018(22)00125-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


