Abstract
Background
Prehypertension (PHT) is a cardiovascular health risk defined by blood pressure (BP). Arterial stiffness (AS) provides beyond brachial BP inference on vascular ageing and pulse wave analysis (PWA) can measure it non-invasively.We compared association between AS and PHT using age and gender matched case-controls.
Methods
This is a sub analysis of previous PWA studies of hypertensives and non-hypertensives. Using oscillometric PWA by Mobil-o-Graph (IEM, Stolberg, Germany), parameters of AS (augmentation pressure and index, reflection magnitude, aortic pulse wave velocity, pulse pressure amplification), brachial hemodynamics (BH), and central hemodynamics (CH; aortic BP, cardiac output related parameters, stroke work) were derived. Age and gender matched case controls were compared as: 1) Nonhypertensives with BP at prehypertensive level (PHT) versus normotensives (NT) (n = 217 each), 2) Under treatment hypertensives with BP at prehypertensive level (PHT-T) versus untreated, nonhypertensives with BP at prehypertensive level (PHT-UT) (n = 74 each).
Results
PHTs had higher AS, BH and CH than NTs, with statistical significance for all but few parameters. PHT-T had comparable BH but higher AS, CH than PHT-UT with significance for few parameters.
Conclusion
Pulse wave analysis derived arterial stiffness is associated with prehypertension compared to normal, after age and gender matching. In hypertensives, arterial stiffness is significantly higher despite being treated to prehypertension level as compared to control. It hints arterial stiffness to be better parameter than brachial BP to study prehypertension.
Keywords: Anti-hypertensive, Blood pressure, Hemodyanmics, Hypertensive, Pre-hypertension
1. Introduction
Prehypertension (PHT) is an intermediate between hypertension and normotension that is being considered abnormal by few guidelines and not so by others.1 Brachial blood pressure(BP) defines PHT but there are beyond BP parameters to infer as well.2 Arterial stiffness (AS) is one such better surrogate of vascular progeria,3 more so after age, gender matching; and same has been published in our newly diagnosed4 and under treatment5,6 hypertensive population. AS parameters like augmentation pressure, augmentation index, aortic pulse wave velocity, aortic blood pressures are derived by pulse wave analysis (PWA). Whether these AS parameters are augmented with prehypertension compared to normotension or not remains largely unknown. Alike, whether residual AS exists or not in hypertensives with BP brought to prehypertensive level, is also unknown. With this background, a case control study was undertaken to test association of PHT and AS in age, gender matched individuals with strata of normotension, prehypertension and hypertension treated to PHT level.
2. Methodology
2.1. Study set up
This is a sub analysis of data from our previously published studies on pulse wave analysis (n = 1468 total). From that database, case control groups were set up from non-hypetensives (n = 911), newly diagnosed never treated hypertensives (n = 275) and treated hypertensives (n = 557). By meticulous age, gender matched selection from that dataset; we came out with two case control comparison scenarios as mentioned below.
2.2. Subgroups for matching of cases and controls for study
For participants enrolled in this sub-analysis, inclusion and exclusion criteria have been described elsewhere. Based on brachial BP,7 study participants were divided into following subgroups before putting into age, gender matching for selection of comparison group.
-
1)
Non-hypertensives (NHT) - are participants without self reported use of anti-hypertensives and PWA derived brachial blood pressure –systolic less than 140 mm Hg and diastolic less than 90 mm Hg which were further divided into untreated prehypertensives (PHT-UT) and normotensives (NT). (n = 911)
-
2)
Prehypertensives (PHT-UT)- are participants with PWA derived brachial blood pressure –systolic between 120 and 139 mm Hg and diastolic between 80 and 89 mm Hg. (n = 229)
-
3)
Normotensives (NT)- are participants with PWA derived brachial blood pressure –systolic less than 120 mm Hg and diastolic less than 80 mm Hg (n = 682)
-
4)
Hypertensives(HT)- are participants with self reported use of anti-hypertensive medications or PWA derived brachial blood pressure –systolic ≥140 mm Hg and diastolic ≥90 mm Hg which were further divided into new hypertensives (HT-UT), hypertensives treated to prehypertensive level(PHT-T) and other hypertensives (HT- O).(n = 832)
-
5)
New hypertensives (HT-UT) are participants with PWA derived brachial blood pressure –systolic ≥140 mm Hg and diastolic ≥90 mm Hg and not having used any anti-hypertensive medications.(n = 275)
-
6)
Hypertensives treated to prehypertensive level(PHT-T) are participants with self reported use of anti-hypertensives and PWA derived brachial blood pressure-systolic between 120 and 139 mm Hg and diastolic between 80 and 89 mm Hg. (n = 86)
-
7)
Other hypertensives (HT- O) are participants with self reported use of anti-hypertensives and PWA derived brachial blood pressure (either (i) systolic ≥140 mm Hg and diastolic ≥90 mm Hg; or (ii) systolic less than 120 mm Hg and diastolic less than 80 mm Hg (n = 471)
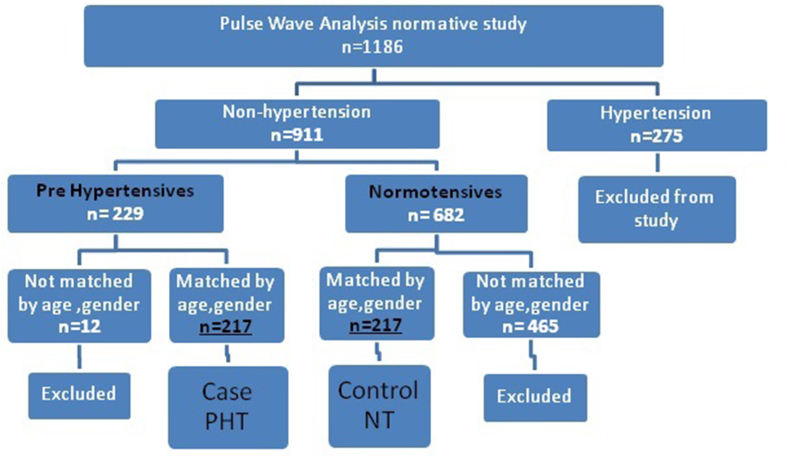
2.3. Case control groups-scenario 1: PHT-UT versus NT
Out of 911 NHT, we selected 229 prehypertensives (PHT-UT) and 229 normotensives (NT) matched by age and gender, setting up case and control group respectively as schematized in Fig. 1.
Fig. 1.
Scheme of study participants' selection for comparison scenario 1.
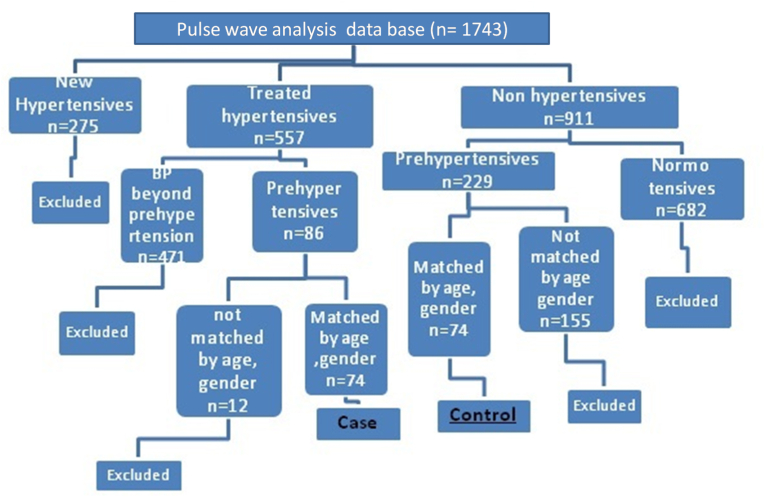
2.4. Case control groups -scenario 2: PHT-T versus PHT-UT
By age and gender matching, 86 hypertensives treated to prehypertensive level (PHT-T) and 86 untreated prehypertensives (PHT-UT) were taken, setting up case and control group respectively as schematized in Fig. 2.
Fig. 2.
Scheme of study participants' selection for comparison scenario 2.
2.5. Pulse wave analysis –instrument
Our research tool is same as used in main studies4,5,6 and described here. We used portable, personal computer attached, calibrated, and validated instrument Mobil-O-Graph (IEM Gmbh, Stolberg, Germany) of the Physiology department that records brachial pulse wave. It undergoes oscillometric pressure PWA as per protocol designed by European Society of Hypertension (ESH).
2.6. Pulse wave analysis - method
Measurement protocol is published elsewhere4,5,6 and described here. A blood pressure cuff of appropriate size (mid-arm circumference: 20–24 cm = small size, 24–32 cm = medium size, 32–38 cm = large size) was chosen based on measured mid-arm circumference and applied to left arm using a standard protocol. All readings were taken after resting for 10 min, in the post absorptive phase while subjects avoiding smoking or alcohol for 12 h before measurement in a calm room without external influences or avoiding arm movement.
Pressure oscillations generated by brachial arterial pulsation is transmitted.
To BP cuff and measured by the transducer to be fed into the microprocessor. Computerized software records pulse wave of the brachial artery and by validated a generalized transfer factor derives central aortic pulse wave. It further undergoes point-based and area-based analysis by software to derive various cardiovascular parameters.
2.7. Pulse wave analysis parameters
Measured study parameters are.
-
(1)
Heart rate (HR), BMI, and body surface area (BSA)
-
(2)
Brachial BP – systolic (bebop), diastolic (bebop), pulse (bPP), and mean (bMBP)
-
(3)
Central BP – systolic (cSBP), diastolic (cDBP), and pulse (cPP)
-
(4)
Central hemodynamics – CO, cardiac index, and systemic vascular resistance
-
(5)
Arterial stiffness – augmentation pressure (AP), augmentation index at heart rate 75 per minute, reflection magnitude percentage (Ref %), and aortic pulse-wave velocity (aPWV)
Derived study parameters are.
-
(1)
Rate pressure product (RPP) − (heart rate per minute) × (systolic blood pressure) × 0.01
-
(2)
Stroke volume − cardiac output/heart rate
-
(3)
Stroke volume index − stroke volume/body surface area
-
(4)
Stroke work (SW) − (pulse pressure) × (stroke volume) × 0.0144
-
(5)
Total arterial stiffness − pulse pressure/stroke volume
-
(6)
Pulse pressure index (PPI) − pulse pressure/systolic blood pressure
-
(7)
Pulse pressure amplification (PPA) − brachial pulse pressure/aortic pulse pressure.
Above parameters were selected to describe peripheral, central or general arterial stiffness and to derive means of central and brachial hemodynamics measured both non-invasively and simultaneously.
2.8. Statistical evaluation
The data of each comparison scenario were entered to and processed by Excel spreadsheets; numerical data were written as mean ± standard deviation until indicated specifically and qualitative data were written as number (%). Statistical calculations were performed on QuickCalcs of GraphPad software (demo version free software of GraphPad Software, Inc. California, USA).In both scenarios of matched cases and controls, numerical data were compared by unpaired t-test for parametric datasets or Mann–Whitney test for non-parametric datasets in two groups. The statistical significance level was taken as p value < 0.05.
3. Results
Comparison was done for various PWA parameters between PHT-UT cases and NT controls, selected by matching as per Fig. 1.Both groups were comparable by age, gender and height. BMI, body weight, heart rate, brachial blood pressures and rate pressure product were significantly higher in PHT - UT case group than NT control group. Alike, arterial stiffness parameters and central heamodynamics were higher in PHT-UT than NT group and all differences were statistically significant except Ref (%), pulse pressure amplification and stroke volume index [Table 1].
Table 1.
Comparison of baseline and study parameters between PHT-UT cases and NT controls, selected by matching as per Fig. 1(n = 217 each).
| Parameter | PHT-UT (n = 217) | NT (n = 217) | P Value |
|---|---|---|---|
| Age,years | 35.63 ± 13.36 | 35.70 ± 13.32 | 0.96 |
| Male/female,no | 121/96 | 121/96 | – |
| Height, Cm | 163.12 ± 7.72 | 162.63 ± 11.12 | 0.59 |
| Weight,Kg | 63.84 ± 11.13 | 59.25 ± 11.34 | 0.0009* |
| Body mass index BMI, kg/m2 | 23.68 ± 4.29 | 22.47 ± 4.06 | 0.0028* |
| bBP(mmHg) | |||
| Systolic blood pressure SBP | 127.78 ± 5.38 | 109.90 ± 6.28 | <0.0001* |
| Diastolic blood pressure DBP | 84.41 ± 2.90 | 71.11 ± 6.07 | <0.0001* |
| Mean blood pressure MBP | 104.13 ± 3.67 | 88.86 ± 5.01 | <0.0001* |
| Pulse pressure PP | 43.14 ± 5.98 | 38.60 ± 7.26 | <0.0001* |
| Pulse pressure index PPI | 33.66 ± 3.53 | 35.08 ± 5.62 | 0.0018* |
| Heart rate HR, bpm | 92.47 ± 14.52 | 85.64 ± 13.73 | <0.0001* |
| RPP,mmHg. Bpm | 118.20 ± 19.45 | 94.14 ± 16.17 | <0.0001* |
| Arterial stiffness | |||
| AP, mmHg | 7.43 ± 3.42 | 6.52 ± 3.64 | 0.0074* |
| Ref(%) | 62.47 ± 9.50 | 62.23 ± 6.67 | 0.76 |
| AIx@75 (%) | 31.44 ± 10.09 | 27.72 ± 11.23 | 0.0003* |
| PWV, m/s | 6.13 ± 1.08 | 5.56 ± 0.99 | <0.0001* |
| TAS, mL/mmHg | 0.80 ± 0.14 | 0.76 ± 0.19 | 0.0069* |
| PPA | 1.38 ± 0.18 | 1.37 ± 0.17 | 0.18 |
| cBP (mmHg) | |||
| cSBP | 117.03 ± 9.71 | 101.05 ± 6.42 | <0.0001* |
| cDBP | 86.17 ± 4.69 | 72.40 ± 6.39 | <0.0001* |
| cPP | 31.83 ± 6.70 | 28.65 ± 6.22 | <0.0001* |
| Central Hemodynamics | |||
| CO, L/min | 4.96 ± 0.43 | 4.40 ± 0.55 | <0.0001* |
| PR, mmHg/ml | 1.26 ± 0.11 | 1.23 ± 0.14 | 0.0069* |
| CI, L/min/m2 | 2.99 ± 0.32 | 2.73 ± 0.38 | <0.0001* |
| SV, ml/beat | 54.75 ± 8.53 | 52.22 ± 10.82 | 0.0071* |
| SVI, ml/m2/beat | 32.91 ± 5.95 | 32.44 ± 6.92 | 0.45 |
| SW, g/beat | 34.02 ± 8.22 | 29.18 ± 8.48 | <0.0001* |
Abbreviations: RPP = rate pressure product,AP = augmentation pressure, Ref = reflection percentage,AIx@75 = augmentation index at heart rate 75 beats per minute, PWV = pulse wave velocity, TAS = total arterial stiffness, PPA = pulse pressure amplification, cSBP = central systolic blood pressure, cDBP = central diastolic blood pressure, cPP = central pulse pressure, CO = cardiac output, PR = peripheral resistance, CI = cardiac index, SV = stroke volume, SVI = stroke volume index, SW = stroke work,‘*’ indicates statistical significance.
PWA parameters were compared between PHT-T cases and PHT-UT controls, selected by matching as per Fig. 2.Both groups were comparable by age, gender,height, BMI, body weight, heart rate, brachial blood pressures(except pulse pressure index) and rate pressure product. Arterial stiffness parameters were higher in PHT-UT than NT group but only augmentation pressure, Ref (%) and pulse wave velocity exhibited statistically significant differences. Central blood pressures and central hemodynamics were larger in PHT-T than PHT-UT group but only central pulse pressure and stroke work showed significant p values for differences observed [Table 2].
Table 2.
Comparison of baseline and study parameters between PHT-T cases and PHT-UT controls, selected by matching as per Fig. 2 (n = 74 each).
| Parameter | PHT-T (n = 74) | PHT-UT (n = 74) | P Value |
|---|---|---|---|
| Age,years | 48.03 ± 7.98 | 47.85 ± 8.06 | 0.89 |
| Male/female,no | 40/34 | 40/34 | – |
| Height, Cm | 160.66 ± 5.97 | 160.88 ± 7.40 | 0.84 |
| Weight,Kg | 63.78 ± 11.59 | 63.83 ± 9.86 | 0.98 |
| Body mass index BMI, kg/m2 | 24.62 ± 3.90 | 24.77 ± 4.05 | 0.82 |
| bBP(mmHg) | |||
| Systolic blood pressure SBP | 129.50 ± 5.54 | 127.80 ± 5.19 | 0.56 |
| Diastolic blood pressure DBP | 84.89 ± 3.03 | 85.28 ± 2.98 | 0.43 |
| Mean blood pressure MBP | 105.34 ± 3.55 | 104.92 ± 5.01 | 0.46 |
| Pulse pressure PP | 44.61 ± 5.63 | 42.30 ± 5.66 | 0.14 |
| Pulse pressure index PPI | 34.35 ± 3.19 | 33.00 ± 3.34 | 0.0013a |
| Heart rate HR, bpm | 89.28 ± 13.75 | 90.89 ± 13.29 | 0.47 |
| RPP, mmHg. bpm | 115.65 ± 18.64 | 116.18 ± 17.56 | 0.86 |
| Arterial stiffness | |||
| AP, mmHg | 7.43 ± 3.42 | 6.52 ± 3.64 | 0.0176a |
| Ref(%) | 66.54 ± 6.04 | 64.5 ± 5.56 | 0.034a |
| AIx@75 (%) | 31.44 ± 10.09 | 27.72 ± 11.23 | 0.21 |
| PWV, m/s | 7.27 ± 0.96 | 6.95 ± 1.20 | 0.037a |
| TAS, mL/mmHg | 0.80 ± 0.17 | 0.78 ± 0.13 | 0.45 |
| PPA | 1.31 ± 0.12 | 1.32 ± 0.13 | 0.76 |
| cBP (mmHg) | |||
| cSBP | 120.05 ± 5.47 | 119.53 ± 5.63 | 0.18 |
| cDBP | 86.46 ± 3.05 | 87.01 ± 2.98 | 0.27 |
| cPP | 31.83 ± 6.70 | 28.65 ± 6.22 | 0.043a |
| Central Hemodynamics | |||
| CO, L/min | 4.96 ± 0.41 | 4.94 ± 0.41 | 0.36 |
| PR, mmHg/ml | 1.28 ± 0.09 | 1.28 ± 0.08 | 0.98 |
| CI, L/min/m2 | 2.98 ± 0.39 | 2.95 ± 0.30 | 0.63 |
| SV, ml/beat | 56.71 ± 8.70 | 55.24 ± 7.63 | 0.27 |
| SVI, ml/m2/beat | 34.18 ± 6.52 | 33.05 ± 5.32 | 0.25 |
| SW, g/beat | 36.54 ± 7.95 | 33.77 ± 7.17 | 0.0274a |
Abbreviations are same as Table 1.
Indicates statistical significance.
4. Discussion
Though brachial blood pressure remains the gold standard for diagnosis of hypertension (HT), there remains a domain to explore in terms of arterial stiffness (AS).8 Alike, prehypertension (PHT) stays as an intermediate state between normal and diseased state with reference to BP. In our previous studies published on PWA, we documented AS to provide inference on cardiovascular health which is not totally dependent on brachial BP, in normative adults,9 newly diagnosed hypertensives,4 normotensive diabetics,10 euglycemic hypertensives5 and diabetic hypertensives.6AS, being more discrete and close parameter than BP, might be distributed differently in prehypertensive than normotensive while the former being considered pre-disease stage. Similarly, residual AS may ensue in hypertensives treated to PHT level11 as pharmacotherapy lowers only blood pressure12 which is one out of many factors affecting AS. How does AS of hypertensives with BP treated to PHT level and that of age, gender matched non-hypertensive with PHT differ,11 remains a question to answer. With this background, by a sub analysis study, we compared AS of i) PHT vs. NT ii) HT treated to PHT vs. never treated PHT.
Significant association was found between AS parameters and PHT as compared to NT. Despite matched age, gender and BMI, PHT group exhibited augmented central AS like aortic pulse wave velocity, central blood pressure and most central hemodynamic. This AS and PHT association is in line with others,13,14,15,16 but our study measured the same by aortic rather than regional arterial stiffness. This AS and PHT association indicates vascular progeria that precedes incident hypertension17 and can be explored further. However, peripheral arterial stiffness parameters like augmentation pressure and pulse pressure amplification were not significantly different indicating lesser affection of small blood vessels in PHT. This is in line with our studies,4,5,6,9,10 indicating central more than peripheral arterial stiffness scenario in our population. PHT and AS make a link that indicates vascular ageing beyond conventionally measured brachial BP proving them better surrogate18 Same can be further followed up with incident HTN as end point to further ascertain AS being a predecessor of actual HTN.
Pharmacotherapy affects AS and brachial BP differently and residual AS stays despite BP lowering in Indian hypertensives as recently published.19 All conventional first line anti-hypertensive drugs used in our set up have no class difference in reducing brachial BP, as documented in our population.20 However, most hypertensives are treated to bring BP below 140/90 mm Hg norm and many would be short of normotensive cut off, having BP between these two limits at PHT level.21 We found that hypertensives treated to PHT level(PHT-T) have higher AS than PHT which are otherwise untreated(PHT-UT).Such comparison between two groups with PHT (treated and non treated) is not done in previous work elsewhere and we did the same in sub analysis here keeping two major confounder age and gender matched. PHT-T group showed significantly raised augmentation pressure, reflection co-efficient, pulse wave velocity, central pulse pressure and stroke work than PHT-UT group. This indicates that PHT stays a significant risk factor for AS and hemodyanamic acceleration when hypertension is treated not to normotension level. It also suggests use of these AS and central hemodynamic parameters to further prove its utility above brachial heamodyanamics, even in treated hypertensives and same is suggested22 by recent research work. In current data-set the proportion of hypertensives treated to normotensive level remains too small to compare with those having BP treated to PHT level and same can be rectified further by another study.
There are clinical implications of our study that demonstrated PHT was associated with AS and CH. There is always a scope to study cardiovascular healths beyond brachial hemodynamics; and AS, CH prove good candidates which are suggested to be incorporated17 even in young adults for the same. Recent findings provided strong evidence that reduction in arterial stiffness by antihypertensive treatment could precede BP lowering.22 In line with us, a Mobil-o-graph based study23 published that arterial stiffness can predict sustained hypertension in patients having high normal blood pressure or grade 1 hypertension alike our prehypertensives. Clinically, PHT can be considered a potential risk factor for cardiovascular health imposing beyond BP effect. If BP is lowered by anti-hypertensves,but only to PHT level, there is associated adverse AS profile. This study also hints to a further study on how change from PHT to NT or PHT to HTN can affect AS and that can further consolidate our results.
Bidirectional relationship exists between arterial stiffness and BP. With PHT as a state between normal and hypertensive state,24 we find opportunity to study it in both directions. Even in treated hypertensives with residual arterial stiffness, further study can enlighten on how it changes when normotension is attained in hypertensives.As recently published in a review,25 AS has better predictive ability than BP or PHT in hypertensives for incident diabetes. Arterial stiffness and prehypertension can be elements of a vicious cycle,26 that with other cardiovascular risk factors, like aging and abnormal glucose metabolism, may aggravate this cycle. In the future, Development of a technique to assess large/small arterial stiffness and an effective strategy to curb arterial stiffness in subjects with prehypertension is needed and our study re-iterate the same. It adds to epidemiological and hemodynamic evidences that raised arterial stiffness is a determinant of incident hypertension. It also suggests the complexity of this relationship between arterial stiffness and blood pressure.27 Persistence of PHT has been associated with accelerated structural stiffening in large-to middle-sized arteries, and that age may exert a synergistic effect on this acceleration of arterial stiffening, that is more pronounced in middle-aged and elderly subjects like our study population.28
Use of novel Mobil-o-graph instrument, selection from large community sample, meticulous matching, and comparison of a large spectrum of parameters were strengths of our study. But still it had limitation of moderate sample size, single point measurement, unavailability of biomarker investigations of vascular progeria and lack of follow up. However, it reaffirmed PHT and AS association, in our population by an oscillometric PWA.
5. Conclusion
PWA based arterial stiffness parameters like wave reflection parameters, aortic haemodynamics, and pulse wave velocity are associated with prehypertension in our population after matching with age and gender. There is residual arterial stiffness in hypertensives treated to prehypertension level as compared to control. It hints arterial stiffness to be a parameter beyond brachial blood pressure to study vascular ageing in prehypertension, either in untreated prehypertensives or in treated hypertensives brought to prehypertensive level.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Gupta K., Jain V., Qamar A., et al. Regional impact of updated guidelines on prevalence and distribution of blood pressure categories for hypertension in India: results from the National Family Health Survey 4. Indian Heart J. 2021;73(4):481–486. doi: 10.1016/j.ihj.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antropova O.N., Silkina S.B., Polyakova I.G., et al. Association of hemodynamic parameters and cardiovascular risk factors with cardiac remodeling in young patients with prehypertension and hypertension Russ. J Cardiol. 2020;25(6):3797. [Google Scholar]
- 3.Oliveira A.C., Cunha P.M., Vitorino P.V., et al. vol. 119. 2022. pp. 604–615. (Vascular Aging and Arterial Stiffness Arquivos Brasileiros de Cardiologia). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solanki J.D., Mehta H.B., Shah C.J. Oscillometric pulse wave analysis in newly diagnosed never treated Gujarati hypertensives Vasc Invest. Therapy. 2018;1(1):62–67. [Google Scholar]
- 5.Solanki J.D., Mehta H.B., Panjwani S.J. Central hemodynamics and arterial stiffness by oscillometric pulse-wave analysis in treated Gujarati euglycemic hypertensives: a case-control study. J Fam Med Prim Care. 2019;8(6):2047–2054. doi: 10.4103/jfmpc.jfmpc_233_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Solanki J.D., Panjwani S.J., Patel R.K., et al. Assessment of arterial stiffness. Brachial Haemodynamics, and Central Haemodynamics in Diabetic Hypertensives: A Pulse Wave Analysis-Based Case-Control Study from an Urban Area of West India Pulse. 2021;9(3):89–98. doi: 10.1159/000519357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flack J.M., Calhoun D D., Schiffrin E.L. The new ACC/AHA hypertension guidelines for the prevention, detection, evaluation, and management of high blood pressure in adults. Am J Hypertens. 2018;31(2):133–135. doi: 10.1093/ajh/hpx207. [DOI] [PubMed] [Google Scholar]
- 8.Vasan R.S., Pan S., Xanthakis V., et al. Arterial stiffness and long-term risk of health outcomes: the Framingham. Heart Study Hypertens. 2022;79(5):1045–1056. doi: 10.1161/HYPERTENSIONAHA.121.18776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solanki J.D., Mehta H.B., Shah C.J. Aortic blood pressure and central hemodynamics measured by noninvasive pulse wave analysis in Gujarati normotensives. Int J Clin Exp Pathol. 2018;5(2):75–80. [Google Scholar]
- 10.Solanki J.D., Munshi Hb H.B., Mehta H.B., Shah C.J. Central hemodynamics and arterial stiffness in Gujarati diabetics not receiving any antihypertensive: a case-control study based on oscillometric pulse wave analysis. J Fam Med Prim Care. 2019;8(4):1352–1358. doi: 10.4103/jfmpc.jfmpc_117_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paapstel K K., Kals J. vol. 1212. 2022. p. 370. (Metabolomics of Arterial Stiffness Metabolites). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schettini I.V., Rios D.R., Figueiredo R.C. Effect of different classes of antihypertensive drugs on arterial stiffness. Curr Hypertens Rep. 2023;25:61–70. doi: 10.1007/s11906-023-01238-4. [DOI] [PubMed] [Google Scholar]
- 13.Haley J.E., Woodly S.A., Daniels S.R., et al. Association of blood pressure–related increase in vascular stiffness on other measures of target organ damage in youth hypertens. 2022;79(9):2042–2050. doi: 10.1161/HYPERTENSIONAHA.121.18765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Leeuw P.W., van Varik B., van Twist D.J., et al. 2019. Hemodynamics of Prehypertension Prehypertension and Cardiometabolic Syndrome; pp. 171–182. [Google Scholar]
- 15.Kim M., Yoo H.J., Kim M., et al. vol. 257. 2017. pp. 179–185. (Associations Among Oxidative Stress, Lp-PLA2 Activity and Arterial Stiffness According to Blood Pressure Status at a 3.5-year Follow-Up in Subjects with Prehypertension Atheroscler). [DOI] [PubMed] [Google Scholar]
- 16.R R., Rigonatto F., Vitorino P.V.O., Oliveira A.C., et al. SAGE score in normotensive and pre-hypertensive patients: a proof of concept arq bras cardiol. 2023;120(2) doi: 10.36660/abc.20220291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agbaje A.O. Arterial stiffness precedes hypertension and metabolic risks in youth: a review. J Hypertens. 2022;40(10):1887–1896. doi: 10.1097/HJH.0000000000003239. [DOI] [PubMed] [Google Scholar]
- 18.Varley B.J., Nasir R.F., Craig M.E., et al. Early life determinants of arterial stiffness in neonates, infants, children and adolescents: a systematic review and meta-analysis Atheroscler. 2022;355:1–10. doi: 10.1016/j.atherosclerosis.2022.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Jin L L., Chen J J., Zhang M., et al. Relationship of arterial stiffness and central hemodynamics with cardiovascular risk in hypertension. Am J Hypertens. 2023;36(4):201–208. doi: 10.1093/ajh/hpad005. [DOI] [PubMed] [Google Scholar]
- 20.Solanki J.D., Mehta H.B., Panjwani S.J., et al. Effect of antihypertensive pharmacotherapy on oscillometric pulse wave analysis parameters in treated Gujarati hypertensives: a cross-sectional study. J Pharmacol Pharmacother. 2018;9(3):153–159. [Google Scholar]
- 21.Solanki J.D., Gadhavi B.P., Makwana A.H., et al. Early screening of hypertension and cardiac dysautonomia in each hypertensive is needed-inference from a study of QTc interval in Gujarat. India Int J Prev Med. 2018;9:62. doi: 10.4103/ijpvm.IJPVM_423_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu S., Tian X., Chen S., et al. Arterial stiffness and blood pressure in treated hypertension: a longitudinal study. J Hypertens. 2023;41(5):768–774. doi: 10.1097/HJH.0000000000003400. [DOI] [PubMed] [Google Scholar]
- 23.Rodilla E., Mendizábal A A., Jiménez I., et al. Arterial stiffness predicts sustained hypertension in patients with high normal blood pressure/grade 1 hypertension. Artery Res. 2023;29(1):S10–S11. [Google Scholar]
- 24.Kim H.L. vol. 29. 2023. p. 31. (Arterial Stiffness and Hypertension Clin Hypertens). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sung K.C. Arterial Stiffness and Incident Diabetes Pulse (Basel, Switzerland) 2023;12(1):12–18. doi: 10.1159/000535775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tomiyama H., Yamashina A. Arterial stiffness in prehypertension: a possible vicious cycle. J Cardiovasc Transl Res. 2012;5:280–286. doi: 10.1007/s12265-011-9345-4. [DOI] [PubMed] [Google Scholar]
- 27.Laurent S S., Cunha P.G. 2019. Arterial Stiffness in Early Phases of Prehypertension Prehypertension and Cardiometabolic Syndrome; pp. 101–126. [Google Scholar]
- 28.Tomiyama H., Hashimoto H., Matsumoto C., et al. Effects of aging and persistent prehypertension on arterial stiffening Atheroscler. 2011;217(1):130–134. doi: 10.1016/j.atherosclerosis.2011.03.028. [DOI] [PubMed] [Google Scholar]