In Brief
This study evaluated the correlation between patient-perceived global change in spine-related health status and commonly used patient-reported outcome measures (PROMs) in lumbar spine surgery and found very weak-to-moderate correlations between PROMs and global rating change. These findings suggest that currently used PROMs may not be as sensitive at detecting these changes or may not be adequately reflecting changes in health conditions that are meaningful to patients undergoing lumbar spine surgery.
Keywords: lumbar spine surgery, patient-reported outcome measures, global rating change, PROs, decompression, microdiscectomy, fusion
ABBREVIATIONS : CCI = Charlson Comorbidity Index, GRC = global rating of change, MCS = Mental Component Summary, ODI = Oswestry Disability Index, PCS = Physical Component Summary, PROM = patient-reported outcome measure, PROMIS-PF = Patient-Reported Outcomes Measurement Information System–Physical Function, SF-12 = 12-Item Short Form Health Survey, VAS = visual analog scale
Abstract
OBJECTIVE
The aim of this study was to assess the correlation between patient-perceived changes in health and commonly utilized patient-reported outcome measures (PROMs) in lumbar spine surgery.
METHODS
This was a retrospective review of prospectively collected data on consecutive patients who underwent lumbar microdiscectomy, lumbar decompression, or lumbar fusion at a single academic institution from 2017 to 2023. Correlation between the global rating of change (GRC) questionnaire, a 5-item Likert scale (much better, slightly better, about the same, slightly worse, and much worse), and PROMs (Oswestry Disability Index, visual analog scale for back and leg pain, 12-Item Short Form Health Survey Physical Component Summary and Mental Component Summary, and PROMIS physical function) was assessed using Spearman’s rank correlation coefficients.
RESULTS
A total of 1871 patients (397 microdiscectomies, 965 decompressions, and 509 fusions) were included. A majority of patients in each group rated their lumbar condition as much better at each postoperative time point compared with preoperatively and reported improved health status at each postoperative time point compared with the previous follow-up visit. Statistically significant but weak to moderate correlations were found between GRC and change in PROM scores from the preoperative time point. Correlation between GRC and change in PROM scores from the prior visit showed some statistically significant correlations, but the strengths ranged from very weak to weak.
CONCLUSIONS
A majority of patients undergoing lumbar microdiscectomy, decompression, or fusion endorsed notable improvements in health status in the early postoperative period and continued to improve at late follow-up. However, commonly used PROMs demonstrated very weak to moderate correlations with patient-perceived changes in overall lumbar spine–related health status as determined by GRC. Therefore, currently used PROMs may not be as sensitive at detecting these changes or may not be adequately reflecting changes in health conditions that are meaningful to patients undergoing lumbar spine surgery.
In light of the shift from fee-for-service to value-based care in spine surgery, the importance of understanding patients’ perception of their health status has increased drastically.1 Thus, patient-reported outcome measures (PROMs) are a valuable tool in quantitatively measuring and tracking clinical outcomes data and evaluating patient health preoperatively and postoperatively. Commonly used PROMs during spine surgery that assess function, pain, and quality of life, such as the Oswestry Disability Index (ODI), visual analog scale (VAS) back and leg, 12-Item Short Form Health Survey (SF-12) Physical Component Summary (PCS) and Mental Component Summary (MCS), and Patient-Reported Outcomes Measurement Information System–Physical Function (PROMIS-PF), have been demonstrated as reliable and valid instruments to evaluate lumbar spinal disorders.2–5 The global rating of change (GRC) is a patient-reported outcome measure that assesses whether a patient’s condition has improved, declined, or remained the same compared with prior to treatment or an earlier time point. It has grown in popularity in clinical practice as a result of its ease and efficiency of use as well as its applicability to a wide range of musculoskeletal conditions.6,7 Unlike other outcome measures that focus on a specific domain of a patient’s health, such as disability, or quality of life, the "global" nature of GRC allows patients themselves to focus on what they consider to be most relevant in assessing their own health status.6
Previously, studies have examined the utility and validity of various PROMs in lumbar spine surgery.8–14 However, there is currently a paucity of data regarding how these PROMs correlate with patients’ own perceptions of change in health status postoperatively. Thus, the purpose of this study was to evaluate the correlation between commonly used PROMs and patients’ perceived changes in spine-related health status, assessed using the GRC, in patients undergoing lumbar spine surgery.
Methods
Institutional review board approval was obtained for this study. All data were collected and managed using REDCap (Research Electronic Data Capture) hosted at Weill Cornell Medicine Clinical and Translational Science Center supported by the National Center for Advancing Translational Science of the National Institutes of Health under award number UL1 TR002384. REDCap is a secure, web-based software platform designed to support data capture for research studies.15,16
Study Design and Patient Population
This was a retrospective review of a prospectively maintained multisurgeon institutional registry at a single academic institution. The registry was queried for consecutive patients who underwent lumbar microdiscectomy, lumbar decompression, or lumbar fusion between 2017 and 2023. For inclusion in this study, patients were required to have completed at least one PROM questionnaire preoperatively and the same PROM questionnaire at least one time point postoperatively, along with the GRC questionnaire at the same time point. For patients who underwent revision surgery or reoperations at other levels in the lumbar spine, PROMs data collection was stopped at the time of the revision to reflect the outcomes of only the index operation. All surgeries were performed by fellowship-trained spine surgeons.
Data Collection
Demographic data included age, BMI, sex, age-adjusted Charlson Comorbidity Index (CCI), race, insurance, and American Society of Anesthesiologists Physical Status class. Perioperative and postoperative data included the number of operative levels, estimated blood loss (in mL), operative time (in minutes), and postsurgical length of stay (in hours).
PROMs were collected prospectively as standard of care. The following PROMs were collected preoperatively and at 6 weeks, 12 weeks, 6 months, and 1 year postoperatively: ODI, VAS for back and leg pain, SF-12 PCS and MCS, and PROMIS-PF. Additionally, at each postoperative visit, patients were administered a GRC questionnaire, which assessed the patient’s spine condition compared with before surgery and their previous visit. This was assessed using a 5-item Likert scale (much better, slightly better, about the same, slightly worse, and much worse).
Statistical Analysis
Demographic, operative, and postoperative variables and PROMs were summarized as means and standard deviations for continuous variables and percentages for categorical variables. The correlation between GRC and changes in PROM scores at each postoperative time point was assessed using Spearman’s rank correlation coefficients. The strength of correlation coefficients was defined as previously described: very weak (0.00–0.20), weak (0.21–0.40), moderate (0.41–0.6), strong (0.61–0.8), and very strong (0.81–1.00). Statistical significance was defined with a Bonferroni-adjusted p value set at < 0.0012 to correct for multiple comparisons. All statistical analyses were conducted using IBM SPSS (version 29, IBM Corp.).
Results
Demographic, Operative, and Postoperative Variables
Demographics and perioperative data are shown in Table 1. A total of 1871 patients were included; 397 patients underwent microdiscectomy (mean age 48.38 years; mean BMI 26.76 kg/m2), 965 patients underwent decompression (mean age 59.12 years, mean BMI 27.47 kg/m2), and 509 patients underwent fusion (mean age 59.52 years, mean BMI 28.09 kg/m2). The age-adjusted CCIs for the microdiscectomy, decompression, and fusion patients were 1.22, 2.37, and 2.18, respectively. The majority of patients were Caucasian (microdiscectomy, 82.4%; decompression, 84.6%; and fusion, 83.3%), had commercial or private insurance (microdiscectomy, 77.3%; decompression, 57.7%; and fusion, 69.0%), were in ASA class II (microdiscectomy, 66.2%; decompression, 73.6%; and fusion, 80.4%), and had 1 level treated (microdiscectomy, 97.0%; decompression, 82.5%; and fusion, 74.5%).
TABLE 1.
Patient demographics and operative data
| Microdiscectomy | Decompression | Fusion | |
|---|---|---|---|
| No. of patients |
397 |
965 |
509 |
| Age, yrs |
48.38 ± 15.35 |
59.12 ± 17.06 |
59.52 ± 12.38 |
| BMI, kg/m2 |
26.76 ± 5.04 |
27.47 ± 4.98 |
28.09 ± 5.96 |
| Sex |
|
|
|
| Male |
237 (59.7) |
589 (61.0) |
253 (49.7) |
| Female |
160 (40.3) |
376 (39.0) |
256 (50.3) |
| Age-adjusted CCI |
1.22 ± 1.63 |
2.37 ± 2.13 |
2.18 ± 1.68 |
| Race |
|
|
|
| White or Caucasian |
327 (82.4) |
816 (84.6) |
424 (83.3) |
| Black or African American |
11 (2.8) |
27 (2.8) |
23 (4.5) |
| American Indian or Alaska Native |
1 (0.3) |
2 (0.2) |
0 (0.0) |
| Asian |
17 (4.3) |
39 (4.0) |
15 (2.9) |
| Other |
22 (5.5) |
44 (4.6) |
26 (5.1) |
| Unavailable |
8 (2.0) |
15 (1.6) |
9 (1.8) |
| Patient declined |
11 (2.8) |
22 (2.3) |
12 (2.4) |
| Insurance type |
|
|
|
| Medicare |
55 (13.9) |
341 (35.3) |
118 (23.2) |
| Workers’ compensation |
6 (1.5) |
8 (0.8) |
14 (2.8) |
| Commercial/private |
307 (77.3) |
557 (57.7) |
351 (69.0) |
| Medicaid |
5 (1.3) |
7 (0.7) |
3 (0.6) |
| Other |
22 (5.5) |
46 (4.8) |
21 (4.1) |
| Unavailable |
2 (0.5) |
6 (0.6) |
2 (0.4) |
| ASA Class |
|
|
|
| I |
102 (25.7) |
128 (13.3) |
46 (9.0) |
| II |
263 (66.2) |
710 (73.6) |
409 (80.4) |
| III |
24 (6.0) |
109 (11.3) |
50 (9.8) |
| IV |
3 (0.8) |
3 (0.3) |
0 (0.0) |
| Missing |
5 (1.3) |
15 (1.6) |
4 (0.8) |
| No. of levels |
|
|
|
| 1 |
385 (97.0) |
796 (82.5) |
379 (74.5) |
| 2 |
11 (2.8) |
144 (14.9) |
106 (20.8) |
| 3 |
1 (0.3) |
22 (2.3) |
24 (4.7) |
| 4 |
0 (0.0) |
2 (0.2) |
0 (0.0) |
| 5 |
0 (0.0) |
1 (0.1) |
0 (0.0) |
| EBL, mL |
21.90 ± 27.83 |
21.01 ± 56.22 |
102.33 ± 184.23 |
| Operative time, mins |
60.56 ± 28.75 |
71.81 ± 35.62 |
144.39 ± 80.40 |
| Postoperative LOS, hrs | 10.67 ± 16.58 | 16.65 ± 31.04 | 43.54 ± 40.29 |
ASA = American Society of Anesthesiologists; EBL = estimated blood loss; LOS = length of stay.
Values are presented as the number of patients (%) or mean ± SD.
Global Rating Change
GRCs at each time point are shown in Tables 2 and 3. Compared with their preoperative condition, 70.0%, 74.0%, 76.1%, and 80.8% of microdiscectomy patients described their lumbar spine condition as "much better" at 6 weeks, 12 weeks, 6 months, and 1 year, respectively. Compared with their condition at previous time points, 43.6%, 46.8%, and 59.0% of microdiscectomy patients described their lumbar spine condition as "much better" at 6 weeks to 12 weeks, 12 weeks to 6 months, and 6 months to 1 year, respectively. Compared with their preoperative condition, 66.6%, 70.5%, 71.7%, and 71.1% of decompression patients described their lumbar spine condition as "much better" at 6 weeks, 12 weeks, 6 months, and 1 year, respectively. Compared with their condition at previous time points, 41.6%, 46.3%, and 51.2% of decompression patients described their lumbar spine condition as "much better" at 6 weeks to 12 weeks, 12 weeks to 6 months, and 6 months to 1 year, respectively. Compared with their preoperative condition, 59.5%, 69.1%, 73.2%, and 71.8% of fusion patients described their lumbar spine condition as "much better" at 6 weeks, 12 weeks, 6 months, and 1 year, respectively. Compared with their condition at previous time points, 43.8%, 38.6%, and 44.7% of fusion patients described their lumbar spine condition as "much better" at 6 weeks to 12 weeks, 12 weeks to 6 months, and 6 months to 1 year, respectively.
TABLE 2.
Evaluation of GRC from preoperatively
| Preop to 6 wks | Preop to 12 wks | Preop to 6 mos | Preop to 1 yr | |
|---|---|---|---|---|
| Microdiscectomy |
|
|
|
|
| Much better |
189 (70.0) |
151 (74.0) |
143 (76.1) |
135 (80.8) |
| Slightly better |
35 (13.0) |
29 (14.2) |
21 (11.2) |
16 (9.6) |
| About the same |
22 (8.1) |
15 (7.4) |
16 (8.5) |
8 (4.8) |
| Slightly worse |
14 (5.2) |
4 (2.0) |
4 (2.1) |
2 (1.2) |
| Much worse |
10 (3.7) |
5 (2.5) |
4 (2.1) |
6 (3.6) |
| Follow-up % |
68.0 |
51.4 |
47.4 |
42.1 |
| Decompression |
|
|
|
|
| Much better |
449 (66.6) |
390 (70.5) |
362 (71.7) |
318 (71.1) |
| Slightly better |
116 (17.2) |
90 (16.3) |
65 (12.9) |
60 (13.4) |
| About the same |
57 (8.5) |
45 (8.1) |
43 (8.5) |
37 (8.3) |
| Slightly worse |
35 (5.2) |
18 (3.3) |
21 (4.2) |
23 (5.1) |
| Much worse |
17 (2.5) |
10 (1.8) |
14 (2.8) |
9 (2.0) |
| Follow-up % |
69.8 |
57.3 |
52.3 |
46.3 |
| Fusion |
|
|
|
|
| Much better |
200 (59.5) |
210 (69.1) |
216 (73.2) |
191 (71.8) |
| Slightly better |
67 (19.9) |
47 (15.5) |
40 (13.6) |
40 (15.0) |
| About the same |
29 (8.6) |
20 (6.6) |
17 (5.8) |
14 (5.3) |
| Slightly worse |
29 (8.6) |
19 (6.3) |
18 (6.1) |
14 (5.3) |
| Much worse |
11 (3.3) |
8 (2.6) |
4 (1.4) |
7 (2.6) |
| Follow-up % | 66.0 | 59.7 | 58.0 | 52.3 |
Values are presented as the number of patients (%) unless stated otherwise.
TABLE 3.
Evaluation of GRC from the previous visit
| 6 wks to 12 wks | 12 wks to 6 mos | 6 mos to 1 yr | |
|---|---|---|---|
| Microdiscectomy |
|
|
|
| Much better |
89 (43.6) |
88 (46.8) |
98 (59.0) |
| Slightly better |
62 (30.4) |
45 (23.9) |
16 (9.6) |
| About the same |
31 (15.2) |
43 (22.9) |
36 (21.7) |
| Slightly worse |
18 (8.8) |
8 (4.3) |
11 (6.6) |
| Much worse |
4 (2.0) |
4 (2.1) |
5 (3.0) |
| Follow-up % |
51.4 |
47.4 |
41.8 |
| Decompression |
|
|
|
| Much better |
230 (41.6) |
234 (46.3) |
228 (51.2) |
| Slightly better |
153 (27.7) |
111 (22.0) |
77 (17.3) |
| About the same |
122 (22.1) |
110 (21.8) |
97 (21.8) |
| Slightly worse |
37 (6.7) |
40 (7.9) |
35 (7.9) |
| Much worse |
11 (2.0) |
10 (2.0) |
8 (1.8) |
| Follow-up % |
57.3 |
52.3 |
46.1 |
| Fusion |
|
|
|
| Much better |
133 (43.8) |
113 (38.6) |
119 (44.7) |
| Slightly better |
106 (34.9) |
98 (33.4) |
66 (24.8) |
| About the same |
43 (14.1) |
53 (18.1) |
60 (22.6) |
| Slightly worse |
18 (5.9) |
26 (8.9) |
15 (5.6) |
| Much worse |
4 (1.3) |
3 (1.0) |
6 (2.3) |
| Follow-up % | 59.7 | 57.6 | 52.3 |
Values are presented as the number of patients (%) unless stated otherwise.
Correlation Between GRC and PROMs in Microdiscectomy Patients
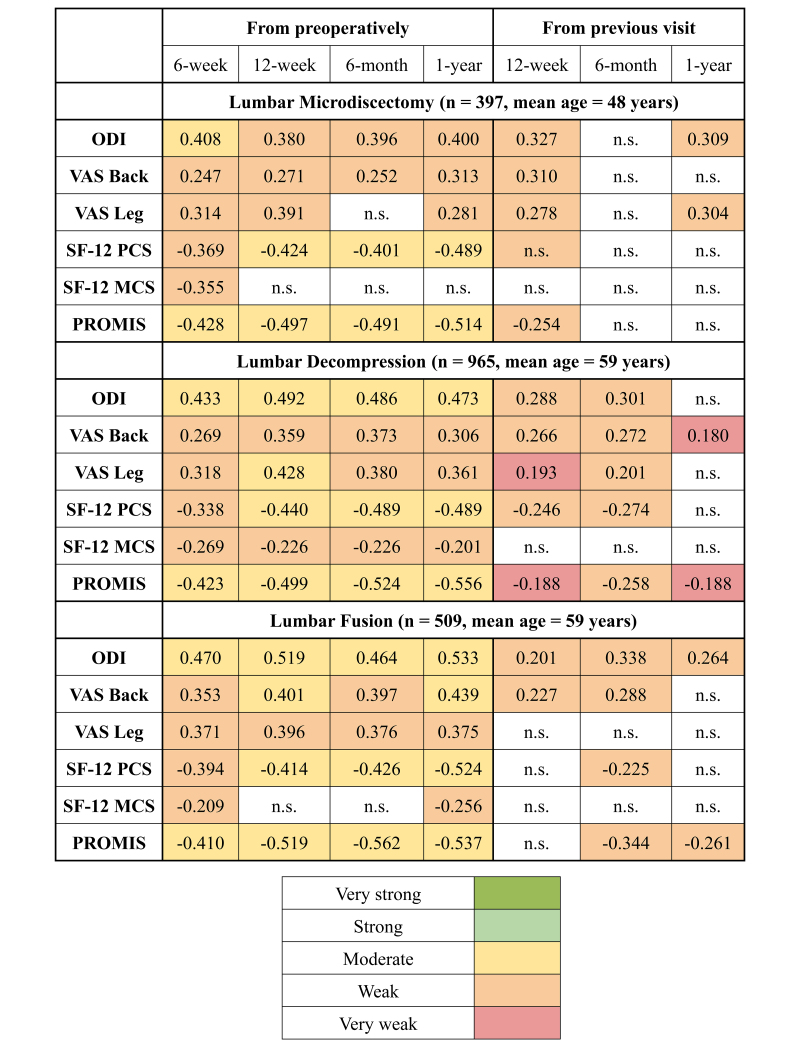
As seen in Table 4 and Fig. 1, changes in PROMs compared with preoperatively demonstrated significant but weak to moderate correlations with GRC at all time points for all PROMs except for leg VAS at 6 months, and SF-12 MCS at 12 weeks, 6 months, and 1 year (Spearman’s rho range |0.247| to |0.514|). Changes in PROMs compared with the previous time point demonstrated significant correlations at 12 weeks for ODI, back VAS, leg VAS, and PROMIS-PF, and at 1 year for ODI and leg VAS. There were no significant correlations found with previous time points for SF-12 PCS and SF-12 MCS. All significant correlations were weak (Spearman’s rho range |0.254| to |0.327|).
TABLE 4.
Correlations between change in PROMs and GRC in the lumbar microdiscectomy cohort
| Preop to 6 wks | Preop to 12 wks | Preop to 6 mos | Preop to 1 yr | 6 wks to 12 wks | 12 wks to 6 mos | 6 mos to 1 yr | |
|---|---|---|---|---|---|---|---|
| ODI |
|
|
|
|
|
|
|
| Correlation coefficient |
0.408 |
0.380 |
0.396 |
0.400 |
0.327 |
NS |
0.309 |
| Strength of correlation |
Moderate |
Weak |
Weak |
Weak |
Weak |
NS |
Weak |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.021 |
0.001
|
| VAS back |
|
|
|
|
|
|
|
| Correlation coefficient |
0.247 |
0.271 |
0.252 |
0.313 |
0.310 |
NS |
NS |
| Strength of correlation |
Weak |
Weak |
Weak |
Weak |
Weak |
NS |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.005 |
0.007 |
| VAS leg |
|
|
|
|
|
|
|
| Correlation coefficient |
0.314 |
0.391 |
NS |
0.281 |
0.278 |
NS |
0.304 |
| Strength of correlation |
Weak |
Weak |
NS |
Weak |
Weak |
NS |
Weak |
| p value |
<0.001
|
<0.001
|
0.004 |
<0.001
|
<0.001
|
0.053 |
0.001
|
| SF-12 PCS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.369 |
−0.424 |
−0.401 |
−0.489 |
NS |
NS |
NS |
| Strength of correlation |
Weak |
Moderate |
Moderate |
Moderate |
NS |
NS |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.006 |
0.021 |
0.002 |
| SF-12 MCS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.355 |
NS |
NS |
NS |
NS |
NS |
NS |
| Strength of correlation |
Weak |
NS |
NS |
NS |
NS |
NS |
NS |
| p value |
<0.001
|
0.008 |
0.008 |
0.066 |
0.499 |
0.139 |
0.94 |
| PROMIS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.428 |
−0.497 |
−0.491 |
−0.514 |
−0.254 |
NS |
NS |
| Strength of correlation |
Moderate |
Moderate |
Moderate |
Moderate |
Weak |
NS |
NS |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.002 | 0.007 |
NS = not significant.
Boldface type indicates statistical significance (p < 0.0012).
FIG. 1.
Heatmap of correlations between change in commonly used PROMs and GRC. n.s. = not significant.
Correlation Between GRC and PROMs in Decompression Patients
As seen in Table 5 and Fig. 1, changes in PROMs compared with preoperatively demonstrated significant but weak to moderate correlations with GRCs at all time points for all PROMs (Spearman’s rho range: |0.201| to |0.556|). Changes in PROMs compared with the previous time point demonstrated significant correlations at all time points for back VAS and PROMIS-PF, at all time points except at 1 year for ODI, leg VAS, and SF-12 PCS, and at no time points for SF-12 MCS. All significant correlations were very weak to weak (Spearman’s rho range: |0.188| to |0.301|).
TABLE 5.
Correlations between change in PROMs and GRC in the lumbar decompression cohort
| Preop to 6 wks | Preop to 12 wks | Preop to 6 mos | Preop to 1 yr | 6 wks to 12 wks | 12 wks to 6 mos | 6 mos to 1yr | |
|---|---|---|---|---|---|---|---|
| ODI |
|
|
|
|
|
|
|
| Correlation coefficient |
0.433 |
0.492 |
0.486 |
0.473 |
0.288 |
0.301 |
NS |
| Strength of correlation |
Moderate |
Moderate |
Moderate |
Moderate |
Weak |
Weak |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.012 |
| VAS back |
|
|
|
|
|
|
|
| Correlation coefficient |
0.269 |
0.359 |
0.373 |
0.306 |
0.266 |
0.272 |
0.180 |
| Strength of correlation |
Weak |
Weak |
Weak |
Weak |
Weak |
Weak |
Very weak |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.001
|
| VAS leg |
|
|
|
|
|
|
|
| Correlation coefficient |
0.318 |
0.428 |
0.380 |
0.361 |
0.193 |
0.201 |
NS |
| Strength of correlation |
Weak |
Moderate |
Weak |
Weak |
Very weak |
Weak |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.056 |
| SF-12 PCS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.338 |
−0.440 |
−0.489 |
−0.489 |
−0.246 |
−0.274 |
NS |
| Strength of correlation |
Weak |
Moderate |
Moderate |
Moderate |
Weak |
Weak |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.006 |
| SF-12 MCS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.269 |
−0.226 |
−0.226 |
−0.201 |
NS |
NS |
NS |
| Strength of correlation |
Weak |
Weak |
Weak |
Weak |
NS |
NS |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.194 |
0.043 |
0.523 |
| PROMIS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.423 |
−0.499 |
−0.524 |
−0.556 |
−0.188 |
−0.258 |
−0.188 |
| Strength of correlation |
Moderate |
Moderate |
Moderate |
Moderate |
Very weak |
Weak |
Very weak |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Boldface type indicates statistical significance (p < 0.0012).
Correlation Between GRC and PROMs in Fusion Patients
As seen in Table 6 and Fig. 1, changes in PROMs compared with preoperatively demonstrated significant but weak to moderate correlations with GRC at all time points for all PROMs, except for SF-12 MCS at 12 weeks and 6 months (Spearman’s rho range |0.209| to |0.562|). Changes in PROMs compared with the previous time point demonstrated significant correlations at all time points for ODI, at 12 weeks and 6 months for back VAS, at no time points for VAS leg and SF-12 MCS, only at 6 months for SF-12 PCS, and at 6 months and 1 year for PROMIS. All significant correlations were weak (Spearman’s rho range |0.201| to |0.338|).
TABLE 6.
Correlations between change in PROMs and GRC in the lumbar fusion cohort
| Preop to 6 wks | Preop to 12 wks | Preop to 6 mos | Preop to 1 yr | 6 wks to 12 wks | 12 wks to 6 mos | 6 mos to 1 yr | |
|---|---|---|---|---|---|---|---|
| ODI |
|
|
|
|
|
|
|
| Correlation coefficient |
0.470 |
0.519 |
0.464 |
0.533 |
0.201 |
0.338 |
0.264 |
| Strength of correlation |
Moderate |
Moderate |
Moderate |
Moderate |
Weak |
Weak |
Weak |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.001
|
<0.001
|
<0.001
|
| VAS back |
|
|
|
|
|
|
|
| Correlation coefficient |
0.353 |
0.401 |
0.397 |
0.439 |
0.227 |
0.288 |
NS |
| Strength of correlation |
Weak |
Moderate |
Weak |
Moderate |
Weak |
Weak |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.002 |
| VAS leg |
|
|
|
|
|
|
|
| Correlation coefficient |
0.371 |
0.396 |
0.376 |
0.375 |
NS |
NS |
NS |
| Strength of correlation |
Weak |
Weak |
Weak |
Weak |
NS |
NS |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.128 |
0.191 |
0.166 |
| SF-12 PCS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.394 |
−0.414 |
−0.426 |
−0.524 |
NS |
−0.225 |
NS |
| Strength of correlation |
Weak |
Moderate |
Moderate |
Moderate |
NS |
Weak |
NS |
| p value |
<0.001
|
<0.001
|
<0.001
|
<0.001
|
0.034 |
<0.001
|
0.002 |
| SF-12 MCS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.209 |
NS |
NS |
−0.256 |
NS |
NS |
NS |
| Strength of correlation |
Weak |
NS |
NS |
Weak |
NS |
NS |
NS |
| p value |
<0.001
|
0.008 |
0.002 |
<0.001
|
0.089 |
0.005 |
0.555 |
| PROMIS |
|
|
|
|
|
|
|
| Correlation coefficient |
−0.410 |
−0.519 |
−0.562 |
−0.537 |
NS |
−0.344 |
−0.261 |
| Strength of correlation |
Moderate |
Moderate |
Moderate |
Moderate |
NS |
Weak |
Weak |
| p value | <0.001 | <0.001 | <0.001 | <0.001 | 0.005 | <0.001 | <0.001 |
Boldface type indicates statistical significance (p < 0.0012).
Discussion
The results of this study demonstrate that a majority of patients undergoing lumbar spine surgery report notable improvements in their spine-related health status in the early postoperative period and continue to have improvements at longer follow-ups. However, changes in PROMs from pre- to postoperatively show a weak to moderate correlation with patient-perceived changes in health status, as assessed by GRC. Furthermore, changes in PROMs from one postoperative visit to the next visit did not consistently show a correlation with GRC, and the strengths of the correlations ranged from very weak to weak when the correlations were statistically significant.
In a review by Guzman et al., VAS, ODI, and SF-12 were identified as the first, second, and 14th most frequently utilized PROMs in spine surgery research, respectively.17 PROMIS, a more recently developed PROM, has gained significant attention as a less burdensome yet highly responsive alternative to legacy PROMs.5,18
Patient perceptions of PROMs have been investigated, as Whitebird et al. assessed outcomes that joint surgery and spine surgery patients deem most important to themselves, as well as their perceived usefulness of standardized PROMs.19 They found that patients found their individual preferred outcomes more meaningful than a standardized PROM score in tracking their recovery. Therefore, patients preferred evaluating surgical success by assessing outcomes specific to their own lives, which are often not fully captured in currently used PROMs.
Multiple studies have investigated the correlation of GRC with PROMs in spine surgery, with the results of the current study differing from those found in the literature. Namely, Hägg et al., who evaluated the efficacy of a single-item global assessment as a substitute for the use of more comprehensive PROMs after fusion surgery for chronic low-back pain, found that their single-item question of global assessment significantly correlated with various PROMs with moderate to strong strength and concluded that global assessment is a substitute for multi-item PROMs in randomized control trials of treatment for chronic low-back pain.20 Parai et al. found that their single-item global assessment question was a useful reference for interpreting PROM scores, as it correlated well with pain-specific items within quality-of-life PROMs and condition-specific VAS and ODI after surgical treatment for degenerative lumbar spine conditions.21 We believe that the ODI, back and leg VAS, SF-12 MCS and PCS, and PROMIS each do not capture the full spectrum of disability experienced by our patient population, which could contribute to the discrepancy between changes in numerical PROM scores and alterations in patient-perceived changes in health status.
However, some of this study’s conclusions are corroborated by previous studies that investigated the association of commonly used PROMs with other measures implemented to assess the whole-person effects of spine conditions. Duculan et al. found weak correlations between the Lumbar Surgery Expectations Survey scores and PROM scores in patients with lumbar degenerative spondylolisthesis, concluding that currently used PROMs do not comprehensively encapsulate patient-centered issues or patient perspectives.22 Similarly, Abtahi et al. found no correlation between patient functional status as determined by PROMs and patient experience of care.23 Key differences between the current study and these previous studies are that the current study assessed correlations between a multitude of PROMs and global assessments of health at multiple postoperative time points, allowing for a long-term analysis of the association of PROMs typically used in clinical practice with GRC.
The version of GRC used in this study asked patients to generally rate their current back condition compared with prior to surgery and compared with the previous visit, thus requiring patients to cognitively appraise their own health. The ability for patients to assess their perceived lumbar condition using any construct they deem most relevant is simultaneously a strength and a weakness of the GRC.6 Hence, the development of PROMs that fully reflect patient voice and experience is an integral component of moving toward a more patient-centered healthcare system, elucidating a clear gap in health services research and the importance of the continuous evolution of how clinicians measure outcomes following lumbar spine surgery.24–26
There are several limitations to the current study. This was a retrospective review of prospectively collected data, which may introduce selection bias. Additionally, this was a single-center study, which may serve to limit the external validity of the study. Furthermore, GRC may introduce recall bias. It is important to consider the relatively limited utilization of GRC in spine surgery research and clinical practice. Although more commonly utilized in other fields of musculoskeletal care, GRC as a tool in spine surgery is not as well described.6 Our study population consisted primarily of privately insured Caucasian patients, and owing to the limited sample size, we were unable to stratify patients by operative level or preoperative diagnosis, which collectively may impact PROM scores. Larger studies involving the stratification of patients by operative level or preoperative diagnosis are warranted.
Conclusions
Our results indicate that a majority of patients undergoing lumbar decompression, fusion, or microdiscectomy reported notable improvements in their lumbar spine condition in the early postoperative period and continued to demonstrate improvements at longer follow-up. However, commonly used PROMs, namely ODI, back and leg VAS, SF-12 PCS and MCS, and PROMIS, demonstrated very weak to moderate correlations with patient-perceived changes in spine-related health status as determined by the GRC questionnaire. These findings suggest that currently used PROMs may not be adequately reflecting changes in patients’ perception of their health status or may not be sufficiently capturing changes in health condition that are meaningful and relevant to patients.
Acknowledgments
This study used REDCap (Research Electronic Data Capture) hosted at Weill Cornell Medicine Clinical and Translational Science Center supported by the National Center For Advancing Translational Science of the National Institute of Health under award number: UL1 TR002384.
Disclosures
Dr. Heuer reported being funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation; project no. 526240791) outside the submitted work. Dr. Iyer reported ownership/equity/investment in HSS ASC Development Network HS2, LLC; research support (either personally or through HSS) from Innovasis; speakers bureau for Globus Medical, Inc.; consultant for Intrinsic Therapeutics Inc.; personal fees from Bioventus, outside the submitted work. Dr. Qureshi reported ownership/equity/investment in HS2, LLC and Tissue Differentiation Intelligence; personal fees royalties from intellectual property, designer, and consultant for Stryker K2M; royalties from intellectual property, speakers’ bureau, and consultant for Globus Medical, Inc.; honoraria from AMOpportunities; consultant for Viseon, Inc., outside the submitted work; medical or scientific advisory board membership for LifeLink.com Inc.; editorial board of Contemporary Spine Surgery and Annals of Transitional Medicine; political engagement committee member, Payor Policy Review Committee member, SpinePAC advisory committee member, and CME committee member for North American Spine Society; editorial board member/senior associate editor of Hospital Special Surgery Journal; program committee member, 2018 annual meeting program chair, board of directors, and professional society member of directors/trustees/governors/managers, member-at-large or committee member of Society of Minimally Invasive Spine Surgery; website committee member and professional society member of directors/trustees/governors/managers, member-at-large or committee member for Lumbar Spine Research Society; publications committee member and Professional Society member of the Cervical Spine Research Society; board of directors (treasurer) of Minimally Invasive Spine Study Group Board of Directors; program committee member and professional society member of Association of Bone and Joint Surgeons; education committee, program committee, 2021 annual meeting program chair, and professional society member of International Society for the Advancement of Spine Surgery; and ownership/equity/investment in HSS ASC Development Network.
Author Contributions
Conception and design: Vaishnav, Qureshi. Acquisition of data: Vaishnav, Kwas, Araghi, Singh, Tuma, Korsun, Simon, Asada, Mai, Zhang, Allen, Kim, Heuer. Analysis and interpretation of data: Vaishnav, Kwas, Mok, Qureshi. Drafting the article: Vaishnav, Kwas, Mok. Critically revising the article: Vaishnav, Kwas, Iyer. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Vaishnav. Statistical analysis: Vaishnav. Administrative/technical/material support: Iyer. Study supervision: Iyer, Qureshi.
Supplemental Information
Previous Presentations
Portions of this work were presented at AANS/CNS Section Spine Summit, Las Vegas, Nevada, February 20–23, 2024.
References
- 1. Lee Y, Issa TZ, Vaccaro AR. State-of-the-art applications of patient-reported outcome measures in spinal care. J Am Acad Orthop Surg. 2023;31(20):e890–e897. doi: 10.5435/JAAOS-D-22-01009. [DOI] [PubMed] [Google Scholar]
- 2. Koivunen K, Widbom-Kolhanen S, Pernaa K, Arokoski J, Saltychev M. Reliability and validity of Oswestry Disability Index among patients undergoing lumbar spinal surgery. BMC Surg. 2024;24(1):13. doi: 10.1186/s12893-023-02307-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13(4):227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 4. Boden SH, Farley KX, Campbell C, Boden SD, Gottschalk MB. Rational selection of patient-reported outcomes measures in lumbar spine surgery patients. Int J Spine Surg. 2020;14(3):347–354. doi: 10.14444/7046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vaishnav AS, McAnany SJ, Iyer S, Albert TJ, Gang CH, Qureshi SA. Psychometric evaluation of Patient-reported Outcomes Measurement Information System Physical Function Computer Adaptive Testing in minimally invasive lumbar spine surgery: an analysis of responsiveness, coverage, discriminant validity, and concurrent validity. J Am Acad Orthop Surg. 2020;28(17):717–729. doi: 10.5435/JAAOS-D-19-00306. [DOI] [PubMed] [Google Scholar]
- 6. Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Manual Manip Ther. 2009;17(3):163–170. doi: 10.1179/jmt.2009.17.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bobos P, Ziebart C, Furtado R, Lu Z, MacDermid JC. Psychometric properties of the global rating of change scales in patients with low back pain, upper and lower extremity disorders. A systematic review with meta-analysis. J Orthop. 2020;21:40–48. doi: 10.1016/j.jor.2020.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Korsun MK, Shahi P, Shinn DJ, et al. Improvement in predominant back pain following minimally invasive decompression for spinal stenosis. J Neurosurg Spine. 2023;39(4):576–582. doi: 10.3171/2023.5.SPINE23278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shahi P, Song J, Dalal S, et al. Improvement following minimally invasive lumbar decompression in patients 80 years or older compared with younger age groups. J Neurosurg Spine. 2022;37(6):828–835. doi: 10.3171/2022.5.SPINE22361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bovonratwet P, Samuel AM, Mok JK, et al. Minimally invasive lumbar decompression versus minimally invasive transforaminal lumbar interbody fusion for treatment of low-grade lumbar degenerative spondylolisthesis. Spine (Phila Pa 1976) 2022;47(21):1505–1514. doi: 10.1097/BRS.0000000000004432. [DOI] [PubMed] [Google Scholar]
- 11. Zhao E, Hirase T, Kim AG, et al. The impact of posterior intervertebral osteophytes on patient-reported outcome measures after L5-S1 anterior lumbar interbody fusion and transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2024;49(9):652–660. doi: 10.1097/BRS.0000000000004904. [DOI] [PubMed] [Google Scholar]
- 12. Shahi P, Dalal S, Shinn D, et al. Improvement following minimally invasive transforaminal lumbar interbody fusion in patients aged 70 years or older compared with younger age groups. Neurosurg Focus. 2023;54(1):E4. doi: 10.3171/2022.10.FOCUS22604. [DOI] [PubMed] [Google Scholar]
- 13. Shahi P, Subramanian T, Araghi K, et al. Comparison of robotics and navigation for clinical outcomes after minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2023;48(19):1342–1347. doi: 10.1097/BRS.0000000000004721. [DOI] [PubMed] [Google Scholar]
- 14. Bovonratwet P, Vaishnav AS, Mok JK, et al. Association between Patient Reported Outcomes Measurement Information System Physical Function with postoperative pain, narcotics consumption, and patient-reported outcome measures following lumbar microdiscectomy. Global Spine J. 2024;14(1):225–234. doi: 10.1177/21925682221103497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guzman JZ, Cutler HS, Connolly J, et al. Patient-reported outcome instruments in spine surgery. Spine (Phila Pa 1976) 2016;41(5):429–437. doi: 10.1097/BRS.0000000000001211. [DOI] [PubMed] [Google Scholar]
- 18. Young K, Steinhaus M, Gang C, et al. The use of Patient-Reported Outcomes Measurement Information System in spine: a systematic review. Int J Spine Surg. 2021;15(1):186–194. doi: 10.14444/8024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Whitebird RR, Solberg LI, Norton CK, Ziegenfuss JY, Asche SE, Grossman ES. What outcomes matter to patients after joint or spine surgery? J Patient Cent Res Rev. 2020;7(2):157–164. doi: 10.17294/2330-0698.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hägg O, Fritzell P, Odén A, Nordwall A. Simplifying outcome measurement: evaluation of instruments for measuring outcome after fusion surgery for chronic low back pain. Spine (Phila Pa 1976) 2002;27(11):1213–1222. doi: 10.1097/00007632-200206010-00014. [DOI] [PubMed] [Google Scholar]
- 21. Parai C, Hägg O, Lind B, Brisby H. The value of patient global assessment in lumbar spine surgery: an evaluation based on more than 90,000 patients. Eur Spine J. 2018;27(3):554–563. doi: 10.1007/s00586-017-5331-0. [DOI] [PubMed] [Google Scholar]
- 22. Duculan R, Fong AM, Cammisa FP, et al. Emerging need for PROMs to measure the impact of spine disorders on overall health and well-being: measuring expectations as an example for lumbar degenerative spondylolisthesis. HSS J. 2023;19(2):163–171. doi: 10.1177/15563316221146123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Abtahi AM, Lyman KS, Brodke DS, Lawrence BD, Zhang C, Spiker WR. Patient satisfaction is not associated with self-reported disability in a spine patient population. Clin Spine Surg. 2017;30(8):E1165–E1168. doi: 10.1097/BSD.0000000000000431. [DOI] [PubMed] [Google Scholar]
- 24. Finkelstein JA, Schwartz CE. Patient-reported outcomes in spine surgery: past, current, and future directions. J Neurosurg Spine. 2019;31(2):155–164. doi: 10.3171/2019.1.SPINE18770. [DOI] [PubMed] [Google Scholar]
- 25. Beighley A, Zhang A, Huang B, et al. Patient-reported outcome measures in spine surgery: a systematic review. J Craniovertebr Junction Spine. 2022;13(4):378–389. doi: 10.4103/jcvjs.jcvjs_101_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rushton A, Elena B, Jadhakhan F, et al. Immediate patient perceptions following lumbar spinal fusion surgery: semi-structured multi-centre interviews exploring the patient journey and experiences of lumbar fusion surgery (FuJourn) Eur Spine J. 2022;31(12):3590–3602. doi: 10.1007/s00586-022-07381-x. [DOI] [PubMed] [Google Scholar]