A year into the coronavirus disease 2019 (COVID-19) pandemic there remains an urgent need to limit severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread and to curb the pandemic in the US through nonpharmaceutical interventions. Clear evidence supports the effectiveness of simple strategies in identifying risks and mitigating the spread of infection, with much of this evidence coming from observational studies. Community risk factors for infection can be identified by comparing recent behaviors and exposures among people who have been infected with those who are not infected using a traditional case-control approach. High-risk environments identified from these investigations need to be clearly communicated to the public to support public health measures and motivate individual behavior change to reduce the risk of infection.
Key Lessons About Community Transmission of SARS-CoV-2
The importance of wearing masks and the clustering of transmission have been shown with COVID-19, with 20% of infected individuals estimated to cause about 80% of SARS-CoV-2 transmissions.1 About 50% of transmissions are thought to occur from asymptomatic or pre-symptomatic persons.2 This presents an important challenge for prevention because it increases the propensity for community spread through diverse high-risk activities involving asymptomatic infected persons who unknowingly spread the virus.
Investigations of COVID-19 outbreaks have shown that the factors influencing the risk of transmission vary across settings. However, these local factors occur in several well-established patterns that can be prevented when identified. For example, compared with well-ventilated outdoor spaces, the risk of infection is higher in poorly ventilated indoor spaces when there is prolonged duration of close contact (within 6 feet of someone for ≥15 minutes over a 24-hour period3) coupled with limited physical barrier to viral transmission because of inconsistent use of masks.2 The context and intensity of exposure are key in the spread of SARS-CoV-2. Large outbreaks or superspreader events have generally been characterized by a confluence of these factors, such ascrowdedindoorspacescombinedwithlackofmaskuse.4Livingand working environments that are characterized by such factors may also contributetothegreaterincidenceofCOVID-19associatedwithrace/ethnicity, poverty, and zip code.2
Identifying Modifiable Behaviors Associated With Spread
Investigations begin with interviewing people who have the disease and tracing timelines of activities and contacts. COVID-19 control efforts in countries that succeeded in limiting early pandemic spread included frequent and strategic testing and use of extensive contact tracing to encourage or enforce quarantine precautions, along with consistent communication and government support for mitigation strategies, such as mask mandates, gathering restrictions, and occupancy limits in business sectors. Contact tracing is resource-intensive but remains critical in identifying, testing, and quarantining close contacts of confirmed COVID-19 cases. Close contact with a person known to be infected with SARS-CoV-2 remains one of the strongest predictors of eventually testing positive for infection. Traditional forward contact tracing can be complemented by “backward” tracing, in which individuals with SARS-CoV-2 are asked about recent prior activities and potential COVID-19 case contacts to identify upstream sources of infection, including potential superspreader events.5
In the context of current widespread community transmission of SARS-CoV-2 in the US, identifying potential sources of infection for individual cases or links between cases becomes more challenging because it can be resource-intensive for health departments. Investigations that employ a comparison group, including traditional case-control studies, become increasingly important for identifying modifiable factors to curb infections when transmission is widespread. Comparison groups provide contrast between common activities and exposures that increase risk of infection. Following easing of stay-at-home orders in mid-2020, Fisher et al6 performed a telephone survey of 314 adults across 10 states to compare exposures and behaviors among symptomatic patients whose test results were positive for SARS-CoV-2 and a control group of individuals evaluated for SARS-CoV-2 whose test results were negative. This was done to identify activities that were more common among cases than controls, indicating an increased risk of infection. In this investigation, an association was identified between SARS-CoV-2 infection and dining at restaurants and going to bars or coffee shops (Figure).6 What these activities share is that they are incompatible with continuous mask use when eating or drinking, they involve prolonged and intense exposure to others who could be infected and potentially asymptomatic, and they can be difficult to maintain safe distances during. A similar 2020 case-control investigation among 397 children in Mississippi found that gatherings with persons outside the household, such as social functions, during which people are less likely to wear masks or maintain social distance, were associated with positive SARS-CoV-2 test results.7 In contrast, attending school or childcare was not associated with positive SARS-CoV-2 test results, suggesting that risk may have been mitigated through regular mask use by staff and children along with other safety measures in the facilities.
Figure. Community Exposures Associated With Confirmed COVID-19 Among Symptomatic Adults (N = 314) in the US, July 1–29, 2020.
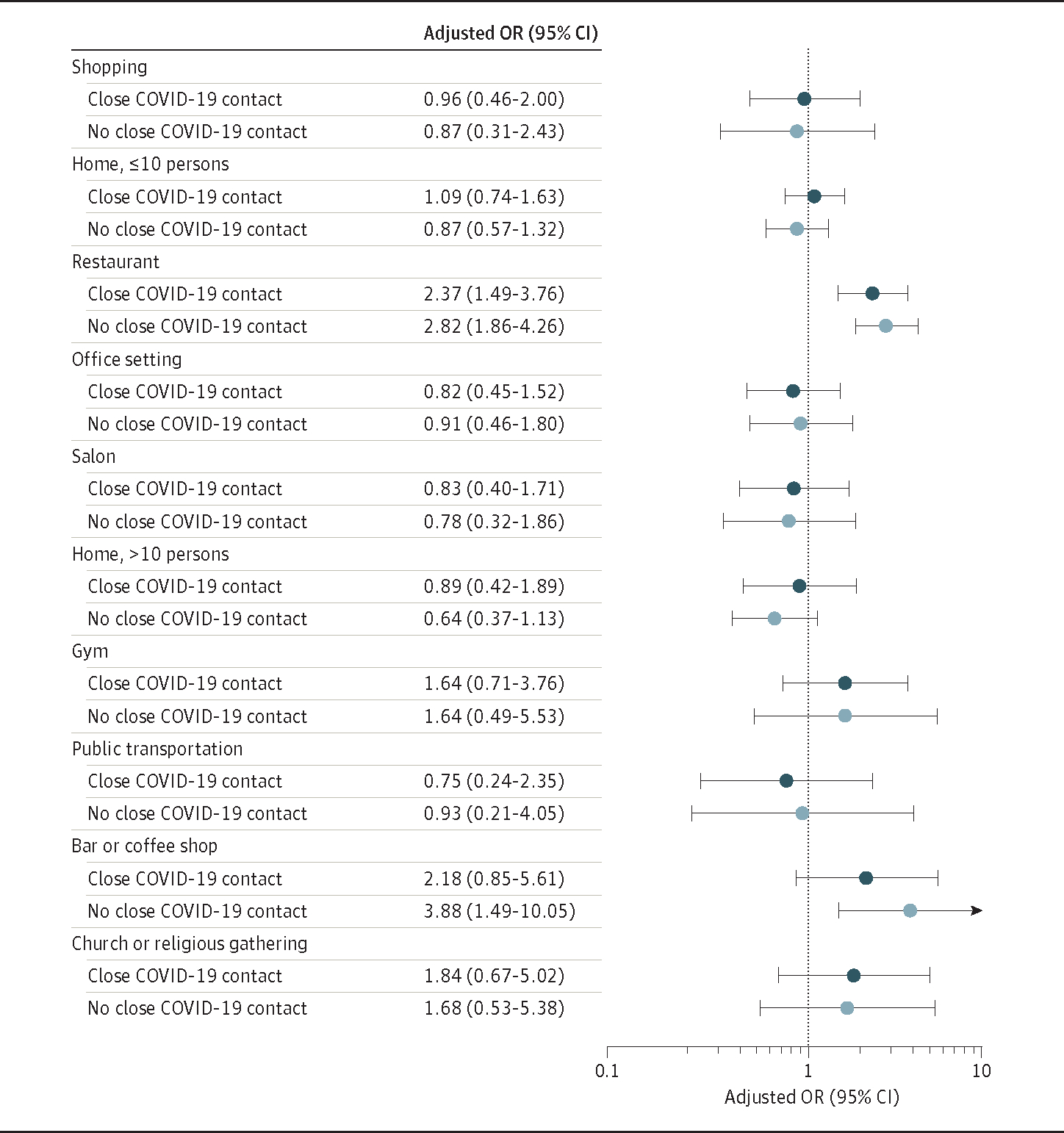
Odds ratios (ORs) represent comparison of exposures by symptomatic patients (n = 154) who tested positive for SARS-CoV-2 and a control group (n = 160) who tested negative. ORs were adjusted for race/ethnicity, sex, age, and reporting ≥1 underlying chronic medical condition. ORs were estimated using unconditional logistic regression with generalized estimating equations, which accounted for Influenza Vaccine Effectiveness in the Critically Ill Network site–level clustering. A second model was restricted to participants who did not report close contact to a person known to have COVID-19 (n = 225). Community exposure questions are specified in the MMWR publication.6 Responses were coded as “never” vs “at least once.” This figure was adapted from Fisher et al.6
Findings from local investigations to identify behaviors or activities associated with increased risk can be used to focus mitigation strategies and inform communication messages. How and what risk factors are identified depends on case investigations, analysis of patterns of infection, and previous findings. Results from these studies can serve to complement evidence from other investigations, such as ecological studies using cell phone data to identify potential transmission hotspots.8
Providing Evidence to Support Mitigation Strategies
Approximately 500 000 deaths from COVID-19 have occurred in the US alone, and the pandemic continues to cause major personal, social, and economic consequences. The role of public health professionals is to provide science-based, data-driven recommendations in a timely manner to curb pandemic spread and prevent disease and deaths. Often, decisions made with the intent to reduce the disease burden during a pandemic are made with incomplete information. Effectiveness of mitigation strategies and adoption of recommended behaviors must be continually reevaluated throughout the pandemic, even as vaccination continues, and prevention strategies must be adapted to the current situation and local context, informed by local data, such as case-control investigations. A tremendous amount has been learned about SARS-CoV-2 transmission over the past year, and a greater awareness of transmission dynamics, including uneven spread of the virus within communities, can be used to guide targeted interventions and policies.
Additional Contributions:
We thank Brendan Flannery, PhD (Influenza Division, Centers for Disease Control and Prevention), for his critical input, for which he did not receive compensation.
Disclaimer:
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Conflict of Interest Disclosures: None reported.
REFERENCES
- 1.Adam DC, Wu P, Wong JY, et al. Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nat Med. 2020;26(11):1714–1719. [DOI] [PubMed] [Google Scholar]
- 2.Honein MA, Christie A, Rose DA, et al. Summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. MMWR Morb Mortal Wkly Rep. 2020;69(49):1860–1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pringle JC, Leikauskas J, Ransom-Kelley S, et al. COVID-19 in a correctional facility employee following multiple brief exposures to persons with COVID-19: Vermont, July-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1569–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang S, Pierson E, Koh PW, et al. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. 2021;589(7840):82–87. [DOI] [PubMed] [Google Scholar]
- 5.Mahale P, Rothfuss C, Bly S, et al. Multiple COVID-19 outbreaks linked to a wedding reception in rural Maine: August 7-September 14, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1686–1690. doi: 10.15585/mmwr.mm6945a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher KA, Tenforde MW, Feldstein LR, et al. Community and close contact exposures associated with COVID-19 among symptomatic adults 18 years in 11 outpatient health care facilities: United States, July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1258–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hobbs CV, Martin LM, Kim SS, et al. Factors associated with positive SARS-CoV-2 test results in outpatient health facilities and emergency departments among children and adolescents aged <18 years: Mississippi, September-November 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1925–1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grantz KH, Meredith HR, Cummings DAT, et al. The use of mobile phone data to inform analysis of COVID-19 pandemic epidemiology. Nat Commun. 2020;11(1):4961. doi: 10.1038/s41467-020-18190-5 [DOI] [PMC free article] [PubMed] [Google Scholar]


