Timeline of heart-lung bloc from crossclamp to end of ischemic time.
Central Message.
Excellent heart-lung bloc preservation was achieved with a multiuse 10 °C static storage system allowing for safe transplantation in a complex redo chest recipient with an extended ischemic time.
Case Presentation
A 26-year-old man with a history of dextro-transposition of the great arteries status post Senning procedure presented with group 1 pulmonary hypertension, congestive hepatopathy, and right heart failure. He was listed for heart-lung transplant. A suitable donor was identified. During procurement, antegrade Perfadex solution (XVIVO) (6 L stored at 4 °C) and antegrade del Nido cardioplegia solution (1200 mL stored at 4 °C) were utilized for the lungs and heart, respectively. The inferior vena cava and the left atrial appendage were incised for venting. Cooled saline was applied topically rather than ice slush to minimize potential cold injury to the heart and lungs, which has been our standard practice since initiating 10 °C storage. This practice is based on our interpretation of published 10 °C data and our as of yet unpublished laboratory data. The heart-lung bloc was excised, placed in a sterile organ storage bag with cooled Perfadex solution (3 L stored at 10 °C), and the bags de-aired. Two outer bags remained empty but were similarly de-aired. The bloc was placed into the 10 °C storage system for transport and temperature monitoring (Figure 1). The heart-lung bloc was placed in a designated 10 °C organ storage refrigerator upon arrival to our hospital.
Figure 1.
A, A storage system that maintains 10 °C with gel packs and a temperature log for heart-lung bloc in transit. B, Average temperature during cooler storage was 10.43 °C.
The recipient underwent a clamshell incision with careful mediastinal dissection and exposure of his ascending aorta. He was placed on venoarterial extracorporeal membrane oxygenation (ECMO) support via femoral drainage and aortic return using our low-dose heparin protocol, consisting of a 2000 U bolus followed by a 200 U/hour heparin drip, for bilateral pneumonectomies and tracheal preparation. No activated clotting time targets are used in our intraoperative ECMO protocol, and the heparin drip remained unchanged.1 Conversion to cardiopulmonary bypass with full-dose heparin was performed for cardiectomy and, subsequently, standard implantation of the heart-lung bloc. The allograft total ischemic time was 589 minutes (ie, 9.8 hours), with 46 minutes of warm ischemic time. The patient required no ECMO support postoperatively and demonstrated good allograft function (Heart: No primary graft dysfunction, Lungs: Primary graft dysfunction 2 at 72 hours). His 21-day intensive care unit stay was complicated by acute-on-chronic hepatic dysfunction, a mild transient acute kidney injury, and intensive care unit delirium despite excellent heart-lung function. His most recent echocardiogram 6 months following transplant demonstrated normal biventricular function and his tracheal anastomosis has healed very well (Figure 2). He remains comfortable on room air.
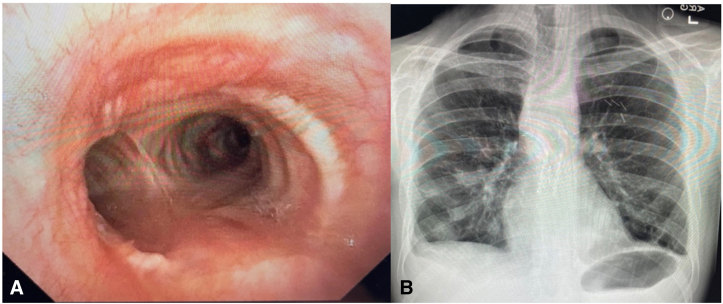
Figure 2.
Tracheal anastomosis 4 months following heart-lung transplant (A) and chest radiograph 4 months following heart-lung transplant (B).
Discussion
This case is the first report of successful extended static preservation of a heart-lung bloc at 10 °C (institutional review board approval was not required; patient consent given for publication). Despite nearly 10 hours of ischemic time, there was no significant allograft dysfunction during the early postoperative period and late function has been excellent.
Historically, ice storage allows for 4 to 6 hours of ischemic time for hearts and lungs, but rapid innovation to expand the existing donor pool has led to a paradigm shift. Machine perfusion and other temperature stabilizing devices promise greater distances and ex vivo time for donor organs, but often with expensive, single-use devices.2,3 Renewed interest in finding the optimal temperature for pulmonary allografts led to the development of a novel 10 °C storage system utilized in this case. A preliminary trial comparing ice storage to 10 °C storage of lungs demonstrated no adverse clinical outcomes and a trend toward improved primary graft dysfunction rates in the 10 °C group.4 Similarly, research has shown an optimal heart storage temperature may be 8°C to 12°C as a balance between energy substrate preservation and cellular integrity is achieved.5
We demonstrated the feasibility of using a simple, multiuse 10 °C storage device for heart-lung transplantation that sustained good allograft function. This case also represents the longest recorded allograft ischemic time (9.8 hours) for a heart-lung transplant to date. The success noted in this case warrants further investigation to better define optimal organ storage temperature and highlights the utility of a simple 10 °C static storage system to meet the needs of increasingly complex transplant recipients.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
Dr Bacchetta receives support through the Shelley and Fred Kleiner Research Fund and the David M. Livingston Lung Transplant Memorial Fund.
IRB Approval: This case report was exempt from IRB review.
Patient Consent: Consent given for publication.
References
- 1.Tucker W.D., Gannon W.D., Petree B., et al. Impact of anticoagulation intensity on blood transfusion for venoarterial extracorporeal membrane oxygenation during lung transplantation. J Heart Lung Transplant. 2024;43(5):832–837. doi: 10.1016/J.HEALUN.2024.02.008. [DOI] [PubMed] [Google Scholar]
- 2.Stamp N.L., Shah A., Vincent V., et al. Successful heart transplant after 10 hours out-of-body time using the TransMedics Organ Care System. Heart Lung Circ. 2015;24(6):611–613. doi: 10.1016/j.hlc.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Neto D., Guenthart B., Shudo Y., Currie M.E. World’s first en bloc heart-lung transplantation using the paragonix lungguard donor preservation system. J Cardiothorac Surg. 2023;18(1):131. doi: 10.1186/s13019-023-02281-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ali A., Hoetzenecker K., Luis Campo-Cañaveral de la Cruz J., et al. Extension of cold static donor lung preservation at 10°C. NEJM Evid. 2023;2(6) doi: 10.1056/EVIDoa2300008. [DOI] [PubMed] [Google Scholar]
- 5.Keon W.J., Hendry P.J., Taichman G.C., Mainwood G.W. Cardiac transplantation: the ideal myocardial temperature for graft transport. Ann Thorac Surg. 1988;46(3):337–341. doi: 10.1016/S0003-4975(10)65939-5. [DOI] [PubMed] [Google Scholar]