Abstract
Background
Within the NICU, there is a delicate equilibrium between providing assistance to parents by nurses and prioritising family-centred care (FCC). The FCC assumes the role of a mediator, effectively conveying compassion. The intricate dynamics between FCC, parental nurse support, and parental stress in neonatal intensive care units (NICUs) necessitate comprehensive investigation.
Objective
This study examines the mediating effect of FCC on the relationship between parental nurse support and parental stress in NICUs.
Methods
This cross-sectional observational study used convenience sampling to select 223 parents (202 mothers) from Mansoura City hospitals in Egypt. Data were collected using the Nurse Parent Support Tool (NPST), Family-Centered Care Self-Assessment Tool (FCCS-NICU), and the Parental Stressor Scale: NICU (PSS: NICU). Mediation analysis was used to examine the relationships between variables.
Results
Nurse support was positively associated with FCC (β = 0.81, p < 0.001) and negatively related to parental stress (β=-1.156, p < 0.001). FCC was found to reduce parental stress (β=-0.18, p < 0.001). Mediation analysis confirmed that FCC partially mediated the relationship between nurse support and parental stress (indirect effect β = 0.145, 95% CI: 0.055–1.007).
Conclusions
This study highlights a significant association in the mediating role of FCC between nurse support and parental stress. Strengthening FCC practices can be an effective strategy for nurses to support parents and alleviate their stress in NICU settings.
Implications to practice
NICUs should implement FCC-oriented training for nurses, foster a culture that supports FCC principles, and develop policies to establish FCC as a cornerstone of neonatal care.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12912-024-02258-4.
Keywords: Family-centered care, Nurse support, Parental stress, Neonatal intensive care, Mediation analysis
Introduction
In NICUs, parental nurse support is crucial in enhancing the well-being and resilience of parents facing the challenges associated with their newborn’s critical care. This support encompasses emotional, informational, and practical dimensions, extending beyond traditional clinical duties to holistically address the needs of families during a neonate’s early and critical stages of life [1]. Given the multifaceted nature of this support, integrating a structured approach that emphasises collaboration and holistic care becomes essential. This is where the FCC comes into play as a cornerstone of a contemporary approach to neonatal care.
FCC is a healthcare approach that ensures the child’s and family’s needs are prioritised at the centre of care planning and delivery. This approach emphasises collaboration between families and healthcare providers, respecting family preferences, and supporting family involvement in decision-making [2]. In the NICU setting, where the health and development of the neonate are intricately linked to the family’s emotional and psychological state, FCC is particularly vital. By fostering a supportive environment, FCC helps parents navigate the NICU experience and strengthens their involvement in their infant’s care [3]. Thus, most health services recognise FCC as essential to maintaining and strengthening family roles in their children’s recovery plan and addressing their needs by providing care [4–7].
Recent research has increasingly underscored the importance of FCC in enhancing the well-being of both parents and infants in NICU settings. For example, a systematic review and meta-analysis by Ding et al. found that FCC interventions significantly improved outcomes such as weight gain, parental satisfaction, knowledge, and skills, and reduced parental anxiety, depression, and stress in parents of preterm infants [8]. Similarly, Kocakabak et al. highlighted the diversity and inconsistency in outcome measures and time points in studies testing FCC interventions in neonatal care, suggesting the need for standardized outcome sets to better evaluate these interventions [9]. Furthermore, Dall’Oglio et al. examined FCC practices across Italian NICUs, revealing variability in the implementation of FCC and emphasizing the necessity of involving parents as partners in the care team [10]. Lastly, a study by He et al. demonstrated that Family Integrated Care (FIC), a form of FCC that involves parents directly in care delivery, can improve clinical outcomes for preterm infants in Chinese NICUs, including increased breastfeeding rates and weight gain [11]. These studies collectively illustrate the critical role of FCC in shaping parental experiences and improving outcomes for both infants and parents in NICU settings.
Moreover, an integrative review investigating the current knowledge of the FCC model and its application in caring for preterm newborns (PN) in NICUs. The review revealed that FCC promotes the integration of health equipment and family, making parents primary caregivers and enabling earlier hospital discharge. This humanised care approach improved healthcare outcomes and suggested that health managers adapt services to meet the needs of families and PNs [12].
Additionally, a prospective multicenter cohort study compared the Family Integrated Care (FICare) model with standard neonatal care (SNC) and found that fathers in the FICare model experienced less stress and had higher participation scores. The study concluded that the FICare model, which supports active parental participation, significantly improved paternal mental health and bonding with their newborns. This highlights the beneficial effects of interventions within the overall model of FCC [13]. This new research offers a solid foundation for comprehending the possible ways in which the FCC can lessen the stress that parents experience in NICUs. They corroborate our study’s justification for looking into the mediation function of FCC in the connection between parental stress and parental nursing support. In light of these findings, our study aims to add to the increasing evidence supporting FCC as a common procedure in NICU settings.
The theoretical foundation for this study is primarily grounded in Peplau’s Interpersonal Relations Theory, which underscores the significance of the nurse-patient relationship [14, 15]. This theory highlights the therapeutic potential of nurse-parent interactions, which are central to FCC practices. By engaging in compassionate and empathetic communication, nurses create a trusting atmosphere that empowers parents to participate actively in their neonate’s care [16]. According to Hildegard Peplau’s Interpersonal Relations Theory, such interactions are fostered through deliberate, evidence-based practices emphasising compassion, empathy, and open communication—foundational to therapeutic nursing relationships. Nurse support facilitates FCC by creating an atmosphere of trust and safety where parents feel valued and empowered to take an active role in caring for their neonates [14]. Social Support Theory further complements the FCC framework by suggesting that nurse-provided support is a crucial buffer against stress, promoting effective coping mechanisms and enhancing psychological resilience among parents [17]. According to this theory, nurses’ emotional, informational, and practical support NICUs align closely with FCC principles, emphasising collaboration, respect for family preferences, and active family involvement in decision-making processes [18].
In the NICU setting, parents often experience heightened levels of stress and anxiety due to the critical condition of their newborn and the unfamiliar, high-tech environment of the NICU. Nurses are pivotal in mitigating these stressors through compassionate and empathetic care practices. Emotional support from nurses involves actively listening to parents, acknowledging their emotions, and providing reassurance during challenging moments. This kind of support helps alleviate immediate stress, fostering a sense of trust and partnership between nurses and parents, which is crucial for effective FCC [19]. Furthermore, nurses provide informational support by educating parents about their infant’s medical condition, treatment plans, and progress. Clear and accurate information empowers parents to make informed decisions and actively participate in their child’s care journey. This support aspect is integral to FCC principles, as it promotes transparency and shared decision-making, ensuring that parents feel knowledgeable and involved in their infant’s healthcare [20]. Consequently, integrating emotional and informational support within the FCC framework illustrates how Social Support Theory operationalises through nurse-parent interactions, enhancing parental resilience and engagement in NICU care [17].
While the two constructs, nurse support and FCC, may appear similar, their scope and focus differ. Nurse support encompasses direct actions and interactions that provide parents emotional, informational, and practical assistance [14, 18]. In contrast, the FCC represents a broader approach to care that integrates these supportive actions into a comprehensive, family-oriented framework [4]. Empirical studies, such as those conducted by Maleki et al. (2022), highlight the critical roles of nurse support and FCC in enhancing parental experiences in NICUs. Furthermore, nurses who utilise supportive communication offer emotional reassurance and encourage parental involvement, effectively bridging clinical care with the comprehensive family engagement envisioned by FCC practices [21]. This theoretical perspective is reinforced by research indicating that increased parental satisfaction with nurse support correlates with higher perceptions of FCC implementation, leading to improved psychosocial outcomes for both parents and infants [22]. Moreover, empirical studies have linked FCC practices with reduced parental anxiety and enhanced competence in caregiving roles, theoretically contributing to the optimal developmental trajectory of hospitalised infants [23].
In addition to the critical role of FCC in supporting parents within NICU settings, understanding parental stress is paramount. Parental stress within the NICU is understood through theoretical constructs that describe stress as a psychological and physiological response to perceived environmental challenges or threats [24, 25]. The unique and often unexpected journey of having a newborn in NICU care introduces a host of potential stressors, including the infant’s medical condition, the unfamiliar high-tech environment, and the alteration of parental roles. According to the Transactional Model of Stress and Coping, parental stress in the NICU evolves as parents appraise the situation and interact with their coping resources [25]. In this challenging environment, the FCC emerges as a pivotal resource, offering essential emotional support and crucial information and facilitating meaningful involvement for parents, all of which help alleviate stress and enhance psychological well-being [16, 26, 27].
Grounded in Social Support Theory, FCC provides a structured framework that integrates emotional, informational, and practical support for families in the NICU. This approach aligns with the principles of collaboration, respect for family preferences, and active involvement in decision-making processes. Theoretical foundations such as Peplau’s Interpersonal Relations and House’s Social Support Model further bolster the understanding of how nurse behaviours influence psychosocial factors, including parental well-being and the overall NICU experience [28]. This study aims to bridge empirical evidence with theoretical models by synthesising these constructs, explicitly exploring how nurse support and FCC contribute to alleviating parental stress. This research fills theoretical gaps and lays a foundation for targeted interventions to enhance FCC practices in NICU settings. Thus, this study examines the mediating effect of FCC on the relationship between parental nurse support and parental stress in NICUs, with three hypotheses serving as the basis for this study. (1) Improved parental nurse support is positively associated with the level of FCC experienced by parents in the NICU; (2) Improved FCC is negatively associated with the parental stress experienced by parents in the NICU; and (3) FCC will mediate the relationship between parental nurse support and parental stress.
Methods
Study design
This cross-sectional observational study explored the relationships between parental nurse support (independent variable), FCC (mediating variable), and parental stress (dependent variable) in NICUs, following the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines [29].
Setting and participants
This study was conducted at the NICUs at Mansoura University Children’s Hospital (MUCH) and Mansoura International Hospital, which provides 24-hour service and accepts infants requiring level II and III specialised care. The nurse-to-patient ratio in these units is maintained at 1:1–2, ensuring personalised and attentive care. In line with Peplau’s emphasis on the importance of nurse-patient interactions, both NICUs have implemented structured supervision and ongoing training programs for nurses to enhance their support capabilities and interaction skills with parents. Convenience sampling was employed to recruit parents of premature infants born before 37 weeks gestational age (GA) and hospitalised in the NICU for longer than seven days due to medical conditions. Parents with previous neonatal deaths in the NICU and with neonatal admissions of less than 24 h were excluded. Parents of infants born in or transferred from other hospitals were excluded from the study due to uncertain prenatal or perinatal conditions.
The parameters of three latent constructs, 81 observed variables, 0.3 expected effect size, 0.95 power, and 0.05 desired probabilities were used to estimate the sample size using a calculator for structural equation modelling software [30]. A sample size of 119 parents was required, and an estimated 20% drop-out rate was calculated for the initial study population of 243 parents. Two hundred twenty-six parents returned the questionnaire out of the 243 parents invited to participate in the study. Three parents’ questionnaires were not included because of incomplete information. Thus, 223 parents made up the final sample, and their effective completion rate was 91.8%.
Tools of data collection
The parents’ demographic data form included five questions regarding age, gender, education, residence, and employment status. The NPST was adapted fromHouse, (1987) ; Miles et al., (1999) to assess parents’ perceptions of nursing support during their infant’s hospitalisation [31, 32]. The NPST included 21 items and assessed four areas of nursing support provided for the parents: (a) nine items covered supportive communication and provision of information related to the infant’s illness, treatments, care, and related issues; (b) four items included parental esteem support focused on respecting, enhancing, and supporting the parental role during the infant’s hospitalisation; (c) three items covered emotional support used to help parents cope with the emotional responses and needs related to the infant’s illness; and (d) where five items included caregiving support, focusing on the quality of care provided to the infant. On a five-point rating scale, parents indicated how much nursing support they received from the staff, from 1, which was ‘almost never’, to 5, which was ‘almost always’. An average was taken out for the scores where higher scores indicated more incredible perceived support. The Arabic version of NPST was validated by Rabie et al. (2021), showing high internal consistency and multidimensional structure for mothers of neonates, suggesting that Egyptian NICUs have stressors similar to Western ones [24–27]. Internal consistency during the current study was high (α = .89).
The FCCS-NICU, developed by Akkaş and Geçkil (2023), is based on the FCC practices. This practice comprises four subscales: Dignity and Respect, Information Sharing, Participation in Care, and Collaboration with the Family. Literature analysis, expert interviews, and validity and reliability testing were used to create the 29-item, 4-subscale scale as follows: The Dignity and Respect subscale includes seven items (1–7), Information Sharing has nine items (8–16), Care Participation comprises five items (17–21), and Collaboration with the Family consists of 8 items (22–29). A 5-point Likert scale was used (1: strongly disagree, 2: disagree, 3: undecided, 4: agree, 5: strongly agree), and subscale and total scores were calculated by dividing the total score by the number of items. Scores ranged from 1 to 5, with higher scores indicating increased or positively improved FCC [33].
Researchers translated the FCCS-NICU into Arabic following the translation back translation technique [34]. Initially, the researcher translated the FCCS-NICU scale from English to Arabic. Subsequently, a back-translation from Arabic to English was conducted by a proficient translator. These two versions were compared to the original English scale for accuracy, and necessary corrections were implemented to ensure close alignment between the translated version and the original English scale. Following this, a panel of five nursing professors reviewed the translation to ensure terminological equivalence and clarity, and some words were adjusted to fit the Egyptian context. The translated scale showed a high content validity index (CVI = 0.90). The confirmatory factor analysis results indicated that all constructs used in this study had factor loadings that exceeded the recommended threshold of 0.5 [35], confirming the structural integrity and validity of the translated tool. The questionnaire’s reliability was verified in terms of Cronbach’s α, which was 0.94.
The PSS: NICU is an adaptation of Miles et al., (1993) designed to evaluate staff interactions, behaviour, and communication [36]. This scale is used to identify sources of stress experienced by parents by presenting situations for them to assess. The scale consists of 26 items distributed across three subscales: Sights and Sounds of the Environment (5 items), Infant’s Appearance (14 items), and Parental Role Alterations (7 items). Parents rate each item on a 5-point scale (1: not at all stressful, 2: stressful, 3: moderately stressful, 4: very stressful, 5: extremely stressful). The Arabic version of the PSS: NICU, translated and assessed for psychometric properties by Rabie et al., (2021), demonstrated high internal consistency, confirming the multidimensional structure of the scale [37]. In the current study, the internal consistency of the PSS: NICU was found to be high (α = 0 0.94).
Data collection
Data was collected from August to October 2023. Permission and support were sought from the hospital administrators by explaining our research and requesting approval to distribute a survey. After receiving approval, we interviewed each of the two NICU managers, during which we presented the research’s purpose, significance, and methodology, obtained consent, and secured their assistance.
Prior to the study, 19 parents with the same inclusion criteria were chosen for a pre-test to determine the study’s validity and were excluded from the primary investigation. These pre-tested parents were debriefed after finishing the survey to get their input on the design and questions in the questionnaires. The parents in the pre-test attested to the survey’s transparency, and none reported feeling overly tired by it. The time taken to complete the survey ranged from 15 to 20 min. The data from the pre-test underwent reliability analysis, revealing that Cronbach’s alpha for the modelled constructs was above 0.7 [38]. Subsequently, the researcher outlined the study’s objectives and ensured confidentiality, anonymity, and voluntary participation for the rest of the participants. The researcher interviewed them during work hours, and the parents completed the questionnaires.
Data analysis
The data analysis was conducted using IBM SPSS 27 with AMOS 23. Descriptive statistics were employed to present the characteristics of both parents and the study variables. Parametric tests were used as the data showed normal distribution according to the Kolmogorov-Siminouv test. Variables’ multicollinearity was assessed, confirmed tolerance was > 0.1, and the variance inflation factor (VIF) was < 3, showing no multicollinearity. Pearson’s correlation was used to analyse bivariate correlations between the study variables. To investigate differences in NPST, FCCS-NICU, and PSS: NICU based on sample characteristics, independent t-tests and analysis of variance (ANOVA) were applied.
Preliminary analysis
The hypothesised model was assessed using AMOS’s structural equation modelling (SEM). Demographic characteristics were not entered into the SEM because there was no difference in the dependent variable (Appendix 1). The confirmatory factor analyses (CFA) findings indicated that the model fit the data well. The tests applied in this study were the chi-square (χ2) test of model fit, with a ratio of χ2/df < 3 representing a good model fit. Other tests used were the comparative fit index (CFI ≥ 0.95), Tucker–Lewis index (TLI ≥ 0.95), and root mean square error of approximation (RMSEA < 0.08). The model fit the data well with χ2/df = 2.6, incremental fit index (IFI) = 0.93, TLI = 0.92, CFI = 0.93, and RMSEA = 0.071 [39, 40].
To ensure the adequacy of our sample for the CFA, the Kaiser–Meyer–Olkin (KMO) test and the Bartlett test of sphericity were conducted. The KMO measure of sampling adequacy was 0.879, and the Bartlett test of sphericity was significant (p < 0.001), indicating that our sample was suitable for conducting the CFA. Following the recommendation of Kelin’s study, we ensured that our sample size exceeded 200 parent participants, which aligns with best practices for conducting structural equation modelling, including CFA [39, 40]. Our study involved 223 parents, which satisfies this criterion and supports the reliability of our CFA results. The study underwent validity and reliability assessments, and statistical significance was set at two-tailed P values of < 0.05. In order to inspect Common method variance (CMV) in the data, Harman’s single-factor test was used, and the total variance explained by one factor was 34.7%, falling below the threshold of 50%, indicating no significant CMV [41].
Results
Demographic data of the parents
Table 1 shows that females represented the majority of parents; about four-fifths were aged ≤ 30 years.
Table 1.
A comprehensive overview of the parents’ demographics (n = 223)
| Characteristic | Category | n | % |
|---|---|---|---|
| Gender | Male | 21 | 9.4 |
| Female | 202 | 90.6 | |
|
Age (years); mean ± SD (32.56 ± 8.37) |
≤ 30 | 177 | 79.4 |
| > 30 | 46 | 20.6 | |
| Educational level | Primary | 70 | 31.4 |
| Intermediate | 114 | 51.1 | |
| High | 39 | 17.5 | |
| Residence | Urban | 119 | 53.4 |
| Rural | 104 | 46.5 | |
| Employment status | Employee | 95 | 42.6 |
| Not employed | 128 | 57.4 |
Table 2 provides significant correlations between NPST and FCCS-NICU, where a positive correlation was seen (r = 0.783, p < 0.01), indicating that higher nurse support is linked with greater FCC perceptions. NPST and PSS: NICU were negatively correlated (r = − 0.857, p < 0.01), suggesting that increased nurse support correlates with reduced parental stress. Furthermore, FCCS-NICU and PSS: NICU scores were negatively correlated (r = − 0.685, p < 0.01), showing that higher perceptions of FCC are associated with lower parental stress. These correlations highlight the importance of nurse support and FCC in mitigating parental stress in neonatal intensive care settings.
Table 2.
Descriptive statistics and correlation between subdomains and total scores of studied (n = 223)
| Variables | M (SD) | 1 | 2 | 3 |
|---|---|---|---|---|
| 1. Total NPST | 3.36 (0.82) | 1 | r = 0.783** | r = -0.857** |
| 2. Total FCCS-NICU | 2.81 (0.45) | 1 | r = -0.685** | |
| 3. Total PSS: NICU | 2.62 (0.68) | 1 |
r = Pearson Correlation, **. Correlation is significant at the 0.01 level (2-tailed), NPST = Nurse Parent Support Tool, FCCS-NICU = family-centered care Self Asseement tool. PSS: NICU = Parental Stressor Scale in NICU.
Measurement model
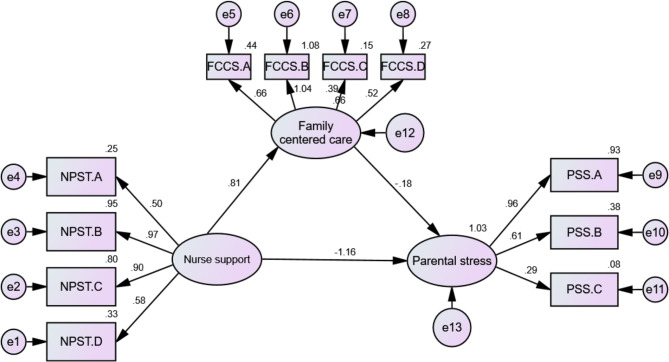
Table 3; Fig. 1 show a significant positive direct effect from NPST to FCCS-NICU (β = 0.81, p < 0.001). The effect size was substantial, with a tight 95% CI (0.763 to 0.934), which does not straddle zerom suggesting a direct relation beween NPST and FCCS-NICU scores. The path from FCCS-NICU to PSS: NICU is significantly negative (β=−0.18, p < 0.001) with a confidence interval ranging from − 1.022 to -0.070, implying higher FCCS-NICU scores are associated with lower PPS scores. A significant negative direct effect was found from NPST to PSS: NICU (β=−1.156, p < 0.001) with a confidence interval between − 2.139 and − 1.056, suggesting that increases in NPST are linked with significant decreases in PPS.
Table 3.
Direct, indirect, and total effects analysis of the mediation model (N = 223)
| Path | β | SE | t | P | 95% CI |
|---|---|---|---|---|---|
| Lower/Upper | |||||
| NPST to FCCS-NICU | 0.81 | 0.062 | 7.346 | < 0.001 | 0.763 /0.934 |
| FCCS-NICU to PSS: NICU | − 0.18 | 0.110 | -4.186 | < 0.001 | -1.022 -/-0.070 |
| NPST to PSS: NICU | -1.156 | 0.171 | -9.811 | < 0.001 | -2.139 /-1.056 |
| Indirect effect of NPST on PSS: NICU | 0.145 | 0.055/1.007 | |||
| Total effect | -1.011 | -1.108 /-0.982 |
NPST = Nurse Parent Support Tool, FCCS-NICU = family-centered care Self Asseement tool. PSS: NICU = Parental Stressor Scale in NICU, β = Beta coefficient, SE = Standard Error, t = t-statistic value, P = Significance level, CI = confidence Interval.
Fig. 1.
Mediation analysis
The indirect effect of NPST on PPS through FCCS-NICU was positive (β = 0.145), with a confidence interval ranging from 0.055 to 1.007. This indicates that FCCS-NICU partially mediates the relationship between NPST and PSS: NICU, attenuating the negative relationship. The total effect of NPST on PSS: NICU was negative (β=−1.011), with a 95% CI of -1.108 to − 0.982, further confirming the strong negative relationship between NPST and PSS: NICU when considering both direct and indirect paths.
Discussion
This study investigated the complex relationship between nurse support, FCC, and parental stress within NICUs, providing significant insights into the intricate dynamics between parental nurse support, FCC, and parental stress in NICUs. The findings reveal that increased parental nurse support is associated with higher levels of FCC and reduced parental stress. Moreover, the FCC partially mediates the relationship between parental nurse support and parental stress, underscoring the critical role of the FCC in mitigating stress among parents in NICUs. Our results strongly supported all three hypotheses.
As for hypothesis 1, the correlation between the NPST and the FCCS-NICU was significantly positive, indicating that higher nurse support is linked with greater perceptions of FCC. Additionally, the direct effect of NPST on FCCS-NICU was significant, with a substantial effect size and a confidence interval that did not straddle zero. These findings suggest that parental support from nurses directly enhances the level of FCC perceived by parents in NICUs. These results could be explained by the fact that when nurses actively support and engage with parents, it fosters a collaborative environment where parents feel more involved in their child’s care. This increased involvement and collaboration are key elements of FCC, enhancing parents’ overall perception of the care provided.
The positive correlation between NPST scores and FCC practices highlights a crucial link in the NICU environment. Nurse support, recognised as a keystone of quality neonatal care, is pivotal in enhancing FCC. Nurses’ supportive interactions contribute significantly to FCC implementation and effectiveness, aligning with literature emphasising their integral role in adopting FCC principles [42, 43] improving neonatal outcomes and enhancing parental satisfaction [44].
The correlation between FCCS-NICU and the Parental Stressor Scale (PSS): NICU was significantly negative, indicating that higher perceptions of FCC are associated with lower parental stress as per our second hypothesis. The direct effect of FCCS-NICU on PSS: NICU was also significantly negative. These results underscore the importance of FCC in reducing parental stress in NICU settings, which could be attributed to the emphasis FCC places on including parents in the care process, providing them with more information, involvement, and control over their infant’s care. This sense of empowerment and active participation can alleviate feelings of helplessness and anxiety, thereby reducing overall stress levels among parents.
The findings regarding the negative correlation between nurse support and parental stress in these studies are consistent with those of previous studies. For instance, several studies, such asAlbayrak & Büyükgönenç, (2022) demonstrated the crucial role of nurse support in enhancing FCC practices and reducing parental stress in NICUs. Furthermore, identifying the strong negative correlation between ‘Parental Esteem Support’ and the ‘Sights and Sounds’ stressor opens new theoretical avenues [45] that specific components of nurse support may have distinct impacts on various stressors in the NICU environment. This aspect has not been extensively explored in previous theoretical models and could lead to refining existing theories or developing new models that more accurately capture the complexities of parent-nurse interactions and their effects in the NICU setting.
The direct effect of NPST on PSS: NICU was significantly negative, indicating that increased nurse support is associated with reduced parental stress, supporting hypothesis 3. Furthermore, the indirect effect of NPST on PSS through FCCS-NICU was positive, indicating partial mediation, suggesting that while nurse support directly reduces parental stress, FCC also plays a crucial role in this relationship by partially mediating the effect of nurse support on stress reduction. Overall, the total effect of NPST on PSS: NICU was negative, confirming the strong negative relationship between nurse support and parental stress when considering both direct and indirect paths. These findings highlight nurse support and FCC’s critical role in alleviating parental stress in NICU settings. This can be explained by the comprehensive approach of FCC, where the emotional, informational, and practical support nurses provide helps parents feel more competent and less overwhelmed. Additionally, the FCC’s focus on establishing trusting relationships between parents and healthcare providers can further reduce parental stress by creating a supportive and reassuring environment.
This connection has been less explicitly documented in earlier research. Our study provides a more comprehensive understanding of the impact of nurse support on parental experiences in NICUs and the interplay between FCC, nurse support, and parental stress in neonatal care. By establishing FCC as a mediator, our research supports and extends the theoretical framework that views FCC not just as a care practice but as an active agent in alleviating parental stress. This aligns with the tenets of FCC theory, that care practices focused on the family can significantly improve health outcomes and satisfaction [4, 46]. Delving deeper into the role of the FCC as a mediator, our study reveals that the application of FCC practices serves as a conduit through which nurse support translates into reduced parental stress in NICU settings. This mediating role of FCC aligns with the growing body of evidence emphasising the stress-buffering effect of FCC in neonatal care [47, 48]. These studies have consistently shown that when parents perceive a high level of FCC, including aspects such as dignity, respect, and information sharing, their stress levels decrease.
Limitations and implications for Future Research
Some limitations were identified in the study, one being the study’s cross-sectional design. While this approach offers a snapshot of the relationships between variables at a specific time, it does not allow for assessing causality or how these relationships may evolve. This limitation is particularly relevant in the context of NICUs, where the dynamics of nurse support, FCC, and parental stress could change significantly as the neonatal and family situations evolve. Additionally, our study’s sample size and demographic scope were limited to parents from Mansoura City hospitals, which constrains the generalizability of our findings. While the sample size was adequate to establish statistical significance, a more extensive and diverse sample would provide a more robust and generalised understanding of the studied relationships. The geographical limitation to a single city means that our findings may not fully represent the experiences of parents and nurses in different cultural, socioeconomic, or geographical settings.
Future studies should consider addressing these limitations. Longitudinal studies, for instance, would be precious in understanding how nurse support, FCC, and parental stress. Furthermore, future research could also benefit from exploring additional variables that might influence the relationship between nurse support, FCC, and parental stress, such as the severity of the neonate’s condition, the duration of the NICU stay, or the existence of prior traumatic experiences could significantly impact these dynamics. Investigating these variables would contribute to a more comprehensive understanding of the factors that affect parental experiences in NICUs, thereby informing more tailored and effective interventions. Additionally, expanding the research to include diverse geographical locations and a broader cultural and socioeconomic context would enhance the generalizability and applicability of the findings, ultimately contributing to the global body of knowledge on family-centred neonatal care.
Implication for nursing practice
The findings from our study highlight the crucial role of FCC in nursing practice within NICUs, emphasising the need for FCC-oriented training for nurses and policy integration. Training programs focused on FCC principles can equip nurses with essential skills to effectively engage with families, fostering an environment supporting neonates and their families, which is vital in the high-stress NICU setting. This approach will improve care quality and enhance family experiences during critical periods. At a policy level, these findings suggest developing guidelines prioritising FCC in neonatal care, advocating for policies that mandate regular FCC training, establishing nurse-family interaction guidelines, and promoting family involvement in neonatal care. Such policy implementations could lead to better infant developmental outcomes, shorter hospital stays, and increased parental satisfaction.
Conclusion
In conclusion, our study significantly contributes to understanding FCC in NICUs by demonstrating a positive correlation between NPST and the implementation of FCC, signifying that enhanced nurse support will likely bolster FCC practices. Conversely, our results reveal a significant negative association between nurse support and parental stress, highlighting the crucial role of nurses in alleviating parental anxiety in these high-stress environments. Most notably, our analysis identifies the FCC as a critical mediator in this dynamic, suggesting that the beneficial effects of nurse support on reducing parental stress are partly facilitated through strengthened FCC practices. Furthermore, the study illuminates an indirect noteworthy impact of NPST on parental stress via FCC, adding a new dimension to our understanding of how nurse support can impact parental experiences in NICUs. These findings may offer new insights into the dynamics of nurse-parent interactions and their impact on parental stress. The significance of our study lies in its potential to influence both practice and policy in neonatal care, the impact of such changes is profound, offering a pathway to better health outcomes and a more compassionate and family-inclusive approach to neonatal care.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are grateful for the facilities and other support given by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R447), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia. The authors would like to thank all of the responded parents for their cooperation.
Author contributions
AL, MAZ, and AA contributed significantly through Conceptualization, Methodology, and Investigation, focusing on the study’s design, planning, data acquisition, analysis, and interpretation. AA, HEE, SA, AE, and MAZ played a pivotal role in Writing - Original Draft, and alongside MAZ, in Writing - Review & Editing, with major contributions to the manuscript’s initial drafting and subsequent revisions. MM, HE, SA, and CB specifically contributed to the Writing - Original Draft of the Discussion section. Additionally, MAZ was responsible for Data Curation and final manuscript revisions. Collectively, all authors were involved in Project Administration and Validation, ensuring the project’s overall coordination, the accuracy and integrity of the work, and have given their final approval for the manuscript’s publication, agreeing to be accountable for all aspects of the work.
Funding
The authors extend their appreciation to Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R447), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Data availability
The datasets generated during and analyzed during the current study are not publicly available due to confidentiality agreements, but are available upon reasonable request from the corresponding author.
Declarations
Ethics approval and consent to participate
The Research Ethics Committee of the Faculty of Nursing, Mansoura University, approved the study (Ref. No. P. 0490). The parents provided informed consent via an online informed consent form. Our study followed the rules and procedures specified by Helsinki (DoH‑Oct2008) declarative formation. The study complied with all ethical requirements, including consent-taking, confidentiality and anonymity maintenance, adequate study information provision, assurance of parents’ ability to withhold at any moment without justifying, and data protection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sidek SM, Marup S, Zolkefli Y. Nurses’ view of the nature of the support given to parents in the neonatal intensive care unit. Belitung Nurs J. 2021;7:522–8. 10.33546/bnj.1668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carrington L, Hale L, Freeman C, Qureshi A, Perry M. Family-centred care for children with Biopsychosocial Support needs: a scoping review. Disabilities. 2021;1:301–30. 10.3390/disabilities1040022 [DOI] [Google Scholar]
- 3.Ramezani T, Hadian Shirazi Z, Sabet Sarvestani R, Moattari M. Family-centered care in neonatal intensive care unit: a concept analysis. Int J Community Based Nurs Midwifery. 2014;2:268–78. [PMC free article] [PubMed] [Google Scholar]
- 4.Kokorelias KM, Gignac MAM, Naglie G, Cameron JI. Towards a universal model of family centered care: a scoping review. BMC Health Serv Res. 2019;19:564. 10.1186/s12913-019-4394-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paraszczuk AM, Feeg VD, Betz CL, Mannino JE. Psychometric testing of family centered Care (FCC) instrument: a mixed methods analysis of pediatric nurses and their workplace perceptions of FCC. J Pediatr Nurs. 2021;61. [DOI] [PubMed]
- 6.Arabiat D, Whitehead L, Foster M, Shields L, Harris L. Parents’ experiences of Family Centred Care practices. J Pediatr Nurs. 2018;42. [DOI] [PubMed]
- 7.Kuo DZ, Houtrow AJ, Arango P, Kuhlthau KA, Simmons JM, Neff JM. Family-centered care: current applications and future directions in pediatric health care. Matern Child Health J. 2012;16. [DOI] [PMC free article] [PubMed]
- 8.Ding X, Zhu L, Zhang R, Wang L, Wang TT, Latour JM. Effects of family-centred care interventions on preterm infants and parents in neonatal intensive care units: a systematic review and meta-analysis of randomised controlled trials. Aust Crit Care. 2019;32:63–75. 10.1016/j.aucc.2018.10.007 [DOI] [PubMed] [Google Scholar]
- 9.Kocakabak C, van den Hoogen A, Rothfus M, Campbell-Yeo M, Kostenzer J, Axelin A, et al. Identifying outcomes and outcome measures in neonatal family-centered care trials: a systematic review. Pediatr Res. 2024. 10.1038/S41390-024-03293-2. 10.1038/S41390-024-03293-2 [DOI] [PubMed] [Google Scholar]
- 10.Dall’Oglio I, Mascolo R, Tiozzo E, Portanova A, Fiori M, Gawronski O, et al. The current practice of family-centred care in Italian neonatal intensive care units: a multicentre descriptive study. Intensive Crit Care Nurs. 2019;50:36–43. 10.1016/j.iccn.2018.07.005 [DOI] [PubMed] [Google Scholar]
- 11.He SW, Xiong YE, Zhu LH, Lv B, Gao XR, Xiong H et al. Impact of family integrated care on infants’ clinical outcomes in two children’s hospitals in China: a pre-post intervention study. Ital J Pediatr. 2018;44. [DOI] [PMC free article] [PubMed]
- 12.Gómez-Cantarino S, García-Valdivieso I, Moncunill-Martínez E, Yáñez-Araque B, Gurrutxaga MIU. Developing a family-centered Care Model in the neonatal Intensive Care Unit (NICU): a New Vision to Manage Healthcare. Int J Environ Res Public Health 2020. 2020;17(7197):17:7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Veenendaal NR, Van Der Schoor SRD, Broekman BFP, De Groof F, Van Laerhoven H, Van Den Heuvel MEN, et al. Association of a Family Integrated Care Model with Paternal Mental Health outcomes during neonatal hospitalization. JAMA Netw Open. 2022;5:e2144720–2144720. 10.1001/jamanetworkopen.2021.44720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peplau HE. Interpersonal relations in nursing: a conceptual frame of reference for psychodynamic nursing. Putnam; 1952.
- 15.Peplau HE. Interpersonal relations in nursing: a conceptual frame of reference for psychodynamic nursing. Springer Publishing Company; 1991.
- 16.Gómez-Cantarino S, García-Valdivieso I, Moncunill-Martínez E, Yáñez-Araque B, Ugarte Gurrutxaga MI. Developing a family-centered Care Model in the neonatal Intensive Care Unit (NICU): a New Vision to Manage Healthcare. Int J Environ Res Public Health. 2020;17. [DOI] [PMC free article] [PubMed]
- 17.Cutrona CE, Russell DW. Type of social support and specific stress: toward a theory of optimal matching. Social support: an interactional view. Oxford, England: Wiley; 1990. pp. 319–66. [Google Scholar]
- 18.House JS. Work stress and social support. Addison-Wesley Publishing Company; 1981.
- 19.El-Gazar HE, Zoromba MA, Zakaria AM, Abualruz H, Abousoliman AD. Effect of humble leadership on proactive work behaviour: the mediating role of psychological empowerment among nurses. J Nurs Manag. 2022;30:2689–98. 10.1111/jonm.13692 [DOI] [PubMed] [Google Scholar]
- 20.Uchino BN, Bowen K, Kent de Grey R, Mikel J, Fisher EB. Social support and physical health: Models, mechanisms, and opportunities. Principles and concepts of behavioral medicine: A global handbook. 2018;:341–72.
- 21.Maleki M, Mardani A, Harding C, Basirinezhad MH, Vaismoradi M. Nurses’ strategies to provide emotional and practical support to the mothers of preterm infants in the neonatal intensive care unit: a systematic review and meta-analysis. Womens Health (Lond). 2022;18:17455057221104674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lim S-J, Bang K-S. The perceptions and performance of family-centered care among pediatric nurses at a children’s hospital in South Korea: a descriptive study. Child Health Nurs Res. 2023;29:207–17. 10.4094/chnr.2023.29.3.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heidari H, Mardani-Hamooleh M. Nurses’ perception of family-centered care in neonatal intensive care units. J Pediatr Intensive Care. 2020;9:16–20. 10.1055/s-0039-1695060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lynch T, Davis SL, Johnson AH, Gray L, Coleman E, Phillips SR, et al. Definitions, theories, and measurement of stress in children. J Pediatr Nurs. 2022;66:202–12. 10.1016/j.pedn.2022.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elsheikh MA, Moriyama M, Rahman MM, Kako M, EL-Monshed AH, Zoromba M, et al. Effect of a tailored multidimensional intervention on the care burden among family caregivers of stroke survivors: a randomised controlled trial. BMJ Open. 2022;12:e049741. 10.1136/bmjopen-2021-049741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hill C, Knafl KA, Santacroce SJ. Family-centered care from the perspective of parents of children cared for in a Pediatric Intensive Care Unit: an integrative review. J Pediatr Nurs. 2018;41:22–33. 10.1016/j.pedn.2017.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coats H, Bourget E, Starks H, Lindhorst T, Saiki-Craighill S, Curtis JR, et al. Nurses’ reflections on benefits and challenges of Implementing Family-centered care in Pediatric Intensive Care Units. Am J Crit Care. 2018;27:52–8. 10.4037/ajcc2018353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Orr E, Ballantyne M, Gonzalez A, Jack SM. Providers’ perspectives of the neonatal intensive care unit context and care provision for adolescent parents: an interpretive description. BMC Pregnancy Childbirth. 2023;23:259. 10.1186/s12884-023-05553-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 30.Soper DS. A-priori sample size calculator for structural equation models. 2022.
- 31.House JS. Social support and social structure. Sociological forum. Springer; 1987. pp. 135–46.
- 32.Miles MS, Carlson J, Brunssen S. The nurse parent Support Tool. J Pediatr Nurs. 1999;14:44–50. 10.1016/S0882-5963(99)80059-1 [DOI] [PubMed] [Google Scholar]
- 33.Akkaş N, Geçkil E. Family-centered care scale in neonatal intensive care unit (FCCS-NICU): development and psychometrics evaluation. J Pediatr Nurs. 2023;72:168–76. 10.1016/j.pedn.2022.11.031 [DOI] [PubMed] [Google Scholar]
- 34.Brislin RW. Back-translation for cross-cultural research. J Cross Cult Psychol. 1970;1:185–216. 10.1177/135910457000100301 [DOI] [Google Scholar]
- 35.Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. 8th edition. London: Cengage Learning; 2019.
- 36.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993;42:148–52. 10.1097/00006199-199305000-00005 [DOI] [PubMed] [Google Scholar]
- 37.Rabie D, Provenzi L, Matta N, Montirosso R. Reliability and validity of the Arabic Version of the parental stressor scale and nurse parental support Tool: opening up research on parental needs in neonatal intensive care units in Egypt. Adv Neonatal Care. 2021;21. [DOI] [PubMed]
- 38.Nunnally J. Psychometric theory. New York: McGraw-Hill; 1978. [Google Scholar]
- 39.Kline RB. Principles and practice of structural equiation modeling - Fifth Edition. Guilford Press; 2023. p. 494.
- 40.Schreiber JB. Core reporting practices in structural equation modeling. Res Social Adm Pharm. 2008;4:83–97. 10.1016/j.sapharm.2007.04.003 [DOI] [PubMed] [Google Scholar]
- 41.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88:879–903. 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- 42.Fonseca SAda, Silveira AO, Franzoi MAH, Motta E. Family centered-care at the neonatal intensive care unit (NICU): nurses’ experiences. Enfermeria: Cuidados Humanizados. 2020;9:170–90. [Google Scholar]
- 43.Zoromba MA, Atta MHR, Ali AS, El-Gazar HE, Amin SM. The Mediating Role of Psychological Capital in the relationship between family sense of coherence and caregiver stress among parents of children with Autism Spectrum Disorder. Int J Ment Health Nurs. 2024;:1–13.
- 44.Skene C, Gerrish K, Price F, Pilling E, Bayliss P, Gillespie S. Developing family-centred care in a neonatal intensive care unit: an action research study. Intensive Crit Care Nurs. 2019;50:54–62. 10.1016/j.iccn.2018.05.006 [DOI] [PubMed] [Google Scholar]
- 45.Albayrak S, Büyükgönenç LA. The impact of family-centered care interventions on neonatal and parental outcomes in a Turkish hospital. Collegian. 2022;29:738–47. 10.1016/j.colegn.2022.05.004 [DOI] [Google Scholar]
- 46.Prasopkittikun T, Srichantaranit A, Chunyasing S. Thai nurses’ perceptions and practices of family-centered care: the implementation gap. Int J Nurs Sci. 2020;7:74–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sigurdson K, Profit J, Dhurjati R, Morton C, Scala M, Vernon L, et al. Former NICU families describe gaps in family-centered care. Qual Health Res. 2020;30:1861–75. 10.1177/1049732320932897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weber A, Harrison TM. Reducing toxic stress in the neonatal intensive care unit to improve infant outcomes. Nurs Outlook. 2019;67:169–89. 10.1016/j.outlook.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and analyzed during the current study are not publicly available due to confidentiality agreements, but are available upon reasonable request from the corresponding author.