Abstract
Introduction
Throughout their academic pursuits, students may encounter various sleep-related issues, including insomnia, sleep apnea, hypersomnia, or sleep terror disorder. These disorders can profoundly impact their well-being, emotional state, and academic achievements.
Objective
This study, of significant relevance to the field of nursing and sleep disorders, aimed to investigate the prevalence of sleep disorders and their impact on academic performance among undergraduate nursing students in the United Arab Emirates.
Methods
A cross-sectional research method was implemented among 177 undergraduate nursing students. Two tools were used: Too I consisted of two parts: sociodemographic and academic performance classifications, whereas Tool II comprised the SLEEP-50 questionnaire.
Results
Our findings revealed that 30.6% of nursing students had one or more sleep disorders. Insomnia was the most prevalent among the nursing students (37.5%), followed by circadian rhythm (33.3%), narcolepsy (26.6%), sleep apnea and restless leg syndrome (25%), nightmares (22.2%), and sleepwalking (11.11%). There was a significant relation between restless leg syndrome and academic performance, while in linear regression analysis, it was found that the variable that most affects sleep is gender.
Conclusion
The implications of this study's findings are clear-nursing schools must intensify their efforts to raise awareness about the detrimental effects of sleep problems on academic performance. Furthermore, subsequent research is crucial to evaluate the execution of interventions aimed at preventing such disorders.
Keywords: nursing students, sleep disorder, academic performance, sleep habits, higher education
Introduction
Adequate sleep is crucial for individuals’ cognitive and physical health, and extended sleep deprivation has been linked to worse neurobehavioral functioning. The prevalence of sleep disorders among college students worldwide has increased in contemporary times, primarily due to the heightened academic pressures leading to stress (Pascoe et al., 2020). Moreover, changes in sleep environment, increased social opportunities, and busy schedules could all be significant factors (Haile et al., 2017). A review by Seoane et al. (2020) indicates that sleep disruption is a pandemic in the population of medical and nursing students. The National Sleep Foundation and the American Academy of Sleep Medicine state that insufficient sleep is a significant hazard for adolescents and young adults. It is advised that adults aim for 7–9 h of sleep per night, while school-aged children and teenagers should strive for up to 11 h (American Medical Association, American Academy of Sleep Medicine, 2010; National Sleep Foundation, 2006). Indeed, the chronic lack of sleep is a recent worry among adolescents and young university students, and it is associated with worse health and clinical outcomes (Dijk & Landolt., 2019; Alfawaz et at., 2021).
Throughout their academic pursuits, students may encounter various sleep-related issues, including insomnia, sleep apnea, hypersomnia, or sleep terror disorder. These disorders can profoundly impact their well-being, emotional state, and academic achievements. Excessive daytime sleepiness (EDS) caused by sleep deprivation is a common sleep issue among university students (Piro et al., 2018). A study by Belingheri et al. (2020) revealed that 44% of nursing students reported at least one symptom of sleep disturbance. Moreover, several studies have discovered a somewhat high occurrence of sleep-related issues, such as insufficient sleep, trouble initiating or maintaining sleep, waking up early in the morning, low sleep quality, feeling sleepy in the morning, and taking daytime naps, among college students (Hershner & Chervin, 2014). Prior research has also demonstrated the adverse effects of several sleep disorders, such as snoring and daytime sleepiness, on the academic achievement of college students (Khassawneh et al., 2018).
Review of Literature
Multiple research has been undertaken to ascertain the prevalence of sleep disorders among college students. Insomnia, restless leg syndrome (RLS), circadian rhythm disorders (CRDs), mood disorders, Narcolepsy, and obstructive sleep apnea (OSA) are prevalent among college students (Gaultney, 2010; Haile et al., 2017; Piro et al., 2018). According to previous studies conducted by Abdalqader et al. (2018) and Sing and Wong (2010), around 69% of college students experience insomnia. Less often identified diseases include CRDs (19.6%), depressive disorders (14.5%), nightmares (6.6%), sleepwalking (5.7%), and Narcolepsy (1.3%) (Piro et al., 2018). A separate study revealed that a range of sleep issues, including snoring and excessive daytime fatigue, detrimentally affect the academic performance of college students (Khassawneh et al., 2018). A recent study by Belingheri et al. (2020) demonstrated a high prevalence of sleep disorders among nursing and medical students and an association between these symptoms and perceived stress.
Grade Point Average (GPA) is a grading system used for both undergraduate and postgraduate students. A student's GPA is crucial in shaping their future, significantly impacting their prospective employment opportunities. Nevertheless, a student's GPA is significantly impacted by their academic performance, which is determined by their sleep patterns. There is a strong and widely recognized connection between sleep and academic performance. Insufficient sleep leads to fatigue and EDS, decreasing cognitive alertness and concentration (Reisi et al., 2017; Piro et al., 2018).
Nursing students experience notably elevated stress levels compared to other college students, making it crucial to obtain sufficient restful sleep to maintain their cognitive and physical health and achieve their objectives. The most susceptible demographic group to a range of sleep problems consists of full-time students who experience high-stress levels due to a significant workload of educational material and academic performance responsibilities. Medical students in their first year commonly experience sleep difficulties, specifically hypersomnia and insomnia. Insomnia, affective disorder, Narcolepsy, and CRD are sleep disorders that have been associated with decreased academic performance. A previous investigation revealed that medical students exhibited a substantial prevalence of symptoms and a heightened susceptibility to several sleep disorders (Yassin et al., 2020). Although sleep difficulties are significant, there is currently no research investigating their influence on the academic performance of nursing students in the United Arab Emirates. Moreover, information regarding the academic performance of college students and the factors that impact it needs to be more comprehensive. The objectives of this study were to assess the prevalence of sleep disorders among undergraduate nursing students in Ras Al Khaimah, United Arab Emirates, to identify the different types of sleep disorders among undergraduate nursing students in Ras Al Khaimah, United Arab Emirates, and to determine the impact of sleep disorders on academic performance among undergraduate nursing students in Ras Al Khaimah, United Arab Emirates.
Methods
Participants
A descriptive cross-sectional research design was used. The study was carried out in the emirates of RAS Al-Khaimah, at RAK Medical and Health Science University, Nursing Faculty (BSN1, BSN2, BSN3, and BSN4). A sample was calculated based on the total number of all the undergraduate nursing students in (hidden) from the four years (N = 309), using the Rao soft program (Sample Size Calculator by Roa soft, Inc, 2014), with an accepted margin of error of 5% and a confidence level of 95% the response distribution is 50%, confidence level at 95%. The sample size is n = 172.
Sampling Method
Consecutive sampling, the sample was drawn from undergraduate Nursing students in years 1, 2, 3, and 4. The estimated duration for data collection was two months, from February to April 2023, and the total number of participants was 177. The data were collected over three months, specifically from October 15, 2022, to February 28, 2023.
Inclusion and Exclusion Criteria
Inclusion criteria included students who agreed to participate in the study. On the other hand, students who were taking medications that affect their sleep status, such as alpha-blockers, corticosteroids, glucosamine and chondroitin, statins, and sedative–hypnotic drugs, including barbiturates and the benzodiazepine group, from the last month until data collection.
Data Collection Tools
The tools are consisted of two parts as following:
Part 1:
Sociodemographic characteristics: Includes questions on gender, age, Nationality, Year in the university, sleep hours, either more or less 8 h, weight, height, and BMI.
Academic performance: Academic performance was assessed using a grading scale from A+ to F. Students were asked to report their grades for the past semester, which were then categorized as follows: A+&A (excellent), B+&B (very good), C (good), D (satisfactory), and F (fail). These grades were collected through a self-reported questionnaire. The reliability and validity of the academic performance data were ensured using Cronbach's alpha for internal consistency α = 0.75. This approach provided a clear and quantifiable measure of academic outcomes among nursing students.
Part 2: The SLEEP-50 questionnaire validated by Spoormaker et al. (2005) for college students. It comprises 50 items meant to test the general population for various sleep problems. The scale is divided into nine subscales that reflect some of the most frequent sleep disorders and symptoms and other sleep features required for DSMIV diagnosis. The SLEEP-50 assesses OSA, periodic limb movement disorder/RLS (PLMD/RLS), insomnia, Narcolepsy, CRDs, sleepwalking, nightmares, affective disorder, hypersomnia, sleep state misperception, sleep hygiene (behaviors and environmental conditions that influence sleep), and impact on daily functioning. To score, participants respond to each item on a scale of 1 (not at all), 2 (somewhat), 3 (quite much), and 4 (very much) to determine which statement applies to their sleep quality during the last four months. The scores for each subscale are added together to determine the total subscore and scores. The internal consistency of the SLEEP-50 scale is 0.85 and its reliability falls between 0.65 and 0.89 (Spoormaker et al., 2005).
Ethical Considerations
This study conducted in accordance with the Declaration of Helsinki. Ethical approval was obtained from the Research and Ethics Committee of RAK Medical and Health Sciences University (RAKMHSU-REC-054-2022/23-UG-N) to conduct the study. Written informed consent was obtained from all participants before the study commenced. The researchers explained the study's purpose and details in the face to face survey, and they were asked to sign the informed consent form on their voluntary agreement to participate in the study. The research was done anonymously and stored in a password-protected computer.
Data Analysis
Data were analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using numbers and percentages. The Kolmogorov–Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation, and median. The significance of the obtained results was judged at the 5% level. The tests used were a Student t-test for normally distributed quantitative variables to compare between two studied groups and an F-test (ANOVA) for normally distributed quantitative variables to compare between more than two groups.
Results
Sociodemographic Characteristics of the Studied Students
Table 1 displays the distribution of the students under study based on their sociodemographic characteristics. The female gender is more predominant among the students under study, accounting for around 72.9% of the total population. Regarding age, 61.6% of the surveyed students fell between the 20- and 24-year age range, while just 10.2% were between the ages of 25 and 30, with a mean of 21.01 ± 3.36. Regarding marital status, the study found that around 94.4% of the students were unmarried, while only 5.6% were married. Approximately 34.5% of the students studied were in the first year, followed by 29.4% in the fourth year, and the second and third years accounted for around 19.2% and 16.9%, respectively.
Table 1.
Distribution of the Studied Students According to Tool I: Sociodemographic Characteristics (n = 177).
| Tool I: 1. Sociodemographic characteristics | No. | % |
|---|---|---|
| Gender | ||
| Male | 48 | 27.1 |
| Female | 129 | 72.9 |
| Age | ||
| 15–19 | 50 | 28.2 |
| 20–24 | 109 | 61.6 |
| 25–30 | 18 | 10.2 |
| Mean ± SD. | 21.01 ± 3.36 | |
| Marital status | ||
| Not married | 167 | 94.4 |
| Married | 10 | 5.6 |
| Year of the University | ||
| 1st | 61 | 34.5 |
| 2nd | 34 | 19.2 |
| 3rd | 30 | 16.9 |
| 4th | 52 | 29.4 |
| Sleep hours | ||
| Less than 8 h | 111 | 62.7 |
| 8 h or more | 66 | 37.3 |
| Weight (kg) | ||
| Min. – Max. | 32.0–135.0 | |
| Mean ± SD. | 60.62 ± 16.75 | |
| Median | 59.0 | |
| Height (cm) | ||
| \Min. – Max. | 148.0–190.0 | |
| Mean ± SD. | 163.05 ± 9.57 | |
| Median | 161.0 | |
| BMI | ||
| Min. – Max. | 13.49–42.61 | |
| Mean ± SD. | 22.63 ± 5.34 | |
| Median | 22.22 | |
| 2.GPA | No. | % |
| A+, A | 92 | 52.0 |
| B+, B | 53 | 29.9 |
| C+, C | 27 | 15.3 |
| D+, D | 4 | 2.3 |
| F | 1 | 0.6 |
SD: standard deviation; GPA: Grade Point Average.
About GPA, over 52.0% of the students surveyed achieved grades of A+ or A, while only roughly 0.6% received an F in their GPA. Furthermore, most (62.7%) students reported sleeping for less than 8 h. The weight of the researched student spans from 32.0 to 135.0 kg, with a mean of 60.62 ± 16.75 kg. Their height ranges from 148.0 to 190.0 cm, with a mean of 163.05 ± 9.57 cm. The BMI ranges from 13.49 to 42.61 kg/m2, with a mean of 22.63 ± 5.34 kg/m2.
Prevalence of Sleep Disorders among Nursing Students
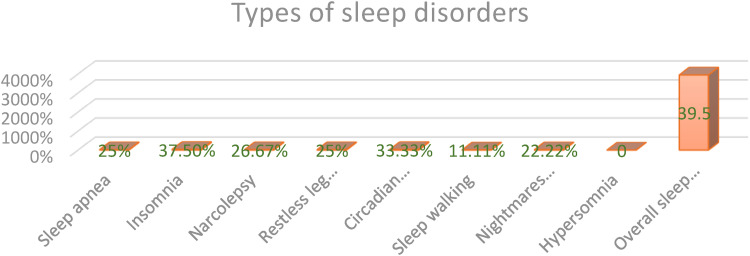
Table 2 presents a descriptive analysis of the students under study based on their sleep disorders. The data indicate that the prevalence of sleep disorders is 30.67%, with a mean of 30.07 ± 20.43. The severity of insomnia is measured on a scale of 0.0–100.0, with an average score of 39.27 ± 24.37. Similarly, the impact of sleep complaints is measured on a scale of 0.0–100.0, with an average score of 34.60 ± 26.03. The circadian rhythm ranges from 0.0 to 100.0 and has a mean value of 31.89 ± 24.90. Similarly, in Narcolepsy, apnea, and RLS, the values range from 0.0 to 100.0, with mean values of 28.74 ± 23.72, 27.07 ± 21.41, and 26.18 ± 25.01, respectively. Similarly, the severity of nightmares and the elements that affect sleep also vary on a scale of 0.0–100.0, with an average of 26.30 ± 22.20. Sleepwalking ranges from 0.0 to 100.0, averaging 23.67 ± 26.83. Insomnia was the most prevalent among the nursing students (37.5%), followed by circadian rhythm (33.3%), Narcolepsy (26.6%), sleep apnea, and RLS both same (25%), nightmares (22.2%), and sleepwalking (11.11%) (Figure 1).
Table 2.
Descriptive Analysis of the Studied Students According to Sleep (n = 177).
| Sleep | Total score | % score |
|---|---|---|
| Apnea | ||
| Min. – Max. | 8.0–32.0 | 0.0–100.0 |
| Mean ± SD. | 14.50 ± 5.14 | 27.07 ± 21.41 |
| Median | 14.0 | 25.0 |
| Insomnia | ||
| Min. – Max. | 8.0–32.0 | 0.0–100.0 |
| Mean ± SD. | 17.42 ± 5.85 | 39.27 ± 24.37 |
| Median | 17.0 | 37.50 |
| Narcolepsy | ||
| Min. – Max. | 5.0–20.0 | 0.0–100.0 |
| Mean ± SD. | 9.31 ± 3.56 | 28.74 ± 23.72 |
| Median | 9.0 | 26.67 |
| Restless leg syndrome | ||
| Min. – Max. | 4.0–16.0 | 0.0–100.0 |
| Mean ± SD. | 7.14 ± 3.0 | 26.18 ± 25.01 |
| Median | 7.0 | 25.0 |
| Circardian rhythm | ||
| Min. – Max. | 3.0–12.0 | 0.0–100.0 |
| Mean ± SD. | 5.87 ± 2.24 | 31.89 ± 24.90 |
| Median | 6.0 | 33.33 |
| Sleep walking | ||
| Min. – Max. | 3.0–12.0 | 0.0–100.0 |
| Mean ± SD. | 5.13 ± 2.41 | 23.67 ± 26.83 |
| Median | 4.0 | 11.11 |
| Nightmares and factors influencing sleep | ||
| Min. – Max. | 12.0–48.0 | 0.0–100.0 |
| Mean ± SD. | 21.47 ± 7.99 | 26.30 ± 22.20 |
| Median | 20.0 | 22.22 |
| Impact of sleep complains | ||
| Min. – Max. | 7.0–28.0 | 0.0–100.0 |
| Mean ± SD. | 14.27 ± 5.47 | 34.60 ± 26.03 |
| Median | 14.0 | 33.33 |
| Overall | ||
| Min. – Max. | 50.0–200.0 | 0.0–100.0 |
| Mean ± SD. | 95.11 ± 30.65 | 30.07 ± 20.43 |
| Median | 96.0 | 30.67 |
Figure 1.
Prevalence of sleep disorders among nursing students.
Relation Between Sleep Disorder and Academic Performance
Table 3 reveals a significant relationship between RLS and total sleep disorders and the student's achievement (p = 0.051 & 0.031), respectively. This result means that the student's level of achievement was higher among those with a low sleep disorder.
Table 3.
Relation Between Sleep Disorder and Academic Performance.
| Sleep disorders | Student achievement | Test of significance (p value) | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | F | ||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| Apnea | 14.11 ± 5.21 | 14.42 ± 5.59 | 14.92 ± 3.54 | 21.00 ± 3.82 | 16.00 ± 0.00 | 1.841 (0.123) |
| Insomnia | 17.16 ± 5.98 | 17.65 ± 6.16 | 17.53 ± 5.37 | 20.00 ± 1.82 | 16.00 ± 0.00 | .273 (0.895) |
| Narcolepsy | 9.15 ± 3.68 | 9.34 ± 3.66 | 9.53 ± 3.20 | 10.75 ± 2.21 | 10.00 ± 0.00 | .244 (0.913) |
| RLS | 6.98 ± 2.96 | 7.26 ± 3.20 | 6.75 ± 2.30 | 11.50 ± 3.41 | 8.88 ± 0.00 | 2.406 (0.051)* |
| Circadian rhythm | 5.77 ± 2.31 | 5.81 ± 2.33 | 6.14 ± 1.99 | 7.00 ± 1.41 | 6.00 ± 0.00 | .408 (0.803) |
| Sleep walking | 5.13 ± 2.46 | 4.86 ± 2.47 | 5.21 ± 2.13 | 7.75 ± 1.5 | 6.00 ± 0.00 | 1.387 (0.241) |
| Night mars | 9.13 ± 3.79 | 9.96 ± 4.06 | 9.46 ± 3.38 | 12.75 ± 4.99 | 10.00 ± 0.00 | 1.122 (0.348) |
| Impact | 13.76 ± 5.51 | 14.59 ± 5.54 | 15.14 ± 5.48 | 15.50 ± 4.12 | 14.00 ± 0.00 | .470 (0.758) |
| Total sleep | 81.21 ± 27.13 | 87.51 ± 26.89 | 96.35 ± 11.34 | 106.25 ± 20.02 | 86.00 ± 0.00 | 2.724 (0.031)* |
Relation Between Sleep and Sociodemographic Characteristics
Table 4 shows the relationship between sleep and sociodemographic characteristics. There is a statistically significant relationship between sleep disorder and both age and academic performance (p = 0.017, p = 0.031).
Table 4.
Relation Between Sleep and Tool I: Sociodemographic Characteristics (n = 177).
| Tool I: Sociodemographic characteristics | N | Overall sleep | Test of sig. | p |
|---|---|---|---|---|
| Mean ± SD. | ||||
| Gender | ||||
| Male | 48 | 36.06 ± 20.11 | t = 2.409* | 0.017* |
| Female | 129 | 27.84 ± 20.18 | ||
| Age | ||||
| 15–19 | 50 | 32.80 ± 19.18 | F = 0.845 | 0.431 |
| 20–24 | 109 | 29.49 ± 21.72 | ||
| 25–30 | 18 | 26.0 ± 14.98 | ||
| Marital status | ||||
| Not married | 167 | 29.90 ± 20.56 | t = 0.466 | 0.642 |
| Married | 10 | 33.00 ± 18.87 | ||
| Year of the University | ||||
| 1st | 61 | 27.02 ± 20.24 | F = 1.480 | 0.222 |
| 2nd | 34 | 29.20 ± 16.03 | ||
| 3rd | 30 | 28.93 ± 14.81 | ||
| 4th | 52 | 34.88 ± 25.15 | ||
| GPA | ||||
| A+, A | 92 | 81.20 ± 27.13 | F = 2.724 | 0.031* |
| B+, B | 53 | 87.51 ± 26.89 | ||
| C+, C | 27 | 96.35 ± 11.34 | ||
| D+, D | 4 | 1.0625 ± 20.02 | ||
| F | 1 | 86.000 | ||
| Sleep hours | ||||
| Less than 8 h | 111 | 29.82 ± 19.28 | t = 0.212 | 0.832 |
| 8 h or more | 66 | 30.49 ± 22.39 |
t: Student t-test.
F: F for One way ANOVA test.
GPA: Grade Point Average.
*Statistically significant at p ≤ 0.05.
Linear Regression Analysis for the Parameters Affecting Sleep
In linear regression analysis, it was found that the variable that most affect sleep is gender (Table 5).
Table 5.
Univariate and Multivariate Linear Regression Analysis for the Parameters Affecting Sleep (n = 177).
| Univariate | # Multivariate | |||
|---|---|---|---|---|
| p | B (LL – UL 95%C.I) | p | B (LL – UL 95%C.I) | |
| Gender | 0.017* | −8.211(−14.938 – −1.483) | 0.017* | −8.211(−14.938 to −1.483) |
| Age | 0.194 | −3.371 (−8.474–1.732) | ||
| Nationality | 0.729 | 2.949 (−13.844–19.742) | ||
| Marital status | 0.642 | 3.104(−10.055–16.263) | ||
| Year of the University | 0.051 | 2.428(−0.012–4.867) | ||
| GPA | 0.127 | 2.764(−0.793–6.322) | ||
| Sleep hours | 0.832 | 0.675(−5.611–6.961) | ||
B: Unstandardized Coefficients.
C.I: confidence interval; LL: lower limit; UL: upper limit; GPA: Grade Point Average.
All variables with p < 0.05 was included in the multivariate.
Statistically significant at p ≤ 0.05.
Discussion
Sleep is a fundamental aspect of human well-being and existence, playing a crucial role in learning, skill development, and overall physical and mental health. It affects an individual's learning capacity, academic performance, and neural–behavioral functioning. Of the students polled, 61.6% were in the age range of 20–24 years. Only 10.2% of the students were between the ages of 25 and 30, with a mean age of 21.01 ± 3.36. The study findings reveal that the occurrence of sleep disturbances is 30.67%, with an average of 30.07 ± 20.43. According to a study conducted by Abdelmoaty et al. (2020), out of 438 medical students ranging from the second year to the sixth year, 73.8% reported experiencing at least one sleep disturbance. In contrast, Thomas in Alabama observed a reduced prevalence of sleep disorders, with only 24% of individuals presenting with such conditions. The survey results indicated that a significant proportion of medical students (21.5%) at Zabol Medical University experienced sleep disorders (Mokarrar et al., 2017).
The outcomes of this study indicated that most surveyed students, precisely 62.7%, were experiencing insufficient sleep, with less than 8 h per day. This finding is in accordance with other findings of Gallego-Gómez et al. (2021), who mentioned that most of the students enrolled in the Nursing Degree slept less than six hours per day and in line with the results of Menon et al. (2015) and Simonelli-Muñoz et al. (2018). The emergence of poor sleep quality can be attributed to several causes, such as late-night study, long-term Internet use, stress produced by clinical settings, and coursework/examinations (Sajadi et al., 2014; Zunhammer et al., 2014).
Approximately 36.06% of male students reported experiencing sleep difficulties, while 27.84% of female students exhibited similar issues. This is in contrast to other studies that have reported contradictory findings. Abdelmoaty et al. (2020) reported that 66.8% of male students experienced sleep disorders, while female students had a significantly higher prevalence of 80.5%. Similarly, Alsaggaf's et al. (2016), at King Saudi University found that 25% of male students had sleep disorders, compared to a higher rate of 54% among female students. Additionally, the study by Toscano-Hermoso et al. (2020) announced that women show a higher risk [OR = 2.61] of presenting poor sleep quality (>5 points on the PSQI) compared with men (p < 0.001). Prior research has shown that women are more susceptible to sleep disturbances than men. The attribution can be related to the higher prevalence of various sleep-disrupting conditions among women, such as stress and depression (Marta et al., 2020; Piro et al., 2018). In our study, the cause that males have more sleep disorders might be attributed to the lifestyle and safety measures in the UAE, which facilitate late-night outings with friends. Additionally, there is an emerging trend of vaping among male students, which may have a potential correlation with sleep disturbances.
The nursing students had the highest incidence of insomnia, with a prevalence rate of 37.5%.it is in line with Al Salmani et al. (2020) of 637 university students. The insomnia prevalence rate was 36.4%, which is near the rate of 25% reported by a study conducted in Iraq (Piro et al., 2018). In contrast, the numbers recorded in American and Asian cohorts are significantly different, with 12% and 68%, respectively (Abdalqader et al., 2018). The possible cause of insomnia migh be attributed to Smoking in male students. Nicotine in cigarettes stimulates the central nervous system to release neurotransmitters such as dopamine, serotonin, norepinephrine, acetylcholine, and gamma-aminobutyric acid, which may regulate the sleep–wake cycle and increase sleep latency (Dugas et al., 2017). Menstruation may cause sleeplessness in female students. Premenstrual syndrome, induced by hormonal disruption, can produce mood swings, severe dysmenorrhea, and sleeplessness (Nicolaus et al., 2018). Dysmenorrheic discomfort from nighttime uterine contractility decreases sleep efficiency, duration, and start latency (Jeon & Baek., 2023).
Circadian rhythm disorder was the second most common disorder observed, accounting for 33.3% of cases. This finding aligns closely with the study conducted by Piro et al. (2018), which reported a prevalence of 19.6% for a CRD. Yassin et al. (2020) also found that circadian rhythm sleep disorder accounted for 22.4% of cases. The prevalence of Narcolepsy was determined to be only 26.6%, which is in opposition to the findings of Al Salmani et al. (2020). Based on the findings, Narcolepsy was the most prevalent sleep condition, with a prevalence rate of 88.2%. The study conducted by Abdelmoaty et al. (2020) found that Narcolepsy was the most common sleep condition among students, with a prevalence rate of 51.6% (226 cases). Subsequent research has reported significantly lower occurrence rates of this condition, ranging from 1.3% to 16.0% (Gaultney, 2010; Piro et al., 2018). The self-reported SLEEP-50 questionnaire may need to correctly indicate the prevalence of this disease due to response bias. Culture may explain why our community has a greater rate of Narcolepsy since individuals nap in the afternoon when the heat is the most. Due to the busy academic life at university, some students may no longer be able to indulge in this habit, which, combined with the fact that most students stay up late, may create daytime sleepiness.
Sleep apnea and RLS have a prevalence rate of 25% each; nightmares have a prevalence rate of 22.2%, and sleepwalking has a prevalence rate of 11.11%. In contrast to the findings of Al Salmani et al. (2020), who reported a prevalence rate of 41.1%, RLS was identified as the second most prevalent sleep condition. Other studies have also revealed similar findings. For example, a study conducted in Iraq indicated that the prevalence of RLS among medical students was 30.7% (Piro et al., 2018). A separate investigation in Saudi Arabia revealed that primary and secondary RLS occurrence rates were 64.1% and 35.9%, respectively (Alsafadi et al., 2018). The study conducted by Piro et al. examined 316 students from various medical colleges (medicine, nursing, dentistry, pharmacy, anesthesia, and medical laboratory sciences) at the public University of Duhok-Iraq. The results revealed that RLS was the most common sleep disorder, affecting 30.7% of the students. Affective disorder was reported by 14.5% of the students, while sleep apnea affected 13.6%. In addition, Yassin et al. (2020) discovered that RLS/PLMD had a prevalence rate of 22.4%, while OSA was observed in 16.4% of the participants. Nightmares were 13.7% of the sample, while sleepwalking had a prevalence rate of 3.7%.
It was found that students with a lower prevalence of sleep disorders exhibited higher levels of academic accomplishment. In accordance with the research conducted by Yassin et al. (2020), a survey was carried out on two medical schools in Jordan. In contrast, Jalili et al. (2020) showed no significant difference between sleep quality and academic achievement. The findings revealed that almost two-thirds of medical students were susceptible to at least one sleep problem, and various sleep disorders had an adverse effect on their academic performance. Nevertheless, longitudinal study should be performed to control for confounding factors.
The findings of this study indicated a significant relationship between RLS and overall sleep disturbance (p = 0.051, p = 0.031), as well as academic performance. In contrast, Abdelmoaty's study found no association between sleep disorders and poor academic performance. According to Thomas, there was no notable disparity between students with sleep difficulties (average rating of 3.43/5) and those without (average rating of 3.42/5). A study by Taylor revealed that students with sleep disorders exhibited a slightly lower, albeit statistically insignificant, difference in GPAs (mean 2.83) compared to those with standard sleep patterns (mean 2.92). Through both univariate and multivariate regression analyses, it was determined that gender is the primary variable that influences sleep disorders. This phenomenon may be attributed to the fact that GPA can be influenced by various other aspects, such as substance misuse, time management abilities, and social well-being (Piro et al., 2018). These characteristics can also influence the frequency of sleep disorders, with specific individuals being more susceptible to sleepwalking and emotional disorders.
Strengths and Limitations
The study identified the prevalence of sleep disorders and their association with academic performance and raised awareness about preventing them. Moreover, using reliable and valid tools enhanced the credibility of the findings. The limitation is that, as a study design, the cross-sectional technique needs to clearly illustrate the sequential relationship over time and show the causation and effect correlations between variables. The data findings cannot be generalized because of the small sample size.
Conclusion
The study findings reveal that the occurrence of sleep disturbances is 30.67%, with an average of 30.07 ± 20.43. Most surveyed students, precisely 62.7%, were experiencing insufficient sleep, with less than 8 h per day, and approximately 36.06% of male students reported experiencing sleep difficulties, while 27.84% of female students exhibited similar issues. Moreover, insomnia and CRD were the most common types among nursing students (37.5% and 33.3%) consequently. The findings of this study indicated a significant relationship between RLS and overall sleep disturbance (p = 0.051, p = 0.031), as well as academic performance and gender were the primary variables that affected the sleep disorder.
Implications for Practice
The findings of this study suggest that nursing schools should enhance their efforts to raise awareness about the detrimental effects of sleep problems on academic performance. Although further research is needed to definitively show a cause-and-effect relationship, professionals responsible for students’ health can still take steps to enhance the sleep patterns of medical students. Through awareness initiatives, nursing students should be educated about the implications of poor sleep habits and disorders. Additionally, they should be encouraged to seek guidance from sleep specialists to diagnose and treat any suspected sleep disorders.
Educational administrators should devise strategies to detect and address students vulnerable to sleep disorders to minimize or restrict the impact of these disorders on academic performance decline. Nevertheless, additional investigation is necessary in this domain. Subsequent research is advised to evaluate the execution of interventions to prevent such diseases.
Acknowledgments
The authors are grateful to all the students who have accepted to be part of this study.
Footnotes
Availability of Data and Materials: The data are available upon request.
Authors’ Contribution: Author FM contributed by formulating the study subject and creating the methodology. Authors FM and RN examined the data and composed the text. Authors FM and AM collaborated in formulating the procedure, analyzing data, and revising the manuscript. Authors FM and MA thoroughly evaluated the paper, made necessary corrections and contributed intellectually.
Consent for Publication: All authors have approved the final version of the manuscript and consent to its publication.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Fatma M Ibrahim https://orcid.org/0000-0002-2762-3350
References
- Abdalqader M. A., Ariffin I. A., Ghazi H. F., AboBakr M. F., Fadzil M. A. (2018). Prevalence of insomnia and its association with social media usage among university students in Selangor, Malaysia, 2018. Folia Medica Indonesiana, 54(4), 289–293. 10.20473/fmi.v54i4.10715 [DOI] [Google Scholar]
- Abdelmoaty Goweda R., Hassan-Hussein A., Ali Alqahtani M., Janaini M. M., Alzahrani A. H., Sindy B. M., Kalantan S. A. (2020). Prevalence of sleep disorders among medical students of Umm Al-Qura University, Makkah, Kingdom of Saudi Arabia. Journal of Public Health Research, 9(1 suppl), jphr–2020. https://doi.org/10.4081/jphr.2020.1921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfawaz R. A., Aljuraiban G. S., AlMarzooqi M. A., Alghannam A. F., BaHammam A. S., Dobia A. M., Aljaloud K. S. (2021). The recommended amount of physical activity, sedentary behavior, and sleep duration for healthy Saudis: A joint consensus statement of the Saudi Public Health Authority. Annals of Thoracic Medicine, 16(3), 239. 10.4103/atm.atm_33_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsafadi S., Abaalkhail B., Wali S. O., Aljammali K., Alotaiby B., Zakaria I., Sabbahi H. (2018). Risk factors of primary and secondary restless legs syndrome among a middle-aged population in Saudi Arabia: A community-based study. Annals of Thoracic Medicine, 13(3), 175–181. 10.4103/atm.ATM_344_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsaggaf M., Wali S., Merdad R., Merdad L. (2016). Sleep quantity, quality, and insomnia symptoms of medical students during clinical years: Relationship with stress and academic performance. Saudi Medical Journal, 37(2), 173–82. 10.15537/smj.2016.2.14288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Salmani A. A., Al Shidhani A., Al Qassabi S. S., Al Yaaribi S. A., sharfi A. M. (2020). Prevalence of sleep disorders among university students and its impact on academic performance. International Journal of Adolescence and Youth, 25(1), 974–981. 10.1080/02673843.2020.1815550 [DOI] [Google Scholar]
- American Medical Association, American Academy of Sleep Medicine (2010). Resolution 503: Insufficient sleep in adolescents.
- Belingheri M., Pellegrini A., Facchetti R., De Vito G., Cesana G., Riva M. A. (2020). Self-reported prevalence of sleep disorders among medical and nursing students. Occupational Medicine, 70(2), 127–130. 10.1093/occmed/kqaa011 [DOI] [PubMed] [Google Scholar]
- Dijk D. J., Landolt H. P. (2019). Sleep physiology, circadian rhythms, waking performance and the development of sleep-wake therapeutics. Handbook of Experimental Pharmacology, 253, 441–481. 10.1007/164_2019_243 [DOI] [PubMed] [Google Scholar]
- Dugas E. N., Sylvestre M. P., O'Loughlin E. K., Brunet J., Kakinami L., Constantin E., O'Loughlin J. (2017). Nicotine dependence and sleep quality in young adults. Addictive Behaviors, 100(65), 154–160. 10.1016/j.addbeh.2016.10.020 [DOI] [PubMed] [Google Scholar]
- Gallego-Gómez J. I., González-Moro M. T. R., González-Moro J. M. R., Vera-Catalán T., Balanza S., Simonelli-Muñoz A. J., Rivera-Caravaca J. M. (2021). Relationship between sleep habits and academic performance in university nursing students. BMC Nursing, 20(1), 100. 10.1186/s12912-021-00635-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaultney F. J. (2010). The prevalence of sleep disorders in college students: Impact on academic performance. Journal of American College Health, 59(2), 91–97. 10.1080/07448481.2010.483708 [DOI] [PubMed] [Google Scholar]
- Haile Y. G., Alemu S. M., Habtewold T. D. (2017). Insomnia and its temporal association with academic performance among university students: A cross-sectional study. Biomed Research International, 2017, 2542367. 10.1155/2017/2542367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hershner S. D., Chervin R. D. (2014). Causes and consequences of sleepiness among college students. Nature and Science of Sleep, 6, 73–84. 10.2147/NSS.S62907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalali R., Khazaei H., Paveh B. K., Hayrani Z., Menati L. (2020). The effect of sleep quality on students’ academic achievement. Advances in Medical Education and Practice, 11, 497–502. 10.2147/AMEP.S261525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon B., Baek J. (2023). Menstrual disturbance and its association with sleep disturbance: Systematic Review. BMC. Women's Health, 23(1), 470. 10.1186/s12905-023-02629-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khassawneh B. Y., Alkhatib L. L., Ibnian A. M., Khader Y. S. (2018). The association of snoring and risk of obstructive sleep apnea with poor academic performance among university students. Sleep and Breathing, 22, 831–836. 10.1007/s11325-018-1665-z [DOI] [PubMed] [Google Scholar]
- Marta O. F. D., Kuo S. Y., Bloomfield J., Lee H. C., Ruhyanudin F., Poynor M. Y., Chiu H. Y. (2020). Gender differences in the relationships between sleep disturbances and academic performance among nursing students: A cross-sectional study. Nurse Education Today, 85, 104270. 10.1016/j.nedt.2019.104270 [DOI] [PubMed] [Google Scholar]
- Menon B., Karishma H. P., Mamatha I. V. (2015). Sleep quality and health complaints among nursing students. Annals of Indian Academy of Neurology, 18(3), 363–4. 10.4103/0972-2327.157252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokarrar M. H., Afsharmanesh A., Afshari M., Mohammadi F. (2017). Prevalence of sleep disorder among medical students in an Eastern university in Iran. Iranian Journal of Health Sciences, 5(1), 49–54. 10.18869/acadpub.jhs.5.1.49 [DOI] [Google Scholar]
- National Sleep Foundation (2006). Summary of findings: 2006 Sleep in America poll.
- Nicolaua Z. F. M., Bezerraa A. i. G., Polesela D. N., Andersena M. L., Bittencourta L., Tufika S., Hachul H. (2018). Premenstrual syndrome and sleep disturbances: Sao Paulo Epidemiologic Sleep Study results. Psychiatry Research, 264, 427–431. 10.1016/j.psychres.2018.04.008 [DOI] [PubMed] [Google Scholar]
- Pascoe M. C., Hetrick S. E., Parker A. G. (2020). The impact of stress on students in secondary school and higher education. International Journal of Adolescence and Youth, 25(1), 104–112. 10.1080/02673843.2019.1596823 [DOI] [Google Scholar]
- Piro R. S., Alhakem S. S. M., Azzez S. S., Abdulah D. M. (2018). Sleep disorders’ prevalence and impact on academic performance in medical students/University of Duhok. Sleep and Biological Rhythms, 16(1), 125–132. 10.1007/s41105-017-0134-6 [DOI] [Google Scholar]
- Reisi M., Jalilian R., Azizi G., Rashti A., Faghihinia J., Akbari M., Babaei N., Sayedi S. J., Rezaei N., Modaresi M. R. (2017). Academic performance, sleep disorders and their association in middle school students in Iran. International Journal of Pediatrics, 5(3), 4541–4549. http://ijp.mums.ac.ir [Google Scholar]
- Sajadi Z., Farsi N., Rajai N. (2014). The relationship between sleep quality with fatigue severity and academic performance of nursing students. Nurse Practice Today, 1(4), 213–220. https://npt.tums.ac.ir/index.php/npt/article/view/31 [Google Scholar]
- Seoane H. A., Moschetto L., Orliacq F., Orliacq J., Serrano E., Cazenave M. I., Perez-Lloret S. (2020). Sleep disruption in medicine students and its relationship with impaired academic performance: a systematic review and meta-analysis. Sleep Medicine Reviews, 53, 101333. 10.1016/j.smrv.2020.101333 [DOI] [PubMed] [Google Scholar]
- Simonelli-Muñoz A. J., Balanza S., Rivera-Caravaca J. M., Vera-Catalán T., Lorente A. M., Gallego-Gómez J. I. (2018). Reliability and validity of the student stress inventory-stress manifestations questionnaire and its association with personal and academic factors in university students. Nurse Educ Today, 64, 156–160. 10.1016/j.nedt.2018.02.019 [DOI] [PubMed] [Google Scholar]
- Sing C. Y., Wong W. S. (2010). Prevalence of insomnia and its psychosocial correlates among college students in Hong Kong. Journal of American College Health, 59(3), 174–182. 10.1080/07448481.2010.497829 [DOI] [PubMed] [Google Scholar]
- Spoormaker V. I., Verbeek I., Van den Bout J., Klip E. C. (2005). Initial validation of the SLEEP-50 questionnaire. Sleep, 3(4), 227–246. 10.1207/s15402010bsm0304_4 [DOI] [PubMed] [Google Scholar]
- Toscano-Hermoso M. D., Arbinaga F., Fernández-Ozcorta E. J., Gómez-Salgado J., Ruiz-Frutos C. (2020). Influence of sleeping patterns in health and academic performance among university students. International Journal of Environmental Research and Public Health, 17(8), 2760. 10.3390/ijerph17082760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yassin A., Al-Mistarehi A. H., Yonis O. B., Aleshawi A. J., Momany S. M., Khassawneh B. Y. (2020). Prevalence of sleep disorders among medical students and their association with poor academic performance: A cross-sectional study. Annals of Medicine and Surgery, 58, 124–129. 10.1016/j.amsu.2020.08.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zunhammer M., Eichhammer P., Busch V. (2014). Sleep quality during exam stress: the role of alcohol, caffeine, and nicotine. PLoS One, 9(10), e109490. 10.1371/journal.pone.0109490 [DOI] [PMC free article] [PubMed] [Google Scholar]