Abstract
Background
Despite extensive literature dedicated to determining the optimal treatment of isolated greater tuberosity (GT) fractures, there have been few studies to guide the management of GT fracture dislocations. The purpose of this review was to highlight the relevant literature pertaining to all aspects of GT fracture dislocation evaluation and treatment.
Methods
A narrative review of the literature was performed.
Results
During glenohumeral reduction, an iatrogenic humeral neck fracture may occur due to the presence of an occult neck fracture or forceful reduction attempts with inadequate muscle relaxation. Minimally displaced GT fragments after shoulder reduction can be successfully treated nonoperatively, but close follow-up is needed to monitor for secondary displacement of the fracture. Surgery is indicated for fractures with >5 mm displacement to minimize the risk of subacromial impingement and altered rotator cuff biomechanics. Multiple surgical techniques have been described and include both open and arthroscopic approaches. Strategies for repair include the use of transosseous sutures, suture anchors, tension bands, screws, and plates. Good-to-excellent radiographic and clinical outcomes can be achieved with appropriate treatment.
Conclusions
GT fracture dislocations of the proximal humerus represent a separate entity from their isolated fracture counterparts in their evaluation and treatment. The decision to employ a certain strategy should depend on fracture morphology and comminution, bone quality, and displacement.
Keywords: Greater tuberosity, Fracture dislocation, Iatrogenic fracture, Proximal humerus fracture, Surgical fixation, Fixation strategies
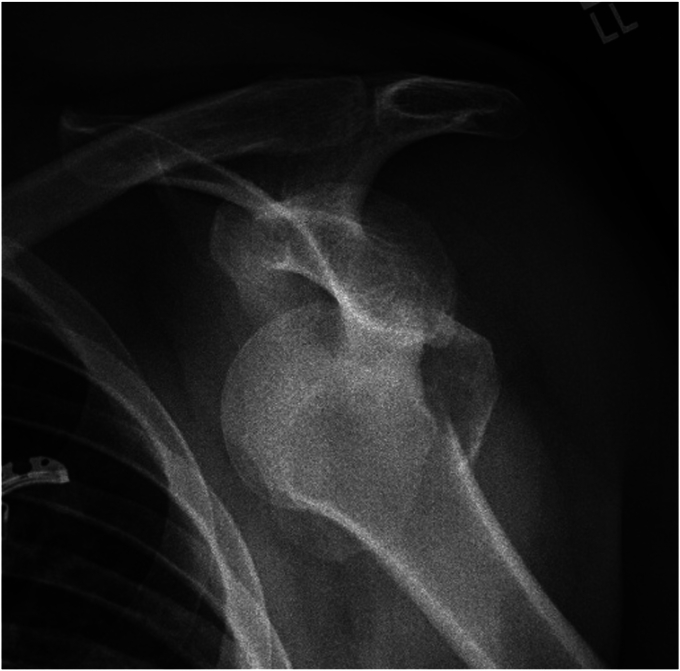
Isolated greater tuberosity (GT) fractures of the humerus are uncommon injuries and comprise approximately 14%-1% of all proximal humerus fractures.4,20,32 Of these injuries, 5%-57% occur in association with an anterior glenohumeral dislocation, whereas 7%-30% of anterior dislocations involve a GT fracture (Fig. 1).4,32,56 Although other fractures of the proximal humerus tend to occur in elderly patients with osteoporosis after a ground-level fall, greater tuberosity fracture dislocations (GTFDs) typically occur in middle-aged patients due to higher energy trauma.12,55
Figure 1.
Anterior greater tuberosity fracture dislocation with a large greater tuberosity fragment.
The mechanism of injury in GTFDs is incompletely understood but has been traditionally attributed to a shear injury.4 As the proximal humerus translates anteriorly during a dislocation, the rotator cuff musculature may counteract this force and result in an avulsion and displacement of the GT. Additionally, it has also been suggested that impaction of the GT against the anteroinferior glenoid rim along with the concomitant pull of the rotator cuff muscles may cause a fracture rather than a Hill-Sachs lesion depending on the degree of humeral external rotation when the dislocation occurs.1 More recent studies have identified inferior displacement of the GT in 20%-32% of glenohumeral dislocations.4,42 These may represent hyperabduction injuries where impaction of the GT against the undersurface of the lateral acromion subsequently levers the humeral head into a dislocated position or direct impaction injuries of the GT against the inferior glenoid.59
Despite extensive literature to ascertain optimal treatment for isolated GT fractures, there have been few studies to guide the treatment of GTFDs. This article will review the pertinent literature regarding all phases of GTFD evaluation and treatment, as well as the senior author’s preferred management.
Classification
In 1970, Neer described the most widely used system for classification of proximal humerus fractures.44 The system is based on the number of fractured parts, magnitude of fracture displacement, and presence or absence of a glenohumeral dislocation. It divided the proximal humerus into the GT, lesser tuberosity, head, and shaft and considers these fracture fragments to be “parts” if they are angulated more than 45° or displaced more than 1 cm.44 The intended purpose of defining these cutoffs for displacement was to classify the fracture fragments as stable or unstable.44 However, these values were chosen arbitrarily, and displacement of the GT is now generally defined to be more than 5 mm.59 The AO/OTA classification is more complex than the Neer classification and is based on the location of the fractures, the presence of articular involvement, and impaction, angulation, or comminution of the metaphyseal segment.41
Although these two classifications are the most commonly used, they are limited by slight to moderate interrater reliabilities.17 Few studies have evaluated the subgroup of GT fractures in isolation. Displacement by more than 5 mm had a reliability of 0.31-0.35 on radiographs.9,42 The fair agreement with radiography is likely the result of difficulty measuring displacement of small fragment sizes and superimposition of the fragment on the humeral head.50 In a study utilizing computed tomography (CT) scans, interobserver reliability of GT displacement was significantly higher on 2D-CT than 3D-CT (κ: 0.35 vs. 0.30), but the overall reliability was still low and differences were small.10
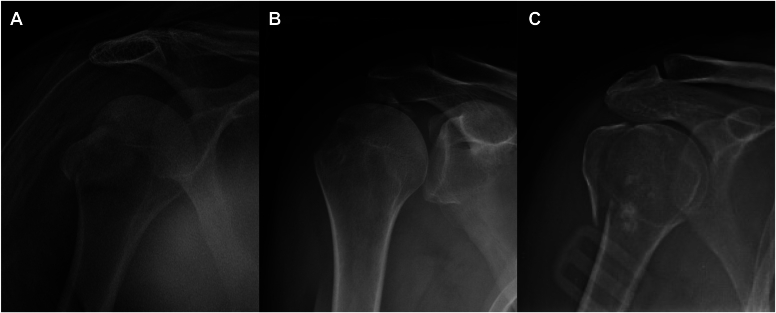
To overcome the limitations of the Neer and AO classification, there has been a shift toward describing the morphology of GT fracture fragment. These systems not only take into account fracture displacement but also consider fragment size, shape, and orientation, which have profound implications in determining surgical fixation. Mutch et al proposed a morphological classification of GT fractures into 3 types: avulsion, split, and depression fractures (Fig. 2).42 Avulsion fractures involve a small fragment of bone with a horizontal fracture line and represent a bony avulsion of the rotator cuff footprint. Split fractures involve a large fragment with a vertical fracture line that begins at the junction of the rotator cuff footprint and humeral head cartilage and extends distally and laterally to the level of the surgical neck. Depression fractures involve a fragment ie, displaced inferiorly and are similar to a Hill-Sachs lesion but are located more laterally on the GT rather than humeral head cartilage. Of 55 GTFDs, 29% were avulsion fractures, 36% were split fractures, and 35% were depression fractures.42 Depression fractures were rarely displaced and required surgical intervention in only 7% of cases.42 Conversely, avulsion and split fractures were displaced more than 5 mm in approximately 35% and 38% of cases, respectively.42 The use of this classification system had good interrater reliability of 0.73-0.77 and has practical implications for guiding surgical fixation technique.42
Figure 2.
Mutch classification of greater tuberosity fractures: (A) depression; (B) avulsion; and (C) split types.
Initial management
The appropriate evaluation of GTFDs is predicated on ability of the treating surgeon to identify the injury in a timely fashion and have a complete and thorough understanding of the fracture pattern. Aside from a focused history, physical exam and imaging remain the mainstays of diagnosis.
Physical examination
Gross deformity of the shoulder or a pronounced subacromial sulcus may suggest a dislocation of the humeral head. There may be ecchymoses around the shoulder. Additional attention should be placed on checking for concomitant injuries to the ipsilateral elbow, forearm, and wrist. A detailed neurologic examination is conducted and documented before and after the reduction. Of patients with GTFDs, 5.7%-34% had a neurologic deficit.18,56 An axillary nerve lesion is the most common deficit occurring in 63% of cases.56 However, a large proportion of nerve injuries involved the brachial plexus and occurred in 21% of cases.56 Vascular injuries after GTFDs are rare and require a high index of suspicion. Collateral circulation can produce a palpable radial pulse despite complete axillary artery occlusion.31 Several risk factors for vascular injuries include an iatrogenic neck fracture with medial displacement of the head or shaft, patient age >50 years, atherosclerosis of the axillary artery, and the presence of neurologic deficits.40,63
Radiographic evaluation
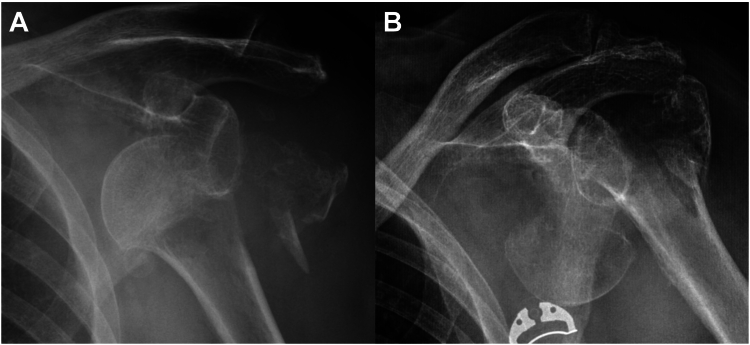
A standard trauma radiographic series of the shoulder, including anteroposterior (AP) view in scapular plane (Grashey view), scapular Y, and an axillary lateral view, is imperative. Systematic assessment of the radiographs begins with determining the direction of dislocation, degree of fracture comminution, orientation of fracture planes, fragment size, bone quality, and associated fractures of the glenoid and coracoid. Furthermore, special attention should also be directed toward an evaluation of the humeral neck for the presence of an occult fracture. Shaw et al reported an occult humeral neck fracture in 7.4% of isolated GT fractures and was missed 4.4% of the time.61 Inferior displacement of the GT can also be suggestive of an occult fracture.66 In the setting of a fracture dislocation, it has been hypothesized that these occult fractures can propagate into a displaced neck fracture during closed reduction. Iatrogenic fracture of the humeral neck occurs in up to 26% of GTFD reductions and has severe clinical consequences, as the clinical outcomes will be worse and treatment options may change from preservation to arthroplasty (Fig. 3).2,24,47,54,67 Risk factors include female sex, age greater than 50 years, and GT size greater than 40% of the distance from the fracture line to the medial calcar.24,47 It is the senior author’s expert opinion that a CT scan should be obtained prior to reduction to evaluate for an occult humeral neck fracture if the patient is over the age of 50 years or if there are findings suspicious for an occult fracture, such as subtle changes in the head-shaft angle or lucent lines along the calcar.
Figure 3.
(A) Anterior greater tuberosity fracture dislocation prior to reduction. (B) Iatrogenic neck fracture of humerus during closed reduction resulting in a 3-part proximal humerus fracture.
Reduction
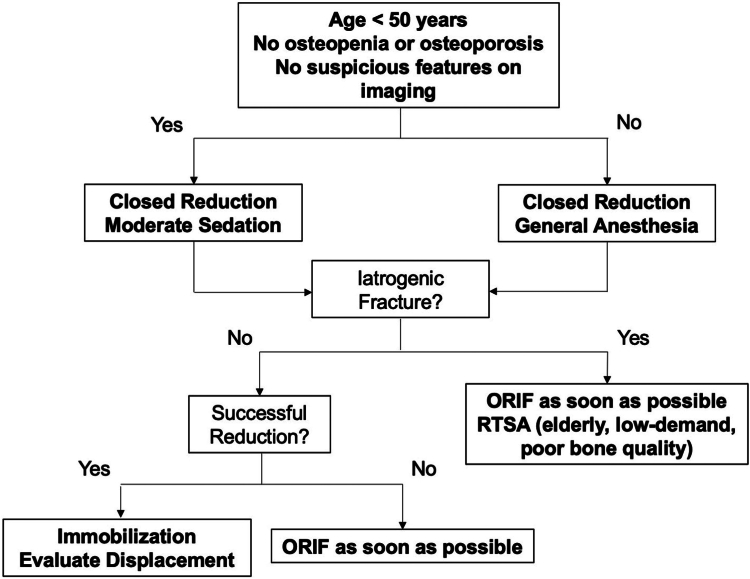
After clinical and radiographic evaluation, the shoulder should be reduced as soon as possible. The patient should be notified beforehand that during the manipulation there is a risk of an iatrogenic fracture. If the patient is less than 50 years old, has good bone quality, and has no suspicious features of a neck fracture, we recommend closed reduction in the emergency department with moderate sedation using the traction-countertraction method (Fig. 4). The closed reduction should be attempted only once and performed by an experienced provider. For those who do not meet all of these criteria, a closed reduction should be performed in the operating room, where general anesthesia and complete muscle relaxation can be achieved. Pan et al reported that 17 cases of iatrogenic fractures occurred under moderate sedation, whereas only 4 cases occurred with general anesthesia, concluding that an ideal state of muscle relaxation minimizes the risk of an iatrogenic fracture.47
Figure 4.
Reduction algorithm for greater tuberosity fracture dislocations. ORIF, open reduction internal fixation; RTSA, reverse total shoulder arthroplasty.
Several scenarios may occur after an attempted closed reduction. When closed reduction is successful, a shoulder immobilizer with an abduction pillow is applied in slight abduction to limit the amount of fracture displacement. When closed reduction with moderate sedation is unsuccessful, a repeat attempt may be performed under general anesthesia.65 For patients with an irreducible GTFD with or without an iatrogenic fracture, open reduction should be performed as soon as possible to maximize patient outcomes and minimize the risk of complications, such as avascular necrosis.47,60,62 In a series of 30 patients with B- and C-type proximal humerus fracture dislocations, 100% of patients who had a delay in reduction and surgery of more than 48 hours developed avascular necrosis.60 Roddy et al found an avascular necrosis rate of 19% in 26 patients with all types of proximal humerus fracture dislocations, though the median time to reduction and surgery was 24 hours.57 After the humeral head is open reduced, it is reasonable to manage an isolated GTFD nonoperatively if there is minimal residual displacement of the fracture fragments. However, the GT fragment has up to a 51% rate of secondary displacement.6 In our experience, we prefer to fix the GT fragment at the initial surgery to minimize the possibility of an additional procedure and allow earlier range of motion. Similarly, we prefer to fix GTFDs with iatrogenic fractures at the time of open reduction as they are often displaced. In a case series of 21 patients with GTFDs and iatrogenic fractures, all patients required surgery to achieve glenohumeral reduction.47 The authors found that pain and functional outcomes were improved among patients who underwent open reduction and internal fixation within 8 hours compared to patients with longer waiting times, though avascular necrosis still occurred in 14% of patients.47 Reverse shoulder arthroplasty is generally reserved for elderly patients with poor bone quality who sustain an iatrogenic humeral neck fracture during an attempted closed reduction of a GTFD.46
Radiographic evaluation after reduction
After glenohumeral reduction, the degree of displacement of the GT fragment is assessed. Some authors have historically reported that the GT was displaced more than 1 cm in 25%-49% of patients.4,39,56 A recent case series of 133 GTFDs similarly found a postreduction displacement greater than 5 mm in 38% of patients.6 Conversely, another study of 55 GTFDs observed that 15% of patients had superior displacement more than 5 mm after shoulder reduction.25 The differences in the reported rates can be attributed to variations in radiographic projections and techniques used to measure displacement.
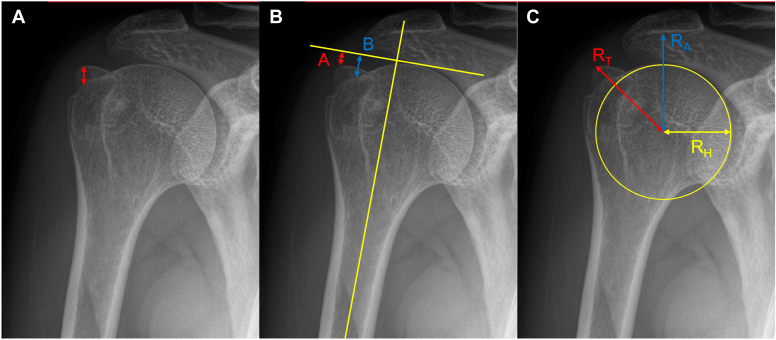
We recommend evaluating the amount of superior-inferior displacement on AP view in external rotation and the amount of anterior-posterior displacement on the axillary lateral view and/or scapular Y view (Fig. 5A). Parsons et al have shown in a cadaveric study that the AP view in external rotation altered treatment in 9 of 48 situations, concluding that this projection best profiles the GT and can demonstrate even smaller displacements.50 However, measurement differences as large as 1 cm can still occur despite standardizing radiographic projections.50 Several other methods to evaluate GT fracture displacement have been developed including the GT ratio (Fig. 5B) and impingement index (Fig. 5C).43,45 A GT ratio >0.50 and an impingement index >0.70 were suggestive of fractures that should be surgically reduced.43,45
Figure 5.
Three methods of determining greater tuberosity (GT) displacement. (A) Superior displacement of 5.5 mm. (B) The GT ratio is calculated as (C) The impingement index is calculated as A GT ratio > 0.50 or an impingement index >0.70 are suggestive of fractures that may benefit from surgery.
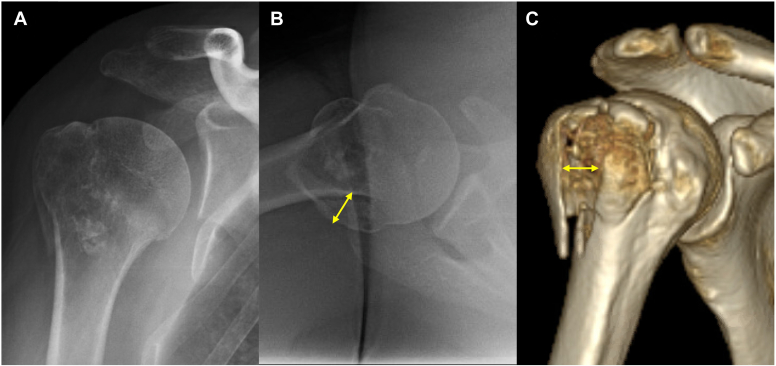
CT scans with or without 3D reconstructions can provide information about fracture morphology, size, comminution, and degree of displacement (Fig. 6). Its benefit, however, in determining surgical treatment has been questioned.27 Among 164 orthopedic surgeons, the addition of 2D or 3D CT did not result in a difference in recommendation for surgery compared to radiographs alone, but did marginally increase the confidence of the surgical decision by 5%.27 A complete radiographic series of good quality should preclude the need for a CT scan, but it can be helpful in borderline cases where the amount of displacement is ambiguous.
Figure 6.
(A) A split-type greater tuberosity fracture with minimal superior displacement on Grashey view with arm in external rotation. (B) Axillary lateral radiograph demonstrating 8 mm posterior displacement. (C) 3D CT reconstructions demonstrating 4.8 mm posterior displacement. The patient was managed successfully nonoperatively. CT, computed tomography.
Other advanced imaging modalities such as magnetic resonance imaging (MRI) may also be used to assess soft tissue injuries. In a series of 32 patients that included nine dislocations, Pitcher et al reported that MRI did not change the measure of fracture displacement or help in making surgical decisions.51 Other MRI studies have found that soft tissue injuries are common with partial-thickness rotator cuff tears occurring in 38%-100% of patients, labral tears in 50%-56% of patients, and biceps tendon injuries in 41% of patients.23,33,38,51 Moreover, full-thickness rotator cuff tears were uncommon in minimally displaced fractures with a prevalence of 0%-9%.23,33,38,51 In patients with nonoperatively managed fractures who have persistent pain, limited motion, weakness, or instability after 3 months, an MRI can be obtained to evaluate for rotator cuff, biceps, or labral pathology. We do not routinely obtain an MRI before surgery, as we do not address capsulolabral injuries acutely. In our experience, concomitant repair of the fracture and capsulolabral complex increases the risk of stiffness significantly. Residual shoulder instability after fixation of the fracture is uncommon and is an easier problem to address than stiffness.
Treatment
Surgical indications
The operative threshold with respect to GT displacement in any direction is generally accepted to be 5 mm after reduction due to concerns about mechanical impingement and altered rotator cuff biomechanics.7,20,22,59 In a biomechanical study of 8 cadavers, Bono et al demonstrated that superior displacement of the GT fragment by 5 mm resulted in subacromial impingement in 1 specimen, whereas superior displacement by 1 cm led to a mechanical block in 7 specimens.7 Moreover, the deltoid force needed to abduct the shoulder increased by 16% and 27% with 5 mm and 1 cm of superior displacement compared to no displacement.7 Subsequent studies have suggested operative treatment with displacement as little as 3 mm, particularly in athletes and heavy laborers.49,53 Platzer et al reviewed 135 patients and found slightly worse Constant, Vienna Shoulder, and University of California Los Angeles Shoulder Scores among patients with 3-5 mm of displacement compared to those with less than 3 mm displacement, albeit the findings were not statistically significant.53 There have been no additional studies that have corroborated these findings, and higher-quality studies are warranted before this lower cutoff can become an accepted practice.
Other authors have recommended operative fixation of all GTFDs due to high rates of secondary GT displacement.14,25,28 They further suggested that the postreduction amount of displacement cannot be used to guide treatment in these cases because the initial displacement when the humeral head is dislocated if often greater than the 5 mm cutoff, averaging 1.1-2.4 cm.14,25,28 In a case series of 27 GTFDs, Hebert-Davies et al found secondary displacement of the GT fragment in 27% of patients and that the odds of further displacement were 5.6-fold higher than those of isolated GT fractures, concluding that even the anatomically reduced GT should be considered highly unstable and at risk of secondary displacement.25 Other studies have similarly reported secondary displacement rates of 40%-51% despite the GT displacement being less than 5 mm after shoulder reduction.5,6 Several predictors of secondary displacement include age > 65 years, split-type fractures, comminuted fractures, rotator cuff atrophy, and ipsilateral fractures to the same extremity.5,6,58 The higher rate of further displacement among GTFDs compared to isolated GT fractures could be from injury to the capsuloligamentous structures after shoulder dislocation, resulting in increased translation of the humeral head.6 Additionally, the mismatch between the fracture surface of the GT fragment and fracture bed in the setting of a dislocation has been implicated to contribute to reduced bony contact and intrinsic stability of the fracture fragments.6,28
We believe that GTFDs represent a separate entity from isolated GT fractures as they are associated with more severe soft tissue injury. For fractures that are displaced less than 5 mm or below the level of humeral head after shoulder reduction, we recommend close observation with weekly radiographs for 3 weeks to evaluate for secondary displacement of the GT. Displacement after this time period is unlikely. We reserve surgery for fractures displaced more than 5 mm or above the level of the humeral head.
Nonoperative management
There is no consensus on the optimal nonoperative management of GTFDs. A summary of rehabilitation protocols and functional outcomes is listed in Table I. We prefer to immobilize patients for a total of 6 weeks in a shoulder immobilizer with an abduction pillow to minimize passive tension of the rotator cuff muscles. Radiographs are initially obtained weekly for the first 3 weeks to evaluate for secondary displacement. Afterward, gentle passive range of motion is initiated. Therapy is advanced to active motion at 6 weeks, and strengthening is begun at 12 weeks. In patients who have persistent pain, limited motion, weakness, or instability after 3 months, an MRI can be obtained to evaluate for rotator cuff, biceps, or labral pathology.
Table I.
Functional outcomes of nonoperative treatment of greater tuberosity fracture dislocations.
| Study | N | Follow-up (y) | Age (y) | Male | Displacement (mm)∗ | Rehab protocol | ROM (°) | PRO | Recurrent instability | Impingement | Delayed ORIF |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Platzer (2005)53 | 26 | 3.7 | 56 (18-75) | NA | 5 | Sling: 3 weeks | NA | Constant: 81 UCLA: 31 Vienna: 7.5 |
1 (3.8%) | NA | 0 (0%) |
| Mattyasovszky (2011)70 | 5 | 3.0 | 62 (26-83) | 2 (40%) | 6 | Sling: 1-2 weeks Active ROM: Week 3-4 Strengthening: Week 6 |
NA | Constant: 65 DASH: 24 |
0 (0%) | 1 (20.0%) | 0 (0%) |
| Hebert-Davies (2015)25 | 27 | 2.3 | 54 (no range) | 16 (59%) | 15 | Sling: 1-2 weeks Active ROM: Week 6 Strengthening: Week 8 |
NA | Constant: 83 | NA | 13 (48.1%) | 3 (11.1%) |
| Dussing (2018)15 | 37 | 4.9 | 58 (23-84) | 23 (62%) | 5 | Sling: 4 weeks Active ROM: Week 6 |
Flexion: 145 Abduction: 144 ER: 44 |
Constant: 75 Rowe: 83 SSV: 80 WOSI: 353 |
3 (8.1%) | NA | 0 (0%) |
| Razaeian (2021)71 | 9 | 1.6 | 57 (22-75) | 4 (44%) | 7 | Sling: 1-2 weeks Active ROM: Week 4 Strengthening: Week 7 |
NA | Constant: 82 SSV: 93 |
0 (0%) | NA | 0 (0%) |
| Summary† | 104 | 3.5 | 57 | 58% | - | - | - | Constant: 79 | 5.2% | 43.8% | 2.9% |
ROM, range of motion; PRO, patient-reported outcomes; UCLA, University of California Los Angeles Shoulder Score; DASH, disability of arm, shoulder, hand; SSV, subjective shoulder value; WOSI, Western Ontario Shoulder Instability.
Maximal superior displacement. Other directions were not consistently assessed.
Weighted means calculated for summarized data.
Patients can expect a good to excellent return of function with a low risk of recurrent instability and reoperation. In 37 GTFDs with postreduction displacement less than 5 mm, Dussing et al noted forward elevation to reach 145° with a mean Constant Score of 75 at 4.9 years.15 Three patients each had one further episode of instability, but there were no reoperations for secondary displacement.15 Hebert-Davies et al reported a Constant Score of 83 among 27 patients with GTFDs, though 48% developed subacromial impingement and 11% required subsequent fixation.25 One study reviewed 9 minimally displaced GTFDs with persistent shoulder pain 8 months after failed conservative therapy and noted partial-thickness articular-sided tears in all patients and Bankart tears in three patients.33 Arthroscopic débridement of the rotator cuff with subacromial decompression and repair of the Bankart lesion resulted in excellent functional scores and no recurrent instability at 2.4 years.33
Surgical treatment
The techniques utilized to treat displaced GTFDs are similar to those used to treat isolated GT fractures and include both open and arthroscopic approaches. Arthroscopy is less invasive and has the added benefit of evaluating and addressing intra-articular structures, such as the rotator cuff, labrum, and biceps tendon, which are commonly injured.37,51 The decision to undergo arthroscopic treatment is dependent on fracture type, fragment size, bone quality, and surgeon preference and experience. In general, fractures are amenable to arthroscopic repair if the injury occurred within the past two weeks, displacement is less than 2 cm, and the fracture does not extend distally beyond the surgical neck of the humerus or involve the bicipital groove anteriorly.29,35,48 A systematic review comparing the clinical outcomes of open and arthroscopic treatment of GT fractures demonstrated no difference in motion and patient-reported outcomes.26 However, the overall complication rate with open surgery was 23% compared to 7% for arthroscopic surgery with the most common complication being stiffness and pain.26
Historically, open or mini-open transosseous repair of the GT using nonabsorbable suture in figure-of-8 fashion was performed with 71%-100% achieving good-to-excellent results.13,14,16 A bone bridge of at least 1 cm and additional nonabsorbable sutures placed around the GT fragment at the bone-tendon junction was recommended to avoid pulling through comminuted or osteoporotic bone.14 Subsequent biomechanical studies, however, have shown that transosseous suture fixation had the lowest yield strength to 5 mm of fracture displacement compared to other fixation constructs, including double row suture bridge, cancellous screws, and locking plate fixation.8,19
In the past decade, multiple variations of the mini-open or arthroscopic double-row suture anchor or double-row suture bridge fixation have been described. One study showed that there is no biomechanical difference in load to displacement between these fixation patterns.36 We prefer arthroscopic repair in small or comminuted fractures, such as an avulsion-type fracture. Our preferred arthroscopic technique is similar to prior techniques and involves a double-row suture bridge construct in the beach chair position.21 After standard diagnostic arthroscopy, the subacromial bursa and fracture hematoma are débrided. The fracture bed and fragment are meticulously cleaned with a shaver to evaluate fracture margins. Inadequate preparation of the fracture bed and fragments can lead to a malreduction. An arthroscopic grasper is used to reduce the fracture, and inspection of the reduction is performed through arthroscopic visualization and fluoroscopy. If the reduction is inadequate, there should be a low threshold to convert to an open procedure. Next, two medial row knotless anchors are inserted at the medial edge of the fracture bed. The anchors are spaced approximately 15 mm apart in the AP direction to maintain an adequate bone bridge. A curved suture shuttling device via the anterior portal is passed through the rotator cuff tendon 3-5 mm medial to the GT fragment to retrieve all suture limbs. There are no knots tied in the medial row. While the grasper holds the GT fragment reduced, the sutures are secured with two lateral row anchors that are inserted 5 mm distal to the edge of the GT fracture. We do not routinely repair Bankart lesions unless there is an associated glenoid rim fracture involving more than 15% of the glenoid.
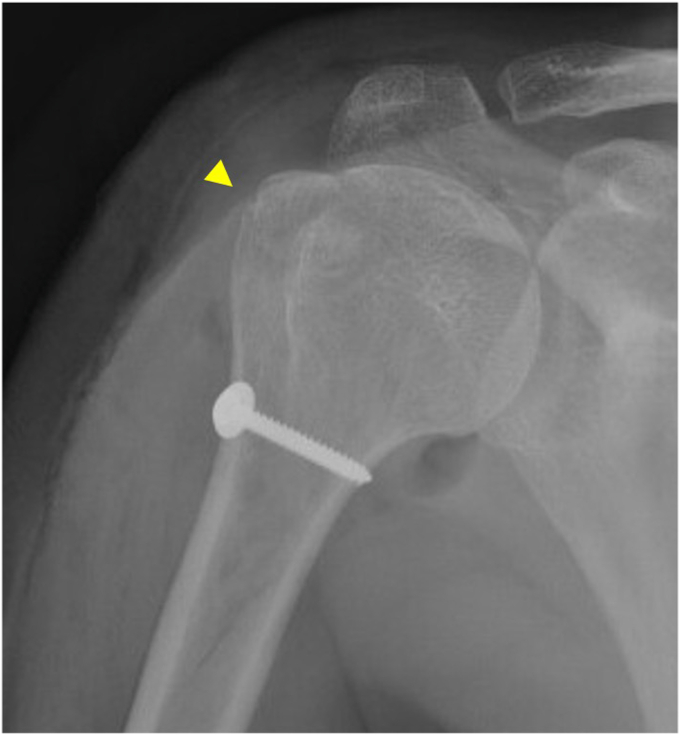
Suture fixation around a screw post can also be used to treat small or comminuted fractures. These constructs are more secure for patients with osteoporosis because the sutures are passed through the rotator cuff tendons, which are stronger than the bone itself. Multiple tension band sutures are anchored just distal to the fracture site with a cortical screw and washer (Fig. 7).
Figure 7.
AP view showing suture fixation with a screw post construct used to secure a small greater tuberosity avulsion fracture. The arrow indicates the location of the fracture line. AP, anteroposterior.
Interfragmentary compression with two cancellous screws can also be placed percutaneously or through a mini-open incision. Both indirect reduction techniques using fluoroscopy or direct reduction with arthroscopic assistance have also been reported.15,52,64 This construct is inexpensive, but the resistance to displacement has been variable in biomechanical studies. Cancellous screws had higher yield strength than transosseous sutures, but not compared to plate fixation or double-row suture anchor constructs.8,34,36 Further augmentation of screw fixation with a cerclage wire around the screw heads can increase the yield strength to a level ie, comparable to suture anchor constructs.11 However, screw fixation can cause additional comminution of small GT fractures during insertion.15 As such, this technique should be reserved only for large split-type fractures with no comminution and good bone quality. We do not use this technique due to lower biomechanical strength, risk of splitting the fragment, and risk of impingement of a prominent screw head.
The senior author’s preferred technique for large-split-type fractures, particularly fragments that extend beyond the level of the surgical neck, is to pass multiple nonabsorbable sutures through the rotator cuff tendons and tie them to the suture holes of a precontoured proximal humerus plate (Fig. 8). This is performed using a deltopectoral approach where the cephalic vein is mobilized medially, if possible, to avoid excess pressure by lateral retractors. Next, a No. 2 nonabsorbable suture is passed 5 mm medially to the supraspinatus tendon insertion. Anterior traction of this suture will expose the infraspinatus and teres minor tendons, allowing two additional No. 2 nonabsorbable sutures to be placed into cuff insertion. After anatomic reduction and provisional fixation of the fragment is obtained, the plate is positioned such that it is 5 mm distal to the most superior aspect of the GT to minimize the risk of subacromial impingement. The No. 2 nonabsorbable sutures that were placed through the posterosuperior rotator cuff are then passed through the plate. Once the plate is fixed to the humeral shaft, the sutures are then tied to the plate. Unicortical locking screws are inserted through the plate, including a screw placed along the medial calcar. We believe this is the most robust construct due to the primary fixation from sutures through the rotator cuff and secondary fixation from the screws through the plate. Moreover, this technique minimizes the risk associated with other techniques, including suture cut-out through bone, suture anchor pull-out, and screw fixation failure. Disadvantages associated with this technique include a larger exposure and the cost of a precontoured plate. However, various small or mini-fragment plates can also be contoured and trimmed to match the GT anatomy. Furthermore, low-profile anatomic plates designed for GT fractures are also available for commercial use.68
Figure 8.
AP radiograph demonstrating a suture and proximal humerus locking plate fixation construct that was used to treat a split-type greater tuberosity fracture in a patient with osteoporotic bone. AP, anteroposterior.
Postoperatively, the arm is placed in a shoulder immobilizer in slight abduction to minimize passive tension on the fixation construct. In contrast to nonoperative management, passive motion is initiated at 1 week to minimize the risk of stiffness. Active motion is started at 6 weeks, and strengthening is permitted at 12 weeks.
A summary of the clinical outcomes following surgical treatment of GTFDs is displayed in Table II. There have been no prospective studies on this topic, and most of the literature reports the combined outcomes of isolated GT fractures and GTFDs. Among patients who undergo surgical fixation of GTFDs, excellent motion and patient-reported outcomes can be achieved. Dimakopoulos et al were the first to report on a series of surgically treated GTFDs and found very good-excellent results in 91% of patients with all patients returning to full work 7 months after surgery.14 Among studies that concomitantly repaired the Bankart tear or glenoid rim fracture, no further episodes of instability were observed.3,29,30,52,69 Among studies that did not repair the Bankart lesion, only one study reported a case of recurrent instability that was successfully treated nonoperatively.68
Table II.
Surgical outcomes of greater tuberosity fracture dsislocations.
| Study | N | Follow-up (y) | Age (y) | Male | Indication | Fixation method | Concomitant procedure | ROM (°) | Patient-reported outcomes | Revision ORIF |
|---|---|---|---|---|---|---|---|---|---|---|
| Zhang (2020)69 | 15 | 3.2 | 48 (22-66) | 7 | NA | Arthroscopic suture bridge: 100% Screw augmentation: 53% |
Glenoid Rim Repair: 15 RC Repair: 13 Biceps Tenodesis: 3 SLAP Repair: 1 Coracoid ORIF: 1 |
Flexion: 157 ER: 40 IR: T11 |
Constant: 95 ASES: 95 VAS pain: 0.4 |
0 (0%) |
| Dussing (2018)15 | 18 | 4.9 | 47 (15-71) | 11 | >3 mm | Percutaneous screw: 39% ORIF screw ± cerclage: 55% |
NA | Flexion: 151 Abduction: 150 ER: 48 |
SSV: 81% WOSI: 357 Rowe: 80 Constant: 79 |
5 (28%) |
| Plachel (2017)52 | 6 | 2.9 | 60 (37-85) | 5 | >5 mm | ORIF wires: 33% Percutaneous screw: 17% ORIF screw: 17% |
Glenoid Rim Repair: 6 Coracoid ORIF: 3 RC Repair: 1 |
Flexion: 133 Abduction: 138 |
Constant: 72 SST: 9.0 SSV: 72% |
1 (17%) |
| Park (2016)48 | 3 | 2.2 | 73 (64-83) | 0 | >5 mm | ORIF plate: 100% Suture anchor: 100% |
NA | Flexion: 132 Abduction: 132 ER: 3 IR: L3 |
ASES: 83 UCLA: 27 SST: 8.3 |
1 (33%) |
| Mattyasovszky (2011)70 | 4 | 3.0 | 54 (31-68) | 1 | NA | ORIF screw or plate: 100% | NA | NA | DASH: 11.4 Constant: 64 |
NA |
| Dimakopoulos (2007)14 | 34 | 4.8 | 53 (18-84) | 19 | All | Open transosseous suture repair: 100% | RC Repair: 6 Interval Repair: 16 |
Flexion: 170 Abduction: ER: 55 IR: T10 |
Constant: 88 | 0 (0%) |
| Summary∗ | 80 | 4.2 | 52 | 54 | - | Open: 5 Arthroscopic: 1 |
- | Flexion: 159 ER: 48 IR: T10 |
Constant: 85 | 7 (9.2%) |
ROM, range of motion; RC, rotator cuff; SLAP, superior labrum anterior posterior; ORIF, open reduction internal fixation; ER, external rotation at side; IR, internal rotation; ASES, American Shoulder and Elbow Sugeons; VAS, visual analog scale; WOSI, Western Ontario Shoulder Instability; SST, simple shoulder test; SSV, subjective shoulder value; UCLA, University of California Los Angeles Shoulder Score; DASH, disability of arm, shoulder, hand.
Weighted means calculated for summarized data.
Conclusion
GTFDs of the proximal humerus represent a separate entity from their isolated fracture counterparts in their evaluation and management. During glenohumeral reduction, an iatrogenic humeral neck fracture may occur due to the presence of an occult neck fracture or forceful reduction attempts with inadequate muscle relaxation. Nondisplaced and minimally displaced GT fragments after shoulder reduction can be successfully treated nonoperatively, but close follow-up is needed to monitor for secondary displacement of the fracture. Surgery is typically reserved for fractures with >5 mm displacement in any direction to minimize the risk of subacromial impingement and altered rotator cuff biomechanics. Multiple surgical techniques have been described, and the decision to employ a certain strategy should depend on fracture morphology and comminution, bone quality, and displacement.
Disclaimers
Funding: The current study was supported by National Institute on Aging grant number R38AG070171. This grant was used to fund the time taken for the literature review process.
Conflicts of interest: Favian Su reports receiving grant support from the National Institute on Aging. Jennifer Tangtiphaiboontana reports being a consultant for Stryker Corporation. Utku Kandemir reports receiving honoraria from AO North America, DePuy Synthes, and Stryker Corporation; committee member of American Academy of Orthopaedic Surgeons.
All authors of the above-referenced manuscript submission, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
The editor making the decision to accept this paper for publication had no conflicts of interest related to the decision. Further, peer review of this paper was handled independently of any author of this paper.
Footnotes
Institutional review board approval was not required for this review.
References
- 1.Alkaduhimi H., van der Woude H.J., Verweij L.P.E., Janssen S.J., Willigenburg N.W., Chen N., et al. Greater tuberosity fractures are not a continuation of Hill-Sachs lesions, but do they have a similar etiology? JSES Int. 2022;6:396–400. doi: 10.1016/j.jseint.2021.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atoun E., Narvani A., Even T., Dabasia H., Van Tongel A., Sforza G., et al. Management of first-time dislocations of the shoulder in patients older than 40 years: the prevalence of iatrogenic fracture. J Orthop Trauma. 2013;27:190–193. doi: 10.1097/BOT.0b013e31826576f8. [DOI] [PubMed] [Google Scholar]
- 3.Bahman M., Costil V., Gaume M., Rousseau M.A., Boyer P. Arthroscopic reduction and fixation with a knotless double-row construct provides good results for displaced greater tuberosity fractures. Arthrosc Sports Med Rehabil. 2021;3:e499–e504. doi: 10.1016/j.asmr.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bahrs C., Lingenfelter E., Fischer F., Walters E.M., Schnabel M. Mechanism of injury and morphology of the greater tuberosity fracture. J Shoulder Elbow Surg. 2006;15:140–147. doi: 10.1016/j.jse.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Bockmann B., Lechler P., Boese C.K., Aigner R., Ruchholtz S., Frink M. Risk factors for secondary displacement in conservatively treated isolated greater tuberosity fractures: an analysis of 82 cases. Orthop Traumatol Surg Res. 2019;105:317–322. doi: 10.1016/j.otsr.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 6.Boksh K., Srinivasan A., Perianayagam G., Singh H., Modi A. Morphological characteristics and management of greater tuberosity fractures associated with anterior glenohumeral joint dislocation: a single centre 10-year retrospective review. J Orthop. 2022;34:1–7. doi: 10.1016/j.jor.2022.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bono C.M., Renard R., Levine R.G., Levy A.S. Effect of displacement of fractures of the greater tuberosity on the mechanics of the shoulder. J Bone Joint Surg Br. 2001;83:1056–1062. doi: 10.1302/0301-620x.83b7.10516. [DOI] [PubMed] [Google Scholar]
- 8.Braunstein V., Wiedemann E., Plitz W., Muensterer O.J., Mutschler W., Hinterwimmer S. Operative treatment of greater tuberosity fractures of the humerus--a biomechanical analysis. Clin Biomech. 2007;22:652–657. doi: 10.1016/j.clinbiomech.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Brien H., Noftall F., MacMaster S., Cummings T., Landells C., Rockwood P. Neer's classification system: a critical appraisal. J Trauma. 1995;38:257–260. doi: 10.1097/00005373-199502000-00022. [DOI] [PubMed] [Google Scholar]
- 10.Bruinsma W.E., Guitton T.G., Warner J.J., Ring D., Science of Variation G. Interobserver reliability of classification and characterization of proximal humeral fractures: a comparison of two and three-dimensional CT. J Bone Joint Surg Am. 2013;95:1600–1604. doi: 10.2106/JBJS.L.00586. [DOI] [PubMed] [Google Scholar]
- 11.Chang C.J., Su W.R., Hsu K.L., Hong C.K., Kuan F.C., Chang C.H., et al. Augmented cerclage wire improves the fixation strength of a two-screw construct for humerus split type greater tuberosity fracture: a biomechanical study. BMC Musculoskelet Disord. 2021;22:350. doi: 10.1186/s12891-021-04215-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Court-Brown C.M., Garg A., McQueen M.M. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72:365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 13.Cuomo F., Flatow E.L., Maday M.G., Miller S.R., McIlveen S.J., Bigliani L.U. Open reduction and internal fixation of two- and three-part displaced surgical neck fractures of the proximal humerus. J Shoulder Elbow Surg. 1992;1:287–295. doi: 10.1016/S1058-2746(09)80055-4. [DOI] [PubMed] [Google Scholar]
- 14.Dimakopoulos P., Panagopoulos A., Kasimatis G., Syggelos S.A., Lambiris E. Anterior traumatic shoulder dislocation associated with displaced greater tuberosity fracture: the necessity of operative treatment. J Orthop Trauma. 2007;21:104–112. doi: 10.1097/BOT.0b013e3180316cda. [DOI] [PubMed] [Google Scholar]
- 15.Dussing F., Plachel F., Grossauer T., Hoffelner T., Schulz E., von Keudell A., et al. Anterior shoulder dislocation and concomitant fracture of the greater tuberosity: clinical and radiological results. Obere Extrem. 2018;13:211–217. doi: 10.1007/s11678-018-0451-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flatow E.L., Cuomo F., Maday M.G., Miller S.R., McIlveen S.J., Bigliani L.U. Open reduction and internal fixation of two-part displaced fractures of the greater tuberosity of the proximal part of the humerus. J Bone Joint Surg Am. 1991;73:1213–1218. [PubMed] [Google Scholar]
- 17.Foroohar A., Tosti R., Richmond J.M., Gaughan J.P., Ilyas A.M. Classification and treatment of proximal humerus fractures: inter-observer reliability and agreement across imaging modalities and experience. J Orthop Surg Res. 2011;6:38. doi: 10.1186/1749-799X-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garg A., McQueen M.M., Court-Brown C.M. Nerve injury after greater tuberosity fracture dislocation. J Orthop Trauma. 2000;14:117–118. [Google Scholar]
- 19.Gaudelli C., Menard J., Mutch J., Laflamme G.Y., Petit Y., Rouleau D.M. Locking plate fixation provides superior fixation of humerus split type greater tuberosity fractures than tension bands and double row suture bridges. Clin Biomech. 2014;29:1003–1008. doi: 10.1016/j.clinbiomech.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 20.George M.S. Fractures of the greater tuberosity of the humerus. J Am Acad Orthop Surg. 2007;15:607–613. doi: 10.5435/00124635-200710000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Godin J.A., Katthagen J.C., Fritz E.M., Pogorzelski J., Millett P.J. Arthroscopic treatment of greater tuberosity avulsion fractures. Arthrosc Tech. 2017;6:e777–e783. doi: 10.1016/j.eats.2017.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gruson K.I., Ruchelsman D.E., Tejwani N.C. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39:284–298. doi: 10.1016/j.injury.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 23.Gumina S., Carbone S., Postacchini F. Occult fractures of the greater tuberosity of the humerus. Int Orthop. 2009;33:171–174. doi: 10.1007/s00264-007-0512-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo J., Liu Y., Jin L., Yin Y., Hou Z., Zhang Y. Size of greater tuberosity fragment: a risk of iatrogenic injury during shoulder dislocation reduction. Int Orthop. 2019;43:1215–1222. doi: 10.1007/s00264-018-4022-8. [DOI] [PubMed] [Google Scholar]
- 25.Hebert-Davies J., Mutch J., Rouleau D., Laflamme G.Y. Delayed migration of greater tuberosity fractures associated with anterior shoulder dislocation. J Orthop Trauma. 2015;29:e396–e400. doi: 10.1097/BOT.0000000000000343. [DOI] [PubMed] [Google Scholar]
- 26.Huntley S.R., Lehtonen E.J., Robin J.X., Arguello A.M., Rouleau D.M., Brabston E.W., et al. Outcomes of surgical fixation of greater tuberosity fractures: a systematic review. Orthop Traumatol Surg Res. 2020;106:1119–1126. doi: 10.1016/j.otsr.2020.05.005. [DOI] [PubMed] [Google Scholar]
- 27.Janssen S.J., Hermanussen H.H., Guitton T.G., van den Bekerom M.P., van Deurzen D.F., Ring D. Greater tuberosity fractures: does fracture assessment and treatment recommendation vary based on imaging modality? Clin Orthop Relat Res. 2016;474:1257–1265. doi: 10.1007/s11999-016-4706-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Janssen S.J., Jayakumar P., Ter Meulen D.P., van Deurzen D.F.P., Ring D. Quantitative 3-dimensional computerized tomography modeling of isolated greater tuberosity fractures with and without shoulder dislocation. Arch Bone Jt Surg. 2019;7:24–32. [PMC free article] [PubMed] [Google Scholar]
- 29.Ji J.H., Jeong J.J., Kim Y.Y., Lee S.W., Kim D.Y., Park S.E. Clinical and radiologic outcomes of arthroscopic suture bridge repair for the greater tuberosity fractures of the proximal humerus. Arch Orthop Trauma Surg. 2017;137:9–17. doi: 10.1007/s00402-016-2586-6. [DOI] [PubMed] [Google Scholar]
- 30.Ji J.H., Shafi M., Song I.S., Kim Y.Y., McFarland E.G., Moon C.Y. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy. 2010;26:600–609. doi: 10.1016/j.arthro.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 31.Kelley S.P., Hinsche A.F., Hossain J.F. Axillary artery transection following anterior shoulder dislocation: classical presentation and current concepts. Injury. 2004;35:1128–1132. doi: 10.1016/j.injury.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 32.Kim E., Shin H.K., Kim C.H. Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci. 2005;10:441–444. doi: 10.1007/s00776-005-0924-6. [DOI] [PubMed] [Google Scholar]
- 33.Kim S.H., Ha K.I. Arthroscopic treatment of symptomatic shoulders with minimally displaced greater tuberosity fracture. Arthroscopy. 2000;16:695–700. doi: 10.1053/jars.2000.9237. [DOI] [PubMed] [Google Scholar]
- 34.Kuan F.C., Hsu K.L., Hong C.K., Chen Y., Chiang C.H., Chang H.M., et al. Biomechanical comparisons of hook plate and screw fixations in split-type greater tuberosity fractures of the humerus. J Shoulder Elbow Surg. 2022;31:1308–1315. doi: 10.1016/j.jse.2021.12.023. [DOI] [PubMed] [Google Scholar]
- 35.Li R., Cai M., Tao K. Arthroscopic reduction and fixation for displaced greater tuberosity fractures using the modified suture-bridge technique. Int Orthop. 2017;41:1257–1263. doi: 10.1007/s00264-017-3461-y. [DOI] [PubMed] [Google Scholar]
- 36.Lin C.L., Hong C.K., Jou I.M., Lin C.J., Su F.C., Su W.R. Suture anchor versus screw fixation for greater tuberosity fractures of the humerus--a biomechanical study. J Orthop Res. 2012;30:423–428. doi: 10.1002/jor.21530. [DOI] [PubMed] [Google Scholar]
- 37.Maman E., Dolkart O., Chechik O., Amar E., Rak O., Rath E., et al. Arthroscopic findings of coexisting lesions with greater tuberosity fractures. Orthopedics. 2014;37:e272–e277. doi: 10.3928/01477447-20140225-60. [DOI] [PubMed] [Google Scholar]
- 38.Mason B.J., Kier R., Bindleglass D.F. Occult fractures of the greater tuberosity of the humerus: radiographic and MR imaging findings. AJR Am J Roentgenol. 1999;172:469–473. doi: 10.2214/ajr.172.2.9930805. [DOI] [PubMed] [Google Scholar]
- 39.McLaughlin H.L. Dislocation of the shoulder with tuberosity fracture. Surg Clin North Am. 1963;43:1615–1620. doi: 10.1016/s0039-6109(16)37150-x. [DOI] [PubMed] [Google Scholar]
- 40.McLaughlin J.A., Light R., Lustrin I. Axillary artery injury as a complication of proximal humerus fractures. J Shoulder Elbow Surg. 1998;7:292–294. doi: 10.1016/s1058-2746(98)90058-1. [DOI] [PubMed] [Google Scholar]
- 41.Meinberg E.G., Agel J., Roberts C.S., Karam M.D., Kellam J.F. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32:S1–S170. doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 42.Mutch J., Laflamme G.Y., Hagemeister N., Cikes A., Rouleau D.M. A new morphological classification for greater tuberosity fractures of the proximal humerus: validation and clinical implications. Bone Joint Lett J. 2014;96-B:646–651. doi: 10.1302/0301-620X.96B5.32362. [DOI] [PubMed] [Google Scholar]
- 43.Mutch J.A., Rouleau D.M., Laflamme G.Y., Hagemeister N. Accurate measurement of greater tuberosity displacement without computed tomography: validation of a method on plain radiography to guide surgical treatment. J Orthop Trauma. 2014;28:445–451. doi: 10.1097/BOT.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 44.Neer C.S., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 45.Nyffeler R.W., Seidel A., Werlen S., Bergmann M. Radiological and biomechanical assessment of displaced greater tuberosity fractures. Int Orthop. 2019;43:1479–1486. doi: 10.1007/s00264-018-4170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Okike K., Lee O.C., Makanji H., Harris M.B., Vrahas M.S. Factors associated with the decision for operative versus non-operative treatment of displaced proximal humerus fractures in the elderly. Injury. 2013;44:448–455. doi: 10.1016/j.injury.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 47.Pan X., Yao Y., Yan H., Wang J., Dai L., Qu X., et al. Iatrogenic fracture during shoulder dislocation reduction: characteristics, management and outcomes. Eur J Med Res. 2021;26:73. doi: 10.1186/s40001-021-00545-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Park S.E., Jeong J.J., Panchal K., Lee J.Y., Min H.K., Ji J.H. Arthroscopic-assisted plate fixation for displaced large-sized comminuted greater tuberosity fractures of proximal humerus: a novel surgical technique. Knee Surg Sports Traumatol Arthrosc. 2016;24:3892–3898. doi: 10.1007/s00167-015-3805-3. [DOI] [PubMed] [Google Scholar]
- 49.Park T.S., Choi I.Y., Kim Y.H., Park M.R., Shon J.H., Kim S.I. A new suggestion for the treatment of minimally displaced fractures of the greater tuberosity of the proximal humerus. Bull Hosp Jt Dis. 1997;56:171–176. [PubMed] [Google Scholar]
- 50.Parsons B.O., Klepps S.J., Miller S., Bird J., Gladstone J., Flatow E. Reliability and reproducibility of radiographs of greater tuberosity displacement. A cadaveric study. J Bone Joint Surg Am. 2005;87:58–65. doi: 10.2106/JBJS.C.01576. [DOI] [PubMed] [Google Scholar]
- 51.Pitcher A., Langhammer C., Feeley B.T. Utility of MRI in the evaluation of acute greater tuberosity proximal humeral fractures. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119851472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Plachel F., Schanda J.E., Ortmaier R., Auffarth A., Resch H., Bogner R. The “triple dislocation fracture”: anterior shoulder dislocation with concomitant fracture of the glenoid rim, greater tuberosity and coracoid process-a series of six cases. J Shoulder Elbow Surg. 2017;26:e278–e285. doi: 10.1016/j.jse.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 53.Platzer P., Kutscha-Lissberg F., Lehr S., Vecsei V., Gaebler C. The influence of displacement on shoulder function in patients with minimally displaced fractures of the greater tuberosity. Injury. 2005;36:1185–1189. doi: 10.1016/j.injury.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 54.Ranawat A.S., DiFelice G.S., Suk M., Lorich D.G., Helfet D.L. Iatrogenic propagation of anterior fracture-dislocations of the proximal humerus: case series and literature review with suggested guidelines for treatment and prevention. Am J Orthop (Belle Mead NJ) 2007;36:E133–E137. [PubMed] [Google Scholar]
- 55.Robinson C.M., Khan L.A., Akhtar M.A. Treatment of anterior fracture-dislocations of the proximal humerus by open reduction and internal fixation. J Bone Joint Surg Br. 2006;88:502–508. doi: 10.1302/0301-620X.88B4.17195. [DOI] [PubMed] [Google Scholar]
- 56.Robinson C.M., Shur N., Sharpe T., Ray A., Murray I.R. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am. 2012;94:18–26. doi: 10.2106/JBJS.J.01795. [DOI] [PubMed] [Google Scholar]
- 57.Roddy E., Kandemir U. High rate of AVN but excellent patient reported outcomes after ORIF of proximal humerus fracture dislocations: should ORIF be considered as primary treatment? J Shoulder Elbow Surg. 2023 doi: 10.1016/j.jse.2023.04.002. [DOI] [PubMed] [Google Scholar]
- 58.Rouleau D.M., Laflamme G.Y., Mutch J. Fractures of the greater tuberosity of the humerus: a study of associated rotator cuff injury and atrophy. Shoulder Elbow. 2016;8:242–249. doi: 10.1177/1758573216647896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rouleau D.M., Mutch J., Laflamme G.Y. Surgical treatment of displaced greater tuberosity fractures of the humerus. J Am Acad Orthop Surg. 2016;24:46–56. doi: 10.5435/JAAOS-D-14-00289. [DOI] [PubMed] [Google Scholar]
- 60.Schnetzke M., Bockmeyer J., Loew M., Studier-Fischer S., Grutzner P.A., Guehring T. Rate of avascular necrosis after fracture dislocations of the proximal humerus: timing of surgery. Obere Extrem. 2018;13:273–278. doi: 10.1007/s11678-018-0452-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shaw L., Hong C.K., Kuan F.C., Lin C.L., Wang P.H., Su W.R. The incidence of occult and missed surgical neck fractures in patients with isolated greater tuberosity fracture of the proximal humerus. BMC Musculoskelet Disord. 2019;20:482. doi: 10.1186/s12891-019-2810-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Siebenburger G., Van Delden D., Helfen T., Haasters F., Bocker W., Ockert B. Timing of surgery for open reduction and internal fixation of displaced proximal humeral fractures. Injury. 2015;46:S58–S62. doi: 10.1016/S0020-1383(15)30019-X. [DOI] [PubMed] [Google Scholar]
- 63.Thorsness R., English C., Gross J., Tyler W., Voloshin I., Gorczyca J. Proximal humerus fractures with associated axillary artery injury. J Orthop Trauma. 2014;28:659–663. doi: 10.1097/BOT.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 64.Wang Y.P., Zhao J.Z., Huangfu X.Q., Liu W.X., Jiang Y., Zhou X.H., et al. Arthroscopic reduction and fixation for isolated greater tuberosity fractures. Chin Med J (Engl) 2012;125:1272–1275. [PubMed] [Google Scholar]
- 65.Wronka K.S., Ved A., Mohanty K. When is it safe to reduce fracture dislocation of shoulder under sedation? Proposed treatment algorithm. Eur J Orthop Surg Traumatol. 2017;27:335–340. doi: 10.1007/s00590-016-1899-z. [DOI] [PubMed] [Google Scholar]
- 66.Wu J., Han Z., Wang Q., Wu X. Inferior displacement of greater tuberosity fracture suggests an occult humeral neck fracture: a retrospective single-centre study. Int Orthop. 2019;43:1429–1434. doi: 10.1007/s00264-019-04294-1. [DOI] [PubMed] [Google Scholar]
- 67.Yuan W., Chua I.T.H. Should closed reduction be attempted in the emergency department for an acute anterior shoulder fracture dislocation? JSES Int. 2021;5:56–59. doi: 10.1016/j.jseint.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zeng L.Q., Chen Y.F., Jiang Y.W., Zeng L.L., Miao X.G., Liang W.G. A new low-profile anatomic locking plate for fixation of comminuted, displaced greater tuberosity fractures of the proximal humerus. J Shoulder Elbow Surg. 2021;30:1402–1409. doi: 10.1016/j.jse.2020.08.036. [DOI] [PubMed] [Google Scholar]
- 69.Zhang Q., Xiang M., Li Y.P., Yang J.S. Arthroscopic management of glenoid and greater tuberosity bipolar fractures. Orthop Surg. 2020;12:1405–1412. doi: 10.1111/os.12786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mattyasovszky S.G., Burkhart K.J., Ahlers C., Proschek D., Dietz S.O., Becker I. Isolated fractures of the greater tuberosity of the proximal humerus: a long-term retrospective study of 30 patients. Acta Orthop. 2011;82:714–720. doi: 10.3109/17453674.2011.618912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Razaeian S., Hawi N., Zhang D., Liodakis E., Krettek C. Conservative treatment of displaced isolated proximal humerus greater tuberosity fractures: preliminary results of a prospective, CT-based registry study. Eur J Trauma Emerg Surg. 2022;48:4531–4543. doi: 10.1007/s00068-020-01453-7. [DOI] [PubMed] [Google Scholar]