Abstract
We conducted a cross-sectional study of hypertension care in public and private services, analyzing gender, color, and socioeconomic status. Using data from the 2013 (n = 60,202) and 2019 (n = 90,846) national health surveys, hypertension prevalence increased from 21.4 to 23.9%. Quality of care declined from 41.7 to 35.4%, particularly in public services, disproportionately affecting low-income Black women. Poisson regression estimated prevalence ratios (PRs), with the lowest adjusted PR for high-quality care among low-income Black women. These findings highlight persistent health inequalities and the urgent need for intersectoral policies to promote health equity.
Keywords: Hypertension, Intersectionality, Health care quality, Health services, Epidemiological surveys
Introduction
Hypertension is a chronic condition that, when not diagnosed and treated correctly, can cause damage to target organs such as cardiovascular and kidney diseases, increasing the risk of premature death.[1, 2] A study on global trends in blood pressure showed a 90% increase in the number of adults with hypertension between 1975 and 2015, with a more pronounced rise in low and middle-income countries [3].
Quality assessment in healthcare has become crucial for improving work processes and developing service standards that ensure effectiveness and safety, particularly considering the differences between public and private healthcare services.[4, 5] The National Health Survey (NHS), conducted by the Ministry of Health in partnership with the Brazilian Institute of Geography and Statistics (IBGE), provides crucial data to guide health strategies and assess the quality of hypertension care. The second edition of the survey in 2019 allowed for an analysis of progress over time and identification of ongoing challenges [6].
Studies based on the NHS have revealed sociodemographic inequalities in health, particularly affecting women and Black individuals. However, there has been insufficient exploration of how these social determinants overlap and impact individuals facing multiple adverse historical health factors [2, 7]. Analyzing the intersectionality of these sociodemographic characteristics is crucial to uncovering complex and simultaneous forms of oppression, such as racism and sexism, which are often not identified when examined separately [8]. Despite advances made by Brazil’s unified health system, Sistema Único de Saúde (SUS), in universalizing access to healthcare, significant challenges remain in overcoming barriers to hypertension care, especially those imposed by social determinants [9].
Therefore, this study aimed to evaluate and compare hypertension care in public and private healthcare services, analyzing quality indicators through the intersection of gender, race, and socioeconomic status.
Methods
Data Source
We used data from the 2013 and 2019 NHSs. Coordinated by the IBGE in partnership with the Ministry of Health, the NHS is a nationwide population-based cross-sectional survey of the domiciled adult population. The data from both surveys are publicly available on the IBGE’s website (https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html). The original questionnaires used in the surveys are available at https://www.pns.icict.fiocruz.br/wp-content/uploads/2021/02/Questionario-PNS-2013.pdf and https://www.pns.icict.fiocruz.br/wp-content/uploads/2023/06/Questionario_PNS_2019_26062023.pdf.
Sampling
The participants were selected using three-stage cluster sampling as follows: stratification of primary sample units (PSUs) consisting of one or more randomly selected census tracts with probability proportional to the number of private households; simple random selection of households in each PSU using the latest version of the national address register; and simple random selection of residents aged 18 and over without replacement based on a list of residents drawn up during the interview. [10, 11] For the purposes of this study, we selected respondents aged 18 years and over who answered the questions from module Q of the questionnaire about chronic diseases. The sample included respondents who had been clinically diagnosed with hypertension and had had a check-up in the last 24 months.
Variables
Outcome variable
High-quality health care for people with hypertension was assessed using the following 12 dichotomous questions about treatment and advice received during check-up in the last 24 months (No = 0 / Yes = 1): (i) Were you advised to maintain a healthy diet? (ii) Were you advised to maintain a healthy weight? (iii) Were you advised to cut down on salt? (iv) Were you advised to engage in regular physical activity? (v) Were you advised not to smoke? (vi) Were you advised not to drink in excess? (vii) Were you advised to do regular check-ups with a health professional? (viii) During your last check-up, did the doctor look at the results of the tests from past appointments? (ix) Were you asked to do a blood test? (x) Were you asked to do a urinalysis? xi. Were you asked to do an electrocardiogram? xii. Were you asked to do a cardiac stress test? An overall score of over 10 was deemed to indicate high-quality health care.
Exposure variables
The exposure variables were divided into three levels: (1) Context – region (North; Northeast; Midwest; Southeast; South); (2) Sociodemographic characteristics: sex (male; female), skin color (white; black/brown), age (18–29; 30–44; 45–59; and 60 years and over), education level (no education/did not complete primary education; completed primary education; completed secondary education; completed higher education), socioeconomic status using economic classification based on the asset index quintiles as a proxy (1st to 5th, lowest to highest), and dichotomized into low (1st, 2nd and 3rd quintiles) and high (4th and 5th quintiles) socioeconomic status; (3) type of health service (public; private). The variable intersection of sociodemographic factors consisted of sex, skin color, and socioeconomic status.
Statistical analysis
The descriptive analysis was performed using absolute (n) and relative (%) frequencies for the exposure variables and outcome variable. Prevalence rates were stratified according to type of service (public and private). Bivariate analysis was performed to determine the association between high-quality care (95% CI) and region, sociodemographic characteristics, type of service, and intersection of sex, skin color and socioeconomic status, based on prevalence ratios (PRs) estimated using Poisson regression. Multivariate analysis was then performed including variables that obtained a p-value of < 0.20 in the crude analysis to estimate adjusted PRs with their respective 95% CI. Forward stepwise regression was used to select the variables. The variables education level and economic classification, the latter of which was used in this study as a proxy for socioeconomic status, showed similar trends in both editions of the NHS. The former was therefore removed from multivariate analysis because the variable economic status was one of the items of the intersectionality variable. A p-value of < 0.05 in the final model was adopted as a threshold for association.
Due to the NHS’s complex sampling design, the analysis of the survey data requires prior definition of sampling weights for households and selected residents. Statistical analysis was therefore performed using Stata 15 with the svy command (StataCorp. 2017. Stata Statistical Software: College Station, TX: StataCorp LP), which considers the weighting of complex sampling designs.
Ethical considerations
The data from the two editions of the NHS are publicly available and both surveys were approved by the National Research Ethics Committee, attached to the National Health Council (2013 edition: reference Nº 328.159; 2019 edition: reference Nº 3.529.376).
Results
A total of 60,202 individuals aged 18 years and over participated in the 2013 survey, compared to 90,846 in the 2019 survey. In 2013, 21.4% (95% CI 20.8–22.0) of the respondents reported having been clinically diagnosed with hypertension, compared to 23.9% in 2019 (95% CI 23.5–24.4).
The sampling distribution was similar in both editions of the survey, with the Southeast accounting for the largest proportion of respondents (47.6% in 2013 and 46.9% in 2019), and the North representing the smallest share (5% in 2013 and 5.2% in 2019). The proportion of women (59.7% in 2013 and 59.4% in 2019) and black/brown people (50.3% in 2013 and 54.8% in 2019) was higher than that of men (40.3% in 2013 and 40.6% in 2019) and white people (49.7% in 2013 and 45.2% in 2019) in both surveys. The following groups also accounted for the highest proportions in their category: people aged 60 years and over (42.7% in 2013 and 48.6% in 2019), people who had completed primary education (45.2% in 2013 and 48.6% in 2019), people who used public services (65.8% in 2013 and 68.4% in 2019), and people who had had a check-up in the last 24 months (77.6% in 2013 and 81.5% in 2019). With regard to economic classification, in 2013, the highest quintile accounted for the highest proportion of respondents (22%) and the lowest quintile represented the lowest share (17.3%), while in 2019 the 2nd income quintile accounted for the highest proportion (24.8%) and the 5th quintile represented the lowest share (15%) (Table 1).
Table 1.
Distribution of individuals clinically diagnosed with hypertension by region, sociodemographic characteristics, type of service, and length of time since last check-up NHS 2013 (n = 12,318) and 2019 (n = 23,819)
| 2013 | 2019 | |||
|---|---|---|---|---|
| Variable | n | % | n | % |
| Region | ||||
| North | 1,871 | 5.0 | 3,625 | 5.2 |
| Northeast | 3,674 | 24.0 | 8,261 | 25.2 |
| Midwest | 1,635 | 7.3 | 2,690 | 6.6 |
| Southeast | 3,355 | 47.6 | 5,989 | 46.9 |
| South | 1,783 | 15.9 | 3,254 | 16.0 |
| Sex | ||||
| Female | 7,856 | 59.7 | 14,441 | 59.4 |
| Male | 4,462 | 40.3 | 9,378 | 40.6 |
| Skin color | ||||
| White | 5,301 | 49.7 | 9,073 | 45.2 |
| Black/brown | 7,016 | 50.3 | 14,384 | 54.8 |
| Age | ||||
| 18–29 | 439 | 3.4 | 846 | 3.3 |
| 30–44 | 2,228 | 17.5 | 3,219 | 14.3 |
| 45–59 | 4,203 | 36.4 | 7,326 | 33.9 |
| 60 and over | 5,548 | 42.7 | 12,428 | 48.6 |
| Education level | ||||
| No education/did not complete primary education | 2,970 | 21.0 | 3,281 | 10.9 |
| Completed primary education | 5,223 | 45.2 | 10,696 | 48.6 |
| Completed secondary education | 2,579 | 21.1 | 5,967 | 28.1 |
| Completed higher education | 1,546 | 12.7 | 2,771 | 12.4 |
| Economic status | ||||
| 1st quintile (lowest) | 2,860 | 17.3 | 6,329 | 20.2 |
| 2nd quintile | 2,796 | 20.4 | 5,775 | 24.8 |
| 3rd quintile | 2,499 | 20.1 | 4,630 | 21.7 |
| 4th quintile | 2,136 | 20.2 | 3,709 | 18.3 |
| 5th quintile (highest) | 2,027 | 22.0 | 3,376 | 15.0 |
| Type of health service | ||||
| Private | 3,482 | 34.2 | 5,407 | 31.6 |
| Public | 7,392 | 65.8 | 12,997 | 68.4 |
| Time since last check-up | ||||
| Less than 2 years | 9,638 | 77.6 | 18,495 | 81.5 |
| 2 years and over | 2,680 | 22.4 | 4,055 | 18.5 |
The prevalence of high-quality care for people with hypertension decreased from 41.7% in 2013 to 35.4% in 2019 (Table 2).
Table 2.
Prevalence of high-quality care for people with hypertension who had had a check-up in the last 24 months, NHS 2013 (n = 9,638) and 2019 (n = 18,495)
| 2013 | 2019 | |||
|---|---|---|---|---|
| Variable | n | % | n | % |
| Were you advised to maintain a healthy diet? | 9,638 | 88.6 | 18,495 | 87.2 |
| Were you advised to maintain a healthy weight? | 9,638 | 85.1 | 18,495 | 84.4 |
| Were you advised to cut down on salt? | 9,638 | 91.4 | 18,495 | 87.8 |
| Were you advised to engage in regular physical activity? | 9,638 | 82.1 | 18,495 | 81.7 |
| Were you advised not to smoke? | 9,638 | 76.4 | 18,495 | 67.3 |
| Were you advised not to drink in excess? | 9,638 | 75.7 | 18,495 | 66.6 |
| Were you advised to do regular check-ups with a health professional? | 9,638 | 88.3 | 18,495 | 85.3 |
| At your last check-up, did the doctor look at the results of the tests from past appointments? | 8,185 | 71.0 | 16,279 | 69.5 |
| Were you asked to do a blood test? | 9,638 | 82.4 | 18,495 | 80.2 |
| Were you asked to do a urinalysis? | 9,638 | 71.5 | 18,495 | 70.2 |
| Were you asked to do an electrocardiogram? | 9,638 | 65.8 | 18,495 | 64.8 |
| Were you asked to do a cardiac stress test? | 9,638 | 36.3 | 18,495 | 33.9 |
| Quality above the threshold (> 10 points) | 8,185 | 41.7 | 16,279 | 35.4 |
This reduction was observed across all groups, but was more pronounced in percentage point terms in the Southeast (-7.8) and among men (-7.8), black/brown people (-6.3), people aged 60 years and over (-7.7), people who had only completed primary education (-8.4), people with high socioeconomic status (-5.6), people who used public services (-7.0), and in white men with a high economic status (-8.2) (Table 3).
Table 3.
Prevalence of high-quality care for people with hypertension who had had a check-up in the last 24 months and absolute prevalence difference by region, sociodemographic characteristics, type of service, and intersection of sex, skin color, and socioeconomic status, NHS 2013 (n = 8,185) and 2019 (n = 16,279)
| 2013 | 2019 | Absolute | |||
|---|---|---|---|---|---|
| Variable | n | % | n | % | differences |
| Region | p-value: 0.000 | p-value: 0.000 | |||
| North | 1,285 | 36.4 | 2,511 | 32.8 | -3.6 |
| Northeast | 2,315 | 33.7 | 5,403 | 27.8 | -5.9 |
| Midwest | 1,041 | 42.9 | 1,818 | 39.7 | -3.2 |
| Southeast | 2,333 | 46.0 | 4,260 | 38.2 | -7.8 |
| South | 1,211 | 41.4 | 2,287 | 37.5 | -3.9 |
| Sex | p-value: 0.005 | p-value: 0.005 | |||
| Female | 5,426 | 39.5 | 9,756 | 33.8 | -5.7 |
| Male | 2,759 | 45.3 | 6,523 | 37.5 | -7.8 |
| Skin color | p-value: 0.000 | p-value: 0.000 | |||
| White | 3,581 | 45.0 | 6,273 | 39.4 | -5.6 |
| Black/brown | 4,603 | 38.3 | 9,759 | 32.0 | -6.3 |
| Age | p-value:0.001 | p-value: 0.012 | |||
| 18–29 | 276 | 27.4 | 353 | 22.0 | -5.4 |
| 30–44 | 840 | 35.0 | 1,827 | 32.9 | -2.1 |
| 45–59 | 2,519 | 42.9 | 5,150 | 37.0 | -5.9 |
| 60 and over | 4,550 | 43.1 | 8,949 | 35.4 | -7.7 |
| Education level | p-value: 0.000 | p-value: 0.000 | |||
| No education/did not complete primary education | 1,996 | 31.3 | 2,305 | 23.3 | -8.0 |
| Completed primary education | 3,477 | 40.1 | 7,395 | 31.7 | -8.4 |
| Completed secondary education | 1,693 | 48.6 | 3,909 | 41.2 | -7.4 |
| Completed higher education | 1,019 | 53.7 | 1,917 | 50.3 | -3.4 |
| Economic status | p-value: 0.000 | p-value: 0.000 | |||
| 1st quintile | 1,823 | 26.2 | 4,229 | 21.7 | -4.5 |
| 2nd quintile | 1,840 | 35.6 | 4,002 | 31.8 | -3.8 |
| 3rd quintile | 1,661 | 41.6 | 3,175 | 36.1 | -5.5 |
| 4th quintile | 1,496 | 45.1 | 2,529 | 42.2 | -2.9 |
| 5th quintile | 1,365 | 55.1 | 2,344 | 49.5 | -5.6 |
| Type of health service | p-value: 0.000 | p-value: 0.000 | |||
| Private | 2,679 | 53.5 | 4,820 | 50.2 | -3.3 |
| Public | 5,438 | 35.5 | 10,864 | 28.5 | -7.0 |
| Intersectionality | p-value: 0.000 | p-value: 0.000 | |||
| Male, white and high SES | 601 | 57.5 | 1,128 | 49.3 | -8.2 |
| Male, white and low SES | 647 | 36.8 | 1,487 | 32.9 | -3.9 |
| Male, black and high SES | 511 | 51.3 | 903 | 46.0 | -5.3 |
| Male, black and low SES | 1,000 | 34.4 | 2,914 | 30.5 | -3.9 |
| Female, white and high SES | 967 | 49.0 | 1,478 | 45.4 | -3.6 |
| Female, white and low SES | 1,366 | 36.4 | 2,180 | 33.4 | -3.0 |
| Female, black and high SES | 782 | 42.9 | 1,280 | 41.0 | -1.9 |
| Female, black and low SES | 2,310 | 33.6 | 4,662 | 27.4 | -6.2 |
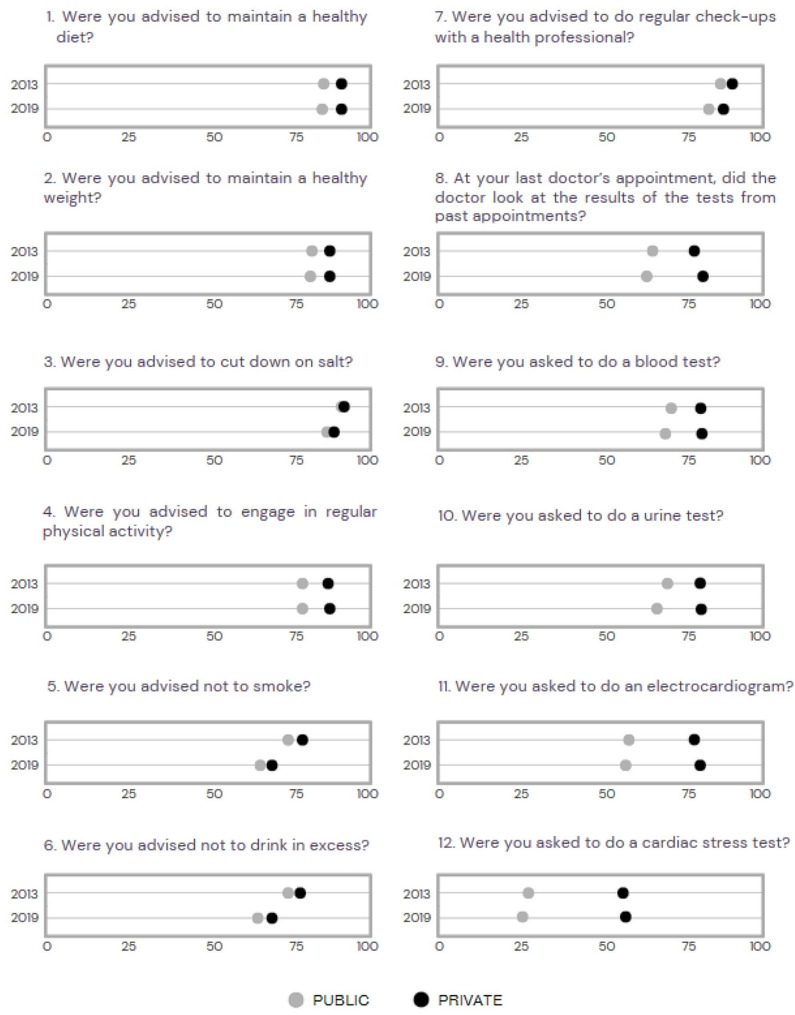
Among public and private healthcare services, a significant quality predominance was observed in private services regarding each component comprising the quality score. Additionally, from 2013 to 2019, there was a substantial decline in the quality of public services concerning most of these components, while private services experienced a significant increase in quality in most items, resulting in the widening disparity between these two types of healthcare services (Fig. 1).
Fig. 1.
Overall proportions for each item of the score for the quality of hypertension care for individuals who had had a check-up in the last 24 months by a service type, NHS 2013 (n = 8,185) and 2019 (n = 16,279)
The results of the crude analysis show that, in 2013, the PR of high-quality care was higher in the Southeast [1.26 (1.08–1.47)] and in people aged 60 years and over [1.57 (1.14–2.18)], and lower in people who used public services [0.66 (0.61–0.73)] and black women with low socioeconomic status [0.59 (0.50–0.69)]. In 2019, PR was higher in the Midwest [1.21 (1.06–1.37)] and among people aged between 45 and 59 years [1.68 (1.18–2.41)], and lower in people who used public services [0.57 (0.52–0.61)] and black women with low socioeconomic status [0.56 (0.48–0.64)] (Table 4).
Table 4.
Crude and adjusted prevalence ratios (PR) for high-quality health care for people with hypertension who had had a check-up in the last 24 months by region, age, type of health service, and patterns of intersectionality. NHS 2013 (n = 8,185) and 2019 (n = 16,279)
| 2013 | 2013 | 2019 | 2019 | |
|---|---|---|---|---|
| Variable | PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) |
| Crude | Adjusted | Crude | Adjusted | |
| Region | p-value: 0.000 | p-value: 0.000 | ||
| North | 1.00 | 1.00 | ||
| Northeast | 0.93 (0.78–1.10) | 0.85 (0.76–0.95) | ||
| Midwest | 1.18 (1.00–1.39) | 1.21 (1.06–1.37) | ||
| Southeast | 1.26 (1.08–1.47) | 1.16 (1.03–1.31) | ||
| South | 1.14 (0.96–1.35) | 1.14 (1.01–1.29) | ||
| Age | p-value: 0.000 | p-value: 0.003 | p-value: 0.091 | |
| 18–29 | 1.00 | 1.00 | 1.00 | |
| 30–44 | 1.28 (0.91–1.79) | 1.29 (0.91–1.81) | 1.50 (1.04–2.16) | |
| 45–59 | 1.56 (1.13–2.16) | 1.55 (1.11–2.16) | 1.68 (1.18–2.41) | |
| 60 and over | 1.57 (1.14–2.18) | 1.60 (1.15–2.22) | 1.61 (1.13–2.30) | |
| Type of health service | p-value: 0.000 | p-value: 0.000 | p-value: 0.000 | p-value: 0.000 |
| Private | 1.00 | 1.00 | 1.00 | 1.00 |
| Public | 0.66 (0.61–0.73) | 0.74 (0.67–0.81) | 0.57 (0.52–0.61) | 0.64 (0.58–0.70) |
| Patterns of intersectionality | p-value: 0.000 | p-value: 0.052 | p-value: 0.000 | p-value: 0.090 |
| Male, white and high SES | 1.00 | 1.00 | 1.00 | 1.00 |
| Male, white and low SES | 0.64 (0.53–0.78) | 0.72 (0.58–0.88) | 0.67 (0.57–0.78) | 0.94 (0.78–1.12) |
| Male, black and high SES | 0.89 (0.74–1.08) | 0.98 (0.81–1.19) | 0.93 (0.80–1.09) | 1.05 (0.90–1.24) |
| Male, black and low SES | 0.60 (0.59–0.74) | 0.73 (0.59–0.92) | 0.62 (0.53–0.72) | 0.95 (0.79–1.14) |
| Female, white and high SES | 0.85 (0.72–1.01) | 0.88 (0.75–1.04) | 0.92 (0.80–1.06) | 0.97 (0.85–1.12) |
| Female, white and low SES | 0.63 (0.53–0.75) | 0.70 (0.59–0.84) | 0.68 (0.59–0.78) | 0.96 (0.80–1.14) |
| Female, black and high SES | 0.75 (0.62–0.89) | 0.82 (0.68–0.98) | 0.83 (0.71–0.97) | 0.96 (0.82–1.12) |
| Female, black and low SES | 0.59 (0.50–0.69) | 0.72 (0.60–0.87) | 0.56 (0.48–0.64) | 0.86 (0.73–1.02) |
In the adjusted analysis, in 2013, the PR continued to be higher among people aged 60 years and over [1.60 (1.15–2.22)] and lower in people who used public services [0.74 (0.67–0.81)]. With regard to intersectionality, the results reveal a pattern whereby people with low socioeconomic status showed lower PR, regardless of color or sex. In 2019, the adjusted prevalence ratios (PRs) indicated that people who used public services continued to have the lowest PR for high-quality health care [0.64 (0.58–0.70)]. With regard to intersectionality, black women with low socioeconomic status continued to have the lowest PR [0.86 (0.73–1,02)] for high-quality health care, although without statistical significance (Table 4).
Discussion
In line with previous research, the findings of the present study reveal that the prevalence of hypertension in Brazil rose between 2013 and 2019 [2, 6, 12, 13]. The data from the two surveys show that there was no significant change in the profile of people with hypertension during the study period. These findings suggest that policies to promote equity in health care among people with hypertension have not been effective. Health actions aimed at controlling hypertension need to be planned, ongoing, integrated and, above all, subjected to quality assessment[14].
Despite the relationship between health and access to and utilization of health services, the latter often fail to meet quality standards for the diagnosis and control of diseases.5 The use of protocols for hypertension care can improve service delivery and quality control and facilitates the identification of factors that influence care quality and outcomes. [15] Despite broad consensus about the importance of clinical guidelines and protocols, their use remains limited, especially when it comes to the implementation of actions based on the risk stratification of a given population group, posing a barrier to improving access and achieving better care outcomes based on current scientific knowledge. [16, 17] It is worth noting that the questions used in the NHS to assess quality of care are derived from protocols and official guidelines.
Access to and utilization of health care services are complex and multidimensional concepts. People who have access to a greater range of sources of care are able to access a more diverse set of preventive and therapeutic services. [18] Our findings show that people who used private services reported higher quality of care; however, most of the respondents used public services. Studies show that patients who use exclusively public services tend to be more vulnerable, especially among the black population with low socioeconomic status living in the North and Northeast [19].
Quality of care declined between 2013 and 2019 across all sociodemographic groups, regions, and types of service. Health inequalities linked to gender, skin color, and socioeconomic status persisted, reflecting deep-rooted inequality in Brazilian society. [7, 20] Previous studies have shown that people with a higher level of education tend to have improved access to health services and receive better quality care. Level of education can also influence health literacy and patient understanding of recommendations and advice provided by health professionals [21].
The decline in quality of hypertension care was more pronounced in public services. Given that most appointments in public services take place in primary care services, the point of entry to the health system, these findings may be attributed to recent changes in the National Primary Health Care Policy (PNAB), which altered the composition of health teams and permitted a reduction in staff and working hours. In view of increasing demand for public services due to the impoverishment of the population, the new PNAB has increased the burden on health professionals, in turn affecting the quality of care. Another factor that may have contributed to the decline in the overall performance of public services is the passing of Constitutional Amendment 95 in 2016 imposing a ceiling on health spending, precisely in the middle of the study period [5]
The results of the NHS highlight the urgent need for research to advance understanding of the complex relationship between social inequalities and chronic disease and quality of health care. In this direction, the findings of the present study suggest that greater emphasis is needed on the implementation of intersectoral policies. In this sense, the use of the concept of intersectionality in policy-making helps policymakers to understand the multiple social determinants of health [25].
Women and men should therefore not be assessed as homogenous groups without taking into account factors such as race/skin color. Women face various social restrictions – including lower salaries and unpaid domestic work – limiting the amount of time available for formal employment, education, and leisure, and impacting health care. In addition, the intersection of sexism and racism, both interlocking forms of oppression, hierarchization, and social exclusion, disproportionately affects black women [23].
The analysis of black women’s health within the context of Brazil’s history requires an intersectional approach that explores the intersection of different categories of analysis: gender, race/color, and socioeconomic status. Intersectionality is a key theoretical and methodological framework for understanding social dynamics that impact women’s lives, enabling researchers to capture the structural consequences and dynamics of interaction between two or more forms of subordination [24].
Social reality in Brazil is characterized by major racial disparities in living conditions, health, and mortality, as well a belief in the superiority of economically and politically dominant groups. [25] These beliefs are ingrained in both common sense and academic knowledge, and bringing to light these inequalities – particularly in public health systems – is a subversive and necessary activity [24, 26].
Black women tend to have a lower level of education and income than other groups and are more likely to have more taxing jobs with longer working hours and little social recognition and a heavier domestic work load. [27] At the confluence of these factors lies the three-fold invisibility and violence to which black women are subjected to, as they are the only group attacked on three fronts: misogyny, racism, and poverty. [28–30] Promoting equity in health care quality is therefore essential for improving well-being, preventing the perpetuation of health disparities, and minimizing the disproportional effects of health inequality on disadvantaged groups [6].
First, the cross-sectional nature of the research design limits our ability to determine temporality and causal relationships between variables. Second, the study may be subject to information and recall biases, particularly regarding the quality score items reported by participants, which could affect the accuracy of responses. Third, there may be specification bias in the variables chosen to compose the quality score, as other variables not included could influence the results. Additionally, the samples from the 2013 and 2019 National Health Surveys (NHS) had different sizes, potentially introducing variations in data comparison over time. Furthermore, it was not possible to stratify clinical risk for hypertension, such as identifying cardiovascular factors. Another limitation is the variable “sex” as the relevant field in the IBGE questionnaires only has two response options (male and female), disregarding gender identity, which is particularly important for constructing the intersectionality variable.
The differences between raw and adjusted prevalence ratios (PRs) highlight the influence of confounding variables on the quality of care. For instance, the raw PRs suggested a higher likelihood of high-quality care in certain groups, but once adjusted for factors like socioeconomic status, the disparities became more pronounced. This indicates that the initial observed differences in care quality might be partly attributed to underlying sociodemographic factors. Adjusting for these factors provides a clearer picture of the true disparities in care quality, underscoring the need for targeted interventions.
The results suggest an urgent need for intersectoral policies that address the multiple forms of oppression exacerbating health inequalities. Implementing specific clinical guidelines and protocols, along with continuous education for health professionals, can improve care quality and reduce the identified disparities. Additionally, public policies must be designed considering the intersectionality of social determinants of health, ensuring that interventions are effective for the most vulnerable groups.
In conclusion, this study highlights the importance of intersectional approaches in analyzing health inequalities and formulating policies. Recognizing the complex interactions between gender, race/color, and socioeconomic status is crucial for promoting health care equity and improving outcomes for individuals with hypertension.
Acknowledgements
Not applicable.
Author contributions
Dear Editor, We would like to submit our article entitled “Assessing hypertension care quality in Brazil: gender, race, and socioeconomic intersection in public and private services, 2013 and 2019 national health surveys.” for consideration for publication in BMC Health Services Research. We declare that all listed authors have made substantial contributions to the work according to the authorship criteria established by the journal. Below, we detail each author’s contributions: PVCA contributed to the study’s conception, statistical analysis of the data, interpretation of the results, creation of figures and tables, as well as manuscript writing. ET actively participated in the study design, critical review of intellectual content, and provided significant insights for the discussion of results.Furthermore, all authors have approved the final version of the submitted manuscript and agreed to be personally responsible for the contributions each has made. We commit to ensuring the accuracy and integrity of the work by investigating and resolving any related issues that may arise and documenting these resolutions in the literature.Corresponding author PVCA assumes responsibility for ensuring that all authors have approved the manuscript before submission and that everyone is aware of and compliant with the transparency and reproducibility standards of the field and the journal.We appreciate your consideration of our work for publication in BMC Health Services Research.Best regards.
Funding
The authors declare that there are no conflicts of interest related to this manuscript. None of the authors have financial, consultant, institutional, or other relationships that could be perceived as biasing the work presented in this manuscript. Additionally, no sources of funding were received for this research.
Data availability
We used data from the 2013 and 2019 NHSs. Coordinated by the IBGE in partnership with the Ministry of Health. The data from both surveys are publicly available on the IBGE’s website (www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html). The original questionnaires used in the surveys are available at www.icict.fiocruz.br/questionarios/.
Declarations
Ethics approval and consent to participate
Both surveys were approved by the National Research Ethics Committee, attached to the National Health Council (2013 edition: reference Nº 328.159; 2019 edition: reference Nº 3.529.376). By participating in this study, all participants provided their informed consent prior to data collection (2013 edition: https://www.pns.icict.fiocruz.br/wp-content/uploads/2021/03/TCLE-Informante-do-domicilio-PNS-2013.pdf; 2019 edition: https://www.pns.icict.fiocruz.br/wp-content/uploads/2021/03/TCLE_Informante_domicilio_2019.pdf.
Consent for publication
I, Paulo Victor Cesar de Albuquerque, the lead author of the article titled “Intersection of sociodemographic factors and the quality health care for people with hypertension in Brazilian public and private services: 2013 and 2019 national health surveys,” agree to submit and publish this work in the BMC Health Services Research. I understand that by granting this consent, I am authorizing the public disclosure of the article, including the text, figures, tables, and other related materials. I also declare that co-author Elaine Tomasi has been informed about this submission and agrees to the publication of the article in the mentioned journal above. I certify that the content of the article is original and has not been previously published in any other journal or publication platform.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Barroso, W. K. S., et al. (2021). Brazilian guidelines of hypertension–2020. Arquivos brasileiros de cardiologia, 116, 516–658. [DOI] [PMC free article] [PubMed]
- 2.Malta, D. C., et al. (2022). Hipertensão arterial autorreferida, uso de serviços de saúde e orientações para o cuidado na população brasileira: Pesquisa Nacional de Saúde, 2019. Epidemiologia e Serviços de Saúde, 31, e2021369. [DOI] [PMC free article] [PubMed]
- 3.Zhou, B., et al. (2017). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19· 1 million participants. The Lancet, 389(10064), 37–55. [DOI] [PMC free article] [PubMed]
- 4.Pereira, P. C. J., Roquete, F. F., & Debôrtoli de Miranda, W. (2022). Aplicabilidade das ferramentas da qualidade nos processos dos serviços de saúde: uma revisão integrativa (2010–2020). Revista Gestão & Saúde, 13(02), 35–46.
- 5.Oliveira, B. L. C. A. D., et al. (2020). A influência da Estratégia Saúde da Família no uso de serviços de saúde por adultos hipertensos no Brasil. Revista Brasileira de Epidemiologia, 23, e200006. [DOI] [PubMed]
- 6.Szwarcwald, C. L., Stopa, S. R., & Malta, D. C. (2022). Situação das principais doenças crônicas não transmissíveis e dos estilos de vida da população brasileira: Pesquisa Nacional de Saúde, 2013 e 2019. Cadernos de Saúde Pública, 38, e00276021. [DOI] [PubMed]
- 7.Cobo, B., Cruz, C., & Dick, P. C. (2021). Desigualdades de gênero e raciais no acesso e uso dos serviços de atenção primária à saúde no Brasil. Ciência & Saúde Coletiva, 26, 4021–4032. [DOI] [PubMed]
- 8.Crenshaw, K. W. (2013). Mapping the margins: Intersectionality, identity politics, and violence against women of color. In The public nature of private violence (pp. 93–118). Routledge.
- 9.Jesus, M. A. D. C., Acioli, S., Silva, M. D. F. B., & Santos, R. G. S. (2023). A interseccionalidade como categoria analítica na saúde com foco na enfermagem na Atenção Primária em Saúde: uma revisão integrativa de literatura. Contribuciones a Las Ciencias Sociales, 16(10), 18773–18793.
- 10.Brasil. Instituto Brasileiro de Geografia e Estatística. (2020). Pesquisa Nacional de Saúde 2019: percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal, Brasil e grandes regiões.
- 11.Stopa, S. R., et al. (2020). National Health Survey 2019: history, methods and perspectives. Epidemiologia e Serviços de Saúde, 29, e2020315. [DOI] [PubMed]
- 12.Gondim, F. S. S., Campos, M. O., Flores, T. R., França, G. V. A. D., & Medeiros, A. C. D. (2022). Pesquisa Nacional de Saúde 2019: avanço no monitoramento da saúde dos brasileiros. Epidemiologia e Serviços de Saúde, 31, e2021309. [DOI] [PMC free article] [PubMed]
- 13.Tomasi, E., Pereira, D. C., Santos, A. V. D., & Neves, R. G. (2022). Adequação do cuidado a pessoas com hipertensão arterial no Brasil: Pesquisa Nacional de Saúde, 2013 e 2019. Epidemiologia e Serviços de Saúde, 31, e2021916. [DOI] [PubMed]
- 14.Borges, F. M., et al. (2022). Estratégias para promoção da saúde e seus impactos na qualidade de vida de adultos hipertensos: revisão integrativa. Cadernos Saúde Coletiva, 30, 146–157.
- 15.Dantas, R. C. O., et al. (2018). O uso de protocolos na gestão do cuidado da hipertensão arterial na atenção primária à saúde: uma revisão integrativa. Revista Ciência Plural, 4(1), 117–131.
- 16.Silva, L. B., et al. (2019). Estratos de risco e qualidade do cuidado à pessoa idosa na Atenção Primária à Saúde. Revista Latino-Americana de Enfermagem, 27, e3166. [DOI] [PMC free article] [PubMed]
- 17.Malta, D. C., Morais Neto, O. L. D., & Silva, J. B. D. (2011). Apresentação do plano de ações estratégicas para o enfrentamento das doenças crônicas não transmissíveis no Brasil, 2011 a 2022. Epidemiologia e serviços de saúde, 20(4), 425–438. [DOI] [PubMed]
- 18.Giovanella, L., et al. (2021). Cobertura da Estratégia Saúde da Família no Brasil: o que nos mostram as Pesquisas Nacionais de Saúde 2013 e 2019. Ciência & Saúde Coletiva, 26, 2543–2556. [DOI] [PubMed]
- 19.Dantas, M. N. P., et al. (2020). Fatores associados ao acesso precário aos serviços de saúde no Brasil. Revista Brasileira de Epidemiologia, 24, e210004. [DOI] [PubMed]
- 20.Viacava, F., Porto, S. M., Carvalho, C. D. C., & Bellido, J. G. (2019). Desigualdades regionais e sociais em saúde segundo inquéritos domiciliares (Brasil, 1998–2013). Ciência & Saúde Coletiva, 24, 2745–2760. [DOI] [PubMed]
- 21.Neves, R. G., et al. (2017). Atenção oferecida aos idosos portadores de hipertensão: Pesquisa Nacional de Saúde, 2013. Cadernos de Saude Publica, 33. [DOI] [PubMed]
- 22.Carvalho, L. P. (2023). Transnacionalismo, interseccionalidade e ativismo na política de saúde para mulheres. Revista Estudos Feministas, 31, e92876.
- 23.Santos, L. A., et al. (2023). Interseções de gênero e raça/cor em insegurança alimentar nos domicílios das diferentes regiões do Brasil. Cadernos de Saúde Pública, 38, e00130422. [DOI] [PubMed]
- 24.Nascimento, S. S. (2018). Saúde da mulher negra brasileira: a necessária intersecção em raça, gênero e classe. Cadernos do CEAS: Revista crítica de humanidades, (243), 91–103.
- 25.Lotufo, P. A., & Bensenor, I. J. M. (2013). Raça e mortalidade cerebrovascular no Brasil. Revista de Saúde Pública, 47, 1201–1204. [DOI] [PMC free article] [PubMed]
- 26.Rosa, W., Bonetti, A., & Abreu, M. A. (2011). Sexo e cor/raça como categorias de controle social: uma abordagem sobre desigualdades socioeconômicas a partir dos dados do Retrato das Desigualdades de Gênero e Raça-Terceira Edição. Bonetti AL, Abreu MA, organizadoras. Faces da desigualdade de gênero e raça no Brasil. Brasília: Instituto de Pesquisa Econômica Aplicada, 111 − 27.
- 27.Sousa, C. C. D., & Araújo, T. M. D. (2024). Efeitos combinados de gênero, raça e estressores ocupacionais na saúde mental. Revista Brasileira de Saúde Ocupacional, 49, edepi12.
- 28.Andrade, T. G. V., Almeida, V. M., Miranda, V. S., & Oliveira, R. S. (2024). Gênero, raça e suas interseccionalidades na academia: o que está sendo produzido sobre a mulher negra?. Revista Serviço Social em Perspectiva, 8(1), 178–204.
- 29.López, L. C. (2012). O conceito de racismo institucional: aplicações no campo da saúde. Interface-Comunicação, Saúde, Educação, 16, 121–134.
- 30.Levorato, C. D., Mello, L. M. D., Silva, A. S. D., & Nunes, A. A. (2014). Fatores associados à procura por serviços de saúde numa perspectiva relacional de gênero. Ciência & saúde coletiva, 19, 1263–1274. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We used data from the 2013 and 2019 NHSs. Coordinated by the IBGE in partnership with the Ministry of Health. The data from both surveys are publicly available on the IBGE’s website (www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html). The original questionnaires used in the surveys are available at www.icict.fiocruz.br/questionarios/.