Abstract
Progressive supranuclear palsy (PSP) is a neurodegenerative movement and cognitive disorder characterized by abnormal accumulation of the microtubule-associated protein tau in the brain. Biochemically, inclusions in PSP are enriched for tau proteoforms with four microtubule-binding domain repeats (4R), an isoform that arises from alternative tau pre-mRNA splicing. While preferential aggregation and reduced degradation of 4R tau protein is thought to play a role in inclusion formation and toxicity, an alternative hypothesis is that altered expression of tau mRNA isoforms plays a causal role. This stems from the observation that PSP is associated with common variation in the tau gene (MAPT) at the 17q21.31 locus which contains low copy number repeats flanking a large recurrent genomic inversion. The complex genomic structural changes at the locus give rise to two dominant haplotypes, termed H1 and H2, that have the potential to markedly influence gene expression. Here, we explored haplotype-dependent differences in gene expression using a bulk RNA-seq dataset derived from human post-mortem brain tissue from PSP (n = 84) and controls (n = 77) using a rigorous computational pipeline, including alternative pre-mRNA splicing. We found 3579 differentially expressed genes in the temporal cortex and 10,011 in the cerebellum. We also found 7214 differential splicing events in the temporal cortex and 18,802 in the cerebellum. In the cerebellum, total tau mRNA levels and the proportion of transcripts encoding 4R tau were significantly increased in PSP compared to controls. In the temporal cortex, the proportion of reads that expressed 4R tau was increased in cases compared to controls. 4R tau mRNA levels were significantly associated with the H1 haplotype in the temporal cortex. Further, we observed a marked haplotype-dependent difference in KANSL1 expression that was strongly associated with H1 in both brain regions. These findings support the hypothesis that sporadic PSP is associated with haplotype-dependent increases in 4R tau mRNA that might play a causal role in this disorder.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40478-024-01839-3.
Keywords: Tauopathy, Progressive supranuclear palsy, RNA-seq, 17q21.31, MAPT haplotype, KANSL1
Introduction
The tau proteinopathies (“tauopathies”) are a group of neurodegenerative disorders characterized neuropathologically by intracellular accumulation of the microtubule-associated protein tau in the brain [1]. The tauopathies have broad clinical heterogeneity and overlap, variably displaying movement disorder, cognitive impairment, motor neuron disease, and psychiatric symptomatology. Thus, obtaining a better understanding of the complex mechanisms that underlie tau accumulation and toxicity has the potential to enable better diagnostic and therapeutic strategies for many patients [2, 3]. Genetic factors play a role, with some kindreds of frontotemporal lobar degeneration (FTLD) harboring autosomal dominant mutations in the tau gene (MAPT) that involve coding regions and splice sites, demonstrating that primary involvement of tau is sufficient to cause neurodegeneration [4–7]. These mutations, which preferentially cluster around exon 10, influence tau pre-mRNA alternative splicing leading to an imbalance of tau proteoform expression [8]. However, the majority of tauopathy cases are sporadic without a family history or autosomal dominant mutation.
Progressive supranuclear palsy (PSP), a dementing movement disorder, is the most common primary sporadic tauopathy [1]. It is characterized neuropathologically by preferential accumulation of tau protein with 4-repeat binding domains (4R tau) in the basal ganglia, brainstem, and cerebellum [9, 10]. The relative abundance of tau isoforms is dictated by alternative pre-mRNA splicing of MAPT exon 10, which encodes the second of the four tandem microtubule-binding domain repeats (which leads to increased binding affinity) [11–14]. While sporadic PSP patients do not have MAPT mutations, such as those in and around exon 10 splice sites that alter 4R tau mRNA, it is associated with common genetic variation [15–17]. MAPT is situated within the highly complex 17q21.31 locus with numerous studies delineating an approximately one megabase inversion region flanked by large insertion-deletion polymorphisms giving rise to the H1 and H2 haplotypes as well as numerous subhaplotypes. H1 is the more common haplotype and has been found to be significantly associated with PSP [18–22]. While MAPT is roughly at the center of the inversion region, the base pair sequence of the six tau isoforms are not predicted to be directly altered by this structural variation. In contrast, both haplotypes contain regions that result in partial duplication of the neighboring KANSL1 gene. The H1 haplotype contains a polymorphic β duplication which affects KANSL1, ARL17, and LRRC37A, while the H2 haplotype contains a shorter α duplication region within β which includes only the 5’ exons of KANSL1 [19, 23, 24]. These structural changes are predicted to give rise to truncated pseudogenes, but these are poorly studied and the extent to which they are transcribed and translated to functional polypeptides remains unclear [25]. These structural variants have the potential to lead to dramatic changes in gene expression in the locus that could participate in the pathogenesis of PSP.
While PSP is characterized by preferential accumulation of 4R tau protein, it has yet to be established whether total tau and the 4R tau isoform mRNA are differentially transcribed and translated [9, 10, 26–28]. Chambers et al. found increased levels of 4R tau mRNA in the brainstem but not in cerebellum or cortex of patients with PSP, while Takanashi et al. did find increased 4R tau mRNA in the frontal cortex and globus pallidus of patients with PSP [10, 29]. One study found increased 4R tau mRNA in the frontal cortex compared to 3R tau, but found lower overall tau mRNA levels in PSP compared to controls [30]. Another study found upregulated total tau expression specifically in the astrocytes of patients with PSP [31]. Further studies considered the association between 4R tau mRNA and the MAPT H1 and H2 haplotypes, with mixed observations. Some studies have found increased total tau expression in the H1 haplotype [22, 32, 33], while another study found no association between tau expression and the H1 haplotype [30]. Additionally, it has been suggested that the association between tau expression and the H1 haplotype is due to a technical artifact, with differences in hybridization affinity secondary to imperfect matches between probes between H1 and H2 [34, 35]. Thus, the extent to which there are haplotype-dependent differences in tau mRNA expression remains controversial, as is the association between PSP and 4R tau mRNA in various brain regions.
In this study, we sought to further test the hypothesis that increased levels of total tau and 4R tau mRNA in post-mortem human brain tissue are associated with PSP, and if there are differences based on regional vulnerability. We also sought to examine whether other genes at the 17q21.31 locus are differentially expressed or spliced which may contribute to pathology. To accomplish this, we leveraged a streamlined computational pipeline, including differential intron excision, to reanalyze an existing RNA-seq dataset from post-mortem brain tissues from a large collection of autopsy-confirmed PSP cases and controls. Genotyping of tagged single nucleotide polymorphisms (SNPs) allowed us to correlate MAPT haplotypes with the expression of candidate genes and isoforms.
Methods
Dataset
The progressive supranuclear palsy (PSP) RNA-seq data (Synapse ID: SYN3163039) was obtained from synapse.org and was derived from the cerebellum and temporal cortex from a total of 164 neuropathologically confirmed cases (n = 84) and controls (n = 80) before quality control (QC) [36]. All 164 data were processed through our pipeline. Tau haplotype was derived from preexisting corresponding genome-wide association study data obtained from NIAGADS (NG00037) using the tagging SNP rs1800547 as previously described [37]. Genomic annotations for α, β, and γ regions within the haplotype were lifted from hg19 to hg38 using the UCSC Genome Browser [19]. All the data was generated at the Mayo Clinic Jacksonville.
RNA-seq processing pipeline
We used the RAPiD-nf pipeline developed as part of the CommonMind consortium [38]. RAPiD-nf is a pipeline in the NextFlow framework and uses Trimmomatic (version 0.36) [39], STAR (version 2.7a) [40], FASTQC (version 0.11.8) [41], featureCounts (version 1.3.1) [42], and Picard (version 2.20.0) [43] for pre-processing and quality control. RSEM (version 1.3.1) [44] was used for differential gene expression, and LeafCutter (version 0.2.8) [45] was used for differential intron excision. After all QC steps, 3 samples were excluded from the temporal cortex, and 4 were excluded from the cerebellum.
Covariate adjustment
The gene expression matrix was normalized using trimmed mean of M values and transformed using the limma::voom() function [46]. Lowly expressed genes were removed. Covariates were selected to minimize gene expression differences based on technical and biological variables. Clinical and technical variables from Picard were combined and correlated using variancePartition [47]. Variables that contributed the most to variance in gene expression and had the least overlap with one another were included. The final variables included as covariates were RNA integrity number (RIN), percent duplicate reads, mean insert size, age, sex, and case–control status. Of note, post-mortem interval (PMI) was not considered as a covariate due to insufficient data availability.
Differential gene expression
After normalization and covariate adjustment, differential gene expression (DGE) analysis was performed using the limma package to compare gene expression of PSP cases and controls [48]. Limma calculated log2-fold change, t statistics, and p values for each gene. Statistics were computed using the treat method which calculates p values from empirical Bayes moderated t-statistics with a minimum log2 fold change (logFC) requirement [46].
Pathway analysis
We used Ingenuity Pathway Analysis (IPA) software (Qiagen, Hilden Germany) to investigate whether the differentially expressed genes were enriched in certain biological processes and pathways. The IPA Core Analysis module was employed to analyze the differentially expressed genes (p < 0.05) against the Ingenuity Knowledge Base (Genes Only) reference set. The analysis produced a list of enriched pathways and processes with corresponding p values and z-scores, and the most significant ones were identified based on these statistical measures.
Differential splicing
We used the LeafCutter package in R with Regtools (version 0.5.2) for differential intron excision analysis to examine splicing [45]. BAM files were preprocessed to generate junction and intron files. Next, Leafcutter was employed to perform the differential splicing analysis. The outputs were processed and visualized using LeafViz (github.com/jackhump/leafviz). To focus on statistically significant intron–exon junction regions, only those with a Bayes factor greater than 10 and a false discovery rate (FDR) less than 0.05 were included in the results. Percent exon inclusion for MAPT exon 10 was calculated as mean(flanking introns %)/(mean(flanking introns %) + skipping intron %). To assess the association between MAPT and KANSL1 isoforms detected through LeafCutter and MAPT haplotype status, an ANOVA was performed which compared expression of each isoform with sample haplotype status (homozygous H1, heterozygous H1H2, and homozygous H2H2).
Deconvolution analysis
To perform gene expression deconvolution analysis, we used BRETIGEA (BRain cEll Type specIfic Gene Expression Analysis) [49]. The raw gene expression count matrix was input to BRETIGEA to estimate the proportions of neuronal and glial cell types present in the samples. These cell-type proportions were used to estimate the cellular composition of the samples but were not incorporated into the gene expression matrix due to lack of ability to validate the cell type proportions.
Results
We leveraged a publicly available bulk RNA-sequencing dataset from post-mortem brain tissue from the cerebellum and temporal cortex [36]. After quality control, the dataset consisted of 84 PSP cases and 77 controls (Table 1). Of these, there were 51 male and 33 female PSP cases that were compared to 38 male and 39 female controls. The average age of temporal cortex controls was 82.3 ± 1.0 (53–90) and the average age of temporal cortex PSP cases was 73.9 ± 0.7 (61–89) (p < 0.0001); the average age of cerebellum controls was 79.6 ± 0.8 (58–89) and the average age of cerebellum PSP cases was 74.1 ± 0.7 (61–89) (p < 0.0001). The average RNA integrity number (RIN) of temporal cortex controls was 7.6 and the average RIN of temporal cortex PSP cases was 8.5 (p < 0.0001); the average RIN of cerebellum controls was 7.7; the average RIN of cerebellum PSP cases was 8.5 (p < 0.0001). The average post-mortem interval (PMI) of temporal cortex controls was 6.2 h and the average PMI of temporal cortex PSP cases was 8.6 h (p = 0.09); The average PMI of cerebellum controls was 6.2 h and the average PMI of cerebellum PSP cases was 8.3 h (p = 0.14).
Table 1.
Clinical data
| Diagnosis | Cerebellum | Temporal cortex | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | M/F (n) | Average age (yr ± SEM, range) | RIN | PMI | n | M/F (n) | Average age (yr ± SEM, range) | RIN | PMI | |
| PSP | 83 | 50/33 | 74.1 ± 0.7 (61–89) | 8.5 | 8.3 | 84 | 51/33 | 73.9 ± 0.7 (61–89) | 8.5 | 8.6 |
| Control | 77 | 40/37 | 79.6 ± 0.8 (58–89) | 7.7 | 6.2 | 77 | 38/39 | 82.3 ± 1.0 (53–90) | 7.6 | 6.2 |
| Total | 160 | 90/70 | 76.7 ± 0.6 (58–89) | 8.1 | 7.3 | 161 | 89/72 | 77.9 ± 0.7 (53–90) | 8 | 7.9 |
| p value | < 0.0001 | < 0.0001 | 0.14 | < 0.0001 | < 0.0001 | 0.09 | ||||
RIN RNA integrity score, PMI Post mortem interval
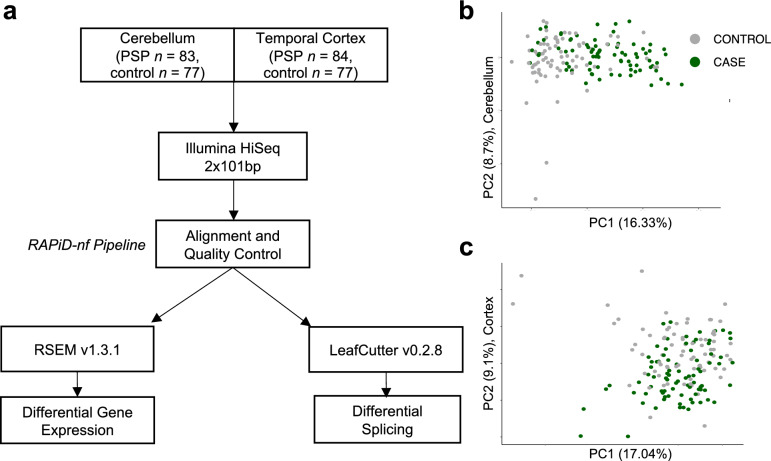
For alignment and quality control, we ran the RAPiD-nf pipeline which trims, aligns, quantifies gene expression, and performs quality control (Fig. 1). The mean read depth was 64.0 million reads for the cerebellum and 62.7 million for the temporal cortex. The mean percentage of reads that were aligned to the reference was 98.7% for the cerebellum and 98.2% for the temporal cortex. The mean percentage of reads mapping to mRNA in the samples was 71.5% for the cerebellum and 73.2% for the temporal cortex. The mean percentage ribosomal RNA was 3.1% for the cerebellum and 4.9% for the temporal cortex. Before filtering, 58,929 genes were included. After removing genes with no reads or a low read depth, 21,478 genes remained (Supplemental Fig. 1). Covariates were selected using variancePartition, and the final variables used for downstream analysis were RIN, percent duplicate reads, mean insert size, age, sex, and case–control status (Supplemental Fig. 2). Raw counts generated were used to estimate relative cell type proportions in each sample using BRETIGEA, which found that the cerebellum contained a different proportion of astrocytes, oligodendrocytes, and OPCs in cases compared to controls, and the temporal cortex contained a different proportion of neurons and oligodendrocytes in cases compared to controls (p < 0.05; Supplemental Fig. 3).
Fig. 1.
RNA sequencing pipeline using RAPiD-nf aligns and quality controls 161 samples for differential expression and splicing analysis. a RNA-seq samples were obtained from Synapse.org [50]. The cohort included 161 PSP cases and controls, with samples taken from the cerebellum and temporal cortex. Samples were processed using RAPiD-nf, a processing pipeline in the NextFlow framework. RAPiD-nf uses Trimmomatic, STAR, FASTQC, featureCounts, Pathogen, and Picard for pre-processing and quality control. RSEM and Limma were used for differential gene expression, and Regtools and LeafCutter were used for differential intron excision. b, c Principal component analysis of the RNA-seq expression matrix after covariate adjustment in cerebellum and temporal cortex shows no remaining outliers. 161 samples were included in downstream analysis
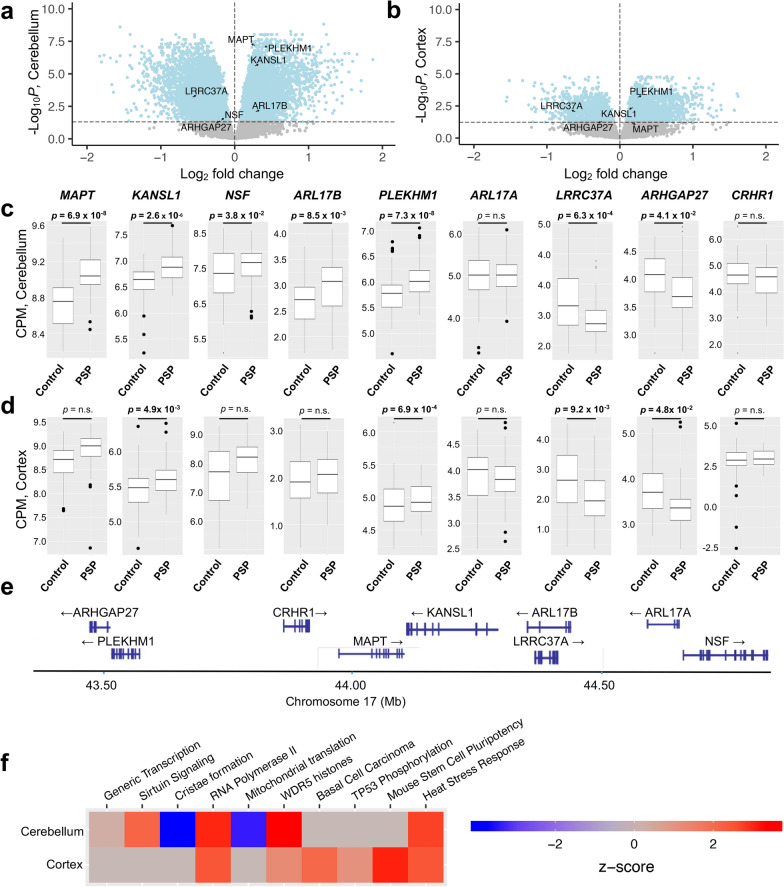
Using a significance threshold of p < 0.05 (FDR adjusted), 3579 genes were differentially expressed in the temporal cortex, with 2217 genes upregulated and 1362 genes downregulated in cases compared to controls (Fig. 2a, Supplemental Table 1). In the cerebellum, 10,011 genes were differentially expressed with 4870 genes upregulated and 5141 genes downregulated in cases compared to controls (Fig. 2b, Supplemental Table 2). Ingenuity pathway analysis (IPA) was used for pathway analysis for all cerebellum and temporal cortex DEGs (Supplemental Tables 3 and 4). The top signaling pathways included activation of the generic transcription, sirtuin, cristae formation, WDR5 histone modification, and tp53 phosphorylation pathways. The five signaling pathways with the lowest p values from each brain region are shown in Fig. 2e.
Fig. 2.
Genes within the 17q21.31 locus are differentially expressed between progressive supranuclear palsy cases and controls. 10,011 genes were differentially expressed in the cerebellum (a) and 3579 genes were differentially expressed in the temporal cortex (b; p < 0.05, FDR adjusted). (c, d) MAPT, KANSL1, NSF, PLEKHM1, LRRC37A, and ARHGAP27 were differentially expressed in the cerebellum. KANSL1, PLEKHM1, LRRC37A, and ARHGAP27 were differentially expressed in the temporal cortex. ARL17A and CRHR1 were not differentially expressed in either brain region. e Map of the MAPT locus with location of genes examined. f IPA pathway analysis of top 5 canonical pathways from both the cerebellum and temporal cortex in order of p value, with z-score displayed
Given the established strong association of the 17q21.31 MAPT locus with PSP, we next focused on the genes within the region (Fig. 2c–e, Table 2). We found that in the cerebellum, a region vulnerable to degeneration in PSP, nearly every gene in the 17q21.31 locus was differentially expressed, including MAPT, KANSL1, NSF, PLEKHM1, ARL17B, LRRC37A, and ARHGAP27. The only genes at the locus that were not differentially expressed were ARL17A and CRHR1. In the temporal cortex, which is typically unaffected by PSP, there was differential expression of KANSL1, PLEHKM1, LRRC37A, and ARGHAP27. MAPT was not differentially expressed in this region but showed a trending increase in expression (p = 0.06, FDR adjusted).
Table 2.
Differentially expressed genes in the MAPT 17q.21.31 locus
| Gene | Cerebellum | Temporal cortex | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| logFC | Average Expression | t-statistic | p value | FDR adjusted p value | Beta | LogFC | Average Expression | t-statistic | p value | FDR adjusted p value | Beta | |
| MAPT | 0.279 | 8.898 | 6.698 | 3.53 × 10−10 | 6.91 × 10−8 | 12.783 | 0.159 | 8.789 | 2.537 | 0.012 | 0.064 | − 3.356 |
| KANSL1 | 0.268 | 6.754 | 5.615 | 8.67 × 10−8 | 2.56 × 10−6 | 7.432 | 0.182 | 5.533 | 3.834 | 1.82 × 10−4 | 4.09 × 10−3 | 0.297 |
| NSF | − 0.182 | 7.471 | − 2.409 | 0.017 | 0.039 | − 4.010 | − 0.115 | 7.830 | − 0.836 | 0.404 | 0.614 | − 6.166 |
| PLEKHM1 | 0.406 | 5.895 | 6.682 | 3.86 × 10−10 | 7.33 × 10−8 | 12.679 | 0.240 | 4.916 | 4.531 | 1.15 × 10−5 | 6.93 × 10−4 | 2.892 |
| ARL17A | 0.023 | 5.007 | 0.264 | 0.792 | 0.848 | − 6.775 | − 0.014 | 3.887 | − 0.151 | 0.880 | 0.940 | − 6.545 |
| LRRC37A | − 0.576 | 3.113 | − 3.951 | 1.17 × 10−4 | 6.28 × 10−4 | 0.797 | − 0.606 | 2.312 | − 3.474 | 6.63 × 10−4 | 9.24 × 10−4 | − 0.646 |
| ARHGAP27 | − 0.195 | 3.869 | − 2.379 | 0.019 | 0.041 | − 3.911 | − 0.242 | 3.537 | − 2.688 | 7.96 × 10−3 | 0.048 | − 3.024 |
| CRHR1 | − 0.141 | 4.523 | − 1.108 | 0.270 | 0.370 | − 6.151 | − 0.021 | 2.887 | − 0.143 | 0.887 | 0.944 | − 6.381 |
| ARL17B | 0.280 | 2.843 | 3.042 | 2.76 × 10−3 | 8.50 × 10−3 | − 2.066 | 0.099 | 1.963 | 0.988 | 0.325 | 0.537 | − 5.764 |
FC Fold change
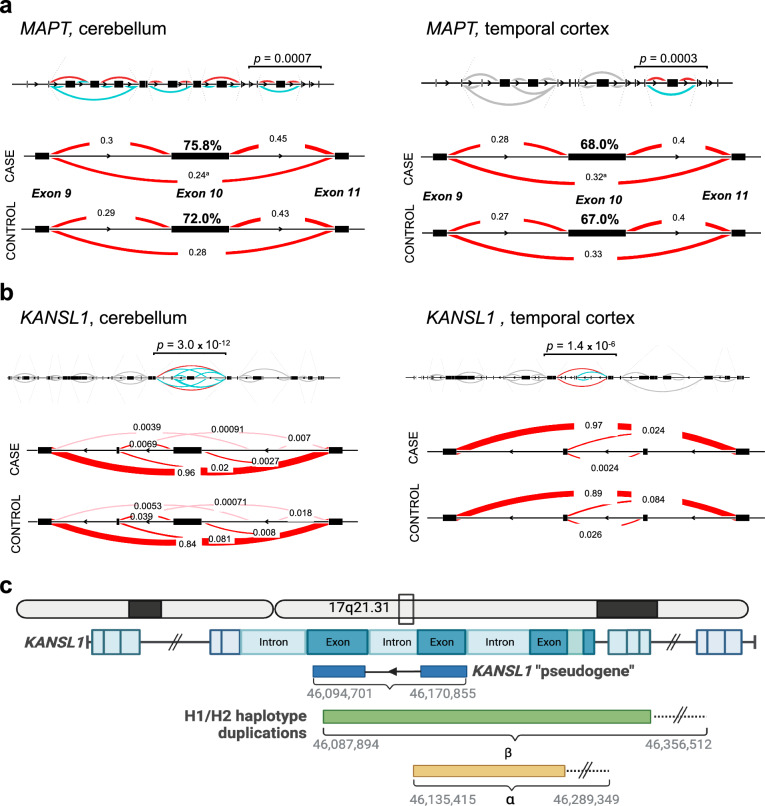
Next, we employed LeafCutter to assess differential intron excision. In total, we found differential detection of intron–exon junctions in 7214 locations in the cortex and 18,802 in the cerebellum between PSP cases and controls. At the 17q21.31 locus, we detected significant differential detection of intron–exon junctions in MAPT and KANSL1 (Fig. 3a, b) as well as ARHGAP27, LRRC37A, NSF, and ARL17A (Supplemental Fig. 3) in both brain regions. The differences in intron–exon junction detection in MAPT at exon 10 indicate greater levels of 4R tau mRNA in the PSP cases compared to controls. Additionally, there was differential detection of intron–exon junctions at KANSL1 in both brain regions. The KANSL1 transcript start and end points contain breakpoints of known duplications associated with the H1/H2 haplotypes, termed α and β duplication regions [19, 23, 24]. Thus, the differences in KANSL1 exon utilization may reflect the presence of a transcribed “pseudogene” [25].
Fig. 3.
Differential alternative pre-mRNA splicing of MAPT and KANSL1 in PSP cases compared to controls. a Full MAPT gene with differential inclusion of exon 10 in both brain regions for PSP cases compared to controls. (FDR adj. p = 0.0007 in cerebellum, FDR adj. p = 0.0003 in temporal cortex). Red lines represent introns annoted in GENCODE, pink lines are novel introns. Each number corresponding to a line represents the relative junction usage within the cluster. b Full KANSL1 gene with differential inclusion of an intron–exon junction in both brain regions (FDR adj. p = 3.0 × 10−13 in cerebellum, FDR adj. p = 0.000001 in temporal cortex). Hg38 Chr17: 46,094,701–46,170,855. c Schematic of H1/H2 haplotype breakpoints occurring within the KANSL1 gene, with potential KANSL1 pseudogene overlaid
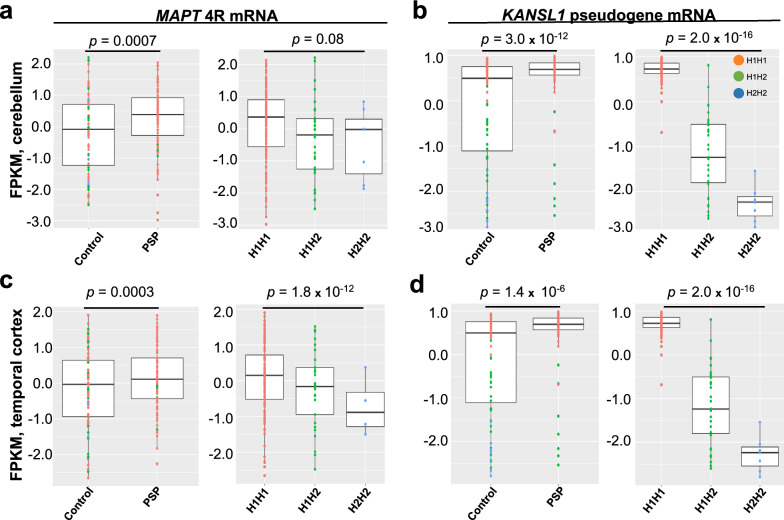
Finally, to assess the underlying basis of our observed differences in MAPT and KANSL1 in PSP, we examined whether the intron–exon junction differences we observed correlate with MAPT haplotype status (Fig. 4). Samples were stratified by haplotype status into H1 homozygotes (n = 77 PSP, n = 44 controls), H1/H2 heterozygotes (n = 7 PSP, n = 22 controls), and H2 homozygotes (n = 0 PSP, n = 4 controls). MAPT exon 10 inclusion was significantly associated with haplotype in the temporal cortex but not in the cerebellum (p = 1.8 × 10−12, p = 0.08 respectively) whereas the KANSL1 isoform was significantly associated with haplotype in both brain regions (p = 1.0 × 10−16, p = 2.0 × 10−16 respectively). When stratifying by status, haplotype is significantly associated with 4R MAPT and KANSL1 isoform for both cases and controls in the cerebellum. In the temporal cortex, the KANSL1 isoform is significantly associated with haplotype but 4R MAPT is not (Supplemental Fig. 5).
Fig. 4.
17q21.31 H1 haplotype and progressive supranuclear palsy are both associated with increased 4R tau mRNA and KANSL1 mRNA isoform expression. Patient haplotype information was determined using the SNP tag at rs1800547. H1 homozygous individuals are shown in orange (n = 77 PSP, n = 44 controls), H1/H2 heterozygous in green (n = 7 PSP, n = 22 controls), and H2 homozygous in blue (n = 0 PSP, n = 4 controls). q values are FDR-adjusted p values and were used to determine significance between cases and controls for each isoform. For haplotype-associated isoform and pseudogene expression analysis, a one-way ANOVA was performed
Discussion
The strong association of PSP and other tauopathies with common variation in the 17q21.31 locus in the absence of a MAPT coding region mutation favors genetic regulatory mechanisms as a causal driver [15–17, 37, 51–60]. The hypothesis that alterations in tau mRNA level drive pathology is supported by extensive data, including the observation that duplication of genomic regions including MAPT, which increases tau mRNA levels in a dose dependent fashion, is sufficient to cause tauopathy [61]. Here, we tested the hypothesis that increased levels of MAPT mRNA and/or changes in alternative MAPT pre-mRNA splicing are drivers of disease in PSP by re-examining a bulk RNA sequencing dataset derived from post-mortem human brain tissues using a rigorous computational transcriptomic pipeline. A key component of this analysis was the LeafCutter algorithm that allowed us to assess mRNA expression at relevant splice junctions. The most important finding was that there are increased levels of both total and 4R tau mRNA in the brain tissue of patients with autopsy-confirmed PSP in the cerebellum but not the temporal cortex, indicating MAPT-specific expression changes in a brain region more vulnerable to degeneration in this disease. These findings suggest a causal mechanism whereby toxic tau accumulation in PSP arises secondarily to increased total tau and 4R tau synthesis.
We also identified a KANSL1 transcript strongly associated with PSP and the H1 haplotype, which arises from transcription of a KANSL1 pseudogene resulting from the H1-haplotype-associated β duplication. Whether this pseudogene is translated and plays a functional role in PSP pathogenesis remains an open question. KANSL1 is a critical gene in neurological development and function, as highlighted by its involvement in Koolen de Vries syndrome (KdVS) [62–65]. KdVS, caused by deletions or mutations in the KANSL1 gene, is characterized by developmental delays, intellectual disability, and distinct facial features, underscoring the importance of KANSL1 in brain development and cognitive function [66, 67]. The association of KANSL1 disruptions with such a profound developmental disorder emphasizes the potential impact of KANSL1-related mechanisms in neurodegenerative diseases like PSP. The gene’s role in KdVS illustrates its broad influence on neurodevelopment, which could provide insights into how its dysregulation may contribute to tauopathies. Understanding the specific contributions of the KANSL1 pseudogene in PSP could, therefore, reveal critical pathways and targets for therapeutic intervention, further underscoring the significant role of KANSL1 in neuronal function.
There are limitations to this study that influence the interpretation of our results. First, the dataset had only the temporal cortex and cerebellum, but PSP involves numerous brain regions, including the subthalamic nucleus, globus pallidus, and substantia nigra which were not sampled here [28, 68]. Another limitation of the study is the dataset was derived from bulk-tissue analysis. RNA-seq studies suffer from the inability to resolve cellular heterogeneity. Using estimates based on canonical markers of neurons and glia, we found that there were significant differences in the cellular composition of our tissue. We were unable to control for these differences due to lack of ability to validate the proportions in the original tissue. Studies with greater cell-type specificity are needed to elucidate cell-specific gene expression changes. To this point, recently published single-cell RNA-seq datasets have emerged that implicate specific cell types in the observed differences in MAPT expression [31, 69, 70], and further studies are warranted. Additionally, advanced isoform-specific in situ hybridization techniques have allowed for the ability to validate RNA sequencing in post-mortem human tissues, although challenges have arisen in validating the specificity of these probes which would greatly strengthen this study as validation. Additionally, we used differential splicing analysis, Leafcutter, a software tool used to detect differences in intron–exon junctions but may not be as specific as long-read sequencing for detecting differences in isoform prevalence [71]. This analysis also should be validated through an additional splicing detection method. Lastly, we did not look at 17q21.31 sub-haplotypes (i.e. alpha, beta, gamma) and other structural variations that may play a role in gene expression changes. Given these limitations we are planning to complete these experiments as follow up studies.
Here, we provided further evidence supporting the argument that in regions vulnerable to disease, increased synthesis of tau, rather than dysregulated tau degradation, is a critical pathogenic aspect of abnormal tau proteostasis in PSP. These findings suggest that the reduction of tau synthesis may be of utility in treating tauopathy. There are currently several therapeutics targeting tau in phase 1, 2, and 3 clinical trials including monoclonal antibodies, tau-aggregation inhibitors, immunotherapy, and mRNA-based therapies [3, 71–75]. The nuanced understanding of the relationship between tau isoform expression, disease pathology and common genetic variation is integral for development of precision medicine approaches in tauopathy. As such, future research should continue to explore the therapeutic efficacy of these approaches, potentially combining them with other strategies aimed at mitigating neurodegeneration. Overall, the insights gained from this study highlight the importance of ongoing research into the molecular underpinnings of tauopathies and reinforce the promise of targeted therapeutic interventions in the context of rebalancing tau isoform levels.
Supplementary Information
Acknowledgements
We acknowledge the following funding sources: NIH Grants, R01AG054008, RF1NS095252, R01NS086736, P30AG066514, R01AG062348, K01AG070326, U54NS115266, T35AG067578, Rainwater Charitable Foundation, CurePSP Pathway Grant (685–2023-06) and a generous gift from Stuart Katz and Jane Martin (J.F.C. and K.F.). NIH National Institute of Neurological Disorders and Stroke grant U54NS123743 (J.H., T.R.).
Author contributions
HWR ran the analysis, gathered the data, drafted the manuscript, and designed the project. JH assisted on the analysis and edited the manuscript and assisted in project design. RA, and BB assisted in the analysis, TR assisted in the design and funded the project, DD and NT provided the data. KF and JC edited the manuscript, funded the project and designed the project.
Availability of data and materials
All the data used in this study was taken from publicly available sources detailed in the methods section of the manuscript and the final processed data is available in the supplementary material.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors have consented for publication.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
John F. Crary, Email: john.crary@mountsinai.org
Kurt Farrell, Email: kurt.farrell@mssm.edu.
References
- 1.Kovacs GG (2017) Tauopathies. Handb Clin Neurol 145:355–368. 10.1016/B978-0-12-802395-2.00025-0 10.1016/B978-0-12-802395-2.00025-0 [DOI] [PubMed] [Google Scholar]
- 2.Chang CW, Shao E, Mucke L (2021) Tau: enabler of diverse brain disorders and target of rapidly evolving therapeutic strategies. Science. 10.1126/science.abb8255 10.1126/science.abb8255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cummings JL, Gonzalez MI, Pritchard MC, May PC, Toledo-Sherman LM, Harris GA (2023) The therapeutic landscape of tauopathies: challenges and prospects. Alzheimers Res Ther 15(1):168. 10.1186/s13195-023-01321-7 10.1186/s13195-023-01321-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leveille E, Ross OA, Gan-Or Z (2021) Tau and MAPT genetics in tauopathies and synucleinopathies. Parkinsonism Relat Disord 90:142–154. 10.1016/j.parkreldis.2021.09.008 10.1016/j.parkreldis.2021.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poorkaj P, Bird TD, Wijsman E, Nemens E, Garruto RM, Anderson L et al (1998) Tau is a candidate gene for chromosome 17 frontotemporal dementia. Ann Neurol 43(6):815–825. 10.1002/ana.410430617 10.1002/ana.410430617 [DOI] [PubMed] [Google Scholar]
- 6.Ghetti B, Oblak AL, Boeve BF, Johnson KA, Dickerson BC, Goedert M (2015) Invited review: frontotemporal dementia caused by microtubule-associated protein tau gene (MAPT) mutations: a chameleon for neuropathology and neuroimaging. Neuropathol Appl Neurobiol 41(1):24–46. 10.1111/nan.12213 10.1111/nan.12213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hutton M, Lendon CL, Rizzu P, Baker M, Froelich S, Houlden H et al (1998) Association of missense and 5’-splice-site mutations in tau with the inherited dementia FTDP-17. Nature 393(6686):702–705. 10.1038/31508 10.1038/31508 [DOI] [PubMed] [Google Scholar]
- 8.Corsi A, Bombieri C, Valenti MT, Romanelli MG (2022) Tau isoforms: gaining insight into MAPT alternative splicing. Int J Mol Sci. 10.3390/ijms232315383 10.3390/ijms232315383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flament S, Delacourte A, Verny M, Hauw JJ, Javoy-Agid F (1991) Abnormal Tau proteins in progressive supranuclear palsy. Similarities and differences with the neurofibrillary degeneration of the Alzheimer type. Acta Neuropathol. 81(6):591–596. 10.1007/BF00296367 10.1007/BF00296367 [DOI] [PubMed] [Google Scholar]
- 10.Takanashi M, Mori H, Arima K, Mizuno Y, Hattori N (2002) Expression patterns of tau mRNA isoforms correlate with susceptible lesions in progressive supranuclear palsy and corticobasal degeneration. Brain Res Mol Brain Res 104(2):210–219. 10.1016/s0169-328x(02)00382-0 10.1016/s0169-328x(02)00382-0 [DOI] [PubMed] [Google Scholar]
- 11.Goedert M, Spillantini MG, Jakes R, Rutherford D, Crowther RA (1989) Multiple isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer’s disease. Neuron 3(4):519–526. 10.1016/0896-6273(89)90210-9 10.1016/0896-6273(89)90210-9 [DOI] [PubMed] [Google Scholar]
- 12.Goedert M, Spillantini MG, Potier MC, Ulrich J, Crowther RA (1989) Cloning and sequencing of the cDNA encoding an isoform of microtubule-associated protein tau containing four tandem repeats: differential expression of tau protein mRNAs in human brain. EMBO J 8(2):393–399. 10.1002/j.1460-2075.1989.tb03390.x 10.1002/j.1460-2075.1989.tb03390.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andreadis A, Brown WM, Kosik KS (1992) Structure and novel exons of the human tau gene. Biochemistry 31(43):10626–10633. 10.1021/bi00158a027 10.1021/bi00158a027 [DOI] [PubMed] [Google Scholar]
- 14.Dayanandan R, Van Slegtenhorst M, Mack TG, Ko L, Yen SH, Leroy K et al (1999) Mutations in tau reduce its microtubule binding properties in intact cells and affect its phosphorylation. FEBS Lett 446(2–3):228–232. 10.1016/s0014-5793(99)00222-7 10.1016/s0014-5793(99)00222-7 [DOI] [PubMed] [Google Scholar]
- 15.Hoglinger GU, Melhem NM, Dickson DW, Sleiman PM, Wang LS, Klei L et al (2011) Identification of common variants influencing risk of the tauopathy progressive supranuclear palsy. Nat Genet 43(7):699–705. 10.1038/ng.859 10.1038/ng.859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang H, Chang TS, Dombroski BA, Cheng PL, Patil V, Valiente-Banuet L et al (2024) Whole-genome sequencing analysis reveals new susceptibility loci and structural variants associated with progressive supranuclear palsy. medRxiv. 10.1101/2023.12.28.23300612 10.1101/2023.12.28.23300612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farrell K, Humphrey J, Chang T, Zhao Y, Leung YY, Kuksa PP et al (2023) Genetic, transcriptomic, histological, and biochemical analysis of progressive supranuclear palsy implicates glial activation and novel risk genes. bioRxiv. 10.1101/2023.11.09.56555238234833 10.1101/2023.11.09.565552 [DOI] [Google Scholar]
- 18.Baker M, Litvan I, Houlden H, Adamson J, Dickson D, Perez-Tur J et al (1999) Association of an extended haplotype in the tau gene with progressive supranuclear palsy. Hum Mol Genet 8(4):711–715. 10.1093/hmg/8.4.711 10.1093/hmg/8.4.711 [DOI] [PubMed] [Google Scholar]
- 19.Boettger LM, Handsaker RE, Zody MC, McCarroll SA (2012) Structural haplotypes and recent evolution of the human 17q21.31 region. Nat Genet. 44(8):881–885. 10.1038/ng.2334 10.1038/ng.2334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bowles KR, Pugh DA, Liu Y, Patel T, Renton AE, Bandres-Ciga S et al (2022) 17q21.31 sub-haplotypes underlying H1-associated risk for Parkinson’s disease are associated with LRRC37A/2 expression in astrocytes. Mol Neurodegener. 17(1):48. 10.1186/s13024-022-00551-x 10.1186/s13024-022-00551-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caffrey TM, Wade-Martins R (2007) Functional haplotypes: bridging the gap between genotype and neuropathology. Neurobiol Dis 27(1):1–10. 10.1016/j.nbd.2007.04.006 10.1016/j.nbd.2007.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers AJ, Pittman AM, Zhao AS, Rohrer K, Kaleem M, Marlowe L et al (2007) The H1c risk haplotype is associated with increased expression of tau and especially of 4 repeat containing transcripts. Neurobiol Dis 25(3):561–570. 10.1016/j.nbd.2006.10.018 10.1016/j.nbd.2006.10.018 [DOI] [PubMed] [Google Scholar]
- 23.Zody MC, Jiang Z, Fung HC, Antonacci F, Hillier LW, Cardone MF et al (2008) Evolutionary toggling of the MAPT 17q21.31 inversion region. Nat Genet. 40(9):1076–1083. 10.1038/ng.193 10.1038/ng.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pedicone C, Weitzman SA, Renton AE, Goate AM (2024) Unraveling the complex role of MAPT-containing H1 and H2 haplotypes in neurodegenerative diseases. Mol Neurodegener 19(1):43. 10.1186/s13024-024-00731-x 10.1186/s13024-024-00731-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campoy E, Puig M, Yakymenko I, Lerga-Jaso J, Caceres M (2022) Genomic architecture and functional effects of potential human inversion supergenes. Philos Trans R Soc B. 10.1098/rstb.2021.0209 10.1098/rstb.2021.0209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Silva R, Lashley T, Strand C, Shiarli AM, Shi J, Tian JZ et al (2006) An immunohistochemical study of cases of sporadic and inherited frontotemporal lobar degeneration using 3R-and 4R-specific tau monoclonal antibodies. Acta Neuropathol 111(4):329–340. 10.1007/s00401-006-0048-x 10.1007/s00401-006-0048-x [DOI] [PubMed] [Google Scholar]
- 27.Kametani F, Yoshida M, Matsubara T, Murayama S, Saito Y, Kawakami I et al (2020) Comparison of common and disease-specific post-translational modifications of pathological Tau associated with a wide range of tauopathies. Front Neurosci-Switz. 10.3389/fnins.2020.581936 10.3389/fnins.2020.581936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roemer SF, Grinberg LT, Crary JF, Seeley WW, McKee AC, Kovacs GG et al (2022) Rainwater Charitable Foundation criteria for the neuropathologic diagnosis of progressive supranuclear palsy. Acta Neuropathol 144(4):603–614. 10.1007/s00401-022-02479-4 10.1007/s00401-022-02479-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chambers CB, Lee JM, Troncoso JC, Reich S, Muma NA (1999) Overexpression of four-repeat tau mRNA isoforms in progressive supranuclear palsy but not in Alzheimer’s disease. Ann Neurol 46(3):325–332. 10.1002/1531-8249(199909)46:3%3c325::aid-ana8%3e3.0.co;2-v [DOI] [PubMed] [Google Scholar]
- 30.Ingelsson M, Ramasamy K, Russ C, Freeman SH, Orne J, Raju S et al (2007) Increase in the relative expression of tau with four microtubule binding repeat regions in frontotemporal lobar degeneration and progressive supranuclear palsy brains. Acta Neuropathol 114(5):471–479. 10.1007/s00401-007-0280-z 10.1007/s00401-007-0280-z [DOI] [PubMed] [Google Scholar]
- 31.Rexach JE, Cheng Y, Chen L, Polioudakis D, Lin LC, Mitri V et al (2023) Disease-specific selective vulnerability and neuroimmune pathways in dementia revealed by single cell genomics. bioRxiv. 10.1101/2023.09.29.560245 10.1101/2023.09.29.560245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Jong S, Chepelev I, Janson E, Strengman E, van den Berg LH, Veldink JH et al (2012) Common inversion polymorphism at 17q21.31 affects expression of multiple genes in tissue-specific manner. BMC Genomics. 10.1186/1471-2164-13-458 10.1186/1471-2164-13-458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tauber CV, Schwarz SC, Rösler TW, Arzberger T, Gentleman S, Windl O et al (2023) Different MAPT haplotypes influence expression of total MAPT in postmortem brain tissue. Acta Neuropathol Commun 11(1):40. 10.1186/s40478-023-01534-9 10.1186/s40478-023-01534-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Naiser T, Ehler O, Kayser J, Mai T, Michel W, Ott A (2008) Impact of point-mutations on the hybridization affinity of surface-bound DNA/DNA and RNA/DNA oligonucleotide-duplexes: comparison of single base mismatches and base bulges. BMC Biotechnol 8:48. 10.1186/1472-6750-8-48 10.1186/1472-6750-8-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trabzuni D, Wray S, Vandrovcova J, Ramasamy A, Walker R, Smith C et al (2012) expression and splicing is differentially regulated by brain region: relation to genotype and implication for tauopathies. Hum Mol Genet 21(18):4094–4103. 10.1093/hmg/dds238 10.1093/hmg/dds238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Allen M, Burgess JD, Ballard T, Serie D, Wang X, Younkin CS et al (2016) Gene expression, methylation and neuropathology correlations at progressive supranuclear palsy risk loci. Acta Neuropathol 132(2):197–211. 10.1007/s00401-016-1576-7 10.1007/s00401-016-1576-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Santa-Maria I, Haggiagi A, Liu XM, Wasserscheid J, Nelson PT, Dewar K et al (2012) The H1 haplotype is associated with tangle-predominant dementia. Acta Neuropathol 124(5):693–704. 10.1007/s00401-012-1017-1 10.1007/s00401-012-1017-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shah H, CW Y, Castellanos R, Pandya C, Giles Z (eds) (2015) RAPiD—an agile and dependable RNA-Seq framework. In: The 65th annual meeting of The American Society of Human Genetics
- 39.Bolger AM, Lohse M, Usadel B (2014) Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30(15):2114–2120. 10.1093/bioinformatics/btu170 10.1093/bioinformatics/btu170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S et al (2013) STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29(1):15–21. 10.1093/bioinformatics/bts635 10.1093/bioinformatics/bts635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.FastQC (2015)
- 42.Liao Y, Smyth GK, Shi W (2014) featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30(7):923–930. 10.1093/bioinformatics/btt656 10.1093/bioinformatics/btt656 [DOI] [PubMed] [Google Scholar]
- 43.Institute B. Picard (2023)
- 44.Li B, Dewey CN (2011) RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinform. 10.1186/1471-2105-12-323 10.1186/1471-2105-12-323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li YI, Knowles DA, Humphrey J, Barbeira AN, Dickinson SP, Im HK et al (2018) Annotation-free quantification of RNA splicing using LeafCutter. Nat Genet 50(1):151–158. 10.1038/s41588-017-0004-9 10.1038/s41588-017-0004-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Law CW, Chen Y, Shi W, Smyth GK (2014) voom: precision weights unlock linear model analysis tools for RNA-seq read counts. Genome Biol 15(2):R29. 10.1186/gb-2014-15-2-r29 10.1186/gb-2014-15-2-r29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoffman GE, Schadt EE (2016) variancePartition: interpreting drivers of variation in complex gene expression studies. BMC Bioinform 17(1):483. 10.1186/s12859-016-1323-z 10.1186/s12859-016-1323-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCarthy DJ, Smyth GK (2009) Testing significance relative to a fold-change threshold is a TREAT. Bioinformatics 25(6):765–771. 10.1093/bioinformatics/btp053 10.1093/bioinformatics/btp053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McKenzie AT, Wang M, Hauberg ME, Fullard JF, Kozlenkov A, Keenan A et al (2018) Brain cell type specific gene expression and co-expression network architectures. Sci Rep 8(1):8868. 10.1038/s41598-018-27293-5 10.1038/s41598-018-27293-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Allen M, Carrasquillo MM, Funk C, Heavner BD, Zou F, Younkin CS et al (2016) Human whole genome genotype and transcriptome data for Alzheimer’s and other neurodegenerative diseases. Sci Data 3:160089. 10.1038/sdata.2016.89 10.1038/sdata.2016.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Conrad C, Andreadis A, Trojanowski JQ, Dickson DW, Kang D, Chen X et al (1997) Genetic evidence for the involvement of tau in progressive supranuclear palsy. Ann Neurol 41(2):277–281. 10.1002/ana.410410222 10.1002/ana.410410222 [DOI] [PubMed] [Google Scholar]
- 52.Farrell K, Kim S, Han N, Iida MA, Gonzalez EM, Otero-Garcia M et al (2022) Genome-wide association study and functional validation implicates JADE1 in tauopathy. Acta Neuropathol 143(1):33–53. 10.1007/s00401-021-02379-z 10.1007/s00401-021-02379-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen JA, Chen Z, Won H, Huang AY, Lowe JK, Wojta K et al (2018) Joint genome-wide association study of progressive supranuclear palsy identifies novel susceptibility loci and genetic correlation to neurodegenerative diseases. Mol Neurodegener 13(1):41. 10.1186/s13024-018-0270-8 10.1186/s13024-018-0270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jabbari E, Koga S, Valentino RR, Reynolds RH, Ferrari R, Tan MMX et al (2021) Genetic determinants of survival in progressive supranuclear palsy: a genome-wide association study. Lancet Neurol 20(2):107–116. 10.1016/S1474-4422(20)30394-X 10.1016/S1474-4422(20)30394-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sanchez-Contreras MY, Kouri N, Cook CN, Serie DJ, Heckman MG, Finch NA et al (2018) Replication of progressive supranuclear palsy genome-wide association study identifies and as new susceptibility loci. Mol Neurodegener. 10.1186/s13024-018-0267-3 10.1186/s13024-018-0267-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Valentino RR, Scotton WJ, Roemer SF, Lashley T, Heckman MG, Shoai M et al (2024) MAPT H2 haplotype and risk of Pick’s disease in the Pick’s disease International Consortium: a genetic association study. Lancet Neurol 23(5):487–499. 10.1016/S1474-4422(24)00083-8 10.1016/S1474-4422(24)00083-8 [DOI] [PubMed] [Google Scholar]
- 57.Kouri N, Ross OA, Dombroski B, Younkin CS, Serie DJ, Soto-Ortolaza A et al (2015) Genome-wide association study of corticobasal degeneration identifies risk variants shared with progressive supranuclear palsy. Nat Commun 6:7247. 10.1038/ncomms8247 10.1038/ncomms8247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Strickland SL, Reddy JS, Allen M, N’Songo A, Burgess JD, Corda MM et al (2020) MAPT haplotype-stratified GWAS reveals differential association for AD risk variants. Alzheimers Dement 16(7):983–1002. 10.1002/alz.12099 10.1002/alz.12099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Allen M, Kachadoorian M, Quicksall Z, Zou F, Chai HS, Younkin C et al (2014) Association of MAPT haplotypes with Alzheimer’s disease risk and MAPT brain gene expression levels. Alzheimers Res Ther 6(4):39. 10.1186/alzrt268 10.1186/alzrt268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Valentino RR, Koga S, Walton RL, Soto-Beasley AI, Kouri N, DeTure MA et al (2020) MAPT subhaplotypes in corticobasal degeneration: assessing associations with disease risk, severity of tau pathology, and clinical features. Acta Neuropathol Commun 8(1):218. 10.1186/s40478-020-01097-z 10.1186/s40478-020-01097-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wallon D, Boluda S, Rovelet-Lecrux A, Thierry M, Lagarde J, Miguel L et al (2021) Clinical and neuropathological diversity of tauopathy in MAPT duplication carriers. Acta Neuropathol 142(2):259–278. 10.1007/s00401-021-02320-4 10.1007/s00401-021-02320-4 [DOI] [PubMed] [Google Scholar]
- 62.Ciaccio C, Dordoni C, Ritelli M, Colombi M (2016) Koolen–de Vries syndrome: clinical report of an adult and literature review. Cytogenet Genome Res 150(1):40–45. 10.1159/000452724 10.1159/000452724 [DOI] [PubMed] [Google Scholar]
- 63.Koolen DA, Pfundt R, Linda K, Beunders G, Veenstra-Knol HE, Conta JH et al (2016) The Koolen–de Vries syndrome: a phenotypic comparison of patients with a 17q21.31 microdeletion versus a KANSL1 sequence variant. Eur J Hum Genet. 24(5):652–659. 10.1038/ejhg.2015.178 10.1038/ejhg.2015.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brand F, Vijayananth A, Hsieh TC, Schmidt A, Peters S, Mangold E et al (2022) Next-generation phenotyping contributing to the identification of a 4.7 kb deletion in KANSL1 causing Koolen–de Vries syndrome. Hum Mutat. 43(11):1659–1665. 10.1002/humu.24467 10.1002/humu.24467 [DOI] [PubMed] [Google Scholar]
- 65.Bernardo P, Madia F, Santulli L, Del Gaudio L, Caccavale C, Zara F et al (2016) 17q21.31 microdeletion syndrome: description of a case further contributing to the delineation of Koolen–de Vries syndrome. Brain Dev-Jpn 38(7):663–668. 10.1016/j.braindev.2016.02.002 10.1016/j.braindev.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 66.Lupski JR (2006) Genome structural variation and sporadic disease traits. Nat Genet 38(9):974–976. 10.1038/ng0906-974 10.1038/ng0906-974 [DOI] [PubMed] [Google Scholar]
- 67.Tan TY, Aftimos S, Worgan L, Susman R, Wilson M, Ghedia S et al (2009) Phenotypic expansion and further characterisation of the 17q21.31 microdeletion syndrome. J Med Genet. 46(7):480–489. 10.1136/jmg.2008.065391 10.1136/jmg.2008.065391 [DOI] [PubMed] [Google Scholar]
- 68.Kovacs GG (2020) Astroglia and tau: new perspectives. Front Aging Neurosci 12:96. 10.3389/fnagi.2020.00096 10.3389/fnagi.2020.00096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Forrest S, Lee S, Martinez-Valbuena I, Sackmann V, Li J, Ittner L, et al (2023) Cell-specific MAPT gene expression is preserved in neuronal and glial tau cytopathologies in progressive supranuclear palsy. Brain Pathol 33 [DOI] [PMC free article] [PubMed]
- 70.Whitney K, Song WM, Sharma A, Dangoor DK, Farrell K, Krassner MM et al (2023) Single-cell transcriptomic and neuropathologic analysis reveals dysregulation of the integrated stress response in progressive supranuclear palsy. bioRxiv. 10.1101/2023.11.17.567587 10.1101/2023.11.17.567587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.DeVos SL, Miller RL, Schoch KM, Holmes BB, Kebodeaux CS, Wegener AJ et al (2017) Tau reduction prevents neuronal loss and reverses pathological tau deposition and seeding in mice with tauopathy. Sci Transl Med. 10.1126/scitranslmed.aag0481 10.1126/scitranslmed.aag0481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mummery CJ, Börjesson-Hanson A, Blackburn DJ, Vijverberg EGB, De Deyn PP, Ducharme S et al (2023) Tau-targeting antisense oligonucleotide MAPT in mild Alzheimer’s disease: a phase 1b, randomized, placebo-controlled trial. Nat Med 29(6):1437. 10.1038/s41591-023-02326-3 10.1038/s41591-023-02326-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Florian H, Wang D, Arnold SE, Boada M, Guo Q, Jin Z et al (2023) Tilavonemab in early Alzheimer’s disease: results from a phase 2, randomized, double-blind study. Brain 146(6):2275–2284. 10.1093/brain/awad024 10.1093/brain/awad024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Monteiro C, Toth B, Brunstein F, Bobbala A, Datta S, Ceniceros R et al (2023) Randomized phase II study of the safety and efficacy of semorinemab in participants with mild-to-moderate Alzheimer disease: Lauriet. Neurology 101(14):e1391–e1401. 10.1212/WNL.0000000000207663 10.1212/WNL.0000000000207663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Callizot N, Estrella C, Burlet S, Henriques A, Brantis C, Barrier M et al (2021) AZP2006, a new promising treatment for Alzheimer’s and related diseases. Sci Rep 11(1):16806. 10.1038/s41598-021-94708-1 10.1038/s41598-021-94708-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data used in this study was taken from publicly available sources detailed in the methods section of the manuscript and the final processed data is available in the supplementary material.