Abstract
Survey research enables the gathering of information on individual perspectives in a large cohort. It can be epidemiological, attitude or knowledge focussed. Assessment of survey studies sampling neurosurgeons is currently lacking in the literature. This study aimed to highlight the characteristics, quality, and citation predictors of the most influential survey research studies published in the neurosurgical literature. Using PubMed and Google Scholar, the 50 most cited survey research publications were identified and reviewed. Data relating to the characteristics of the articles, participants and questionnaires were retrieved. The studies’ quality and citation patterns were assessed. The median articles' age and publishing journal impact factor (IF) were 15.5 years and 2.82, respectively. Thirty-two (64%) articles were first authored by researchers from the USA while 28(56%) studies were focussed on specific disease management. The median number of participants and response rates were 222 and 51%, respectively. A full version of the questionnaire was provided in 18 (36%) articles. Only four (8%) articles reported validation of the questionnaire. The overall quality of reporting of the surveys was considered fair (based on good grading in five parameters, fair grading in one parameter, and poor grading in four parameters). The median citation number was 111. The citation analysis showed that the participant number, article age (≥15.5 years), and questionnaire category (surgical complications) were significant predictors of citation numbers. The citation rates were not influenced by the response rates or the journal’s IF. In conclusion, high-impact survey publications in the neurosurgical literature were moderately cited and of fair quality. Their citation numbers were not affected by response rates but were positively influenced by the publication age, number of participants, and by novel data or the questions raised in the survey category. Surveys are valuable forms of research that require extensive planning, time, and effort in order to produce meaningful results. Increasing awareness of the factors that could affect citations may be useful to those who wish to undertake survey research
Keywords: citation rates, pubmed, publication trends, bibliometrics, spine journals, neurosurgical journals, survey questionnaire
Introduction and background
Surveys are research methods in which information is typically collected by asking a subset of people questions on a specific topic and generalizing the results to a larger population [1,2]. They are widely used in many specialities, but mostly in public health, politics, ethics, and education [1,2]. Surveys are particularly valuable in studies that need patients or clinicians to self-report their experiences, satisfaction, and attitudes towards concepts that are difficult to measure using alternative approaches [1,2]. They are useful at the beginning of exploratory studies and can be the basis for going on to the next levels of evidence [1,2]. Surveys are generally considered low-cost research tools that are easy to apply [2]. However, to be reliable, they require good planning and construction as well as clear reporting so readers can judge the strengths and weaknesses of the study as well as the generalizability of the results [1-3]. The number of surveys published in the medical literature has increased in recent years [1,3]. Furthermore, assessing the quality of survey research is a topic of current interest in the literature [1-5]. Most of the published reviews stated that the quality of the reporting of surveys was either poor [1,3] or moderate [2,4,5]. The issues raised included weak designs of questionnaires, lack of validation and reliability tests of the instruments used, low response rates, shortage of information on the representativeness of the samples, and deficiency of explanations on how missing data was handled [1-5]. Recent guidelines for clinical survey research emphasized the need to reduce potential sources of bias by using validated questions, pre-testing the questionnaires, and enhancing response rates by using incentives or reminders [2,4].
The number of citations a published article receives is arguably one of the most important indicators of its impact and clinical weight. Identification of the predictors of citations is valuable for researchers to enhance the impact of their work. It is a topic that has been the subject of numerous studies in recent years. Most publications on the matter concentrated on determining the predictors of citations in articles relating to certain medical specialties, disease processes, peer-reviewed journals, or a specific research methodology [6,7]. Analysis of the citation patterns of survey research remains limited in the literature. Furthermore, assessments of survey studies sampling neurosurgeons are also lacking. The purpose of this study is to identify and review the most-cited survey research studies that were published in the neurosurgical literature. The review aimed to highlight the characteristics and quality of survey research studies that sampled neurosurgeons and determine the factors that affect the citation numbers of the top 50 most-influential studies on the subject.
Review
Methods
Search Strategy
No ethical approval was necessary by our institutions as the study was based on data obtained from open-access sources. The PubMed database was searched on 1st October 2023 for suitable articles using the following combinations: [Title] “survey” AND [Journal] “individual neurosurgical and spine journals by name”. The list of journals searched, and the number of screened articles is shown in Table 1. The search yielded a total of 921 publications in 30 neurosurgical and spine journals which will be referred to as neurosurgical journals in this study.
Table 1. List of the searched neurosurgical journals showing numbers of the screened and selected articles.
| Searched journals | Screened articles number | Selected most cited studies number |
| Spine | 100 | 7 |
| Journal of Neurosurgery | 66 | 7 |
| World Neurosurgery | 136 | 6 |
| Neurosurgery | 45 | 6 |
| Acta Neurochirurgica | 69 | 3 |
| Pediatric Neurosurgery | 14 | 3 |
| Child's Nervous System | 36 | 3 |
| Clinical Neurology and Neurosurgery | 32 | 2 |
| Spine Journal | 22 | 2 |
| Journal of Neurosurgery Pediatrics | 22 | 2 |
| Stereotactic and Functional Neurosurgery | 9 | 2 |
| Journal of Neurosurgery Spine | 20 | 2 |
| Surgical Neurology | 14 | 2 |
| European Spine Journal | 60 | 1 |
| British Journal of Neurosurgery | 39 | 1 |
| Pituitary | 8 | 1 |
| Spinal Cord | 63 | 0 |
| Journal of Neurology Neurosurgery and Psychiatry | 41 | 0 |
| Joint Bone Spine | 34 | 0 |
| Neurologia Medico-Chirurgica | 19 | 0 |
| Neurosurgical Review | 11 | 0 |
| Journal of Neurosurgical Sciences | 11 | 0 |
| Neurosurgical Focus | 10 | 0 |
| Surgical Neurology International | 10 | 0 |
| Journal of Neurological Surgery Part B Skull Base | 8 | 0 |
| Journal of Neurological Surgery Part A Central European Neurosurgery | 7 | 0 |
| Journal of Korean Neurosurgical Society | 6 | 0 |
| Neurospine | 3 | 0 |
| Asian Journal of Neurosurgery | 3 | 0 |
| Clinical Neurosurgery | 3 | 0 |
| Total | 921 | 50 |
Using Google Scholar, the citation numbers for all screened articles were documented. In view of the regular changes in the citation numbers, the findings on a single day (15th December 2023) were documented and used for analysis. The 50 most-cited articles were identified and chosen for this review. The selection was limited to surveys published in the neurosurgical journals in which the participants were surgeons, surgical residents or a combination of surgeons and non-surgeons. We excluded studies in which all participants were non-surgeons and articles that did not provide an adequate description of the survey process or other pertinent data. The selected articles are referred to as "most cited", or "most influential", or as "high-impact survey research articles sampling neurosurgeons" interchangeably in this review.
Analysis of Characteristics
Using the full articles, relevant information relating to each of the selected studies was collected by two of the authors independently and any discrepancies were resolved by consensus. Missing data was referred to as not available (NA). The extracted data was grouped into: Articles’ characteristics: publication year, publishing journal, its impact factor (IF), number of authors, number of centres, number of specialties, number of countries and first authors’ countries. The journals' IF data was obtained from an online source [8]. Participants’ characteristics: their number, population (whether individuals, groups, or centres), selection method (whether from affiliation to associations or workgroups, medical meeting attendees, panel of experts or random individuals or hospitals), response rates, specialties, and worldwide regions. Questionnaires’ characteristics: number of items on the questionnaire, subspecialties, categories (whether specific disease management, training and career, surgical complications, or methods and techniques) and the individual topics.
Analysis of Quality
The quality assessment was comparable to others [1-5] and was based on whether several parameters were clearly reported in the articles. These were: study population, sample selection methods, sample size, response rate, incomplete response rate, non-responders characteristics, the full version of the questionnaire, number of items on the questionnaire, and whether the questionnaire was validated or pretested. The quality of reporting of each parameter in ≥ 66% of articles was graded as good, in 34%-65% of articles was graded as fair and in ≤ 33% of articles was graded as poor. The quality grading was determined by two of the authors independently and any discrepancies were resolved by consensus.
Analysis of Citation Predictors
The citation predictors assessment was carried out by correlating the citation numbers for the selected studies with the various article, participant, and questionnaire characteristics. The correlation testing was done by calculating the Pearson correlation coefficient (R) using the Social Sciences Statistics website [9], and significance was determined when p ≤ 0.05. A secondary citation predictors analysis was carried out by comparing the mean citation numbers [± standard deviation (SD)] between the following subgroups: articles’ ages [≥15.5 versus (vs.) <15.5 years], journals’ IF (≥2.82 vs. <2.82), number of authors (>4 vs. ≤4), number of centres (1 vs. >1), number of specialties (1 vs. >1), number of countries (1 vs. >1), first authors’ countries (USA vs. others), participants’ numbers (≥222 vs. <222), participants’ response rates (≥51% vs. <51%), participants’ specialties (general neurosurgeons vs. others), participants’ selections (associations/groups vs. others), participants’ worldwide regions (North America vs. others), questionnaires’ number of items (≥12 vs. <12), questionnaires’ subspecialties (spine vs. others), questionnaires’ categories (management/ training and career/ complications vs. others). The median was taken as a cut-off point in the numerical parameters The statistical analysis was carried out by calculating the mean difference (MD) using the MedCalc website [10]. Significance was determined when p ≤ 0.05.
Results
The 50 most-cited survey research studies sampling neurosurgeons are summarised in Table 2 [11-60].
Table 2. The selected 50 high-impact studies of survey research among neurospine surgeons.
*Respondents only
Abbreviations: NA: not available, Ref: Reference, Particip.: Participants, Neurosurg: Neurosurgery, Neurol: Neurology, Pediatr: Pediatric, Sterotact Funct: Stereotactic and Functional, SSEP: somatosensory evoked potential, SCI: spinal cord injury, s.: spondylotic, ICP: intracranial pressure, MR: magnetic resonance, MCA: middle cerebral artery.
| Rank | 1st Authors Year [Ref] | Journals | Particip. number | Response Rate (%) | Categories | Topics | Cites |
| 1 | Ciric I 1997 [11] | Neurosurgery | 3172 | 82% | Complications | Transsphenoidal surgery | 1345 |
| 2 | Wright N 1998 [12] | Journal of Neurosurgery | 847 | 25% | Complications | Vertebral artery injury during C1-2 fixation | 628 |
| 3 | Dawson E 1991 [13] | Spine | 330 | 74% | Techniques | SSEP during spine surgery | 306 |
| 4 | Neo M 2008 [14] | Spine | 36 groups | 89% | Complications | Vertebral artery injury in cervical spine surgery | 275 |
| 5 | Schijman E 2004 [15] | Child's Nervous System | 246 | 31% | Management | Chiari and syringomyelia | 262 |
| 6 | Härtl R 2013 [16] | World Neurosurgery | 3348 | 20% | Techniques | Navigation in spine surgery | 228 |
| 7 | Sanford R 1994 [17] | Pediatric Neurosurgery | 40 | 28% | Management | Craniopharyngioma | 221 |
| 8 | Haroun R 2000 [18] | Pediatric Neurosurgery | 234 | 33% | Management | Chiari and syringomyelia | 204 |
| 9 | Santarius T 2008 [19] | British Journal of Neurosurgery | 215 | 52% | Management | Chronic subdural hematoma practice survey | 187 |
| 10 | Laitinen L 1985 [20] | Journal of Neurosurgery | 16 | 100% | Management | Parkinson Disease surgical targets | 163 |
| 11 | Krauss J 2004 [21] | Acta Neurochirurgica | 82 | 65% | Management | Normal Pressure Hydrocephalus | 160 |
| 12 | Belzberg A 2004 [22] | Journal of Neurosurgery | 126 | 39% | Management | Brachial plexus injury | 154 |
| 13 | Rocque B 2011 [23] | Journal of Neurosurg Pediatr | 710 | 30% | Management | Chiari and syringomyelia | 143 |
| 14 | Fujibayashi S 2017 [24] | Spine | 583 | 12.3% | Complications | Lateral interbody fusion complications | 136 |
| 15 | Eck J 2006 [25] | Spine | 1322 | 23% | Management | Prednisolone in acute SCI | 135 |
| 16 | Cohen-Gadol A 2005 [26] | Neurosurgery | 710 | 26% | Training & career | Residents duty hours reform | 127 |
| 17 | Dipaola C 2009 [27] | Spine Journal | 133 | 86% | Management | Osteoporosis and osteomalacia | 125 |
| 18 | Whitehead W 2001 [28] | Pediatric Neurosurgery | 129 | 65% | Management | Shunt infections practice survey | 124 |
| 19 | Tamburrini G 2008 [29] | Child's Nervous System | 60 | 75% | Management | Sylvian fissure arachnoid cysts | 123 |
| 20 | McAbee J 2015 [30] | Journal of Neurosurgery | 3247 | 24% | Training & career | Satisfaction among neurosurgeons | 123 |
| 21 | Abosch A 2013 [31] | Sterotact Funct Neurosurgery | 146 | 45% | Techniques | Deep Brain Stimulation procedural steps | 120 |
| 22 | Cheng M 2000 [32] | Neurosurgery | 986 | 40% | Complications | Visual loss after spine surgery | 120 |
| 23 | Giustina A 2011 [33] | Pituitary | 73 | 89% | Management | Acromegaly management practices | 118 |
| 24 | Jhawar B 2007 [34] | Journal of Neurosurg Spine | 138 | 68% | Complications | Wrong side and level in neurosurgery | 118 |
| 25 | Attenello F 2018 [35] | Journal of Neurosurgery | 1643 | 21% | Training & career | Burnout among residents | 112 |
| 26 | Favre J 1996 [36] | Neurosurgery | (28 centres*) | NA | Management | Pallidotomy practice survey | 109 |
| 27 | Ganju A 2013 [37] | World Neurosurgery | 99 | 53.5% | Training & career | Simulation in neurosurgical education | 108 |
| 28 | Auerbach J 2011 [38] | Spine | 904 | 62% | Training & career | Musculoskeletal disorders among spine surgeons | 107 |
| 29 | O'Neill B 2008 [39] | Surgical Neurology | 3100 | 30.4% | Techniques | ICP monitor placement | 104 |
| 30 | Kaufman H 1991 [40] | Surgical Neurology | 2969 | 38% | Management | Care of gunshot wounds to the head | 97 |
| 31 | Steinbok P 2006 [41] | Journal of Neurosurgery | (105)* | NA | Management | Occult tethered cord syndrome | 92 |
| 32 | Uribe J 2015 [42] | European Spine Journal | 77 | 52% | Complications | Lateral interbody fusion complications | 92 |
| 33 | Ondo W 2005 [43] | Sterotact Funct Neurosurgery | 47 | 77% | Techniques | Deep Brain Stimulation placement and adjustment | 87 |
| 34 | Bible J 2009 [44] | Spine Journal | 142 | 83% | Management | Bracing after spine surgery | 86 |
| 35 | Haines S 1991 [45] | Neurosurgery | 152 | 63% | Management | Chiari malformation Types I and II | 86 |
| 36 | Rapport R 2nd 1973 [46] | Journal of Neurosurgery | 1354 | 78.6% | Management | Prophylaxis for posttraumatic epilepsy | 86 |
| 37 | Ghogawala Z 2007 [47] | Spine | 239 | 38% | Management | Ventral vs. dorsal decomp in cervical s. myelopathy | 81 |
| 38 | Ikezaki K 1997 [48] | Clinical Neurol Neurosurg | 2096 | 53% | Management | Haemorrhagic Moyamoya disease | 79 |
| 39 | Rofes A 2017 [49] | Acta Neurochirurgica | 28 centres | 75% | Management | Cognition in low-grade glioma | 76 |
| 40 | Schroeder G 2014 [50] | Spine | (84)* | NA | Management | Methylprednisolone in acute SCI | 75 |
| 41 | Hayashi K 2013 [51] | Clinical Neurol Neurosurg | 2998 | 39.5% | Management | Moyamoya Disease in Japan | 71 |
| 42 | Kshettry V 2014 [52] | World Neurosurg | 100 | 65% | Training & career | Laboratory dissection in neurosurgical residency | 71 |
| 43 | Oi S 1992 [53] | Child's Nervous System | 30 | 50% | Management | Worldwide survey of pineal tumors | 70 |
| 44 | Ratliff J 2009 [54] | Journal of Neurosurg Spine | (229)* | NA | Complications | Spinal surgery complications | 69 |
| 45 | Hankinson T 2011 [55] | Journal of Neurosurg Pediatr | 269 | 32% | Management | MR of diffuse intrinsic pontine glioma | 69 |
| 46 | Fontanella M 2020 [56] | World Neurosurgery | (446)* | NA | Training & career | Effect of Covid on neurosurgical practice | 68 |
| 47 | Suyama K 2014 [57] | World Neurosurgery | 556 | 46.6% | Management | Hemicraniectomy for MCA infarction | 63 |
| 48 | Sakowitz O 2006 [58] | Neurosurgery | 130 centres | 77% | Management | Ruptured intracranial aneurysm in Germany | 64 |
| 49 | Stienen M 2016 [59] | Acta Neurochirurgica | (532)* | NA | Training & career | Quality of resident training in Europe | 62 |
| 50 | Al Khalili K 2014 [60] | World Neurosurgery | 100 | 46% | Training & career | Neurosurgery resident selection | 60 |
The studies’ characteristics were as follows:
Article Characteristics
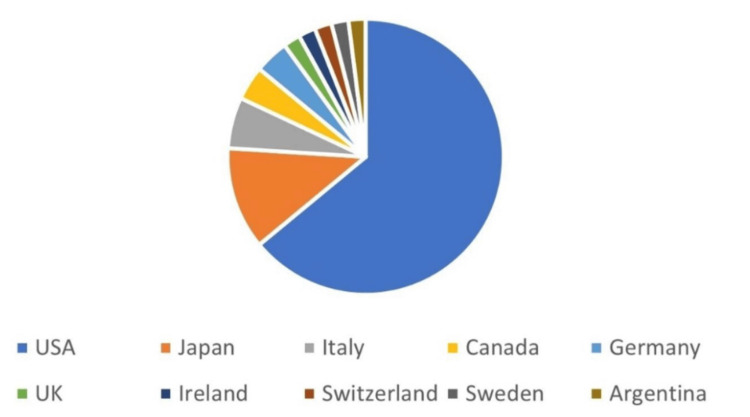
The median (range) publication year and articles’ age were 2007-2008 (1973-2020) and 15.5 (3-50) years respectively. The publishing journals are listed in Table 1. The most common journals were Spine seven (14%), Journal of Neurosurgery seven (14%), World Neurosurgery six (12%), Neurosurgery six (12%), Acta Neurochirurgica three (6%), Pediatric Neurosurgery 3 (6%), and Child's Nervous System three (6%). The median (range) journals’ IF was 2.82 (1.12- 5.41). The median (range) number of authors was four (1- 30). The median (range) number of centres was 1.5 (1- 25). The median (range) number of specialties was one (1-6). The median (range) number of countries was one (1- 9). The distribution of the articles according to the first authors’ countries is shown in Figure 1. These countries were USA: 32 (64%), Japan: six (12%), Italy: three (6%), Canada: teo (4%), Germany: two (4%), UK: one (2%), Ireland: one (2%), Switzerland: one (2%), Sweden: one (2%), and Argentina: one (2%).
Figure 1. The distribution of the 50 high0impact articles according to the first authors’ countries .
Participant Characteristics
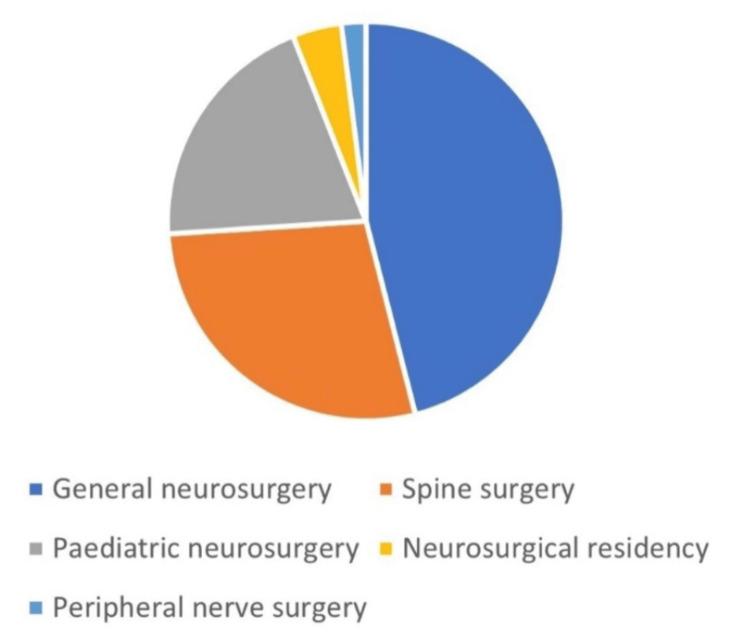
The median (range) number of participants and percentage response rates were 222 (28-3348) and 51% (20%-100%), respectively. The distribution of the articles according to the participants’ specialties is illustrated in Figure 2. These were general neurosurgery: 23 (46%), spine surgery: 14 (28%), paediatric neurosurgery: 10 (20%), neurosurgical residency: two (4%), and peripheral nerve surgery: one (2%).
Figure 2. The distribution of the 50 high-impact articles according to the participants’ specialties.
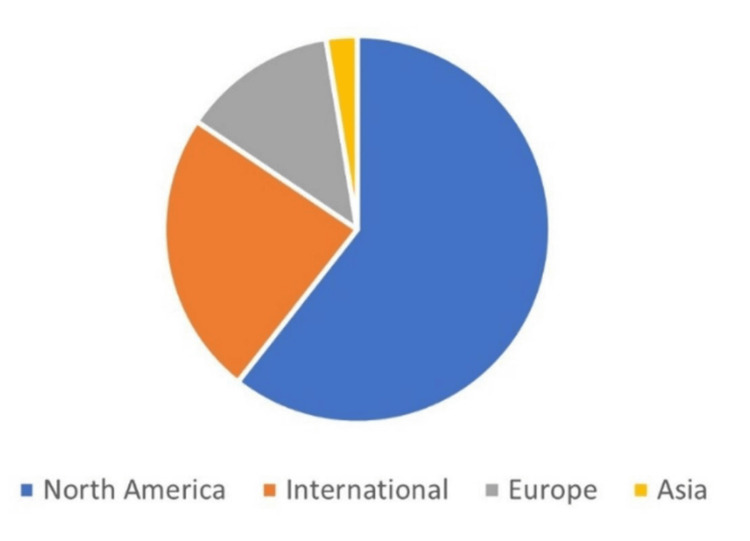
The distribution of the articles according to the participants’ worldwide regions is shown in Figure 3. These were North America: 28 (56%), International: 11 (22%), Europe: six (12%), and Asia: five (10%).
Figure 3. The distribution of the 50 high-impact articles according to the participants’ worldwide regions.
Questionnaire Characteristics
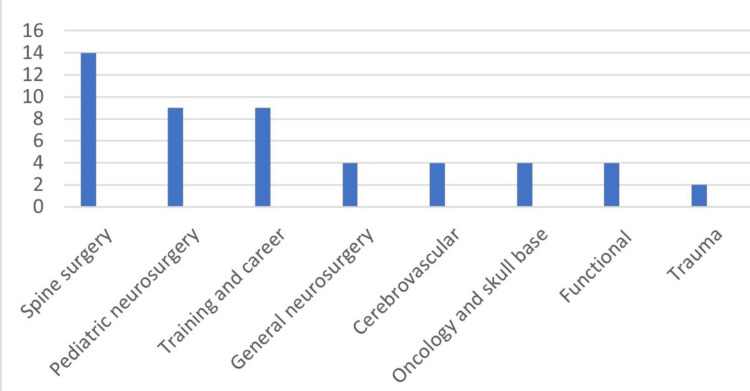
The median (range) number of items on the survey questionnaires was 12 (2- 86). The distribution of the articles according to the questionnaires’ subspecialties is illustrated in Figure 4. These were spine surgery: 14 (28%), paediatric neurosurgery: nine (18%), training and career: nine (18%), general neurosurgery: four (8%), cerebrovascular: four (8%), oncology and skull base: four (8%), functional: four (8%), and trauma: two (4%).
Figure 4. The distribution of the 50 high-impact articles according to the surveys’ subspecialties.
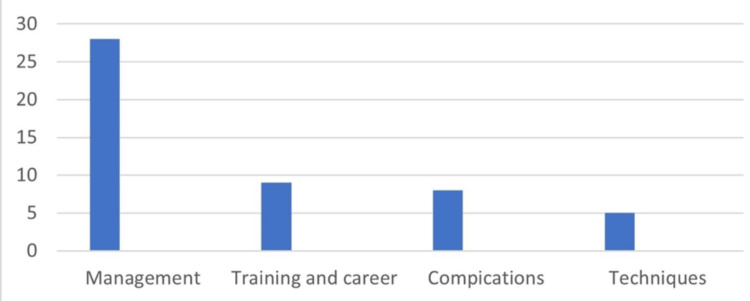
The distribution of the articles according to the questionnaires’ categories is shown in Figure 5. These were specific disease management: 28 (56%), training and career: nine (18%), surgical complications: eight (16%), and methods and techniques: five (10%).
Figure 5. The distribution of the 50 high impact articles according to the surveys’ categories.
The most common survey topics among the 50 most-cited articles were residency training-related matters (five articles). These were duty hours reform [26], burnout and career dissatisfaction [35], the role of laboratory dissection in residency training [52], quality of residency training [59], and the residency selection process [60]. The other common topics were Chiari and syringomyelia (four articles) [15,18,23,45], the use of prednisolone in spinal cord injury (two articles) [25, 50], vertebral artery injury in cervical spine surgery (two articles) [12, 14], deep brain stimulation procedures (two articles) [31,43], complications of lateral interbody fusion (two articles) [24, 42], and Moyamoya disease (two articles) [48,51]. A full list of the topics is shown in Table 2.
Study Quality
The quality of reporting of the study population and sample selection methods was considered good, documented in 50 (100%) articles. The participants were individuals in 46 (92%) articles and centres or groups in four (8%) articles [14,36,49,58]. They were selected from associations (and working groups) in 27 (54%) articles [12,13,15-19,23-25,28,30,32, 33,35, 38,41,42,45,47-50,52-56], from random individuals or hospitals in 17 (34%) articles [11,14,21,22,26,29,34,37,39,40,46,51,54, 57-60], from meeting attendees in three (6%) articles [27,36,44], and from a panel of experts in three (6%) articles [20,31,43]. The quality of reporting of the sample size and response rates was considered good, documented in 44 (88%) articles. Six (12%) articles [36,41,50,54,56,59] reported the numbers of responders only and were not included in the calculations of the total number of participants or the response rates. The quality of reporting of the questionnaires’ number of items was considered good, documented in all articles but three [13,48,51]. The quality of reporting of the full version of the questionnaire was considered fair, documented in 18 (36%) articles [16,21,23,27,30,32, 33,35,37,42,43,45,46, 49,50, 52,55,60]. The quality of reporting of the following data was considered poor: the non-respondents characteristics, documented in two (4%) articles [19,47], the incomplete response rates (not documented in any article), the questionnaires’ validation, documented in four (8%) articles [30,34,35, 38], and the questionnaires’ pretesting, documented in one (2%) article [40]. The overall quality of reporting of the surveys was considered fair (based on good grading in five parameters, fair grading in one parameter, and poor grading in four parameters).
Study Citation Predictors
The median (range) and mean (±SD) article citation numbers were 110.5 (60- 1345) and 155.8 (± 194.6) cites, respectively. Table 3 and Table 4 summarize the correlation and secondary analysis findings between the citation numbers and the various characteristics of the selected articles. The correlation analysis showed a significant association between citation numbers and participant number (p=0.0261). The secondary analysis demonstrated significantly higher mean citation numbers in articles aged ≥15.5 years (p=0.0236) and studies in which the surveys' categories were complications-related (P=0.0016). None of the other parameters, in particular the response rates and the journals IF, reached significance
Table 3. Summary of the primary analysis correlation findings between the citation numbers and the various characteristics for the 50 most-cited survey research publications in the neurosurgical literature.
| Features | R-Value | P-Value |
| Articles’ age in years | 0.2255 | 0.1154 |
| Articles’ publishing journals | 0.1762 | 0.2209 |
| Articles’ journals IF | 0.2265 | 0.1137 |
| Articles’ number of Authors | 0.1436 | 0.3198 |
| Articles’ number of centres | 0.12 | 0.4065 |
| Articles’ number of specialties | 0.0878 | 0.5443 |
| Articles’ number of countries | 0.0913 | 0.5283 |
| Articles’ first author’s countries | 0.0548 | 0.7054 |
| Participants’ numbers | 0.3146 | 0.0261* |
| Participants’ response rates | 0.0984 | 0.5351 |
| Participants’ specialties | 0.031 | 0.8308 |
| Participants’ selection | 0.0046 | 0.9747 |
| Participants’ worldwide regions | 0.1064 | 0.4621 |
| Questionnaires’ number of items | 0.1128 | 0.4503 |
| Questionnaires’ subspecialties | 0.0185 | 0.8985 |
| Questionnaires’ categories | 0.2705 | 0.0574 |
Table 4. Summary of the secondary analysis mean difference findings between the citation numbers and the various characteristics for the 50 most-cited survey research publications in the neurosurgical literature.
*Denotes significance
| Feature | Variables | Number | Mean Citation Numbers (±SD) | Mean Difference | P-value |
| Articles’ age (years) | ≥15.5 | 25 | 199.8(±265.5) | 88 | 0.0236* |
| <15.5 | 25 | 111.8(±52.8) | |||
| Articles’ journals impact factor | ≥2.82 | 26 | 190.4(±261.5) | 54.7 | 0.1935 |
| <2.82 | 24 | 118.3(±59.2) | |||
| Articles’ number of Authors | >4 | 24 | 110.8(±54.3) | 78.5 | 0.1544 |
| ≤4 | 26 | 197.3(±260.4) | |||
| Articles’ number of centres | 1 | 25 | 200(±266.4) | 89.3 | 0.1053 |
| >1 | 25 | 111.3(±46.9) | |||
| Articles’ number of specialties | 1 | 40 | 162.9(±214.6) | 35.7 | 0.609 |
| >1 | 10 | 127.2(±74.6) | |||
| Articles’ number of countries | 1 | 41 | 163.1(±212.2) | 40.8 | 0.5743 |
| >1 | 9 | 122.3(±73) | |||
| Articles’ first authors countries | USA | 32 | 175.1(±237.5) | 53.6 | 0.3552 |
| Others | 18 | 121.5(±66) | |||
| Participants’ numbers | ≥222 | 22 | 210.3(±281.8) | 87.9 | 0.1581 |
| <222 | 22 | 122.4(±53.8) | |||
| Participants’ response rates | ≥51% | 20 | 191.8(±278.6) | 46.9 | 0.4572 |
| <51% | 24 | 144.9(±117.1) | |||
| Participants’ specialties | General neurosurgery | 23 | 153.9(±262) | 3.500 | 0.9502 |
| Others | 27 | 157.4(±115.3) | |||
| Participants’ selection | Associations/Groups | 27 | 151.3(±116.7) | 9.3 | 0.8664 |
| Others | 23 | 160.6(±256.6) | |||
| Participants’ worldwide regions | North America | 28 | 172.4(±252.4) | 37.7 | 0.5022 |
| Others | 22 | 134.7(±75) | |||
| Questionnaires’ number of items | ≥12 | 25 | 169.6(±251) | 29 | 0.6232 |
| <12 | 22 | 140.6(±119.1) | |||
| Questionnaires’ subspecialties | Spine surgery | 14 | 175.9(±150.2) | 28 | 0.6526 |
| Others | 36 | 147.9(±210.8) | |||
| Questionnaires’ categories | Management | 28 | 118.7(±52.1) | 84.3 | 0.1297 |
| Others | 22 | 203(±284.1) | |||
| Training and career | 9 | 93(±27.4) | 76.4 | 0.2908 | |
| Others | 41 | 169.5(±212.4.5) | |||
| Complications | 8 | 347.9(±442.5) | 228.7 | 0.0016* | |
| Others | 42 | 119.2(±57) |
Discussion
Surveys are popular among clinical researchers, including neurosurgeons. The challenges of planning, designing, and implementing questionnaire surveys are often underestimated. A good survey requires an important topic, an appropriate sample size, an acceptable tool, a good response rate, precise results, and conclusions consistent with findings [61]. A quality survey should have the smallest possible number of high-quality essential items that will interest the population. It should also provide reproducible results (reliable) and measure what it is supposed to measure (valid) [61]. Surveys can be problematic as ensuring impartial, voluntary participation is not always easy. A large questionnaire with many nondirected questions not only deters potential respondents but also makes it difficult to evaluate validity [61]. Badgering respondents is quite likely to provoke an untruthful response, simply to meet an obligation. The participants’ responses to the questions can fluctuate due to multiple confounding reasons. The questions may be leading, unclear, or display an inherent bias of the researcher [62,63]. Surveys within small communities come with added validity drawbacks. Unlike patient or public surveys that are normally anonymous, surveys among colleagues mean that the respondents and researchers are known to each other and some responses may occur simply with the aim of pleasing the researcher rather than through a true intention to participate [62,63]. All survey measures, whether quantitative or qualitative, are subject to error. The four most common areas of survey errors are coverage (selected sample is different from the surveyed population), sampling (sample size miscalculated or not truly random), measurement (answer is inaccurate or imprecise due to poor question), and non-response (responders are different for the non-responders on the question of interest) [62,63].
Over the last decade, numerous articles reviewed survey research publications from the perspectives of several specialties. These included dentistry [2], nephrology [3], anaesthesia [4], pharmacy [5], radiology [64], critical care [65], colorectal surgery [66] and plastic surgery [67]. The number of articles evaluated in this review (50) is within the range (38-199) of articles reviewed in these studies [2-5,64-67]. Our selected articles were published over 48 years (1973-2020), which is much longer than the 1-to-21-year period covered by the other reviews [2-5,64-67]. Most of our articles were relatively old (median age 15.5 years) which may account for the deficient reporting of certain aspects of data. Our articles were published in journals with a fairly good IF (median 2.82) which is similar to others [4,66]. The majority of our surveys (56%) were carried out in North America which is within the range of 41% to 59% stated by others [2-4,65]. The reporting of the research question, study population and sample selection was considered good in all articles which is in agreement with others [2,5,64]. The majority of participants (54%) were members of associations or groups which is not surprising as it is common for surveys to sample readily available groups (convenience sampling) [3,65]. Some reviewers may have applied stricter criteria and indicated that survey reporting was weak in the description of the study population in 24% [2], the eligibility criteria for the participants in 35% [3] and the characteristics of the respondents in 10% [3].
The sample size was documented in 88% of our articles which is at the upper limit of the range of 53%-88% stated for the reporting of the sample size by other reviews [2,5]. The median response rate was 51% which is within the range of 37%-66% recorded by others [4,64]. None of our articles mentioned whether there were incomplete responses. It has been observed that the reporting of missing data in survey research has improved over the years [3]. Nevertheless, it remains a weak spot that was addressed in only 1.3% to 27% of surveys [1,2,4,5,65]. Only 4% of our articles provided data relating to the characteristics of the non-respondents. Reporting descriptions of the non-respondents is another weak point in survey research that was tackled in only 7% to 11% of studies [2,4,5]. None of our articles reported the use of incentives or reminders. Incentives were used in 7% to 30% of studies [2-5] while reminders were used in 43% to 73% of surveys [3,4,65]. A recent study however concluded that the use of reminders was not associated with higher response rates [4].
The full version of the questionnaire was provided in 36% of our articles which is within the range of 13% to 61% stated in the literature [2,5,65,67]. Only 8% of studies reported that the questionnaires were validated. In the literature, the use of validated instruments has been reported in 19% to 63% of surveys [1-5,64] while the use of previously published questionnaires was reported in 7%-50% of studies [2,5,65]. Only 2% of our articles reported that the questionnaires were pretested which is relatively low compared to the range 26%-76% mentioned by others [2,4,64,65]. The majority of questionnaires in our articles were disease-specific-management-related (56%), which is in agreement with others [3, 65]. Some authors reported that the majority of the questionnaires were current practice [66], opinion-related [67], or education [64]. This could be related to differences in the categorization of the focus of the survey between the various reports.
The median citation number for the 50 most-cited survey research studies among neurosurgeons was 111 cites. This was lower than the citation number for higher levels of evidence research studies such as the top 100 glioblastoma trials (median 349 citations) [7]. Variation in citation rates according to study design and subject is well recognized in the literature [68-70]. We found that the number of participants and the age of the publication (≥15.5) were significant predictors of citation numbers. We also observed that a research question related to specific complications in a survey was also a positive predictor of citation rates. This supports the observation that the novel data or the questions raised in the survey are an important predictor of citations [4]. In this review and comparable to others, we did not establish a positive link between citation rates and the participants’ response rates [4] or the publishing journal's IF [5]. Furthermore, none of the other parameters tested in this review affected citations. These were the number of authors, centers, specialities, countries, and the first author's country, participants’ specialty, participants’ selection, participants’ worldwide regions, surveys’ number of items, and survey subspecialties.
Limitations
There are several limitations to this study which include the general limitations of bibliometric studies. The study relied on the precision of online search engines PubMed and Google Scholar. The review did not include survey research studies among neurosurgeons that were published outside the neurosurgical literature. The presence of a good number of neurosurgical journals in one country (USA) could be a possible source of bias in both publications and citations depending on the degree of network between authors, reviewers and editors within that country. The selection of the 50 most-cited studies was based on their total citations at a certain point which was likely to change relatively quickly. This could have influenced the inclusion or exclusion of a few of the lower-impact surveys. The wide duration from publication may have affected the citations of older studies. The changing trends in the reporting of surveys over the years were not addressed. There may have been errors in the data collection. There may have been discrepancies in the grouping of articles into the various categories. The quality assessment may have not been comprehensive. Not providing the full version of the questionnaire may have been due to editorial restrictions. The review did not look at mode of administration of the questionnaires. Defining the specialty and affiliation based on the first author may not reflect all authors of multi-disciplinary papers. The impact of articles using the Altmetric score of news media and social media mentions was not done.
Conclusions
High-impact survey publications in the neurosurgical literature were relatively old, moderately cited, and of fair quality. The majority of articles were first authored by researchers from the USA and focussed on specific disease management. Their citation numbers were not affected by response rates but were positively influenced by the publication's age, number of participants, and novel data or the questions raised in the survey category. Surveys are valuable forms of research that require extensive planning, time, and effort in order to produce meaningful results. Increasing awareness of the factors that could affect citations may be useful to those who wish to undertake survey research.
Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Abdulhakim B. Jamjoom, Abdulhadi Y. Gahtani, Moajeb T. AlZahrani
Acquisition, analysis, or interpretation of data: Abdulhakim B. Jamjoom, Abdulhadi Y. Gahtani, Jude M. Jamjoom, Belal M. Sharab, Omar M. Jamjoom
Drafting of the manuscript: Abdulhakim B. Jamjoom, Jude M. Jamjoom, Belal M. Sharab, Omar M. Jamjoom
Critical review of the manuscript for important intellectual content: Abdulhakim B. Jamjoom, Abdulhadi Y. Gahtani, Moajeb T. AlZahrani
Supervision: Abdulhakim B. Jamjoom
References
- 1.Reporting guidelines for survey research: an analysis of published guidance and reporting practices. Bennett C, Khangura S, Brehaut JC, Graham ID, Moher D, Potter BK, Grimshaw JM. PLoS Med. 2010;8:0. doi: 10.1371/journal.pmed.1001069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quality of survey-based study reports in dentistry. Mattos-Vela MA, Evaristo-Chiyong TA, Siquero-Vera K. BMC Oral Health. 2023;23:320. doi: 10.1186/s12903-023-02979-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quality of survey reporting in nephrology journals: a methodologic review. Li AH, Thomas SM, Farag A, Duffett M, Garg AX, Naylor KL. Clin J Am Soc Nephrol. 2014;9:2089–2094. doi: 10.2215/CJN.02130214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quality and impact of survey research among anesthesiologists: a systematic review. Geyer ED, Miller R, Kim SS, Tobias JD, Nafiu OO, Tumin D. Adv Med Educ Pract. 2020;11:587–599. doi: 10.2147/AMEP.S259908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reporting quality of survey research articles published in the pharmacy literature. Rybakov KN, Beckett R, Dilley I, Sheehan AH. Res Social Adm Pharm. 2020;16:1354–1358. doi: 10.1016/j.sapharm.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Predictors of citation rates for research publications in Neurosciences. Jamjoom HZ, Gahtani AY, Jamjoom AB. Neurosciences (Riyadh) 2022;27:116–120. doi: 10.17712/nsj.2022.2.20210145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Predictors of citation rates in high-impact glioblastoma clinical trials. Jamjoom AM, Gahtani AY, Jamjoom AB. Cureus. 2021;13:0. doi: 10.7759/cureus.19229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bioxbio Journal Impact website. . [ Dec; 2023 ]. 2022. https://www.bioxbio.com/journal https://www.bioxbio.com/journal
- 9.Social sciences statistics website. . [ Dec; 2023 ]. 2021. https://www.socscistatistics.com https://www.socscistatistics.com
- 10.MedCalc web site. [ Dec; 2023 ]. 2021. https:// www. medcalc.org https:// www. medcalc.org
- 11.Complications of transsphenoidal surgery: results of a national survey, review of the literature, and personal experience. Ciric I, Ragin A, Baumgartner C, Pierce D. Neurosurgery. 1997;40:225–236. doi: 10.1097/00006123-199702000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Vertebral artery injury in C1-2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. Wright NM, Lauryssen C. J Neurosurg. 1998;88:634–640. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]
- 13.Spinal cord monitoring. Results of the Scoliosis Research Society and the European Spinal Deformity Society survey. Dawson EG, Sherman JE, Kanim LE, Nuwer MR. https://pubmed.ncbi.nlm.nih.gov/1785088/ Spine (Phila Pa 1976) 1991;16:0–4. [PubMed] [Google Scholar]
- 14.Vertebral artery injury during cervical spine surgery: a survey of more than 5600 operations. Neo M, Fujibayashi S, Miyata M, Takemoto M, Nakamura T. Spine (Phila Pa 1976) 2008;33:779–785. doi: 10.1097/BRS.0b013e31816957a7. [DOI] [PubMed] [Google Scholar]
- 15.International survey on the management of Chiari I malformation and syringomyelia. Schijman E, Steinbok P. Childs Nerv Syst. 2004;20:341–348. doi: 10.1007/s00381-003-0882-2. [DOI] [PubMed] [Google Scholar]
- 16.Worldwide survey on the use of navigation in spine surgery. Härtl R, Lam KS, Wang J, Korge A, Kandziora F, Audigé L. World Neurosurg. 2013;79:162–172. doi: 10.1016/j.wneu.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Craniopharyngioma: results of survey of the American Society of Pediatric Neurosurgery. Sanford RA. Pediatr Neurosurg. 1994;21 Suppl 1:39–43. doi: 10.1159/000120860. [DOI] [PubMed] [Google Scholar]
- 18.Current opinions for the treatment of syringomyelia and chiari malformations: survey of the Pediatric Section of the American Association of Neurological Surgeons. Haroun RI, Guarnieri M, Meadow JJ, Kraut M, Carson BS. Pediatr Neurosurg. 2000;33:311–317. doi: 10.1159/000055977. [DOI] [PubMed] [Google Scholar]
- 19.The management of primary chronic subdural haematoma: a questionnaire survey of practice in the United Kingdom and the Republic of Ireland. Santarius T, Lawton R, Kirkpatrick PJ, Hutchinson PJ. Br J Neurosurg. 2008;22:529–534. doi: 10.1080/02688690802195381. [DOI] [PubMed] [Google Scholar]
- 20.Brain targets in surgery for Parkinson's disease. Results of a survey of neurosurgeons. Laitinen LV. J Neurosurg. 1985;62:349–351. doi: 10.3171/jns.1985.62.3.0349. [DOI] [PubMed] [Google Scholar]
- 21.Normal pressure hydrocephalus: survey on contemporary diagnostic algorithms and therapeutic decision-making in clinical practice. Krauss JK, Halve B. Acta Neurochir (Wien) 2004;146:379–388. doi: 10.1007/s00701-004-0234-3. [DOI] [PubMed] [Google Scholar]
- 22.Surgical repair of brachial plexus injury: a multinational survey of experienced peripheral nerve surgeons. Belzberg AJ, Dorsi MJ, Storm PB, Moriarity JL. J Neurosurg. 2004;101:365–376. doi: 10.3171/jns.2004.101.3.0365. [DOI] [PubMed] [Google Scholar]
- 23.Treatment practices for Chiari malformation type I with syringomyelia: results of a survey of the American Society of Pediatric Neurosurgeons. Rocque BG, George TM, Kestle J, Iskandar BJ. J Neurosurg Pediatr. 2011;8:430–437. doi: 10.3171/2011.8.PEDS10427. [DOI] [PubMed] [Google Scholar]
- 24.Complications associated with lateral interbody fusion: nationwide survey of 2998 cases during the first 2 years of its use in Japan. Fujibayashi S, Kawakami N, Asazuma T, et al. Spine (Phila Pa 1976) 2017;42:1478–1484. doi: 10.1097/BRS.0000000000002139. [DOI] [PubMed] [Google Scholar]
- 25.Questionnaire survey of spine surgeons on the use of methylprednisolone for acute spinal cord injury. Eck JC, Nachtigall D, Humphreys SC, Hodges SD. Spine (Phila Pa 1976) 2006;31:0–3. doi: 10.1097/01.brs.0000214886.21265.8c. [DOI] [PubMed] [Google Scholar]
- 26.Resident duty hours reform: results of a national survey of the program directors and residents in neurosurgery training programs. Cohen-Gadol AA, Piepgras DG, Krishnamurthy S, Fessler RD. Neurosurgery. 2005;56:398–403. doi: 10.1227/01.neu.0000147999.64356.57. [DOI] [PubMed] [Google Scholar]
- 27.Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Dipaola CP, Bible JE, Biswas D, Dipaola M, Grauer JN, Rechtine GR. Spine J. 2009;9:537–544. doi: 10.1016/j.spinee.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 28.The treatment of cerebrospinal fluid shunt infections. Results from a practice survey of the American Society of Pediatric Neurosurgeons. Whitehead WE, Kestle JR. Pediatr Neurosurg. 2001;35:205–210. doi: 10.1159/000050422. [DOI] [PubMed] [Google Scholar]
- 29.Sylvian fissure arachnoid cysts: a survey on their diagnostic workout and practical management. Tamburrini G, Dal Fabbro M, Di Rocco C. Childs Nerv Syst. 2008;24:593–604. doi: 10.1007/s00381-008-0585-9. [DOI] [PubMed] [Google Scholar]
- 30.Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. McAbee JH, Ragel BT, McCartney S, et al. J Neurosurg. 2015;123:161–173. doi: 10.3171/2014.12.JNS141348. [DOI] [PubMed] [Google Scholar]
- 31.An international survey of deep brain stimulation procedural steps. Abosch A, Timmermann L, Bartley S, et al. Stereotact Funct Neurosurg. 2013;91:1–11. doi: 10.1159/000343207. [DOI] [PubMed] [Google Scholar]
- 32.Visual loss after spine surgery: a survey. Cheng MA, Sigurdson W, Tempelhoff R, Lauryssen C. Neurosurgery. 2000;46:625–630. doi: 10.1097/00006123-200003000-00020. [DOI] [PubMed] [Google Scholar]
- 33.Current management practices for acromegaly: an international survey. Giustina A, Bronstein MD, Casanueva FF, et al. Pituitary. 2011;14:125–133. doi: 10.1007/s11102-010-0269-9. [DOI] [PubMed] [Google Scholar]
- 34.Wrong-sided and wrong-level neurosurgery: a national survey. Jhawar BS, Mitsis D, Duggal N. J Neurosurg Spine. 2007;7:467–472. doi: 10.3171/SPI-07/11/467. [DOI] [PubMed] [Google Scholar]
- 35.Factors associated with burnout among US neurosurgery residents: a nationwide survey. Attenello FJ, Buchanan IA, Wen T, et al. J Neurosurg. 2018;129:1349–1363. doi: 10.3171/2017.9.JNS17996. [DOI] [PubMed] [Google Scholar]
- 36.Pallidotomy: a survey of current practice in North America. Favre J, Taha JM, Nguyen TT, Gildenberg PL, Burchiel KJ. Neurosurgery. 1996;39:883–890. doi: 10.1097/00006123-199610000-00060. [DOI] [PubMed] [Google Scholar]
- 37.The role of simulation in neurosurgical education: a survey of 99 United States neurosurgery program directors. Ganju A, Aoun SG, Daou MR, et al. World Neurosurg. 2013;80:0–8. doi: 10.1016/j.wneu.2012.11.066. [DOI] [PubMed] [Google Scholar]
- 38.Musculoskeletal disorders among spine surgeons: results of a survey of the Scoliosis Research Society membership. Auerbach JD, Weidner ZD, Milby AH, Diab M, Lonner BS. Spine (Phila Pa 1976) 2011;36:0–21. doi: 10.1097/BRS.0b013e31821cd140. [DOI] [PubMed] [Google Scholar]
- 39.A survey of ventriculostomy and intracranial pressure monitor placement practices. O'Neill BR, Velez DA, Braxton EE, Whiting D, Oh MY. Surg Neurol. 2008;70:268–273. doi: 10.1016/j.surneu.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 40.A national survey of neurosurgical care for penetrating head injury. Kaufman HH, Schwab K, Salazar AM. Surg Neurol. 1991;36:370–377. doi: 10.1016/0090-3019(91)90026-6. [DOI] [PubMed] [Google Scholar]
- 41.Occult tethered cord syndrome: a survey of practice patterns. Steinbok P, Garton HJ, Gupta N. J Neurosurg. 2006;104:309–313. doi: 10.3171/ped.2006.104.5.309. [DOI] [PubMed] [Google Scholar]
- 42.Visceral, vascular, and wound complications following over 13,000 lateral interbody fusions: a survey study and literature review. Uribe JS, Deukmedjian AR. Eur Spine J. 2015;24 Suppl 3:386–396. doi: 10.1007/s00586-015-3806-4. [DOI] [PubMed] [Google Scholar]
- 43.The North American survey of placement and adjustment strategies for deep brain stimulation. Ondo WG, Bronte-Stewart H. Stereotact Funct Neurosurg. 2005;83:142–147. doi: 10.1159/000088654. [DOI] [PubMed] [Google Scholar]
- 44.Postoperative bracing after spine surgery for degenerative conditions: a questionnaire study. Bible JE, Biswas D, Whang PG, Simpson AK, Rechtine GR, Grauer JN. Spine J. 2009;9:309–316. doi: 10.1016/j.spinee.2008.06.453. [DOI] [PubMed] [Google Scholar]
- 45.Current treatment of Chiari malformations types I and II: a survey of the Pediatric Section of the American Association of Neurological Surgeons. Haines SJ, Berger M. https://pubmed.ncbi.nlm.nih.gov/2011216/ Neurosurgery. 1991;28:353–357. [PubMed] [Google Scholar]
- 46.A survey of attitudes toward the pharmacological prophylaxis of posttraumatic epilepsy. Rapport RL 2nd, Penry JK. J Neurosurg. 1973;38:159–166. doi: 10.3171/jns.1973.38.2.0159. [DOI] [PubMed] [Google Scholar]
- 47.Ventral versus dorsal decompression for cervical spondylotic myelopathy: surgeons' assessment of eligibility for randomization in a proposed randomized controlled trial: results of a survey of the Cervical Spine Research Society. Ghogawala Z, Coumans JV, Benzel EC, Stabile LM, Barker FG 2nd. Spine (Phila Pa 1976) 2007;32:429–436. doi: 10.1097/01.brs.0000255068.94058.8a. [DOI] [PubMed] [Google Scholar]
- 48.The current status of the treatment for hemorrhagic type moyamoya disease based on a 1995 nationwide survey in Japan. Ikezaki K, Fukui M, Inamura T, Kinukawa N, Wakai K, Ono Y. Clin Neurol Neurosurg. 1997;99:183–186. doi: 10.1016/s0303-8467(97)00077-2. [DOI] [PubMed] [Google Scholar]
- 49.Survey on current cognitive practices within the European Low-Grade Glioma Network: towards a European assessment protocol. Rofes A, Mandonnet E, Godden J, et al. Acta Neurochir (Wien) 2017;159:1167–1178. doi: 10.1007/s00701-017-3192-2. [DOI] [PubMed] [Google Scholar]
- 50.Survey of Cervical Spine Research Society members on the use of high-dose steroids for acute spinal cord injuries. Schroeder GD, Kwon BK, Eck JC, Savage JW, Hsu WK, Patel AA. Spine (Phila Pa 1976) 2014;39:971–977. doi: 10.1097/BRS.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 51.An epidemiological survey of moyamoya disease, unilateral moyamoya disease and quasi-moyamoya disease in Japan. Hayashi K, Horie N, Suyama K, Nagata I. Clin Neurol Neurosurg. 2013;115:930–933. doi: 10.1016/j.clineuro.2012.09.020. [DOI] [PubMed] [Google Scholar]
- 52.The role of laboratory dissection training in neurosurgical residency: results of a national survey. Kshettry VR, Mullin JP, Schlenk R, Recinos PF, Benzel EC. World Neurosurg. 2014;82:554–559. doi: 10.1016/j.wneu.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 53.Controversy pertaining to therapeutic modalities for tumors of the pineal region: a worldwide survey of different patient populations. Oi S, Matsumoto S. Childs Nerv Syst. 1992;8:332–336. doi: 10.1007/BF00296564. [DOI] [PubMed] [Google Scholar]
- 54.Complications in spinal surgery: comparative survey of spine surgeons and patients who underwent spinal surgery. Ratliff JK, Lebude B, Albert T, et al. J Neurosurg Spine. 2009;10:578–584. doi: 10.3171/2009.2.SPINE0935. [DOI] [PubMed] [Google Scholar]
- 55.Interpretation of magnetic resonance images in diffuse intrinsic pontine glioma: a survey of pediatric neurosurgeons. Hankinson TC, Campagna EJ, Foreman NK, Handler MH. J Neurosurg Pediatr. 2011;8:97–102. doi: 10.3171/2011.4.PEDS1180. [DOI] [PubMed] [Google Scholar]
- 56.Neurosurgical practice during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic: a worldwide survey. Fontanella MM, De Maria L, Zanin L, et al. World Neurosurg. 2020;139:0–26. doi: 10.1016/j.wneu.2020.04.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nationwide survey of decompressive hemicraniectomy for malignant middle cerebral artery infarction in Japan. Suyama K, Horie N, Hayashi K, Nagata I. World Neurosurg. 2014;82:1158–1163. doi: 10.1016/j.wneu.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 58.Contemporary management of aneurysmal subarachnoid hemorrhage in germany: results of a survey among 100 neurosurgical departments. Sakowitz OW, Raabe A, Vucak D, Kiening KL, Unterberg AW. Neurosurgery. 2006;58:137–145. doi: 10.1227/01.neu.0000194532.47239.7c. [DOI] [PubMed] [Google Scholar]
- 59.Neurosurgical resident education in Europe--results of a multinational survey. Stienen MN, Netuka D, Demetriades AK, et al. Acta Neurochir (Wien) 2016;158:3–15. doi: 10.1007/s00701-015-2632-0. [DOI] [PubMed] [Google Scholar]
- 60.Programs selection criteria for neurological surgery applicants in the United States: a national survey for neurological surgery program directors. Al Khalili K, Chalouhi N, Tjoumakaris S, Gonzalez LF, Starke RM, Rosenwasser R, Jabbour P. World Neurosurg. 2014;81:473–477. doi: 10.1016/j.wneu.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 61.Survey research. Story DA, Tait AR. Anesthesiology. 2019;130:192–202. doi: 10.1097/ALN.0000000000002436. [DOI] [PubMed] [Google Scholar]
- 62.Understanding and evaluating survey research. Ponto J. https://pubmed.ncbi.nlm.nih.gov/26649250/ J Adv Pract Oncol. 2015;6:168–171. [PMC free article] [PubMed] [Google Scholar]
- 63.Questionnaire surveys - sources of error and implications for design, reporting and appraisal. Shelley A, Horner K. Br Dent J. 2021;230:251–258. doi: 10.1038/s41415-021-2654-3. [DOI] [PubMed] [Google Scholar]
- 64.Survey research reporting in radiology publications: a review of 2017 to 2018. Shankar PR, Maturen KE. J Am Coll Radiol. 2019;16:1378–1384. doi: 10.1016/j.jacr.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 65.Quality of reporting of surveys in critical care journals: a methodologic review. Duffett M, Burns KE, Adhikari NK, et al. Crit Care Med. 2012;40:441–449. doi: 10.1097/CCM.0b013e318232d6c6. [DOI] [PubMed] [Google Scholar]
- 66.The benefits of colorectal surgery surveys in Australia and New Zealand. Ricardo Hamilton AE, Lin AA, Young CJ. Ann Coloproctol. 2020;36:102–111. doi: 10.3393/ac.2019.09.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Critical assessment of surveys in plastic and reconstructive surgery: a systematic review. Chung WH, Gudal RA, Nasser JS, Chung KC. Plast Reconstr Surg. 2019;144:912–922. doi: 10.1097/PRS.0000000000006101. [DOI] [PubMed] [Google Scholar]
- 68.Factors affecting number of citations: a comprehensive review of the literature. Tahamtan I, Safipour Afshar A, Ahamdzadehn K. Scientometrics. 2016;107:1195–1225. [Google Scholar]
- 69.Predictors of citations in neurosurgical research. Oravec CS, Frey CD, Berwick BW, Vilella L, Aschenbrenner CA, Wolfe SQ, Fargen KM. World Neurosurg. 2019;130:0–9. doi: 10.1016/j.wneu.2019.05.226. [DOI] [PubMed] [Google Scholar]
- 70.Predictors of citation rate in the spine literature. Yom KH, Jenkins NW, Parrish JM, et al. Clin Spine Surg. 2020;33:76–81. doi: 10.1097/BSD.0000000000000921. [DOI] [PubMed] [Google Scholar]