Abstract
Biceps tenodesis is an accepted treatment option for various pathologies of the long head of the biceps tendon and labrum. Many techniques have been published, both arthroscopic and open, that utilize various fixation techniques and locations of the tenodesis, yet none has been proven to be superior. We introduce a novel method, the SALSA (subacromial locking stitch anchor), an all-arthroscopic suprapectoral biceps tenodesis utilizing a running locking stitch from a double-loaded biocomposite anchor. This technique provides a reliable method of multipoint fixation including the transverse humeral ligament that avoids many of the potential complications encountered with other techniques.
Keywords: Arthroscopic biceps tenodesis, Suprapectoral, Biceps brachii, Locking stitch, Biceps tenodesis, Arthroscopic, Long head of the biceps, Shoulder
Pathology of the long head of the biceps tendon (LHBT), whether in isolation or associated with other shoulder conditions, has long been recognized as a significant generator of pain and dysfunction.2,4,8 When conservative efforts fail to improve a patient’s symptoms, operative treatment becomes a viable option. The 2 main surgical options for the LHBT are tenotomy and tenodesis. Tenodesis has the advantages of lowering the incidence of cosmetic deformity and decreasing muscle spasms and fatigue by maintaining the tension-length relationship of the biceps muscle.3,10,12 Multiple techniques have been published for both arthroscopic and open biceps tenodesis. They vary by location of tenodesis and type of fixation used. Techniques can be divided into 2 main groups: suprapectoral and subpectoral. Fixation techniques include bone tunnels, simple sutures, cortical buttons, interference screws, and various types of anchors. All have advantages and disadvantages.
We describe a novel arthroscopic technique, the SALSA (subacromial locking stitch anchor), utilizing running, locking stitches from a double-loaded biocomposite anchor placed in the suprapectoral region of the bicipital groove at the LHBT’s normal resting length that incorporates the transverse humeral ligament for added stability.
Surgical technique
The patient is positioned in the beach chair position under general anesthesia with an interscalene block placed preoperatively. The operative arm is attached to a limb positioner such as the SPIDER2 (Smith & Nephew, Andover, MA, USA) to allow for manipulation throughout the procedure. The arm is placed in slight abduction and neutral rotation.
Diagnostic glenohumeral arthroscopy is performed first with the 30° arthroscope placed through the standard posterior portal. An anterior portal is established centrally in the rotator interval and a disposable cannula is inserted. Biceps pathology is visualized by pulling the LHBT into the joint utilizing a probe and looking into the bicipital groove. The location of the bicipital groove is marked percutaneously utilizing a spinal needle through which a 3-0 Prolene marking suture is placed (Fig. 1). The suture is retrieved via the anterior portal and serves to mark the location of the bicipital groove in the subacromial space. The arthroscope is then redirected via the posterior portal into the subacromial space. A mid-lateral portal is established and a working cannula is placed in the subacromial space. A subacromial bursectomy is performed using a full radius resector and thermal ablation device. Next, the recess between the tuberosities and undersurface of the deltoid is cleared. Care is taken to avoid bleeding as much as possible by utilizing the thermal ablation probe. This device should be used with caution in the area of the axillary neurovascular bundle on the undersurface of the deltoid.
Figure 1.
A 3-0 Prolene marking suture is placed percutaneously with a spinal needle into the LHBT to ease finding the location of the bicipital groove in the subacromial space. LHBT, long head of the biceps tendon.
Next, the shoulder is externally rotated approximately 45 degrees to allow better visualization of the bicipital groove via the posterior portal. In very large patients, it is sometimes advantageous to move the scope to a posterolateral portal for better visualization. The mid-lateral portal functions as a working portal for suture passage and tying. An anterolateral portal is established for anchor placement. Its location is anterior to the mid-lateral portal approximately 4 cm distal to the anterolateral margin of the acromion (Fig. 2).
Figure 2.
Portal placement with reference to anatomic landmarks: posterior portal (P), lateral portal (L), anterolateral portal (AL), anterior portal (A).
The thermal ablation probe is used to cautiously palpate for the bicipital groove through the lateral portal. The Prolene marking suture is helpful in identifying the general location of the groove. The probe can usually be felt to fall over the rim of the groove and release of the ligament may be started at this point. The posterior insertion of the transverse humeral ligament is released utilizing the thermal probe beginning at the most superior aspect of the bicipital groove and passing inferiorly for approximately 4 cm (Fig. 3). This must be done cautiously to avoid bleeding from adjacent vessels and inadvertent transection of the tendon. The ascending branch of the anterior humeral circumflex vessels is located anterior to the bicipital groove making release of the posterior attachment of the transverse humeral ligament a safer option. After releasing the ligament, the biceps tendon can be visualized.
Figure 3.
With the arm in abduction and external rotation, the posterior insertion of the transverse humeral ligament is released utilizing the thermal probe beginning at the most superior aspect of the bicipital groove and passing inferiorly for approximately 4 cm.
A spinal needle is used to localize the position of the anterolateral portal to facilitate direct insertion of an anchor into the mid-portion of the exposed bicipital groove. Once the appropriate positioning is determined, an incision is made and the HEALICOIL Awl-Dilator is introduced followed by insertion of the HEALICOIL REGENESORB 4.75 mm Anchor with double-loaded #2 ULTRABRAID sutures (Blue, Cobraid Blue; Smith & Nephew, Andover, MA, USA).
While viewing from the posterior portal, one Blue suture limb is retrieved via the mid-lateral portal utilizing a crab claw suture retriever. The Blue suture limb is loaded onto a self-retrieving suture passing device and inserted via the mid-lateral portal. Sutures are passed inferior to the anchor initially. The Blue suture is passed through both the biceps tendon and transverse humeral ligament. The Blue suture is retrieved back through the mid-lateral portal and the suture passer is reloaded with the same Blue suture. The same Blue suture limb is passed through the tendon a total of 4 times. In order to create a locking stitch, the suture passer is looped around the stitch before passing the suture through the tendon a second time. In the right shoulder, the suture passer is rotated in a counterclockwise direction around the suture while progressing inferiorly. The opposite is true on the left shoulder. The fourth pass with this suture is placed adjacent to the anchor again in a locking stitch fashion by rotating the suture passer around the stitch prior to placement in the biceps tendon and transverse humeral ligament (Fig. 4). This maneuver avoids over- or under-tensioning of the biceps. The Blue suture limb is now retrieved back through the anterolateral portal and one suture limb from the other Cobraid Blue suture is retrieved via the mid-lateral portal. The sequence is then repeated this time moving progressively superiorly. In the right shoulder, the suture passer is rotated in a clockwise direction around the suture while progressing superiorly. The opposite is true on the left shoulder. Again, the final pass of the suture is placed adjacent to the anchor. The suture pairs are retrieved via the mid-lateral portal and tied using non-sliding Revo knots. The suture tails are cut and the arthroscope is redirected via the posterior portal back into the glenohumeral joint. A thermal ablation device is passed via the anterior portal into the joint to release the biceps tendon from its origin at the superior labrum. The tendon should remain in the joint and not pass down through the bicipital groove if the tenodesis has been performed properly (Fig. 5). The described surgical steps for the SALSA technique including arthroscopic footage of passing the locking stitches are shown in Supplementary Video S1.
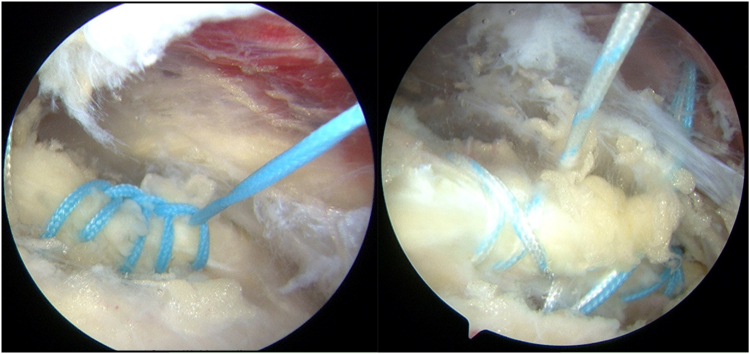
Figure 4.
The inferior Blue suture limb is passed through the tendon and transverse humeral ligament a total of 4 times utilizing a locking stitch configuration with the fourth pass placed adjacent to the anchor.
Figure 5.
LHBT remains in the joint and does not pass down through the bicipital groove if the tenodesis has been performed properly. LHBT, long head of the biceps tendon.
Discussion
Tenodesis is a widely accepted treatment option for various pathologies affecting the LHBT; however, there is no consensus as to the ideal technique and site of tenodesis. Arthroscopic bicipital tenodesis continues to evolve with improvements in instrumentation and fixation devices since its first description by Gartsman et al in 2000.1 Our technique offers multiple advantages compared to previously reported techniques.
The SALSA technique is an all-arthroscopic technique. There is no need for a separate incision in the axilla; this lessens the chance of a deep wound infection, increased blood loss, and poor cosmesis from a larger incision. Although the axillary nerve is adjacent to the area of tenodesis, it is protected during our technique by staying posterior to the bicipital groove and maintaining visualization with the arthroscope. Unlike an open axillary approach, the SALSA technique tenodesis site is far from the musculocutaneous nerve which is at risk during subpectoral techniques with musculocutaneous neuropathy and brachial plexopathy described as potential complications during dissection and retraction.7
Our technique describes a tenodesis in situ, performed prior to releasing the LHBT from its superior attachment to the labrum thereby fixing the tendon anatomically and decreasing the possibility of over- or under-tensioning. Multiple points of fixation are achieved between the biceps tendon, sheath, and the static transverse humeral ligament during our technique by the locking sutures which run both superior and inferior to the anchor. Other techniques rely on a single point of fixation which may fail more easily. While the minimum load to failure required to achieve a clinically reliable tenodesis is unknown, a recent biomechanical study of suture anchors compared to interference screws and a compressive rivet resulted in favorable results for the suture anchor.11
The SALSA tenodesis is performed in the area identified as containing significant amounts of pathology. The biceps tendon is secured within this area eliminating tension on an abnormal tendon which may occur from superior placement of the anchor at the entry of the bicipital groove. McCrum et al found no difference in anterior shoulder pain, cramping, weakness, or deformity for suprapectoral vs. subpectoral tenodesis; however, subpectoral tenodesis had an increased risk of transient nerve injury.5
Another advantage of our technique is the relatively small unicortical hole made in the metaphyseal portion of the proximal humerus minimizing the chances of fracture. The creation of a large drill hole in the proximal diaphysis of the humerus as required in subpectoral interference screw techniques has been shown to increase the susceptibility of humeral fracture with an applied torsional load.6 Techniques that involve bicortical drilling, such as transhumeral button fixation, increase the risk of injury to the posterolateral neurovascular structures (axillary nerve, posterior humeral circumflex artery, and radial nerve).9
This technique does have its challenges. It may be difficult to visualize the bicipital groove in larger individuals via the posterior portal but modifications in the technique discussed above are usually successful. Use of the ablation probe adjacent to the axillary neurovascular bundle results in contraction of the muscle and must be performed cautiously. The marking suture will guide the surgeon to the general location of the bicipital groove but the surgeon must release the transverse humeral ligament cautiously and determine the direction of the bicipital groove to avoid inadvertent transection of the biceps tendon utilizing the thermal ablation probe. This technique is easier to perform with a self-retrieving suture passer although a grasper can also be placed into the anterolateral portal to assist with this step.
Conclusion
The SALSA technique is an all-arthroscopic suprapectoral biceps tenodesis that utilizes a double-loaded biocomposite anchor with a running, locking stitch securing the LHBT at the normal resting tension with multiple points of fixation along the transverse humeral ligament. This technique provides a reliable method of robust fixation that avoids the potential complications including cramping, neurologic injury, or cosmetic deformity.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: Xavier Duralde is a paid consultant for Smith & Nephew. The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this technical note.
Supplementary data to this article can be found online at 10.1016/j.xrrt.2024.02.006.
Supplementary Data
Surgical steps summarizing the SALSA technique.
References
- 1.Gartsman G.M., Hammerman S.M. Arthroscopic biceps tenodesis: operative technique. Arthroscopy. 2000;16:550–552. doi: 10.1053/jars.2000.4386. [DOI] [PubMed] [Google Scholar]
- 2.Hitchcock H.H., Bechtol C.O. Painful shoulder: observations on the role of the tendon of the long head of the biceps brachii in its causation. J Bone Joint Surg Am. 1948;30:263–273. [PubMed] [Google Scholar]
- 3.Hsu A.R., Ghodadra N.S., Provencher M.T., Lewis P.B., Bach B.R. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326–332. doi: 10.1016/j.jse.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 4.Lippmann R.K. Frozen shoulder; periarthritis; bicipital tenosynovitis. Arch Surg. 1943;47:283–296. [Google Scholar]
- 5.McCrum C.L., Alluri R.K., Batech M., Mirzayan R. Complications of biceps tenodesis based on location, fixation, and indication: a review of 1526 shoulders. J Shoulder Elbow Surg. 2019;28:461–469. doi: 10.1016/j.jse.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Mellano C.R., Frank R.M., Shin J.J., Jain A., Zuke W.A., Mascarenhas R., et al. Subpectoral biceps tenodesis with PEEK interference screw: a biomechanical analysis of humeral fracture risk. Arthroscopy. 2018;34:806–813. doi: 10.1016/j.arthro.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Nho S.J., Reiff S.N., Verma N.N., Slabaugh M.A., Mazzocca A.D., Romeo A.A. Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19:764–768. doi: 10.1016/j.jse.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Nho S.J., Strauss E., Lenart B., Provencher M.T., Mazzocca A.D., Verma N.N., et al. Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18:645–656. doi: 10.5435/00124635-201011000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Saithna A., Longo A., Jordan R.W., Leiter J., MacDonald P., Old J. A cadaveric assessment of the risk of nerve injury during open subpectoral biceps tenodesis using a bicortical guidewire. Knee Surg Sports Traumatol Arthrosc. 2017;25:2858–2863. doi: 10.1007/s00167-015-3972-2. [DOI] [PubMed] [Google Scholar]
- 10.Slenker N.R., Lawson K., Ciccotti M.G., Dodson C.C., Cohen S.B. Biceps tenotomy versus tenodesis: clinical outcomes. Arthroscopy. 2012;28:576–582. doi: 10.1016/j.arthro.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 11.Vestermark G., Hartigan D., Piasecki D., Fleischli J., Odum S.M., Zheng N., et al. Biceps tenodesis: biomechanical assessment of 3 arthroscopic suprapectoral techniques. Orthopedics. 2017;40:e1009–e1016. doi: 10.3928/01477447-20170925-03. [DOI] [PubMed] [Google Scholar]
- 12.Werner B.C., Lyons M.L., Evans C.L., Griffin J.W., Hart J.M., Miller M.D., et al. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of restoration of length-tension and mechanical strength between techniques. Arthroscopy. 2015;31:620–627. doi: 10.1016/j.arthro.2014.10.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical steps summarizing the SALSA technique.