Abstract
Fournier’s gangrene is a severe, life-threatening form of necrotizing fasciitis that predominantly affects the perineal, genital, and perianal areas. It is characterized by a rapid onset and progression, often developing from urogenital infections, diabetes, compromised immune function, or trauma. This report describes the case of a 64-year-old woman who presented with perianal pain and purulent discharge persisting for a week. Upon examination, a substantial necrotic wound was identified in her perineal region, necessitating urgent surgical debridement followed by aggressive postoperative management, including antibiotic therapy and meticulous blood sugar control. Despite initial signs of improvement, the patient’s condition deteriorated due to complications from diabetes, acidosis, and pneumonia, ultimately leading to a fatal outcome. This case highlights the critical need for prompt recognition and comprehensive management of Fournier’s gangrene, particularly in female patients exhibiting similar symptoms.
Keywords: Fournier’s gangrene, necrotizing fasciitis, perineal infection, genital sepsis, polymicrobial infection, debridement, antibiotic therapy
Introduction
Fournier’s gangrene (FG) is a life-threatening bacterial infection characterized by rapid necrosis of the fascia and tissues in the genital, perianal, and perirectal areas. First described in 1883 by Jean Alfred Fournier, the condition primarily affects males, with a reported incidence of 1.6 per 100,000 and a male-to-female ratio of 10:1.1,2,4,5 It typically originates from infections in the genitourinary tract, anorectal region, or as a consequence of trauma.1,2,4,5
The progression of FG involves both aerobic and anaerobic bacteria. These bacteria produce enzymes that facilitate the rapid spread of the infection, which can lead to severe systemic symptoms. FG is most common in older adults who often have other health conditions such as diabetes, alcoholism, or liver disease, which can complicate the infection and treatment outcomes.1–3
Treatment of Fournier’s gangrene requires urgent medical intervention, typically involving aggressive surgical debridement of necrotic tissues, broad-spectrum antibiotic therapy, and supportive care for any underlying conditions. Despite these measures, the prognosis can be poor, especially in patients with significant comorbidities or delayed presentation.1–3 This case exemplifies the severe nature of FG in an elderly woman following perianal sepsis, who despite initial treatment success, succumbed to the condition due to her compromised health status
Case report
Patient presentation
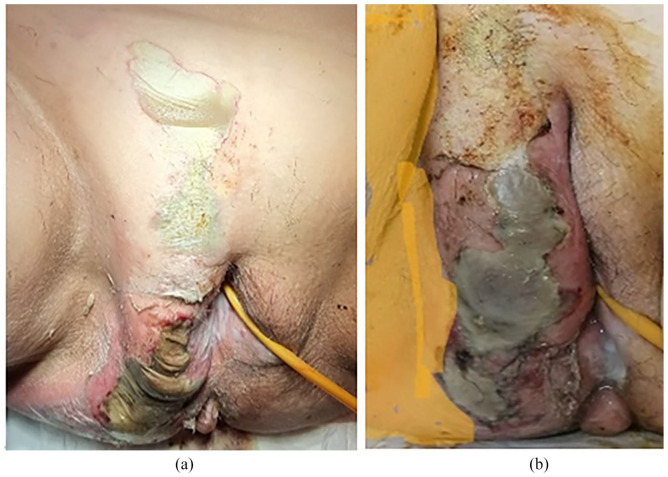
A 64-year-old nulliparous woman with Type 2 Diabetes Mellitus, Hypertension, and Coronary Artery Disease presented with severe perianal pain and a week-long history of purulent discharge. Examination revealed a significant perineal wound extending from the gluteal area to the right labia majora, characterized by foul-smelling discharge and necrosis, suggestive of necrotizing fasciitis or gangrene (Figure 1(a) and (b)). Despite appearing well-nourished, she was pallor, disoriented, and uncooperative, with severe hypotension and bradycardia (Figure 1).
Figure 1.
Right-sided vulvar bulge and green-black discoloration, necrotizing fasciitis from labia major since posterior glutea (a, b) peri-anal wound with necrotic patch and slough.
Initial management
Immediate management involved broad-spectrum antibiotics (vancomycin, amikacin, and meropenem) and norepinephrine to stabilize her condition. Laboratory tests indicated anemia, neutrophilic leukocytosis, and impaired kidney function, while a Computed tomography (CT) scan confirmed extensive inflammation and gas formation.
Surgical intervention
Emergency surgical debridement preserved the anal sphincter but revealed a deep fascial plane infection (Figure 2). Following surgery, the patient was admitted to the intensive care unit (ICU) for continued critical care. Initial empiric antibiotic therapy was adjusted based on culture results identifying Escherichia coli and Staphylococcus aureus, optimizing antimicrobial efficacy.
Figure 2.
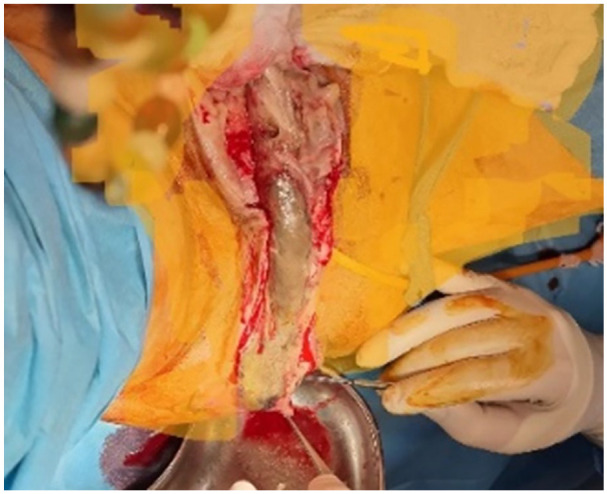
Extensive debridement of the necrotic tissue preserving the anal sphincter. Intraoperatively, wound seen extending to the ischiorectal fossa.
Intensive care management
In the ICU, continuous cardiovascular support with norepinephrine was necessary to maintain adequate blood pressure. Renal function was closely monitored due to acute kidney injury, and nephrotoxic drugs were avoided. Although dialysis was considered, conservative management, including fluid optimization and electrolyte monitoring, was initially preferred.
Chest physiotherapy was initiated early to prevent respiratory complications, given the patient’s reduced mobility and the development of mild pleural effusion. Despite these preventive measures, the patient developed pneumonia, which was aggressively treated with targeted antibiotics and supportive respiratory care (Figure 3). Customized nutritional support was critical due to the patient’s catabolic state, designed to meet her caloric and nutritional needs considering her diabetes and the metabolic demands of severe infection and surgical recovery.
Figure 3.

Intensive dressing. Despite 24-h dressings, after 3 weeks of intensive management, granulation tissue started to appear on the wound site (Figure 4).
Wound management and recovery
Upon admission, the patient underwent immediate surgical debridement to remove necrotic tissue, critical for reducing the load of infective material and preventing further spread of the infection. This procedure preserved the anal sphincter and prepared the wound for subsequent recovery phases. Negative pressure wound therapy (NPWT) was initiated shortly after stabilization to promote wound healing. This therapy helped maintain a clean wound environment, reduced edema, and enhanced granulation tissue formation over the extensive perineal wound. Given the location and severity of the wound, fecal diversion via a temporary colostomy was performed to prevent fecal contamination and reduce secondary infection risks. This intervention was crucial for allowing undisturbed wound healing in the perineal area and was discussed with the patient to ensure understanding and consent.
Regular monitoring indicated fluctuating kidney function, suggesting acute kidney injury superimposed on preexisting chronic kidney disease. Management strategies were adapted to avoid nephrotoxic medications and ensure adequate hydration. Dialysis was considered but deferred, opting for conservative management initially. The decision was based on a comprehensive assessment of fluid and electrolyte balance, and renal function trends, with dialysis equipment prepared for immediate use if required.
Outcome
Despite intensive management, the patient suffered recurrent infections and renal issues, complicating her recovery. Postoperative care included blood transfusions, tailored parenteral nutrition, and intensive metabolic management. Granulation tissue started forming at the wound site after 3 weeks (Figure 4). However, persistent wound issues and renal instability 5 weeks post-treatment complicated her recovery, ultimately leading to her demise. Histology confirmed Fournier’s syndrome (Figure 5).
Figure 4.

Granulation tissue started to appear on the wound site.
Figure 5.

The wound was not closed and recurrent infection on the buttocks.
This case underscores the complexity of managing Fournier’s gangrene in patients with significant comorbidities, highlighting the challenges of surgical management, the critical need for timely intervention, and the importance of comprehensive postoperative care in improving outcomes.
Discussion
Fournier’s gangrene, though uncommon in women, represents a severe medical emergency due to its rapid progression to sepsis if untreated, exhibiting a mortality rate of 20%–30% largely due to anatomical differences.5,6 In men, anatomical features provide some protection, limiting the spread of infection predominantly to the scrotum. Conversely, in women, while pelvic drainage reduces susceptibility, the anatomical layout of Colles’ fascia can allow the infection to extend extensively to the abdominal wall, potentially increasing mortality to 70% if complications such as sepsis and organ failure ensue. 7
Distinguishing Fournier’s gangrene from other skin infections like cellulitis and gas gangrene is challenging, particularly in the early stages where necrotizing fasciitis is confined to the epidermis, making it difficult to differentiate from cellulitis.1,2 Diagnostic accuracy at initial presentation is notably low, ranging from 15% to 34%. 3 The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score, proposed by Wong et al., serves as a crucial early differentiation tool, with scores ⩾6 strongly indicating necrotizing fasciitis. 9 In the described case, a LRINEC score of 9 affirmed the presence of necrotizing fasciitis from the outset.
Diabetes mellitus significantly heightens the risk of Fournier’s gangrene, with the role of glycemic control in patient outcomes still debated. Insulin pumps are often preferred for managing glucose levels in the early disease stages to address severe inflammation and immune challenges. 11 Critical risk factors include perineal and perianal abscesses, hypertension, trauma, chronic catheterization, neoplasms, and notably, renal failure, all influencing disease incidence and mortality.12,13 The infection’s polymicrobial nature, involving aerobic and anaerobic bacteria like E. coli and Staphylococcus species, emphasizes the complexity of its management, requiring a comprehensive approach that integrates metabolic control, antimicrobial therapy, surgical debridement, and advanced wound care.6,14–16 This complexity is further heightened in females, where additional factors like diabetes and obesity increase susceptibility. 17
Treatment strategies prioritize early surgical intervention, hemodynamic support, and broad-spectrum antibiotics. NPWT offers healing benefits, although it presents challenges. 18 Techniques such as urinary and fecal diversion are crucial for preventing wound contamination, enhancing healing, and supporting nutritional well-being, necessitating careful evaluation of both patient and disease severity. 19 The involvement of a wide range of microorganisms underscores the importance of precise culture and sensitivity analyses for effective antibiotic selection. Diagnostic imaging is pivotal in assessing the extent of the gangrene and guiding therapeutic decisions.20,21
Additional considerations in treatment strategy include the potential use of hyperbaric therapy, silver dressings, frequency of surgical wound cleaning, and early imaging studies in clinical diagnosis uncertainties. Subsequent reconstructive surgery may be required. Comprehensive patient management is critical, particularly due to the frequent presence of multiple comorbidities in these patients, as meticulous care can significantly reduce mortality.
Conclusion
Fournier’s gangrene, though rare in women, demands urgent attention for those showing necrotizing fasciitis symptoms. Its seriousness necessitates prompt diagnosis, rapid debridement, targeted antibiotics, and thorough wound care. Managing coexisting conditions like diabetes is crucial for prognosis. A collaborative care approach is essential for comprehensive treatment. Awareness among healthcare professionals is vital for quick intervention, aiming to improve survival rates and reduce complications.
Acknowledgments
We extend our gratitude to our esteemed colleagues for their unwavering support and invaluable insights that significantly contributed to this research.
Footnotes
Author contributions: Dr. Kariman Ghazal and Georges Yared spearheaded this case report encompassing the conception and design, data acquisition, analysis, and interpretation. They played a pivotal role in drafting the manuscript and provided final approval for the version to be submitted. Dr. Charlotte El Hajjar, Dr. Jihad Al Hassan, Dr. Nour Madi, and Dr. Saad Abou Hammin further enriched the manuscript by critically revising it for significant intellectual content and also extended their approval for the final version to be submitted. Finally, Hamza Nakib played a crucial role in the editorial process of this manuscript, significantly enhancing its overall quality. His expertise not only improved the clarity and accuracy of the content but also ensured that the arguments presented were coherent and compelling. His contributions were instrumental in refining our paper and bringing it to publication standards.
Data availability: The data supporting the findings of this study are available from Rafic Hariri University Hospital.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval to report this case was obtained from RAFIC HARIRI UNIVERSITY HOSPITAL BY DR. GEORGES YARED
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article
ORCID iD: Kariman Ghazal  https://orcid.org/0000-0002-3199-631X
https://orcid.org/0000-0002-3199-631X
References
- 1. Pernetti R, Palmieri F, Sagrini E, et al. Fournier’s gangrene: clinical case and review of the literature. Arch Ital Urol Androl 2016; 88(3): 237–238. [DOI] [PubMed] [Google Scholar]
- 2. Khalid A, Devakumar S, Huespe I, et al. A comprehensive literature review of Fournier’s gangrene in females. Cureus. 2023; 15(5): e38953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guliyeva G, Huayllani MT, Sharma NT, et al. Practical review of necrotizing fasciitis: principles and evidence-based management. Plast Reconstr Surg Glob Open 2024; 12(1): e5533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leslie SW, Rad J, Foreman J. Fournier gangrene. StatPearls Publishing: Treasure Island, FL, USA, 2024. [PubMed] [Google Scholar]
- 5. Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis 2014; 59(2): 147–159. [DOI] [PubMed] [Google Scholar]
- 6. Aslanidis T, Athena M, Maria G. Management of a young female patient with Fournier’s gangrene and Lemierre’s syndrome. Pan Afr Med J 2014; 18: 275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhang JY, Xiao CF, Wang C, et al. Bibliometric insights in Fournier’s gangrene: research landscapes, turning points, and global trends. Front Surg 2023; 10: 1057486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tang LM, Su YJ, Lai YC. The evaluation of microbiology and prognosis of Fournier’s gangrene in past five years. Springerplus 2015; 4: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wong CH, Khin LW, Heng KS, et al. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing ne crotizing fasciitis from other soft tissue infections. Crit Care Med 2004; 32: 1618–1619. [DOI] [PubMed] [Google Scholar]
- 10. Burner E, Henderson S, Burke G, et al. Inadequate sensitivity of laboratory risk indicator to rule out necrotizing fasciitis in the emergency department. West J Emerg Med 2016; 17(3): 333–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gülşen T, Sücüllü I, Balta AZ, et al. Fournier’s gangrene. Turk J Colorectal Dis 2019; 29: 206–210. [Google Scholar]
- 12. Hahn HM, Jeong KS, Park DH, et al. Analysis of prognostic factors affecting poor outcomes in 41 cases of Fournier gangrene. Ann Surg Treat Res 2018; 95: 324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Morais H, Neves J, Ribeiro HM, et al. Case series of Fournier’s gangrene: affected body surface area—the underestimated prognostic factor. Ann Med Surg (Lond) 2017; 16: 19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ylmazlar T. Fournier Gangreni: Sinsi, Öldürücü, Ancak TedaviEdilebilir Hastalık. Kolon Rektum Hast Derg 2012; 22: 45–49. [Google Scholar]
- 15. Iacovelli V, Cipriani C, Sandri M, et al. The role of vacuum-assisted closure (VAC) therapy in the management of Fournier’s gangrene: a retrospective multi-institutional cohort study. World J Urol 2021; 39(1): 121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cabello RR, Mancilla NG, Feregrino NR, et al. A case report of a woman with Fournier’s gangrene and morbid obesity. Rev Mex Patol Clin Med Lab 2016; 63: 82–86. [Google Scholar]
- 17. Beecroft NJ, Jaeger CD, Rose JR, et al. Fournier’s gangrene in females: presentation and management at a tertiary center. Urology 2021; 151: 113–117. [DOI] [PubMed] [Google Scholar]
- 18. Assenza M, Cozza V, Sacco E, et al. VAC (vacuum assisted closure) treatment in Fournier’s gangrene: personal experience and literature review. Clin Ther 2011; 162(1): e1–e5. [PubMed] [Google Scholar]
- 19. Hahn HM, Jeong KS, Park DH, et al. Analysis of prognostic factors affecting poor outcomes in 41 cases of Fournier gangrene. Ann Surg Treat Res 2018; 95: 324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ioannidis O, Kitsikosta L, Tatsis D, et al. Fournier’s gangrene: lessons learned from multimodal and multidisciplinary management of perineal necrotizing fasciitis. Front Surg 2017; 4: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Insua-Pereira I, Ferreira PC, Teixeira S, et al. Fournier’s gangrene: a review of reconstructive options. Cent European J Urol 2020; 73(1): 74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]