Abstract
Background
In malaria-endemic countries, asymptomatic carriers of plasmodium represent an important reservoir for malaria transmission. Estimating the burden at a fine scale and identifying areas at high risk of asymptomatic carriage are important to guide malaria control strategies. This study aimed to estimate the prevalence of asymptomatic carriage at the communal level in Burkina Faso, the smallest geographical entity from which a local development policy can be driven.
Methods
The data used in this study came from several open sources: the 2018 Multiple Indicator Cluster Survey on Malaria and the 2019 general census of the population data and environmental. The analysis involved a total of 5489 children under 5 from the malaria survey and 293,715 children under 5 from the census. The Elbers Langjouw and Langjouw (ELL) approach is used to estimate the prevalence. This approach consists of including data from several sources (mainly census and survey data) in a statistical model to obtain predictive indicators at a sub-geographical level, which are not measured in the population census. The method achieves this by finding correlations between common census variables and survey data.
Findings
The findings suggest that the spatial distribution of the prevalence of asymptomatic carriage is very heterogeneous across the communes. It varies from a minimum of 5.1% (95% CI 3.6–6.5) in the commune of Bobo-Dioulasso to a maximum of 41.4% (95% CI 33.5–49.4) in the commune of Djigoué. Of the 341 communes, 208 (61%) had prevalences above the national average of 20.3% (95% CI 18.8–21.2).
Contributions
This analysis provided commune-level estimates of the prevalence of asymptomatic carriage of plasmodium in Burkina Faso. The results of this analysis should help to improve planning of malaria control at the communal level in Burkina Faso.
Keywords: Small area estimates, Communes, Malaria, Spatial analysis, Burkina Faso
Introduction
Numerous efforts have been made worldwide to fight malaria. These efforts have led to a significant reduction in malaria-related morbidity and mortality, especially among children under 5. However, morbidity and mortality remain below expectations. Indeed, severe malaria remains one of the main causes of mortality, contributing to 6% of malaria deaths in sub-Saharan Africa (SSA) [1].
In 2022, the West African sub-region had approximately 121 million estimated cases and approximately 324,000 estimated deaths: an increase of 2% and a decrease of 15% respectively compared to 2010 [2]. Five countries accounted for more than 80% of the estimated cases, including Burkina Faso with 7% of cases [2]. Globally, Burkina Faso is among the ten countries most affected by malaria (3.4% of cases and 3.2% of deaths worldwide in 2020) [3]. In Burkina Faso, several initiatives such as the distribution of long-acting insecticide-treated mosquito nets (LLINs), seasonal malaria chemoprevention (SMC), indoor residual spraying (IRS) and the use of artemisinin-based combination therapies (ACTs) have been implemented to reduce the incidence and mortality of malaria. However, as in other SSA countries, malaria remains a major public health problem in the country. In 2017, Ministry of Health statistics show that malaria was the main reason for consultations (53%), hospitalization (48%) and 66% of deaths of children under 5 in hospitals and health facilities [4].
In view of the persistence of high morbidity and mortality due to malaria, several studies have focused on different aspects of the malaria disease process [1, 4–9] including factors associated with transmission and spatio-temporal inequalities in morbidity. Most of this research is based on survey or routine data, sometimes geographically targeted [5, 10] giving rise to only a partial analysis of the national situation or to an analysis on a relatively large geographical scale [1, 4–6] or unstructured [7]. For example, Ouédraogo and al. [4] using data from the baseline survey on "Assessing the impact of results-based financing in Burkina Faso", identified districts at higher risk of asymptomatic malaria infection in children in 24 districts of Burkina Faso. Along the same line, Rouamba and al. [5] used a hierarchical Bayesian spatio-temporal modeling to explore spatio-temporal patterns to identify health districts with probably of severe malaria incidence during pregnancy and high rates of mortality from routine data between 2013 and 2018.
Current guidelines on malaria elimination are based on the principle of "High burden to high impact: A targeted malaria response". In other words, interventions should target localities or entire towns where the incidence of malaria is higher, until only individual episodes of malaria remain. [10]. To contribute to optimize the elimination/control program by targeting the high risk area, the aim of this study was therefore to estimate malaria prevalence at commune level, using survey data designed to be representative at regional level.
Materials and methods
Study setting
A landlocked country of 274,200 km2, Burkina Faso is located in the heart of West Africa. The country shares borders with Côte d’Ivoire, Ghana, Togo and Benin to the south, Mali to the north and Niger to the northwest. Its total population is estimated at 20 million (RGPH 2019). Burkina Faso has a dry, tropical climate of the Sudano-Sahelian type, characterized by highly variable rainfall ranging from 350 mm in the northern part of the country to over 1000 mm in its southwestern part [11]. There are two very distinct seasons. The first, the rainy season, lasts around 5 months (generally between mid-May and September), with a relatively shorter duration in the north of the country. The second season, the dry season, is the longest and is characterized by the Harmattan, a hot, dry, dust-laden wind from the Sahara desert. Based on rainfall and temperature, there are three main climatic bands in Burkina Faso [12]. Firstly, there's the Sahelian strip, which covers the north of the country, with its highly capricious rainfall of less than 600 mm per year and its extreme thermal oscillations (15 to 45 degrees). Then we have the Sudano-Sahelian band, a median zone for temperatures and rainfall that covers the central strip of the country. Finally, we have the Sudanian band covering the southern part of the country, the wettest with over 900 mm of rain per year and relatively low average temperatures. Rainfall thus decreases from the south-west to the north of the country.
This research complements these numerous studies to propose estimates of malaria infection at the scale of the three hundred and forty-two (342) communes covered by the census in 2019. The last administrative entity in the country, after the region and the province, the commune is a grouping of localities that are geographically close, often with cultural and economic ties. It is the only administrative entity managed by an elected official, the mayor. The management of communes is partly the responsibility of the local population, who contribute to their management through the payment of communal taxes. The commune is therefore the smallest geographical administrative entity from which a local development policy can be driven and coordinated by the community, under the watchful eye of the central administration. The choice of the commune is also justified by the fact that spatial disparities become more pronounced as the scale of analysis moves down to a finer level [13, 14]. This choice is also in line with one of the recommendations of the Sustainable Development Goals (SDGs), which call for the results of sustainable development actions to be assessed at finer geographical scales for greater effectiveness. [15, 16].
Sources of data
Three main data sources were used in this study: the general population and housing census (RGPH) carried out in 2019, the Malaria indicator survey carried out in 2018 and environmental data downloaded from the Climate Hazards Group InfraRed Precipitation with Station data (CHIRPS) website and the MOD11C3.006 module [17].
The RGPH is a complex operation carried out in 2019 that involved enumerating the Burkinabe population and its characteristics using a digitized questionnaire. It began on November 15, 2019 and officially ended on December 31, 2019. This nationwide operation was carried out against a backdrop of security crisis that led to partial coverage of the national territory. Of the country's 351 communes, 52 were only partially covered, and nine (9) were not covered at all. [18]. Estimates will therefore not include the nine (9) communes not covered by the census.
DHS program malaria indicator survey is a household survey based on a stratified 2-stage random sample selection. The primary sampling unit is the Enumeration Area (EA). Each area was subdivided into urban and rural parts to build the sampling strata, and the sample was drawn independently in each stratum. Overall, twenty-six strata were created. In the first stage, 252 EAs were drawn (52 in urban areas and 200 in rural areas)1 with probability proportional to size. In the second stratum, 26 households were systematically selected with equal probability from each of the EA drawn in the first stratum. In all, 6552 households were selected, including 1352 in urban areas and 5500 in rural areas. This survey, unlike the census, was conducted on paper and took place between November 2017 and March 2018. The Survey involved a representative sample of 6500 households and 7600 women aged 15–49. Blood samples were taken from 50% of selected households, for malaria screening. All children aged 6–59 months living in these households were eligible for malaria screening. Parental or guardian consent was required for their children's participation.
The Terra Moderate Resolution Imaging Spectroradiometer (MODIS) Land Surface Temperature/Emissivity Monthly (MOD11C3) Version 6.1 product provides monthly Land Surface Temperature and Emissivity (LST&E) values in a 0.05 degree (5600 m at the equator) latitude/longitude Climate Modeling Grid (CMG). A CMG granule is a geographic grid with 7200 columns and 3600 rows representing the entire globe. Climate Hazards Group In-fraRed Precipitation with Station data (CHIRPS) is a 35+ year quasi-global rainfall data set. Span-ning 50°S–50°N (and all longitudes) and ranging from 1981 to near-present, CHIRPS incorporates our in-house climatology, CHPclim, 0.05° resolution satellite imagery, and in-situ station data to create gridded rainfall time series for trend analysis and seasonal drought monitoring.
For the purposes of our analysis, precipitation and temperature were used. Monthly data for each geographical entity in 2019 were downloaded and then aggregated into annual values.
Study population
Target population study is children under five. The study population is represented by 5482 children from DHS program malaria survey in 2018 and 293,715 children from a random sample 10% Census (2019) database.
Variables of interest
Outcome variable
Response or the main outcome variable in this study was asymptomatic malaria infection (asymptomatic carriage) in children under 5 detected by rapid diagnostic test (RDT) during the survey. Malaria was diagnosed using serological biomarkers, SD Bioline Pan/Pf which is based on the detection of the HRP-2 antigen and specific pLDH for the five species of Plasmodium. The antibodies directed against Plasmodium antigens are sensitive biomarkers of malaria exposure to detect malaria in the community and to monitor variations over time or the impact of interventions, and to confirm malaria elimination. RDT requires 5 μL of blood drawn using a loop from the same finger prick taken for the hemoglobin test. The lancets included in the SD Bioline Pan/Pf kit have not been used and have been destroyed with other biohazardous waste.
Interpretation test is done after 15 min and the result and its interpretation have been communicated to the parents/adults responsible for the children who have taken the test.
Independent variables
The choice of variables is based on a review of the literature which highlighted factors associated with the prevalence of malaria in SSA. Commonly cited factors include:
Socio-demographic and residential factors: child's age, gender (male/female), household standard of living (very poor, poor, average, rich, very rich), mother's education, measured here as the proportion of educated women aged 15–49 in the region (for the survey) and in the commune (for the census), head of household's gender (male/female), head of household's age (15–34, 35–49, 50–64, 65 and over), religion of head of household (Muslim, Christian, Traditional), place of residence (Urban/Rural), region of residence (Boucle du Mouhoun, Cascades, Centre, Centre Est, Centre Nord, Centre Ouest, Centre Sud, Est, Hauts-Bassins, Nord, Plateau Central, Sahel, Sud-Ouest) and climatic factors such as temperature and rainfall [4, 7, 13, 14, 19].
Factors related to malaria control interventions: possession of LLINs (LLINs) (Yes/No), use of LLINs (Yes/No).
Environmental factors: cumulative monthly rainfall by commune and average monthly temperatures by commune for 2019.
Data processing and analysis
For the covariates retained in the two databases, the names and coding were harmonized before the two databases were assembled. Since differences in the distribution of the variables retained in the two databases could be a source of estimation bias, a consistency analysis was carried out (see Appendix A) to exclude variables with large distribution deviations. In addition, we ensured that the co-variables in the two data sources were comparable by examining the data collection methods and the definitions of the various concepts.
Ultimately, the variables retained at individual level are region and area of residence, age and sex of the head of household, age and sex of the child and household standard of living. At communal level, the proportion of educated women aged 15–49, annual rainfall and annual temperature were used in this secondary analysis. The distribution of these variables is shown in Appendix A.
Modeling approach
The estimation approach is that proposes by Elbers Langjouw and Langjouw (ELL),2 which consists of combining data from several sources in an econometric model. In this study, we assembled data from the census and the malaria survey [13]. The variable of interest (here RDT positivity) was present only for survey participants. We conducted a binary logistic regression and estimated the regression coefficients from the survey data, then predicted the value of the variable of interest using the census data. Confidence intervals are calculated using the Delta method.3 The procedure is described as follows.
A logistic regression model was used to predict the probability of child i testing positive for asymptomatic malaria infection using data from the malaria survey. The logistic regression model is expressed as follows:
| 1 |
where is the probability that a child i has asymptomatic malaria infection. are the predictors variables included in the model. The coefficients are the coefficients of each of the predictor variables included in the model. is the intercept.
The probability of a child under 5 years of age testing positive for asymptomatic malaria is defined as follows:
| 2 |
A stepwise regression was applied and Akaike's information criterion (AIC) [20] was used to select the best model to explain asymptomatic malaria infection in children under 5. Thus, the model with the lowest AIC was selected. We also used the ROC (Receiver Operating Characteristic) curve to assess model quality. This assessment is based on the predictive power of the model. The ROC curve is recognized as one of the best tools for evaluating the predictive power of a logistic model [21].
In addition to these econometric evaluations, we compared direct estimates of the prevalence of asymptomatic malaria infection from the survey with predicted estimates at regional level. Furthermore, to refine the t-model, we ensured that a replication of the estimates from the census co-variates offered relevant results. This check on the model's consistency and relevance is carried out at regional level, where the actual values from the officially published survey report are available [22].
For the model selected, coefficients are applied to the same covariates in the census data to predict the probabilities of a child under 5 testing positive for asymptomatic malaria infection. These individual probabilities are then aggregated to obtain estimates of the prevalence of asymptomatic malaria at communal, regional and national levels (Appendix D). After estimation at different geographical levels, an important challenge is to assess the uncertainty associated with the estimates. As these estimates are averages of predictions, confidence intervals can be estimated using the Delta [23, 24]. In this study, we used the STATA post estimation "margins" which produce both the average of the predictive margins [25] and calculate the associated standard errors by the Delta method.
Results
Analysis of the consistency of the results
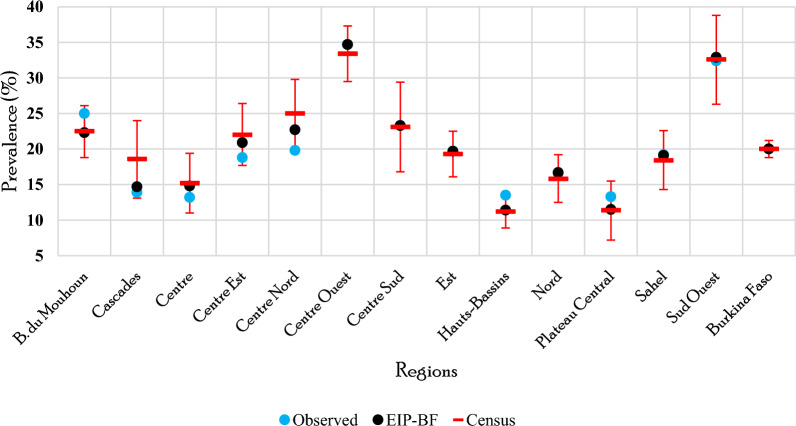
Evaluation of the final model gives the Area Under the ROC curve (AUC) of 69.0% (Fig. 1). This value shows that the model provides non-random estimates.
Fig. 1.
The ROC curve: overall assessment of model performance by plotting sensitivity against specificity 1
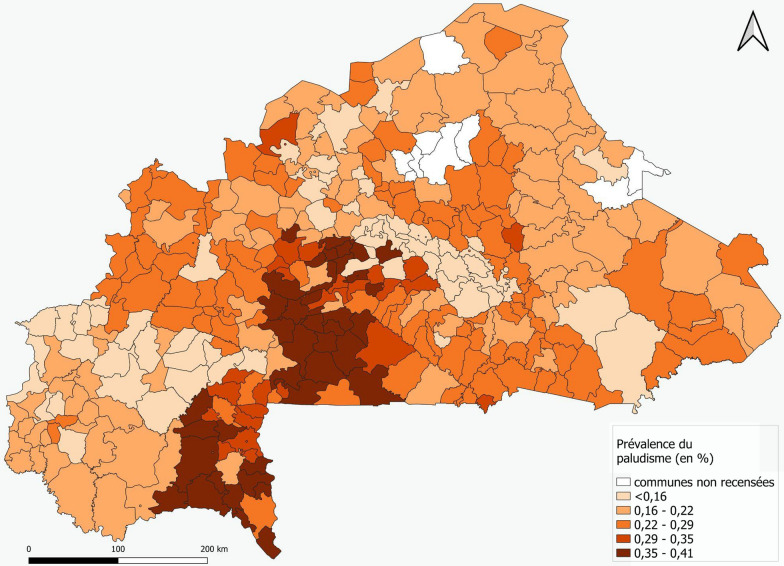
Estimation of the prevalence of asymptomatic malaria in children under 5 years of age at regional level, using data from the malaria survey, provides estimates that are more or less equal to those observed, i.e. those derived from the survey analysis report [22]. In fact, for all 13 administrative regions of Burkina Faso, the confidence intervals derived from estimates based on survey data contain the prevalence of asymptomatic malaria observed in each region (cf. Table 1 and Fig. 2).
Table 1.
Regional prediction of malaria prevalence and values observed in the survey report
| Region | Observed 2018 | Malaria survey 2018 | Census data 2019 |
|---|---|---|---|
| Boucle du Mouhoun | 25.0 | 22.3 (18.7, 26.0) | 22.5 (18.8, 26.1) |
| Cascades | 13.9 | 14.7 (10.3, 19.2) | 18.6 (13.1, 24.0) |
| Centre | 13.2 | 14.8 (10.8, 18.7) | 15.2 (11.0, 19.4) |
| Centre Est | 18.8 | 20.9 (16.8, 25.0) | 22.0 (17.7, 26.4) |
| Centre Nord | 19.8 | 22.7 (18.2, 27.1) | 25.0 (20.1, 29.8) |
| Centre Ouest | 34.7 | 34.7 (30.8, 38.6) | 33.4 (29.5, 37.3) |
| Centre Sud | 23.3 | 23.3 (17.1, 29.6) | 23.1 (16.8, 29.4) |
| Est | 19.7 | 19.7 (16.4, 22.9) | 19.3 (16.1, 22.5) |
| Hauts-Bassins | 13.5 | 11.4 (9.1, 13.6) | 11.2 (8.9, 13.5) |
| Nord | 16.6 | 16.7 (13.3, 20.1) | 15.8 (12.5, 19.2) |
| Plateau Central | 13.3 | 11.5 (7.3, 15.6) | 11.4 (7.2, 15.5) |
| Sahel | 19.2 | 19.1 (14.8, 23.3) | 18.4 (14.3, 22.6) |
| Sud-Ouest | 32.4 | 32.9 (26.7, 39.1) | 32.6 (26.3, 38.8) |
| Total (National average) | 20.02 | 20.02 (19.1, 21.3) | 20.03 (18.8, 21.2) |
Fig. 2.
Regional predictions of malaria prevalence from the two sources and values observed in the survey report
Verification of the consistency of estimates derived from census data also attests to better regional estimates. Indeed, cross-analysis of the confidence intervals of regional estimates from the two sources (Table 1) shows that estimates of asymptomatic malaria prevalence from census data are significantly the same as those observed and those derived from the survey.
Results description: exploring geographical heterogeneity
Figure 3 shows the spatial distribution of the prevalence of asymptomatic malaria in children under 5. It shows that the prevalence of asymptomatic malaria infection in children is similar across regions, whatever the data source considered. The regions with the highest prevalences were Centre-Ouest (33.4; 95% CI [29.5; 37.3]) and Sud-Ouest (32.6 with 95% CI [26.3; 38.8]), while Centre (15.2 with 95% CI [11.0; 19.4]), Hauts-Bassins (11.2 with 95% CI [8.9; 13.5]) and Plateau-central (11.4 with 95% CI [7.2; 15.5]) have the lowest levels of prevalence of asymptomatic malaria infection.
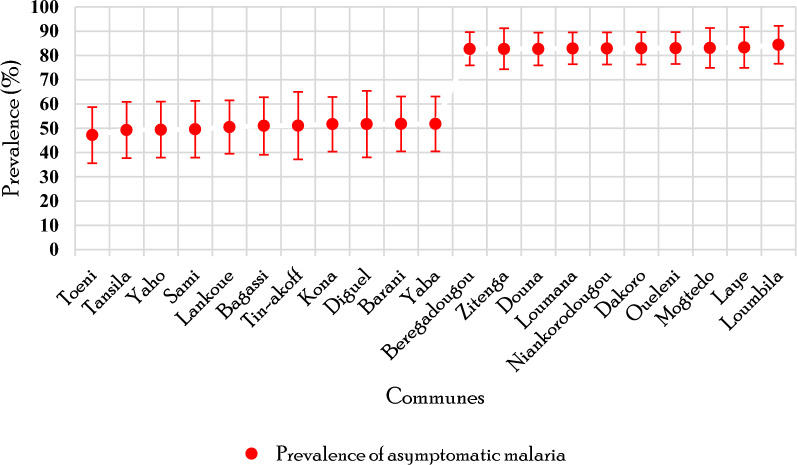
Fig. 3.
Mapping of prevalence predictions for asymptomatic malaria in children under 5 at the communal level.
Source of the data: Map created by Bassinga et al. (2024)
The consistency of estimates at regional level supports the idea that the model is suitable for predicting reliable estimates at communal level, as communal and regional results are the result of aggregating individual malaria infection probabilities.
Thus, analysis of estimates at commune level reveals heterogeneity in the prevalence of asymptomatic malaria in children between these entities (Fig. 3).
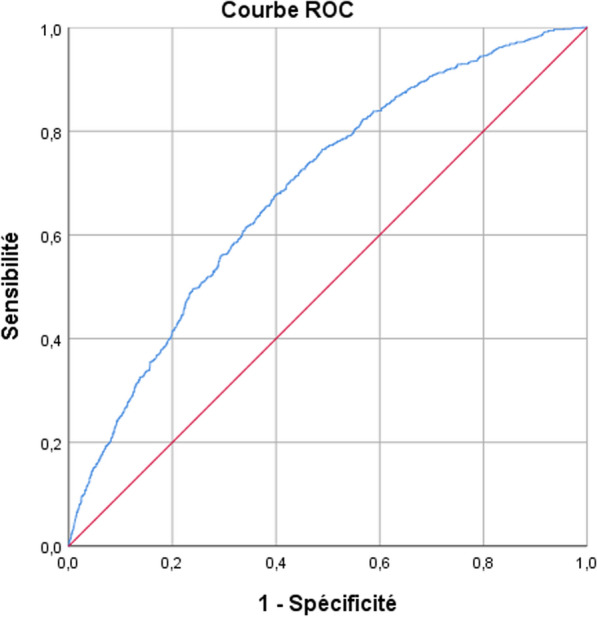
Of the 341 communes in which estimates were made, 208 had prevalences higher than the national average of 20.3% (95% CI [18.8; 21.2]). The ten communes (Fig. 4) with the highest prevalences were Djigoué (41.4% with 95% CI [33.5; 49.4]), Périgban (40.9% with 95% CI [33; 48.8]), Bougnounou (40.1% with 95% CI [35.5; 44.8]), Loropéni (39.9% with 95% CI [32.3; 47.5]), Siglé (39.7% with 95% CI [35.2; 44.2]), Kpuéré (39.7% with 95% CI [32.2; 47.2]), Zamo (39% with 95% CI [34.5; 43.4]), Nébiélianayou (38.7% with 95% CI [34.2; 43.1]), Silly (38.7% with 95% CI [34.3; 43.0]), and Zawara (38.6% with 95% CI [34.3; 42.9]). At the other end of the scale in terms of prevalence of asymptomatCI malaria, the communes of Bobo-Dioulasso (5.1% with 95% CI [3.6; 6.5]), Houndé (8.4% with 95% CI [6.4; 10.4]), Ziniaré (8.7% with 95% CI [5.4; 11.9]), Zorgho (8.9% with 95% CI [5.5; 12.3]), Oula, Ouagadougou, Boussé, Orodara, Djibo and Pouytenga are the ten communes where malaria prevalence is relatively low.
Fig. 4.
Malaria prevalence in the ten communes with the highest and ten with the lowest indicator values
When we look at heterogeneity within regions, we generally find that rural communes have the highest prevalence of asymptomatic malaria infection, compared to the urban communes. For instance, in the Centre region, the regional level prevalence of asymptomatic malaria is 15.3%, while this varies considerably between the urban commune of Ouagadougou (9,7%) and the region's rural communes of Komki-Ipala (36.1%), Komsilga (31.5%), Koubri (34.9%), Pabré (35.4%), Saaba (30.7%) and Tanghuin-Dassouri (34.6%), with an average malaria prevalence of 33%. The same is true for the Haut-Bassins region (11.2%), where the urban communes of Bobo-Dioulasso (5.1%), Houndé (8.2%) and Orodara (10.0%) have the lowest levels of malaria infection in children under five, compared with the other communes in the region, where prevalence varies from 14.0 to 19.0%. In the Centre-West and South-West regions, where levels of the indicator are the highest in the country, there are also strong communal disparities in malaria infection.
Discussion
Geographical identification of health problems is an important element of efforts control as it facilitates better allocation of the limited resources, improved health management and better targeting of interventions to maximize risk reduction [8, 23, 26, 27]. Analysis of the geographical distribution of the prevalence of asymptomatic malaria infection across the communes of Burkina Faso has highlighted sub-regional inequalities or heterogeneity that are often overlooked and difficult to highlight using survey data. The most perceptible communal differences are found between urban and rural communes within the same region, which is in itself a very useful result.
Geostatistical modeling of malaria risk among children in Burkina Faso using 2010 DHS data showed that low-risk areas were mainly concentrated in large urban centers such Ouagadougou the capital city [8]. This variation in malaria relative risk between localities in endemic regions is not surprising. It has always been recognized in other contexts [28, 29]. Differences between communes may be the result of heterogeneous ecological conditions that sustain larval breeding sites and thus facilitate the proliferation of mosquitoes, the vectors of malaria [30]. These vectors mainly determine the distribution and intensity of the disease [30]. In Kenya, for example, researchers noted that exposure to malaria could not be homogeneous, as malaria incidence did not follow a Poisson distribution, a phenomenon they described as over-dispersion [28]. Hence, the heterogeneity of malaria distribution at commune level could be explained mainly by socio-economic, health, hygiene and sanitation inequalities between communes, inequalities that are more prevalent between urban and rural communes [23]. These factors generally depend on the level of development of the various localities, since malaria and poverty are closely linked [30].
As Zhang et al. (2020) have already done in Nepal [16], we have succeeded in showing how the ELL small-area estimation model can be used to combine high-resolution census data with household survey data to produce more detailed and useful estimates. Compared with other small area estimation approaches (Bayesian models in particular), this one is relatively simple to implement and provides reasonably accurate results, provided certain precautions are taken to ensure data consistency and relevance. The steps required to implement the ELL method appear to be less complex, which represents a good opportunity to produce indicators at finer scales and adapt them to the needs of development policies, as recommended by the MDGs [18]. One of the prerequisites for this estimation approach is that the two operations (survey and census) are carried out at similar times, to avoid any major change in population and household structure. The data used in this analysis are collected at 1-year intervals, which is a major strength of this approach.
However, as is common knowledge, statistical estimates are sometimes subject to errors related to the estimation or sampling model. It is therefore important to assess the extent of these errors. In this study, the ROC curve reveals that the final model does not fully explain malaria prevalence, no doubt due to the failure to account for important and necessary variables. However, the robustness of the survey and census data helps to improve the accuracy of the estimates.
Another important fact to note, and one that remains a limitation of this study, is the failure to consider spatial autocorrelation. In fact, in the geographical analysis of a phenomenon measured in several places, it is generally observed that there is a relationship between the values of areas that are relatively close to each other [31]. As a result, other approaches to accounting for this spatial autocorrelation as a random effect in the analysis may be important. Such approaches may help to explain unmodeled variability more effectively, and would probably present a better picture of the spatial distribution of these data, albeit at the cost of reduced precision of the estimates [16].
Conclusions
The geographical inequalities in malaria prevalence highlighted among children under five suggest significant disparities between communes. Within the same region, this disparity is particularly marked between urban and rural communes. This highlights a pattern of dichotomy between urban and rural communities within the same region. Children in urban communes are relatively less exposed to malaria than those in rural communes. This situation seems to depend on the level of development of the targeted communes, especially since the factors associated with malaria prevalence easily demonstrate this.
This analysis shows that, while malaria control measures for children under 5 years of age need to be strengthened, regardless of their place of residence, rural communes need to be given greater attention in order to achieve greater gains in reducing malaria morbidity and mortality. Given the government's efforts to combat malaria, it's undeniable that we need to take account of the specific features of rural areas, where sanitation levels are sometimes poor.
Abbreviations
- AUC
Area under the curve
- CI
Confidence interval
- CMG
Climate modeling grid
- ELL
Elbers Langjouw and Langjouw
- INSD
National Institute of Statistics and Demography
- LST&E
Land surface temperature and emissivity
- ROC
Receiver operating characteristic
- SDGs
Sustainable development goals
- SSA
Sub-Saharan Africa
- WHO
World Health Organization
Appendix
Appendix A: frequency and mean distributions of variables
| Variables | Malaria survey 2018 | Census 2019 | ||
|---|---|---|---|---|
| Number | N % | Number | N % | |
| Region of residence | ||||
| Boucle du Mouhoun | 558 | 10.2 | 28,898 | 9.8 |
| Cascades | 255 | 4.6 | 13,344 | 4.5 |
| Centre | 313 | 5.7 | 36,483 | 12.4 |
| Centre Est | 441 | 8.0 | 24,757 | 8.4 |
| Centre Nord | 526 | 9.6 | 25,222 | 8.6 |
| Centre Ouest | 553 | 10.1 | 24,082 | 8.2 |
| Centre Sud | 167 | 3.1 | 10,807 | 3.7 |
| Est | 566 | 10.3 | 30,141 | 10.3 |
| Hauts-Bassins | 762 | 13.9 | 31,065 | 10.6 |
| Nord | 466 | 8.5 | 26,762 | 9.1 |
| Plateau Central | 255 | 4.6 | 14,931 | 5.1 |
| Sahel | 406 | 7.4 | 14,341 | 4.9 |
| Sud-Ouest | 214 | 3.9 | 12,882 | 4.4 |
| Place of residence | ||||
| Urban | 878 | 16.0 | 64,487 | 22.0 |
| Rural | 4604 | 84.0 | 229,228 | 78.0 |
| Child's gender | ||||
| Male | 2800 | 51.1 | 147,362 | 50.2 |
| Female | 2682 | 48.9 | 146,353 | 49.8 |
| Child's age | ||||
| 0 an | 605 | 11.0 | 51,963 | 17.7 |
| 1 an | 1098 | 20.0 | 53,276 | 18.1 |
| 2 ans | 1206 | 22.0 | 64,018 | 21.8 |
| 3 ans | 1326 | 24.2 | 62,399 | 21.2 |
| 4 ans | 1247 | 22.8 | 62,059 | 21.1 |
| Gender of head of household | ||||
| Male | 5175 | 94.4 | 264,041 | 89.9 |
| Female | 307 | 5.6 | 29,674 | 10.1 |
| Age of head of household | ||||
| 15–34 ans | 1652 | 30.1 | 110,538 | 37.6 |
| 35–49 ans | 2345 | 42.8 | 122,721 | 41.8 |
| 50–64 ans | 1079 | 19.7 | 45,204 | 15.4 |
| 65 ans ou+ | 406 | 7.4 | 15,252 | 5.2 |
| Wealth index | ||||
| Poorest | 1148 | 20.9 | 63,950 | 21.8 |
| Poorer | 1147 | 20.9 | 65,420 | 22.3 |
| Middle | 1129 | 20.6 | 64,658 | 22.0 |
| Richer | 1102 | 20.1 | 57,306 | 19.5 |
| Richest | 956 | 17.4 | 42,174 | 14.4 |
| Other variables | Malaria survey 2018 | Census 2019 |
|---|---|---|
| Mean | Mean | |
| Proportion of women aged 15–49 with education | 42.5 | 56.4 |
| Net usage rate | 55.2 | 89.4 |
| Annual rainfall | 928.8 | 907.6 |
| Annual temperatures | 35.9 | 35.9 |
Appendix B: ELL method
It consists in building an econometric model linking the malaria infection status of each child to a set of explanatory variables common to both the IBHS and the RGPH. The coefficients of the model's exogenous variables obtained from the survey data are fed into the census database to generate a prevalence of malaria infection per census child. Finally, the malaria prevalence is constructed for different geographical groups. The process thus comprises three stages.
First step: we begin by identifying a set of explanatory variables present in both databases that meet certain comparability criteria. We check that the wording of the questions and answers is the same in both questionnaires. From the selected questions, we then construct a series of variables whose comparability we test.
Second step: the per capita malaria prevalence model is estimated using the survey data. To maximize accuracy, the model is estimated at the lowest geographical level for which the survey remains representative. This level is usually the sampling strata. In this analysis, the geographical level considered is the region.
Third step: to complete the map, we associate the parameters estimated in the second step with the characteristics of each child in the census, to predict per capita prevalence. Individual prevalences are then aggregated at the regional and commune levels.
Appendix C: logistic regression result of the final model
| Predictor | Odds ratio (95% CI) |
|---|---|
| Regions | |
| Boucle du Mouhoun | 0.713 (0.474, 1.074) |
| Cascades | 0.461 (0.281, 0.756) |
| Centre | 1.324 (0.781, 2.244) |
| Centre Est | 0.747 (0.484, 1.152) |
| Centre Nord | 0.927 (0.572, 1.503) |
| Centre Ouest | 1.262 (0.873, 1.824) |
| Centre Sud | 0.673 (0.412, 1.099) |
| Est | 0.555 (0.363, 0.849) |
| Hauts-Bassins | 0.348 (0.236, 0.513) |
| Nord | 0.494 (0.322, 0.758) |
| Plateau Central | 0.336 (0.191, 0.592) |
| Sahel | 0.634 (0.369, 1.090) |
| Sud-Ouest | 1 |
| Place of residence | |
| Rural | 3.331 (2.289, 4.845) |
| Urban | 1 |
| Child's age | |
| 0 year | 1 |
| 1 year | 1.764 (1.259, 2.473) |
| 2 years | 2.282 (1.646, 3.164) |
| 3 years | 2.624 (1.904, 3.616) |
| 4 ans | 3.312 (2.404, 4.564) |
| Age of head of household | |
| 15–34 ans | 0.747 (0.625, 0.892) |
| 35–49 ans | 0.945 (0.765, 1.169) |
| 50–64 ans | 1.230 (0.929, 1.629) |
| 65 ans et+ | 1 |
| Wealth index | |
| Poorest | 1 |
| Poorer | 0.882 (0.708, 1.097) |
| Middle | 0.624 (0.494, 0.786) |
| Richer | 0.757 (0.601, 0.954) |
| Richest | 0.443 (0.311, 0.631) |
| Temperature | |
| Mean | 0.854 (0.766, 0.952) |
Appendix D: results from estimation at commune level using census and survey data
| Region | Province | Commune | Prevalence (95% CI) |
|---|---|---|---|
| Boucle du mouhoun | Bale | Bagassi | 25.1 (20.8, 29.4) |
| Boucle du mouhoun | Bale | Bana | 24.4 (20.2, 28.7) |
| Boucle du mouhoun | Bale | Boromo | 17.6 (14.0, 21.2) |
| Boucle du mouhoun | Bale | Fara | 20.7 (17.0, 24.4) |
| Boucle du mouhoun | Bale | Oury | 23.6 (19.6, 27.6) |
| Boucle du mouhoun | Bale | Pa | 25.8 (21.2, 30.3) |
| Boucle du mouhoun | Bale | Pompoi | 24.6 (20.4, 28.7) |
| Boucle du mouhoun | Bale | Poura | 19.6 (16.0, 23.2) |
| Boucle du mouhoun | Bale | Siby | 25.1 (20.6, 29.6) |
| Boucle du mouhoun | Bale | Yaho | 26.1 (21.7, 30.5) |
| Boucle du mouhoun | Banwa | Balave | 22.1 (18.4, 25.8) |
| Boucle du mouhoun | Banwa | Kouka | 24.7 (20.3, 29.1) |
| Boucle du mouhoun | Banwa | Sami | 26.5 (22.0, 30.9) |
| Boucle du mouhoun | Banwa | Sanaba | 24.0 (20.1, 28.0) |
| Boucle du mouhoun | Banwa | Solenzo | 23.1 (19.2, 27.0) |
| Boucle du mouhoun | Banwa | Tansila | 24.8 (20.7, 28.9) |
| Boucle du mouhoun | Kossi | Barani | 24.7 (20.5, 28.9) |
| Boucle du mouhoun | Kossi | Bomborokuy | 21.2 (16.8, 25.6) |
| Boucle du mouhoun | Kossi | Bourasso | 22.6 (18.6, 26.5) |
| Boucle du mouhoun | Kossi | Djibasso | 23.8 (19.8, 27.8) |
| Boucle du mouhoun | Kossi | Dokuy | 23.7 (19.7, 27.7) |
| Boucle du mouhoun | Kossi | Doumbala | 23.1 (19.1, 27.1) |
| Boucle du mouhoun | Kossi | Kombori | 22.9 (18.9, 26.9) |
| Boucle du mouhoun | Kossi | Madouba | 21.6 (17.9, 25.3) |
| Boucle du mouhoun | Kossi | Nouna | 17.2 (13.9, 20.6) |
| Boucle du mouhoun | Kossi | Sono | 25.0 (20.1, 30.0) |
| Boucle du mouhoun | Mouhoun | Bondokuy | 25.4 (21.1, 29.6) |
| Boucle du mouhoun | Mouhoun | Dedougou | 14.5 (11.7, 17.2) |
| Boucle du mouhoun | Mouhoun | Douroula | 22.3 (18.6, 26.1) |
| Boucle du mouhoun | Mouhoun | Kona | 23.5 (19.6, 27.4) |
| Boucle du mouhoun | Mouhoun | Ouarkoye | 24.6 (20.6, 28.7) |
| Boucle du mouhoun | Mouhoun | Safane | 23.0 (19.2, 26.8) |
| Boucle du mouhoun | Mouhoun | Tcheriba | 25.0 (20.9, 29.1) |
| Boucle du mouhoun | Nayala | Gassan | 19.7 (16.0, 23.5) |
| Boucle du mouhoun | Nayala | Gossina | 24.5 (20.5, 28.5) |
| Boucle du mouhoun | Nayala | Kougny | 20.7 (16.7, 24.6) |
| Boucle du mouhoun | Nayala | Toma | 18.0 (14.7, 21.3) |
| Boucle du mouhoun | Nayala | Yaba | 24.2 (20.1, 28.3) |
| Boucle du mouhoun | Nayala | Ye | 22.8 (19.0, 26.7) |
| Boucle du mouhoun | Sourou | Di | 24.2 (19.9, 28.4) |
| Boucle du mouhoun | Sourou | Gomboro | 23.2 (19.3, 27.1) |
| Boucle du mouhoun | Sourou | Kassoum | 21.5 (17.3, 25.6) |
| Boucle du mouhoun | Sourou | Kiembara | 24.4 (20.3, 28.4) |
| Boucle du mouhoun | Sourou | Lanfiera | 22.5 (18.7, 26.2) |
| Boucle du mouhoun | Sourou | Lankoue | 24.5 (20.4, 28.6) |
| Boucle du mouhoun | Sourou | Toeni | 25.0 (20.5, 29.5) |
| Boucle du mouhoun | Sourou | Tougan | 20.5 (16.9, 24.1) |
| Cascades | Comoe | Banfora | 10.3 (6.9, 13.6) |
| Cascades | Comoe | Beregadougou | 20.6 (14.3, 26.9) |
| Cascades | Comoe | Mangodara | 20.8 (14.7, 26.9) |
| Cascades | Comoe | Moussodougou | 22.9 (15.9, 29.9) |
| Cascades | Comoe | Niangoloko | 17.7 (12.4, 23.0) |
| Cascades | Comoe | Ouo | 21.3 (15.1, 27.6) |
| Cascades | Comoe | Sideradougou | 20.5 (14.5, 26.5) |
| Cascades | Comoe | Soubakaniedougou | 19.6 (13.7, 25.4) |
| Cascades | Comoe | Tiefora | 20.8 (14.7, 27.0) |
| Cascades | Leraba | Dakoro | 19.7 (13.8, 25.6) |
| Cascades | Leraba | Douna | 20.9 (14.6, 27.1) |
| Cascades | Leraba | Kankalaba | 20.7 (14.6, 26.9) |
| Cascades | Leraba | Loumana | 19.8 (13.9, 25.6) |
| Cascades | Leraba | Niankorodougou | 18.7 (13.0, 24.4) |
| Cascades | Leraba | Oueleni | 21.7 (15.3, 28.2) |
| Cascades | Leraba | Sindou | 17.1 (12.0, 22.2) |
| Cascades | Leraba | Wolonkoto | 22.8 (16.0, 29.6) |
| Centre | Kadiogo | Komki-Ipala | 36.1 (27.0, 45.3) |
| Centre | Kadiogo | Komsilga | 31.5 (23.0, 40.0) |
| Centre | Kadiogo | Koubri | 34.9 (26.1, 43.8) |
| Centre | Kadiogo | Ouagadougou | 9.7 (6.3, 13.1) |
| Centre | Kadiogo | Pabre | 35.4 (26.5, 44.4) |
| Centre | Kadiogo | Saaba | 30.7 (22.3, 39.1) |
| Centre | Kadiogo | Tanghin Dassouri | 34.6 (25.7, 43.5) |
| Centre est | Boulgou | Bagre | 28.2 (22.5, 33.9) |
| Centre est | Boulgou | Bane | 28.4 (22.6, 34.1) |
| Centre est | Boulgou | Beguedo | 23.3 (18.3, 28.2) |
| Centre est | Boulgou | Bissiga | 26.2 (21.1, 31.3) |
| Centre est | Boulgou | Bittou | 22.5 (18.0, 27.0) |
| Centre est | Boulgou | Boussouma | 27.0 (21.2, 32.8) |
| Centre est | Boulgou | Boussouma | 26.2 (21.1, 31.3) |
| Centre est | Boulgou | Garango | 17.5 (13.7, 21.2) |
| Centre est | Boulgou | Komtoega | 22.4 (17.8, 27.1) |
| Centre est | Boulgou | Niaogho | 26.9 (21.5, 32.4) |
| Centre est | Boulgou | Tenkodogo | 18.0 (14.3, 21.6) |
| Centre est | Boulgou | Zabre | 24.7 (19.8, 29.6) |
| Centre est | Boulgou | Zoaga | 29.6 (23.8, 35.4) |
| Centre est | Boulgou | Zonse | 23.1 (18.4, 27.8) |
| Centre est | Koulpelogo | Comin-Yanga | 23.5 (18.7, 28.4) |
| Centre est | Koulpelogo | Dourtenga | 23.5 (18.7, 28.2) |
| Centre est | Koulpelogo | Lalgaye | 27.5 (21.9, 33.1) |
| Centre est | Koulpelogo | Ouargaye | 21.2 (17.0, 25.4) |
| Centre est | Koulpelogo | Sanga | 26.7 (21.5, 31.9) |
| Centre est | Koulpelogo | Soudougui | 26.5 (21.4, 31.6) |
| Centre est | Koulpelogo | Yargatenga | 24.0 (19.2, 28.8) |
| Centre est | Koulpelogo | Yonde | 24.6 (19.8, 29.4) |
| Centre est | Kouritenga | Andemtenga | 24.2 (19.4, 29.0) |
| Centre est | Kouritenga | Baskoure | 25.4 (20.3, 30.4) |
| Centre est | Kouritenga | Dialgaye | 23.1 (18.4, 27.8) |
| Centre est | Kouritenga | Gounghin | 24.4 (19.6, 29.3) |
| Centre est | Kouritenga | Kando | 24.2 (19.4, 29.0) |
| Centre est | Kouritenga | Koupela | 15.2 (11.8, 18.5) |
| Centre est | Kouritenga | Pouytenga | 10.3 (7.4, 13.2) |
| Centre est | Kouritenga | Tensobentenga | 23.6 (18.9, 28.3) |
| Centre est | Kouritenga | Yargo | 23.9 (19.1, 28.7) |
| Centre nord | Bam | Bourzanga | 27.3 (22.0, 32.7) |
| Centre nord | Bam | Guibare | 26.8 (21.5, 32.1) |
| Centre nord | Bam | Kongoussi | 20.8 (16.4, 25.2) |
| Centre nord | Bam | Rollo | 27.1 (21.8, 32.5) |
| Centre nord | Bam | Rouko | 27.9 (22.5, 33.3) |
| Centre nord | Bam | Sabce | 28.2 (22.5, 33.9) |
| Centre nord | Bam | Tikare | 26.1 (21.1, 31.2) |
| Centre nord | Namentenga | Boala | 27.1 (21.7, 32.4) |
| Centre nord | Namentenga | Boulsa | 25.5 (20.5, 30.5) |
| Centre nord | Namentenga | Bouroum | 26.2 (20.9, 31.6) |
| Centre nord | Namentenga | Dargo | 29.4 (23.6, 35.2) |
| Centre nord | Namentenga | Nagbingou | 26.2 (20.9, 31.5) |
| Centre nord | Namentenga | Tougouri | 25.3 (19.9, 30.7) |
| Centre nord | Namentenga | Yalgo | 24.7 (19.7, 29.7) |
| Centre nord | Namentenga | Zeguedeguin | 26.6 (21.2, 32.1) |
| Centre nord | Sanmatenga | Kaya | 16.5 (12.9, 20.1) |
| Centre nord | Sanmatenga | Korsimoro | 23.7 (18.8, 28.6) |
| Centre nord | Sanmatenga | Mane | 27.3 (22.0, 32.6) |
| Centre nord | Sanmatenga | Pibaore | 28.5 (23.0, 33.9) |
| Centre nord | Sanmatenga | Pissila | 27.4 (22.0, 32.7) |
| Centre nord | Sanmatenga | Ziga | 27.5 (22.3, 32.8) |
| Centre ouest | Boulkiemde | Bingo | 35.7 (31.4, 40.0) |
| Centre ouest | Boulkiemde | Imasgho | 36.5 (32.2, 40.9) |
| Centre ouest | Boulkiemde | Kindi | 37.5 (33.0, 42.0) |
| Centre ouest | Boulkiemde | Kokoloko | 34.7 (30.7, 38.8) |
| Centre ouest | Boulkiemde | Koudougou | 18.6 (15.3, 21.8) |
| Centre ouest | Boulkiemde | Nandiala | 35.1 (30.6, 39.6) |
| Centre ouest | Boulkiemde | Nanoro | 35.7 (31.4, 40.0) |
| Centre ouest | Boulkiemde | Pella | 35.7 (31.4, 40.1) |
| Centre ouest | Boulkiemde | Poa | 33.1 (28.9, 37.3) |
| Centre ouest | Boulkiemde | Ramongo | 38.3 (34.0, 42.6) |
| Centre ouest | Boulkiemde | Sabou | 33.8 (29.4, 38.2) |
| Centre ouest | Boulkiemde | Sigle | 39.7 (35.2, 44.2) |
| Centre ouest | Boulkiemde | Soaw | 36.5 (32.0, 41.0) |
| Centre ouest | Boulkiemde | Sourgou | 35.6 (31.5, 39.7) |
| Centre ouest | Boulkiemde | Thyou | 33.8 (29.6, 37.9) |
| Centre ouest | Sanguie | Dassa | 33.7 (29.4, 37.9) |
| Centre ouest | Sanguie | Didyr | 34.3 (29.6, 39.0) |
| Centre ouest | Sanguie | Godyr | 35.4 (30.6, 40.2) |
| Centre ouest | Sanguie | Kordie | 34.8 (29.9, 39.7) |
| Centre ouest | Sanguie | Kyon | 34.9 (30.0, 39.7) |
| Centre ouest | Sanguie | Pouni | 35.4 (30.8, 40.0) |
| Centre ouest | Sanguie | Reo | 24.7 (20.8, 28.5) |
| Centre ouest | Sanguie | Tenado | 37.1 (32.7, 41.5) |
| Centre ouest | Sanguie | Zamo | 39.0 (34.5, 43.4) |
| Centre ouest | Sanguie | Zawara | 38.6 (34.3, 42.9) |
| Centre ouest | Sissili | Bieha | 37.4 (33.1, 41.7) |
| Centre ouest | Sissili | Boura | 38.0 (33.7, 42.2) |
| Centre ouest | Sissili | Leo | 22.2 (18.7, 25.7) |
| Centre ouest | Sissili | Nebielianayou | 38.7 (34.2, 43.1) |
| Centre ouest | Sissili | Niabouri | 37.4 (33.1, 41.7) |
| Centre ouest | Sissili | Silly | 38.7 (34.3, 43.0) |
| Centre ouest | Sissili | To | 36.5 (32.3, 40.6) |
| Centre ouest | Ziro | Bakata | 38.5 (34.0, 42.9) |
| Centre ouest | Ziro | Bougnounou | 40.1 (35.5, 44.8) |
| Centre ouest | Ziro | Cassou | 38.4 (34.1, 42.8) |
| Centre ouest | Ziro | Dalo | 38.2 (33.7, 42.7) |
| Centre ouest | Ziro | Gao | 36.8 (32.6, 41.0) |
| Centre ouest | Ziro | Sapouy | 33.5 (29.4, 37.5) |
| Centre sud | Bazega | Doulougou | 24.7 (18.0, 31.5) |
| Centre sud | Bazega | Gaongo | 21.5 (15.1, 27.9) |
| Centre sud | Bazega | Ipelce | 23.5 (16.9, 30.0) |
| Centre sud | Bazega | Kayao | 25.5 (18.7, 32.4) |
| Centre sud | Bazega | Kombissiri | 17.3 (12.3, 22.3) |
| Centre sud | Bazega | Sapone | 23.6 (17.1, 30.0) |
| Centre sud | Bazega | Toece | 24.1 (17.5, 30.6) |
| Centre sud | Nahouri | Guiaro | 26.3 (19.2, 33.3) |
| Centre sud | Nahouri | Pô | 19.4 (13.9, 25.0) |
| Centre sud | Nahouri | Tiebele | 25.7 (18.9, 32.5) |
| Centre sud | Nahouri | Zecco | 23.0 (16.6, 29.4) |
| Centre sud | Nahouri | Ziou | 25.5 (18.7, 32.4) |
| Centre sud | Zoundweogo | Bere | 22.8 (16.4, 29.1) |
| Centre sud | Zoundweogo | Binde | 21.4 (15.1, 27.6) |
| Centre sud | Zoundweogo | Gogo | 26.9 (19.7, 34.1) |
| Centre sud | Zoundweogo | Gomboussougou | 27.6 (19.7, 35.6) |
| Centre sud | Zoundweogo | Guiba | 24.0 (17.4, 30.6) |
| Centre sud | Zoundweogo | Manga | 11.6 (7.8, 15.3) |
| Centre sud | Zoundweogo | Nobere | 24.4 (17.7, 31.1) |
| Est | Gnagna | Bilanga | 19.6 (16.2, 23.0) |
| Est | Gnagna | Bogande | 17.3 (14.1, 20.4) |
| Est | Gnagna | Coalla | 16.1 (12.8, 19.3) |
| Est | Gnagna | Liptougou | 18.4 (15.0, 21.9) |
| Est | Gnagna | Mani | 16.9 (13.4, 20.3) |
| Est | Gnagna | Piela | 19.3 (16.0, 22.5) |
| Est | Gnagna | Thion | 18.0 (14.3, 21.7) |
| Est | Gourma | Diabo | 19.2 (15.8, 22.6) |
| Est | Gourma | Diapangou | 20.6 (17.0, 24.2) |
| Est | Gourma | Fada N'Gourma | 13.6 (11.2, 16.0) |
| Est | Gourma | Matiacoali | 22.6 (18.7, 26.5) |
| Est | Gourma | Tibga | 19.4 (16.2, 22.7) |
| Est | Gourma | Yamba | 19.6 (16.3, 22.9) |
| Est | Komandjoari | Bartibougou | 20.5 (17.0, 24.1) |
| Est | Komandjoari | Foutouri | 19.7 (16.4, 23.0) |
| Est | Komandjoari | Gayeri | 17.6 (14.4, 20.8) |
| Est | Kompienga | Kompienga | 25.1 (19.4, 30.9) |
| Est | Kompienga | Madjoari | 26.7 (21.3, 32.1) |
| Est | Kompienga | Pama | 15.2 (12.6, 17.9) |
| Est | Tapoa | Botou | 22.8 (18.8, 26.8) |
| Est | Tapoa | Diapaga | 19.0 (15.8, 22.3) |
| Est | Tapoa | Kantchari | 22.1 (18.3, 25.8) |
| Est | Tapoa | Logobou | 24.0 (19.6, 28.4) |
| Est | Tapoa | Namounou | 20.4 (17.0, 23.8) |
| Est | Tapoa | Partiaga | 22.8 (18.9, 26.7) |
| Est | Tapoa | Tambaga | 23.9 (19.5, 28.4) |
| Est | Tapoa | Tansarga | 21.6 (18.0, 25.1) |
| Hauts-bassins | Houet | Bama | 16.0 (12.8, 19.2) |
| Hauts-bassins | Houet | Bobo-Dioulasso | 5.1 (3.6, 6.5) |
| Hauts-bassins | Houet | Dande | 16.8 (13.4, 20.2) |
| Hauts-bassins | Houet | Faramana | 15.8 (12.4, 19.2) |
| Hauts-bassins | Houet | Fo | 15.2 (12.1, 18.4) |
| Hauts-bassins | Houet | Karankasso Sambla | 16.9 (13.2, 20.5) |
| Hauts-bassins | Houet | Karankasso-Vigue | 15.0 (11.9, 18.1) |
| Hauts-bassins | Houet | Koundougou | 16.3 (12.9, 19.6) |
| Hauts-bassins | Houet | Lena | 17.6 (14.1, 21.2) |
| Hauts-bassins | Houet | Padema | 14.6 (11.5, 17.7) |
| Hauts-bassins | Houet | Peni | 16.8 (13.4, 20.3) |
| Hauts-bassins | Houet | Satiri | 16.4 (13.1, 19.7) |
| Hauts-bassins | Houet | Toussiana | 17.6 (13.5, 21.7) |
| Hauts-bassins | Kenedougou | Banzon | 16.9 (13.1, 20.8) |
| Hauts-bassins | Kenedougou | Djigouera | 17.4 (13.5, 21.3) |
| Hauts-bassins | Kenedougou | Kangala | 19.0 (14.1, 23.9) |
| Hauts-bassins | Kenedougou | Kayan | 15.0 (11.9, 18.2) |
| Hauts-bassins | Kenedougou | Koloko | 16.2 (12.6, 19.9) |
| Hauts-bassins | Kenedougou | Kourignon | 18.7 (14.0, 23.3) |
| Hauts-bassins | Kenedougou | Kourouma | 15.5 (12.4, 18.7) |
| Hauts-bassins | Kenedougou | Morolaba | 14.2 (11.0, 17.3) |
| Hauts-bassins | Kenedougou | N'Dorola | 14.6 (11.5, 17.7) |
| Hauts-bassins | Kenedougou | Orodara | 10.0 (7.0, 13.1) |
| Hauts-bassins | Kenedougou | Samogohiri | 19.0 (14.2, 23.8) |
| Hauts-bassins | Kenedougou | Samorogouan | 14.7 (11.7, 17.8) |
| Hauts-bassins | Kenedougou | Sindo | 14.0 (10.9, 17.1) |
| Hauts-bassins | Tuy | Bekuy | 16.3 (13.0, 19.7) |
| Hauts-bassins | Tuy | Bereba | 16.0 (12.7, 19.2) |
| Hauts-bassins | Tuy | Bony | 14.7 (11.1, 18.3) |
| Hauts-bassins | Tuy | Founzan | 14.3 (10.9, 17.6) |
| Hauts-bassins | Tuy | Hounde | 8.4 (6.4, 10.4) |
| Hauts-bassins | Tuy | Koti | 14.4 (11.0, 17.8) |
| Hauts-bassins | Tuy | Koumbia | 15.1 (12.0, 18.2) |
| Nord | Loroum | Banh | 18.7 (14.7, 22.7) |
| Nord | Loroum | Ouindigui | 17.9 (14.1, 21.7) |
| Nord | Loroum | Solle | 19.5 (15.3, 23.6) |
| Nord | Loroum | Titao | 12.2 (9.4, 15.0) |
| Nord | Passore | Arbole | 17.9 (14.2, 21.6) |
| Nord | Passore | Bagare | 19.5 (15.5, 23.5) |
| Nord | Passore | Bokin | 17.9 (14.2, 21.6) |
| Nord | Passore | Gomponsom | 23.4 (17.6, 29.3) |
| Nord | Passore | Kirsi | 16.0 (12.4, 19.6) |
| Nord | Passore | La-Todin | 17.4 (13.7, 21.0) |
| Nord | Passore | Pilimpikou | 17.8 (14.0, 21.5) |
| Nord | Passore | Samba | 18.2 (14.4, 22.0) |
| Nord | Passore | Yako | 14.5 (11.5, 17.6) |
| Nord | Yatenga | Barga | 15.2 (11.5, 18.9) |
| Nord | Yatenga | Kain | 18.3 (14.2, 22.4) |
| Nord | Yatenga | Kalsaka | 18.0 (14.3, 21.7) |
| Nord | Yatenga | Kossouka | 15.6 (12.1, 19.2) |
| Nord | Yatenga | Koumbri | 16.4 (12.7, 20.1) |
| Nord | Yatenga | Ouahigouya | 16.3 (12.7, 19.8) |
| Nord | Yatenga | Oula | 9.7 (7.5, 11.9) |
| Nord | Yatenga | Rambo | 15.8 (12.2, 19.4) |
| Nord | Yatenga | Seguenega | 17.0 (13.5, 20.6) |
| Nord | Yatenga | Tangaye | 16.0 (12.5, 19.5) |
| Nord | Yatenga | Thiou | 16.9 (13.2, 20.7) |
| Nord | Yatenga | Zogore | 18.7 (14.8, 22.5) |
| Nord | Zondoma | Bassi | 15.7 (12.2, 19.3) |
| Nord | Zondoma | Boussou | 19.8 (15.8, 23.8) |
| Nord | Zondoma | Gourcy | 14.0 (11.0, 17.0) |
| Nord | Zondoma | Leba | 17.4 (13.8, 21.0) |
| Nord | Zondoma | Tougo | 17.7 (14.1, 21.4) |
| Plateau central | Ganzourgou | Boudry | 11.5 (7.2, 15.7) |
| Plateau central | Ganzourgou | Kogho | 14.1 (9.0, 19.3) |
| Plateau central | Ganzourgou | Meguet | 11.4 (7.2, 15.6) |
| Plateau central | Ganzourgou | Mogtedo | 10.4 (6.4, 14.3) |
| Plateau central | Ganzourgou | Salogo | 13.1 (8.3, 17.9) |
| Plateau central | Ganzourgou | Zam | 10.6 (6.5, 14.7) |
| Plateau central | Ganzourgou | Zorgho | 8.9 (5.5, 12.3) |
| Plateau central | Ganzourgou | Zoungou | 11.2 (7.0, 15.4) |
| Plateau central | Kourweogo | Bousse | 10.0 (6.2, 13.8) |
| Plateau central | Kourweogo | Laye | 13.8 (8.6, 19.1) |
| Plateau central | Kourweogo | Niou | 13.0 (8.2, 17.7) |
| Plateau central | Kourweogo | Sourgoubila | 14.9 (9.4, 20.4) |
| Plateau central | Kourweogo | Toeghin | 12.9 (8.2, 17.6) |
| Plateau central | Oubritenga | Absouya | 11.9 (7.5, 16.2) |
| Plateau central | Oubritenga | Dapelogo | 13.0 (8.3, 17.8) |
| Plateau central | Oubritenga | Loumbila | 12.4 (7.7, 17.1) |
| Plateau central | Oubritenga | Nagreongo | 12.5 (7.9, 17.0) |
| Plateau central | Oubritenga | Ourgou-Manega | 13.0 (8.3, 17.8) |
| Plateau central | Oubritenga | Ziniare | 8.7 (5.4, 11.9) |
| Plateau central | Oubritenga | Zitenga | 11.2 (6.9, 15.4) |
| Sahel | Oudalan | Deou | 19.6 (15.1, 24.0) |
| Sahel | Oudalan | Gorom-Gorom | 17.7 (13.6, 21.8) |
| Sahel | Oudalan | Markoye | 17.7 (13.2, 22.1) |
| Sahel | Oudalan | Oursi | 20.3 (15.7, 24.9) |
| Sahel | Oudalan | Tin-Akoff | 19.4 (14.8, 23.9) |
| Sahel | Seno | Bani | 19.7 (15.2, 24.1) |
| Sahel | Seno | Dori | 17.6 (13.7, 21.6) |
| Sahel | Seno | Falagountou | 18.9 (14.5, 23.3) |
| Sahel | Seno | Gorgadji | 20.8 (16.1, 25.4) |
| Sahel | Seno | Sampelga | 20.8 (16.2, 25.5) |
| Sahel | Seno | Seytenga | 20.5 (15.9, 25.0) |
| Sahel | Soum | Arbinda | 20.0 (15.5, 24.5) |
| Sahel | Soum | Baraboule | 22.6 (17.5, 27.6) |
| Sahel | Soum | Diguel | 23.4 (18.1, 28.7) |
| Sahel | Soum | Djibo | 10.2 (7.3, 13.1) |
| Sahel | Soum | Kelbo | 19.6 (14.9, 24.3) |
| Sahel | Soum | Nassoumbou | 22.0 (17.1, 26.9) |
| Sahel | Soum | Pobe-Mengao | 20.8 (15.6, 25.9) |
| Sahel | Soum | Tongomayel | 21.8 (16.9, 26.7) |
| Sahel | Yagha | Sebba | 15.6 (12.0, 19.2) |
| Sahel | Yagha | Solhan | 20.6 (15.9, 25.2) |
| Sahel | Yagha | Tankougounadie | 19.9 (15.4, 24.4) |
| Sahel | Yagha | Titabe | 21.4 (16.7, 26.2) |
| Sud ouest | Bougouriba | Bondigui | 35.5 (28.8, 42.3) |
| Sud ouest | Bougouriba | Diebougou | 24.2 (18.9, 29.4) |
| Sud ouest | Bougouriba | Dolo | 34.7 (28.0, 41.4) |
| Sud ouest | Bougouriba | Iolonioro | 37.2 (30.2, 44.2) |
| Sud ouest | Bougouriba | Tiankoura | 38.0 (31.0, 44.9) |
| Sud ouest | Ioba | Dano | 23.7 (18.0, 29.4) |
| Sud ouest | Ioba | Dissin | 30.7 (23.8, 37.5) |
| Sud ouest | Ioba | Gueguere | 31.9 (25.1, 38.6) |
| Sud ouest | Ioba | Koper | 32.0 (24.5, 39.4) |
| Sud ouest | Ioba | Niego | 31.3 (23.6, 39.1) |
| Sud ouest | Ioba | Oronkua | 32.1 (25.1, 39.1) |
| Sud ouest | Ioba | Ouessa | 27.6 (20.2, 35.0) |
| Sud ouest | Ioba | Zambo | 32.3 (25.3, 39.2) |
| Sud ouest | Noumbiel | Batie | 27.7 (22.1, 33.4) |
| Sud ouest | Noumbiel | Boussoukoula | 37.7 (30.7, 44.7) |
| Sud ouest | Noumbiel | Kpuere | 39.7 (32.2, 47.2) |
| Sud ouest | Noumbiel | Legmoin | 37.4 (30.5, 44.3) |
| Sud ouest | Noumbiel | Midebdo | 38.0 (30.9, 45.2) |
| Sud ouest | Poni | Bouroum-Bouroum | 34.8 (28.2, 41.5) |
| Sud ouest | Poni | Boussera | 35.3 (28.0, 42.6) |
| Sud ouest | Poni | Djigoue | 41.4 (33.5, 49.4) |
| Sud ouest | Poni | Gaoua | 21.7 (16.9, 26.6) |
| Sud ouest | Poni | Gbomblora | 36.7 (29.9, 43.5) |
| Sud ouest | Poni | Kampti | 38.5 (31.1, 46.0) |
| Sud ouest | Poni | Loropeni | 39.9 (32.3, 47.5) |
| Sud ouest | Poni | Malba | 34.7 (27.6, 41.7) |
| Sud ouest | Poni | Nako | 34.6 (27.7, 41.4) |
| Sud ouest | Poni | Perigban | 40.9 (33.0, 48.8) |
Author contributions
Conceptualization: BH, MO, RT; methodology: BH, MO.; validation: MK, OM, formal analysis: BH, MO; data curation: BH, MOYP, OC, NA; writing—original draft: BH; writing—review and editing: BH, OM, OC, CK, RT; funding acquisition: this research received no external funding; project administration: BH.; supervision: MK. All authors read and approved the final manuscript.
Funding
This research received no external funding.
Availability of data and materials
Malaria Indicators Survey dataset is available on the dhs program (https://dhsprogram.com) website and the General Population and Housing Census dataset is available at the National Institute of Statistics and Demography (INSD) in Burkina Faso.
Declarations
Ethics approval
Permission to access the data was obtained from the measure DHS program (http://www.dhsprogram.com) via online request. The website and the data used were publicly available with no personal identifier. All methods were carried out in accordance with relevant guidelines and regulations.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Competing interests
The authors declare that they have no competing interests. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Disclaimer/Publisher’s Note
The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of Population Health Metrics and/or the editor(s). Population Health Metrics and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
Footnotes
ZDs were allocated to strata in proportion to the number of ZDs in each stratum.
See Appendix A2 for more details.
In probability and statistics, the delta method is a method for approximating the asymptotic distribution of the transform of an asymptotically normal random variable.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ouédraogo M, et al. Spatial distribution and determinants of asymptomatic malaria risk among children under 5 years in 24 districts in Burkina Faso. Malar J. 2018;17(1):460. 10.1186/s12936-018-2606-9. 10.1186/s12936-018-2606-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. World malaria report 2023, 2023.
- 3.World Health Organisation. World malaria report 2021, 2021.
- 4.Ouedraogo M, Kangoye D, Samadoulougou S, Rouamba T, Donnen P, Kirakoya-Samadoulougou F. Malaria case fatality rate among children under five in Burkina Faso: an assessment of the spatiotemporal trends following the implementation of control programs. Int J Environ Res Public Health. 2020;17:1840. 10.3390/ijerph17061840. 10.3390/ijerph17061840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rouamba T, Samadoulougou S, Tinto H, Alegana VA, Kirakoya-Samadoulougou F. Severe-malaria infection and its outcomes among pregnant women in Burkina Faso health-districts: hierarchical Bayesian space-time models applied to routinely-collected data from 2013 to 2018. Spat Spatio-Temporal Epidemiol. 2020;33:100333. 10.1016/j.sste.2020.100333. 10.1016/j.sste.2020.100333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rouamba T, Samadoulougou S, Tinto H, Alegana VA, Kirakoya-Samadoulougou F. Bayesian spatiotemporal modeling of routinely collected data to assess the effect of health programs in malaria incidence during pregnancy in Burkina Faso. Sci Rep. 2020;10(1):2618. 10.1038/s41598-020-58899-3. 10.1038/s41598-020-58899-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samadoulougou S, Maheu-Giroux M, Kirakoya-Samadoulougou F, De Keukeleire M, Castro MC, Robert A. Multilevel and geo-statistical modeling of malaria risk in children of Burkina Faso. Parasit Vectors. 2014;7:350. 10.1186/1756-3305-7-350. 10.1186/1756-3305-7-350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Negatou M, Ouedraogo M, Donnen P, Paul E, Samadoulougou S, Kirakoya-Samadoulougou F. Care-seeking for fever for children under the age of five before and after the free healthcare initiative in Burkina Faso: evidence from three population-based surveys. Risk Manag Healthc Policy. 2021;14:2065–77. 10.2147/rmhp.s297983. 10.2147/rmhp.s297983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bationo CS, et al. Spatio-temporal analysis and prediction of malaria cases using remote sensing meteorological data in Diébougou health district, Burkina Faso, 2016–2017. Sci Rep. 2021;11(1):1. 10.1038/s41598-021-99457-9. 10.1038/s41598-021-99457-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Organisation mondiale de la santé. Malaria elimination: a field manual for low and moderate endémique countries. OMS, Genève, Suisse, 2007.
- 11.INSD et Macro International Inc. Enquête démographique et de santé 2010. Institut National de la Statistique et de la Demographie, Burkina Faso, 2012.
- 12.Kaboré B, Kam S, Ouedraogo G, Bathiebo D. Etude de l’evolution climatique au Burkina Faso de 1983 a 2012 : cas des villes de Bobo Dioulasso, Ouagadougou et dori, 2017.
- 13.Elbers C, Lanjouw JO, Lanjouw P. Micro-level estimation of poverty and inequality. Econometrica. 2003;71(1):355–64. 10.1111/1468-0262.00399 [DOI] [Google Scholar]
- 14.Diboulo E, Sié A, Vounatsou P. Assessing the effects of malaria interventions on the geographical distribution of parasitaemia risk in Burkina Faso. Malar J. 2016;15(1):228. 10.1186/s12936-016-1282-x. 10.1186/s12936-016-1282-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bassinga H, Soura A. inégalités géographiques de mortalité infanto-juvénile au Burkina Faso : une analyse des recensements de 1996 et de 2006. In: promouvoir et confronter les sources statistiques existantes pour répondre aux enjeux démographiques en Afrique subsaharienne, in Collection Sociétés africaines en mutation. Canada: Presses de l’Université du Québec; 2024, p. 504. [En ligne]. Disponible sur: https://extranet.puq.ca/media/produits/documents/4481_9782760560550.pdf#page=341.
- 16.Zhang S, Bird T, Kuepie M, Simelane S, Jhamba T, Snow R. Small area estimation based prediction methods in measurement of family planning indicators(a); 2020. p. 41.
- 17.Wan Z, Hook S, Hulley G. MOD11C3 MODIS/Terra Land Surface Temperature/Emissivity Monthly L3 Global 0.05Deg CMG V006. NASA EOSDIS Land Processes DAAC, 2015. 10.5067/MODIS/MOD11C3.006.
- 18.Darin E, Kuépié M, Bassinga H, Boo G, Tatem AJ, Reeve P. The population seen from space: when satellite images come to the rescue of the census. Population. 2022;77(3):437–64. [Google Scholar]
- 19.Druetz T, Ridde V, Kouanda S, Ly A, Diabaté S, Haddad S. Utilization of community health workers for malaria treatment: results from a three-year panel study in the districts of Kaya and Zorgho, Burkina Faso. Malar J. 2015;14:71. 10.1186/s12936-015-0591-9. 10.1186/s12936-015-0591-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bozdogan H. Model selection and Akaike’s Information Criterion (AIC): the general theory and its analytical extensions. Psychometrika. 1987;52(3):345–70. 10.1007/BF02294361. 10.1007/BF02294361 [DOI] [Google Scholar]
- 21.Hosmer DW Jr, Lemeshow S, Sturdivant RX. Applied logistic regression. New York: Wiley; 2013. [Google Scholar]
- 22.INSD et icf Maryland. Enquête sur les Indicateurs du Paludisme (EIPBF) 2017–18. INSD, PNLP, ICF Maryland, Ouagadougou et Rockville, Rapport final., 2018.
- 23.Bousema T, et al. Hitting hotspots: spatial targeting of malaria for control and elimination. PLOS Med. 2012;9(1):e1001165. 10.1371/journal.pmed.1001165. 10.1371/journal.pmed.1001165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carter R, Mendis KN, Roberts D. Spatial targeting of interventions against malaria. Bull World Health Organ. 2000;78:1401–11. [PMC free article] [PubMed] [Google Scholar]
- 25.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–9. 10.1111/j.0006-341x.1999.00652.x. 10.1111/j.0006-341x.1999.00652.x [DOI] [PubMed] [Google Scholar]
- 26.Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI. The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature. 2005;434(7030):214–7. 10.1038/nature03342. 10.1038/nature03342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hay SI, et al. A world malaria map: Plasmodium falciparum endemicity in 2007. PLoS Med. 2009;6(3):e1000048. 10.1371/journal.pmed.1000048. 10.1371/journal.pmed.1000048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mwangi TW, Fegan G, Williams TN, Kinyanjui SM, Snow RW, Marsh K. Evidence for over-dispersion in the distribution of clinical malaria episodes in children. PLoS ONE. 2008;3(5):e2196. 10.1371/journal.pone.0002196. 10.1371/journal.pone.0002196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bassinga H. Mortalité des enfants à partir des recensements de 1996 et 2006 au Burkina Faso: une analyse des inégalités provinciales et des effets individuels et contextuels. These de doctorat, Universitvé Joseph Ki-Zerbo, Ouagadougou, 2020.
- 30.Gallup JL, Sachs JD. The economic burden of malaria. Am J Trop Med Hyg. 2001;64(1_Suppl):85–96. 10.4269/ajtmh.2001.64.85. 10.4269/ajtmh.2001.64.85 [DOI] [PubMed] [Google Scholar]
- 31.Flahaut B. L’autocorrélation spatiale comme outil géostatistique d’identification des concentrations spatiales des accidents de la route. Cybergeo. 2001. 10.4000/cybergeo.4011. 10.4000/cybergeo.4011 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Malaria Indicators Survey dataset is available on the dhs program (https://dhsprogram.com) website and the General Population and Housing Census dataset is available at the National Institute of Statistics and Demography (INSD) in Burkina Faso.