Abstract
Background:
Screws for graft fixation are available in 3 different materials for anterior cruciate ligament reconstruction (ACLR) with the Tape Locking Screw (TLS) technique: titanium, poly-l-lactic acid bioabsorbable, and polyetheretherketone (PEEK).
Purpose:
To compare the effect of the 3 different fixation materials on graft and implant survival after ACLR with the TLS technique.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Included were 521 patients from the French Prospective ACL Study (FAST) cohort who underwent primary surgical ACLR with the TLS technique. Patients were divided into 3 groups depending on the type of screw material used: titanium (TLS-T group), poly-l-lactic acid bioabsorbable (TLS-B group), or PEEK (TLS-P group). The primary endpoint was a retear within 2 years after ACLR. The secondary endpoints were complication rate, return to sports rate, and functional scores. Objective and subjective functional scores—including the International Knee Documentation Committee, the Knee injury and Osteoarthritis Outcome Score (KOOS), and the Lysholm score—were evaluated preoperatively and at the 2-year follow-up. Pain was assessed with the KOOS-Pain subscore recorded pre- and postoperatively every 6 months up to 2 years. Patient satisfaction was recorded at the 2-year follow-up.
Results:
No significant differences between the study groups were found in retear rates (4.4%, 4.5%, and 4.3% in the TLS-T, TLS-P, and TLS-B groups 2 years after surgery) or subjective and objective outcomes. The TLS-T group had the lowest rate of intraoperative implant-related complications (0.9%) compared with the TLS-P (4.3%) and TLS-B (7.7%) groups. Young age was a significant risk factor for retear in the TLS-T (P = .03) and TLS-B (P = .0001) groups, while a high level of sports was found to be a significant risk factor in the TLS-P (P = .04) group. All functional scores improved significantly at the 2-year follow-up (P < .0001), with no significant group difference. The KOOS-Pain subscore improved continuously with no significant group difference. The rate of return to preinjury sports was between 43.4% and 58.6%. The rate of highly satisfied patients at the final follow-up was between 86.2% and 91.8%.
Conclusion:
There was no difference in retear rate or objective and subjective functional scores between implant materials for TLS ACLR in this study.
Keywords: anterior cruciate ligament reconstruction, bioabsorbable, polyetheretherketone, screw material, titanium, Tape Locking Screw
The failure of anterior cruciate ligament (ACL) reconstruction (ACLR) is multifactorial.1,9,14 Trauma and technical and biological factors are the leading causes of ACLR failure. 4 Thus, ACLR techniques have been modified with new methods and fixation materials to improve graft survival after ACLR.6-10
Screws are extensively used for graft fixation. They are designed to attach a soft graft, bone, or synthetic material into bone tunnels with potential complications such as graft slippage or movement in the tunnel, causing widening and graft damage. 12 Materials can be nonabsorbable (eg, titanium, polyetheretherketone [PEEK], or steel) or bioabsorbable (poly-l-lactic acid or poly-d-lactic acid, polyglycolic acid, or polycaprolactone). 10 Images of nonmetallic screws are better on postoperative magnetic resonance imaging. 11 On the other hand, no clinical difference has been found between metallic and bioabsorbable screws, except for fewer complications with metallic screw5,21,22,23 or no difference neither clinically nor in terms of complications.2-8 In their systematic review of the literature, Speziali et al 20 reported a failure rate of 3.3% for metallic and 6.1% for bioabsorbable screws, with no statistical significance between the 2. Shumborski et al 19 published similar clinical results after comparing PEEK and titanium tibial screws at a 2-year follow-up.
The Tape Locking Screw (TLS) System (FH Orthopaedics) is a 4-strand short, semitendinosus autograft loaded on synthetic (polyethylene terephthalate) anchoring bands that are attached from the outer tibial and femoral cortices. Thus, the graft is suspended in the bone tunnel, but an outer aperture fixation is done at the far cortex with a conical screw. A bony barrier is preserved between the graft and the cortex by retrograde drilling of the tunnels. 13
Titanium, PEEK, and bioabsorbable screws are available for use with the TLS technique. All these options have the same structural form. 7 The mean reported pullout strength of the TLS is 523 ± 269 N and 578 ± 245 N with the PEEK and titanium screws, respectively, a difference which is not statistically significant. The leading cause of TLS failure is tape slippage at the bone-screw interface, 3 which only occurs during violent trauma and is less probable in a braced knee. This study aimed to compare these 3 different screw materials for TLS reconstruction. These screws have the same form but differ in their performance, security, and patient satisfaction. We hypothesized that the different screw materials would influence clinical results, especially graft failure and complication rates.
Methods
This comparative study was based on prospective data from a continuous series of patients registered with the French Prospective ACL Study (FAST) cohort. 5 Ethical approval was waived by our institution, and the study protocol was registered on ClinicalTrials.gov (trial number NCT02511158). All patients provided written informed consent.
This study included consecutive adult patients (age >16 years old) who underwent isolated primary ACLR with the TLS technique between January 1, 2013, and December 31, 2015, after a total or partial tear. Although patients with collateral ligament injuries were not excluded from the study, patients with pivot injuries such as associated posterior cruciate ligament injury, those with tibial spine avulsion, and those who refused to participate or had incomplete follow-up were excluded (Figure 1). The patients were not randomized according to screw type. Because of a lack of valid criteria for implant selection, screws were selected either according to availability or the surgeon’s preference.
Figure 1.
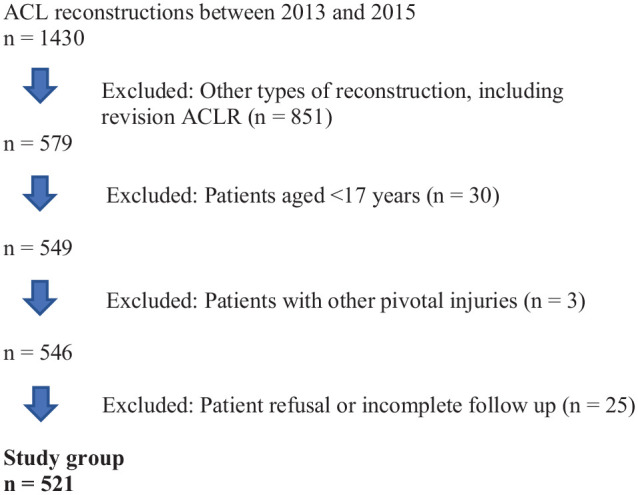
Flowchart of participant inclusion in the study. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction.
The included patients were divided into 3 study groups depending on the type of screw material used: titanium (TLS-T group), poly-l-lactic acid bioabsorbable (TLS-B group), or PEEK (TLS-P group).
Surgical Technique
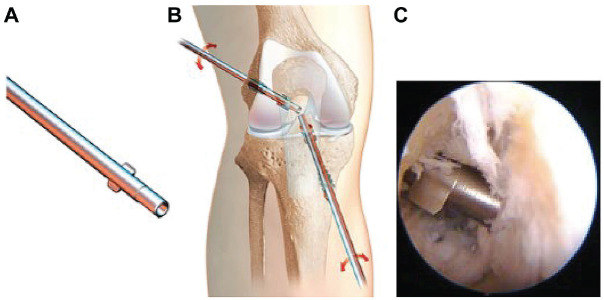
TLS is a fixation system using 4 folded semitendinosus tendon grafts suspended on tapes (Figure 2). The graft was pretensioned at 500 N. Femoral and tibial tunnels were prepared by the inside-out technique using special retrograde reamers (Figure 3). After intra-articular placement of the graft, the tapes were fixed in the far cortices using screws after first tapping to facilitate screw insertion (Figure 4).
Figure 2.

Preparation of 4 folded semitendinosus autografts. Reproduced with permission of FH Orthopaedics.
Figure 3.
(A) Retrograde reamer, (B) reaming of femoral and tibial tunnels, and (C) intra-articular appearance. Images A and B were reproduced with permission of FH Orthopaedics.
Figure 4.
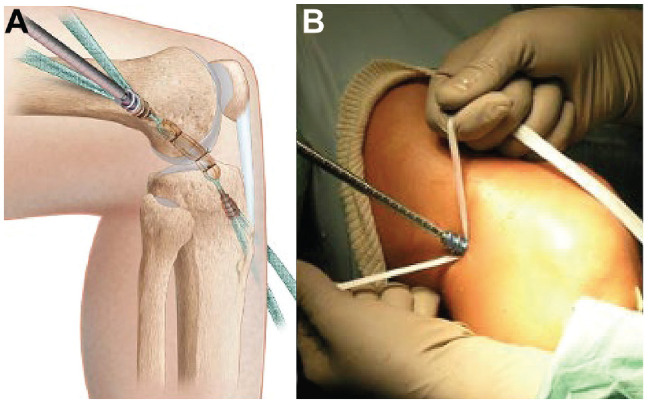
(A) Graft and screw placement. (B) Fixation of tapes in the outer cortex (operative view). Figure 4A was reproduced with permission of FH Orthopaedics.
Outcome Measures
All patients completed follow-up examinations by the operating surgeon (N.L.) at 4 weeks, 12 weeks, 6 months, 1 year, and 2 years postoperatively to identify complications, with radiographs at each visit and magnetic resonance imaging at the 6-month and 1-year follow-ups. In addition, patients completed an online survey preoperatively then at 4 weeks, 3 months, 6 months, 1 year, and 2 years postoperatively conducted using Websurvey.fr software. Patients were provided with the web link to an electronic version of the survey, and a second email was sent as a reminder if the patient did not respond or was contacted by telephone. In the survey, patients were asked to provide descriptive data, functional scores, and surgical data.
The primary outcome measure was the occurrence of retears at a 2-year follow-up. Graft failure was suspected when there was either >5 mm side-to-side difference in anterior laxity as measured by the Genourob knee arthrometer under a 200-N force or a positive Lachman test and a giving-way sensation and inability to return to sports (RTS). The secondary outcome measures were complications, RTS rate, and functional scores. Adverse events—such as intraoperative complications and postoperative hematoma, hemarthrosis, septic arthritis, deep vein thrombosis, cyclops syndrome, and reflex sympathetic dystrophy—were recorded during the first 2 postoperative years. Functional scores consisted of objective and subjective International Knee Documentation Committee (IKDC), Knee injury and Osteoarthritis Outcome Score (KOOS), and Lysholm scores completed preoperatively and at the 2-year follow-up. Pain was evaluated according to the KOOS-Pain subscale. The KOOS-Pain subscale includes 9 questions (1 general and 8 describing different positions for the onset of pain) and is presented as a percentage from 0 (extreme pain) to 100 (no pain) before surgery and at 6-month, 1-year, and 2-year follow-ups.
The level of play was defined as professional, competitive, regular, and occasional leisure. Sports were categorized as pivot contact, pivot noncontact, and nonpivot. Patients who played sports at any level and of any type were categorized as athletic; otherwise, they were categorized as nonathletic. The subgroup of athletic patients was evaluated for RTS. The return to jogging and the preferred sport was noted, and the level of play at 2 years postoperatively was compared with the best level before the injury.
At the 2-year follow-up, a patient satisfaction questionnaire was recorded. Satisfaction was graded as very satisfied, satisfied, somewhat satisfied, or not satisfied.
Statistical Analysis
Statistical analysis was performed with R software Version 4.2 (R Core Team). Quantitative variables were recorded as means with standard deviations, and qualitative variables were recorded as absolute values with percentages. Comparisons between the 3 study groups (TLS-T, TLS-B, and TLS-P) were performed for quantitative variables with the analysis of variance or Kruskal-Wallis tests and qualitative variables with the chi-square test. When the P value of the analysis of variance or the Kruskal-Wallis test was significant, a post hoc analysis was performed with the Bonferroni correction or Dunn test to compare the groups pairwise. Graft survival was estimated using the Kaplan-Meier nonparametric method. The event was a recurrent ACL tear on the same knee and was evaluated with the log-rank test. Multivariate survival analysis was performed to assess the association between ACL retears and risk factors. The selection of covariates was based on the results of univariate analysis (only factors with P < .05 were selected). Hazard ratios (HRs) were estimated using the Cox proportional hazard model. P < .05 was considered to be statistically significant.
Results
A total of 521 patients were included, with 177 women and 344 men. There were 507 athletes (97.3%), including 205 athletes (39.4%) who had a professional contract in a club or were competitive players (high-level athletes who had a license and practiced regularly at a competitive level). The mean age was 30.1 ± 9.3 years. There were 229 patients in the TLS-T group, 70 in the TLS-P group, and 222 in the TLS-B group. Patient characteristics and preoperative scores by study group are listed in Table 1. There was a significant difference in anterior laxity side-to-side difference among the groups, which was higher in the TLS-B group than in the TLS-T group (P = .02, Dunn test), and the IKDC objective score, with more D grades in the TLS-T group (P < .0001). A total of 174 patients (76%) in the TLS-T group, 53 patients (75.7%) in the TLS-P group, and 180 patients (81.1%) in the TLS-B group completed all questionnaires at all follow-ups.
Table 1.
Comparison of Preoperative Data Between the Study Groups a
| Preoperative Data | TLS-T (n = 229) | TLS-P (n = 70) | TLS-B (n = 222) | P |
|---|---|---|---|---|
| Age at surgery, y | 30.7 ± 9.1 | 30.6 ± 10.1 | 29.2 ± 9.2 | .17 |
| Sex | .56 | |||
| Male | 156 (68.1) | 43 (61.4) | 145 (65.3) | |
| Female | 73 (31.9) | 27 (38.6) | 77 (34.7) | |
| BMI, kg/m2 | 24 ± 3 | 23.3 ± 3.2 | 23.7 ± 3.1 | .25 |
| Dominance | .15 | |||
| Right knee | 125 (54.6) | 30 (42.9) | 124 (55.9) | |
| Left knee | 104 (45.4) | 40 (57.1) | 98 (44.1) | |
| Previous knee surgery | 5 (2.2) | 1 (1.4) | 6 (2.7) | .9 |
| Meniscectomy, n | 5 | 1 | 5 | |
| Patellar fracture, n | 0 | 0 | 1 | |
| Level of sport practice | .3 | |||
| Professional | 10 (4.4) | 2 (2.9) | 14 (6.3) | |
| Competition | 79 (34.5) | 17 (24.3) | 83 (37.4) | |
| Regular | 02 (44.5) | 33 (47.1) | 92 (41.4) | |
| Occasional | 32 (14) | 16 (22.8) | 26 (11.7) | |
| No sport played | 6 (2.6) | 2 (2.9) | 7 (3.2) | |
| Type of sport | .5 | |||
| Pivot contact b | 129 (56.3) | 28 (40) | 121 (54.5) | |
| Pivot noncontact c | 46 (20.1) | 20 (28.6) | 54 (24.3) | |
| Nonpivot d | 35 (15.3) | 12 (17.1) | 32 (14.4) | |
| No sport played | 6 (2.6) | 2 (2.9) | 7 (3.2) | |
| Missing data | 13 (5.7) | 8 (11.4) | 8 (3.6) | |
| Circumstances of the accident | .6 | |||
| Sport | 192 (83.8) | 52 (74.3) | 194 (87.4) | |
| Domestic | 10 (4.4) | 5 (7.1) | 6 (2.7) | |
| Working | 9 (3.9) | 2 (2.9) | 9 (4.1) | |
| Traffic accident | 7 (3.1) | 3 (4.3) | 4 (1.8) | |
| Missing data | 11 (4.8) | 8 (11.4) | 9 (4) | |
| Anterior laxity difference, mm e | 3.4 ± 2 | 3.4 ± 2 | 3.9 ± 2.2 | .046 |
| IKDC objective score | <.0001 | |||
| A | 0 (0) | 0 (0) | 0 (0) | |
| B | 23 (9.6) | 8 (11.4) | 33 (14.9) | |
| C | 128 (55.9) | 41 (58.6) | 161 (72.5) | |
| D | 69 (30.1) | 10 (14.3) | 21 (9.5) | |
| Missing data | 10 (4.4) | 11 (15.7) | 7 (3.1) | |
| IKDC subjective score (0-100) | 55.5 ± 18.5 | 58.6 ± 17.7 | 59.3 ± 17.3 | .14 |
| KOOS-Symptoms (0-100) | 71.4 ± 16.5 | 75.6 ± 15.6 | 71.4 ± 18.3 | .18 |
| KOOS-Pain (0-100) | 73.6 ± 17.4 | 76.4 ± 15.2 | 74.8 ± 17.8 | .92 |
| KOOS-ADL (0-100) | 83.6 ± 16 | 85.6 ± 15.4 | 84.2 ± 18.2 | .5 |
| KOOS-Sport (0-100) | 41 ± 26.4 | 46.1 ± 28.5 | 44 ± 27.8 | .2 |
| KOOS-QoL (0-100) | 28.3 ± 20 | 31.3 ± 23.6 | 30.8 ± 20.8 | .95 |
| Lysholm (0-100) | 68.5 ± 20.7 | 71 ± 16.3 | 71.2 ± 19.5 | .35 |
Data are reported as n (%) or mean ± SD unless otherwise indicated. Bold P values indicate statistically significant differences between groups (P < .05). ADL, activities of daily living; BMI, body mass index; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; QoL, quality of life; TLS-B, Tape Locking Screw with bioabsorbable screws; TLS-P, Tape Locking Screw with polyetheretherketone screws; TLS-T, Tape Locking Screw with titanium screws.
Examples: football, handball, rugby, basketball, and judo.
Examples: tennis, skiing, badminton, and volleyball.
Examples: jogging, cycling, and swimming.
Side-to-side difference measured with Genourob knee arthrometer at 200 N of force.
The results of the surgical data are presented in Table 2. More patients in the TLS-T group were admitted as inpatients (71.6%) and had drainage tubes (92.1%) (P < .0001). More dynamometers were used in the TLS-B group (P = .001), while there were higher rates of cyclic loading and Lemaire extra-articular tenodesis in the TLS-P group (P < .001). A total of 60 patients (11.5%) underwent Lemaire anterolateral extra-articular tenodesis. The population had 12 collateral ligament surgeries (2.3%).
Table 2.
Comparison of Surgical Data Between the Study Groups a
| Operative Data | TLS-T (n = 229) | TLS-P (n = 70) | TLS-B (n = 222) | P |
|---|---|---|---|---|
| Mode of admission | <.0001 | |||
| Outpatient | 65 (28.4) | 38 (54.3) | 113 (50.9) | |
| Inpatient | 164 (71.6) | 32 (45.7) | 109 (49.1) | |
| Anesthesia | ||||
| General | 52 (22.7) | 9 (12.9) | 43 (19.4) | .19 |
| Regional | 177 (77.3) | 61 (87.1) | 179 (80.6) | |
| Drain tube placement (yes) | 211 (92.1) | 33 (47.1) | 164 (73.9) | <.0001 |
| Type of rupture | .45 | |||
| Total | 224 (97.8) | 70 (100) | 209 (94.1) | |
| Partial | 5 (2.2) | 0 (0) | 13 (5.6) | |
| Cartilage lesion | 71 (31) | 15 (21.4) | 49 (22.1) | .06 |
| Chondroplasty, n | 3 | 2 | 4 | |
| Microfracture, n | 9 | 13 | 3 | |
| Nonoperative, n | 59 | 0 | 42 | |
| Medial meniscus injury | 83 (36.2) | 25 (35.7) | 77 (34.7) | .9 |
| Partial, n | 32 | 10 | 32 | |
| Suture, n | 2 | 2 | 3 | |
| Nonoperative, n | 49 | 13 | 42 | |
| Lateral meniscus injury | 80 (34.9) | 21 (30) | 77 (34.7) | .7 |
| Partial meniscectomy, n | 36 | 9 | 32 | |
| Suture, n | 13 | 2 | 3 | |
| Nonoperative, n | 31 | 10 | 42 | |
| Graft diameter, mm | 8.6 ± 0.7 | 8.8 ± 0.9 | 8 ± 0.7 | .8 |
| Graft length, mm | 52.8 ± 6.4 | 53.2 ± 3.8 | 52.9 ± 4.2 | .5 |
| Tibial tunnel diameter, mm | 8.6 ± 0.8 | 8.6 ± 1.3 | 8.8 ± 0.8 | .15 |
| Femoral tunnel diameter, mm | 8 ± 0.7 | 8.1 ± 0.8 | 8 ± 0.8 | .99 |
| Dynamometer (yes) | 9 (3.9) | 3 (4.3) | 27 (12.2) | .001 |
| Cyclic loading (yes) | 122 (53.3) | 57 (81.4) | 157 (70.7) | <.0001 |
| Lemaire extra-articular tenodesis | 15 (6.6) | 17 (24.3) | 28 (12.6) | .0002 |
| Other ligament surgeries, n | .98 | |||
| LCL | 0 | 1 | 5 | |
| MCL | 3 | 2 | 1 | |
Data are reported as n (%) or mean ± SD unless otherwise indicated. Bold P values indicate statistically significant differences between groups (P < .05). LCL, lateral collateral ligament; MCL, medial collateral ligament; TLS-B, Tape Locking Screw with bioabsorbable screws; TLS-P, Tape Locking Screw with polyetheretherketone screws; TLS-T, Tape Locking Screw with titanium screws.
Primary Outcome Measure: Retear Rate
A total of 23 retears (4.4%) occurred after a mean of 14.4 ± 4.8 months. The rate of retears at 2 years of follow-up was 4.4%, 2.8%, and 5.0% in the TLS-T, TLS-P, and TLS-B groups, respectively. Kaplan-Meier curves are presented in Figure 5. There was no statistically significant difference among the 3 groups on the log-rank test (P = .99). All retears were sports injuries. The type of sport for the retears was pivot contact in 6, pivot noncontact in 3, and nonpivot in 1 patient in the TLS-T group; only pivot contact in the TLS-P group; and pivot contact in 7, pivot noncontact in 2, and nonpivot in 2 patients in the TLS-B group.
Figure 5.
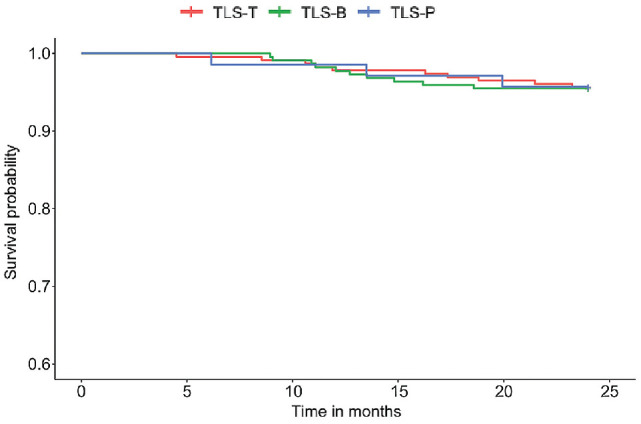
The Kaplan-Meier curve estimates for the 3 study groups. TLS-B, Tape Locking Screw with bioabsorbable screws; TLS-P, Tape Locking Screw with polyetheretherketone screws; TLS-T, Tape Locking Screw with titanium screws.
The results of the univariate analysis of risk factors for a recurrent ACL tear at 2 years postoperatively are presented in Table 3. Participants with a retear were significantly younger (24.3 vs 30.3 years; P < .0001), with a higher rate of competitive sports (70% vs 33%; P = .005). Moreover, the graft length was longer in those with than without a retear (P = .006).
Table 3.
Risk Factors for Retear at 2 Years After ACLR With TLS Technique a
| Retear (n = 23) | No Retear (n = 498) | P | |
|---|---|---|---|
| Screw type | .99 | ||
| Titanium | 10 (43) | 219 (44) | |
| PEEK | 3 (13) | 67 (13) | |
| Bioabsorbable | 10 (43) | 212 (43) | |
| Age at surgery, y | 24.3 ± 5.9 | 30.3 ± 9.3 | <.0001 |
| Sex | .11 | ||
| Male | 19 (83) | 325 (65) | |
| Female | 4 (17) | 173 (35) | |
| BMI, kg/m2 | 23.8 ± 3.1 | 23.1 ± 2.9 | .23 |
| Level of play | .005 | ||
| Professional | 2 (9) | 24 (5) | |
| Competitive | 16 (70) | 163 (33) | |
| Regular | 4 (17) | 223 (45) | |
| Occasional | 1 (4) | 73 (15) | |
| No sports | 0 (0) | 15 (3) | |
| Type of sport b | .11 | ||
| Pivot contact | 19 (83) | 259 (52) | |
| Pivot noncontact | 3 (13) | 117 (24) | |
| Nonpivot | 1 (4) | 78 (16) | |
| No sport | 0 (0) | 18 (4) | |
| Missing data | 0 (0) | 26 (5) | |
| Laxity difference at GNRB 200 N | 4.2 ± 2.2 | 3.7 ± 2.1 | .28 |
| IKDC objective score | |||
| A | 0 (0) | 1 (0.2) | |
| B | 2 (9) | 61 (12) | |
| C | 16 (70) | 314 (63) | |
| D | 4 (17) | 96 (20) | |
| Missing data | 1 (4) | 26 (5) | |
| Drain tube placement (yes) | 16 (70) | 392 (79) | .30 |
| Cartilage lesion | 3 (13) | 132 (27) | .22 |
| Medial or lateral meniscus injury | 16 (70) | 283 (57) | .28 |
| Graft diameter, mm | 8.2 ± 0.8 | 8 ± 0.7 | .23 |
| Graft length, mm | 55.1 ± 3.4 | 52.8 ± 5.7 | .006 |
| Tibial tunnel diameter, mm | 8.8 ± 1.3 | 8.7 ± 0.7 | .20 |
| Femoral tunnel diameter, mm | 8.1 ± 1.2 | 8 ± 0.8 | .25 |
| Dynamometer (yes) | 4 (17) | 35 (7) | .10 |
| Cyclic loading (yes) | 14 (60) | 322 (65) | ≥.99 |
| Lemaire extra-articular tenodesis (yes) | 2 (9) | 58 (12) | .98 |
Data are reported as n (%) or mean ± SD unless otherwise indicated. Bold P values indicate statistically significant differences between retear and no-retear groups (P < .05). ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; GNRB, Genourob knee arthrometer; IKDC, International Knee Documentation Committee; PEEK, polyetheretherketone; TLS, Tape Locking Screw.
See Table 1 for examples of sports for each type.
No significant difference was found in retear rates among the 3 groups (Table 4). Older age was associated with a lower risk of retear on multivariate analysis (HR, 0.93 [95% CI, 0.87-0.99]; P = .017). On the other hand, practicing sports at the regular level (ie, below the competitive and professional levels) was associated with a lower risk of retear (HR, 0.25 [95% CI, 0.08-0.77]; P = .016). Young age was a significant risk factor for retear in the TLS-T (P = .03) and TLS-B (P = .0001) groups, while a high level of sports was found to be a significant risk factor in the TLS-P (P = .04) group.
Table 4.
Results of Multivariate Cox Model Analysis a
| Hazard Ratio (95% CI) | P | |
|---|---|---|
| Screw type | ||
| Titanium | 1 b | |
| PEEK | 1.35 (0.36-5.04) | .781 |
| Bioabsorbable | 0.88 (0.36-2.14) | .652 |
| Age at surgery, y | 0.93 (0.87-0.99) | .017 |
| Level of sport practice | ||
| Professional | 0.69 (0.16-3.01) | .619 |
| Competition | 1 b | |
| Regular | 0.25 (0.08-0.77) | .016 |
| Occasional | 0.17 (0.02-1.49) | .109 |
| No sport (no case of rerupture) | — | |
| Graft length | 1.06 (0.99-1.13) | .051 |
Bold P values indicate statistical significance (P < .05). PEEK, polyetheretherketone. Dash indicates no patients.
Reference.
Revision Surgeries
Eight (3.5%) of the patients in the TLS-T group underwent revision surgery. Five patients (2.2%) were operated using the Kenneth-Jones technique (4 cases [1.8%] associated with Lemaire extra-articular tenodesis), 2 reconstructions (0.9%) were performed with a fascia lata graft, and 1 patient (0.44%) underwent surgery in another center. Three patients (4.3%) in the TLS-P group underwent revision ACLR using the Kenneth-Jones technique associated with a Lemaire extra-articular tenodesis. Eight patients (3.60%) in the TLS-B group underwent revision ACLR. One patient (0.45%) was found to have an elongated graft resulting in laxity. Three patients (1.35%) did not undergo revision surgery, including 2 (0.9%) with a partial graft tear with a stable knee, and 1 (0.45%) patient was lost to follow-up at 2 years of follow-up.
Complications
Intraoperative Complications
There was a significant difference in the rate of intraoperative complications among the 3 groups (P = .02), with 7.7%, 4.3%, and 2.2% in the TLS-B, TLS-P, and TLS-T groups, respectively (Table 5). The complication rates during and after the first week were not significantly different among the 3 TLS groups.
Table 5.
Complication Rates Among the 3 Groups a
| TLS-T (n = 229) | TLS-P (n = 70) | TLS-B (n = 222) | P | |
|---|---|---|---|---|
| Intraoperative complication | .02 | |||
| Yes | 5 (2) | 3 (4) | 17 (8) | |
| No | 224 (98) | 67 (96) | 205 (92) | |
| Complications during the first postoperative week | .59 | |||
| Yes | 19 (8) | 3 (4) | 17 (8) | |
| No | 210 (92) | 67 (96) | 205 (92) | |
| Complications after the first postoperative week | .21 | |||
| Yes | 22 (10) | 12 (17) | 28 (13) | |
| No | 207 (90) | 58 (83) | 194 (87) |
Data are reported as n (%). The bold P value indicates a statistically significant difference between groups (P < .05). TLS-B, Tape Locking Screw with bioabsorbable screws; TLS-P, Tape Locking Screw with polyetheretherketone screws; TLS-T, Tape Locking Screw with titanium screws.
Two (0.9%) of the 5 (2.2%) adverse events in the TLS-T group were intraoperative and related to the screws. One tibial and 1 femoral screw was not sufficiently tight but was considered satisfactory and left in place. The graft was too short in 1 patient, resulting in a 3-strand graft. The tape was changed in 1 patient, and the cord to pull the tape got stuck in the tunnel, and the cord had to be passed again in another patient.
In the TLS-P group, all 3 (4.3%) intraoperative adverse events were due to fixation. Fixation was insufficient with two 25-mm femoral screws, which were changed to size 30 mm. Although 1 screw was broken, the graft was found to be stable. The screw was left in the femur with no graft failure during the follow-up.
The 17 intraoperative adverse events (7.7%) in the TLS-B group were related to fixation. Either the tibial or femoral screws were broken in 13 patients (5.9%). In 1 case (0.45%), a broken femoral screw was left in place because fixation was sufficient, with no graft failures. A poorly attached tibial screw (0.45%) was left in place and augmented by a staple. One broken bioabsorbable screw (0.45%) was replaced with a titanium screw. A total of 4 intraoperative tape ruptures occured but only one was (0.45%), was long enough to be used.
Postoperative Complications
The postoperative complications according to groups are listed in Supplemental Table S1 (available separately). Fourteen (2%) immediate complications, were events that occurred in the first postoperative week, occured (hematoma, hemarthrosis,infection) in all patients. Two patients in each group, thus 6 patients (1%) overall, had simple diffuse subcutaneous hematomas occured but did not require surgery. Out of four hemarthroses occurred in the TLS-T group; 1 required an arthroscopic intervention on the third day.
Deep vein thrombosis was diagnosed in 1 patient in the TLS-B group. None of these patients required reoperation. Three patients had septic arthritis, 1 in each group, which was treated with arthroscopic irrigation and debridement followed by antibiotics.
In addition to retears, the number of complications after the first postoperative week in the TLS-T, TLS-P, and TLS-B groups was 22 (9.6%), 12 (17.1%), and 28 (12.6%), respectively. The number of contralateral retears in the 3 groups was 10 (4.4%), 3 (4.3%), and 10 (4.5%), respectively.
Functional Scores and Pain
All functional scores (objective and subjective IKDC, KOOS subscales, and Lysholm) improved significantly from preoperatively to the 2-year follow-up (P < .0001 for all). Moreover, no significant difference was observed in scores among the 3 groups at 2 years postoperatively (Table 6).
Table 6.
Comparison of Functional Scores at 2-Year Follow-up a
| TLS-T (n = 229) | TLS-P (n = 70) | TLS-B (n = 222) | P | |
|---|---|---|---|---|
| IKDC objective | .08 | |||
| A | 36 (15.7) | 20 (28.6) | 62 (27.9) | |
| B | 108 (47.2) | 25 (35.7) | 100 (14.9) | |
| C | 26 (11.3) | 12 (17.1) | 26 (72.5) | |
| D | 2 (0.9) | 0 (0) | 3 (9.5) | |
| NR | 57 (24.9) | 12 (18.6) | 31 (3.1) | |
| IKDC subjective | 83.4 ± 15.4 | 83.4 ± 12.5 | 85.4 ± 12.9 | .77 |
| KOOS-Symptoms | 84.7 ± 14 | 87.9 ± 12.3 | 86.5 ± 12 | .30 |
| KOOS-Pain | 90.8 ± 11.6 | 92.4 ± 7.8 | 92.5 ± 8.8 | .90 |
| KOOS-ADL | 95.8 ± 7.7 | 97.7 ± 5.3 | 96.7 ± 7.6 | .58 |
| KOOS-Sport | 81.2 ± 20.9 | 82.3 ± 20.2 | 82.2 ± 19.9 | .61 |
| KOOS-QoL | 74.2 ± 24.3 | 73.1 ± 20.7 | 75.1 ± 23.1 | .97 |
| Lysholm | 89.3 ± 12 | 90.3 ± 10 | 90.2 ± 11.3 | .83 |
Data are reported as n (%) or mean ± SD. ADL, activities of daily living; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; NR, no response; QoL, quality of life; TLS-B, Tape Locking Screw with bioabsorbable screws; TLS-P, Tape Locking Screw with polyetheretherketone screws; TLS-T, Tape Locking Screw with titanium screws.
KOOS-Pain subscores improved continuously over time (Figure 6). The mean KOOS score improved from a preoperative value of 74.5 ± 17.3 to 91.8 ± 10 at the 2-year follow-up. No significant difference was found among the 3 groups in KOOS-Pain subscores at any follow-up period.
Figure 6.
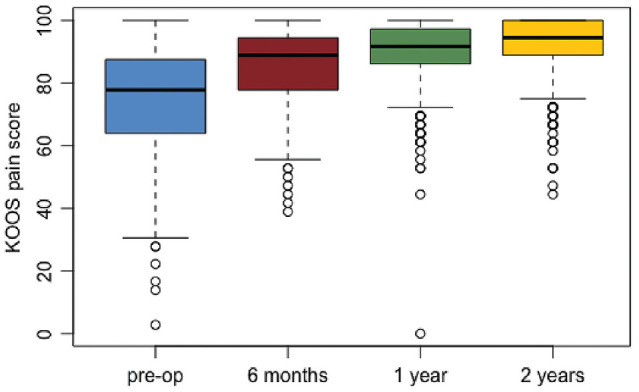
Changes in KOOS-Pain scores. The center black line indicates the median, the top and bottom of the boxes indicate the upper and lower quartiles, the whiskers indicate the ranges, and the circles indicate outliers. KOOS, Knee injury and Osteoarthritis Outcome Score.
Return to Sports
At the 2-year follow-up, 174 (76%) patients in the TLS-T group, 53 (75.7%) patients in the TLS-P group, and 180 (81.1%) patients in the TLS-B group answered the RTS questionnaire. A total of 128 (73.6%), 40 (75.7%), and 123 (68.3%) patients returned to jogging in the TLS-T, TLS-P, and TLS-B groups, respectively; this difference was not statistically significant (Table 7). A total of 76 (43.7%), 20 (37.7%), and 82 (45.6%) patients in TLS-T, TLS-P, and TLS-B groups reported an RTS at the same level or higher (P = .84) (Table 7).
Table 7.
Return to Sports at 2-Year Follow-up a
| TLS-T (n = 174) | TLS-P (n = 53) | TLS-B (n = 180) | P | |
|---|---|---|---|---|
| Returned to jogging | 128 (73.6) | 40 (75.7) | 123 (68.3) | .54 |
| Time to return to jogging, mo | 12 ± 8.4 | 11.4 ± 7.2 | 9.9 ± 8.3 | .47 |
| Returned to the preferred sport | 102 (58.6) | 23 (43.4) | 99 (55) | .16 |
| Time to return to preferred sport, mo | 13.6 ± 7.5 | 13.2 ± 6 | 12.6 ± 8 | .34 |
| Level of play | .84 | |||
| Higher | 9 (5.2) | 2 (3.8) | 14 (7.8) | |
| Same | 67 (38.5) | 18 (34) | 68 (37.8) | |
| Lower | 60 (34.5) | 23 (43.4) | 58 (32.2) | |
| Changed sport | 21 (12) | 5 (9.4) | 17 (9.4) | |
| No sports | 17 (9.8) | 5 (9.4) | 23 (12.8) |
Data are reported as n (%) or mean ± SD. TLS-B, Tape Locking Screw with bioabsorbable screws; TLS-P, Tape Locking Screw with polyetheretherketone screws; TLS-T, Tape Locking Screw with titanium screws.
Patient Satisfaction
The patient satisfaction questionnaire was filled out by 174 (76%), 53 (75.7%), and 178 (80.1%) patients in the TLS-T, TLS-P, and TLS-B groups, respectively. The number of patients who stated that they were very satisfied or satisfied was 150 (86.2%), 48 (90.6%), and 165 (91.6%) in the TLS-T, TLS-P, and TLS-B groups, respectively (Table 8). There was no statistically significant difference in satisfaction among the groups (P = .26).
Table 8.
Satisfaction at 2-Year Follow-up a
| Patient Satisfaction | TLS-T (n = 174) | TLS-P (n = 53) | TLS-B (n = 178) | P |
|---|---|---|---|---|
| Satisfied/very satisfied | 150 (86.2) | 48 (90.6) | 165 (91.6) | .26 |
| Somewhat satisfied | 20 (11.5) | 4 (7.5) | 12 (6.7) | |
| Not satisfied | 4 (2.3) | 1 (1.9) | 1 (0.7) |
Data are reported as n (%). TLS-B, Tape Locking Screw with bioabsorbable screws; TLS-P, Tape Locking Screw with polyetheretherketone screws; TLS-T, Tape Locking Screw with titanium screws.
Discussion
The findings of the present study indicated no differences in clinical results among the different tested fixation materials regarding ACLR with the TLS technique. Variables that were found to be statistically significant, such as age in the TLS-T (P = .03) and TLS-B groups (P = .0001) and level of play in the TLS-P group (P = .04), cannot be considered statistically valid because the groups were not homogeneous. This study did not validate our hypothesis that different fixation materials would affect clinical results. As expected, the TLS-T group had the lowest rate of intraoperative complications (2.2%) compared to the TLS-P (4.3%) and TLS-B (7.7%) groups. Multivariate analysis showed that older age and regular leisure level of play helped protect patients from retear.
There are numerous fixation techniques, each with advantages and disadvantages. 16 Most existing studies on implant-related failures have compared different types and fixation materials at the same time.15,16,17 Metallic interference screws have been shown to have lower rates of complications than other fragile materials, such as bioabsorbable poly-l-lactic acid.19,20,21,22,23 In our study, we used the same surgical technique to test 3 different fixation materials. Moreover, all reconstructions were performed by 2 senior surgeons (N.L.,Y.B.) using the same approach.
The TLS technique uses a 4-strand short semitendinosus graft loaded on tapes attached to the femur and tibia in the dense cortical bone of the metaphyseal-diaphyseal outer cortex. TLS is comparable to the 4-strand hamstring technique for clinical outcomes and safety. 13 Unlike the 4-strand hamstring technique, which uses a suspensory cortical button on the femoral side and a screw for the tibia to hold the graft, TLS fixation uses screws to secure the tapes. Although this may be considered an advantage because it preserves the graft-screw interface, softer screws may be more fragile in dense cortical bone during application.
The TLS-technique graft diameter and screw size are independent. The outer cortices of the femur and tibia are drilled with a 4.5-mm drill bit but tapped with a standard tapping device before passing the graft. The number of turns of the conical tap defines the depth of the screw. This aspect of the TLS technique may place pressure on the screw and may cause screw breakage in PEEK and bioabsorbable screws. The reported rate of intraoperative screw breakage with bioabsorbable screws is between 0.3% and 16.7%. 22 In our study, the overall rate of screw breakage was 2.7%, with 1 broken screw in the TLS-P and 13 in the TLS-B groups.
In a recent review of the literature on the risk factors of graft retear, Shen et al 18 reported that the 3 major sources of risk of retear were technical, patient, and knee joint-related. The rate of knee joint-related problems was low in that study, and the patients were young and athletic.
Limitations
There are certain limitations to this study. First, although the data were collected prospectively, this was a retrospective study with consecutive, nonrandomized data from heterogeneous groups. Also, the rate of complications was low and distributed among the 3 groups, making statistical validation difficult. Evaluating risk factors was also difficult because of the limited number of events and categories. The number of failures and complications could increase over time, which this study could not address. On the other hand, this study evaluated 1042 screws in 521 patients with the same type of fixation in both the tibia and the femur.
Conclusion
The results of this study confirmed the performance and safety of ACLR with the TLS system. There were no differences in the intraoperative or postoperative clinical or functional results between titanium, PEEK, and bioabsorbable screws with the reconstruction system. Two-year postoperative results showed that the TLS ACLR system was an acceptable option using all 3 fixation materials, with overall retear and intraoperative complication rates of 4.4% and 4.8%, respectively, and a patient satisfaction rate of 89.6%.
Supplemental Material
Supplemental material, sj-pdf-1-ojs-10.1177_23259671241258505 for Effect of Different Screw Materials on ACL Reconstruction With the Tape Locking Screw Technique: A Retrospective Study From the FAST Cohort by Hasan Basri Sezer, Yoann Bohu, Alexandre Hardy, Adam Coughlan and Nicolas Lefevre in Orthopaedic Journal of Sports Medicine
Footnotes
Final revision submitted November 9, 2023; accepted December 10, 2023.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by Pitie-Salpetriere University Hospital.
ORCID iD: Hasan Basri Sezer  https://orcid.org/0000-0002-9995-2620
https://orcid.org/0000-0002-9995-2620
Supplemental material: Supplemental Material for this article is available at https://journals.sagepub.com/doi/full/10.1177/23259671241258505#supplementary-materials.
References
- 1. Andernord D, Björnsson H, Petzold M, et al. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register on 13,102 patients. Am J Sports Med. 2014;42(7):1574-1582. [DOI] [PubMed] [Google Scholar]
- 2. Arama Y, Salmon LJ, Sri-Ram K, et al. Bioabsorbable versus titanium screws in anterior cruciate ligament reconstruction using hamstring autograft: a prospective, blinded, randomized controlled trial with 5-year follow-up. Am J Sports Med. 2015;43(8):1893-1901. [DOI] [PubMed] [Google Scholar]
- 3. Ayzenberg M, Arango D, Gershkovich GE, et al. Pullout strength of a novel hybrid fixation technique (Tape Locking Screw™) in soft-tissue ACL reconstruction: a biomechanical study in human and porcine bone. Orthop Traumatol Surg Res. 2017;103(4):591-595. [DOI] [PubMed] [Google Scholar]
- 4. Cohen D, Yao PF, Uddandam A, de Sa D, Arakgi ME. Etiology of failed anterior cruciate ligament reconstruction: a scoping review. Curr Rev Musculoskelet Med. 2022;15(5):394-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chevallier R, Klouche S, Gerometta A, et al. Bioabsorbable screws, whatever the composition, can result in symptomatic intra-osseous tibial tunnel cysts after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:76-85. [DOI] [PubMed] [Google Scholar]
- 6. Chen W, Li H, Chen Y, Jiang F, Wu Y, Chen S. Bone-patellar tendon-bone autografts versus hamstring autografts using the same suspensory fixations in ACL reconstruction: a systematic review and meta-analysis. Orthop J Sports Med. 2019;7(11):2325967119885314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Collette M, Cassard X. The Tape Locking Screw technique (TLS): a new ACL reconstruction method using a short hamstring graft. Orthop Traumatol Surg Res. 2011;97(5):555-559. [DOI] [PubMed] [Google Scholar]
- 8. Emond CE, Woelber EB, Kurd SK, Ciccotti MG, Cohen SB. A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: a meta-analysis. J Bone Joint Surg Am. 2011;93(6):572-80. [DOI] [PubMed] [Google Scholar]
- 9. Li X, Yan L, Li D, et al. Failure modes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Int Orthop. 2023. ;47(3):719-734. [DOI] [PubMed] [Google Scholar]
- 10. Luo Y, Chao Z, Wang J, et al. Clinical translation and challenges of biodegradable magnesium-based interference screws in ACL reconstruction. Bioact Mater. 2021;6:(10)3231-3243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mascarenhas R, Saltzman BM, Sayegh ET, et al. Bioabsorbable versus metallic interference screws in anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:561-568. [DOI] [PubMed] [Google Scholar]
- 12. McDermott E, DeFoor MT, Blaber OK, Aman ZS, DePhillipo NN, Dekker TJ. Biomechanical comparison of anterior cruciate ligament reconstruction fixation methods and implications on clinical outcomes. Ann Joint. 2023;8:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Orfeuvre B, Pailhé R, Sharma A, et al. Independent clinical appraisal of the Tape Locking Screw (TLS®) anterior cruciate ligament reconstruction technique compared with the hamstring graft technique with a minimum of 12-month follow-up. Eur J Orthop Surg Traumatol. 2019;29(6):1271-1276. [DOI] [PubMed] [Google Scholar]
- 14. Özbek EA, Winkler PW, Nazzal EM, et al. Failure rates and complications after multiple-revision ACL reconstruction: comparison of the over-the-top and transportal drilling techniques. Orthop J Sports Med. 2023;11(7):23259671231186972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peez C, Greßmann M, Raschke MJ, et al. The bone bridge for tibial ACL graft fixation: a biomechanical analysis of different tibial fixation methods for ACL reconstruction. Orthop J Sports Med. 2023;11(1):23259671221143478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pereira VL, Medeiros JV, Nunes GRS, et al. Tibial-graft fixation methods on anterior cruciate ligament reconstructions: a literature review. Knee Surg Relat Res. 2021;33:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sharma P, Baghel A, Keshav K, et al. Functional outcomes of anterior cruciate ligament reconstruction using titanium adjustable loop button and poly-l-co-dl-lactic acid-beta tricalcium phosphate (PLDLA-bTCP) interference screws: a single-center, retrospective, observational study. Cureus. 2023;15(2):e34542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shen X, Qin Y, Zuo J, et al. A systematic review of risk factors for anterior cruciate ligament reconstruction failure. Int J Sports Med. 2021;2(8):682-693. [DOI] [PubMed] [Google Scholar]
- 19. Shumborski S, Heath E, Salmon LJ. A randomized controlled trial of PEEK versus titanium interference screws for anterior cruciate ligament reconstruction with 2-year follow-up. Am J Sports Med. 2019;47(10):2386-2393. [DOI] [PubMed] [Google Scholar]
- 20. Speziali A, Delcogliano M, Tei M, et al. Fixation techniques for the anterior cruciate ligament reconstruction: early follow-up. A systematic review of level I and II therapeutic studies. Musculoskelet Surg. 2014;98(3):179-187. [DOI] [PubMed] [Google Scholar]
- 21. Sundaraj K, Salmon LJ, Heath EL, et al. Bioabsorbable versus titanium screws in anterior cruciate ligament reconstruction using hamstring autograft: a prospective, randomized controlled trial with 13-year follow-up. Am J Sports Med. 2020;48(6):1316-1326. [DOI] [PubMed] [Google Scholar]
- 22. Watson J N, McQueen P, Kim W, Hutchinson MR. Bioabsorbable interference screw failure in anterior cruciate ligament reconstruction: a case series and review of the literature. Knee. 2015;22(3):256-261. [DOI] [PubMed] [Google Scholar]
- 23. Xu B, Yin Y, Zhu Y, Yin Y, Fu W. Comparison of bioabsorbable and metallic interference screws for graft fixation during ACL reconstruction: a meta-analysis of randomized controlled trials. Orthop J Sports Med. 2021;9(8):23259671211021577. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ojs-10.1177_23259671241258505 for Effect of Different Screw Materials on ACL Reconstruction With the Tape Locking Screw Technique: A Retrospective Study From the FAST Cohort by Hasan Basri Sezer, Yoann Bohu, Alexandre Hardy, Adam Coughlan and Nicolas Lefevre in Orthopaedic Journal of Sports Medicine